Abstract
Background:
Higher education attempts to ameliorate the learning experience through match between learning subjects and students’ learning styles.
Aim:
This study evaluates the efficacy of three different instructional modalities aimed at teaching veterinary students how to make simple suture knots.
Methods:
A cohort of 43 fourth-year students were split into 3 groups and provided with different instructional modalities: presentation with pictures and descriptions, hard copy text, and muted video. The student’s surgical simulation performance was evaluated. Then, they answered a 23 question-survey, Fleming VARK questionnaire based, investigating their learning profile. Kruskal Wallis test evaluated different instructional modalities effect on student’s performance. The chi-square test assessed differences between instructional modalities and learning profiles, profile self evaluation, and training session comprehension.
Results:
Students showed auditory unimodal VARK profile (16/43), did not know their learning profile (26/43), and favored personalized teaching strategies (43/43). No differences were found for: surgical performance, except for forceps handling; and between instructional modalities: either for learning profiles (p-value = 0.43), or profile self evaluation (p-value = 0.42). Differences were found between instructional modalities and training session comprehension. As limitations, auditory instructional modalities, participants’ age, and gender were not recorded or evaluated.
Conclusion:
Our study provides feedback on modern teaching modalities in which students play a key role. Participants showed a variety of learning profiles although displaying no significant performance differences.
Keywords: Learning styles, Veterinary students, Higher education, VARK
Introduction
Learning styles are a composite of cognitive, affective, and physiological features that enable the learner to understand, interact with, and respond to the environment (Baykan and Nacar, 2007). The latest educational research highlights that everyone has a unique learning style (Murphy et al., 2004). Recent studies have highlighted the utility of understanding students’ different learning styles to solve learning problems and markedly improve the effectiveness of lectures (Collins, 2004; Kim and Gilbert, 2015).
With this aim, various evaluation models of learning style have been investigated, including the Fleming VARK model (Fleming, 1995). With this model, students are categorized according to how they prefer to acquire new information, as the expression of sensory modalities (Fleming, 1995; Shenoy et al., 2013; Kim and Gilbert, 2015; Retrosi et al., 2019). For example (Fleming, 1995): visual (V), which means that students prefer to learn using printed information, flow charts and diagrams; auditory (A), meaning that students prefer to learn from spoken words, tutorials and discussions; read and write (R), meaning students prefer printed words, reading and written texts, such as textbooks and notes; and kinaesthetic (K), where students prefer to learn through sensory experiences, by handling or using objects, and through simulations of real life activities. A multiple-choice survey provides a profile of the learning style (Forrest, 2004). The validity of the different categorizations used in the VARK model has been demonstrated across a broad spectrum of populations (Lujan and DiCarlo, 2006; Alkhasawneh et al., 2008, Leite et al., 2010; Koch et al., 2011; Horton et al., 2012; Alkhasawneh, 2013).
Today, students greatly enjoy and actively take part in all learning style-based groups and active educational programs. Thus, the kinaesthetic learning style seems better than traditional teaching methods for today’s students (Kim et al., 2018). Kim and colleagues reported how resident surgery students showed different learning styles compared to the general population of students, and that the group of resident students with an auditory profile achieved greater progress in their training (Kim et al., 2018).
Recent systematic reviews compared different simulation-based instructional design features, and highlighted the following as best practices for simulation-based education: repetitive practice, cognitive interactivity, multiple learning strategies, feedback, and individualized learning (Cook et al., 2013).
However, especially in higher education, it is not possible for teachers to follow each individual learning style (Newton, 2015; Newton and Miah, 2017). Higher education attempts to tailor the learning experience to students thanks to more efficient and effective teaching strategies (Romanelli et al., 2009, Prithishkumar and Michael, 2014). A better match between the teacher, subjects, and styles will have a greater impact on a wider population of students. However, to date, it is not known which method is the most effective at engaging the attention of students.
