Abstract
Background and Objectives
Fall injuries are prevalent in older adults, yet whether higher spending occurs after nonfracture (NFFI) and fracture is unknown. We examined whether incident fall injuries, including NFFI and fractures, were associated with higher Medicare spending in 12 months after incident events in older adults.
Research Design and Methods
The Health, Aging, and Body Composition Study included 1 595 community-dwelling adults (53% women, 37% Black; 76.7 ± 2.9 years) with linked Medicare Fee-For-Service (FFS) claims at 2000/01 exam. Incident outpatient and inpatient fall injuries (N = 448) from 2000/01 exam to December 31, 2008 were identified using the first claim with a nonfracture injury diagnosis code with a fall E-code, or a fracture diagnosis code with/without an E-code. Up to 3 participants without fall injuries (N = 1 147) were matched on nonfall events to 448 participants in the fall injury month. We calculated the change in monthly FFS spending in 12 months before versus after index events in both groups. Generalized linear regression with centered outcomes and gamma distributions examined the association of prepost expenditure changes with fall injuries (including NFFI and fractures) adjusting for related covariates.
Results
Monthly spending increased after versus before fall injuries (USD$2 261 vs $981), nonfracture (N = 105; USD$2 083 vs $1 277), and fracture (N = 343; USD$2 315 vs $890) injuries (all p < .0001). However, after adjusting for covariates in final models, fall injuries were not significantly associated with larger increases in spending/month versus nonfall events (differential increase: USD$399.58 [95% CI: −USD$44.95 to $844.11]). Fracture prepost change in monthly spending was similar versus NFFI (differential increase: USD$471.93 [95% CI: −USD$21.17 to $965.02]).
Discussion and Implications
Although substantial increases occurred after injuries, with fracture and NFFI increasing similarly, changes in monthly spending after fall injury were not different compared to nonfall events. Our results contribute to the understanding of subsequent spending after fall injury that may inform further research on fall injury-related health care spending.
Keywords: Community-dwelling older adults, Fractures, Nonfracture fall injuries
Translational Significance: Our study is the first to assess how nonfracture (NFFI) and fracture fall injuries separately affect Medicare spending. We used a fall injury algorithm to define fall injury, including NFFI and fractures, based on claims linked with epidemiologic cohort data to examine how different types of fall injuries and subclinical factors affect health care spending. Results from this study suggest that NFFI and fracture had similar changes in Medicare spending after adjustment, and these findings may affect future efforts to address fall injury-related health care utilization and spending in older adults with Medicare FFS.
Background and Objectives
Falls are a critical public health concern and a leading cause of both nonfatal and fatal injuries among older adults. Among adults aged ≥65 years, 27.6% reported falls and 10.2% reported a fall-related injury in the past 12 months (1,2). The prevalence of fall injury significantly increases with age with almost 14% of those aged ≥85 reporting a fall injury (1). Although some studies demonstrate fracture incidence declining over recent decades, overall fall injury incidence continues to increase possibly due to increasing nonfracture fall injuries (NFFI) (3–5).
Fall injury is related to decreased function and independence, as well as increased disability, health care utilization, long-term care, and mortality in older adults (6–8). A study determined that health care spending associated with falls accounts for an estimated USD$50 billion per year with 99% related to nonfatal falls (9). For nonfatal falls specifically, Medicare, Medicaid, and private/other payers paid approximately USD$29 billion, $9 billion, and $12 billion, respectively (9). Fall spending may pose a greater burden on our health care system moving forward due to growth of the U.S. older population, especially for age groups at the highest risk for falls (≥85 years) (10).
Although there is available data on health care spending related to falls and nonfatal falls, few studies offer a detailed analysis of the economic burden associated with various types of fall-related injuries. This nuanced examination is crucial for informing future prevention strategies and enhancing our understanding of the distinct health care spending implications of different injury types. Previous evidence indicates that fracture, one of leading causes of fall-related hospitalization, was associated with substantial increases in health care utilization and spending in Medicare beneficiaries (11,12). In contrast to the accumulating evidence on fractures, little is known about the burden of NFFI, particularly when the presenting injury is not severe. We aimed to determine if incident outpatient and inpatient fall injuries, including NFFI and fractures, among community-dwelling older adults with Medicare fee-for-service (FFS) were associated with a greater magnitude of changes in spending after events versus nonfall events.
Research Design and Methods
Study Design and Study Population
We used data from the Health, Aging, and Body Composition (Health ABC) Study, a population-based, prospective, longitudinal study of community-dwelling older adults. In 1997–98, 3 075 well-functioning older White and Black adults (52% women; 42% Black), aged 70–79 years were recruited from a random sample of Medicare FFS beneficiaries and all age-eligible Black community residents in Pittsburgh, PA and Memphis, TN, USA (13). Eligible participants reported no difficulty walking a quarter of a mile (400 m), climbing 10 steps, or performing activities of daily living; had no cancer or active treatment in <3 years; and planned to remain in the study area for >3 years. This study was approved by the University of Pittsburgh and University of Tennessee Health Science Center institutional review boards.
