Abstract
Despite their importance, little is known about how social drivers of health shape communicative outcomes in autism. Even less is known when considering the intersection of race and language impairment. An understanding of factors in communicative outcomes is key for characterizing developmental trajectories and informing supports. This cross-sectional observational study examined the role of social drivers of health in communicative outcomes of racially and ethnically minoritized autistic adolescents and adults. Participants ages 13 to 30 (N = 73) completed a behavioral assessment protocol, including language and nonverbal cognitive skills, as well as social drivers of health (sense of community, unmet services, barriers to services). Correlational analyses revealed associations between social drivers of health on social communication impairment and real-world communication. Generalized linear mixed-effects modeling revealed that language predicted real-world communication, but sense of community predicted social communication impairment. Findings point to the importance of assessing both individual differences and social drivers of health in outcomes in autism research. Future work should focus on social drivers of health in larger-scale analyses of outcomes in minoritized autistic individuals during the transition to adulthood, considering supports that align with service eligibility and person-centered outcomes.
Keywords: adolescents, adults, autism spectrum disorders, communication and language, environmental factors
Lay Abstract
Where people live, work, and spend their time is important. Environments can have more or less services or differ in how much they help people feel like they belong to their community. These parts of the environment are called social drivers of health. Social drivers of health are important for outcomes in autism, but we do not know much about them in racially and ethnically minoritized autistic teens or adults. We recruited 73 minoritized autistic teens and adults ages 13 to 30 years and 52 caregivers (parents, grandparents, sibling) to our study. Teens and adults did language and NVIQ tests on Zoom. Teens, adults, and caregivers also answered questionnaires. Sense of community was important for social communication impairment, and language was important for real-world communication. These findings tell us two things. First, thinking about how to create supportive communication environments for autistic teens and adults is important. Second, understanding how social drivers of health shape outcomes is important. In the future, we should focus on how improving environments can help minoritized autistic teens and adults meet their communication goals.
Autistic individuals are likely to be put at risk of poor outcomes in adulthood (Mason et al., 2021) and to have structural language impairment (LI) (Boucher, 2012), or difficulties with morphology, syntax, and phonology (Schaeffer et al., 2023). Prior work focuses on the role of individual differences in language and cognitive skills in communicative outcomes of autistic adolescents and adults (Brignell et al., 2018; Lord et al., 2020; Magiati et al., 2014), but little is known about the role of environmental factors (Anderson et al., 2018a). These factors, or social drivers of health, are aspects of where individuals live and spend time that impact myriad life outcomes (Centers for Disease Control and Prevention [CDC], 2021; Commission on Social Determinants of Health, 2008). This information is critical for developing supports and advocacy, especially given intersectional health disparities (Rast et al., 2023; Schott et al., 2022). This study examines the role of social drivers of health in communicative outcomes of racially and ethnically minoritized autistic adolescents and adults (ages 13-30 years) varying in language and cognitive skills. Specifically, we ask if: 1) social drivers of health or communicative outcomes differ by LI status, and 2) social drivers of health predict communicative outcomes.
Communicative Outcomes in Autism
Research to date has documented developmental patterns in communicative outcomes of autistic adults (Anderson et al., 2014; Billstedt et al., 2007; Gillespie-Lynch et al., 2012; Howlin et al., 2013; Levy & Perry, 2011). These outcomes often include real-world communication, or how an individual meets communicative demands in daily life using verbal and written language (Sparrow et al., 2016), and social communication impairment, or challenges with social communication and interaction (Constantino, 2012). While one perspective is to take these outcomes as indicative of social competence (Gillespie-Lynch et al., 2012), this report assumes communicative outcomes are relational, as interactions between autistic individuals and environments shape their experiences with communication (Bronfenbrenner, 1977).
