Abstract
Background
During aging, the face loses volume with progressive sagging of the soft tissues, while the neck demonstrates skin laxity and muscle banding. The treatment of facial and neck aging usually involves a traditional facelift, which can cause noticeable scarring and distortion of anatomy.
Objectives
Modern facelift surgery must avoid such shortcomings and still address aging in all layers of the face. To achieve this goal a novel surgical technique was developed and coined the “ponytail lift” (PTL). When global facial rejuvenation is indicated, this procedure is combined with neck skin excision and referred to as the “ponytail facelift” (PTFL).
Methods
A retrospective analysis of 600 consecutive cases over 22 years (2000-2022) of facial rejuvenation employing the endoscopic techniques of PTL and PTFL was performed. Patients were followed for at least 12 months postoperatively. Demographics, surgical data, and complications were recorded and analyzed. Additionally, technical details of the PTL and PTFL are discussed.
Results
There were no instances of postoperative skin flap necrosis, and no permanent nerve injuries were recorded. An additional surgical touch-up procedure to address unsatisfied aesthetic needs was performed in 20 cases.
Conclusions
The ponytail procedures offer a stepwise approach matched to the extent of the problem and are intended to refresh or transform the face with minimal incisions. The procedures represent a deep plane facelift without the scar burden, with incisions that are hidden in the temple, postauricular, and posterior scalp. The described techniques are safe and effective while providing reliable and satisfying results.
摘要
背景
随着年龄的增长,面部体积会逐渐减小,软组织会逐渐下垂,而颈部会出现皮肤松弛和肌肉带状。面部和颈部衰老的治疗通常涉及传统的面部拉皮术,这会导致明显的疤痕和解剖结构扭曲。
目标
现代面部拉皮手术必须避免此类缺点,同时还要解决面部所有层面的衰老问题。为了实现这一目标,开发了一种新颖的手术技术,创造了“马尾辫提升术”(PTL)这一名称。当需要进行整体面部年轻化时,该手术与颈部皮肤切除术相结合,称为“马尾辫拉皮术”(PTFL)。
方法
回顾性分析了 22 年间(2000-2022 年)采用 PTL 和 PTFL 内窥镜技术进行面部年轻化的 600 个连续病例。术后对患者进行至少 12 个月的随访。记录并分析了人口统计学、手术数据和并发症。此外,还讨论了 PTL 和 PTFL 的技术细节。
结果
没有出现术后皮瓣坏死的情况,也没有记录到永久性神经损伤。在 20 个病例中进行了额外的外科修补手术,以解决未满足的美学需求。
结论
马尾辫手术提供了一种与问题程度相匹配的分步方法,旨在以最小的切口使面部得以改造或焕然一新。这些手术代表了一种深层平面拉皮术,没有疤痕负担,切口隐藏在太阳穴、耳后和头皮后部。所描述的技术是安全有效的,同时提供可靠且令人满意的结果。
证据等级:
3 级(治疗性)
Level of Evidence: 3

See the commentaries on articles sjae017 and sjae105.
During aging, the upper face loses volume with descent of soft tissue while the lower face and neck develop excess skin and muscle banding.1 Most plastic surgeons treat facial and neck aging with various superficial musculoaponeurotic system (SMAS)–manipulating techniques. Commonly in facelift surgery an incision is made in the tragal area extending up into the temple scalp or along the temple hairline.2 The incision curves around the earlobe and then behind the ear, usually running along the hairline on the back of the neck. After the skin incision is made, the skin is undermined and separated from the subcutaneous fat and deeper tissues with a scalpel or scissors over the cheeks and neck. The subcutaneous fat is retained on the SMAS. The SMAS is developed above the underlying mimetic muscles, mobilized and tightened with sutures, serving as a vehicle to lift the fat. The skin is then redraped horizontally, and excess skin is removed.2
This traditional approach if poorly executed can cause noticeable scarring in front of the ear, shortening of the sideburns, and distortion of the ear's anatomy.3 Also, the traditional facelift separates the skin from the fat and lifts the fat tissues off the muscle. This inevitably devascularizes the skin and traumatizes the fat, which potentially results in atrophy of the skin and fat, leading to an unnatural or even more aged appearance accompanied by skin telangiectasia due to increased collateral vascularization.4
This classic technique with its plethora of variations involves preauricular incisions that has led both patients and surgeons to call for a more scar-minimizing approach.5 A modern facelift must be a comprehensive facial rejuvenation procedure simultaneously addressing aging in all 3 layers of the face: the SMAS layer which is prone to sagging and descent; the subcutaneous fat layer that tends to atrophy and results in volume loss and sagging; and finally the skin, which loses collagen and elastin, leading to lines, wrinkles, and textural problems.6 We rethought the modern facelift by developing a novel approach addressing the aging face in all dimensions, harnessing minimally invasive modalities including an endoscopic brow rotation, deep plane cheek lift, skin-only lower blepharoplasty (when indicated), microfat grafting, and trichloroacetic acid (TCA) peeling or fractionated CO2 laser treatment. This refined surgical technique is coined the “ponytail lift” (PTL) because it results from lifting in a vertical vector, simulating the youthful appearance of having the hair pulled up in a high ponytail. Deep contouring of the anterior neck can be included if there is a presence of double chin or an obtuse neck. When a global facial rejuvenation is indicated, with redundant skin of the lower face and neck, this procedure is combined with deep contouring of the anterior neck and limited incision neck lift that is called the “ponytail facelift” (PTFL).
In this study we report our experience in 600 ponytail procedures over a period of 22 years performed by a single surgeon (C.C.K.). Patient demographics, surgical data, and complications were recorded and analyzed. Additionally, technical nuances of the PTL and PTFL are shared.
METHODS
This study was a retrospective assessment of data collected over a period of 22 years. From 2000 until 2022, 600 consecutive patients underwent facial rejuvenation by a ponytail procedure conducted by the first author (C.C.K.) (Table 1). A detailed history was taken and basic examinations were performed to ensure that all patients were in good overall health. Exclusion criteria included unrealistic expectations regarding the aesthetic outcome of the operation, pregnancy or breastfeeding, a medical condition interfering with wound healing, active fever (temperature > 38°C), severe lung disease such as chronic obstructive pulmonary disease or cystic fibrosis, active cutaneous or systemic infections, radiation or chemotherapy, and alcohol or drug abuse within 6 months before surgery. The authors followed the Declaration of Helsinki protocols in this research.
Table 1.
Patient Demographics
| Demographic information | n |
|---|---|
| Total | 600 (100%) |
| Female | 571 (95%) |
| Male | 29 (5%) |
| Age, average (range) | 50.9 (17-82) |
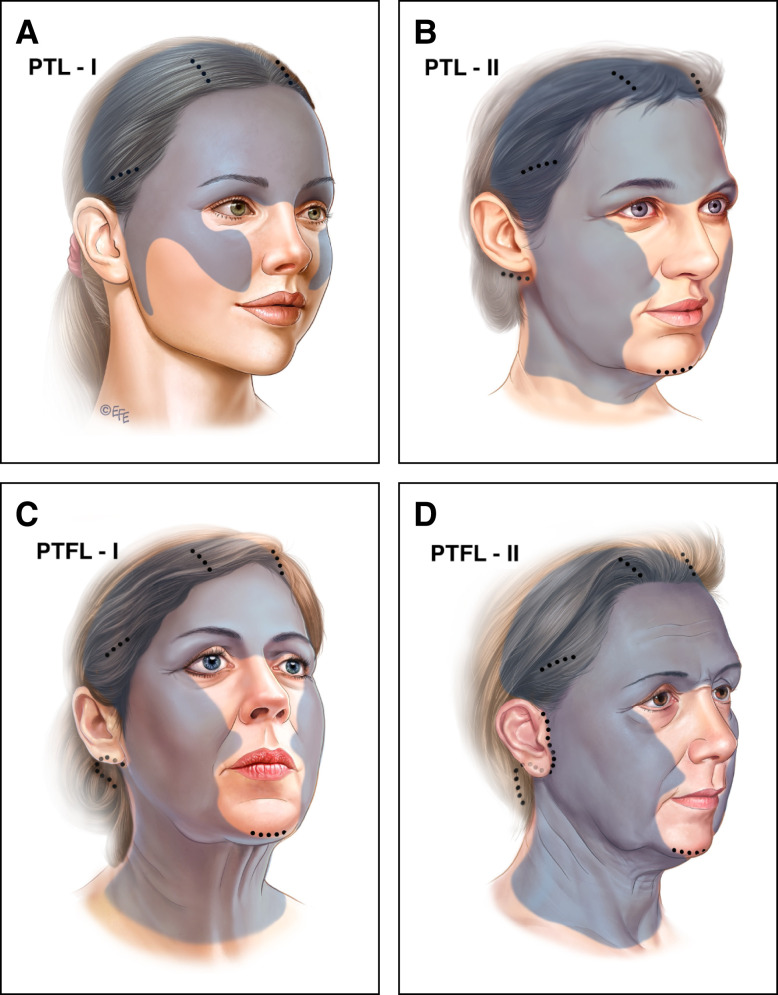
Appropriate candidates for the ponytail procedure were divided into 4 groups based on clinical examination, including physical examination of skin excess and video assessment of facial features in movement, to determine the extent of treatment required to achieve optimal facial rejuvenation (Figure 1).
Figure 1.
The 4 ponytail types, the incisions, and the extent of the dissection. There are 4 types of ponytail procedures: (A) Ponytail Lift I (PTL-I) is designed for patients presenting in their 30s or 40s with signs of early aging, commonly seen in the upper two-thirds of the face, or younger patients for facial beautification. The incisions are all hidden in the scalp. (B) Ponytail Lift II (PTL-II) is typically indicated for patients 40 to 45 years of age with early jowling but only minimal skin laxity of the neck. A 2-cm endoscopic access incision in the postauricular sulcus is added to thin the lower face and jowls and allow endoscopic deep plane dissection and tightening of the SMAS layer. When submental fullness (double chin) is present, deep contouring of the anterior neck is added through a 1.5-cm incision under the chin, however, no skin in the neck is removed. (C) Ponytail Facelift I (PTFL-I) is indicated when there is enough laxity and redundancy of the lower face and neck skin requiring resection. The PTFL-I procedure includes an extended posterior auricular incision for a deep plane lower face and necklift. Correction of the anterior neck by deep contouring and platysma plication as well as application of a posterior corset is necessary. The typical patient age for this cohort is 45 to 65 years, presenting with jowls and a mild to moderate amount of neck skin laxity. Importantly, there are no incisions in the pretragal area or temporal hairline. (D) For a Ponytail Facelift II (PTFL-II) the typical age is 65 years and older. The issues to address include heavy jowling, significant skin excess in the neck, and poor skin tone and elasticity. A limited pretragal incision is added to the PTFL-I approach to help manage the significant excess skin. Importantly there is no incision in the sideburns or any extension into the temporal hairline. SMAS, superficial musculoaponeurotic system.