The aim of the present study was to evaluate the efficacy of three different instructional modalities used to teach a cohort of fourth-year veterinary medicine students how to make simple suture knots.
Materials and Methods
The present prospective research was conducted for 3 months (from March 2021 to May 2021), at the clinical Skill-Lab, Department of Veterinary Sciences, University of Pisa, Italy.
Study population
In the present study, 43 undergraduate students attending to the course class of the fourth year of a master’s degree course in Veterinary Medicine were enrolled. The students who were invited to participate in this study underwent the scheduled training session on surgical pathology, part of the module of the integrated course of surgical pathology and semeiotics, and diagnostic imaging. The inclusion criteria were as follows: the student should attend the surgical training session for the first time, the planned surgical procedure should be entirely ultimate and the learning profile survey fully filled and submitted at the end of the session. Moreover, all students provided informed consent before participating in accordance with the Declaration of Helsinki, and the study was approved by the Bioethical Committee of the University of Pisa (Review No. 18/2021).
Surgical simulation
During the training session, the students had to learn one individual surgical skill: how to perform a simple interrupted stitch. The class was randomly split into three groups: Group A (GA) (14/43 students), Group B (GB) (15/43 students), and Group C (GC) (14/43 students).
Before starting the training session, each group was provided with one of the three different instructional modalities materials that explained the technique, of “how to perform a simple interrupted stitch,” based on the current literature for surgical skill practice (Fossum, 2019). The learning materials were administered in the following formats: a Power Point presentation with pictures and accompanying text for Group A, hard copy text for Group B, and muted video for Group C. Each student had 30 minutes to understand and memorize the surgical procedure, before performing it. The surgical simulation was carried out on a three layer suture pad held by a tensioning base (SurgiReal Products, Inc, Loveland, Colorado), and all the students used the same surgical instruments: a mayo hegar needle holder, a tissue forceps, mayo scissors, and a cutting needle threaded with 3-0 non absorbable nylon suture. Each student carried out the surgical procedure individually, and the other participants were not allowed to assist or participate, to prevent any experience exchange.
During the surgical simulation, each student’s performance was individually assessed and blind judged by an experienced operator (G.B.). Table 1 lists the surgical steps that were evaluated for each performance.
Table 1. Surgical technique steps scored for each student group.
| Surgical steps | Instrument use | Needle holder grip |
| Forceps grip | ||
| Needle placement | ||
| Scissor use | ||
| Execution technique | Needle pierce | |
| First knot tying | ||
| Second knot tying | ||
| Third knot tying |
Since no previous studies are available in the literature, each surgical step was scored according to a grading scale specifically designed for this study, from 1 to 4 (Table 2).
Table 2. Scores of the surgical technique steps.
| Surgical technique step score | |
|---|---|
| 1 | In no way, never |
| 2 | Sometimes, little |
| 3 | Sufficient, most of the time |
| 4 | Much, always |
No time limitation was set for the completion of the surgical simulation.
The learning profile survey
After the surgical simulation, each student was asked to complete an anonymous 23-question survey, investigating the characteristics of their learning profile. A learning style was established for each participant using the Fleming VARK (V = visual, A = auditory, R = read/write, or K = kinaesthetic) questionnaire version 7.1 (Kim and Gilbert, 2015, Retrosi et al., 2019), which consisted of 16 multiple choice questions, with four possible answers. For each question, students could select one or more answers.
Seven additional questions were added to the VARK survey to assess the student’s experience of the training session, the degree of satisfaction, and the student’s knowledge of their own learning style, as shown in Table 3.
