Sexual and reproductive health in the United Kingdom urgently needs improving,1 and the government is developing the first integrated national strategy on sexual health.2,3 Theoretical models describing the main determinants of the incidence of sexually transmitted infections suggest that reducing the mean duration of infectiousness is likely to lead to substantially lower levels of disease.4 One way of achieving such reductions is by the earlier ascertainment of cases through screening for infection. The chief medical officer's expert advisory group on Chlamydia trachomatis has recently evaluated the evidence for chlamydia screening in the United Kingdom.5 In this report we summarise the main evidence addressed by the group and outline how its conclusions have been implemented through a screening pilot in two health authorities in England.
Summary points
Chlamydia trachomatis is the most common curable, bacterial, sexually transmitted disease in the United Kingdom
Detection outside genitourinary clinics is limited because the infection is largely asymptomatic
If untreated, infection can lead to severe reproductive morbidity in women
Screening programmes have produced a reduction in prevalence of infection and pelvic inflammatory disease
A pilot of opportunistic screening in England is described targeting mainly young women in primary and secondary healthcare settings
The problem
C trachomatis infection is the most common curable, bacterial, sexually transmitted infection in England.6 Since 1988, the number of cases seen in genitourinary medicine clinics in England has risen by 46% from 30 349 to 44 196 in 1998. The greatest rise over the past 10 years has been in the younger sexually active population (16-19 year old women and 20-24 year old men), and rates of infection are currently highest in these groups.7 Chlamydial infection is largely asymptomatic and, if untreated, the long term consequences of pelvic inflammatory disease, ectopic pregnancy, and tubal factor infertility are especially detrimental.8 Although professional awareness of the infection is rising, genitourinary medicine clinics remain the only clinical setting that undertakes nationwide systematic screening. Less than 10% of prevalent infections are thought to be diagnosed in genitourinary medicine clinics.9 Substantial numbers of people are therefore untreated and remain at risk of developing severe complications.
The questions
There are several questions that relate to this problem. Firstly, is screening for chlamydia an effective intervention strategy? Secondly, if so, who should be targeted and in which clinical settings should they be screened? And, thirdly, what is the preferred method of screening and will it be feasible and cost effective in Britain?
The evidence
Evidence for effectiveness of screening for chlamydia
Several case studies10,11 and one randomised controlled trial12 have shown that screening significantly reduces the prevalence of genital tract infections and pelvic inflammatory disease in women. Since 1985 in Sweden, a countrywide testing initiative for chlamydia has been implemented in various health settings including primary care and specialist clinics. Rates of testing increased each year from 1985 to 1991, and a corresponding decrease occurred in the number of cases diagnosed; in one county, the number of cases had fallen to 40% of initial levels by 1991.10 In 1986, a state-wide screening initiative began in family planning clinics in Wisconsin, United States, using risk factors to determine who was screened.11 By 1990, a 53% decrease in prevalence was seen. In a large randomised trial of 2607 women, 1009 were assigned to screening and the rest to usual care.12 At the end of 12 months' follow up, there were 33 cases of pelvic inflammatory disease in the control group and nine in the screened women, a 56% reduction in incidence of disease.
Who should be screened and where?
Prevalence of infection varies considerably in differ- ent populations (range 1%-29%).5 Prevalence is consistently higher in certain groups (such as women attending genitourinary clinics (median prevalence 16%) and clinics for termination of pregnancy (8%)) than in others (such as people tested in general practice and family planning clinics (5%)). The number of infections is still rising, and it seems unlikely that the current restricted systematic screening will have a great effect on prevalence and incidence because the general population makes limited use of genitourinary medicine clinics.13 Future screening will have to be based in more widely used health settings.
Several studies have identified various demographic or behavioural risk factors that are associated with infection, including younger age (particularly under 25 years), multiple partners, recent change in partner, single marital status, ethnic group, low school leaving age, genital symptoms, or the presence of another sexually transmitted infection.5 Young age and recent change in sexual partner are the most commonly reported risk factors for infection. On this basis, the expert advisory group concluded that in addition to testing of all symptomatic patients and those at higher risk (people attending genitourinary medicine clinics and women seeking termination of pregnancy), the evidence supported opportunistic screening of the general population. The group concluded that screening should be offered to sexually active women under 25 and also to those over 25 with a new sexual partner or who have had two or more partners in the past year. It advocated the use of general practice and family planning clinics for screening and also stressed the importance of notifying partners, which should be undertaken in collaboration with genitourinary medicine clinics.
Methods of screening and feasibility issues
The advisory group recommended opportunistic screening rather than a call-recall system based on age or sex. An age based call-recall system could be very inefficient because resources are wasted in inappropriately contacting people who are not sexually active. In addition, a recent study in Amsterdam showed that opportunistic screening for chlamydia can achieve higher participation rates than postal invitations and identify greater numbers of infections.14 Economic analyses have shown that the proposed model of screening will be cost effective, and modelling suggested that screening women only (when men are identified and treated through notification of partners) is the most cost efficient approach.15
Implementation
The proposed screening programme would demand changes in clinical practice and closer alliances between health services. In the light of the evidence reviewed and with advice from the National Screening Committee, the Department of Health commissioned a pilot study to determine the logistic implications of opportunistic screening. The pilot will take place for one year and is currently under way in two sites, Portsmouth and the Wirral.
