Abstract
Background:
Older adults are interested and able to complete video visits, but often require coaching and practice to succeed. Data show a widening digital divide between older and younger adults using video visits. We conducted a qualitative feasibility study to investigate these gaps via ethnographic methods, including a team member in older participants’ homes.
Methods:
This ethnographic feasibility study included a virtual medication reconciliation visit with a clinical pharmacist for Veterans aged 65 and older taking 5 or more medications. An in-home study team member joined the participant and recorded observations in structured fieldnotes derived from the Updated Consolidated Framework for Implementation Research and Age-Friendly Health Systems. Fieldnotes included behind-the-scenes facilitators, barriers, and solutions to challenges before and during the visits. We conducted a thematic analysis of these observations and matched themes to implementation solutions from the Expert Recommendations for Implementing Change.
Results:
Twenty participants completed a video visit. Participants were 74 years old (range 68–80) taking 12 daily medications (range 7–24). Challenges occurred in half of the visits and took the in-home team member and/or pharmacist an average of 10 minutes to troubleshoot. Challenges included notable new findings, such as that half of the participants required technology assistance for challenges that would not have been able to be solved by the pharmacist virtually. Furthermore, although many participants had a device or had used video visits before, some did not have a single device with video, audio, Internet, and access to their email username and password.
Conclusions:
Clinicians may apply these evidence-based implementation solutions to their approach to video visits with older adults, including having a team member join the visit before the clinician, involving tech-savvy family members, ensuring the device works with the visit platform ahead of time, and creating a troubleshooting guide from our common challenges.
Keywords: geriatrics, home telehealth, telehealth, video visit, virtual care
BACKGROUND
Older adults are interested and able to complete video visits, but often require coaching and practice to succeed.1–4 Data from the past 3 years have emphasized that video visits are a persistent part of care for older adults1,5–7 and that Medicare beneficiaries’ access to and usage of virtual care continues to increase.8,9 However, this data also shows a widening digital divide between older adults and younger ones.7,10 Especially for older adults in rural areas, access to video visits remains low while access for other, younger adults continues to climb.7,10
We described our experience with a rapid implementation pilot of video visits for older adults in the spring through fall of 2020.11 Beyond 2020, older adults continued to complete virtual visits and faced similar and new barriers and facilitators.5,7,10 Although some aspects of virtual care have been well-studied, only a little is known about the challenges that older adults face just before joining their visit and during their visit periods where technological challenges occur.7–9,11,12 For example, in a 2021 study of older adults in California, 77% of patients had access to a smart device, yet only 37% of patients could connect via a video visit.5
To address this access gap and this knowledge gap, we changed our approach to virtual visits with older adults11 to include an in-home team member. Having an in-home team member might provide us a new vantage point, a behind-the-scenes look at the facilitators and barriers to video visits for older adults. The team member would join older adults in their home just before they attempted to connect for their video visit. We used an implementation science-informed approach to identify these less understood, behind-the-scenes barriers that required in-person troubleshooting and mapped them to implementation solutions for clinicians to apply to their approach to video visits with older adults.
METHODS
Design
Study overview
This was a qualitative feasibility study using ethnographic methods at a suburban Veterans Affairs (VA) facility in New England. The intervention included a virtual visit for medication reconciliation and management with a clinical pharmacist. Prior to the video visit, study personnel ensured participants had access to a device or arranged to get them a VA-loaned device and conducted training if necessary. An in-home study team member joined the participant at their home. The participant and pharmacist connected via the VA’s synchronous video platform, VA Video Connect. The VA Central Institutional Review Board (IRB) reviewed and approved this study.
Ethnography
In the field of anthropology, ethnography is a form of field research that relies on several methods (direct and participant observation, fieldnotes, interviewing, etc.). Our in-home team member was a medical anthropologist with extensive cultural and international fieldwork experience as well as training in geriatric health research. Prior to this study, her work included a qualitative study of technology-based treatment for depression among homebound older adults using ethnographic methods. We utilized direct observation and participant observation, including the following novel steps:
We ensured participants had a device and offered training before their visit,
We sent a study team member into the participant’s home for direct observation just before the video visit, and
The in-home team member resolved technology challenges before and during the video visit.
Implementation framework
The Consolidated Framework for Implementation Research (CFIR) is an implementation framework comprised of core domains and constructs within domains that influence implementation outcomes on many levels.11,13 We used the Updated CFIR Constructs14 to structure our ethnographic fieldnotes and to create our preliminary codebook. We matched facilitators and barriers to video visits with implementation strategies from the Expert Recommendations for Implementing Change (ERIC) matching tool, v1.15 This tool maps barriers with targeted, evidence-based implementation strategies and provides a consensus rating for each barrier-strategy pairing.15
Theoretical framework
Age-Friendly Health Systems (AFHS) was our theoretical framework.16 AFHS utilize a person-centered approach to maintain the health of older adults via evidence-based care that improves health outcomes, value and satisfaction with care, and prevents avoidable harm.17,18 We reviewed our thematic analysis using AFHS in order to refine our final set of implementation solutions for clinicians to align with Age-Friendly care.
Study design
Setting and participants
Recruitment occurred from August 2020 to July 2021 and study visits occurred from November 2020 to August 2021. Participants were identified from an auto-generated list in the electronic health record of individuals aged 65 and older with at least 2 chronic medical conditions and no dementia diagnosis who had a visit to our suburban VA medical center in the last year. Our catchment area was not rural, as we recruited participants who were within driving distance of the medical center. Additional eligibility screening occurred after participants responded to an initial letter with information about the study, indicating they were interested in learning more.
After they indicated their interest, the in-home team member assessed their eligibility and enrolled them in the study. All participants provided consent for the video visit. At the time of consent, participants were informed that they would receive a $50 gift card for completing the video visit. Participants were given the option to complete all steps of the process from their home, in accordance with strict infection control protocols enforced at that time, either on the day of or prior to the visit. On the day of the visit, the in-home team member arrived 15 min early to begin observing the facilitators and barriers the participant faced.