Ponytail Lift I
Ponytail Lift I (PTL-I) was designed for patients presenting in their 30s or 40s with signs of early aging, commonly seen in the upper two-thirds of the face. Classically, the issues these patients suffer from are ptosis of the forehead and brow, hooding of the upper eye lid, lower eyelid blepharochalasis, descent of the cheek fat pad, accentuation of the nasolabial fold, volume depletion in the upper two-thirds of the face, and skin dyschromia and rhytids. A combination of endoscopic brow rotation, deep plane cheek lift, skin-only blepharoplasty, microfat grafting, and skin resurfacing with 15% to 20% TCA or fractionated CO2 laser was performed in this patient cohort. This procedure was also suitable for younger female patients who had congenitally low-set masculine brows with a sad appearance of the eyes and cheek ptosis or hypoplasia, who wished to soften and beautify their appearance. Recently this procedure has been increasingly popular because of social media trends.
Ponytail Lift II
Ponytail Lift II (PTL-II) was typically indicated for patients 40 to 45 years of age with early jowling but with only minimal skin laxity of the neck. In addition to the work described for PTL-I, a 2-cm endoscopic access incision in the postauricular sulcus was performed to thin the lower face and jowls and allow endoscopic deep plane dissection and tightening of the SMAS layer. When submental fullness redundancy (double chin) was present, deep contouring of the anterior neck was added through a 1.5-cm incision under the chin, however, no skin in the neck was removed. The PTL-II cohort was traditionally smaller because patients did not know about the option of surgical correction of early jowling. Therefore, they usually presented at a later stage when there was already enough neck skin laxity and a ponytail facelift procedure was indicated.
Ponytail Facelift I
This procedure was indicated when there was enough laxity and redundancy of the lower face and neck skin requiring resection. The Ponytail Facelift I (PTFL-I) procedure included an extended posterior auricular incision for a deep plane lower face and neck lift. Correction of the anterior neck by deep contouring and platysma plication as well as application of a posterior corset was necessary (see below). The typical patient age for this cohort was 45 to 65 years, presenting with jowls and a mild to moderate amount of neck skin laxity. These patients did not have extreme amounts of excess skin around the neck or submental area. The incision was perilobular in the posterior auricular sulcus and extended into the posterior mastoid scalp. The dissection of the neck was complete, all the way down to the clavicle and all the way back toward the anterior edge of the trapezius. The deep neck structures such as subplatysmal fat and the anterior belly of the digastric were contoured. Submandibular glands were reduced selectively based on preoperative physical assessment and intraoperative findings. Laterally the platysma muscle edge was tightened and sutured to the posterior neck fascia to further enhance the jawline. Importantly, there were no incisions in the pretragal area or at the temporal hairline.
Ponytail Facelift II
The typical age for this cohort was closer to 60 years and older. The issues to address included heavy jowling, significant skin excess in the neck, and poor skin tone and elasticity. A limited pretragal incision was added to the PTFL-I approach described above to help manage significant excess skin. When the excess neck skin was redraped to the mastoid area, skin bunching occurred at the perilobular area. This bunching of skin was removed along a pretragal incision. There was no dissection or creation of a skin or SMAS advancement flap. Importantly there was no incision in the sideburns or any extension into the temporal hairline. An amputation or shortening of sideburns was strictly avoided.
An overview of the patient distribution over procedural types is provided in Table 2. To provide a better understanding of surgical planning and decision-making, we share surgical details below.
Table 2.
Patient Distribution by Procedure
| Procedure | No. patients | Average age, years (range) |
|---|---|---|
| Ponytail Lift I | 197 (184 female, 13 male) | 42 (21-67) |
| Ponytail Lift II | 12 (all female) | 41 (17-71) |
| Ponytail Facelift I | 257 (251 female, 6 male) | 54 (31-76) |
| Ponytail Facelift II | 134 (124 female, 10 male) | 57 (39-82) |
Anesthesia and General Preparation
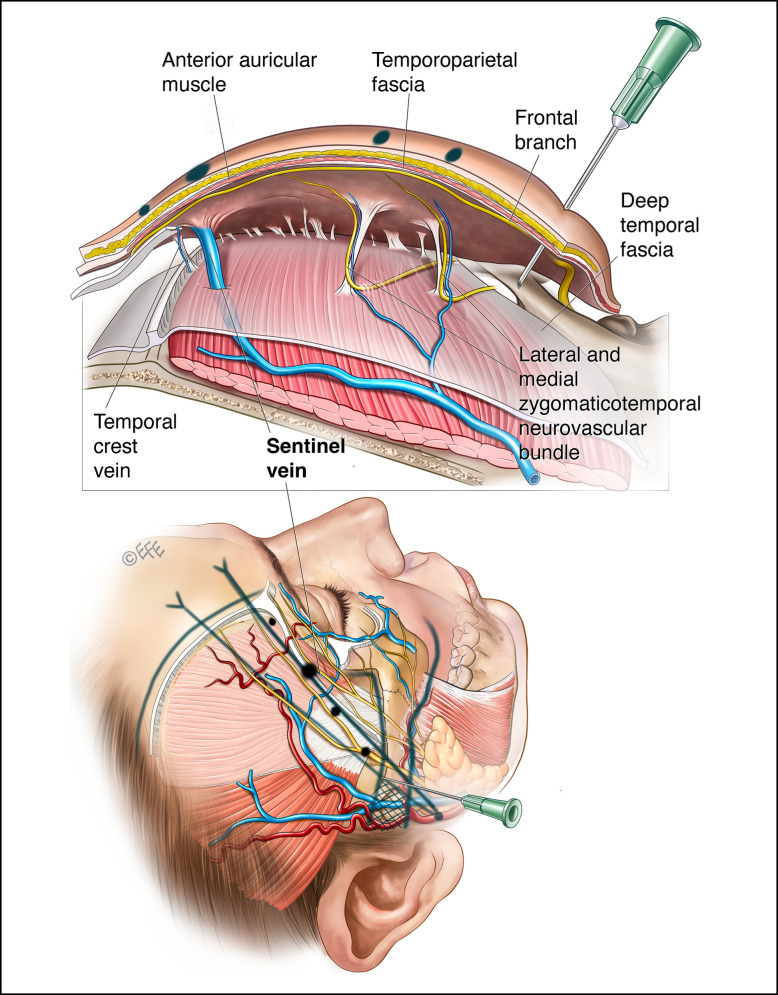
Preoperative medication included a Medrol Dosepak (Pfizer, New York, NY; oral methylprednisolone) 1 day before and valium the night before surgery. Antibiotics were administered perioperatively (cephalexin). Surgical marking included the bony architecture, Pitanguy's line, the anticipated location of the sentinel vein in the temporal area 1 cm superior to the superior zygomatic arch and 1 cm lateral to the zygomatic process, and areas of desired fat transfer.7 For PTFL cases we marked the anterior border of the masseter muscle as well as a line from the earlobe to the ala of the nose, delineating the upper limit of the subcutaneous lower face and neck dissection (Figure 2).
Figure 2.
Surgical marking. Surgical marking includes the bony architecture, Pitanguy's line, the anticipated location of the sentinel vein in the temporal area 1 cm superior to the superior zygomatic arch and 1 cm lateral to the zygomatic process, and areas of desired fat transfer. For PTFL cases we mark the anterior border of the masseter muscle as well as a line from the earlobe to the ala of the nose delineating the upper limit of the subcutaneous lower face and neck dissection. PTFL, ponytail facelift.
MAC (monitored anesthesia care) with propofol sedation was administered in all cases. Intubation was avoided to prevent distortion of the face. A nasal trumpet or an oral airway was placed. A Foley catheter was placed in all cases. During the onset of sedation, the hair was braided by the surgeon in accordance with incision planning.
The areas of dissection were infiltrated with local anesthesia solution (a mixture of 50 mL lidocaine 1% with epinephrine and 50 mL bupivacaine diluted 1:4 with saline, resulting in a 500-mL solution) for the regions of the lower face and neck. Typically, not all solution was utilized.
For the endoscopic forehead, brow, and cheek dissection, an extra ampule (1-mL 1:1000 epinephrine) was added to the solution and the approach was different to classic tumescent infiltration. Especially in regions such as the forehead, the volume of local anesthesia was limited to mitigate swelling. First, the temple incisions were injected subcutaneously and along the dissection plane. The paramedian incisions were injected subcutaneously and deep at the level of the periosteum. Next, the solution was injected along the temporal crest fusion line in the subperiosteal plane down to the brow. The orbital rims and glabellar region were then injected deeply along the periosteum. The final injections were placed along the superior and inferior zygomatic arch in the subcutaneous plane.
The typical duration of the procedures was 4 to 6 hours for PTL-I, 6 to 8 hours for PTL-II, 8 to 10 hours for PTFL-I, and 10 to 12 hours for PTFL-II. Local anesthesia with intravenous propofol was employed during the active dissection phase of the operation. During the second phase, in which suspension sutures for lifting, liposculpting, and final tailoring of the skin flaps was performed, the propofol was tapered to a minimal dose for a light sedation until the completion of the operation.
Surgical Details and Technical Considerations
Recommended Sequencing of the Ponytail Facelift
The sequencing of each procedure was paramount to the success of the entire operation. The goal was to maximize the vertical vector of tissue displacement before lateral SMAS/platysma tightening and skin excision in the neck. It was critical for both precision and to maximize the efficacy and synergistic effects of each maneuver (Table 3).
Table 3.
Procedural Steps
| Steps |
|---|
| 1. Skin-only lower blepharoplasty |
| 2. Limited incision of lower face and neck lift |
| 3. Contouring of deep neck structures (subplatysmal fat, anterior belly of the digastric, +/− submandibular glands) and anterior plication of the platysmal bands (anterior corset) |
| 4. Endoscopic forehead lift, brow rotation, deep plane cheek lift |
| 5. Lateral tightening of the SMAS and platysma (posterior corset) |
| 6. Redraping of excess neck skin, excision and tailoring of the post auricular incision or pretragal incision (if needed), and meticulous closure |
| 7. Microfat grafting for volume and shape, SNIF technique with micronized fat for deep wrinkles and retexturization |
| 8. Skin resurfacing with TCA peel or fractionated CO2 laser |
SMAS, superficial musculoaponeurotic system; SNIF, sharp-needle intradermal fat grafting; TCA, trichloroacetic acid.
