Abstract
Objectives
Implementation and sustainability of new care processes in emergency departments (EDs) is difficult. We describe experiences of implementing geriatric care processes in EDs that upgraded their accreditation level for the Geriatric Emergency Department Accreditation (GEDA) program. These EDs can provide a model for adopting and sustaining guidelines for evidence‐based geriatric care.
Methods
We performed qualitative interviews with geriatric ED nurse and physician leaders overseeing their ED's geriatric accreditation processes. The interview guide was based on the Consolidated Framework for Implementation Research (CFIR), a framework consisting of a comprehensive set of factors that impact implementation of evidence‐based interventions. We used inductive analysis to elucidate key themes from interviews and deductive analysis to map themes onto CFIR constructs.
Results
Clinician leaders from 15 of 19 EDs that upgraded accreditation status by March 1, 2023 participated in interviews. Motivations to upgrade accreditation level centered on improving patient care (73%) and achieving recognition (56%). Rationales for choosing specific care processes were more commonly related to feasibility (40%) and ability to integrate the processes into the electronic health record (33%) than to site‐specific patient needs (20%). Several common experiences in implementation were identified: (1) financing from the larger health system or philanthropy was crucial; (2) translating the Geriatric ED Guidelines into clinical practice was challenging for clinician leaders; (3) motivational barriers existed among frontline ED staff; (4) longitudinal staff education was needed given frontline ED staff attrition and turnover; and (5) the electronic health record facilitated implementation of geriatric screenings.
Conclusions
Geriatric ED accreditation involves significant time, resource allocation, and longitudinal staff commitment. EDs pursuing geriatric accreditation balance aspirations to improve patient care with resource availability to implement new care processes and competing priorities.
Keywords: emergency medicine, geriatric emergency department accreditation, geriatrics, implementation science, qualitative, screening
1. INTRODUCTION
1.1. Background
Over 20% of emergency department (ED) visits are by older adults. 1 Geriatric ED Accreditation (GEDA) is a program that formally recognizes EDs that implement best practices related to geriatric‐specific staffing, education, care processes, infrastructure changes, and quality improvement metrics. GEDA requirements are based on the Geriatric ED Guidelines, a set of evidence‐ and consensus‐based recommendations developed by leading national organizations in emergency medicine and geriatrics in 2014. 2 EDs can select care processes from the guidelines based on local needs and capabilities, and then through a formal application and evaluation process, they receive designation from the American College of Emergency Physicians (ACEP) as level 1, 2, or 3 depending on the extent of care processes, specialized staffing, equipment, and environmental changes they adopt. Since the initiation of GEDA in 2017, 418 EDs worldwide have achieved geriatric accreditation with the majority being level 3 geriatric EDs. 3 While less than 10% of the approximately 5500 EDs in the United States are currently geriatric accredited, the movement is growing.
1.2. Importance
Research on GEDA to date has evaluated the impact of geriatric accredited EDs on healthcare utilization and costs of care 4 , 5 , 6 or has described the care processes implemented. 7 , 8 Less is known about institutions’ experiences implementing care processes required for accreditation. One single‐site implementation‐focused study found that frontline ED staff faced motivational barriers and desired more infrastructure and equipment to support care processes. 9 Scholarship has also highlighted how health system‐level support and structured mentoring programs in the Veterans Health Administration and a New York health system facilitated local institutional changes required for acccreditation. 10 , 11 Individual sites’ motivations for pursuing accreditation and their implementation experiences remain largely uncharacterized.
1.3. Goals of this investigation
We performed a qualitative study with EDs that upgraded their level of accreditation, that is, went from level 3 to 2 or level 2 to 1 status. Our study goal was to understand motivations for upgrading, rationales for choosing specific care processes, and implementation experiences. We focused on upgraded sites for three reasons. First, 85% of geriatric EDs have level 3 accreditation, which at the time of the study required only one care process. Upgraded sites have experience implementing 10–20 care processes. Second, focusing on upgraded sites, rather than those maintaining their accreditation level, can provide insights into how perceived return on investment impacts selection and implementation of additional geriatric care processes. Third, implementation experiences in upgraded sites may provide insights into how EDs can expand, rather than simply maintain, geriatric care processes. Upgraded sites can serve as models for how to navigate, uphold, and increase time and resource commitments required for accreditation. Such lessons can inform EDs seeking to pursue and/or upgrade geriatric accreditation.
2. METHODS
We performed a qualitative interview‐based study with clinicians who led their institution's GEDA upgrade. Our qualitative approach was rooted in case study‐based research, which refers to in‐depth examination of an individual, institution, or small group of individuals or institutions that experience a unique phenomenon of interest. 12 Research is reported using the Consolidated Reporting Qualitative (COREQ), with checklist provided as Supporting Information Appendix A. 13 The Institutional Review Board of Baylor College of Medicine provided ethics approval (H‐50838).