Procedures
Our study coordinators used mailings and telephone calls to recruit participants, completed informed consent and baseline assessments19 via telephone or in the participant’s home, and scheduled the video visit with the pharmacist.
To attempt a visit, all participants needed internet access at home and an internet-compatible device with a camera and microphone. If participants did not have access to a video-capable device, the study coordinator arranged for them to receive a VA-loaned tablet.7 Participants who received a VA-loaned tablet were scheduled for a test visit with a local VA employee, and all other participants were given a demonstration by the study coordinator prior to the pharmacist video visit. To join the visit, participants must have had access to email to click an autogenerated hyperlink to start their visit. Next, participants followed prompts to enable and turn on their camera and microphone. At this point, the clinician would do the same, and the two parties could interact via synchronous audio and video.
The purpose of the visit was to complete a full medication reconciliation, including visualizing medications and their organization.11,20 Upon arrival at the participant’s home, the in-home team member observed the participant as they attempted to join the visit and intervened as necessary to assist them with connecting to and completing the video visit. Both the pharmacist and in-home team member recorded observations as fieldnotes using a semi-structured template (Figure 1). If a technology challenge occurred before the pharmacist joined, the in-home team member noted this, allowed the participant to attempt to solve the problem, and then assisted the participant as needed. During the visit, the pharmacist took the lead troubleshooting all technical challenges, with help from the in-home team member as necessary. Both parties noted challenges that occurred as well as any subsequent intervention(s) for resolution.
FIGURE 1.
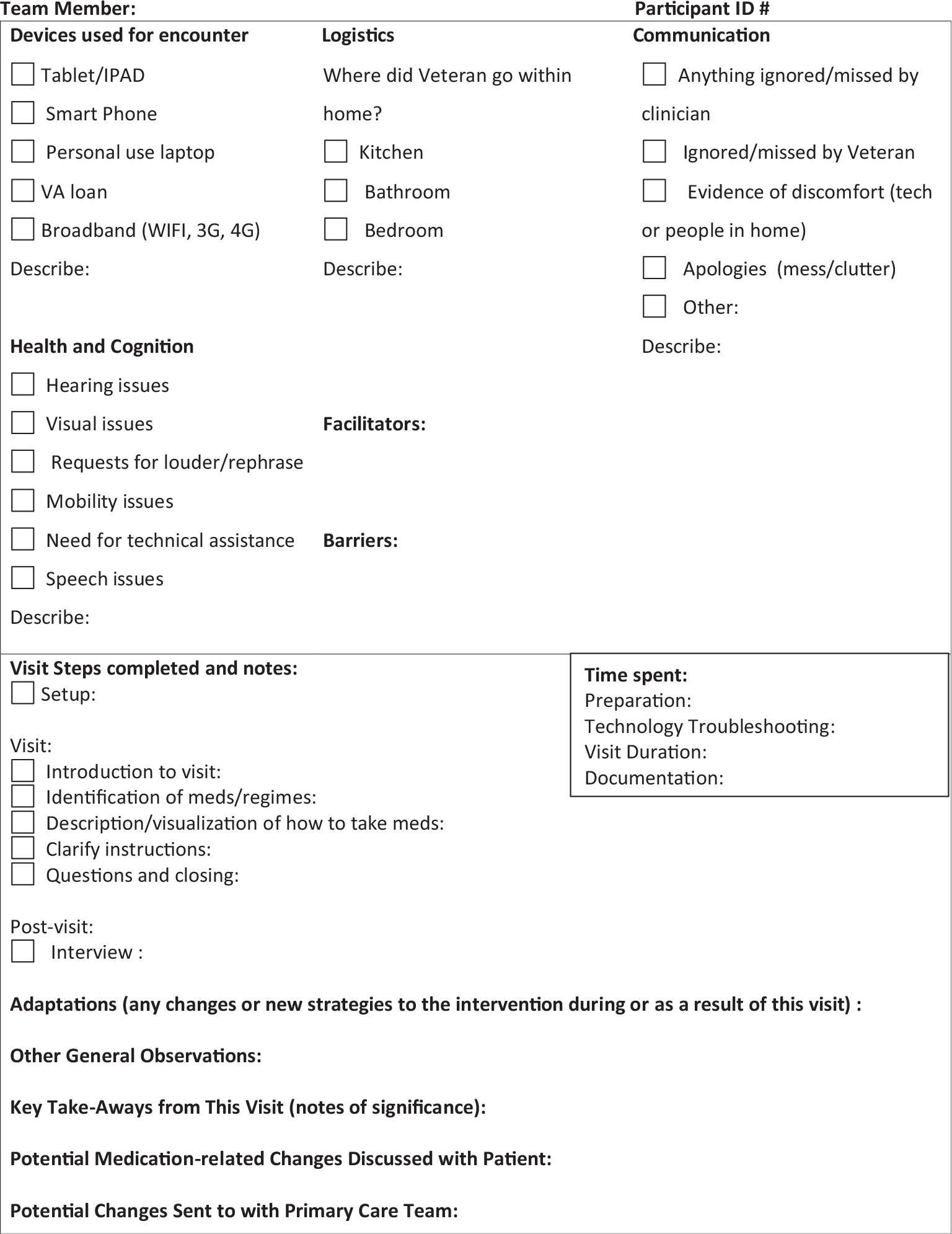
Template for fieldnotes. This includes the full template that our in-home team member and pharmacist used to note all observations just before and during the visit. Upon arrival at the participant’s home, the in-home team member observed the participant as they attempted to join the visit and intervened as necessary to assist them with connecting to and completing the video visit. Both the pharmacist and in-home team member recorded observations as fieldnotes using this template. Both parties noted challenges that occurred as well as any subsequent intervention(s) for resolution.