Technical Details of the Procedural Steps
Skin pinch lower blepharoplasty: See Video 1. This step was completed first, before any swelling of the face occurred. A specific preparation of local anesthesia was administered. Lidocaine 2% was combined with hyaluronidase mixed 0.1:10 to help diffuse the solution evenly from a single injection point.8
The skin of the lower eyelid was pinched along the eyelash margin with fine forceps and a straight clamp, and the resection and closure were performed as previously described.9
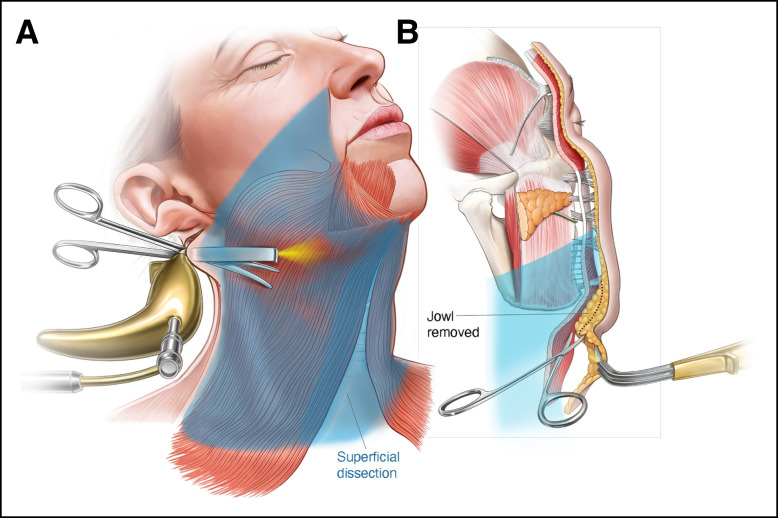
Limited-incision lower face and neck lift: See Videos 2-5. A perilobular incision was made initially to avoid the pretragal incision, if possible, which depended on the extent of skin that could be mobilized after completed dissection. The dissection plane was immediately superficial to the platysma and the neck fascia down to the clavicle, extending anteriorly across the midline of the neck and posteriorly to the anterior border of the trapezius muscle, where the spinal accessory nerve was protected (Figure 3A). The subcutaneous fat was lifted with the skin to preserve cutaneous blood supply. The purpose of this extensive undermining was to allow the skin flap to redrape naturally and to take tension off the skin closure. The added benefit was that the décolletage was also tightened.
Figure 3.
Limited incision of lower face and neck lift. On the left (A), the dissection plane is immediately superficial to the platysma and the posterior neck fascia down to the clavicle, extending anteriorly across the midline of the neck and posteriorly to the anterior border of the trapezius muscle. The subcutaneous fat is lifted with the skin to preserve cutaneous blood supply. On the right (B), the dissection plane is kept immediately above the SMAS, preserving the subcutaneous fat and blood supply with the skin. The medial extent of the subcutaneous dissection approaches the oral commissure. It is also important to release the mandibular retaining ligaments. Any thickening of the subcutaneous fat in the jowl area is directly trimmed with scissors to ensure even thickness. SMAS, superficial musculoaponeurotic system.
Care was taken not to injure the transverse cervical nerves and the great auricular nerves. It was very important to ensure all the subcutaneous fat was elevated with the skin and the platysma/SMAS fascia was cleanly dissected. Surgical loupes helped to better visualize the anatomy. The superior extent of the lower face dissection was limited to a line drawn from the ear lobule to the lateral ala of the nose. Also in this area the dissection plane was kept immediately above the SMAS, preserving the subcutaneous fat and blood supply with the skin.10 The medial extent of the subcutaneous dissection approached the oral commissure. It was also important to release the mandibular retaining ligaments.11 Any thickening of the subcutaneous fat in the jowl area was directly trimmed with scissors to ensure even thickness. Liposuction was avoided (Figure 3B). Attention was then turned to the deep plane dissection (Figure 4).
Figure 4.
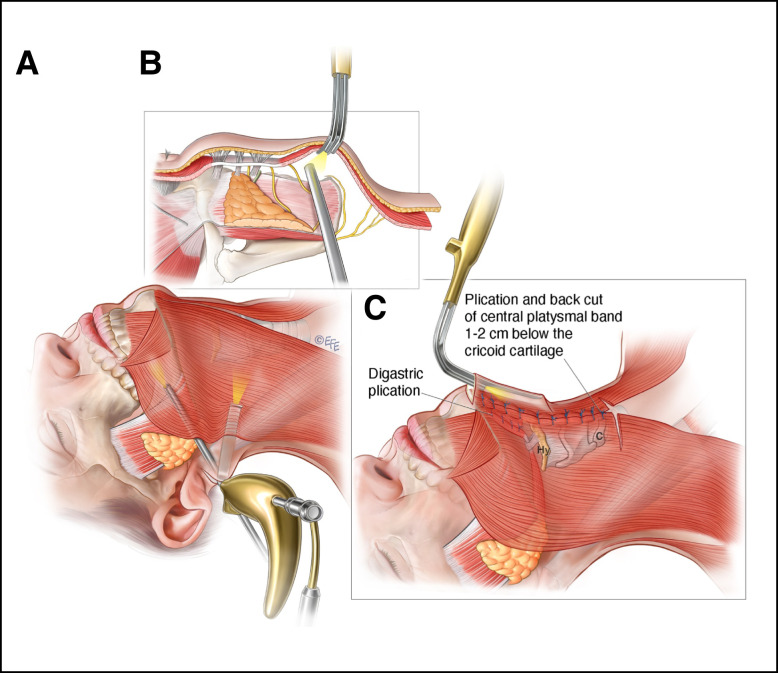
Lower face and neck deep plane dissection. (A) The lateral edge of the platysma/SMAS is sharply dissected off of the parotid fascia. Medially, the dissection of the SMAS is extended 2 cm past the anterior boarder of the masseter muscle (fixed SMAS), into the mobile SMAS. Inferiorly, the platysma/SMAS dissection continues 3 to 4 cm below the jawline. The subplatysmal dissection in the neck is extended about 4 cm medially to the area of the submandibular glands. (B) The buccal branch of the facial nerve may be visualized running in the parotid masseteric fascia. Care is taken to avoid injury to the marginal mandibular branch of the facial nerve. (C) A 2.5-cm submental curvilinear keyhole incision is made very anteriorly on the chin pad skin. The plane of dissection is immediately above the platysma. At the level of the submental incision, a horizontal entry is made perpendicular to the platysmal muscle fibers to dissect and lift the platysma muscle. Subplatysmal fat is then resected. The anterior belly of the digastric muscle is debulked with needle cautery as needed for contour and then plicated with 4.0 Ethibond interrupted sutures. Submandibular gland reduction is performed when indicated. The anterior edge of the platysma is plicated with interrupted suture, starting 2 cm below the cricoid cartilage and proceeding all the way up to the chin incision to avoid a cobra neck deformity. A 2-cm back cut on the bands is made below the most inferior plication suture. SMAS, superficial musculoaponeurotic system.
The lateral edge of the platysma/SMAS was sharply dissected from the platysma-auricular fascia with tenotomy scissors (Figure 4A). A very meticulous dissection was required here because the true SMAS fascia was thin medially and devoid of subcutaneous fat after the preservation of the fat with the skin in the previous surgical step. Medially, the dissection of the SMAS was extended 2 cm past the anterior border of the masseter muscle (fixed SMAS), into the mobile SMAS. The buccal branch of the facial nerve might be visualized running in the parotid masseteric fascia (Figure 4B). Beyond this point, the SMAS layer became very fragile, almost nonexistent. Any damage to the SMAS created during dissection was repaired with 4.0 Vicryl suture (Ethicon, Johnson and Johnson, New Brunswick, NJ) on a tapered needle. Inferiorly, the platysma/SMAS dissection continued 3 to 4 cm below the jawline (Figure 4A). The subplatysmal dissection in the neck was extended about 4 cm medially to the area of the submandibular glands. No transection of the platysma was performed here, as advocated by other surgeons.12 Care was taken to avoid injury to the marginal mandibular branch of the facial nerve. No attempt was made to dissect and denervate the cervical motor branches to the platysma. A traction test was performed; pulling on the lateral SMAS should have a tightening effect on the lower face and jawline. The posterior corset procedure (described later) was done after the endoscopic vertical suspension sutures were placed to avoid restriction of vertical lift of the platysma and the lower SMAS.
Anterior neck deep contouring and anterior platysmal plication: See Figure 4C. A 2.5-cm short submental curvilinear keyhole incision was made very anteriorly on the chin pad skin. The authors felt that it was worthwhile to work through a smaller anterior access and not to enlarge the skin incision, which would also necessitate moving it further down the neck. This avoided indentation or visibility of the scar. Again the plane of dissection was immediately above the platysma, keeping the fat supporting the skin. Dissection proceeded along the platysmal bands past the cricoid cartilage and connected the 2 sides of the neck dissection, working all the way down to the sternal notch. At the level of the submental incision, a horizontal entry was made perpendicular to the platysmal muscle fibers to dissect and lift the platysma muscle. Subplatysmal fat was then resected. The anterior belly of the digastric muscle was debulked with needle cautery as needed for contour and then plicated with 4.0 Ethibond interrupted sutures.13 Small and shallow bites near the digastric tendon were required to avoid entrapment of the hypoglossal nerve which ran posterior and deep to the digastric tendon. Submandibular gland reduction was performed when indicated. This anterior approach has been well described.13-15 The technical difference applied here was that a smaller incision in the chin pad was placed, in an effort to best hide the scar, despite the additional surgical challenge this might impose. By excising the subplatysmal fat and shaving the digastric muscles first, there was more space to work. It was important to plicate the remaining digastrics first, because they would pull the glands toward the midline where they could be more easily visualized. The cut edge of the glands was oversewn with 4.0 Vicryl sutures on a tapered SH needle (Ethicon) that was manually bent into a U shape. This facilitated suture maneuvering in a small space. This was important to help prevent postoperative bleeding and salivary leak. In addition, the cut surface of the submandibular gland was sutured to the platysma muscle with 4.0 Vicryl mattress sutures to reduce dead space and the risk of sialocele.