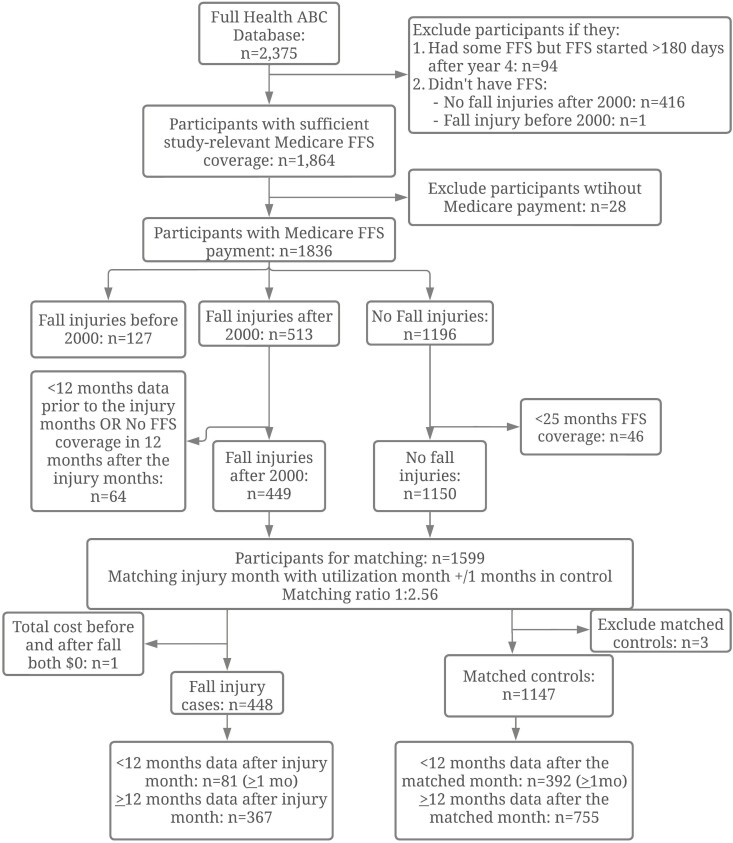
At Health ABC 2000/01 exam, 2 375/2 399 (99%) participants had monthly Medicare Entitlement/Buy-in and 1 864/2 399 (78%) had FFS Parts A and B alone. Before matching, we excluded participants (a) who did not have FFS coverage (N = 417) or started FFS > 180 days after 2000/01 exam (N = 94), (b) who did not have any Medicare payments during study period (N = 28), (c) who had fall injuries from 1997/98 to 2000/01 (N = 127); (d) who had <12 months of FFS coverage before or <12 months after fall injury (N = 64), and (d) nonfall injury participants with <25 months (the coverage period which was the same as the fall injury participants) of FFS coverage (N = 46). After the matching process (see subsequent section describing the comparison group), all participants with fall injuries after 2000 (n = 449) and no fall injuries (n = 1 150) were able to be matched; however, 1 case had USD$0 for total FFS both before and after event. This subject was excluded along with their matched controls (n = 3). Our final analytic sample size included 1 595 participants: 448 fall injury cases and 1 147 matched controls with nonfall-related Medicare utilization (ie, any nonfall events, regardless of severity) from 2000 to 2008 (Figure 1). Participants were censored at death, FFS disenrollment, or December 31, 2008.
Figure 1.
Flow chart of population selection.
Primary Independent Variable
Incident outpatient and inpatient fall injuries were identified using claims diagnoses codes from 2000/01 Health ABC study visit through December 31, 2008. All ICD-9 (the International Classification of Diseases, 9th Revision) diagnoses codes for fall injuries (codes E880-888 for fall with concurrent injury code) and fractures (codes 800-829) were considered, excluding traumatic injury, intentional injuries, and pathologic fractures (N = 38). Of fall injuries, events were: (a) fall code (E880-888) with NFFI, or (b) nonvertebral fracture (800-804, 807-829) +/− fall code, or vertebral fracture (805-806) + fall code (E880-888) (13). The index date for fall injury cases was the date of service for the incident fall injury. In the adjudication of our diagnoses code algorithm, we reviewed fall injuries with medical records due to potential uncertainty of certain diagnoses codes to classify a primary fall injury (N = 192): concurrent stroke code (N = 13); fall code with uncertain injury (N = 50); fracture that was not in first or second code position (N = 34); vertebral column/rib fracture code only (N = 95). Overall, the adjudication showed an excellent agreement with our Medicare algorithms, although for vertebral fractures only about 50% were related to falls so those without concurrent fall codes were excluded (13). Our diagnostic code algorithm is unique since it identifies fall-related utilization across outpatient, inpatient, and emergency department visits through a claims-based algorithm, unlike self-report in previous epidemiological cohort studies.