Measurements
Our primary measurements were our fieldnotes and the baseline Technology Comfort Assessment.21 Participants were considered confident if they answered that they strongly agreed or agreed with this statement from the Technology Comfort Assessment: “Overall, I feel confident using computers, tablets, smartphones, or other electronic devices to do the things I need to do online.”21 Participants were considered not confident if they answered that they disagreed or strongly disagreed. Participants may also have selected “neither agree nor disagree.”
Analysis
Two study team members analyzed structured fieldnote data for common themes related to facilitators and barriers that occurred, including whether associated interventions were from the study team or participant’s own actions. Our team coded fieldnote data using an adaptive deductive approach, specifying codes a priori and allowing for the emergence of new codes.22–24 A priori codes were defined based on our previous work11 and clinical experiences, and our thematic analysis guided by CFIR and refined by AFHS.24,25 Two members of our team (CH and CW) separately coded both the in-home team member and pharmacist fieldnote data, and a third member (NG) acted as a referee to resolve coding discrepancies.
After coding, we mapped common themes from CFIR constructs to implementation strategies through the ERIC Matching Tool, v1.15 We considered all CFIR constructs in our analysis. We selected high-consensus strategies, defined as such by ERIC, to develop a menu of evidence-based, implementation solutions (categorized as high or low effort based on clinical experience and past studies5,25–30).
RESULTS
Technology interest, access, capability, and confidence
Twenty participants completed a video visit. On average, they were 74 years old (range 68–80) and taking 12 daily medications (range 7–24). Additional characteristics included (Table 1):
Interest: Participants were interested in enrolling in the study because they wanted to learn or improve technology skills (6, 30%) and were looking for help from a pharmacist for medication support (5, 25%).
Access: 15 (75%) participants had access to their own video-visit capable device and 13 (65%) planned to use it for the video visit. Seven (35%) required a VA-loaned tablet to use for the video-visits. Six (30%) participants had completed video visits with a clinician prior to this study.
Capability: Three participants intended to use their own device but were unable to do so: one was unable to enable his camera in the VA platform, one did not know his email password to locate the visit hyperlink, and one did not know how to access his email whatsoever.
Confidence: 11 (55%) participants were confident and nine (45%) were not per the Technology Comfort Assessment.21
TABLE 1.
Participant characteristics (N = 20).
| Characteristic | Count |
|---|---|
|
| |
| Age, years, mean ± SD, range | 74 ± 3, 68–80 |
| Male, count (%) | 19 (95) |
| Race, count (%) | |
| Non-Hispanic White | 19 (95) |
| Non-Hispanic Black | 0 |
| Non-Hispanic Asian | 1 (5) |
| Daily medications, mean, range | 12, 7–24 |
| Device used for video visit, count (%) | |
| Patient used their own device | 13 |
| Desktop computer | 3 |
| Laptop | 6 |
| Tablet | 4 |
| Patient used VA-loaned tablet | 7 |
| Functional health literacy score,a average, range | 34, 19–36 |
| Technology access, count (%) | |
| Access to email address | 16 (80) |
| Access to any internet-capable device | 15 (75) |
| Prior use of any synchronous video technology | 7 (35) |
| Technology assistance | |
| Family member assisted with technology at a previous visit, count (%) | 7 (35) |
| Family member assisted with technology just before this visit, count (%) | 2 (10) |
| Participant required any technology assistance from in-home team member or pharmacist, count (%) | 10 (50) |
| Participant required technology assistance from in-home team member just before this visit, count (%) | 7 (35) |
| Participant required technology assistance from pharmacist during this visit, count (%) | 6 (30) |
| Pharmacist able to solve challenge, count (%) | 3 (15) |
| Pharmacist unable to solve challenge, requiring assistance from in-home team member, count (%) | 3 (15) |
| Participant required any technology assistance that was not/would not have been able to be solved by the pharmacist virtually, count (%) | 10 (50) |
| Technology capability, count (%) | |
| Capable of using their own device for visit | 10 (50) |
| Intended to but incapable of using their own device and/or the video visit platform for visit | 3 (15) |
| Intended to and did use VA-loaned device for visit | 7 (35) |
| Technology confidence,b count (%) | |
| Confident using electronic devices to do the things they need to do online | 11 (55) |
| Not confident using electronic devices to do the things they need to do online | 9 (45) |
Participants completed the Short Test of Functional Health Literacy in Adults (S-TOFHLA, Baker et al.19). This measures functional health literacy. A score of 0–16 is considered Inadequate Health Literacy, defined as “unable to read and interpret health texts.” A score of 17–22 is considered Marginal Health Literacy, defined as “has difficulty reading and interpreting health texts.” A score of 23–36 is considered Adequate Health Literacy, defined as “can read and interpret most health texts.” One participant scored a 19 (Marginal) and all other participants scored a 27–36 (Adequate).
Participants were considered confident if they answered that they strongly agreed or agreed with this statement from the Technology Comfort Assessment:
“Overall, I feel confident using computers, tablets, smartphones, or other electronic devices to do the things I need to do online” (Zulman et al.21). Participants were considered not confident if they answered that they disagreed or strongly disagreed.
Ten (50%) unique participants required assistance before or during the visit. Seven of these required in-home assistance just before joining the visit and six required assistance during the visit with the pharmacist. The pharmacist was able to solve the challenges for three participants. For the remaining three, assistance from the in-home team member was required to solve the challenges. Thus, there were 10 instances where the challenges could not have been solved without the in-home team member present (Table 1). The average time to solve a challenge was 10 minutes.
Facilitators, barriers, in-home technology troubleshooting, and new findings
We identified emerging themes that required addition of new codes and codebook adaptation (see Figure 2 and Supplemental Table 1). We found that although many participants had a device or had used video visits before, some did not have a single device with audio, video, internet, and access to their email username and password. Additionally, some participants did not have access to email at all.