The anterior edge of the platysma was also plicated with 4.0 Ethibond interrupted suture (Ethicon), starting 2 cm below the cricoid cartilage and proceeding all the way up to the chin incision. We did not separate the platysma in the midline, but we did plicate the anterior border because we wanted to imbricate the interplatysmal tissue to strengthen the neck corset and avoid cobra neck deformity if there was cheese wiring of sutures postoperatively. A 2-cm back cut on the bands was made below the most inferior plication suture. At this point, any excess subcutaneous tissue in the submental area was directly excised with scissors. Similarly, through the posterior auricular incision, any excess fat in the submandibular jawline area was thinned. The skin and subcutaneous flap should be 1 uniform thickness from the lower face to the jowls, and throughout the entire neck. Liposuction was avoided to prevent dimpling and irregularities.
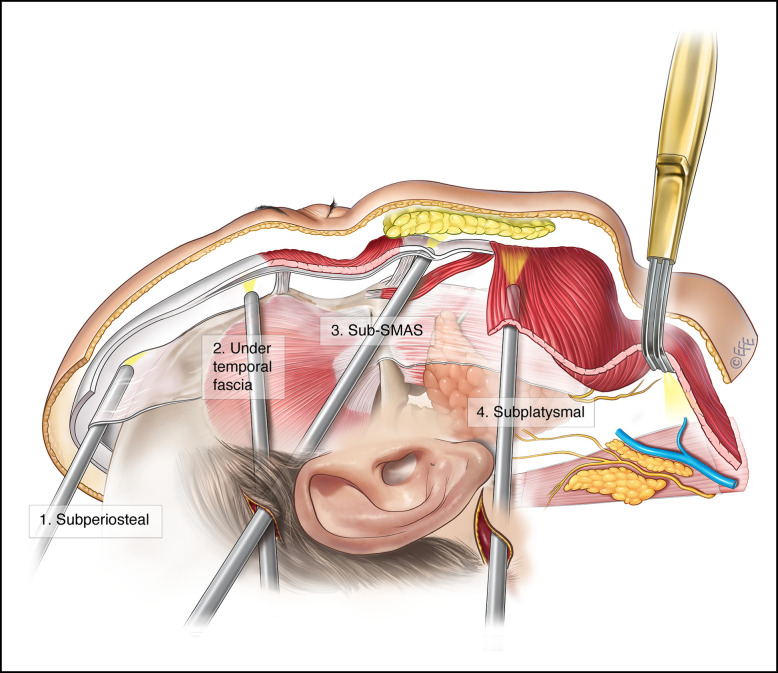
Endoscopic forehead lift, brow rotation, cheek lift: See Figures 5-7, Videos 6-12. A 2-cm temporal incision was placed in an oblique orientation parallel to the hair follicles, and a 1-cm paramedian incision was designed with a sagittal orientation. To successfully employ the cable suture technique (described later) to suspend and shape the brows, the placement of these incisions was important, not only for endoscopic access but also for the final position and shape of the brows.
Figure 5.
Endoscopic access and dissection planes: total deep plane dissection from cranium to clavicle. The dissection is performed between deep and superficial temporal fascia and done completely endoscopically. In the forehead and brow region, dissection is performed in the subperiosteal plane, all the way down past the orbital rim. In the temporal area, dissection proceeds endoscopically between the superficial and deep temporal fascia and continues down toward the zygomatic arch. The sentinel vein and the medial and lateral zygomaticotemporal neurovascular bundles are identified and preserved. Dissection continues to the arch, and the arch ligament is sharply released. The zygomaticomalar ligament also needs to be released to gain access to the midface. In the midface, the dissection plane is between the SOOF and the orbicularis oculi muscle. The dissection continues along the zygomaticus major and minor muscles, down across the nasolabial fold. The zygomatic branch of the facial nerve must be preserved in this region. To minimize the risk of nerve injury it is necessary to stay on the body of the zygoma and proceed medially, avoiding any lateral deviation. The midface flap that is mobilized across the nasolabial fold is suspended from several fixation points to the deep temporal fascia. SOOF, suborbicularis oculi fat.
Figure 7.
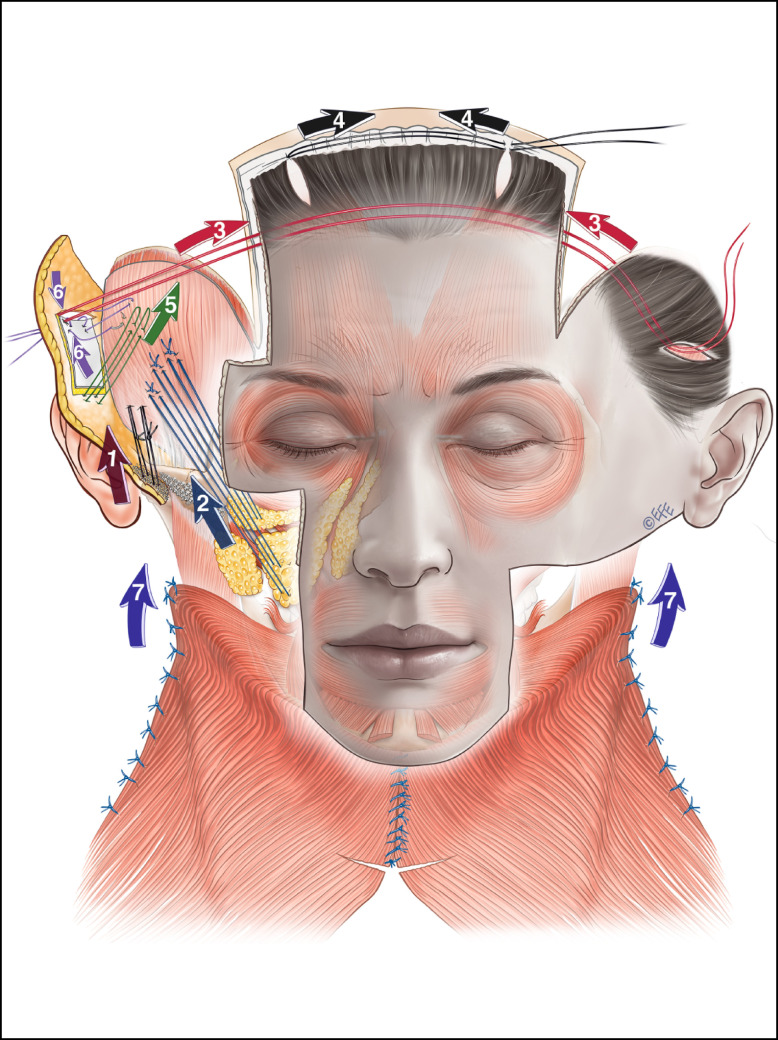
Suture tying sequence. After completion of the anterior platysma corset the following suture placement algorithm is extremely important to maximize vertical rotational tissue displacement. (1) We begin with the superior zygomatic arch sutures to the temporal fascia, usually 2 to 3 laterally in the “safe lane.” The exact positioning is determined by the relationship of the medial and lateral zygomatic lateral neurovascular bundles. (2) Next, we place 2 or 3 cheek sutures lifting the cheek fat pads toward the temple area. (3, 4) The next level of suturing connects the bitemporal (anterior wound edge) and paramedian (posterior wound edge) incisions to perform the brow rotation. (5) As a next step we place stiches that grab the TPF island on its distal cut edge and tie them to the temporal fascia. (6) The proximal edge of the TPF island flap is sutured to the temporal incision wound edge and fascia. (7) Finally, the posterior platysma corset is completed. Importantly, the assistant lifts the face vertically during the entire suture tying sequence, with hooks deploying tension from the paramedian incisions. TPF, temporoparietal fascia.
The temporal incision was placed lower than most incisions described for an endoscopic brow lift. Shifting the cheek fat pad toward the temporal hairline in the most effective vector and determination of an optimal vector for endoscopic visualization helped to pinpoint the ideal location for placement of the incision. Similarly, the vertically orientated paramedian incision was located to allow for the most aesthetically ideal brow rotation and shaping. Usually, a midline forehead incision is not necessary, unless the forehead is very broad (male patient) or very curved.
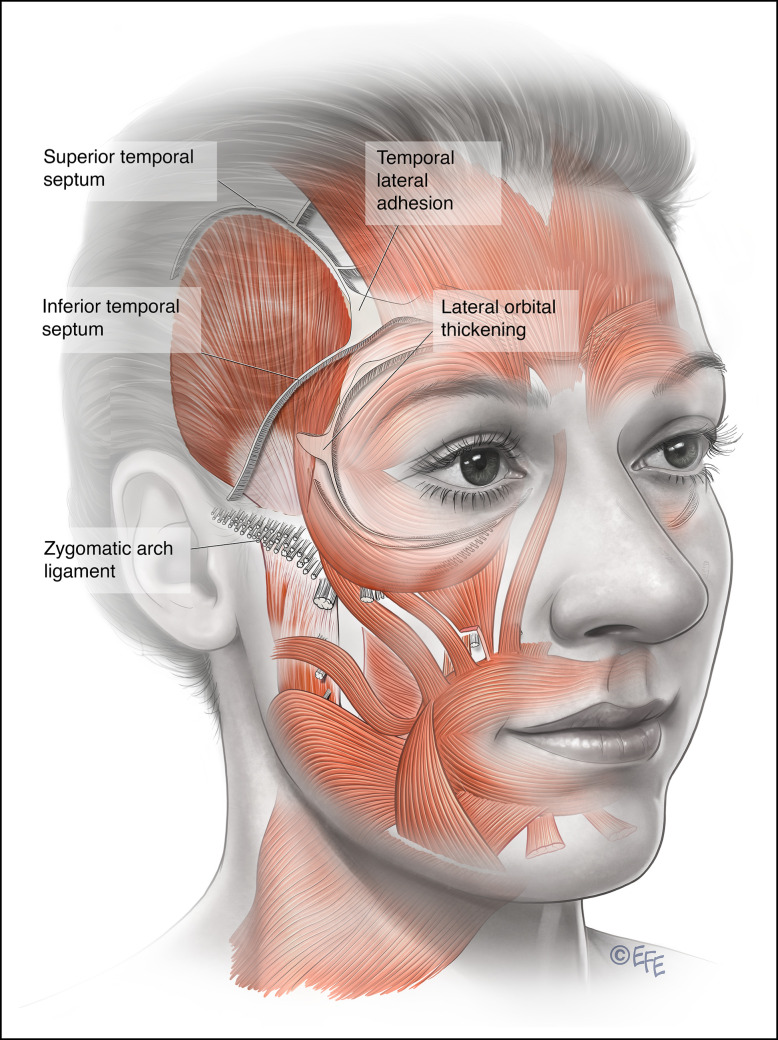
The dissection began with the formation of the optical cavity. Through the temporal incision, the space between the superficial and deep temporal fascia was entered. A flat elevator was inserted into this loose space to bluntly dissect toward the top of the ear. Then the elevator was swept posteriorly toward the vertex of the head and then pushed across the temporal crest, popping into the subperiosteal plane of the forehead, connecting to the paramedian scalp incision. On the right side of the patient's head, the endoscope was inserted in the paramedian incision, as the elevator was working from the temporal incision. On the left side of the patient's head, the endoscope was looking through the temporal incision and the elevator was dissecting through the paramedian incision (Figure 5). For a successful and long-lasting forehead lift and brow rotation, there were 5 anatomical entities that needed to be completely released (Figure 6):
Figure 6.
