Abstract
Background:
In the US, low-income individuals generally smoke more than high-income individuals. However, detailed information about how smoking patterns differ by income, especially differences by birth cohort, are lacking.
Methods:
Using the National Health Interview Survey (NHIS) 1983-2018 data, individual family income was calculated as a ratio of the federal poverty level (FPL). Missing income data from 1983-1996 were imputed using sequential regression multivariate imputation. Age-period-cohort models with constrained natural splines were used to estimate annual probabilities of smoking initiation and cessation, and smoking prevalence and intensity by gender and birth cohort (1900 to 2000) for five income groups: <100%, 100%-199%, 200%-299%, 300%-399%, and ≥400% of the FPL. Analysis was conducted in 2020–2021.
Results:
Across all income groups, smoking prevalence and initiation probabilities are decreasing by birth cohort while cessation probabilities are increasing. However, relative differences between low- and high-income groups are increasing markedly, such that there were greater declines in prevalence among those in high-income groups in more recent cohorts. Smoking initiation probabilities are lowest in the ≥400% FPL group for males across birth cohorts; whereas for females, this income group has the highest initiation probabilities in older cohorts but the lowest in recent cohorts. People living below the FPL have the lowest cessation probabilities across cohorts.
Conclusions:
Smoking prevalence has been decreasing in all income groups; however, disparities in smoking by family income are widening in recent birth cohorts. Future studies evaluating smoking disparities should account for cohort differences. Intervention strategies should focus on reducing initiation and improving quit success among low-income groups.
Introduction
Cigarette smoking has declined considerably in the US for the general population.1 From 1997 to 2018, adult smoking prevalence fell from 24.7% to 13.7%, a 44% reduction.2 However, the decrease in smoking prevalence differed greatly by socioeconomic status.2–5 For instance, during that same time period, smoking prevalence among people living at or above the poverty level decreased from 24.6% to 12.8%, a 48% reduction, compared to only a 32% reduction among those living below the poverty level for whom smoking fell from 33.3% to 22.6%.2 The association between higher cigarette smoking and lower income level continues today;6 adult cigarette smoking prevalence in 2019 was 21.4%, 15.7%, 11.4%, and 7.1% among people whose annual household income was <$35,000, $35,000-$74,999, $75,000-$99,999, and ≥$100,000, respectively.7 Thus despite overall reductions in smoking due to tobacco control policies, high-income groups are benefiting more from this public health progress than low-income groups.
Differences in smoking trends by sociodemographic factors may be partially due to varying smoking cessation responses to tobacco control policies. For example, a previous study reported that young female smokers quit at higher rates than young male smokers in the late 1960s through the mid 1970 due to public health campaigns that highlighted the impacts of smoking on pregnancy and birth outcomes.8 The higher smoking prevalence among low-income groups is due in part to lower cessation rates compared to high-income groups.1,9–12 A longitudinal study for US adults aged ≥18 years showed that the odds of abstinence from cigarette use for 30+ days is higher among adults with income ≥300% of the federal poverty level (FPL) compared to the adults with income below 300% FPL (24.4% vs.13.7%; AOR= 1.9, 95% CI=1.4–2.7).13 Another study based on the Tobacco Use Supplement to the Current Population Survey from 2014-2019 showed that people with an annual income lower than $25,000 are less likely quit smoking compared to people with higher annual income.14 Differences in patterns of smoking initiation, duration, and smoking intensity (cigarettes per day) likely also explain smoking prevalence disparities, though differences by income in these smoking measures have been studied in less detail.11,12,15–18
Smoking disparities by socioeconomic status have commonly been evaluated using levels of educational attainment as a measure of status, rather than family income.19 However socioeconomic status encompasses both family income and education level—in addition to a range of other attributes that are connected to social class—and are not interchangeable as indicators of socioeconomic status.20,21 Besides, there exists a potential causal link between education and smoking, where adolescent smoking could lead to lower educational attainment in adulthood.22,23 Family income can also be a useful metric for socioeconomic status as it captures the level of access to health care, improved living conditions, and other psychosocial resources.24,25 Income furthermore determines eligibility for government social services and benefits, including Medicaid coverage, based on whether individuals are below or above the FPL.24,25 Thus, analyses of smoking disparities by income facilitate a more comprehensive understanding of socioeconomic differences in health behaviors and in access to care,26 and how these translate into disparities in long-term health outcomes.3,27–29 In particular, the risk of smoking-related diseases, such as lung cancer, COPD, and cardiovascular disease has been declining more rapidly among high-income compared to low-income individuals, thereby widening overall tobacco-related health disparities by socioeconomic status in recent years.3,27,29,30
Previous studies have shown that age-specific smoking patterns for some US populations vary dramatically by birth cohort.1,31–38 In particular, Holford et al. showed that cohort patterns in US smoking prevalence, initiation, cessation, and intensity vary considerably by gender36 and race.39 Another study by Escobedo et al. found variations in smoking prevalence trends by education, with decreases among those with higher educational attainment, but not in those lower educational attainment.34 Smoking trends may also be determined by birth cohort specific smoking patterns by income level, but this has not been examined yet. This study focus on evaluating gender and birth cohort specific smoking patterns by income level in the US population. Using a methodology previously developed by the Cancer Intervention and Surveillance Modeling Network-Lung Working Group (CISNET-LWG) investigators,36,39 age-specific smoking prevalence, initiation probabilities, cessation probabilities, mean cigarettes per day, mean smoking duration, and mean pack-years were estimated by gender and birth cohort for five income groups, categorized by family income relative to the FPL. The resulting smoking parameters facilitate a more in-depth understanding of variations of smoking patterns across income groups and their implications for health disparities when used to inform simulation models of smoking and smoking related morbidity and mortality.