FIGURE 2.
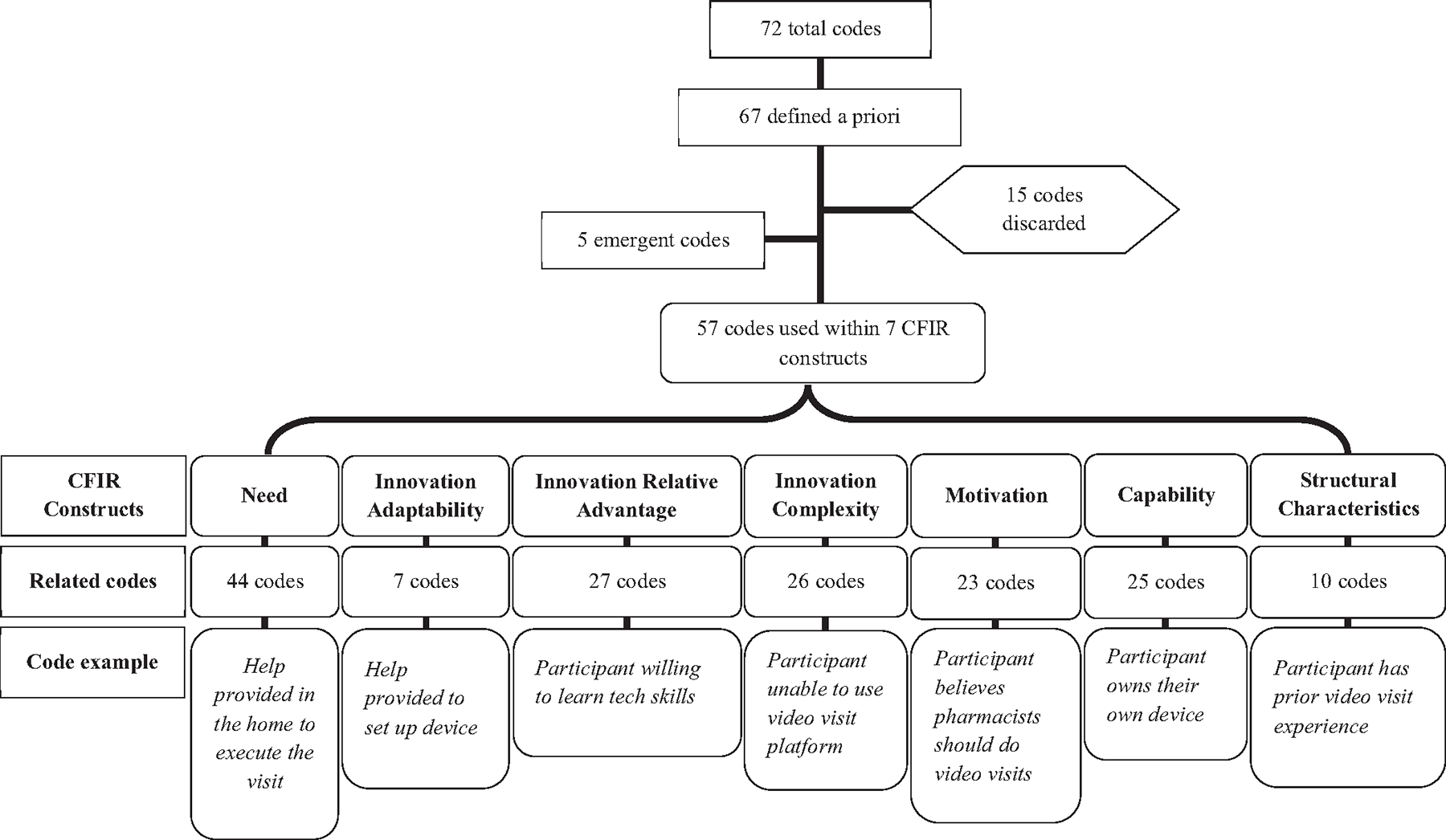
Coding strategy and representative codes. Coding strategy with representative codes. The final codebook used to code fieldnotes contained 72 codes. Sixty seven codes were defined according to prior work’s codebook and anticipated codes according to data extraction. Fifteen codes were discarded or not used, and five codes were added throughout the coding process, upon which all participants were reviewed again for applicability. Fifty-seven unique codes were used overall, representing seven unique Consolidated Framework for Implementation Research (CFIR) constructs. Codes were grouped and associated with one or more related CFIR constructs, by group. This figure depicts the number of codes related to each individual CFIR construct and provides an example of a code within that construct.
We summarize the most common facilitators, barriers, in-home technology troubleshooting, and new findings in Figure 3.
FIGURE 3.