2.1. Study setting and sample selection
We developed an interview guide (Supporting Information Appendix B) based on a framework designed for health services implementation called the Consolidated Framework for Implementation Research (CFIR) 1.0. CFIR offers a comprehensive set of factors that impact implementation of healthcare innovations. 14 We asked participants about motivations for geriatric ED accreditation/upgrade and experiences selecting and implementing care processes with particular attention to geriatric screenings, a commonly selected 7 , 8 and highly structured process in geriatric EDs. 2 Our interview questions addressed the five domains outlined in CFIR: (1) intervention characteristics, that is, attributes of the intervention being adopted; (2) outer setting, that is, the external environment; (3) inner setting, that is, the work environment; (4) individuals, that is, the people involved; and (5) process, that is, the activities used to carry out the innovation. Within CFIR domains, the researchers chose specific constructs as foci of the interview based on prior experiences leading geriatric healthcare improvements. We pilot tested questions with an emergency physician from a geriatric‐accredited ED.
We aimed to obtain a comprehensive sample of interviewees from the 19 sites that successfully upgraded accreditation status by study initiation in March 2023. Based on a roster of upgraded sites on the GEDA website, we emailed site contacts. In this study, we prioritized obtaining perspectives of individuals directly involved with implementation and familiar with ground‐level barriers and facilitators encountered in routine, daily ED operations. Therefore, we sought to interview physicians and nurses with leadership positions in their institution's geriatric ED operations and accreditation application process.
2.2. Data collection
Semistructured interviews were performed by a public health professional (VR) with formal qualitative research training and no formal role in GEDA/ACEP. Interviews were conducted by videoconference and digitally audio‐recorded. Recordings were transcribed using the artificial intelligence program Otter.ai, edited for accuracy, and de‐identified.
2.3. Data analysis
We performed a thematic content analysis, which aims to uncover and quantify patterns of repeated meaning. 15 We began by using an inductive approach, in which themes emerge from participants’ responses. First, we reviewed all transcripts and developed a coding scheme through consensus discussions (Supporting Information Appendix C). Subsequently, two researchers independently coded each transcript and organized data in a matrix using Microsoft Excel (AB, VR). A senior qualitative researcher (ANC) adjudicated discrepancies. We subsequently held consensus discussions to elucidate themes and map them onto CFIR constructs using a deductive approach that analyzes data based on pre‐existing codes or frameworks. For data analysis, we used CFIR 2.0 constructs, as revision of the framework occurred in the period between initial design of the interview guide and data analysis. 16 Changes from CFIR 1.0 to 2.0 were related to sharpening definitions related to the outer and inner setting of implementation and reorganizing constructs related to individuals involved with implementation. CFIR 1.0 constructs used to frame the interview guide map onto CFIR 2.0 constructs without significant changes.
As we aimed to include as many institutions as possible that had successfully upgraded, we performed data analysis after all interviews were completed rather than conducting interviews until thematic saturation, or the point at which no new information emerges. To ensure we had achieved thematic saturation, we used a base of themes uncovered from the first six interviews and examined the number of new themes that emerged with each additional interview performed. 17 We achieved thematic saturation by 12 interviews.
The Bottom Line
Among 15 American College of Emergency Physicians (ACEP)‐accredited Geriatric Emergency Departments (EDs) who upgraded their accreditation level by March 2023, most (73%) were motivated to upgrade to improve patient care, but in terms of care improvement programs pursued, most EDs (40%) selected “low hanging fruit” programs while only 20% selected based on patient needs. Although funding and resources influenced care program choices, the needs of the patients must be paramount.
3. RESULTS
Twenty individuals representing 15 EDs completed interviews. The response rate was 71% at the individual level (n = 20 of 28) and 79% at the institutional level (n = 15 of 19 institutions). Interviews lasted an average of 33 min.
All participants were ED physicians or nurses. Among institutions represented in the sample, the proportion of annual ED visits by geriatric patients ranged from 20% to 60%. Five EDs had upgraded from level 2 to 1, and 10 from level 3 to 2 accreditation. Most EDs were urban and located in socioeconomically advantaged areas based on the Area Deprivation Index. 18 Characteristics of individuals and institutions are outlined in Table 1.
TABLE 1.
Characteristics of interviewees and emergency departments with upgraded geriatric accreditation status.
| Interviewee characteristics, n = 20 | % (N) |
|---|---|
| Clinical profession of interviewee | |
| Nurse | 50 (10) |
| Physician | 50 (10) |
| Emergency department characteristics, n = 15 | |
|---|---|
| ED accreditation level | |
| Level One | 33 (5) |
| Level Two | 66 (10) |
| Teaching Institution | 60 (9) |
| Location | |
| Urban | 87 (13) |
| Rural | 13 (2) |
| Area Deprivation Index (national), n = 13 a | |
| 1–10 (least socioeconomically disadvantaged) | 7 (1) |
| 11–20 | 46 (6) |
| 21–30 | 15 (2) |
| 31–40 | 0 (0) |
| 41–50 | 0 (0) |
| 51–60 | 7 (1) |
| 61–70 | 7 (1) |
| 71–80 | 7 (1) |
| 81–90 | 0 (0) |
| 91–100 (most socioeconomically disadvantaged) | 7 (1) |
Abbreviation: ED, emergency department.