While important, there are critical gaps in the literature. First, many studies measure language and cognitive skills in a way that disallows understanding nuance and do not assess adult language (Howlin & Taylor, 2015). Yet per diagnostic criteria, autism can co-occur with LI and intellectual disability (American Psychiatric Association, 2013), and language and cognitive skills can also dissociate (World Health Organization, 2022). Assessing cognitive skills such that they can dissociate from language skills, such as by using nonverbal intelligence (NVIQ), is important. On one hand, 68 autistic youth (ages 4-14) with communication age equivalents < 4.5 years had verbal IQ (VIQ) that was 13 points lower than NVIQ (61 versus 74; Grondhuis et al., 2018). Concurrent IQ and communicative outcomes also have showed mixed findings, with some samples showing links between VIQ and real-world communication (Lord et al., 2020) and others showing weak to no ties between full-scale IQ (which includes VIQ) and real-world communication (Matthews et al., 2015; Tamm et al., 2022). Relatedly, many studies use too-few measures to make inferences about LI, independent of autism (Calder et al., 2023; Girolamo et al., 2023). For example, using a singular caregiver report item of overall expressive language level as an indicator of language level may be tied to social communication impairment (Bal et al., 2019), but it will not adequately inform precise clinical planning. Conversely, when using independently normed language assessments, LI has differentiated real-world communication skills of autistic and nonautistic adults, but not quality of life or social support networks, which may be tied to social communication (Johnson et al., 2010).
Second, despite increasing attention to environmental factors in outcomes, such as educational programming (Howlin, 2021) and services access (Shattuck et al., 2020), many studies fail to consider social drivers of health, particularly at interpersonal and community levels (Anderson et al., 2018a). For autistic individuals, the extent to which environments are supportive is key (Lai et al., 2020). In adolescence, environmental supports play an important role in social communication and real-world communication (Chen et al., 2023). In post-secondary settings, others may not know how to communicate with autistic adults, leading to poor environmental fit (Billstedt et al., 2010). The environment of communicative outcomes involves responsiveness to access needs (Tobin et al., 2014). This responsiveness can be measured via unmet service needs, barriers to services, and sense of community.
Services access shows racial disparities in autistic youth, yet differences by geographic region indicate that access cannot be reduced to race or ethnicity alone (Liu et al., 2023). Unmet service needs and barriers to services at an individual level, motivating use of person-centered measures (Burke et al., 2023). In the transition to adulthood, all autistic individuals lose access to child- and education-based services (“Every Student Succeeds Act [ESSA],” 2015; “Individuals with Disabilities Education Act [IDEA],” 2004) and have more unmet service needs compared to youth (Anderson et al., 2018b; Laxman et al., 2019; Turcotte et al., 2016). Autistic adolescents may lose access to services and have greater unmet service needs even prior to high school exit (Taylor & Henninger, 2015). Such loss means there is reduced access to opportunities for social interaction and communication (Eilenberg et al., 2019). Post-high school, autistic adults face greater barriers to services (Anderson & Butt, 2018), as well as intersectional disparities in unmet service needs (Schott et al., 2021). Given barriers to services, including access and quality (Ishler et al., 2023), autistic adolescents and adults may face inadequate access to supports for exercising communicative skills (Doherty et al., 2022; Müller & Cannon, 2016).
A third social driver of health is sense of community, or sense of belonging and feeling that individual needs can be met within a community (McMillan & Chavis, 1986). Sense of community is tied to community access and participation, as well as adaptive behavior (Cameron et al., 2022; Mahmoudi Farahani, 2016; Talò et al., 2014; Zidrou et al., 2021). It is also a proxy for sociocultural capital (Pooley et al., 2005) and tends to be lower in marginalized populations, who respond adaptively to contextual constraints (Littman, 2022). For instance, a minoritized autistic young adult may opt to not engage in social interaction out in the community due to concerns of systemic racism and ableism, even though they have the capacity to do so (blinded for review). In this way, sense of community is important for understanding real-world communication and social communication impairment (Tobin et al., 2014). Specifically, the extent to which autistic adolescents and adults experience communicative challenges in an environment or are denied opportunities for communication may impact sense of community (Bolick, 2008; Morrison et al., 2020a, 2020b; Orsmond et al., 2013). At the same time, sense of community is not purely due to race (Cardenas et al., 2021).