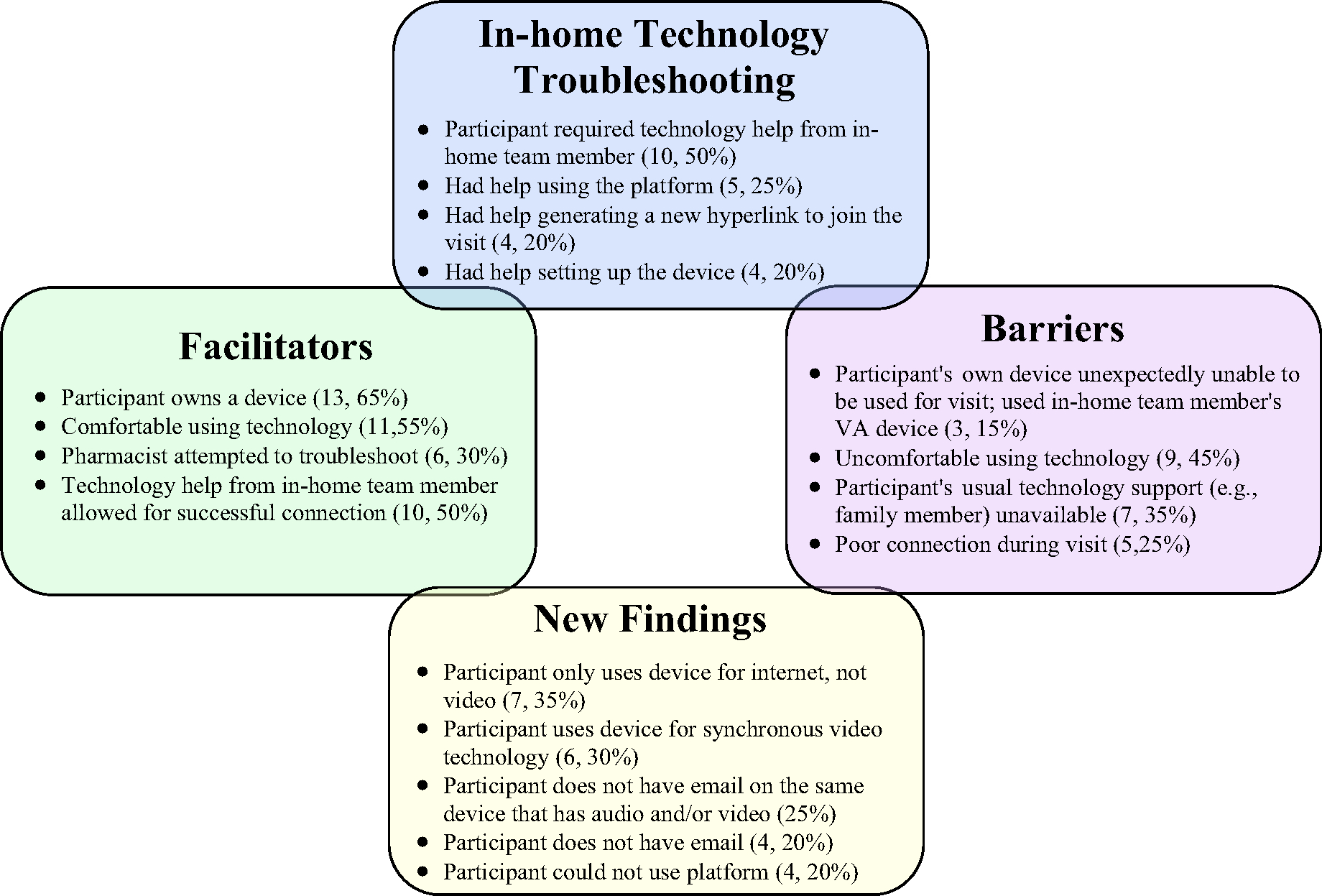
Facilitators, barriers, in-home technology troubleshooting, and new findings. We present the most common facilitators, barriers, in-home technology troubleshooting, and new findings that the in-home team member and pharmacist observed in their fieldnotes. The most common facilitators to successful visits were participants owning a device (13, 65%) and were comfortable using technology (11, 55%). The most common barriers were that a participant’s usual support, like a tech-savvy family member, was not available during the visit (7, 35%), or they were uncomfortable using technology (9, 45%). The in-home team member assisted 10 (50%) participants and the pharmacist assisted six (30%), most often this was help with the platform (5, 25%), the hyperlink (4, 20%) or the device (4, 20%). Notable new findings were that although many participants had a device or used video visits before, some did not have a single device with video, audio, internet, and access to their email username and password (7, 35%). Additionally, some participants did not have access to email at all (4, 20%).
Implementation strategies and solutions for facilitators and barriers
The six highest-consensus strategies from the ERIC Matching Tool, v115 that were applicable to our context are italicized below.15 Within each strategy, we outline related high-effort and low-effort implementation solutions (Table 2).
TABLE 2.
Evidence-based implementation solutions for common technology challenges.
| ERIC strategy | High-effort solutions | Low-effort solutions |
|---|---|---|
|
| ||
| Identify and prepare champions | Individual has a focus on training, empowering older patients to use video visit tech before visit occurs15 Someone available for in-home help5 |
Individual joins the video visit just before it begins to troubleshoot tech challenges before clinic visit starts15 Someone available during the video visit for on-demand tech help5 |
| Involve patients and family members | Schedule in-person training with patient and tech-savvy caregiver(s)/family member(s) days before visit5 Schedule visits when tech-savvy family member(s)/caregiver(s) are available15,16 |
Inquire about tech-savvy caregivers/family members before scheduling Schedule telephone practice session with the patient and tech-savvy caregiver(s)/family member(s)6 |
| Assess for readiness and identify barriers and facilitators | Complete in-person test visit using the patient’s preferred device to test camera, audio, and email access, including access to their email login and password Consider if patient has experience with using video on their device for other purposes and implement an approach that is similar for the visit Institute a program to connect patients with loaned devices if they do not have one with camera, audio, internet, and email access15 Provide on-demand access to tech help during all video visits5 |
Inquire whether patient has one device that includes all of the following: camera, audio, internet, and email access, including access to their email login and password15 Continue to offer video visits for patients who are interested but who have not tried one before15,17 If a patient does not have an email account, assist them in creating a free email account that they can access on their video visit device Ensure all patients and clinicians receive the same tech trouble-shooting guide, so that they may use it together when solving problems over the phone during a visit15 |
| Promote Adaptability Conduct cyclical small tests of change Create a learning collaborative | Consider each video visit a small test of change, and approach future visits with an eye for improvement: What went well? How can I replicate that for future patients? What went wrong? How could I prevent that problem in the future? How can I solve that problem in the moment? Consider sharing and receiving best practices for Age-Friendly video visits as a part of the larger Age-Friendly network, outside of your local site29 |
Ensure clinicians conducting video visits have a set protocol for what to do for tech challenges—including a tech troubleshooting guide—as well as a backup plan for video visits (e.g., Who calls the patient if they do not join video visit? When?)16,29 Share best practices within your local site to continue to create opportunities for Age-Friendly video visits29 |
Abbreviation: ERIC, Expert Recommendations for Implementing Change.