Data were unavailable for two EDs.
Sites commonly chose to adopt geriatric screenings as care processes to fulfill requirements for accreditation upgrade. 8 Table 2 describes the proportion of EDs in our sample performing key geriatric screening types by upgraded accreditation level (falls, elder abuse, polypharmacy, delirium, dementia, and frailty/risk for adverse health outcomes).
TABLE 2.
Geriatric screenings performed in sample EDs by accreditation level.
| Type of screening | Level 1 EDs (n = 5) | Level 2 EDs (n = 10) |
|---|---|---|
| Delirium | 100% (5) | 70% (7) |
| Dementia | 60% (3) | 50% (5) |
| Elder abuse | 100% (5) | 70% (7) |
| Falls | 100% (5) | 80% (8) |
| Frailty/risk for adverse health outcomes | 100% (5) | 100% (10) |
| Polypharmacy | 100% (5) | 60% (6) |
Abbreviation: ED, emergency department.
We identified key themes related to (1) motivations for upgrading accreditation status, (2) rationales for adopting specific care processes, and (3) experiences implementing care processes. Illustrative quotations are provided both herein and in Supporting Information Appendix C.
3.1. Motivations for upgrading geriatric ED accreditation
3.1.1. Improving patient care
Most sites (n = 11, 73%) sought to upgrade accreditation status due to operational leadership and/or geriatric champions’ desires to improve patient care. Participants wanted to follow a standardized approach and adhere to best practices in care of their geriatric patients. For example, one interviewee stated wanting older patients in their ED to “[get] better resources, [connect] to community partners, and…[have] better outcomes overall” (ID 110).
3.1.2. Achieving recognition
Nine sites (56%) upgraded accreditation with a goal of achieving recognition. Participants sought to cultivate departmental pride and acknowledgment from local leadership of achieving a high standard of care. Participants valued developing a reputation among patients and the community as a qualified geriatric resource. They also anticipated that upgrading would lead peer institutions to perceive their institution as a leader in geriatric emergency medicine. As an example, one participant saw accreditation as a “stamp of approval” and valued “being able to publicize” the accreditation status. They perceived accreditation as “helping us be recognized as a center where people want to come for their care” (ID 101).
3.1.3. Obtaining staffing resources
Three sites (20%) pursued the upgrade to persuade ED or hospital leadership to invest in specific dedicated ED staff, specifically a physical therapist, case manager, or social worker. In these cases, the potential for external recognition prompted healthcare administrators to increase geriatric resources available to the ED. As one participant described: “The accreditation itself to me was a tool to increase services to our older adults in the emergency department. So it sounds a little backwards” (ID 113).
3.2. Rationales for choosing specific care processes
3.2.1. Perceived complexity
For accreditation, EDs select from care processes outlined in the Geriatric ED Guidelines. The most common rationale for choosing specific care processes for an upgrade was ease of implementation (n = 6 sites, 40%). Participants found attractive care processes that staff could conduct with minimal training or those that could be conducted by technicians, thereby decreasing the burden for nurses and physicians. Interviewees described these processes as “low‐hanging fruit” (ID 115). Participants also reported choosing care processes that were similar to existing processes or already familiar to staff, referring to these as “quick wins” requiring only minor modifications. For example, in one ED, staff who had worked in other hospital settings were already familiar with the Confusion Assessment Method to assess for delirium. Local leaders of the GEDA upgrade therefore selected delirium screening as a care process due to perceived ease of administration by staff. Another ED modeled its care processes from a nationally renowned GED whose leadership shared experiences about the most feasible processes to implement.
3.2.2. Electronic health record integration
Participants selected care processes they anticipated would be relatively easy to integrate into and track within the electronic health record (EHR, n = 5 sites, 33%). As an example, one ED chose a falls risk assessment that was already built into the EHR for inpatient care. Processes where a follow‐up measure could be embedded into the EHR, such as polypharmacy assessment triggering a pharmacy consult for a positive screen, were also valued.
3.2.3. Patient needs
A minority of EDs (n = 3, 20%) chose care processes based on patient‐centered needs they had identified. Two of these EDs established interdisciplinary committees to evaluate available institutional data and prioritize specific processes.
3.3. Key considerations in implementation of GEDA care processes
3.3.1. Financing and resources
Eight sites (53%) highlighted the role of funding and resource availability in their upgrade process. Resources required for GEDA include application fees and expenses for staffing, training, equipment, supplies, and EHR infrastructure. Five sites relied on grant funding through their health system or philanthropy. Two EDs pertaining to the Veterans Health Administration had resources allocated due to a system‐wide initiative to achieve geriatric accreditation in all EDs. Participants at three sites described that even when institutional leaders had prioritized geriatric ED accreditation, they had to lobby ED administrators for resources for staffing, equipment, and access to health information technology.