Table 3. A total of 7 questions which were added to each VARK survey to assess the student’s experience of the training session, the degree of satisfaction, and the student’s knowledge of their own learning style.
| Questions | Answers |
|---|---|
| 1. Profile self evaluation. How do you think you learn best? |
a. Reading from a book and taking notes. |
| b. Listening to someone’s explanations. | |
| c. Learning from flow charts and diagrams. | |
| d. Learning by practicing. | |
| 2. Learning materials. What kinds of learning material were you provided with? |
a. Hard copy text. |
| b. Pictures and text. | |
| c. Podcast | |
| d. Muted video. | |
| 3. Previous experience. Have you already had practise with simple interrupted surgical stitches? |
a. Yes. |
| b. No. | |
| 4. Skill level. How do you consider your skill level? |
a. Scarce. |
| b. Sufficient. | |
| c. Good. | |
| d. Excellent. | |
| 5. Understanding of teaching session. Did you think the teaching was easy to understand? |
a. Yes. |
| b. No. | |
| 6. Teaching session score. How would do you score the session? |
a. 1, poor/negative |
| b. 2, fairy | |
| c. 3, good | |
| d. 4, very good | |
| c. 5, excellent/positive | |
| 7. Usefulness of personalised teaching strategies. Do you think personalised teaching strategies would be useful? |
a. Yes. |
| b. No. |
The questionnaire was provided as a hard copy, on which the students had to record their answers. No interaction among the students was permitted and no clarifications of the questions were offered. The students had a time limit of 15 minutes to fill in the questionnaire. To minimize any potential bias, the students completed and submitted the survey immediately after the training session.
The surveys were then evaluated by an individual operator, and answers were recorded. The learning style profiles were categorized as unimodal for each learning style, or as multimodal, which could encompass any combination of 2, 3, or all 4 of the unimodal learning styles. The self-evaluation profile answers were then matched with the actual learning profile shown from the corresponding survey, and the results were recorded as yes/no answers.
Statistical analysis
To detect the number of required students, a chi-square analysis was applied using G-power software (Ver. 3.1, Heinrich-Heine-Universität, Düsseldorf, Germany). An effect size of 0.5 (medium), α error of 5% (type I), a confidence interval of 95%, and a test power of 80% were used. The minimum sample size was 39 students, which was increased by 10%. The number of survey answers was registered and detailed, for each student group. The effect of the different teaching materials on the surgical simulation score was estimated by the Kruskal Wallis test and Dunn’s multiple comparison tests as a post-hoc analysis. Differences between the different teaching materials administered and the learning profile, self-evaluation profile, and training comprehension were assessed respectively, using a chi-square test. Statistical significance was set at p < 0.05. Statistical analysis was performed using Rstudio software (SAS, Boston, MA, US).
Ethical approval
The study protocol was approved by the Bioethical Committee of the University of Pisa (Review No. 18/2021), and all the participants provided informed consent in accordance with the Declaration of Helsinki.
Results
All the students completed the surgical simulation (43/43 students) and the survey (43/43 questionnaires). The survey results obtained for each group are summarized in Table 4.
Table 4. Survey results recorded for each group.