Identify and prepare champions
The pharmacist assisted during six (30%) visits, but the in-home team member was needed to troubleshoot in 10 (50%) visits, all of which could not have been resolved without in-home help (e.g., three did not have a device with camera, video, internet, and email access; the other seven who used a VA-loaned device did not know how to set it up for video visit use by themselves).
The in-home team member was the implementation champion; a lower effort solution may be to have a team member join the visit virtually 10 minutes before the clinician to troubleshoot challenges via telephone until the older adult successfully connects, and to be available for on-demand help when challenges occur.5,26 In cases where the older adult cannot connect, the visit can be rescheduled ahead of time, before the clinician joins.5,26 Prior to the rescheduled visit, the older adult can again attempt a practice visit with an implementation champion.
Involve patients and family members
We did not deliberately involve tech-savvy caregivers or family members before the visit or during the visit with the pharmacist. However, we propose doing this for all visits (low effort) and considering involving tech-savvy individuals in the training, setup, and execution of video visits for older adults (higher effort) as possible.5,6,26 In the case above, when the older adult is having challenges, a family member could also work with the implementation champion to troubleshoot challenges before or during the visit, as well as in a designated practice visit before the visit with the clinician.
Assess for readiness and identify barriers and facilitators
We will continue to inquire during scheduling if patients have one device that includes all of the following: camera, audio, Internet, and email access, including access to their email login and password (low effort). We also suggest continuing to offer video visits to patients who have not completed one before (low effort).28
For patients without access to a device, we suggest instituting a program to connect patients with loaned devices (high effort)26 or at a minimum, assisting those patients in creating a free email account with easy access to their login information (low effort). When on-demand access to technology assistance is not possible,26 providing a simple technology troubleshooting guide to all patients and clinicians ahead of the visit is a lower-effort strategy.
Promote adaptability and conduct cyclical small tests of change
As the visits progressed, we could better anticipate possible challenges and troubleshoot them according to previous experiences. An effective solution in accordance with these ERIC strategies is to consider each video visit a small test of change, and approach future visits with older adults with an eye for improvement: What went well? How can I replicate that for future patients? What went wrong? How could I prevent that problem in the future?
For a lower effort strategy, we suggest focusing on clinician adaptability.27,30 Ensure clinicians conducting video visits have a set protocol for what to do for technology challenges—including a technology troubleshooting guide—as well as a back-up plan for video visits that is communicated clearly to patients30 (e.g., Who calls the patient if they do not join the video visit? When? Is there a landline or another phone in the home to call, which is not being used for this visit?).
Create a learning collaborative
Our study’s aim aligns with Age Friendly Health Systems18 4M’s: What Matters, Medication, Mentation and Mobility. AFHS and our study also emphasize training for the care team in geriatric principles and cultivation of an information ecosystem that facilitates information sharing across settings, including patient goals and care preferences. We suggest sharing best practices for assisting older adults with technology within your local site to continue to create opportunities for Age-Friendly video visits (low effort).29,31,32 On a broader scale, consider sharing your best practices as part of the larger Age-Friendly network to advance the care of older adults and communicate using the AFHS shared language and philosophy (high effort).27
DISCUSSION
Our objective was to build on prior knowledge by including an in-home team member who conducted direct observation, rather than relying on what can only be observed remotely or through patient report.11 Despite the growing literature on virtual care, our in-home approach generated several new findings. We found that while some older adults do not have access to technology, even those who own video-visit capable devices are not necessarily equipped with the prior knowledge, education and support to successfully connect. In some instances, we were able to provide visits to people who had no access to technology at home, engaging a previously unreached population within VA. Our final table includes high- and low-effort implementation solutions, which in our experience, allowed older adults to complete video visits with some troubleshooting. On average, these solutions only took 10 minutes to implement.
Studies over the past 3 years have identified barriers for video visits for older adults and have called for implementation of Age-Friendly technology solutions.5,26–28 Our study aligns with these and illuminated several key findings.5,10,26–28,33 We found that three participants who owned their own device still required a VA-loaned device, and 50% of participants required in-home trouble-shooting that was not able to be solved by the pharmacist virtually. Additionally, we also identified new barriers for those intended to use their own device, such as not being able to access email on a device with audio and video capability (Figure 3). Through qualitative analysis with an implementation framework, coupled with the CFIR-EIRC tool,14,15 we were able to generate and categorize high- and low-effort solutions to the important problem of older adult ability to easily engage in video visits using an Age-Friendly approach.18
In the future, we will implement a mix of high- and low-effort solutions from Table 2:
Having a team member join the visit 10 minutes before the clinician to troubleshoot and to remain on-call for challenges that arise,
Involving tech-savvy family members in scheduling and video visit practice,
Taking steps to ensure ahead of time that a device will work with the visit platform (and to practice with that same device), and
Creating one user-friendly troubleshooting guide for patients and clinicians with our most common challenges and how to solve them.
Telehealth technologies have expanded and grown over the past few years, and so has the population of older adults engaging with them.5,26–28 Medicare reports continue to show an increase in access to and use of virtual care8,9 in tandem with a widening digital divide between older adults and younger ones.7,10 We invite clinicians to apply these solutions to their approach to visits with older adults to close this gap. Many of these older adults have a device and have attempted a video visit but they may still require some assistance. Clinicians may also consider the AFHS philosophy and our implementation solutions when advocating for additional resources from leadership that may be necessary for successful video visits with older adults.18
Our study has several strengths. While previous literature relied mostly on patient-reported barriers and experiences through interviews and surveys,28,34 our in-home team member and virtual pharmacist both observed and solved challenges first-hand. Our paper is unique in that it leverages our experience in rapid telehealth integration at the onset of COVID-19 in order to illuminate how barriers have changed and what challenges remain constant. Additionally, our proposed high- and low-effort solutions have methodologic rigor through the use of CFIR-ERIC14,15 and are bolstered by the evidence base from 2020 to now.