Comparison Group
For each participant with a fall injury, we selected up to 3 comparison participants who did not have a fall injury but had any nonfall-related Medicare utilization within ±1 month of the cases’ incident fall injury month. If a comparison participant had previously been matched with another fall injury case, we selected the next comparison participant with the lowest number of matched candidate cases (ie, an optimized 1:3 matching process without replacement). We assigned comparison individuals the same index date as the matched fall injury cases. We retained matched comparisons who had at least 12 months of FFS coverage from the index date. To maximize the sample size, we allowed comparison participants to have at least 1 month of FFS coverage after the index date. In order to examine the differences in demographic factors across fall injury events and nonfall injury events, we did not match the comparison group on any other factors except the date within 1 month of the fall event.
Primary Outcome
The primary outcome variable was Medicare FFS monthly spending for 12 months prior versus 12 months after incident fall injuries for cases and any nonfall events for controls. Spending on the date of the event was included in the postperiod. We did not have access to the diagnosis codes for any nonfall events and only had aggregated monthly expenditure data. Expenditure data from 2000 to 2008 was inflated to 2015 U.S. dollars to match the end of Health ABC data collection (14). Monthly aggregate payment to providers for claims was calculated for 12 months prior versus 12 months after index date of fall or nonfall event (post-minus pre-payment, USD$/month). Our Medicare expenditure data included spending for inpatient, outpatient/physician supplier, durable medical equipment, and skilled nursing facility/Home health agencies.
Covariates
All covariates were assessed at 2000/01 clinic visit and consisted of demographic, health status, behavioral, and clinical factors that may be potentially associated with the fall injuries or spending outcome. Demographic factors included age (years), sex (men/women), race (White/Black), study site (Memphis/Pittsburgh), and education (high school graduate: yes/no). Health behaviors included smoking status (yes, no, and former smoker), alcohol use (>1 drink/day: yes/no), and interview-administered physical activity assessment (kcal/kg/week) (15). Health status factors included a total number of prescription medications, body mass index (kg/m2), sensory detection (monofilament insensitivity: none, 1.4 g, and 10 g), kidney function (Cystatin C > 1.0: yes/no), subclinical peripheral arterial disease (ankle arm index: ≤0.9, 0.9–1.3, >1.3), self-reported cardiovascular disease (ie, bypass or coronary artery bypass graft, carotid endarterectomy, myocardial infarction, angina pectoris, or congestive heart failure), cerebrovascular disease (ie, stroke or transient ischemic attack), and poor vision (poor eyesight, cataract, glaucoma, retinal disease, and/or macular degeneration) (16). We defined diabetes as self-reported physician diagnosis, hypoglycemic medication use, or 8-hour fasting glucose ≥126 mg/dL (16). Hypertension was defined as self-reported hypertension, use of antihypertensive medications, or sitting systolic blood pressure ≥140 mmHg or/and sitting diastolic blood pressure ≥ 90 mmHg (16). Depressive symptoms were assessed using the Short Center for Epidemiologic Studies–Depression Scale (CES-D) and cognitive impairment was assessed with The Modified Mini-Mental State Test (3MS) (16).
Statistical Analysis
To evaluate the differences between the groups with fall injury versus nonfall events, Chi-square tests, univariate t tests, and Kruskal–Wallis tests were used for categorical variables and continuous variables, respectively. Two-part generalized linear regressions with centered outcomes and a gamma distribution were used to account for highly skewed zero-inflated data (17). These models were used to estimate the monthly FFS spending differences in the 12 months before versus after index event (ie, the index fall injury for the fall group and the matched nonfall event for the comparison group). We compared fall injury (NFFI and fractures) versus the nonfall events, and fracture versus NFFI. Forward stepwise selection was used to include covariates with p < .2, a recommended conservative threshold when including important confounders (18). This criterion was applied with the exception of fixed covariates including age, sex, race, and study site. Interaction terms between fall injuries and behavioral and subclinical factors that were associated with monthly FFS spending were included in final models. Collinearity was not violated in covariates. All analyses were performed in SAS, version 9.4 (SAS Institute, Cary, NC, USA).
Results
A total of 28.1% (n = 448) of the sample had an incident fall injury during follow-up, with 6.6% for NFFI (n = 105) and 21.5% for fracture (n = 343). Over half the sample were women, 37% identified as Black, and the mean age was 76.7 ± 2.9 years. Those with fall injuries were more likely to be older, White, women, high school graduates, and never-smokers, and had higher CES-D scores and lower BMI compared to the nonfall group (Table 1).
Table 1.