Methods
Smoking and Family Income Data
Data were obtained from the NHIS for smoking status (i.e., current, former, never smoking; 1983, 1985, 1987, 1990-1995, 1997-2018), age at which respondents started smoking regularly (1987, 1988, 1992, 1995, 1997-2018), years since quit smoking (1983, 1985, 1990, 1992, 1994, 1995, 1997–2018), and cigarettes smoked per day (1983, 1985, 1988, 1990-1995, 1997-2018). Individuals who smoked 100 cigarettes or more in their lifetime were classified as current smokers if they currently smoked every day or some days at the time of survey completion, and classified as former smokers if they did not currently smoke at all at the time of the survey. Data from the NHIS 2019 and 2020 were excluded because the survey design was substantially changed in 2019.40
Family income data were also obtained from the NHIS from 1983-2018. To estimate smoking patterns by the level of family income and to avoid issues of rising income and inflation, individuals were categorized according to their family income-to-poverty ratio, using the FPL for each year and family composition. The FPL is defined by the Census Bureau as the minimum amount of gross income that a family needs for survival, and it varies by family size and structure (i.e., number of adults and related children under 18 years of age).41 The FPL is adjusted for inflation annually. For this analysis, five categories of family income-to-poverty ratio were used: below poverty (<100% FPL), near poverty (100%-199% FPL), 200%-299% FPL, 300%-399% FPL, and ≥400% FPL.
Imputation for continuous family income
Detailed family income in the NHIS is often subject to high rates of missing values due to the sensitive nature of income-related questions for survey respondents. To address this shortcoming, the NHIS provides five imputed datasets for the family income-to-poverty ratio for 1997-2018. For these, missing continuous family incomes were imputed by NHIS investigators using the sequential regression multivariate imputation (SRMI) method.42 Prior to 1997, only categorical family income data were included in the NHIS. Following a similar SRMI approach, continuous family income for NHIS years 1982-1996 was imputed by calculating a family income-to-poverty ratio for each survey individual by dividing the continuous family income by the corresponding year FPL, accounting for the individual’s family size and structure. Five imputed datasets for family income-to-poverty ratio were generated for years 1982-1996. Additional details regarding the continuous family income imputation procedure for NHIS 1982-1996 are provided in the supplement (S1 Text).
Smoking parameter estimation
Using age-period-cohort (APC) models with constrained natural splines,36,39 annual probabilities of smoking initiation, cessation, and intensity (cigarettes per day or CPD) by gender and cohort (1900 to 2000 birth cohorts) were estimated separately for each income group. The underlying analysis framework assumes that individuals who never smoked can transition into current smoking status (smoking initiation), and individuals with current smoking status can then transition into former smoking status (smoking cessation). The estimated rates or probabilities from the APC models were presented, which are identifiable and not affected by the known identifiability issue of these models.43
Smoking initiation probabilities were estimated using data on respondents’ reported age of initiation. For each gender and birth cohort, age-specific initiation probabilities were estimated as conditional probabilities of smoking initiation among individuals who had never smoked up to the time of the interview. To address differential mortality between individuals who smoked and individuals who did not smoke up to the time at interview, as well as recall bias in self-reported age at smoking initiation, the cumulative initiation probabilities by cohort were calibrated to match the estimated ever smoking prevalence at age 30. The latter was obtained by fitting an age-period-cohort model to ever smoking data from all surveys. Age-specific cessation probabilities were estimated as conditional probabilities of quitting for individuals who reported current smoking, with the minimum age of quitting set as age 15. Smoking cessation is based on having quit for at least 2 years, thereby minimizing the need to account for relapse among recent quitters. Risk of relapse is higher immediately following a quit attempt, but permanent abstinence is high among former smokers who quit more than 2 years.44–46 In the NHIS surveys, age is top coded at age 85, thus the cessation probabilities were set as constant beyond age 85.
For estimating smoking intensity by age for each gender and birth cohort, CPD was classified into six categories (approximate mean CPD of each category): CPD≤5 (3); 5< CPD≤15 (10); 15<CPD≤25 (20); 25<CPD≤35 (30); 35<CPD≤45 (40); and 45<CPD (60). Age- and cohort-specific probabilities for each dose category was estimated by a cumulative logistic age-period-cohort model using constrained natural splines for temporal effects.
For each birth cohort, the current smoking prevalence at a given age was estimated by multiplying the ever-smoking prevalence by the cumulative proportion of individuals who smoked in the cohort who had not quit smoking at that age. Former smoking prevalence was estimated by subtracting the proportion of current smoking from the proportion of ever smoking. Never smoking prevalence was estimated by the complement of ever smoking prevalence. Based on the estimated distribution of smoking initiation, current smoking prevalence, former smoking prevalence, and mean cigarettes per day, the mean smoking duration and mean pack-years were also estimated by age, gender, and birth cohort.
All smoking parameters for age, period, and cohort effects were estimated separately for each of the five income-to-poverty ratio groups: below poverty (<100% FPL), near poverty (100%-199% FPL), 200%-299% FPL, 300%-399% FPL, and ≥400% FPL, using the PROC SURVEYLOGISTIC in SAS 9.4, accounting for sample weights.
Results
The distribution of US adults across income groups from NHIS 1983-2018 is shown in Supplement Figure S1. The percentage of the population living below the FPL is quite stable across years in both females and males, approximately 10%. The percentage of the population in the highest income (≥400% FPL) group has been growing over time from 1983 to 2018, increasing from 24% to 40% of females and from 28% to 44% of males.
Smoking initiation
Figure 1 shows age-specific initiation probabilities by the family income-to-poverty ratio for five selected birth cohorts (1910, 1930, 1950, 1970, 1990) by gender. In general, smoking initiation increases during adolescence and decreases during young adulthood, with very little or no initiation occurring beyond age 30. Differences in initiation between income groups were relatively modest in earlier birth cohorts, but more prominent in recent cohorts. Among females, the highest income (≥400% FPL) group had the highest initiation probabilities in older birth cohorts but the lowest in recent birth cohorts. On the other hand, among males, the ≥400% FPL group has the lowest initiation across all birth cohorts. In earlier birth cohorts, the below poverty (<100% FPL) group had the lowest initiation probabilities compared to other income groups, but with more recent birth cohorts this group had the highest or second highest initiation probabilities for both genders. The age at peak initiation increases with the level of family income, where lower income groups have earlier ages at smoking onset. Figure S2 shows age-specific initiation probabilities for additional cohorts by calendar year, comparing each income group to the highest income (≥400% FPL) group. Among females, the initiation probabilities increased through the 1940-1960 birth cohorts, before decreasing in later birth cohorts. Conversely, the male initiation probabilities decreased by birth cohort since the early 1900s across all income groups. Initiation probabilities were much higher in males compared to females in early birth cohorts but became similar by gender with more recent birth cohorts across all income groups.