| Group | GA (n = 14) |
GB (n = 15) |
GC (n = 14) |
Total (n = 43) |
||
|---|---|---|---|---|---|---|
| Questions | ||||||
| VARK learning profile | Unimodal | A | 5 | 5 | 6 | 16 |
| R | 3 | 3 | 2 | 8 | ||
| K | 3 | 1 | 2 | 6 | ||
| V | 0 | 2 | 0 | 2 | ||
| Multimodal | A+K | 2 | 1 | 1 | 4 | |
| A+R | 0 | 0 | 2 | 2 | ||
| A+V | 0 | 1 | 0 | 1 | ||
| K+V | 0 | 1 | 0 | 1 | ||
| K+R | 0 | 1 | 0 | 1 | ||
| R+V | 1 | 0 | 0 | 1 | ||
| A+K+R | 0 | 0 | 1 | 1 | ||
| Learning profile and self evaluation match | Yes | 6 | 4 | 7 | 17 | |
| No | 8 | 11 | 7 | 26 | ||
| Learning materials | Hard copy text | 0 | 15 | 0 | 15 | |
| Pictures and text | 14 | 0 | 0 | 14 | ||
| Podcast | 0 | 0 | 0 | 0 | ||
| Muted video | 0 | 0 | 14 | 14 | ||
| Previous experience | Yes | 14 | 15 | 13 | 42 | |
| No | 0 | 0 | 1 | 1 | ||
| Skill level | Scarce | 7 | 13 | 12 | 32 | |
| Sufficient | 6 | 2 | 2 | 10 | ||
| Good | 1 | 0 | 0 | 1 | ||
| Excellent | 0 | 0 | 0 | 0 | ||
| Understanding of teaching session | Yes | 13 | 9 | 14 | 36 | |
| No | 1 | 6 | 0 | 7 | ||
| Teaching session score | 1 | 0 | 0 | 0 | 0 | |
| 2 | 1 | 1 | 0 | 2 | ||
| 3 | 2 | 5 | 2 | 9 | ||
| 4 | 5 | 6 | 4 | 15 | ||
| 5 | 6 | 3 | 8 | 17 | ||
| Usefulness of personalised teaching | Yes | 14 | 15 | 14 | 43 | |
| No | 0 | 0 | 0 | 0 |
GA = power point group; GB = text group; GC = video group; V = visual, A = auditory, R = read/write; K = kinaesthetic.
The results showed a higher prevalence of the unimodal auditory profile, (16/43). The learning profile and self-evaluation match revealed that most of the students (60%, 26/43) could not identify their own learning profile, compared to 40% (17/43) of students who correctly identified it. Most of the students reported that they had a K learning profile (K = 33/43, A = 7/43, R = 2/43, V = 1/43). The great majority (42/43) of students stated that they had previous experience of performing a simple interrupted surgical stitch, but many assessed their own skill level as scarce (32/43) to sufficient (10/43). None of the instructional modalities were scored negatively (i.e., a score of only 1/5) by any of the students (0/43 questionnaires). However, groups A and C had excellent scores (5/5) in the 6/14 and 8/14 questionnaires, respectively, while in group B only 3/15 of the scores were excellent. All of the participants (43/43) expressed favorable opinions regarding the benefits of personalized teaching strategies.
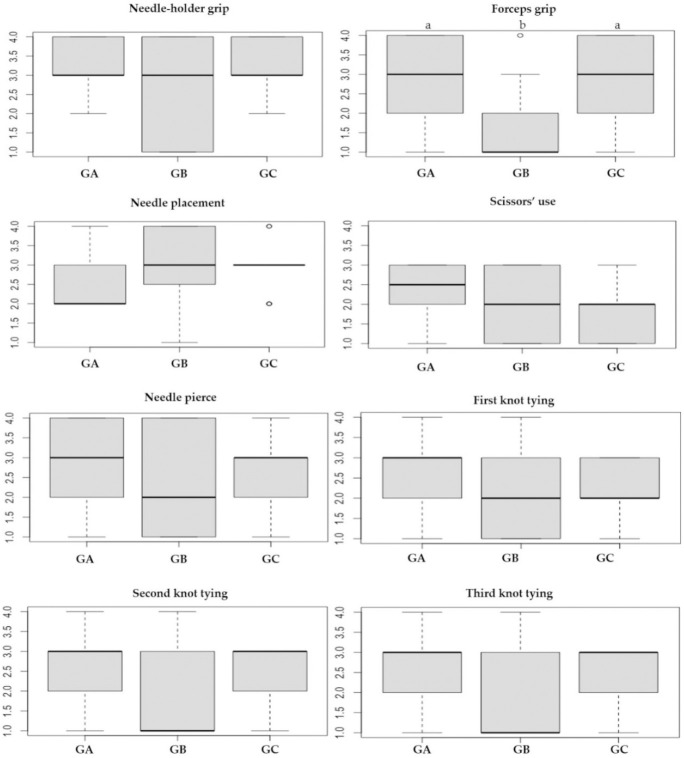
The students’ performance score results are shown in Figure 1, detailed for each step of the surgical technique. No significant statistical differences were detected between groups, except for the forceps handling, for which groups GA and GC obtained a mean value of 3, while GB obtained a mean value of 1 (p-value = 0.012).