Objectives of pilot scheme
The main objectives of the pilot are to assess the feasibility and acceptability of opportunistic screening in a range of healthcare settings, including primary and secondary care. Although the screening pilot will aim to estimate the true costs of opportunistic screening, it has not been designed to assess the effect of screening on long term morbidity. This will require either a randomised control trial or the development of new techniques that will permit the monitoring of trends in pelvic inflammatory disease.
Inclusion criteria
A targeted approach to screening has been adopted, focusing on sexually active young people (16-24 year olds) attending testing sites. Women will be offered screening in primary care settings (general practice and family planning) and certain defined specialist services—for example, women's services in hospitals, termination of pregnancy, and genitourinary medicine clinics—whereas men will be offered screening only at genitourinary medicine and young people's sexual health clinics. The advisory group proposed that screening be focused predominantly on women partly because women use health services more often and so form a more accessible population. However, the pilot is including young men attending clinics as they form an easy to reach subgroup who are also at higher risk of infection. The inclusion of men in these settings will foster greater recognition of male responsibility in sexual health issues and will encourage sharing of responsibility for sexual health, a burden currently placed mainly on women.16 This approach will also help to assess the feasibility and cost efficiency of extending full screening to both sexes.
Screening process
All screening for chlamydia in the pilot programme will be by a ligase chain reaction test on a first catch urine sample. Use of urine samples, rather than the more invasive endocervical or endourethral swabs that were required for older screening tests such as enzyme linked immunosorbent assay (ELISA), should greatly increase acceptability and uptake of screening. A recent survey in the pilot areas found that 95% of 16-24 years olds were willing to have a urine test for chlamydia during a routine visit to their general practitioner.17 After screening, patients will be informed of their results from a local coordinating office and will be able to discuss the implications of the results with specially trained research nurses. People who have positive results will be referred to local genitourinary medicine clinics for treatment, notification of partners, and further testing for other infections. Patients who do not wish to be referred to clinics will have the option to be treated where they were tested. In these cases, research nurses working within the coordinating offices will liaise with clients to ensure that partners are notified.
General issues
Several of the detailed issues that need to be addressed within the pilot, including resource allocation and implications of screening for health insurance have been previously highlighted.18 All resources (including cost of treatment) required for screening have been provided from a central pilot budget, and participating centres are also paid for each test completed to reflect increased demands on staff time. The actual costs of screening will be estimated as part of the overall evaluation of the pilot.
Before the start of the pilot, general practitioners expressed concerns about the effect of screening for a sexually transmitted infection on future insurance premiums. The Department of Health discussed this issue with the Association of British Insurers, and the trend in future policies is towards omitting specific questions regarding sexually transmitted infections. However, practice varies between companies; some insurers say that they find it relevant to know when an applicant has a series of sexually transmitted infections. During the pilot, general practitioners were advised to consider adding a caveat that the test was carried out through a screening programme and not because of perceived risk or history of the individual.
Screening programmes should allow individuals to make their own decisions and assess their personal health costs and benefits before accepting an offer of screening.19 It may be unacceptable to offer screening during a consultation that is not for a sexual health reason, as such an offer could affect communication about the original purpose of the consultation. Although uptake rates will be a key measure of the success of the pilot, measures of the public perception of the acceptability and benefits of screening will also be important. All people offered screening will be provided with a comprehensive information booklet and have the opportunity to discuss the implications of testing with trained staff before making their decision. The pilot includes an independent component (using both qualitative and quantitative techniques) to determine and monitor the emotional impact and acceptability of screening in both sexes. It will also evaluate the effect of the education materials provided to the public and professionals.
Conclusions
Opportunistic testing is a well recognised mode of screening.19 However, concerns have been raised regarding its use in screening for genital chlamydial infection.20 Opportunistic screening is likely to offer greater opportunity for young and behaviourally vulnerable individuals to ask questions about the disease, its mode of acquisition, and the implications of a positive test result than would postal based screening. It should also have lower administrative costs. The methods used in the pilot require changes to current clinical practice and closer collaboration between primary care and specialist services. This provides an opportunity for new partnerships to be formed and facilitates a more integrated approach to health care. In many ways, it heralds the approach that is required to manage the wide variety of sexual health issues that confront us today.
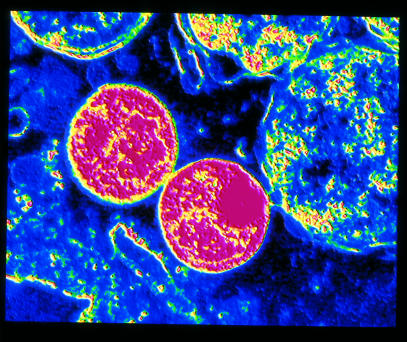
Figure.