Figure 1.
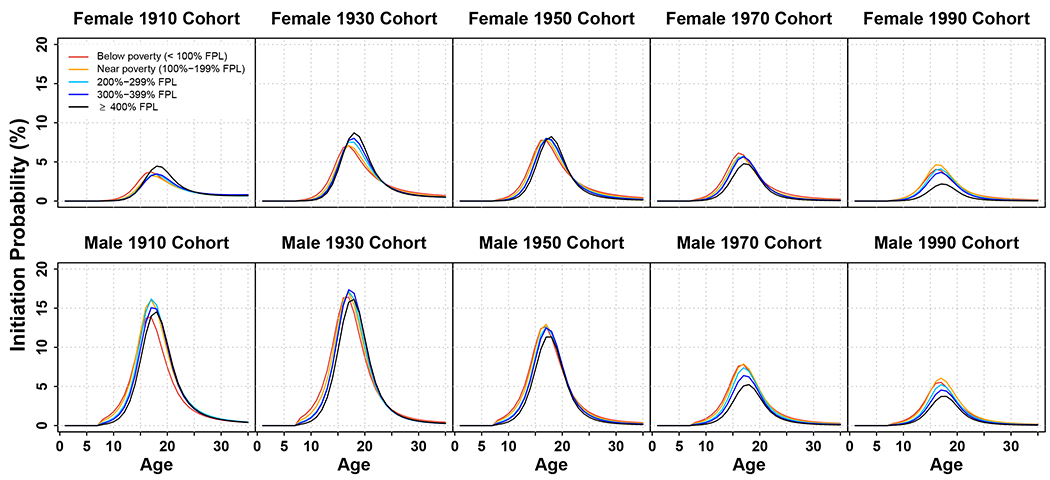
Age-specific smoking initiation probabilities (percentage) for selected birth cohorts by family income-to-poverty ratio and gender (females – top panels, males – bottom panels). Lines represent the initiation probabilities for Below poverty (<100% FPL, red), Near poverty (100%-199% FPL, orange), 200%-299% FPL (sky blue), 300%-399% FPL (blue), and ≥400% FPL (black). FPL=Federal Poverty Level. An interactive version of this figure’s data can be found at: https://apps.cisnetsmokingparameters.org/income/
Smoking cessation
In general, smoking cessation probabilities increased with age, and declined slightly at older ages. For both genders, there was a clear positive gradient in age-specific cessation probabilities by level of family income, especially in recent birth cohorts: cessation probabilities were highest in the ≥400% FPL group and lowest in the below poverty group (Figure 2). Differences in cessation probabilities by income group became larger with more recent birth cohorts. Figure 2 shows that males in the ≥400% FPL group generally have higher cessation probabilities than females in the same income group across birth cohorts. However, there were no major gender differences in cessation for each of the other income groups except in the 1910 birth cohort. Cessation probabilities increased by birth cohort across all income groups in both females and males (Figure S3).
Figure 2.
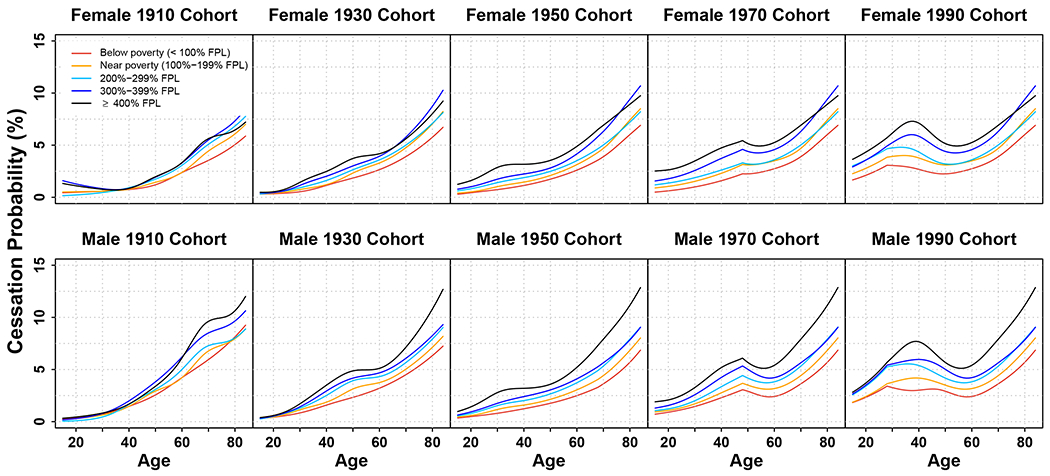
Age-specific smoking cessation probabilities (percentage) for selected birth cohorts by family income-to-poverty ratio and gender (females – top panels, males – bottom panels). Lines represent the initiation probabilities for Below poverty (<100% FPL, red), Near poverty (100%-199% FPL, orange), 200%-299% FPL (sky blue), 300%-399% FPL (blue), and ≥400% FPL (black). FPL=Federal Poverty Level. An interactive version of this figure’s data can be found at: https://apps.cisnetsmokingparameters.org/income/
Current smoking prevalence
Across all income groups, smoking prevalence increased through young adulthood and gradually declined with age for both females and males. For both genders, there was a clear negative gradient in age-specific current smoking prevalence by income group in all selected birth cohorts, except in the 1910 birth cohort (Figure 3); across birth cohorts and ages, smoking prevalence is highest in the below poverty group, followed by near poverty, 200%-299% FPL, 300%-399% FLP, and lowest in the ≥400% FPL group. In Figure S4, similar to initiation trends, smoking prevalence in females increased through the 1940-1960 birth cohorts, then decreased with later birth cohorts, with modest variation by income group. For males across all income groups, prevalence has been decreasing by birth cohort since the early 1900s birth cohorts. Smoking prevalence was much higher among males than females in early birth cohorts, but gender differences in smoking prevalence have decreased in recent birth cohorts.
Figure 3.