Baseline Characteristics of Older Adults with Fall Injury versus Nonfall Events in the Health, Aging, and Body Composition Study, 2000–08
| Variable | Fall injuries (NFFI and fracture) | Non-fall event group | p Value |
|---|---|---|---|
| N = 1 595 | 448 (28.1%) | 1 147 (71.9%) | . |
| Age, mean (SD) | 76.97 (2.99) | 76.48 (2.80) | .004 |
| Body mass index, mean (SD) | 26.81 (4.90) | 27.44 (4.73) | .02 |
| 3MS, mean (SD) | 90.88 (7.66) | 89.83 (8.71) | .09 |
| CES-D score, mean (SD) | 6.97 (6.69) | 6.14 (6.19) | .03 |
| Number of Rx meds, mean (SD) | 3.68 (2.81) | 3.23 (2.60) | .004 |
| Physical activity, kcal/kg/wk, mean (SD) | 5.57 (20.88) | 6.05 (17.89) | .86 |
| Sex | |||
| Women | 303 (67.63%) | 538 (46.90%) | <.0001 |
| Race | |||
| White | 333 (74.33%) | 670 (58.41%) | <.0001 |
| Black | 115 (25.67%) | 477 (41.59%) | |
| Study site | |||
| Memphis | 255 (56.92%) | 740 (64.52%) | .005 |
| Pitt | 193 (43.08%) | 407 (35.48%) | . |
| High school grad | 363 (81.57%) | 822 (72.61%) | .0002 |
| Monofilament insensitivity | |||
| None | 228 (52.17%) | 629 (55.76%) | .28 |
| 1.4 g | 172 (39.36%) | 395 (35.02%) | |
| 10 g | 37 (8.47%) | 104 (9.22%) | . |
| Poor vision | 251 (56.03%) | 585 (51.00%) | .07 |
| High Cystatin C | 129 (29.93%) | 301 (26.83%) | .22 |
| >1 drink per wk | 206 (46.61%) | 571 (50.58%) | .16 |
| Diabetes | 88 (19.64%) | 258 (22.49%) | .21 |
| AAI | |||
| ≤0.9 | 79 (17.63%) | 226 (19.70%) | .34 |
| >0.9–≤1.3 | 348 (77.68%) | 882 (76.90%) | . |
| >1.3 | 21 (4.69%) | 39 (3.40%) | . |
| Hypertension | 355 (79.24%) | 900 (78.47%) | .73 |
| Cerebrovascular disease | 34 (7.64%) | 75 (6.61%) | .47 |
| Cardiovascular disease | 72 (16.25%) | 187 (16.58%) | .88 |
| Smoking status | |||
| Never | 228 (54.03%) | 497 (45.31%) | .006 |
| Current | 22 (5.42%) | 85 (7.75%) | . |
| Former smoker | 172 (40.64%) | 515 (46.95%) | . |
Notes: AAI = ankle arm index; CES-D = the Short Center for Epidemiologic Studies–Depression Scale; 3MS = The modified mini-mental state test; NFFI = nonfracture fall injuries; Rx meds = prescription medications. Chi-square test and t test or Kruskal–Wallis test were used for categorical variables and continuous variables, respectively.
We observed a significant increase in monthly FFS spending after any fall injuries (USD$2 261 vs $981), NFFI (USD$2 083 vs $1 277), and fracture (USD$2 315 vs $890) versus before the fall event (all p < .0001, Supplementary Table 1). Monthly FFS spending also increased after versus before nonfall-related events (USD$1 834 vs $835; p < .0001) in the comparison group (Supplementary Table 1). In unadjusted generalized linear models comparing fall injury and the nonfall events, monthly FFS spending was not significantly higher after the index event versus before (differential increase: +USD$280.79 [95% CI: −USD$136.00 to $697.60], p = .19). After adjustments for covariates, the magnitude of difference increased, though remained nonsignificant (differential increase: +USD$399.58 [95% CI: −USD$44.95 to $844.11], p = .08, Table 2).
Table 2.
Adjusted Payment Differences Before and After Fall Injuries and Non-Fall Events in Older Adults in the Health, Aging, and Body Composition Study, 2000–08
| Parameter | β | [95% CI] | p Value |
|---|---|---|---|
| Fall injuries vs nonfall events | 399.58 | (−44.95, 844.11) | .08 |
| Age | 10.71 | (−60.02, 81.44) | .77 |
| Men (Women = ref.) | 219.68 | (−201.45, 640.81) | .31 |
| White (Black = ref.) | 55.57 | (−421.96, 533.10) | .82 |
| Pittsburgh (Memphis = ref.) | −355.14 | (−760.43, 50.15) | .09 |
| Body mass index | −49.93 | (−91.71, −8.15) | .02 |
| 3MS score | −39.83 | (−70.06, −9.59) | .01 |
| CES-D score | 41.39 | (8.91, 73.86) | .01 |
| High Cystatin C | 326.39 | (−127.68, 780.46) | .16 |
| Smoking status (former smoker = ref.) | |||
| Yes | −661.85 | (−1 427.94, 104.24) | .09 |
| Never | −279.16 | (−697.35, 139.03) | .19 |
| Number of Rx meds | 82.99 | (5.82, 160.16) | .04 |
| Diabetes | 828.64 | (317.23, 1 340.05) | .00 |
| AAI (≤0.9 = ref.) | |||
| >1.3 | −789.17 | (−1 884.90, 306.56) | .16 |
| >0.9–≤1.3 | −219.80 | (−740.19, 300.59) | .41 |
| Poor vision | −458.14 | (−852.03, −64.25) | .02 |
| Less than high school | −627.35 | (−1 166.39, −88.30) | .02 |
Notes: AAI = ankle arm index; CES-D = the Short Center for Epidemiologic Studies–Depression Scale; 3MS = The modified mini-mental state test. β estimates (USD$/month per unit) and 95% confidence intervals are presented earlier.