Our study was limited by several factors. All participants were interested in telehealth as they were consented to enroll in this study. This may or may not reflect the attitudes of general clinic patients. In addition, we did not consider e-health literacy in the recruitment process, nor did we collect information on e-health literacy, so we are unable to comment on the objective abilities of our participants to “appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem.”35 Being conducted at VA, our population was predominantly male and white, which does not reflect the demographics of older adults in the United States or worldwide. We met our aim to complete 20 video visits over the course of 1 year. The major limitation to enrolling and completing the visits sooner was COVID-19-related. We received approval to start recruitment for in-person research in August 2020. We enrolled our first three participants from September–December 2020. Of note, the first COVID-19 vaccines were available to our staff and older veterans beginning in December. We enrolled the next six participants from January–March 2021, when the second vaccine was available to older veterans at our site and the first vaccine was becoming available to veterans of all ages at our site. We enrolled the final eleven participants thereafter. Our final limitation was that our in-home team member provided one-on-one help, which may not be feasible in practice: thus we suggest lower effort alternatives to troubleshooting in Table 2 or adapting high-effort solutions to become lower effort in a given context.
CONCLUSIONS
Twenty interested older adults completed a video medication reconciliation visit with a pharmacist, half of whom required in-home troubleshooting beyond the virtual support that could be provided by the pharmacist. We offer evidence-based implementation solutions of varying levels of effort to these behind-the-scenes barriers using an Age-Friendly approach, including having a team member join the visit before the clinician, involving tech-savvy family members, ensuring the device works with the visit platform ahead of time, and creating a trouble-shooting guide with our most common challenges and solutions. Clinicians may apply these solutions to their approach to video visits with older adults.
Supplementary Material
Supplemental Table 1. CFIR constructs and related codes from our analysis. This table shows how each CFIR construct was related to categories in our thematic analysis, with examples of matching codes that were either pre-determined or emerged from our fieldnotes.
Key points.
We conducted a qualitative feasibility study using ethnographic methods to include a team member who entered participants’ homes and observed what happened just before and during a video visit with a pharmacist.
Challenges occurred in half of the visits and took the in-home team member and/or pharmacist an average of 10 minutes to troubleshoot.
Of note, half of the participants required technology assistance from the in-home team member that was not able or would not have been able to be solved by the pharmacist virtually.
Why does this paper matter?
Older adults are interested and able to complete video visits, but often require coaching and practice to succeed. While overall access to and usage of virtual care continues to increase, data shows a widening digital divide between older adults and younger ones using video visits. Having an in-home team member provided us a new vantage point, a behind-the-scenes look at facilitators and barriers to video visits for older adults, to offer evidence-based solutions to clinicians to begin to address these gaps.
ACKNOWLEDGMENTS
We would like to recognize members of our Bronx, NY and Bedford, MA study teams who have been involved in translating this work into Phase 2 of this study. Their contributions to our next steps are invaluable.
Funding information
Office of Research and Development
SPONSOR’S ROLE
This work was funded by a VHA Health Services Research & Development IIR Award 18–286 (Co-PIs: Hung, Moo). The opinions expressed herein are those of the authors and do not necessarily reflect those of the US Government or any of its agencies.
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts to declare.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
REFERENCES
- 1.Telehealth was critical for providing services to Medicare beneficiaries during the first year of the COVID-19 pandemic. Accessed April 25, 2023. https://oig.hhs.gov/oei/reports/OEI-02-20-00520.asp
- 2.Bhatia R, Gilliam E, Aliberti G, et al. Older adults’ perspectives on primary care telemedicine during the COVID-19 pandemic. J Am Geriatr Soc. 2022;70(12):3480–3492. doi: 10.1111/jgs.18035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hastings SN, Mahanna EP, Berkowitz TSZ, et al. Video-enhanced care management for medically complex older adults with cognitive impairment. J Am Geriatr Soc. 2021;69(1):77–84. doi: 10.1111/jgs.16819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Donaghy E, Atherton H, Hammersley V, et al. Acceptability, benefits, and challenges of video consulting: a qualitative study in primary care. Br J Gen Pract. 2019;69(686):e586–e594. doi: 10.3399/bjgp19X704141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mao A, Tam L, Xu A, et al. Barriers to telemedicine video visits for older adults in independent living facilities: mixed methods cross-sectional needs assessment. JMIR Aging. 2022;5(2):e34326. doi: 10.2196/34326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mechanic OJ, Lee EM, Sheehan HM, et al. Evaluation of telehealth visit attendance after implementation of a patient navigator program. JAMA Netw Open. 2022;5(12):e2245615. doi: 10.1001/jamanetworkopen.2022.45615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wray CM, Van Campen J, Hu J, Slightam C, Heyworth L, Zulman DM. Crossing the digital divide: a veteran affairs program to distribute video-enabled devices to patients in a supportive housing program. JAMIA Open. 2022;5(2):ooac027. doi: 10.1093/jamiaopen/ooac027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.COVID-19 experiences among the Medicare population. Summer 2020. https://www.cms.gov/files/document/medicare-current-beneficiary-survey-summer-2020-covid-19-data-snapshot.pdf