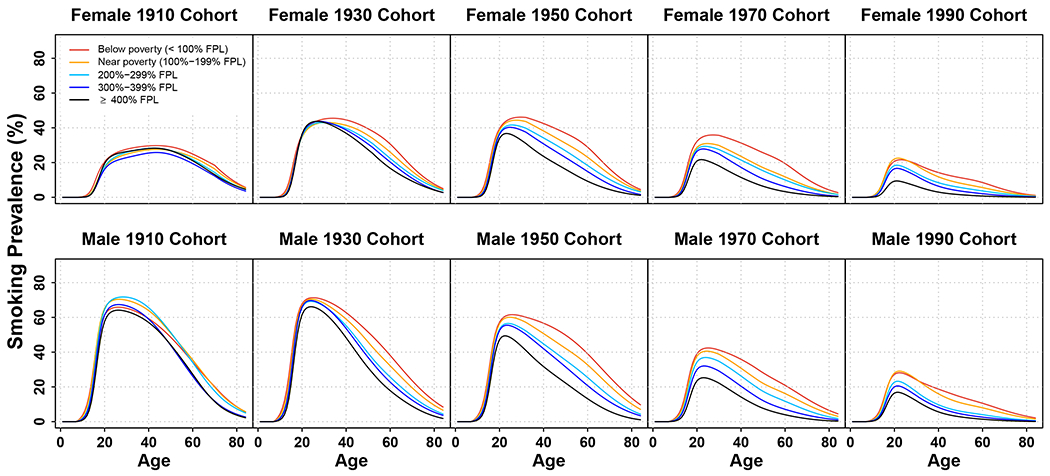
Age-specific smoking prevalence (percentage) for selected birth cohorts by family income-to-poverty ratio and gender (females – top panels, males – bottom panels). Lines represent the initiation probabilities for Below poverty (<100% FPL, red), Near poverty (100%-199% FPL, orange), 200%-299% FPL (sky blue), 300%-399% FPL (blue), and ≥400% FPL (black). FPL=Federal Poverty Level. An interactive version of this figure’s data can be found at: https://apps.cisnetsmokingparameters.org/income/
Mean cigarettes per day among individuals who currently smoke
Figure 4 shows age-specific mean cigarettes per day (CPD) among individuals who currently smoke by income group and gender for five selected birth cohorts. In early birth cohorts, the mean CPDs were highest in the ≥400% FPL group and lowest in the below poverty group. However, in recent birth cohorts, the mean CPDs were lowest in the ≥400% FPL group and highest in the below poverty and near poverty groups. In early birth cohorts (1910 and 1930), the mean CPDs increased until around age 55 and decreased thereafter. In contrast, for the 1950 birth cohort, the peak occurred around age 40. Mean CPDs became relatively flat, slightly decreasing by age, in recent birth cohorts. This pattern was consistent across all income groups and genders. In general, mean CPDs decreased by birth cohort for both genders, and were higher in males compared to females in all income groups (Figure S5).
Figure 4.
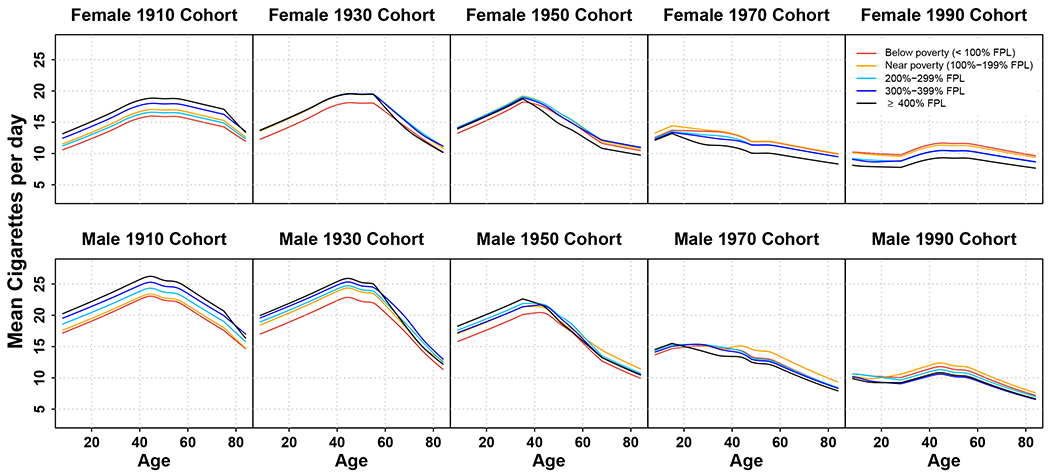
Age-specific mean cigarettes per day among current smokers for selected birth cohorts by family income-to-poverty ratio and gender (females – top panels, males – bottom panels). Lines represent the initiation probabilities for Below poverty (<100% FPL, red), Near poverty (100%-199% FPL, orange), 200%-299% FPL (sky blue), 300%-399% FPL (blue), and ≥400% FPL (black). FPL=Federal Poverty Level. An interactive version of this figure’s data can be found at: https://apps.cisnetsmokingparameters.org/income/
Mean duration of cigarette use among individuals who smoke
Across all selected birth cohorts except for the 1910 birth cohort, there was a negative gradient in the age-specific mean smoking duration by the level of family income, where smoking duration was shorter with higher income (Figure S6); the mean smoking duration was longest in the below poverty group, followed by near poverty, 200%-299% FPL, 300%-399% FLP, and shortest in the ≥400% FPL group. Figure S6 shows that in general the mean smoking duration has been decreasing by birth cohort in all income groups, and that males had higher mean smoking duration compared to females in early birth cohorts, but differences by gender have narrowed with recent birth cohorts.
Mean pack-years among individuals who smoke
Figure S7 shows a negative gradient in age-specific mean pack-years by the level of family income in relatively recent birth cohorts for both genders. Similar to patterns in smoking duration, mean pack-years decreased by birth cohort in all income groups and for both genders, with males having higher mean pack-years compared to females in early birth cohorts, but reaching similar levels in recent birth cohorts (Figure S7).