Ligamentous release points. For a successful and long-lasting forehead lift and brow rotation, there are 5 anatomical entities that need to be completely released: the superior temporal septum; temporal lateral adhesion; zygomatic arch ligament; inferior temporal septum; lateral orbital thickening; and external canthal tendon (if lateral canthal tilt is desired).
superior temporal septum (STS)
temporal lateral adhesion (TLA)
zygomatic arch ligament
inferior temporal septum
(+/−) lateral orbital thickening (LOT) or external canthal tendon (if a lateral canthal tilt was desired)
The frontal orbital periosteum at the glabellar/galea area was dissected in accordance with the planned shape of the eyebrow (brow fashioning). The dissection started high on the temporal fusion line, releasing the STS. Near the orbital rim there was a small vein that was unnamed in anatomical literature, but we found it to be a consistent structure and referred to it as the temporal crest vein. At the edge of the orbital rim was the TLA. This was a very dense structure that needed to be completely released. The endpoint was when the elevator was seen dropping off of the bony rim and dipping into the orbit under the orbicularis oculi. Sharp-tip scissors were required to spread and expand the lateral orbicularis. Failure to completely release the TLA and lateral orbicularis would lead to inadequate elevation of the lateral brow and early recurrent brow ptosis.
Next, the zygomatic arch ligament was dissected with both the endoscope and the sharp-tip scissors through the temporal incision. The loose tissue in this area was easily dissected until near the zygomatic arch ligament where the fibers became dense. Sharp scissors were necessary to dissect around the superficial temporal artery and vein. A 25-gauge needle was inserted percutaneously where the lateral Pitanguy's line crossed the superior arch in the surface marking (Figure 2, Video 6). The needle was then visualized endoscopically. Lateral to the needle constituted a “safe lane” for crossing the body of the arch into the lower face. The dissection transitioned to a deep subcutaneous/supra-SMAS plane at the lower border of the arch and continued downward to connect with the previous dissection in the lower third of the face. This created an approximately 2-cm tunnel connecting the temporal dissection to the lower face dissection.
In PTL-I patients, when some degree of tightening of the lower face/jowls was desired, an endoscopic platysma/SMAS cranial suspension was performed as an adjunct (Video 7). In this case the dissection was continued from the superior arch along the safe lane. At the inferior arch the dissection plane changed to the subcutaneous plane and was continued on top of the platysma/SMAS to the gonial angle. A 3.0 nylon suture was placed on the platysma/SMAS and was anchored to the deep temporal fascia. This maneuver tightened the platysma/SMAS and corrected any early jowling together with laxity of the neck.
In the forehead and brow region, dissection was performed in the subperiosteal plane, all the way down to the orbital rim. The periosteum and the galea were sharply released across the entire width of the forehead and undermined back to the vertex of the head. Dissection continued past the orbital rim, under the orbicularis oculi muscle, on top of the orbital septum, and all the way to the upper eyelid cartilage. This allowed the upper eyelid skin to be redraped; this was the basis of the nonincisional upper blepharoplasty. If a more dramatic look was desired, the corner of the eye could be rotated (almond eyes or fox eyes) by an endoscopic release and suspension of the LOT with a stitch to the temporal fascia. The glabellar frown lines were the result of the collective actions of the corrugator muscles, the depressor muscles, and the procerus muscle. These muscles were treated selectively by cutting the muscle fibers with sharp scissors under direct endoscopic vision.16 When indicated, multiple myotomies were performed in the lateral orbicularis oculi muscle, because it was the depressor of the lateral brow. The supraorbital neurovascular bundle was carefully identified and preserved.
The dissection continued down to the midface through the loose areolar tissue of the inferior orbital septum. In the midface, the dissection plane was between the suborbicularis oculi fat (SOOF) and the orbicularis oculi muscle. The dissection continued on to the midface in the sub-SMAS or the deep plane, on top of the zygomaticus major and minor muscles. It was critical not to dive into the bodies of the zygomaticus muscles, which might affect upper lip function. A Trepsat dissector (Carnegie Surgical, East Windsor, NJ) was helpful in defining the sub-SMAS plane and the zygomaticus muscles. The endpoint of midface dissection was across the nasolabial fold. This helped to efface the nasolabial folds as the cheek was lifted. The zygomatic branch of the facial nerve innervating the lower orbicularis oculi muscle was just at the lateral border of the zygomaticus major and was usually not exposed. To minimize the risk of nerve injury it was necessary to stay on the body of the zygoma and proceed medially, avoiding any lateral deviation (Videos 8, 9).
No screws or Endotine (MicroAire Surgical Instruments, Charlottesville, VA) were placed for fixation, in contrast to the published literature.17 The direct suspension by fixation at the paramedian incision utilizing screws or Endotine tends to peak the brow at the midpoint which, in our opinion, is not an ideal shape for a beautiful brow aesthetic and may lead to a surprised look. It is preferable to rotate the lateral brow with a cable suture suspension system, similar to an approach pioneered by Nicanor Isse (personal communication; Figure 7). Suspension sutures with 3.0 nylon between the 2 temporal incisions were placed to rotate and suspend the lateral brow when tied to each other. This was a free-floating cable suture taking a bite of temporoparietal fascia (TPF) on the medial aspect of the temporal incision on the right side, then passing both ends underneath the forehead flap all the way across the forehead and out of the left temporal incision. Another bite of the TPF was taken on the left temporal medial incision. When this free-floating suture was tied, the shortening length of the suture across the forehead acted to rotate the lateral brow. Another cable suture was placed between the 2 paramedian incisions, taking a bite of the galea to provide additional lift and rotation of the brow (Videos 10, 11).
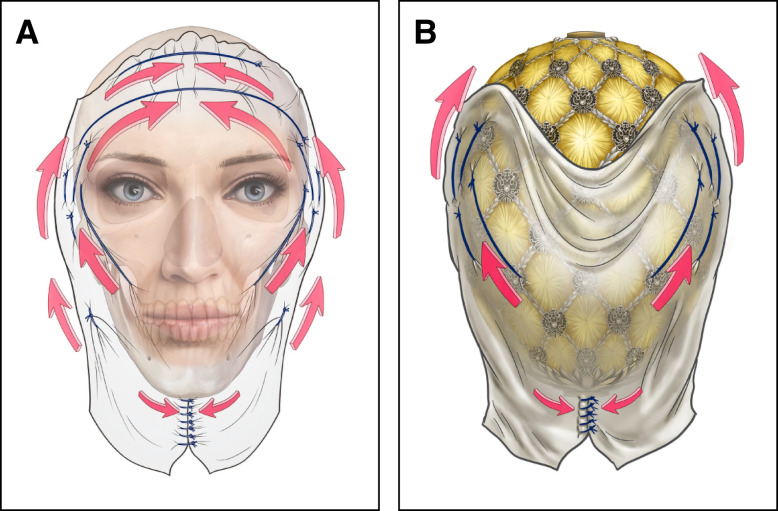
The midface flap that was mobilized across the nasolabial fold was suspended from several fixation points to the deep temporal fascia. The combination of wide dissection and anterior suture placement at the high point of the malar fat pad allowed for an effective and long-term lift of the anterior face (which is the part that ages), without relying on traction on lateral sutures.18 Number 3.0 nylon sutures were placed under direct endoscopic vision from the cheek fat pad, lateral orbicularis oculi muscle, and superficial temporal fascia to the deep temporal fascia. Temporal fixation points were very important for elevation of the cheek and the lateral brow (Video 12). A TPF “island” was created to serve as a relaxing incision and to transmit the force of the vertical pull from the deep TPF plane to a subcutaneous plane. An approximately 1 × 1 cm square patch was incised with the needle cautery from the edge of the temporal scalp incision. The incision was made in the TPF until the subcutaneous fat was visualized. Care was taken to control the superficial temporal artery and veins with cautery or suture ligation. Once the TPF island was created, the first set of 3.0 nylon sutures was fixated from the distal edge of the TPF island to the deep temporal fascia. Then a second set was fixated from the proximal edge of the temporal scalp incision to the deep temporal fascia to transmit the pulling force to the subcutaneous plane and help tighten the skin of the temporal and cheek area. The sequence of suture tying was extremely important for maximizing a vertical lift and a central rotation. The resulting vector of suspension was a novel concept in facelifting, which we call a “Fabergé vector.” We have summarized the process in illustrations (Figures 7, 8, Video 13).
Figure 8.
Progressive tension concept of the vertical-central lift (Fabergé vector). Tying the sutures from bottom to top enables an ideal brow positioning and vertical lifting of all tissues from clavicle to cranium, as depicted in (A). This leads to a heart shaped tapered face with the ideal proportions of an inverse Fabergé egg, as depicted in (B).
Posterior neck corset: See Videos 14, 15. The posterior neck corset was performed by plicating the lateral edge of the platysma muscle to the posterior neck fascia starting from 2 cm superior to the level of the occipital triangle and proceeding to the lower third of the face. This was done with a 4.0 interrupted Vicryl suture followed by 4.0 Vicryl running suture. In the lower face, the platysma/SMAS was pulled vertically by the jowl suspension sutures. A small 1-cm back cut similar to the platysmal window was performed to reorient the vector of pull in the neck posteriorly.19 Care was taken to avoid strangulating the great auricular nerve. This maneuver resulted in a longer and sleeker-appearing neck contour and a sharper jawline, and allowed more neck skin to be excised posteriorly.