3.3.2. Uncertainty about accreditation requirements
Participants at seven institutions (47%) felt uncertain about accreditation requirements. When reviewing the GEDA website and the GED Guidelines, they desired more specific instructions about how to implement care processes. Interviewees also described wanting to know if their current geriatric care processes met accreditation requirements for upgrade or needed modification. Participants wanted more support from the GEDA program while planning, implementing, and modifying care processes, noting they otherwise largely interacted with ACEP post‐implementation. As an example, one participant described feeling “a little disappointed” when she reached out to the ACEP for additional resources and connections and was referred to the GEDA website: “So I took that as, well, okay then, we're just on our own, and we'll do our own thing” (ID 108).
3.3.3. Frontline ED staff motivations and training
In the EDs represented in our sample, a core of geriatrics champions drove develoment and refinement of GEDA care processes. Some champions were designated by their EDs due to intrinsic motivation for the work. Others were appointed by hospital leadership in service of broader institutional goals such as becoming an age‐friendly health system. Interviewees at five institutions (33%) reported that frontline clinicians, in contrast, did not necessarily have intrinsic motivation or external leadership pressures to adopt or adhere to GEDA care processes. These care processes translated to added responsibilities for an already time‐constrained workforce. Interviewees felt that burnout and personnel turnover associated with COVID‐19 and the nursing shortage contributed to poor participation from frontline staff. Our participants highlighted a need for longitudinal engagement and education of frontline staff about geriatric care processes. One participant labeled this “stakeholder buy‐in” and described efforts of “getting people at the point of care to understand why they're having to learn new things” (ID 107).
Interviewees from 12 institutions (80%) described a major aspect of implementing geriatric screenings was training frontline staff to properly perform them. Delirium and dementia screening were difficult to teach and challenging for frontline staff to administer. Participants felt that some aspects of delirium and dementia assessments seemed subjective or had a “provider gestalt portion to [them]” (ID 109), though particular tools or questions were not specified. Dementia was the least commonly adopted screening (40% level 1, 50% level 2), due to perceptions that it was too complex and time‐intensive and more relevant to outpatient care.
3.3.4. Electronic health record
Interviewees from 10 EDs (67%) highlighted a crucial role of the electronic health record in facilitating geriatric screenings adopted for their upgrade. Screenings were easier to implement once they were integrated into the EHR as clinician documentation requirements, linking positive screening results to order sets or clinical pathways to facilitate follow‐up, and automated tracking of protocol adherence. Pre‐existing EHR tools supporting geriatric screening in the inpatient setting or at other sites in participants’ health systems facilitated adoption for ED use. EHR‐related implementation challenges included obtaining health information technology resources and waiting for screenings and high‐quality data reporting mechanisms to be built into the EHR. For example, one participant described their screening EHR integration process as requiring meetings with “a million people” over the course of months (ID 106). In fact, some sites reported choosing not to adopt specific screenings because builds for them did not already exist in their health system's EHR.
3.4. Synthesis: An implementation science approach to geriatric accreditation
We mapped participants’ responses onto CFIR 2.0 constructs to systematically delineate challenges and facilitators in implementation of GEDA care processes within each of the five CFIR domains. These are described in Table 3 and depicted in Figure 1. Resource availability (regarding financing and site infrastructure) and frontline staff engagement (through education, evaluation, and feedback) were factors associated with successful implementation across CFIR domains. Reviewing and addressing these factors in planning, execution, and evaluation may facilitate successful accreditation and maintenance of geriatric care processes.
TABLE 3.
Challenges and facilitators in implementation of Geriatric Emergency Department Accreditation (GEDA) care processes using the Consolidated Framework for Implementation Research (CFIR) 2.0.
| Construct | Definition from CFIR 2.0 | Role in accreditation |
|---|---|---|
| Innovation | ||
| Design | The innovation is well designed and packaged, including how it is assembled, bundled, and presented. | EDs had difficulty interpreting the Geriatric ED Guidelines and GEDA website and translating outlined care processes into clinical practice. Participants leveraged leadership contacts from EDs that already achieved accreditation (peer support) to answer questions about implementation and feasibility of specific care processes. |
| ED geriatric champions developed presentations and training materials to effectively describe selected care processes to ED operational leadership and frontline staff. | ||
| Complexity | The innovation is complicated, which may be reflected by its scope and/or the nature and number of connections and steps. | These are complex, often multi‐step care processes with multiple ED staff members involved. Geriatric ED champions made decisions about which improvements were most feasible to implement based on their complexity: whether existing processes could be modified, what resources/staff/staff training would be needed, and how/whether workflows for each process could be easily optimized. |
| Outer setting | ||
| Local attitudes | Sociocultural values (e.g., shared responsibility in helping recipients) and beliefs (e.g., convictions about the worthiness of recipients) encourage the outer setting to support implementation and/or delivery of the innovation. | Institutional and hospital system leadership shared a sense of responsibility to improve care for older adults. |
| Local conditions | Economic, environmental, political, and/or technological conditions enable the outer setting to support implementation and/or delivery of the innovation. | Health system‐wide initiatives such as pursuing age‐friendly hospital status or geriatric accreditation of multiple health system EDs help promote implementation. |