Fig. 1. Box plot graphics showing results relative to students’ performance, scored by the judge. Forces grip shows significant differences between groups (a≠b, p-value = 0.012). GA = power point group; GB = text group; GC = video group.
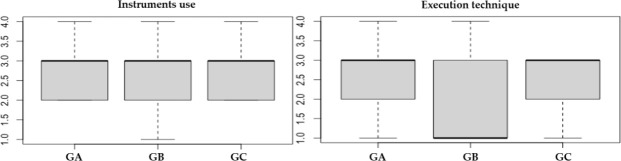
Figure 2 reports students’ performance scores summarized for instrument use and execution technique. No statistically significant differences were detected between groups, either for instrument use (p-value = 0.592) or for execution technique (p-value = 0.252).
Fig. 2. Box plot graphics showing results relative to students’ performance scored by the judge, grouped for instrument use and execution technique. GA = power point group; GB = text group; GC = video group.
No statistically significant differences were detected for the different instructional modalities administered: either for the learning profiles (p-value = 0.43) or for profile self-evaluation (p-values = 0.42). On the other hand, statistically significant differences were shown between the teaching materials administered and training session comprehension, where GA and GC showed a statistically significant higher score compared to GB (p-value = 0.008).
Discussion
University education aims to reach as many students as possible thanks to the match between the teaching strategies, learning subjects, and styles (Romanelli et al., 2009, Prithishkumar and Michael, 2014). The present study investigated how fourth-year students of the Veterinary Medicine class responded to three different instructional modalities explaining one single surgical skill.
According to the VARK survey, most of the students of our study were unimodal auditory learners, namely they learned better by listening, instead of reading, doing, and watching schemes. Previous research, using the VARK learning style questionnaire reports contrasting results: for undergraduates in health sciences (Alkhasawneh et al., 2008; Breckler et al., 2009; James et al., 2011), and for first-year medical students (Padmalatha et al., 2022), kinaesthetic was the most common learning style profile. In contrast, 29.5% of university students from a business school (Chiclayo, Peru) preferred to receive written information for example in handouts or books (Espinoza-Poves et al., 2019). In terms of the VARK categories preferred by students, previous research has shown similar results, and wide ranges have been detected for both unimodal (13,8%–69,9%) (Husmann and O’Loughlin, 2019) and multimodal (14,3%–62%) profiles (Kim et al., 2013; Espinoza-Poves et al., 2019; Husmann and O’Loughlin, 2019).
Our study highlights a slight incongruity in the study population, in which 60% of students revealed an inability to correctly identify their learning style profile. Moreover, most of the students (33/43; 77%) reported that they were kinaesthetic learners. It has also been reported that rather than a correct match between the students’ learning profile and the educational method, what is more, important for effective learning is the correct understanding of the student’s own learning modalities (Hawk and Shah, 2007). Thus, the student who has understood his own study method will be able to acquire concepts/skills even if presented through a not-preferred teaching method (Hawk and Shah, 2007).
In our study, there were no significant differences between each group in terms of surgical score performance. The only exception was for forceps handling; in this case, students of GC and GA performed better compared with the GB. Interestingly, the students belonging to GB evaluated the teaching modality with a lower score compared to the other two groups. It is possible that a text description might be inadequate to teach practical surgical skills. Previous studies have found contrasting results on this issue. Academic performance was found not to be associated with learning style (Espinoza-Poves et al., 2019). However, Foster and colleagues showed that veterinary students with an auditory style consistently performed less well in all types of university course assessments (p < 0.05) (Foster et al., 2010). Recent studies have highlighted that practical learning activities might lead to intrinsic differences, since medical anatomy students who performed best in practices were kinaesthetic, visual, auditory as well as multimodal learners (Padmalatha et al., 2022), and general surgery residents mainly showed a multimodal profile (Kim et al., 2013).