Contouring the neck skin flap: Now that all of the muscle plication in the posterior corset was completed, the neck skin flap had to be contoured evenly. In a heavy neck the skin flap was thick in the submental region and lateral jawline area. A direct excision thinning with scissors was preferred. Liposuction was minimized to avoid irregularity and scar band tethering.
At this point, the neck should look perfectly contoured with a sharp cervical mental angle and a clean jawline. However, the neck skin was not tailored and closed until the vertical lift of the upper face redistributed the skin. This was important because if the neck skin was only transposed posteriorly there would be fullness and bunching in the periauricular and pretragal area. To ameliorate this skin bunching, the perilobular incision might need to be extended superiorly into the pretragal area. However, for most patients, this pretragal/perilobular skin could be distributed vertically with the endoscopic temporal and cheek lift, avoiding an extension of the incision up into the pretragal skin.
Microfat grafting: Fat was harvested from wherever the patient had excess, preferably accessible from the supine position. The inner thigh was most preferred, followed by the lateral thigh, lower abdomen, and upper abdomen. The approach taken was similar to a classic Coleman technique (hand suction with a 10-mL syringe).20 For facial detailing, sharp-needle intradermal fat grafting (SNIF) was employed.21 The average grafting volumes are summarized in Table 4.
Table 4.
Fat Grafting Volumes
| Region | Volume |
|---|---|
| Total | 40-60 mL |
| Sub brow/eyelid area | 3-5 mL per side |
| Brow | 1 mL per side |
| Glabella and nasal bridge | 2-3 mL |
| Temple area | 10 mL per side |
| Lower lid cheek junction | 2-3 mL per side |
| Nasolabial fold | 3-5 mL per side |
| Lip (upper and lower) | 2-3 mL upper; 3-4 mL lower |
| Chin point | 2-3 mL |
| Chin groove | 2-3 mL |
| Marionette area | 3-5 mL per side |
| Forehead | 10-15 mL |
| Submalar area | 2-3 mL per side |
| Masseter area | 2-3 mL per side |
Skin resurfacing: Until 2010, TCA peel was done exclusively. Depending on the skin thickness, 15% to 20% TCA was employed. Later in the case series, TCA was utilized for skin types Fitzpatrick 4 and above only and Asian patients in general. All other patients were treated with fractionated CO2 laser. We utilized the laser very conservatively (30 J around the orbit, 40 J in the forehead and cheeks, and 40 to 45 J in the perioral and nasal areas).
Skin closure was performed in layers and begun in the postauricular space. Interrupted 4-0 nylon clear sutures were placed deep, and subcutaneously 5-0 PDS interrupted sutures (Ethicon) were placed 5 mm apart. The skin was closed with a 6-0 Prolene (Ethicon) running suture. In the scalp, 5-0 clear nylon is placed. Chin closure was performed with 5-0 PDS interrupted and running suture. Preauricular skin closure was performed with 5-0 clear nylon in the deep layers, and 6.0 PDS interrupted and 6-0 Prolene running sutures were placed at the skin level. Drains were placed across the forehead and diverted to the mastoid area. A drain was placed underneath the chin and another was placed at the bottom of the neck dissection. Drains come out after 5 days, sutures in the auricular area and the lower eyelids were removed after 4 days, and all other sutures were removed after 7 days.
Our standard postoperative regimen included taping the cheek, forehead, and brow area to reduce periorbital edema. For the same reason, we advised our patients to rest in a supine position for 2 days (also to assist with lymphatic drainage). We kept the patient supine because we had performed extensive undermining to the scalp posterior to the vertex. Although there was a drain in place, we preferred that fluid dissipated back toward the vertex, avoiding accumulation around the eyes. Hyperbaric oxygen therapy was advised to improve wound healing. Checkups took place every day for 5 days. After that follow-up was weekly for 3 weeks postoperatively, followed by 6 weeks postoperatively, and then at 3 months and 1 year.
RESULTS
A PTL was conducted in 209 patients (196 female, 13 male), with an average age of 42 years (range 17-71). Global facial rejuvenation by PTFL was performed in 391 patients (375 female, 16 male) with an average age of 55 years (range 31-82). All perioperative and postoperative complications including reoperations and reasons for revisions were recorded in a prospective patient database. The patients included in the study were followed for a minimum of 1 year postoperatively, and the average follow-up was 2.7 years, with a range of 1 to 17 years. (Figures 9-13). The results were analyzed by means of descriptive statistics (Table 5).
Figure 9.
Representative result of Ponytail Lift Type I. This 36-year-old female patient was battling early signs of aging (sagging of the brows, hooding of the upper lids, drooping of the cheeks, deepening of the nasolabial folds, formation of jowls). She had been receiving fillers for the last 8 years unsuccessfully trying to lift her face, resulting in distortion of her delicate features. We dissolved the fillers in her cheeks, undereye areas, and jawline, performed a Ponytail Lift Type I and an upper lip lift. This allowed us to restore the delicate features and harmonize the face without any visible scars. Parts A, C, E, and G show the patient preoperatively, and parts B, D, F, and H show her results 1 year postoperatively.
Figure 13.
Representative result of Ponytail Facelift Type II. We performed a Ponytail Facelift Type II in this 58-year-old female patient to achieve a panfacial rejuvenation from the top of the head to the bottom of the neck. She was looking for a transformation in the shape of her face: from a square jowly shape to a V-shape of youth. (A), (C), (E), and (G) show the patient preoperatively, and (B), (D), (F), and (H) show her results 3 years postoperatively.
Table 5.
Complications and Revisions
| Complication | Prevalence (%) | Revision |
|---|---|---|
| Hematoma | 2 (0.33) | Evacuation |
| Seroma | 1 (0.17) | Needle aspiration |
| Fat graft lumpiness | 4 (0.67) | Needle aspiration or mini liposuction under sedation (office setting) |
| Infection/delayed healing | 3 (0.5) | Dressing changes, local ABs |
| Sialocele | 1 (0.17) | Neurotoxin injection |
| Transient neuropraxia of the frontal branch of the facial nerve | 29 (4.88) | None, resolved after 6-12 weeks |
| Transient neuropraxia of the hypoglossal nerve | 2 (0.33) | None, resolved after 4 weeks |
| Transient alopecia at the incision site | 2 (0.33) | None, resolved after 3-4 months |
| Transient asymmetry of the lower lid with scleral show | 2 (0.33) | None, resolved after 6 months |
ABs, Antibiotics.
Figure 10.
Representative result of Ponytail Lift Type II. This 42-year-old female patient desired facial rejuvenation because of laxity of the upper eyelids and flat cheeks with early jowling. She also complained about submental fullness, an undefined jawline, and neck laxity. However, skin quality overall was still good and there was not enough skin redundancy to require resection. Therefore, her needs were addressed with a Ponytail Lift Type II without any skin removal. Additionally, correction of an unsatisfactory lip lift scar was performed. (A), (C), (E), and (G) show the patient preoperatively, and (B), (D), (F), and (H) show her results [x] years postoperatively.
Figure 11.
Representative result of Ponytail Facelift Type I. This 57-year-old female patient is now 2 years following her Ponytail Facelift Type I. She complained about general signs of aging with a particular focus on her neck. We lifted the entire deep plane from the top of her head to the bottom of her neck and tightened it without the traditional facelift incisions along the temple hairline and in front of the ear. An upper lip lift with an internal corner lift was also performed. (A), (C), (E), and (G) show the patient preoperatively, and (B), (D), (F), and (H) show her results 2 years postoperatively.
Figure 12.
Representative result of Ponytail Facelift Type I with extended follow-up. This 69-year-old female patient received a Ponytail Facelift Type I 17 years ago. No fillers or other minimal invasive treatments or surgical interventions have been performed elsewhere in the meantime. Even after this period of time, her brow has maintained its corrected position and the midface and neck are still satisfactory. (A), (C), (E), (G), and (I) show the patient preoperatively, and (B), (D), (F), (H) and (J) show her results 17 years postoperatively.
There were no instances of postoperative skin flap necrosis. Simultaneous skin resurfacing healed in 5 to 7 days without hyperpigmentation or hypopigmentation. Hematoma occurred in 2 cases and 1 patient had a seroma that only required needle aspiration. Transient neuropraxia of the frontal branch of the facial nerve developed in 29 patients (4.88%) and resolved in 6 to 12 weeks spontaneously. No permanent nerve injuries were recorded. Fat grafting resulted in minor palpable lumpiness in 4 cases. Infection or delayed healing occurred in 3 cases and required regular dressing changes and local antibiotics. An additional surgical touch-up procedure to address unsatisfied aesthetic needs was performed in 20 cases (see Table 6 for details).
Table 6.
Revisions for Aesthetic Reasons
| Complication | Prevalence (%) | Revision |
|---|---|---|
| Asymmetry of the canthal tilt | 3 (0.5) | Readjustment of the midface suspension |
| Canthal indentation | 1 (0.17) | Readjustment of the midface suspension |
| Transient cheek indentation | 12 (2) | Hyaluronic acid fillers to bridge time until spontaneous resolution |
| Persistent nasolabial fold | 5 (0.84) | Readjustment of the cheek suspension |
| Persistent skin redundancy in the lower face and neck | 12 (2) | Additional tightening (tuck-up) |
Taken together our clinical data clearly demonstrate the ponytail procedures to be safe and effective. These endoscopic facelifts result in aesthetically pleasing results with a natural appearance. Applicable to the full spectrum of facial aging, these novel techniques enable the skilled surgeon to deliver very satisfying outcomes with an acceptable complication rate.
DISCUSSION
Facial aging as a process is more than descent and stretch of tissues. The perception that the aging face is falling is only partially true; there are areas of the face that expand and contract with aging. It is that expansion or contraction that makes it look like things are descending.22 The focus of modern facelifting has therefore shifted to providing necessary volume restoration and overall facial shaping. Volume deflation is a major component of facial aging but cannot be corrected solely by rhytidectomy.23 In recent years, a large majority of plastic surgeons have adopted fat grafting as an important supplement to facelift surgery.24 However, the classic incisions can cause noticeable scarring in front of the ears, shortening of the sideburns, and distortion of the ear's anatomy.3 Also, facelifts continued to be mostly lateral vector techniques (with some surgeons advocating a vertical-lateral vector).25 The possible unfortunate results of these traditional procedures are becoming easy to recognize.26 The unopposed tension of lateral vector facelifts allows the cheek tissues to descend eventually over the tightened jawline, creating a “lateral sweep” or pulled appearance of the face.27 In addition, due to devascularization and thinning of the skin, some patients develop new skin capillaries over the areas of skin undermining. This neovascularization may be induced by chronic hypoxia. Patients with friable thin skin may be more prone to this complication and therefore less suitable for the traditional SMAS dissection and lifting with lateral vector approaches.