In the final model, 1 unit increase in BMI and 3MS score were associated with a reduction in FFS spending by USD$49.93 (95% CI: −USD$91.71 to −$8.15)/months and USD$39.83 (95% CI: −USD$70.06 to −$9.59)/month, respectively. One unit increase in CES-D score and the number of prescription medications were associated with an increase in FFS spending by USD$41.39 (95% CI: USD$8.91 to $73.86)/months and USD$82.99 (95%CI: USD$5.82 to $160.16)/month, respectively. The total FFS spending increased by USD$828.64 (95% CI: USD$317.23 to $1 340.05)/month after the index event in those with diabetes, however, decreased by USD$458.14 (95% CI: −USD$852.03 to −$64.25)/month in those with self-reported poor vision. Less than a high school education was associated with a decrease of USD$627.35 (−USD$1 166.39 to −USD$88.30)/month after the index event (Table 2). Age and smoking status were not significantly associated with monthly spending. The interaction terms between fall injuries and these subclinical factors were not statistically significant. In the final adjusted model, the fracture group demonstrated a nonsignificant differential increase of USD$736.80 [95% CI: −USD$122.84 to $1 596.14], p = .09)/month after index events versus the nonfall group (Supplementary Table 2). No differential increase in monthly spending (USD$264.87 [95% CI: −USD$518.90 to $1 048.64]; p = .51) was found for NFFI versus the nonfall group (Supplementary Table 2). However, the prepost change of spending in fracture group was not significantly different from NFFI (differential increase: USD$471.93 [95% CI: −USD$21.17 to $965.02], p = .06).
Discussion and Implications
In our study, Medicare FFS spending increased substantially after both NFFI and fractures. However, the increased spending after fall injury was similar though not significantly higher than after nonfall-related events, which included a range of severity of events in older adults. Past studies of Medicare fall injury spending only considered serious fall injuries from fracture and hospitalization, but less is known about outpatient-treated fall injuries, which represent the majority of fall injuries (19,20). Using adjudicated ICD-9 diagnoses codes and E-codes, we were able to identify fall injuries treated in outpatient/physician care settings and emergency departments, which are lower costs than hospitalized fall injuries, but far more common (21). Therefore, our estimated spending differences between fallers and nonfallers were smaller than previous studies for hospitalized fall injuries, but closer to the spending among all Medicare beneficiaries with treated fall injuries in both inpatient and outpatient settings (21). In addition, previous studies included younger ages than our participants (76–78 vs 82 years old at index event) and selected the midpoints of a year or random dates, rather than matching to month of nonfall-related events, as the index date for comparison groups (12,21). Differences in study populations and index date selection strategies for the comparison groups may be responsible for varied results. Future research is needed to examine if increased spending after fall injuries is comparable to common nonfall events in older age ranges such as ≥85 years, the fastest-growing segment of the older population, and those with the highest fall injuries (10).
Interestingly, our study showed that individuals with NFFI had similar increases in FFS spending compared to those with fracture injuries. Another study demonstrated that older adults with NFFI had a similar likelihood of having a long-term nursing home admission and similar declines in disability score as those with fractures, suggesting that excess spending after NFFI may be associated with subsequent utilization after initial injury (22). However, the lower number of NFFI events in our sample compared to fracture events may have resulted in higher variability in spending differences for NFFI and overfitting in the models. Future work should assess health care spending by varying types of fall injuries including NFFI, as these injuries may represent key events for future health care utilization. Our findings underscore the significance of preventing not only fractures but all fall injuries. Advocating for comprehensive fall prevention programs that target modifiable risk factors, incorporate physical therapy and home-based exercises, and enhance the safety of living environments is crucial (23,24). Implementing such programs likely has the potential to substantially decrease Medicare costs (25). Our results may also highlight the necessity for accessing supplemental coverage to reduce out-of-pocket costs associated with treating various fall injuries, particularly NFFI. Further research is warranted to assess the effectiveness of insurance coverage in ensuring timely treatment for diverse fall injuries. Additionally, investigating the influence of policy interventions on different types of fall injuries within this population is crucial for informing future health care strategies.