Last, many studies fail to consider the intersection of race with disability, amid systematic exclusion of racially and ethnically minoritized individuals from autism research (Maye et al., 2021). A common practice is to compare white to minoritized participants (McCauley et al., 2020), which may document disparities. Yet without careful framing, this comparison perpetuates a monolithic, scientifically flawed narrative of a one-to-one ratio between race and experiences (Plaut, 2010). In reality, disparities in social drivers of health and outcomes arise from structural factors (Braveman & Gottlieb, 2014). For instance, U.S. law segregated racially minoritized students and students with disabilities in education (Turnbull III et al., 2006). Such policy reflected social perceptions about race and disability versus minoritized individuals (Powell, 2012). Hence, while individual differences in autism traits and language clearly exist, race and disability are also social constructs that involve the reactions of others, exacerbate one another, and cause social experiences of marginalization (Annamma et al., 2013). Characterizing social drivers of health and outcomes in minoritized autistic adolescents and adults must be inclusive of race and disability, while focusing on heterogeneity.
The Current Study
This report examines communicative outcomes in racially and ethnically minoritized autistic adolescents and adults within the U.S. Given heterogeneity within minoritized communities (Plaut, 2010), the premise of this paper is that systematic exclusion in research motivates purposeful inclusion of minoritized autistic adolescents and adults to produce broadly applicable findings (Maye et al., 2021; National Institutes of Health, 2021). The focus is on to what extent individual differences, social drivers of health, and communication relate to one another. Specifically, this study had two research questions:
Do participants with and without LI differ in communicative outcomes (real-world communication and social communication impairment) and social drivers of health (sense of community, unmet service needs, and barriers to having service needs met), accounting for NVIQ band?
To what extent do individual differences and social drivers of health predict communicative outcomes?
In contrast to most prior work, this study directly assessed language across linguistic domains, enhancing confidence in determination of LI status and allowing for examination of language as a continuous measure on communicative outcomes. In addition, this study directly assessed NVIQ, which yields scores that are nearly 1 SD higher than verbal IQ in autistic youth with LI (Grondhuis et al., 2018). In using norm-referenced measures of communicative outcomes, language, and NVIQ, this approach also provides information on the contribution of language to communicative outcomes using measures that are immediately interpretable and align with clinical practice patterns for service eligibility in the United States (Burke et al., 2023; Selin et al., 2022). Given the burden of autistic adults to prove a need for services (“Americans with Disabilities Act of 1990,” 2008; “Rehabilitation Act of 1973,” 1973), use of such measures in the evidence base is of clinical and practical relevance. Last, in assessing unmet service needs, barriers to services, and sense of community using person-centered measures, this study provides new information on social drivers of health critical to informing services (Burns et al., 2011).
Method
Participants
Selection criteria were: (a) racially and/or ethnically minoritized per U.S. Census guidelines (Office of Management and Budget, 2024), with the option to select multiple options for race and to write in options; (b) formal clinical diagnosis of autism, per requirements for inclusion in recruitment sources (e.g., community organizations providing services to autistic individuals), and confirmation using the Social Responsiveness Scale-2nd Ed. (SRS-2) (Constantino, 2012) and expert clinical judgment; (c) ages 13 to 30, coinciding with when transition planning begins in some states within the U.S. and 10 years post-federal eligibility for special education services (“ESSA,” 2015; “IDEA,” 2004); (d) proficiency in English per self-report during screening, as assessments were in English; (e) adequate hearing and vision thresholds for responding to audiovisual stimuli on a computer screen, and; (f) use of primarily spoken language to communicate, as study activities required oral responses. Participants could be of any sex assigned at birth and gender, and could self-report options.