Discussion
This is the first study to provide a comprehensive analysis of smoking behaviors by family income for US birth cohorts. Previous studies have looked at birth cohort smoking patterns by gender,1,31,36,39,47 race,39 or education47 in the US population, however, income group differences in smoking patterns by birth cohort have not been studied. This study extends the CISNET age, period, cohort modeling methodology to estimate smoking behaviors—smoking initiation, cessation, and intensity—by family income level in the US. Smoking prevalence and initiation probabilities have been decreasing by birth cohort starting with the early 1900s cohorts in males and with the 1940-1960 cohorts in females, although the extent of decrease varied across income groups. Cessation probabilities have been increasing by birth cohort in all income groups, especially young adult males and females. For all income groups, mean cigarettes per day, smoking duration, and pack-years have been decreasing by birth cohort. However, differences in smoking initiation and cessation probabilities between income groups have been widening in more recent birth cohorts, resulting in increasing disparities in smoking prevalence by income level. These findings are consistent with other studies showing differences in smoking prevalence and cessation probability by income level to be widening in recent years.4,7,9,13
Findings from this study illustrate the social transition of smoking behaviors from high- to low-income groups as it varies by gender.48 While males from the lowest income group had the highest smoking levels since early cohorts covered in this analysis, females’ smoking progressively shifted from higher-income to lower-income groups with increasing time/birth cohorts. This social transition increases smoking disparities and progressively concentrates the disproportionate burden of smoking-related morbidity and mortality on the lowest income population. It is particularly problematic because low-income groups have the least access to health care resources and are most vulnerable to housing and food insecurity, all of which exacerbate risks to health.49,50 It is plausible that a similar cohort transition of smoking behaviors from higher-income to lower-income groups also would have been observed among males if data from even earlier cohorts were available.
Strengths and Limitations
In this study, the NHIS imputation methods were used and extended to fill in gaps in historical income data, addressing the absence of continuous income data prior to 1997. This allowed using NHIS data from NHIS 1983-2018. Future researchers that wish to use this imputation methodology to analyze the relationship between family income and other NHIS outcomes and behaviors besides smoking can refer to the supplement for details. Another methodological strength is the use of the CISNET-LWG approach which jointly estimates historical age-period-cohort specific initiation and cessation probabilities with the prevalence of ever, never, current and former smoking, resulting in consistent estimates across smoking behaviors.
This study has some limitations. The analysis used a simplifying assumption that categorized recent quitters as current smokers unless they had quit for at least 2 years. Consequently, more complex smoking trajectories, such as repeated quitting and relapse back to smoking in one lifetime, are not evaluated. The smoking parameters were estimated for age, gender, and birth cohort, separately for each income group, without adjusting for additional potential confounding factors, such as race/ethnicity, education, or US region.1,51,52 The analysis focuses on national data and trends; however, smoking patterns are a reflection of policy environments shaped at the state and local levels, and therefore vary geographically. Although both family income and educational attainment are different aspects of socioeconomic status, they are also highly correlated.20,21 Another limitation is that the analysis focused exclusively on cigarette smoking, but the landscape of tobacco use has changed dramatically with the emergence of e-cigarettes in recent years.1 Recent changes in smoking initiation or cessation that may be associated with rising e-cigarette use are still not fully captured by the NHIS data, including potentially different changes by income level. Nonetheless, this analysis found considerable decreases in smoking initiation in recent cohorts, particularly for high-income groups, which could be related to replacement of cigarette smoking by e-cigarettes among youth and young adults.53,54 Variations in use of other tobacco products by income, particularly cigars and cigarillos, might also be contributing to differences in cigarette smoking patterns and trends across income groups.55 Last, this analysis defined income levels according to the census federal poverty line, which ignores geographical differences in cost of living and purchasing power across regions, states and localities.
Implications
Cohort-specific smoking patterns may reflect changes in both the tobacco control policy and tobacco product landscapes over time. People born in 1950 vs. 1990 were exposed to very different sets of social norms and public health policies during key life stages for initiation (adolescence, young adulthood) and cessation (middle age, older adulthood). For instance, the strong decreases in smoking initiation and prevalence across income groups since the 1950 birth-cohort likely reflects the continuous impact of strengthened tobacco control policies and regulations implemented since the 1964 Surgeon General’s Report.
Estimates of age-specific initiation and cessation probabilities, and the distribution of cigarettes per day by birth cohort for the overall US population have been used as input parameters for simulation models of smoking.36,39,56–59 These models have been used to examine the potential impact of health intervention strategies such as tobacco policies on smoking and lung cancer,37,57–61 the benefits and harms of different cancer screening strategies on health outcomes,62–66 as well as their effectiveness and cost-effectiveness.67–69 This study provides smoking parameters for different income groups, which facilitates similar analyses to examine the impact of prevention strategies on health outcomes by income level.
Income-based analysis of smoking disparities are important because of vulnerability to smoking and related morbidity and mortality in low-income populations. Research has revealed tobacco industry targeting of low-income individuals70,71 and the larger presence of tobacco advertising and tobacco product availability in low-income neighborhoods.72,73 High rates of smoking initiation and low rates of quitting among low-income group are especially concerning. Targeted interventions, such as cell phone-delivered counseling, have shown promise for improving quit success for smokers living in poverty.74 Efforts to reduce tobacco retailer density may have the potential to address smoking among low-income youth, who are disproportionately exposed to both tobacco advertising and retail outlets in their neighborhoods.73,75–77 This study highlights persistent disparities by income and changing trends by birth cohort. The adoption of effective smoking intervention strategies specifically for low-income groups will be important to reduce tobacco-related health disparities.
Conclusions
Smoking prevalence has been decreasing in all income groups, but disparities in smoking by family income are widening in recent birth cohorts. These trends are shaped by the social transition of harmful smoking behaviors from high-income groups in earlier cohorts to low-income groups in recent cohorts. Future studies evaluating smoking disparities should take into account these differences by birth cohort. Intervention strategies should focus on decreasing initiation and improving quit success among low-income groups.
Supplementary Material
Conflict of interest statement:
This project was funded through National Cancer Institute (NCI) grants U01CA199284 & U01CA253858. The study sponsor had no role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Footnotes
Financial disclosure: No financial disclosures were reported by the authors of this paper.
References
- 1.U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014. https://www.ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf. Accessed December 25, 2021. [Google Scholar]
- 2.IPUMS NHGIS | National Historical Geographic Information System. https://www.nhgis.org/. Accessed January 13, 2022.