| Financing | Funding from external entities (eg, grants and reimbursement) is available to implement and/or deliver the innovation | Grants, philanthropic, and/or dedicated health system‐level funding earmarked for geriatric ED accreditation were crucial in facilitating implementation of care processes and meeting other requirements for accreditation such as employing dedicated geriatric‐trained staff or purchasing equipment/supplies. |
| External pressure | External pressures drive implementation and/or delivery of the innovation. | Market pressures to create a reputation as the best local ED for geriatric care helped drive EDs to pursue accreditation. |
| Top‐down pressure from a larger health system drove individual EDs to adopt care improvements. | ||
| Inner setting | ||
| Structural characteristics: Work infrastructure | Organization of tasks and responsibilities within and between individuals and teams, and general staffing levels, support functional performance of the inner setting. | EDs involved frontline staff to establish how new care processes could best fit into existing workflows and team structures or determine if new workflows needed to be developed. |
| Adequate staffing is necessary to avoid overburdening frontline staff with additional tasks. | ||
| Structural characteristics: IT infrastructure | Technological systems for tele‐communication, electronic documentation, and data storage, management, reporting, and analysis support functional performance of the inner setting. | EHR integration was crucial to support new care processes, automate follow‐up or direct users to management protocols for positive screenings, and to track quality metrics associated with geriatric care processes. |
| Integrating care processes into the EHR de novo often took months to years. | ||
| If EHR tools for specific care processes existed in other care settings within a hospital or other hospitals within a health system, adopting them into the ED could occur relatively rapidly. | ||
| Available resources | Resources are available to implement and deliver the innovation. | Multiple types of resources are required for geriatric ED accreditation including staffing, equipment, and supplies. Some care processes require availability of specialized consults (physical therapy, occupational therapy, pharmacy, and case management). |
| Access to knowledge and information | Guidance and/or training is accessible to implement and deliver the innovation. | The complexity of some geriatric care processes requires specific instructions/education to properly perform them. |
| Attrition of ED staff, burnout, and turnover negatively impacted maintenance of geriatric care processes. Continual education was needed to promote uptake of care processes in new staff members while assuring quality and fidelity of implementation. | ||
| Individuals | ||
| Midlevel leaders | Individuals with a moderate level of authority, including leaders supervised by a high‐level leader and who supervise others. | Accreditation was facilitated when ED leadership outside of the local geriatrics champions/accreditation team recognized and responded to needs for additional resource allocation, modified workflows, team reorganization to support geriatric care processes. |
| Implementation leads | Individuals who lead efforts to implement the innovation. | Geriatric champions were crucial in planning, driving change, educating and incentivizing frontline staff, and monitoring and evaluating progress and achievements. |
| Implementation deliverers | Individuals who are directly or indirectly delivering the innovation. | Establishing buy‐in and providing education about the potential benefits of geriatric care processes to frontline staff helped improve motivations to assume new or added work responsibilities. |
| Involving frontline staff in decisions about how to implement specific care processes helped promote their uptake. | ||
| Implementation process | ||
| Engaging | Attract and encourage participation in implementation and/or the innovation. | Participation and engagement of frontline ED staff in selecting and planning how to implement processes helped with adherence to screening protocols and departmental policy changes. |
| Providing frontline staff with feedback about and patient impacts from their performance helped promote uptake of geriatric care processes. | ||
| Reflecting and evaluating | Collect and discuss quantitative and qualitative information about the success of implementation. | The EHR automated tracking adherence to geriatric care processes and specifically for screenings. |
| Tracking processes and providing local leadership and frontline staff with feedback about their performance helped demonstrate implementation success and drive local departmental‐level buy‐in. | ||
Abbreviations: ED, emergency department; EHR, electronic health record.
FIGURE 1.
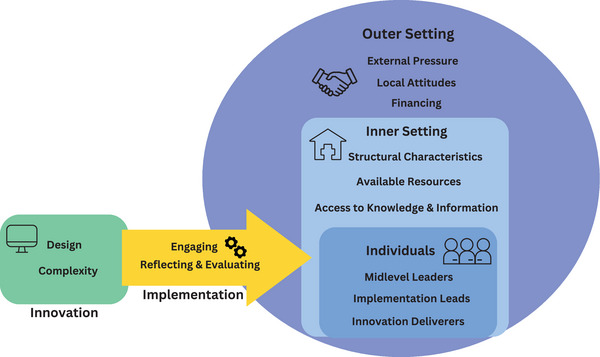
Key factors for implementing geriatric care processes based on the Consolidated Framework for Implementation Research.
4. Limitations
This study faces several limitations. First, interviews were conducted during a COVID‐19 pandemic‐related nursing shortage, and staff turnover challenges may be specific to that time period. However, staff shortages are likely to persist for the foreseeable future. Second, all interviews were conducted before requirements for geriatric accreditation increased on July 1, 2023. Additions to geriatric ED requirements were developing a dashboard (level 1), creating process maps (levels 1 and 2), monitoring boarding (levels 1 and 2), having a quality improvement plan (level 3), and mandatory adoption of three specific care processes (levels 1, 2, and 3), as described further in Supporting Information Appendix D. Our findings remain applicable to these added requirements, in particular those related to electronic health record infrastructure and frontline staff engagement; however, EDs currently pursuing accreditation or upgrading accreditation status may have experiences related to the added requirements that are not identified in this study. Third, as our study focused on those with direct implementation experience, we did not include non‐clinical administrators who provide support for GED initiatives and who likely have additional insights into institutional adoption of GED processes. Fourth, this study focused on sites that successfully upgraded accreditation status. Likely, there exist EDs that considered but did not pursue upgrade, and some sites have not been able to maintain accreditation. Perspectives from such sites about accreditation sustainability are an important area for future study.