In an attempt to resolve these shortcomings, and following the trend toward short scars and a less invasive facelift, the MACS (minimal-access cranial suspension) lift was introduced by Tonnard et al in 2002.28,29 This approach utilizes a short incision, confined to the preauricular region and the temporal hair tuft, through which 3 purse-string sutures are placed that elevate the jowls, the central cheeks, and the malar fat. We feel that the vertical vector–based facelift concept of pull is a major improvement over the traditional SMAS facelift. However, the looping sutures utilized may create some distortion and pretragal incisions result in scars with a shifted hairline.
Combining Hamra’s deep plane technique with the vertical vector concept of the Tonnard et al MACS lift resulted in the MADE (minimal-access deep-plane extended) lift approach popularized by Jacono et al over the last decade.30 However, the incisions placed at and around the sideburns and in the tragal area require exceptional finesse in both planning and execution. Trichophytic closure may help but still does not guarantee success for every patient. If not done diligently the scars and hairline distortions are noticeable. This is a highly cosmetically sensitive area. When the sideburns are foreshortened or displaced or the scar is wide or the tragus is flattened or pulled open, it is an easily recognizable facelift stigma.31
The authors’ preference is to avoid tampering with the tragal area if at all possible. This concept is not entirely new and was previously described by Besins, however without dissection of the retaining ligaments of the face (Figure 6), limiting the release and redistribution of tissue vertically.32 An important point is that the pretragal incision only rarely is needed for skin resection. Excess skin is predominantly formed in the neck and the lower third of the face, where movement of the head and mouth takes place.22 The excess skin mobilized during the facelift is removed as needed by tailoring behind the ear. In contrast, the upper two-thirds of the face suffers from deflation and descent in the process of aging, leading to the need for resuspension and redraping of tissue rather than excision. Consequently, if the pretragal incision is only needed for better access to the operating field, it can be avoided by employing advanced endoscopic dissection with hidden incisions. The advent of endoscopy in plastic surgery was initiated by pioneers such as Nicanor Isse, Louis Vasconez, and Grady Core, who introduced the new modality to brow lifting in the early 1990s.16,33 Renato Saltz and Oscar Ramirez advanced the endoscopic approach to facial rejuvenation further. Nicanor Isse invented the use of cable sutures to suspend the brow. Renato Saltz popularized Endotine.34 Oscar Ramirez championed the subperiosteal plane of dissection for the midface.35 All these innovative endoscopic techniques were largely limited to the face, and hardly any endoscopic approaches were applied to the lower face and neck.36
Integrating all advantages and avoiding all disadvantages of the previously described open and endoscopic methods for facial rejuvenation, the ponytail lift is a fully endoscopic approach based on vertical tension vectors. In comparison to the MACS lifting procedure, it is possible to accomplish a comparable vertical lifting result without the cutting of the sideburns. PTL-II allows for lifting and tightening the jowls and jawline and results in a heart-shaped, tapered face. Conducting extended endoscopic dissection across the face and posterior neck, the ponytail lift yields superior results in the midface, where many short scar techniques fail. Despite the minimal incisions and the preservation of the natural blood supply to the skin and facial tissues, the ponytail technique allows for extensive shaping and sculpting of the face and neck. Microfat transfer is a safe adjunct for delivery of shape and support. Simultaneous CO2 laser can be performed because the skin is not devascularized.
Our analysis demonstrates the ponytail procedures to have globally low complications. Specifically, hematoma, seroma, skin necrosis, and tuck-up rates are below the numbers reported in the literature.37 With regard to hematoma prevention, the hemostatic net is gaining traction among plastic surgeons worldwide.38 We do not utilize the net and feel comfortable with our approach despite a very complete release. In our technique algorithm the lateral neck dissection is followed by the deep neck dissection. The plane of dissection is supraplatysmal, which is an anatomical plane that has few crossing perforators, and we visualize and cauterize them as we encounter them. Also because of the sequence of the operation the neck is left open while we turn our attention to the endoscopic part of the operation. This gives us time to manage any bleeding that occurs after the epinephrine has dissipated.
A possible explanation for the subsequent low tuck-up rates is that in traditional facelift procedures the skin tends to get thinned out, leading to atrophy and a loss of support over time. When vasculature is deprived, subcutaneous tissue shrinks and the overlying skin becomes loose. Additionally, the fat transfer component of the ponytail procedures further leads to skin quality improvement and explains the distinctly lower tuck-up rates of 2% in our cohort, compared to around 50% with SMAS-ectomy, more than 20% for SMAS-plication, and around 4% for the MADE lift.37,39,40 Importantly, we consider a tuck-up procedure a surgical correction for a patient who is not entirely satisfied with the level of tightness of the face within the first year postoperatively. A secondary facelift is for a patient who was initially satisfied but has aged further and requires more tightening because of recurring skin laxity.
The reported incidence of temporary neuropraxia in a survey of more than 12,000 facelifts was 2.1%.41 However this is not the average for endoscopic facelift approaches, which have a frontal branch neuropraxia rate of about 4% in expert hands, and for pure endoscopic brow lifts an even higher rate, according to the literature.42 The 4.9% of transient neuropraxias that all completely resolved within 6 to 12 weeks in our study cohort were therefore within the reported incidence. Neuropraxia is generally due to the extensive endoscopic dissection at the zygomatic arch at the junction with the midface. The nerve is located right above the dissection plane and the slightest stretching or rubbing against the nerve can lead to transient neuropraxia. Also, fat grafting and associated postoperative swelling can be a root cause of this complication and is difficult to avoid completely.
In this paper we report our approach in as much detail as possible to enable the reader to understand the “ins and outs” of the ponytail lift and its preoperative preparation and aftercare. Key limitations of this paper include the lack of objective measures of success and reported patient-related outcomes. This caveat will be addressed further in planned research studies, with certain aspects of the procedures presented in greater detail. The presented technique is complicated and expert mentoring is certainly beneficial, but the ponytail lift is a skill most surgeons can acquire if they have the hand and eye coordination for endoscopy, patience, and stamina. We recommend starting with just the brow portion of the procedure, followed by the midface and zygomatic arch dissection. The lower face dissection and the neck lift should be added last. A pivotal factor for the success of the procedure is the collaboration with an experienced anesthesia team comfortable with prolonged MAC anesthesia cases. If performed correctly endoscopic procedures will be effective. In contrast to the hypotheses and observations of Chiu and Baker, who described a 70% decline of endoscopic brow lifts from 1997 to 2001 at the Manhattan Eye, Ear and Throat Hospital, we consider these kinds of procedures to be the future of facial plastic surgery.43 We agree with Biggs in his reply to this study that the technique performed by Chiu and Baker is questionable and should be reviewed before dismissing this approach.44 We share with Biggs and numerous other surgeons worldwide the finding that endoscopic techniques in the face are effective in nearly all cases and carry an extremely low complication rate. We rank procedures evaluated with a risk-reward ratio higher than any others in our surgical armamentarium. It is noteworthy that other specialties like ENT and oculoplastic surgery have incorporated endoscopic techniques developed by plastic surgeons as standard procedures in facial surgery without questioning their effectiveness if performed correctly. We consider the negative impact the publication of Chiu and Baker had, and maybe still has, on the development of endoscopy in our specialty very unfortunate, and we hope that this manuscript helps stimulate the enthusiasm of young plastic surgeons regarding the value of endoscopic procedures in facial plastic surgery.43
CONCLUSIONS
In this study we summarize the lessons we have learned and some innovative approaches we developed for a modern facelift approach to improve outcomes. The ponytail lift intends to harness all the benefits and to avoid potential shortcomings of previously described facelift techniques. However, the implementation of an innovative method can pose a challenge for surgeons, and as with any advanced technique there will always be many who reject these innovations for their own reasons. When employing the ponytail approach, unlike in the traditional SMAS facelift, the skin is not delaminated from the underlying fat and not devascularized. There is no formal SMAS elevation in the upper face and, unlike in the MADE, short scar, or MACS facelift, the aesthetically sensitive tragal area and the sideburns remain undisturbed. Being a total deep plane facelift without the scar burden means that most of the incisions are hidden in the temple, postauricular, and posterior scalp. We found in our study cohort of 600 patients over 22 years that ponytail procedures were able to refresh or transform the face with minimal incisions while preserving the natural blood supply to the skin and facial tissues. The described techniques are safe and effective and provide reliable and satisfying results.
Supplemental Material
This article contains supplemental material located online at www.aestheticsurgeryjournal.com.