Our results also show that hard copy text modalities were penalized by student scores and led to a slightly worse performance, compared to the other strategies. This highlights how practical learning would be better perceived and enjoyed through videos, photos, and hands-on practice (Kim et al., 2013; Padmalatha et al., 2022). Personalized teaching seems to be commonly accepted by students, suggesting that teachers should adapt the learning sessions to the preferences of students (Espinoza-Poves et al., 2019). Although this could lead to optimal student performance, on the other hand, it might be very challenging for the trainer, given the heterogeneous nature of different learners.
The present study has some limitations. The auditory learning material was not included within the teaching modalities (i.e., in the form of podcast recording), thus, its potential as a teaching method was not tested. Since most of our students affirmed to be auditory learners, it would have been interesting to check whether they might have performed better if the learning material had been provided as a podcast. Comparison between the three modalities tested in the present study and the current teaching standard was not evaluated, which might limit the chance to assess the efficacy of different instructional modalities. Moreover, the participants’ age was not recorded or evaluated. This might represent a limitation since a relationship between age and learning style has been demonstrated. A single learning profile predominated in younger students (aged 18–23 years old) (Espinoza-Poves et al., 2019), while a multimodal learning style predominated in older students (aged 24–26 years old) (Espinoza-Poves et al., 2019). Martín and Rodríguez reported that as people get older (Martín-García, 2003), they lose their dominant character and start to combine different styles according to the particular phase of their lives. In addition, gender was not recorded. However, no significant association between learning style and sociodemographic variables has been reported (i.e., sex, marital status, and level of education) (Martín-García, 2003).
The present study highlights a generally low-performance score in our student population. This might be because knowledge of surgical skills is strictly dependent on how often the surgical procedure is repeated and on experience. Recent studies reported that the sequence of steps and overall standardization of surgical procedures are key to make learners deal with procedural training and positively increasing surgical quality (Apramian et al., 2015, 2016; Fesco et al., 2017).
In conclusion, the educational modalities provided might be insufficient to cover the students’ learning needs. Moreover, in our study, the undergraduate teaching strategies were evaluated through the personal opinions of students and through an objective evaluation of their performance. This is essential feedback for modern teaching methods, in which the students play an active role. As a future goal, research on a similar high educational level of students could investigate how matching the correct student learning profile with appropriate instructional modalities might help the learner in his education; especially, how auditory teaching modalities could be more effective in terms of communication and learning.
Acknowledgments
None.
Conflict of interest
The authors declare that there is no conflict of interest.
Authors’ contributions
Valentina Vitale, Giovanni Barsotti, Irene Nocera, and Micaela Sgorbini conceived the study, developed the methodology, and distributed the survey. All authors contributed to the interpretation and conducted the data analysis. Valentina Vitale and Irene Nocera wrote the first draft of the manuscript, and all authors contributed to the manuscript revisions and approved the submitted version.
Funding
This research received no specific grant.
Data availability
The data presented in this study are available on request from the corresponding author.