Compared to previous studies that used either longitudinal cohorts or Medicare claims data, our linked data approach, including both cohort data and FFS claims, provided a more comprehensive understanding of demographics and subclinical factors that may be associated with increased spending. Our study found that lower education and several baseline subclinical indicators (eg, depression as measured by increased CES-D scores, cognitive impairment as measured by decreased 3MS scores, diabetes as measured by fasting glucose levels, self-reported diagnosis, or medication use) were associated with increased FFS spending regardless of whether enrollees had a fall injury. These findings were aligned with previous research which showed the association between Medicare FFS spending and some clinical diagnoses. For example, Medicare spending, particularly inpatient spending, increases temporally after the diagnosis of dementia (26). This increase may be attributed to heightened requirements for expensive acute and postacute care, stemming from functional limitations and cognitive impairment (26). A diagnosis of mental health disorder is associated with higher Medicare spending for mental health services and physical health services (27). A diagnosis of diabetes is associated with significantly higher FFS spending compared with those without a diabetes diagnosis likely due to more health care needs for comorbidities (28,29). Prior work also showed that Medicare enrollees with high socioeconomic status were likely to have obtained more education, had better access to health care, and were more likely to have higher levels of medical care utilization which may incur higher Medicare payment (30). Evidence on the association between other subclinical factors identified by survey screening or clinician assessment such as poor vision and health care spending is limited since previous studies with claims data alone lack key subclinical measures compared to cohort studies (31). These associations between subclinical factors and increasing spending highlight the necessity for a comprehensive and holistic approach to reduce Medicare spending for community-dwelling older adults, especially when they are encountering multiple health conditions. In addition to clinical diagnoses in claims data, future studies should incorporate subclinical factors to examine modifiable multimorbidity indicators that may affect health care spending over time. An additional strength of cohort data linked to claims data is that outcomes are not dependent on in-person or self-reported follow-up, as a loss to follow-up in longitudinal cohorts is strongly related to health and function (32–34).
This study had several limitations. Importantly, non-treated fall injuries that are likely the least severe would not be captured by claims. Another limitation is potential miscoding of fall injuries in Medicare claims data which could be addressed by refining the incident fall injury definitions to be more comprehensive (eg, requiring a casting or splinting procedure on the same day or an imaging study in less than 10 days of fall injuries treated in ED visits or outpatient clinics) (35–37). Additionally, our study did not capture spending from supplemental insurance such as Medicaid which may lead to an underestimation in low-income older adults. Diagnosis codes for the nonfall events were not available in our data, which limits our ability to compare fall injuries with other costly events such as hospitalizations for acute myocardial infarction, pneumonia, or cancer. Also, predictors and covariates at one time point may not comprehensively account for comorbidity over time leading to possible unmeasured confounding in fall injury versus nonfall groups. Our spending estimates do not include nonmedical spending such as house modifications because of a fall. Several unmeasured confounders related to Medicare spending such as marital status and household income were not included in the model due to high missingness in the data. We also did not have fall circumstances, a factor that may affect FFS spending. Finally, the generalizability of our results to older adults outside Pittsburgh, PA, or Memphis, TN, or in different care settings is unknown. The generalizability of our findings to frail older adults is uncertain since our population had moderate functional limitations and were expected to live for longer periods of time than older adults with frailty who have been shown to have an exponential increase in spending as their frailty status worsened (38,39). Although we had a sample with almost 40% Black participants, future work should prioritize recruitment of additional underrepresented populations to understand health care utilization in diverse older adults.
Our study using a fall injury algorithm from linked claims with cohort data demonstrated that fall injuries, both fracture and NFFI, were associated with subsequent increases in FFS spending. The increase in Medicare spending after fall injury was similar to that after non-fall events. Our results contribute to the understanding of subsequent Medicare spending after fall injury in community-dwelling old adults which may provide a focus for further research on fall injury-related health care spending.
Supplementary Material
Contributor Information
Lingshu Xue, Department of Health Policy and Management, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Jenna M Napoleone, Omada Health Inc, San Francisco, California, USA.
Mary E Winger, Department of Health Economics, UPMC Insurance Services Division, Pittsburgh, Pennsylvania, USA.
Robert M Boudreau, Department of Epidemiology, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Jane A Cauley, Department of Epidemiology, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Julie M Donohue, Department of Health Policy and Management, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Anne B Newman, Department of Epidemiology, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Teresa M Waters, Institute for Public and Preventive Health, Augusta University, Augusta, Georgia, USA.
Elsa S Strotmeyer, Department of Epidemiology, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Funding
This work was supported by the National Institute on Aging (NIA) Contracts [N01-AG-6-2101; N01-AG-6-2103; N01-AG-6-2106]; NIA Grant [R01-AG028050, R01-AG029232, R01-AG034056, R01 AG061136]; AHRQ grant [R01-HS017695]; National Institute of Nursing Research Grant [R01-NR12459]; and University of Pittsburgh Claude D. Pepper Older Americans Independence Center Pilot Grants [P30-AG024827]; in part by the Intramural Research Program of the National Institutes of Health, NIA; and NIA Aging Training Grant T32 [AG000181].