Supplementary Material
Acknowledgments
The authors thank Jessica Jane de Felipe, Chrissy Quiambao, and Carol Francisco for their support in data acquisition. The authors also want to thank Dr Levent Efe for the contribution of brilliant illustrations and Victor Bruno for arrangement of the video content.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1.Swift A, Liew S, Weinkle S, Garcia JK, Silberberg MB. The facial aging process from the “inside out”. Aesthet Surg J. 2021;41(10):1107–1119. doi: 10.1093/asj/sjaa339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carniol PJ, Ganc DT. Is there an ideal facelift procedure? Curr Opin Otolaryngol Head Neck Surg. 2007;15(4):244–252. doi: 10.1097/MOO.0b013e32825a678d [DOI] [PubMed] [Google Scholar]
- 3.Hashem AM, Couto RA, Surek C, Swanson M, Zins JE. Facelift part II: surgical techniques and complications. Aesthet Surg J. 2021;41(10):NP1276–NPNP94. doi: 10.1093/asj/sjab081 [DOI] [PubMed] [Google Scholar]
- 4.Hashem AM, Couto RA, Duraes EFR, et al. Facelift part I: history, anatomy, and clinical assessment. Aesthet Surg J. 2020;40(1):1–18. doi: 10.1093/asj/sjy326 [DOI] [PubMed] [Google Scholar]
- 5.Luu NN, Friedman O. Facelift surgery: history, anatomy, and recent innovations. Facial Plast Surg. 2021;37(5):556–563. doi: 10.1055/s-0040-1715616 [DOI] [PubMed] [Google Scholar]
- 6.Ramirez OM. High-tech facelift. Aesthetic Plast Surg. 1998;22(5):318–328. doi: 10.1007/s002669900210 [DOI] [PubMed] [Google Scholar]
- 7.Pitanguy I, Ramos AS. The frontal branch of the facial nerve: the importance of its variations in face lifting. Plast Reconstr Surg. 1966;38(4):352–356. doi: 10.1097/00006534-196610000-00010 [DOI] [PubMed] [Google Scholar]
- 8.Nathan N, Benrhaiem M, Lotfi H, et al. The role of hyaluronidase on lidocaine and bupivacaine pharmacokinetics after peribulbar blockade. Anesth Analg. 1996;82(5):1060–1064. doi: 10.1097/00000539-199605000-00032 [DOI] [PubMed] [Google Scholar]
- 9.Rosenfield LK. The pinch blepharoplasty revisited. Plast Reconstr Surg. 2005;115(5):1405–1412; discussion 1413-4. doi: 10.1097/01.PRS.0000157020.67216.31 [DOI] [PubMed] [Google Scholar]
- 10.Hoefflin SM. Facial rejuvenation-my personal evolution. Aesthet Surg J. 1998;18(4):286–289. doi: 10.1016/S1090-820X(98)70062-7 [DOI] [PubMed] [Google Scholar]
- 11.Hoefflin SM. The ligamentous facial fence: the cause of nasolabial folds and jowling. Plast Reconstr Surg. 1998;101(4):1148. doi: 10.1097/00006534-199804040-00048 [DOI] [PubMed] [Google Scholar]
- 12.Jacono AA, Alemi AS, Harmon JJ, Ahmedli N. The effect of a novel platysma hammock flap during extended deep plane facelift on the signs of aging in the neck. Aesthet Surg J. 2022;42(8):845–857. doi: 10.1093/asj/sjac086 [DOI] [PubMed] [Google Scholar]
- 13.Marten T, Elyassnia D. Neck lift: defining anatomic problems and choosing appropriate treatment strategies. Clin Plast Surg. 2018;45(4):455–484. doi: 10.1016/j.cps.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 14.Bravo FG. Reduction neck lift: the importance of the deep structures of the neck to the successful neck lift. Clin Plast Surg. 2018;45(4):485–506. doi: 10.1016/j.cps.2018.05.002 [DOI] [PubMed] [Google Scholar]
- 15.Auersvald A, Auersvald LA. Management of the submandibular gland in neck lifts: indications, techniques, pearls, and pitfalls. Clin Plast Surg. 2018;45(4):507–525. doi: 10.1016/j.cps.2018.06.001 [DOI] [PubMed] [Google Scholar]
- 16.Isse N. Endoscopic facial rejuvenation: endoforehead the functional lift-brief update. Aesthetic Plast Surg. 2020;44(4):1171–1172. doi: 10.1007/s00266-020-01774-3 [DOI] [PubMed] [Google Scholar]
- 17.Stevens WG, Apfelberg DB, Stoker DA, Schantz SA. The Endotine: a new biodegradable fixation device for endoscopic forehead lifts. Aesthet Surg J. 2003;23(2):103–107. doi: 10.1067/maj.2003.21 [DOI] [PubMed] [Google Scholar]
- 18.Minelli L, Brown CP, Warren RJ, van der Lei B, Mendelson BC, Little JW. Lifting the anterior midcheek and nasolabial fold: introduction to the melo fat pad anatomy and its role in longevity and recurrence. Aesthet Surg J. 2023;43(9):941–954. doi: 10.1093/asj/sjad126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cruz RS, O'Reilly EB, Rohrich RJ. The platysma window: an anatomically safe, efficient, and easily reproducible approach to neck contour in the face lift. Plast Reconstr Surg. 2012;129(5):1169–1172. doi: 10.1097/PRS.0b013e31824a2d8c [DOI] [PubMed] [Google Scholar]
- 20.Coleman SR. Structural fat grafting. Aesthet Surg J. 1998;18(5):386–388. doi: 10.1016/S1090-820X(98)70098-6 [DOI] [PubMed] [Google Scholar]
- 21.Zeltzer AA, Tonnard PL, Verpaele AM. Sharp-needle intradermal fat grafting (SNIF). Aesthet Surg J. 2012;32(5):554–561. doi: 10.1177/1090820X12445082 [DOI] [PubMed] [Google Scholar]
- 22.Lambros V. Facial aging: a 54-year, three-dimensional population study. Plast Reconstr Surg. 2020;145(4):921–928. doi: 10.1097/PRS.0000000000006711 [DOI] [PubMed] [Google Scholar]
- 23.Rohrich RJ, Durand PD, Dayan E. The lift-and-fill facelift: superficial musculoaponeurotic system manipulation with fat compartment augmentation. Clin Plast Surg. 2019;46(4):515–522. doi: 10.1016/j.cps.2019.06.001 [DOI] [PubMed] [Google Scholar]
- 24.Sinno S, Mehta K, Reavey PL, Simmons C, Stuzin JM. Current trends in facial rejuvenation: an assessment of ASPS members’ use of fat grafting during face lifting. Plast Reconstr Surg. 2015;136(1):20e–30e. doi: 10.1097/PRS.0000000000001329 [DOI] [PubMed] [Google Scholar]
- 25.Marten TJ. High SMAS facelift: combined single flap lifting of the jawline, cheek, and midface. Clin Plast Surg. 2008;35(4):569–603; vi-vii. doi: 10.1016/j.cps.2008.04.002 [DOI] [PubMed] [Google Scholar]
- 26.Lambros V, Stuzin JM. The cross-cheek depression: surgical cause and effect in the development of the “joker line” and its treatment. Plast Reconstr Surg. 2008;122(5):1543–1552. doi: 10.1097/PRS.0b013e31818894d3 [DOI] [PubMed] [Google Scholar]
- 27.Hamra ST. Frequent face lift sequelae: hollow eyes and the lateral sweep: cause and repair. Plast Reconstr Surg. 1998;102(5):1658–1666. doi: 10.1097/00006534-199810000-00052 [DOI] [PubMed] [Google Scholar]
- 28.Baker DC. Lateral SMASectomy. Plast Reconstr Surg. 1997;100(2):509–513. doi: 10.1097/00006534-199708000-00039 [DOI] [PubMed] [Google Scholar]
- 29.Tonnard P, Verpaele A, Monstrey S, et al. Minimal access cranial suspension lift: a modified S-lift. Plast Reconstr Surg. 2002;109(6):2074–2086. doi: 10.1097/00006534-200205000-00046 [DOI] [PubMed] [Google Scholar]
- 30.Jacono AA, Parikh SS. The minimal access deep plane extended vertical facelift. Aesthet Surg J. 2011;31(8):874–890. doi: 10.1177/1090820X11424146 [DOI] [PubMed] [Google Scholar]
- 31.Knize DM. Periauricular face lift incisions and the auricular anchor. Plast Reconstr Surg. 1999;104(5):1508–1520; discussion 1521-3. doi: 10.1097/00006534-199910000-00043 [DOI] [PubMed] [Google Scholar]
- 32.Besins T. The “R.A.R.E.” technique (reverse and repositioning effect): the renaissance of the aging face and neck. Aesthetic Plast Surg. 2004;28(3):127–142. doi: 10.1007/s00266-004-3002-0 [DOI] [PubMed] [Google Scholar]
- 33.Vasconez LO, Core GB, Gamboa-Bobadilla M, Guzman G, Askren C, Yamamoto Y. Endoscopic techniques in coronal brow lifting. Plast Reconstr Surg. 1994;94(6):788–793. doi: 10.1097/00006534-199411000-00006 [DOI] [PubMed] [Google Scholar]
- 34.Saltz R. Endoscopic temporal-incision only midface lift is enhanced by Endotine technique. Aesthet Surg J. 2005;25(1):80–83. doi: 10.1016/j.asj.2004.12.005 [DOI] [PubMed] [Google Scholar]
- 35.Ramirez OM. Endoscopic subperiosteal browlift and facelift. Clin Plast Surg. 1995;22(4):639–660. doi: 10.1016/S0094-1298(20)31166-4 [DOI] [PubMed] [Google Scholar]
- 36.de la Fuente A, Santamaria AB. Endoscopic subcutaneous and SMAS facelift without preauricular scars. Aesthetic Plast Surg. 1999;23(2):119–124. doi: 10.1007/s002669900253 [DOI] [PubMed] [Google Scholar]
- 37.Jacono AA, Rousso JJ. The modern minimally invasive face lift: has it replaced the traditional access approach? Facial Plast Surg Clin North Am. 2013;21(2):171–189. doi: 10.1016/j.fsc.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 38.Auersvald A, Auersvald LA. Hemostatic net in rhytidoplasty: an efficient and safe method for preventing hematoma in 405 consecutive patients. Aesthetic Plast Surg. 2014;38(1):1–9. doi: 10.1007/s00266-013-0202-5 [DOI] [PubMed] [Google Scholar]
- 39.Prado A, Andrades P, Danilla S, Castillo P, Leniz P. A clinical retrospective study comparing two short-scar face lifts: minimal access cranial suspension versus lateral SMASectomy. Plast Reconstr Surg. 2006;117(5):1413–1425; discussion 1426-7. doi: 10.1097/01.prs.0000207402.53411.1e [DOI] [PubMed] [Google Scholar]
- 40.Kamer FM, Parkes ML. The two-stage concept of rhytidectomy. Trans Sect Otolaryngol Am Acad Ophthalmol Otolaryngol. 1975;80(6):546–550. [PubMed] [Google Scholar]
- 41.Matarasso A, Elkwood A, Rankin M, Elkowitz M. National plastic surgery survey: face lift techniques and complications. Plast Reconstr Surg. 2000;106(5):1185–1195; discussion 1196. doi: 10.1097/00006534-200010000-00033 [DOI] [PubMed] [Google Scholar]
- 42.Ramirez OM. Endoscopic assisted facial rejuvenation: a 35 year personal journey. Plast Aesthet Res. 2020;7:25. doi: 10.20517/2347-9264.2019.78 [DOI] [Google Scholar]
- 43.Chiu ES, Baker DC. Endoscopic brow lift: a retrospective review of 628 consecutive cases over 5 years. Plast Reconstr Surg. 2003;112(2):628–633; discussion 634-5. doi: 10.1097/01.PRS.0000071042.11435.2E [DOI] [PubMed] [Google Scholar]
- 44.Biggs TM. Endoscopic brow lift: a retrospective review of 628 consecutive cases over 5 years. Plast Reconstr Surg. 2004;113(7):2219; author reply 2219-20. doi: 10.1097/01.PRS.0000123600.67295.57 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.