- 9.COVID-19 experiences among the Medicare population. Winter 2021. https://www.cms.gov/files/document/medicare-current-beneficiary-survey-covid-19-data-snapshot-infographic-winter-2021.pdf
- 10.Frydman JL, Li W, Gelfman LP, Liu B. Telemedicine uptake among older adults during the COVID-19 pandemic. Ann Intern Med. 2022;175(1):145–148. doi: 10.7326/M21-2972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hawley CE, Genovese N, Owsiany MT, et al. Rapid integration of home telehealth visits amidst COVID-19: what do older adults need to succeed? J Am Geriatr Soc. 2020;68(11):2431–2439. doi: 10.1111/jgs.16845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coe AB, Rowell BE, Whittaker PA, et al. Impact of an area agency on aging pharmacist-led community care transition initiative. J Am Pharm Assoc. 2023;63(4):1230–1236.e1. doi: 10.1016/j.japh.2023.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated consolidated framework for implementation research based on user feedback. Implement Sci. 2022;17(1):75. doi: 10.1186/s13012-022-01245-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21. doi: 10.1186/s13012-015-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grant C, Osanloo A. Understanding, selecting, and integrating a theoretical framework in dissertation research: developing a “blueprint” for your ‘house’. Adm Issues J. 2015;4. doi: 10.5929/2014.4.2.9 [DOI] [Google Scholar]
- 17.Mate KS, Berman A, Laderman M, Kabcenell A, Fulmer T. Creating age-friendly health systems – a vision for better care of older adults. Healthcare. 2018;6(1):4–6. doi: 10.1016/j.hjdsi.2017.05.005 [DOI] [PubMed] [Google Scholar]
- 18.Mate K, Fulmer T, Pelton L, et al. Evidence for the 4Ms: interactions and outcomes across the care continuum. J Aging Health. 2021;33(7–8):469–481. doi: 10.1177/0898264321991658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42. [DOI] [PubMed] [Google Scholar]
- 20.Hawley CE, Triantafylidis LK, Paik JM. The missing piece: clinical pharmacists enhancing the interprofessional nephrology clinic model. J Am Pharm Assoc. 2019;59(5):727–735. doi: 10.1016/j.japh.2019.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zulman DM, Piette JD, Jenchura EC, Asch SM, Rosland AM. Facilitating out-of-home caregiving through health information technology: survey of informal caregivers’ current practices, interests, and perceived barriers. J Med Internet Res. 2013;15(7):e123. doi: 10.2196/jmir.2472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Damschroder LJ, Lowery JC. Evaluation of a large-scale weight management program using the consolidated framework for implementation research (CFIR). Implement Sci. 2013;8:51. doi: 10.1186/1748-5908-8-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamilton AB, Finley EP. Qualitative methods in implementation research: an introduction. Psychiatry Res. 2019;280:112516. doi: 10.1016/j.psychres.2019.112516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watkins DC. Rapid and rigorous qualitative data analysis: the “RADaR” technique for applied research. Int J Qual Methods. 2017;16(1):160940691771213. doi: 10.1177/1609406917712131 [DOI] [Google Scholar]
- 25.Castleberry A, Nolen A. Thematic analysis of qualitative research data: is it as easy as it sounds? Curr Pharm Teach Learn. 2018;10(6):807–815. doi: 10.1016/j.cptl.2018.03.019 [DOI] [PubMed] [Google Scholar]
- 26.Watt JA, Fahim C, Straus SE, Goodarzi Z. Barriers and facilitators to virtual care in a geriatric medicine clinic: a semi-structured interview study of patient, caregiver and healthcare provider perspectives. Age Ageing. 2022;51(1):afab218. doi: 10.1093/ageing/afab218 [DOI] [PubMed] [Google Scholar]
- 27.Onorato S, Joshi A, Schwartz AW. Lights, camera, action: optimizing virtual video visits to provide high-quality care. J Gen Intern Med. 2021;36(6):1751–1754. doi: 10.1007/s11606-020-06278-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Şahin E, Yavuz Veizi BG, Naharci MI. Telemedicine interventions for older adults: a systematic review. J Telemed Telecare. 2021:1357633X211058340. doi: 10.1177/1357633X211058340 [DOI] [PubMed] [Google Scholar]
- 29.Dryden EM, Kennedy MA, Conti J, et al. Perceived benefits of geriatric specialty telemedicine among rural patients and caregivers. Health Serv Res. 2023;58(suppl 1):26–35. doi: 10.1111/1475-6773.14055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Powers BB, Van Zuilen RM, Schwartz AW, et al. Competencies for video telemedicine with older adult patients. J Am Geriatr Soc. 2023;71(4):1283–1290. doi: 10.1111/jgs.18246 [DOI] [PubMed] [Google Scholar]
- 31.Moo LR. Home video visits: two-dimensional view of the geriatric 5 M’s. J Am Geriatr Soc. 2020;68(11):2425–2427. doi: 10.1111/jgs.16843 [DOI] [PubMed] [Google Scholar]
- 32.Moo LR, Schwartz AW. The urgent need for rigorous studies of telehealth for older adults who are homebound. JAMA Netw Open. 2021;4(9):e2113451. doi: 10.1001/jamanetworkopen.2021.13451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Danila MI, Sun D, Jackson LE, et al. Satisfaction with modes of telemedicine delivery during COVID-19: a randomized, single-blind, parallel group, noninferiority trial. Am J Med Sci. 2022;364(5):538–546. doi: 10.1016/j.amjms.2022.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wardlow L, Roberts C, Archbald-Pannone L; The Collaborative for Telehealth and Aging. Perceptions and uses of telehealth in the Care of Older Adults. Telemed J E Health. 2023;29(8):1143–1151. doi: 10.1089/tmj.2022.0378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res. 2006;8(2):e9. doi: 10.2196/jmir.8.2.e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. CFIR constructs and related codes from our analysis. This table shows how each CFIR construct was related to categories in our thematic analysis, with examples of matching codes that were either pre-determined or emerged from our fieldnotes.