Conflict of Interest
J. Napoleone is an employee of Omada Health, Inc. and receives salary and stock options. Other authors declare that they have no conflict of interest.
Data Availability
Our analytic methods or materials are available to other researchers upon request. Original data used in this study is not available to other researchers for replication purposes due to CMS Data use agreement limitations. This study was not preregistered.
References
- 1. Moreland B, Kakara R, Henry A.. Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years - United States, 2012-2018. MMWR Morb Mortal Wkly Rep. 2020;69(27):875–881. 10.15585/mmwr.mm6927a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kakara R, Bergen G, Burns E, Stevens M.. Nonfatal and fatal falls among adults aged ≥65 Years — United States, 2020–2021. MMWR Morb Mortal Wkly Rep. 2023;72(35):938–943. 10.15585/mmwr.mm7235a1 [DOI] [PubMed] [Google Scholar]
- 3. Swayambunathan J, Dasgupta A, Rosenberg PS, Hannan MT, Kiel DP, Bhattacharyya T.. Incidence of Hip Fracture Over 4 Decades in the Framingham Heart Study. JAMA Int Med. 2020;180(9):1225–1231. 10.1001/jamainternmed.2020.2975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hoffman G, Franco N, Perloff J, Lynn J, Okoye S, Min L.. Incidence of and county variation in fall injuries in US residents aged 65 years or older, 2016-2019. JAMA Network Open. 2022;5(2):e2148007. 10.1001/jamanetworkopen.2021.48007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Watson WL, Mitchell R.. Conflicting trends in fall-related injury hospitalisations among older people: Variations by injury type. Osteoporos Int. 2011;22(10):2623–2631. 10.1007/s00198-010-1511-z [DOI] [PubMed] [Google Scholar]
- 6. Stevens JA, Sogolow ED.. Gender differences for non-fatal unintentional fall related injuries among older adults. Injury Prev: J Int Soc Child Adolescent Injury Prev. 2005;11(2):115–119. 10.1136/ip.2004.005835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ambrose AF, Paul G, Hausdorff JM.. Risk factors for falls among older adults: A review of the literature. Maturitas. 2013;75(1):51–61. 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 8. Houry D, Florence C, Baldwin G, Stevens J, McClure R.. The CDC Injury Center’s response to the growing public health problem of falls among older adults. Am J Lifestyle Med. 2016;10(1):74–77. 10.1177/1559827615600137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C.. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. 2018;66(4):693–698. 10.1111/jgs.15304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Colby SL, Ortman JM.. Projections of the Size and Composition of the U.S. Population: 2014 to 2060 . Washington, DC: U.S. Census Bureau; 2014. Current Population Reports, P25-1143. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. [Google Scholar]
- 11. Kilgore ML, Morrisey MA, Becker DJ, et al. Health care expenditures associated with skeletal fractures among Medicare beneficiaries, 1999-2005. J Bone Miner Res. 2009;24(12):2050–2055. 10.1359/jbmr.090523 [DOI] [PubMed] [Google Scholar]
- 12. Hoffman GJ, Hays RD, Shapiro MF, Wallace SP, Ettner SL.. The costs of fall-related injuries among older adults: Annual per-faller, service component, and patient out-of-pocket costs. Health Serv Res. 2017;52(5):1794–1816. 10.1111/1475-6773.12554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sagawa N, Marcum ZA, Boudreau RM, et al. Health Aging Body Composition Study Low blood pressure levels for fall injuries in older adults: The Health, Aging and Body Composition Study. Eur J Ageing. 2018;15(3):321–330. 10.1007/s10433-017-0449-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. U.S. Bureau of Labor Statistics. https://data.bls.gov/timeseries/CUUR0000SA0L1E?output_view=pct_12mths. Accessed February 2, 2023. [Google Scholar]
- 15. Colbert LH, Visser M, Simonsick EM, et al. Physical activity, exercise, and inflammatory markers in older adults: Findings from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2004;52(7):1098–1104. 10.1111/j.1532-5415.2004.52307.x [DOI] [PubMed] [Google Scholar]
- 16. Xue L, Boudreau RM, Donohue JM, et al. Persistent polypharmacy and fall injury risk: The Health, Aging and Body Composition Study. BMC Geriatr. 2021;21(1):710. 10.1186/s12877-021-02695-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Deb P, Norton EC.. Modeling health care expenditures and use. Ann Rev Public Health. 2018;39(1):489–505. 10.1146/annurev-publhealth-040617-013517 [DOI] [PubMed] [Google Scholar]
- 18. Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE.. Predictor selection. In: Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE, eds. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. Statistics for Biology and Health. Springer US; 2012:395–429. 10.1007/978-1-4614-1353-0_10 [DOI] [Google Scholar]