- 3.Odutayo A, Gill P, Shepherd S, et al. Income Disparities in Absolute Cardiovascular Risk and Cardiovascular Risk Factors in the United States, 1999-2014. JAMA Cardiol. 2017;2(7):782–790. doi: 10.1001/jamacardio.2017.1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Current Cigarette Smoking Among Adults — United States, 2005–2014. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6444a2.htm. Accessed December 25, 2021.
- 5.Kanjilal S, Gregg EW, Cheng YJ, et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971–2002. Arch Intern Med. 2006;166(21):2348–2355. doi: 10.1001/archinte.166.21.2348 [DOI] [PubMed] [Google Scholar]
- 6.Casetta B, Videla AJ, Bardach A, et al. Association Between Cigarette Smoking Prevalence and Income Level: A Systematic Review and Meta-Analysis. Nicotine Tob Res. 2017;19(12):1401–1407. doi: 10.1093/ntr/ntw266 [DOI] [PubMed] [Google Scholar]
- 7.Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco Product Use Among Adults - United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(46):1736–1742. doi: 10.15585/mmwr.mm6946a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gilpin EA, Pierce JP. Demographic differences in patterns in the incidence of smoking cessation: United States 1950-1990. Ann Epidemiol. 2002;12(3):141–150. doi: 10.1016/S1047-2797(01)00266-6 [DOI] [PubMed] [Google Scholar]
- 9.Babb S, Malarcher A, Schauer G, Asman K, Jamal A. Quitting Smoking Among Adults — United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457–1464. doi: 10.15585/mmwr.mm6552a1 [DOI] [PubMed] [Google Scholar]
- 10.Barbeau EM, Krieger N, Soobader MJ. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health. 2004;94(2):269–278. doi: 10.2105/ajph.94.2.269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siahpush M, Singh GK, Jones PR, Timsina LR. Racial/ethnic and socioeconomic variations in duration of smoking: results from 2003, 2006 and 2007 Tobacco Use Supplement of the Current Population Survey. J Public Health. 2010;32(2):210–218. doi: 10.1093/pubmed/fdp104 [DOI] [PubMed] [Google Scholar]
- 12.Binkley J Low Income and Poor Health Choices: The Example of Smoking. J Agric Econ. 2010;92(4):972–984. doi: 10.1093/ajae/aaq036 [DOI] [Google Scholar]
- 13.Vijayaraghavan M, Benmarnhia T, Pierce JP, et al. Income disparities in smoking cessation and the diffusion of smoke-free homes among U.S. smokers: Results from two longitudinal surveys. PLoS One. 2018;13(7):e0201467. doi: 10.1371/journal.pone.0201467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leventhal AM, Dai H, Higgins ST. Smoking Cessation Prevalence and Inequalities in the United States: 2014–2019. J Natl Cancer Inst. 2022;114(3):381–390. doi: 10.1093/jnci/djab208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hersch J. Gender Income Levels, and the Demand for Cigarettes. J Risk Uncertain. 2000;21(2/3):263–282. [Google Scholar]
- 16.Lawrence D, Fagan P, Backinger CL, Gibson JT, Hartman A. Cigarette smoking patterns among young adults aged 18-24 years in the United States. Nicotine Tob Res. 2007;9(6):687–697. doi: 10.1080/14622200701365319 [DOI] [PubMed] [Google Scholar]
- 17.Ackerson LK, Viswanath K. Communication Inequalities, Social Determinants, and Intermittent Smoking in the 2003 Health Information National Trends Survey. Prev Chronic Dis. 2009;6(2):A40. doi: 10.13016/xtcv-1yga [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Webb MS, Carey MP. Tobacco smoking among low-income Black women: demographic and psychosocial correlates in a community sample. Nicotine Tob Res. 2008;10(1):219–229. doi: 10.1080/14622200701767845 [DOI] [PubMed] [Google Scholar]
- 19.Cancer Institute N, Department of Health U, Services H. Monograph 22 A Socioecological Approach to Addressing Tobacco-Related Health Disparities. http://cancercontrol.cancer.gov/brp/tcrb/monographs. Accessed January 31, 2022.
- 20.Daly MC, Duncan GJ, McDonough P, Williams DR. Optimal Indicators of Socioeconomic Status for Health Research. Am J Public Health. 2002;92(7):1151–1157. doi: 10.2105/ajph.92.7.1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Geyer S, Hemström Ö, Peter R, Vågerö D. Education, income, and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. J Epidemiol Community Health. 2006;60(9):804–810. doi: 10.1136/jech.2005.041319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Latvala A, Rose RJ, Pulkkinen L, Dick DM, Korhonen T, Kaprio J. Drinking, smoking, and educational achievement: cross-lagged associations from adolescence to adulthood. Drug Alcohol Depend. 2014;137(1):106–113. doi: 10.1016/j.drugalcdep.2014.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maralani V Understanding the links between education and smoking. Soc Sci Res. 2014;48:20–34. doi: 10.1016/j.ssresearch.2014.05.007 [DOI] [PubMed] [Google Scholar]
- 24.Eligibility | Medicaid. https://www.medicaid.gov/medicaid/eligibility/index.html. Accessed February 18, 2022.
- 25.SNAP Eligibility | Food and Nutrition Service. https://www.fns.usda.gov/snap/recipient/eligibility. Accessed February 18, 2022.