5. DISCUSSION
Our qualitative study revealed that while EDs pursuing GEDA upgrades held patient‐centered motivations, they chose to implement care processes largely based on their feasibility. Frontline staff engagement and resource availability, especially related to electronic health record integration, were key factors that affected implementation. Our findings have important implications for understanding the impacts of GEDA and developing models for implementation.
First, our study highlights a tension between participants’ motivations to improve patient care and common choices to implement the most feasible geriatric care processes—that is, “low‐hanging fruit” (ID 115)—rather than meeting patient‐centered needs specific to the local context. Using CFIR to inform the interview guide and analysis helped us elucidate this theme. Respondents confirmed that these interventions are complex and require sustained investment of time and resources. Participants’ pragmatism is an understandable consequence of the complexity of the ED setting and geriatric care processes. The worst possible consequence of selecting a care process based on practicality rather than patient needs is an imbalance in the benefits that institutions reap from GEDA via public recognition versus those that patients experience. For instance, at the time of our study, the two most common quality initiatives enacted at level 3 GEDs were fall risk assessment and minimizing use of urinary catheters. These two quality initiatives align with national and safety reporting requirements, and as such level 3 EDs could use pre‐existing processes to achieve accreditation while not necessarily offering additional patient‐centered benefits. This dynamic is less applicable for higher level geriatric EDs given the larger number of care processes that must be implemented and these EDs’ tendencies to adopt care processes that are bundled, that is, co‐dependent and linked. 7 Overall, studies from accredited EDs have shown reduced length of stay, hospital admissions, and 30‐day re‐admissions, 4 , 5 , 19 suggesting that geriatric EDs do confer specific benefits to patients. The dynamic of selecting innovations to adopt based on pragmatism of implementation rather than first addressing top patient care gaps likely contributes to significant heterogeneity in the care processes that EDs choose to adopt. 7 , 8 As research increasingly examines the impacts of GEDA on patient outcomes across sites, 4 it will be important to consider that care processes and uptake of them may vary significantly from site to site—even with the same accreditation level. It remains important to understand associations between specific care processes and benefits observed at single sites, which have reported cost savings, 20 improved patient referral follow‐up rates, 21 and continual process improvements. 22 Such associations may be related to feasibility of the interventions.
Second, our study provides critical information about providing incentives and supports for sustainability of geriatric care processes even after establishing accreditation. Our study participants represented institutions that had already made a commitment to geriatric care processes through their initial accreditation. While one might imagine that geriatric accredited EDs develop a culture that prioritizes geriatric care among frontline staff, these sites grappled with frontline staff turnover and buy‐in. Workforce attrition and burnout are longstanding problems in emergency medicine, 23 , 24 which have been exacerbated by the COVID‐19 pandemic. 25 Other studies have similarly described motivational barriers in frontline ED staff. 9 A recent study at a level 1 geriatric ED highlighted variable uptake of care processes over time and moral injury resulting from feedback to frontline staff about improving adherence. 26 Improving and sustaining geriatric care processes appears to require ED leadership to longitudinally engage frontline staff through continuous education and feedback, and targeted incentives.
Third, our findings demonstrate the challenges of upgrading geriatric accreditation status in single sites. The Geriatric ED Guidelines outline care practices, but do not provide a blueprint for implementation. Prior scholarship has described models of GED dissemination and implementation within health systems. 10 , 11 Even with external funding and administrative support, uptake varied among EDs within a health system. The Veterans Administration system developed the Geriatric ED Bootcamp, a series of virtual conferences and longitudinal mentorship meetings that brought together local leaders from accredited sites and sites pursuing accreditation. 10 Knowledge sharing about implementation in major hospitals in St. Louis, Missouri allowed sites pursuing accreditation to incorporate lessons learned into planning and execution of GEDA processes. 27 Similarly, a New York health system has detailed how having its multiple EDs pursue geriatric accreditation simultaneously helped facilitate implementation knowledge exchange. 11 One value of health system‐wide accreditation is facilitation of the electronic health record infrastructure to support new geriatric care processes, which our study and others have demonstrated is a requisite for adopting geriatric screenings. 28 , 29 Other system‐wide benefits may include development and distribution of enduring educational resources as well as shared knowledge of accreditation guidelines. For EDs that are not part of a health system supporting accreditation at multiple sites, partnering with an accredited site may help with access to resources. Simultaneously, the GEDA Program should consider ways to offer tailored support to sites pursuing accreditation or upgrading accreditation. Strategies include providing toolkits, consulting, action communities, and forums for exchange of best practices, all of which have been used by the Institute for Healthcare Improvement in creating Age‐Friendly Health Systems. 30
Finally, our study has important implications for health equity. Most of the sites that successfully upgraded accreditation status were in urban areas with a relatively socioeconomically advantaged local population based on the Area Deprivation Index (reported in Table 1). The GEDA program may inadvertently magnify disparities in geriatric care and outcomes between sites with resources to achieve accreditation and those without. 31 This could also indicate that GEDA is more complex and less feasible in rural or poorly resourced EDs. Some of our participants highlighted how philanthropy facilitated their pursuit of accreditation, and this could be an important mechanism to facilitate GEDA implementation in resource‐poor sites.