- 19. Stevens JA, Corso P, Finkelstein E, Miller T.. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12:290–295. 10.1136/ip.2005.011015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Strotmeyer ES, Buchner DM.. Fall injuries in older men and women: Novel assessments and predictors. Innov Aging. 2017;1(Suppl 1):1004–1004. 10.1093/geroni/igx004.3644 [DOI] [Google Scholar]
- 21. Hoffman GJ, Hays RD, Shapiro MF, Wallace SP, Ettner SL.. Claims-based identification methods and the cost of fall-related injuries among US older adults. Med Care. 2016;54(7):664–671. 10.1097/MLR.0000000000000531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gill TM, Murphy TE, Gahbauer EA, Allore HG.. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidem. 2013;178(3):418–425. 10.1093/aje/kws554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. STEADI - Older Adult Fall Prevention | CDC. Published May 17, 2023. Accessed November 27, 2023. https://www.cdc.gov/steadi/index.html [Google Scholar]
- 24. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;2012(9):CD007146. 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stevens JA, Lee R.. The potential to reduce falls and avert costs by clinically managing fall risk. Am J Prev Med. 2018;55(3):290–297. 10.1016/j.amepre.2018.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hoffman GJ, Maust DT, Harris M, Ha J, Davis MA.. Medicare spending associated with a dementia diagnosis among older adults. J Am Geriatr Soc. 2022;70(9):2592–2601. 10.1111/jgs.17835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Figueroa JF, Phelan J, Orav EJ, Patel V, Jha AK.. Association of mental health disorders with health care spending in the Medicare population. JAMA Netw Open. 2020;3(3):e201210. 10.1001/jamanetworkopen.2020.1210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–928. 10.2337/dci18-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Landon BE, Zaslavsky AM, Saunders RC, Pawlson LG, Newhouse JP, Ayanian JZ.. Analysis of Medicare advantage HMOs compared with traditional Medicare shows lower use of many services during 2003–09. Health Aff. 2012;31(12):2609–2617. 10.1377/hlthaff.2012.0179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rogowski J, Freedman VA, Wickstrom SL, Adams J, Escarce JJ.. Socioeconomic disparities in medical provider visits among Medicare managed care enrollees. Inquiry. 2008;45(1):112–129. 10.5034/inquiryjrnl_45.01.112 [DOI] [PubMed] [Google Scholar]
- 31. Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: The health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059–1064. 10.1093/gerona/61.10.1059 [DOI] [PubMed] [Google Scholar]
- 32. Allman RM, Sawyer P, Crowther M, Strothers HS 3rd, Turner T, Fouad MN.. Predictors of 4-year retention among African American and white community-dwelling participants in the UAB study of aging. Gerontologist. 2011;51(Suppl 1):S46–S58. 10.1093/geront/gnr024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Strotmeyer ES, Arnold AM, Boudreau RM, et al. Long-term retention of older adults in the Cardiovascular Health Study: Implications for studies of the oldest old. J Am Geriatr Soc. 2010;58(4):696–701. 10.1111/j.1532-5415.2010.02770.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cauley JA, Hochberg MC, Lui LY, et al. Long-term risk of incident vertebral fractures. JAMA. 2007;298(23):2761–2767. 10.1001/jama.298.23.2761 [DOI] [PubMed] [Google Scholar]
- 35. Wilchesky M, Tamblyn RM, Huang A.. Validation of diagnostic codes within medical services claims. J Clinical Epidem. 2004;57(2):131–141. 10.1016/S0895-4356(03)00246-4 [DOI] [PubMed] [Google Scholar]
- 36. Iezzoni LI. Assessing quality using administrative data. Ann Intern Med. 1997;127(8 Pt 2):666–674. 10.7326/0003-4819-127-8_part_2-199710151-00048 [DOI] [PubMed] [Google Scholar]
- 37. Min L, Tinetti M, Langa KM, Ha J, Alexander N, Hoffman GJ.. Measurement of fall injury with health care system data and assessment of inclusiveness and validity of measurement models. JAMA Netw Open. 2019;2(8):e199679. 10.1001/jamanetworkopen.2019.9679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Álvarez-Bustos A, Rodríguez-Sánchez B, Carnicero-Carreño JA, Sepúlveda-Loyola W, Garcia-Garcia FJ, Rodríguez-Mañas L.. Healthcare cost expenditures associated to frailty and sarcopenia. BMC Geriatr. 2022;22(1):747. 10.1186/s12877-022-03439-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Chernew ME, Goldman DP, Pan F, Shang B. Disability And Health Care Spending Among Medicare Beneficiaries | Health Affairs. Accessed November 24, 2023. https://www-healthaffairs-org.pitt.idm.oclc.org/doi/full/10.1377/hlthaff.W5.R42 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Our analytic methods or materials are available to other researchers upon request. Original data used in this study is not available to other researchers for replication purposes due to CMS Data use agreement limitations. This study was not preregistered.