This study includes 73 minoritized autistic individuals ages 13 to 30 years (Mage = 19.69); see Table 1. Over one-third of the sample (35.6%) was multiracial, which was not mutually exclusive with other categories nor fully reported in order to protect participant confidentiality and privacy. That said, about half of the sample was Black (52.1%). The female-to-male ratio for both sex at birth and gender was approximately 1:2. Over half the sample was in educational programming (n = 41, or 56.2%), and over one quarter each was in secondary education (n = 21, or 28.8%) or various post-secondary educational programs (n = 20, or 27.4%).
Table 1.
Participant Characteristics (N = 73)
| Variable | ASD (n = 33) | ASD+LI (n = 40) |
|---|---|---|
| Age | 20.38 (5.35), 13.35-30.43 | 19.12 (4.09), 13.27-29.67 |
| Race | ||
| American Indian, Native American, Alaska Native | 24.24% | 10.00% |
| Asian | 33.33% | 20.00% |
| Black | 42.42% | 60.00% |
| multiracial | 6.06% | 30.00% |
| Pacific Islander | 6.06% | 5.00% |
| white | 30.30% | 25.00% |
| other | 12.12% | 12.50% |
| Hispanic/Latine: Yes | 15.15% | 20.00% |
| Sex Assigned at Birth: Female to Male | ||
| Female | 45.45% | 20.00% |
| Male | 54.55% | 80.00% |
| Gender | ||
| Female | 45.45% | 22.50% |
| Male | 54.55% | 77.50% |
| NVIQ | 98.73 (13.77) | 84.03 (15.00) |
| SRS-2 overall t-score | 74.42 (11.95) | 71.15 (10.81) |
| PPVT-5 receptive vocabulary standard score | 105.82 (12.62) | 80.65 (18.91) |
| EVT-3 expressive vocabulary standard score | 107.36 (10.66) | 82.90 (14.43) |
| SRT percent accuracy | 94.44 (5.53) | 87.25 (10.39) |
| CELF-5 Receptive Language Index | 98.88 (10.80) | 68.18 (15.31) |
| CELF-5 Expressive Language Index | 92.45 (10.09) | 64.97 (14.88) |
Note. LI = language impairment. % = percent. All other variables = M (SD). Multiracial non-exclusive with other racial/ethnic categories. ASD other = Latine (n = 4). ASD+LI other = Middle Eastern (n = 1), Latine (n = 3), and Puerto Rican (n = 1). CELF-5 = Clinical Evaluation of Language Fundamentals-5th Ed. (Wiig et al., 2013). PPVT-5 = Peabody Picture Vocabulary Test-5th Ed. (Dunn, 2018). EVT-3 = Expressive Vocabulary Test-3rd Ed. (Williams, 2018). SRT = Syllable Repetition Task (Shriberg et al., 2009). SRS-2 = Social Responsiveness Scale-2nd Ed. (Constantino, 2012).
Procedures
This study received institutional board approval. The research team recruited participants in a multi-step process: (a) sharing flyers with information about the study with organizations serving diverse autistic adolescents and adults, (b) providing personalized consultation about the study to individuals and families about the study by phone, Zoom, or email, (c) obtaining informed consent using a dynamic process, and (d) collecting data. Recruitment and data collection took place from 2022 to 2023 remotely on HIPAA-compliant Zoom. The first author administered a behavioral assessment protocol to participants and caregivers at their convenience using test developer guidance on remote assessment for measures of language and NVIQ (Pearson, 2023). Participants and caregivers completed questionnaires.
Measures
Autism Status
Autism traits were assessed using SRS-2 caregiver and self-report forms for students and adults (Constantino, 2012). Respondents indicate the frequency of 65 items on a four-point scale, yielding an overall t-score. T-scores of ≤ 59 indicate sub-clinical, 60 to 65 mild, 66 to 76 moderate, and >76 high levels of autism traits. Formal diagnosis, SRS-2 t-scores, and expert clinical judgment were triangulated to determine autism status. Overall t-score means of caregiver student forms (n = 37), caregiver adult forms (n = 15), and adult self-report forms (n =21) did not differ (p = .061). Thus, forms were combined into one group.