In summary, geriatric ED accreditation is complex and requires significant resource and personnel commitments. The practical need to balance aspirations to improve patient care and resource limitations leads to heterogeneity in care processes implemented by different EDs, even with the same accreditation level. To sustain geriatric care processes, implementation must be carefully planned and monitored—ideally with support from already accredited sites—and frontline staff must be longitudinally engaged. These findings can be applied in EDs interested in pursuing geriatric accreditation and also highlight the need to understand implementation of new geriatric ED care processes.
CONFLICT OF INTEREST STATEMENT
Maura Kennedy serves on the Board of Governors of the Geriatric Emergency Department Accreditation Program. The remaining authors declare no conflicts of interest.
Supporting information
Supporting information
Supporting information
Supporting information
Supporting information
ACKNOWLEDGMENTS
The research was funded by the NIA (R03AG078943), Baylor College of Medicine Chao Physician‐Scientist Award, and Baylor College of Medicine Curtis Hankamer Basic Research Award to A.N.C. A.N.C., A.B., A.D.N., and K.M.G. receive support from the Houston Veterans Administration Health Services Research and Development Center for Innovations in Quality, Effectiveness, and Safety (CIN13‐413). L.S. receives support from the National Institute on Aging (K23AG061284). Research was funded by the NIA, Grant Number: R03AG078943; Baylor College of Medicine Chao Physician‐Scientist Award; Curtis Hankamer Basic Research Award
Biography
Anita Chary, MD, PhD, is an Assistant Professor for the Section of Health Services Research, Department of Medicine and Department of Emergency Medicine at Baylor College of Medicine in Houston, Texas.

Chary A, Bhananker A, Ramont V, et al. Pragmatism and feasibility: A qualitative study of experiences implementing and upgrading care in geriatric emergency departments. JACEP Open. 2024;5:e13216. 10.1002/emp2.13216
Supervising Editor: Alexander X. Lo, MD, PhD.
REFERENCES
- 1. Ashman J, Schappert S, Santo L. Emergency department visits among adults aged 60 and over: United States, 2014–2017. Natl Cent Health Stat Data Briefs. 2020;367:1‐8. [PubMed] [Google Scholar]
- 2. American College of Emergency Physicians , American Geriatrics Society , Emergency Nurses Association , Society for Academic Emergency Medicine . Geriatric emergency department guidelines. Ann Emerg Med. 2014;63(5):e7‐e25. doi: 10.1016/j.annemergmed.2014.02.008 [DOI] [PubMed] [Google Scholar]
- 3. American College of Emergency Physicians . Geriatric Emergency Department Accreditation Program (GEDA). Accessed August 2, 2022. https://www.acep.org/geda/
- 4. Gettel CJ, Hwang U, Janke AT, et al. An outcome comparison between geriatric and nongeriatric emergency departments. Ann Emerg Med. 2023;82:681‐689. doi: 10.1016/j.annemergmed.2023.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Keene SE, Cameron‐Comasco L. Implementation of a geriatric emergency medicine assessment team decreases hospital length of stay. Am J Emerg Med. 2022;55:45‐50. doi: 10.1016/j.ajem.2022.02.027 [DOI] [PubMed] [Google Scholar]
- 6. Haynesworth A, Gilmer TP, Brennan JJ, et al. Clinical and financial outcome impacts of comprehensive geriatric assessment in a level 1 geriatric emergency department. J Am Geriatr Soc. 2023;71(9):2704‐2714. doi: 10.1111/jgs.18468 [DOI] [PubMed] [Google Scholar]
- 7. Santangelo I, Ahmad S, Liu S, et al. Examination of geriatric care processes implemented in level 1 and level 2 geriatric emergency departments. J Geriatr Emerg Med. 2022;3(4). doi: 10.17294/2694-4715.1041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kennedy M, Lesser A, Israni J, et al. Reach and adoption of a geriatric emergency department accreditation program in the United States. Ann Emerg Med. 2022;79(4):367‐373. doi: 10.1016/j.annemergmed.2021.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Southerland LT, Hunold KM, Van Fossen J, et al. An implementation science approach to geriatric screening in an emergency department. J Am Geriatr Soc. 2022;70(1):178‐187. doi: 10.1111/jgs.17481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hwang U, Runels T, Han L, et al. Dissemination and implementation of age‐friendly care and geriatric emergency department accreditation at Veterans Affairs hospitals. Acad Emerg Med. 2023;30(4):270‐277. doi: 10.1111/acem.14665 [DOI] [PubMed] [Google Scholar]