References
- Alkhasawneh E. Using VARK to assess changes in learning preferences of nursingstudents at a public university in Jordan: implications for teaching. Nurse Educ. Today. 2013;33:1546. doi: 10.1016/j.nedt.2012.12.017. [DOI] [PubMed] [Google Scholar]
- Alkhasawneh I.M., Mrayyan M.T., Docherty C., Alashram S., Yousef H.Y. Problem-based learning (PBL): assessing students’ learning preferences using VARK. Nurse Educ. Today. 2008;28:572. doi: 10.1016/j.nedt.2007.09.012. [DOI] [PubMed] [Google Scholar]
- Apramian T., Cristancho S., Watling C., Ott M., Lingard L. Thresholds of principle and preference: exploring procedural variation in postgraduate surgical education. Acad. Med. 2015;90:S70–S76. doi: 10.1097/ACM.0000000000000909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apramian T., Cristancho S., Watling C., Ott M., Lingard L. “They Have to Adapt to Learn”: Surgeons’Perspectives on the role of procedural variation in surgical education. J. Surg. Educ. 2016;73:339–347. doi: 10.1016/j.jsurg.2015.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baykan Z., Nacar M. Learning styles of first-year dental students attending Erciyes University in Kayseri, Turkey. Adv. Physiol. Edu. 2007;31:158–160. doi: 10.1152/advan.00043.2006. [DOI] [PubMed] [Google Scholar]
- Breckler J., Joun D., Ngo H. Learning styles of physiology students interested in the health professions. Adv. Physiol. Educ. 2009;33:30–36. doi: 10.1152/advan.90118.2008. [DOI] [PubMed] [Google Scholar]
- Collins J. Education techniques for lifelong learning: principles of adult learning. Radiographics. 2004;4:1483–1489. doi: 10.1148/rg.245045020. [DOI] [PubMed] [Google Scholar]
- Cook D.A., Hamstra S.J., Brydges R., Zendejas B., Szostek J.H., Wang A.T., Erwin P.J., Hatala R. Comparative effectiveness of instructional design features in simulation-based education: systematic review and meta-analysis. Med. Teacher. 2013;35(1):e867–e898. doi: 10.3109/0142159X.2012.714886. [DOI] [PubMed] [Google Scholar]
- Espinoza-Poves J.L., Miranda-Vílchez W.A., Chafloque-Céspedes R. The Vark learning styles among university students of business schools. J. Educ. Psychol. Propositos Representaciones. 2019;7:401–415. [Google Scholar]
- Fesco A.B., Szasz P., Kerezov G., Grantcharov T.P. The effect of technical performance on patient outcomes in surgery. Ann. Surg. 2017;265:492–501. doi: 10.1097/SLA.0000000000001959. [DOI] [PubMed] [Google Scholar]
- Fleming N.D. I’m different; not dumb. Modes of presentation (VARK) in the tertiary classroom. In: Zelmer A, editor. Research and development in higher education. Proceedings of the 1995. Annual Conference of the Higher Education and Research Development Society of Australasia (HERDSA) Volume 18. HERDSA; 1995. pp. 308–313. [Google Scholar]
- Forrest S. Learning and teaching: the reciprocal link. J. Contin. Educ. Nurs. 2004;35:74–79. doi: 10.3928/0022-0124-20040301-09. [DOI] [PubMed] [Google Scholar]
- Fossum T. 5th. Philadelphia, PA: Elsevier; 2019. Small animal surgery. [Google Scholar]
- Foster N., Gardner D., Kydd J., Robinson R., Roshier M. Assessing the influence of gender, learning style, and pre-entry experience on student response to delivery of a novel veterinary curriculum. J. Vet. Med. Educ. 2010;37:266–275. doi: 10.3138/jvme.37.3.266. [DOI] [PubMed] [Google Scholar]
- Hawk T.F., Shah A.J. Using learning style instruments to enhance student learning. Decis. Sci. J. Innov. Educ. 2007;5:1–19. [Google Scholar]
- Horton D.M., Wiederman S.D., Saint D.A. Assessment outcome is weakly correlated with lecture attendance: influence of learning style and use of alternative materials. Adv. Physiol. Educ. 2012;36:108. doi: 10.1152/advan.00111.2011. [DOI] [PubMed] [Google Scholar]