- 26.Shahu A, Okunrintemi V, Tibuakuu M, et al. Income disparity and utilization of cardiovascular preventive care services among U.S. adults. Am J Prev Cardiol. 2021;8:100286. doi: 10.1016/j.ajpc.2021.100286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh GK, Jemal A. Socioeconomic and Racial/Ethnic Disparities in Cancer Mortality, Incidence, and Survival in the United States, 1950-2014: Over Six Decades of Changing Patterns and Widening Inequalities. J Environ Public Health. 2017;2017:2819372. doi: 10.1155/2017/2819372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lewer D, McKee M, Gasparrini A, Reeves A, de Oliveira C. Socioeconomic position and mortality risk of smoking: evidence from the English Longitudinal Study of Ageing (ELSA). Eur J Public Health. 2017;27(6):1068–1073. doi: 10.1093/eurpub/ckx059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chetty R, Stepner M, Abraham S, et al. The Association Between Income and Life Expectancy in the United States, 2001-2014. JAMA. 2016;315(16):1750–1766. doi: 10.1001/jama.2016.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gershon A, Hwee J, Victor JC, Wilton AS, To T. Trends in socioeconomic status-related differences in mortality among people with chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11(8):1195–1202. doi: 10.1513/AnnalsATS.201403-094OC [DOI] [PubMed] [Google Scholar]
- 31.Harris JE. Cigarette Smoking Among Successive Birth Cohorts of Men and Women in the United States During 1900–1980. J Natl Cancer Inst. 1983;71(3):473–479. doi: 10.1093/jnci/71.3.473 [DOI] [PubMed] [Google Scholar]
- 32.Escobedo LG, Remington PL. Birth cohort analysis of prevalence of cigarette smoking among Hispanics in the United States. JAMA. 1989;261(1):66–69. doi: 10.1001/jama.1989.03420010076036 [DOI] [PubMed] [Google Scholar]
- 33.Escobedo L, Remington P, Anda R. Long-term secular trends in initiation of cigarette smoking among Hispanics in the United States. Public Health Rep. 1989;104(6):583–587. [PMC free article] [PubMed] [Google Scholar]
- 34.Escobedo LG, Peddicord JP. Smoking prevalence in US birth cohorts: the influence of gender and education. Am J Public Health. 1996;86(2):231–236. doi: 10.2105/ajph.86.2.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anderson CM, Burns DM, Dodd KW, Feuer EJ. Chapter 2: Birth-cohort-specific estimates of smoking behaviors for the U.S. population. Risk Anal. 2012;32 Suppl 1(0 1):S14–24. doi: 10.1111/j.1539-6924.2011.01703.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Holford TR, Levy DT, McKay LA, et al. Patterns of birth cohort-specific smoking histories, 1965-2009. Am J Prev Med. 2014;46(2):e31–37. doi: 10.1016/j.amepre.2013.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jeon J, Holford TR, Levy DT, et al. Smoking and Lung Cancer Mortality in the United States From 2015 to 2065: A Comparative Modeling Approach. Ann Intern Med. 2018;169(10):684–693. doi: 10.7326/M18-1250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Manuel DG, Wilton AS, Bennett C, Rohit Dass A, Laporte A, Holford TR. Smoking patterns based on birth-cohort-specific histories from 1965 to 2013, with projections to 2041. Health Rep. 2020;31(11):16–31. doi: 10.25318/82-003-x202001100002-eng [DOI] [PubMed] [Google Scholar]
- 39.Holford TR, Levy Phd DT, Meza R. Comparison of Smoking History Patterns Among African American and White Cohorts in the United States Born 1890 to 1990. Nicotine Tob Res. 2016;18 Suppl 1(Suppl 1):S16–29. doi: 10.1093/ntr/ntv274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.NHIS - 2019 Questionnaire Redesign. https://www.cdc.gov/nchs/nhis/2019_quest_redesign.htm. Accessed January 13, 2022.
- 41.Prior HHS Poverty Guidelines and Federal Register References | ASPE. https://aspe.hhs.gov/topics/poverty-economic-mobility/poverty-guidelines/prior-hhs-poverty-guidelines-federal-register-references. Accessed January 6, 2022. [Google Scholar]
- 42.IVEware: Imputation and Variance Estimation Software | Survey Research Center. https://www.src.isr.umich.edu/software/iveware/. Accessed December 23, 2021. [Google Scholar]
- 43.Holford TR. The Estimation of Age, Period and Cohort Effects for Vital Rates. Biometrics. 1983;39(2):311–324. doi: 10.2307/2531004 [DOI] [PubMed] [Google Scholar]
- 44.Herd N, Borland R, Hyland A. Predictors of smoking relapse by duration of abstinence: findings from the International Tobacco Control (ITC) Four Country Survey. Addiction. 2009;104(12):2088–2099. doi: 10.1111/j.1360-0443.2009.02732.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hughes JR, Peters EN, Naud S. Relapse to smoking after 1 year of abstinence: a meta-analysis. Addict Behav. 2008;33(12):1516–1520. doi: 10.1016/j.addbeh.2008.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Krall EA, Garvey AJ, Garcia RI. Smoking relapse after 2 years of abstinence: findings from the VA Normative Aging Study. Nicotine Tob Res. 2002;4(1):95–100. doi: 10.1080/14622200110098428 [DOI] [PubMed] [Google Scholar]
- 47.Escobedo LG, Peddicord JP. Smoking prevalence in US birth cohorts: the influence of gender and education. Am J Public Health. 1996;86(2):231–236. doi: 10.2105/ajph.86.2.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fleischer NL, Mckeown RE. The Second Epidemiologic Transition from an Epidemiologist’s Perspective. In: Zuckerman MK, ed. Modern Environments and Human Health: Revisiting the Second Epidemiologic Transition. John Wiley & Sons, Ltd; 2014. doi: 10.1002/9781118504338.ch19 [DOI] [Google Scholar]
- 49.Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff (Millwood). 2015;34(11):1830–1839. doi: 10.1377/hlthaff.2015.0645 [DOI] [PubMed] [Google Scholar]