- 11. Liberman T, Roofeh R, Herod SH, Maffeo V, Biese K, Amato T. Dissemination of geriatric emergency department accreditation in a large health system. J Am Coll Emerg Physicians Open. 2020;1(6):1281‐1287. doi: 10.1002/emp2.12244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bernard HR. Research Methods in Anthropology: Qualitative and Quantitative Approaches. 4th ed. AltaMira Press; 2011. [Google Scholar]
- 13. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32‐item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349‐357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 14. CFIR Research Team‐Center for Clinical Management Research . Consolidated Framework for Implementation Research (CFIR). Accessed June 3, 2021. https://cfirguide.org/
- 15. Kiger ME, Varpio L. Thematic analysis of qualitative data: aMEE Guide No. 131. Med Teach. 2020;42(8):846‐854. doi: 10.1080/0142159X.2020.1755030 [DOI] [PubMed] [Google Scholar]
- 16. Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17:75. doi: 10.1186/s13012-022-01245-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guest G, Namey E, Chen M. A simple method to assess and report thematic saturation in qualitative research. PLoS ONE. 2020;15(5):e0232076. doi: 10.1371/journal.pone.0232076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kind AJH, Buckingham WR. Making neighborhood‐disadvantage metrics accessible—the neighborhood atlas. N Engl J Med. 2018;378(26):2456‐2458. doi: 10.1056/NEJMp1802313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Huded JM, Lee A, Song S, et al. Association of a geriatric emergency department program with healthcare outcomes among veterans. J Am Geriatr Soc. 2022;70(2):601‐608. doi: 10.1111/jgs.17572 [DOI] [PubMed] [Google Scholar]
- 20. Southerland LT, Savage EL, Duff KM, et al. Hospital costs and reimbursement model for a Geriatric Emergency Department. Acad Emerg Med Off J Soc Acad Emerg Med. 2020;27(10):1051‐1058. doi: 10.1111/acem.13998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Simpson M, Sergi C, Malsch A, Ryer S, Rubach C, Singh M. Association of Geriatric Emergency Department post‐discharge referral order and follow‐up with healthcare utilization. J Am Geriatr Soc. 2023;71(3):821‐831. doi: 10.1111/jgs.18137 [DOI] [PubMed] [Google Scholar]
- 22. Shams C, Eshman Y, Factora R, Meldon S, Saxena S. The missed and the misdiagnosed: geriatric delirium in the emergency department. J Geriatr Emerg Med. 2023;4(3). doi: 10.17294/2694-4715.1061 [DOI] [Google Scholar]
- 23. Gettel CJ, Courtney DM, Janke AT, et al. The 2013 to 2019 emergency medicine workforce: clinician entry and attrition across the US geography. Ann Emerg Med. 2022;80(3):260‐271. doi: 10.1016/j.annemergmed.2022.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhang Q, Mu M‐C, He Y, Cai Z‐L, Li Z‐C. Burnout in emergency medicine physicians. Medicine (Baltimore). 2020;99(32):e21462. doi: 10.1097/MD.0000000000021462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gettel CJ, Courtney DM, Bennett CL, Keim SM, Camargo CA, Venkatesh AK. Attrition from the US emergency medicine workforce during early stages of the COVID‐19 pandemic. Ann Emerg Med. 2023;82:234‐236. doi: 10.1016/j.annemergmed.2023.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Southerland LT, Gulker P, Van Fossen J, et al. Implementation of geriatric screening in the emergency department using the Consolidated Framework for Implementation Research. Acad Emerg Med. 2023;30(11):1117‐1128. doi: 10.1111/acem.14776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Carpenter CR, Melady D, Krausz C, et al. Improving emergency department care for aging Missourians: guidelines, accreditation, and collaboration. Mo Med. 2017;114(6):447‐452. [PMC free article] [PubMed] [Google Scholar]
- 28. Chary AN, Brickhouse E, Torres B, et al. Leveraging the electronic health record to implement emergency department delirium screening. Appl Clin Inform. 2023;14(03):478‐486. doi: 10.1055/a-2073-3736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Saxena S, Meldon S, Hashmi AZ, Muir M, Ruwe J. Use of the electronic medical record to screen for high‐risk geriatric patients in the emergency department. JAMIA Open. 2023;6(2):ooad021. doi: 10.1093/jamiaopen/ooad021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Institute for Healthcare Improvement . Age‐friendly health systems resources and news. Accessed November 28, 2023. https://www.ihi.org/initiatives/age‐friendly‐health‐systems/resources‐and‐news
- 31. Chary AN, Cameron‐Comasco L, Shankar K, Samuels‐Kalow ME. Diversity, equity, and inclusion: considerations in the geriatric emergency department patient. Clin Geriatr Med. 2023;39(4):673‐686. doi: 10.1016/j.cger.2023.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information
Supporting information
Supporting information
Supporting information