- Husmann P.R., O’Loughlin V.D. Another nail in the coffin for learning styles? disparities among undergraduate anatomy students’ study strategies, class performance, and reported VARK learning styles. Anat. Sci. Educ. 2019;12:6–19. doi: 10.1002/ase.1777. [DOI] [PubMed] [Google Scholar]
- James S., D’Amore A., Thomas T. Learning preferences of first year nursing and midwifery students: utilising VARK. Nurs. Educ. Today. 2011;313:417–423. doi: 10.1016/j.nedt.2010.08.008. [DOI] [PubMed] [Google Scholar]
- Kim R.H., Gilbert T. Learning style preferences of surgical residency applicants. J. Surg. Res. 2015;198:61–65. doi: 10.1016/j.jss.2015.05.021. [DOI] [PubMed] [Google Scholar]
- Kim R.H., Gilbert T., Ristig K., Chu Q.D. Surgical resident learning styles: faculty and resident accuracy at identification of preferences and impact on ABSITE scores. J. Surg. Res. 2013;184:31–36. doi: 10.1016/j.jss.2013.04.050. [DOI] [PubMed] [Google Scholar]
- Kim R.H., Viscusi R.K., Collier A.N., Hunsinger M.A., Shabahang M.M., Fuhrman G.M., Korndorffer J.R. Learning preferences of surgery residents: a multi-institutional study. Surgery. 2018;163:901–905. doi: 10.1016/j.surg.2017.10.031. [DOI] [PubMed] [Google Scholar]
- Koch J., Salamonson Y., Rolley J.X., Davidson P.M. Learning preference as a predictor of academic performance in first year accelerated graduate entry nursing students: a prospective follow-up study. Nurse. Educ. Today. 2011;31:611. doi: 10.1016/j.nedt.2010.10.019. [DOI] [PubMed] [Google Scholar]
- Leite W.L., Svinicki M., Shi Y. Attempted validation of the scores of the VARK: learning styles inventory with multitraitemultimethod confirmatory factor analysis models. Educ. Psychol. Meas. 2010;70:323. [Google Scholar]
- Lujan H.L., DiCarlo S.E. First-year medical students prefer multiple learning styles. Adv. Physiol. Educ. 2006;30:13. doi: 10.1152/advan.00045.2005. [DOI] [PubMed] [Google Scholar]
- Martín-García A. Estilos de aprendizaje en la vejez. Un estudio a la luz de la teoría del aprendizaje experiencial. Rev. Esp. Geriatr. Gerontol. 2003;38:258–265. [Google Scholar]
- Murphy R.J., Gray S.A., Straja S.R., Bogert M.C. Student learning preferences and teaching implications. J. Dental. Educ. 2004;6:859–866. [PubMed] [Google Scholar]
- Newton P.M. The learning styles myth is thriving in higher education. Front. Psychol. 2015;6:1908. doi: 10.3389/fpsyg.2015.01908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton P., Miah M. Evidence-based higher education—is the learning styles ‘Myth’ Important? Front. Psychol. 2017;8:1. doi: 10.3389/fpsyg.2017.00444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padmalatha K., Kumar J.P., Shamanewadi A.N. Do learning styles influence learning outcomes in anatomy in first-year medical students? J. Family Med. Prim. Care. 2022;11:2971–2976. doi: 10.4103/jfmpc.jfmpc_2412_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prithishkumar I.J., Michael S.M. Understanding your student: using the VARK model. J. Postgrad. Med. 2014;60:183–186. doi: 10.4103/0022-3859.132337. [DOI] [PubMed] [Google Scholar]
- Retrosi G., Morris M., McGavock J. Does personal learning style predict the ability to learn laparoscopic surgery? a pilot study. J. Laparoendosc. Adv. Surg. Tech. 2019;29:98–102. doi: 10.1089/lap.2018.0196. [DOI] [PubMed] [Google Scholar]
- Romanelli F., Bird E., Ryan M. Learning styles: a review of theory, application, and best practices. Am. J. Pharm. Educ. 2009;73:9. doi: 10.5688/aj730109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shenoy N., Shenoy A., Ratnakar U.P. The perceptual preferences in learning among dental students in clinical subjects. J. Clin. Diagn. Res. 2013;7:1683. doi: 10.7860/JCDR/2013/4940.3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.