ALFRED PASIEKA/SCIENCE PHOTO LIBRARY
Transmission electron micrograph of C trachomatis: a screening programme is being piloted in England
Footnotes
Funding: Department of Health.
Competing interests: None declared.
References
- 1.Nicoll A, Catchpole M, Cliffe S, Hughes G, Simms I, Thomas D. Sexual health of teenagers in England and Wales analysis of national data. BMJ. 1999;318:1321–1322. doi: 10.1136/bmj.318.7194.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Department of Health. First ever government strategy on sexual health launched. London: DoH; 1999. . (Press release 1999/0166, 23 March.) [Google Scholar]
- 3.Department of Health. Sexual health strategy: Professor Adler to lead development of sexual health. London: DoH; 1999. . (Press release 1999/0456, 21 July.) [Google Scholar]
- 4.Yorke J, Hethcote H, Nold A. Dynamics and control of the transmission of gonorrhoea. Sex Transm Dis. 1978;5:51–56. doi: 10.1097/00007435-197804000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Chief Medical Officer's Expert Advisory Group. Main report of the CMO's expert advisory group on Chlamydia trachomatis. London: Department of Health; 1998. [Google Scholar]
- 6.Hughes G, Simms I, Rogers P, Swan A, Catchpole M. New cases seen at genitourinary medicine clinics: England 1997. Commun Dis Rep. 1998;8(suppl):S1–12. [PubMed] [Google Scholar]
- 7.Lamagni T, Hughes G, Rogers P, Paine T, Swan AV, Catchpole M. New cases seen at genitourinary medicine clinics: England 1998. Commun Dis Rep. 1999;9(suppl):S1–12. [PubMed] [Google Scholar]
- 8.Paavonen J, Lehtinen M. Chlamydial pelvic inflammatory disease. Hum Reprod Update. 1996;2:519–529. doi: 10.1093/humupd/2.6.519. [DOI] [PubMed] [Google Scholar]
- 9.Renton A, Taylor-Robinson D. The need for an assessment of health technology for screening for Chlamydia trachomatis in the population. Leeds: NHS Executive; 1994. [Google Scholar]
- 10.Herrmann B, Johnsson A, Mårdh P-A. A retrospective study of efforts to diagnose infections by Chlamydia trachomatis in a Swedish county. Sex Transm Dis. 1991;18:233–237. doi: 10.1097/00007435-199110000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Addiss DG, Vaughn ML, Ludka D, Pfister J, Davis JP. Decreased prevalence of Chlamydia trachomatis infection associated with a selective screening programme in family planning clinics in Wisconsin. Sex Transm Dis. 1993;20:28–34. doi: 10.1097/00007435-199301000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Scholes D, Stergachis A, Heidrich F, Andrilla H, Holmes KK, Stamm W. Prevention of pelvic inflammatory disease by screening for cervical chlamydial infection. N Engl J Med. 1996;334:1362–1366. doi: 10.1056/NEJM199605233342103. [DOI] [PubMed] [Google Scholar]
- 13.Johnson A, Wadworth J, Wellings K, Field J. Sexual attitudes and lifestyles. Oxford: Blackwell; 1994. [Google Scholar]
- 14.Van den Hoek J, Mulder-Folkerts D, Coutinho R, Dukers N, Buimer M, van Doornum GJJ. Opportunistic screening for genital infections with Chlamydia trachomatis among the sexually active population of Amsterdam. 1. Over 90% participation and almost 5% prevalence. Ned Tijidschr Geneeskd. 1999;143:668–672. [PubMed] [Google Scholar]
- 15.Turner H, Townshend J. Cost effectiveness: modelling for chlamydia screening. In: Chief Medical Officer's Expert Advisory Group. Main report of the CMO's expert advisory group on Chlamydia trachomatis. London: Department of Health, 1998. (Chapter 11.)
- 16.Duncan B, Hart G. Sexuality and health: the hidden costs of screening for Chlamydia trachomatis. BMJ. 1999;318:931–933. doi: 10.1136/bmj.318.7188.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Opinion Polls Social and Political. Health evaluation survey. London: NOP; 1999. . (JN430458.) [Google Scholar]
- 18.Boag F, Kelly F. Screening for Chlamydia trachomatis: the case for screening is made but much detail remains to be worked out. BMJ. 1998;316:1474. doi: 10.1136/bmj.316.7143.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Screening Committee. First report of the National Screening Committee. Health Departments of the United Kingdom; 1998. [Google Scholar]
- 20.Macleod J, Davey Smith G. Chlamydia screening can have high take-up rates if right methodology is used. BMJ. 1999;319:188–189. doi: 10.1136/bmj.319.7203.188b. [DOI] [PMC free article] [PubMed] [Google Scholar]