- 50.Hernández D, Swope CB. Housing as a platform for health and equity: Evidence and future directions. Am J Public Health. 2019;109(10):1363–1366. doi: 10.2105/AJPH.2019.305210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Omole T, McNeel T, Choi K. Heterogeneity in past-year smoking, current tobacco use, and smoking cessation behaviors among light and/or non-daily smokers. Tob Induc Dis. 2020;18:74. doi: 10.18332/tid/125724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ni K, Wang B, Link AR, Sherman SE. Does Smoking Intensity Predict Cessation Rates? A Study of Light-Intermittent, Light-Daily, and Heavy Smokers Enrolled in Two Telephone-Based Counseling Interventions. Nicotine Tob Res. 2020;22(3):423–430. doi: 10.1093/ntr/nty257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gentzke AS, Wang TW, Jamal A, et al. Tobacco Product Use Among Middle and High School Students — United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1881–1888. doi: 10.15585/mmwr.mm6950a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meza R, Jimenez-Mendoza E, Levy DT. Trends in Tobacco Use Among Adolescents by Grade, Sex, and Race, 1991-2019. JAMA Netw Open. 2020;3(12):e2027465. doi: 10.1001/jamanetworkopen.2020.27465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Corey CG, Holder-Hayes E, Nguyen AB, et al. US Adult Cigar Smoking Patterns, Purchasing Behaviors, and Reasons for Use According to Cigar Type: Findings From the Population Assessment of Tobacco and Health (PATH) Study, 2013–2014. Nicotine Tob Res. 2018;20(12):1457–1466. doi: 10.1093/ntr/ntx209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jeon J, Meza R, Krapcho M, Clarke LD, Byrne J, Levy DT. Chapter 5: Actual and counterfactual smoking prevalence rates in the U.S. population via microsimulation. Risk Anal. 2012;32 Suppl 1(Suppl 1):S51–68. doi: 10.1111/j.1539-6924.2011.01775.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Apelberg BJ, Feirman SP, Salazar E, et al. Potential Public Health Effects of Reducing Nicotine Levels in Cigarettes in the United States. N Engl J Med. 2018;378(18):1725–1733. doi: 10.1056/NEJMsr1714617 [DOI] [PubMed] [Google Scholar]
- 58.Levy DT, Tam J, Sanchez-Romero LM, et al. Public health implications of vaping in the USA: the smoking and vaping simulation model. Popul Health Metr. 2021;19(1):19. doi: 10.1186/s12963-021-00250-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Le TT, Mendez D. An estimation of the harm of menthol cigarettes in the United States from 1980 to 2018. Tob Control. 2021;0:1–5. doi: 10.1136/tobaccocontrol-2020-056256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moolgavkar SH, Holford TR, Levy DT, et al. Impact of reduced tobacco smoking on lung cancer mortality in the United States during 1975-2000. J Natl Cancer Inst. 2012;104(7):541–548. doi: 10.1093/jnci/djs136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tam J, Levy DT, Jeon J, et al. Projecting the effects of tobacco control policies in the USA through microsimulation: a study protocol. BMJ Open. 2018;8(3):e019169. doi: 10.1136/bmjopen-2017-019169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.de Koning HJ, Meza R, Plevritis SK, et al. Benefits and harms of computed tomography lung cancer screening strategies: a comparative modeling study for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;160(5):311–320. doi: 10.7326/M13-2316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Meza R, ten Haaf K, Kong CY, et al. Comparative analysis of 5 lung cancer natural history and screening models that reproduce outcomes of the NLST and PLCO trials. Cancer. 2014;120(11):1713–1724. doi: 10.1002/cncr.28623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McMahon PM, Meza R, Plevritis SK, et al. Comparing benefits from many possible computed tomography lung cancer screening programs: extrapolating from the National Lung Screening Trial using comparative modeling. PLoS One. 2014;9(6):e99978. doi: 10.1371/journal.pone.0099978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Meza R, Jeon J, Toumazis I, et al. Evaluation of the Benefits and Harms of Lung Cancer Screening with Low-Dose Computed Tomography: Modeling Study for the US Preventive Services Task Force. JAMA. 2021;325(10):988–997. doi: 10.1001/jama.2021.1077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Meza R, Jeon J, Toumazis I, et al. Evaluation of the Benefits and Harms of Lung Cancer Screening With Low-Dose Computed Tomography: A Collaborative Modeling Study for the U.S. Preventive Services Task Force [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US). 2021;Report No.:20-05266-EF-2. [PubMed] [Google Scholar]
- 67.Han SS, ten Haaf K, Hazelton WD, et al. The impact of overdiagnosis on the selection of efficient lung cancer screening strategies. Int J Cancer. 2017;140(11):2436–2443. doi: 10.1002/ijc.30602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Toumazis I, de Nijs K, Cao P, et al. Cost-effectiveness Evaluation of the 2021 US Preventive Services Task Force Recommendation for Lung Cancer Screening. JAMA Oncol. 2021;7(12):1833–1842. doi: 10.1001/jamaoncol.2021.4942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Criss SD, Cao P, Bastani M, et al. Cost-Effectiveness Analysis of Lung Cancer Screening in the United States: A Comparative Modeling Study. Ann Intern Med. 2019;171(11):796–804. doi: 10.7326/M19-0322 [DOI] [PubMed] [Google Scholar]
- 70.Brown-Johnson CG, England LJ, Glantz SA, Ling PM. Tobacco Industry Marketing to Low Socio-economic Status Women in the US. Tob Control. 2014;23(e2):e139–146. doi: 10.1136/tobaccocontrol-2013-051224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liber AC, Sánchez-Romero LM, Cadham CJ, et al. Tobacco Couponing: A Systematic Review of Exposures and Effects on Tobacco Initiation and Cessation. Nicotine Tob Res. 2022;ntac037. doi: 10.1093/ntr/ntac037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tobacco companies target poorer neighborhoods with advertising | News | Harvard T.H. Chan School of Public Health. https://www.hsph.harvard.edu/news/hsph-in-the-news/tobacco-advertising-poor-neighborhoods/. Accessed January 13, 2022. [Google Scholar]
- 73.Giovenco DP, Spillane TE, Merizier JM. Neighborhood Differences in Alternative Tobacco Product Availability and Advertising in New York City: Implications for Health Disparities. Nicotine Tob Res. 2019;21(7):896–902. doi: 10.1093/ntr/nty244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Daly AT, Deshmukh AA, Vidrine DJ, et al. Cost-effectiveness analysis of smoking cessation interventions using cell phones in a low-income population. Tob Control. 2019;28(1):88–94. doi: 10.1136/tobaccocontrol-2017-054229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ribisl KM, Luke DA, Bohannon DL, Sorg AA, Moreland-Russell S. Reducing Disparities in Tobacco Retailer Density by Banning Tobacco Product Sales Near Schools. Nicotine Tob Res. 2017;19(2):239–244. doi: 10.1093/ntr/ntw185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Glasser AM, Roberts ME. Retailer Density Reduction Approaches to Tobacco Control: A Review. Health Place. 2021;67:102342. doi: 10.1016/j.healthplace.2020.102342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.D’Angelo H, Ammerman A, Gordon-Larsen P, Linnan L, Lytle L, Ribisl KM. Sociodemographic disparities in proximity of schools to tobacco outlets and fast-food restaurants. Am J Public Health. 2016;106(9):1556–1562. doi: 10.2105/AJPH.2016.30325 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