Language Skills
Participants completed a comprehensive battery of normed assessments across linguistic domains: semantics, morphology, syntax, and phonology (Schaeffer et al., 2023). Expressive language and receptive language were assessed by the Clinical Evaluation Language Fundamentals-5th Ed. (CELF-5) Expressive Language Index and Receptive Language Index (M = 100, SD = 15) (Wiig et al., 2013). For participants over age 21 (n =25), CELF-5 age 21 norms were used per prior studies of adults ages 18 to 49 (Botting, 2020; Clegg et al., 2021; Fidler et al., 2011). Receptive and expressive vocabulary were assessed by the Peabody Picture Vocabulary Test-5th Ed. (PPVT-5) (Dunn, 2019) and Expressive Vocabulary Test-3rd Ed. (EVT-3; M = 100, SD = 15) (Williams, 2019). Phonological working memory was assessed by percent accuracy on the Syllable Repetition Task (SRT), a measure of nonword repetition (M = 92, SD = 5.9 in six-year-old autistic children with FSIQ ≥ 70) (Shriberg et al., 2009; Shriberg & Mabie, 2017). LI was defined as ≤ −1.25 SD on ≥2 measures: CELF-5 Expressive Language Index, CELF-5 Receptive Language Index, PPVT-5 standard, EVT-3 standard score, or SRT overall accuracy. This cutoff aligns with epidemiological criteria for LI in nonautistic U.S.-based youth (Tomblin et al., 1997). While more stringent than the Ottawa study cutoff of −1 SD on a receptive vocabulary measure or omnibus language measure, a −1 SD cutoff may not be as stringent as clinical criteria and may be specific to local norms (e.g., the Ottawa study) (Johnson et al., 1999). To be more conservative and consistent with U.S. study, a −1.25 SD cutoff was used.
NVIQ
Nonverbal general cognitive ability was assessed using the digital long form of the Raven’s Progressive Matrices-2nd Ed. (Raven’s 2; M = 100, SD = 15) (Raven et al., 2018). The Raven’s 2 does not rely on language and is untimed, which enhances accessibility (Grondhuis et al., 2018). NVIQ was classified into bands for group comparisons: <75, 75 to 84, and ≥85. While prior work has used a cutoff as high as 80 on the Raven’s for low NVIQ (Silleresi, 2023), guidelines suggest 70 to 75 on cognitive tests is clinically significant (American Association on Intellectual and Developmental Disabilities, 2024). Note that the Raven’s alone does not convey intellectual disability, which requires comprehensive assessment (Raven et al., 2018).
Social Drivers of Health
Sense of community was measured using the Brief Sense of Community Scale, a validated measure for diverse youth and adults (α = .92) (Cardenas et al., 2021; Lardier Jr et al., 2018; Peterson et al., 2008). Respondents rate eight statements on a five-point scale, with higher scores indicating higher sense of community. Item scores are averaged to provide an overall score (Peterson et al., 2008). Unmet service needs and barriers to services were measured using adapted items from the National Longitudinal Transition Study-2 (NLTS-2) (Newman et al., 2011), per Taylor and Henninger (2015). Respondents were self or caregiver and reported if: a) each of 16 services were received (psychological, speech-language, vocational, aide, medical, occupational, tutor, transportation, social work, assistive technology, respite, reader/interpreter, physical therapy, mobility, audiology, other); b) each service not received is an unmet need; and c) each of 12 items are barriers to having service needs met (cost, location, doctor or specialist does not accept insurance, not available, scheduling conflicts, ineligible, lack of information, transportation, quality, lack of time, language barrier, physical accessibility). Item scores provide counts. Independent sample t-tests revealed non-significant differences by respondent in unmet needs (p = .335) and barriers to services (p = .842). However, sense of community was lower in self- versus caregiver report (2.53 versus 3.27), t(71) = −3.63, p < .001.
Communication Outcomes
Social communication impairment was assessed using SRS-2 social communication impairment t-scores (Constantino, 2012). Group means of caregiver student report, caregiver adult report, and adult self-report forms did not differ (p = .131), so forms were combined into one group. Real-world communication was assessed using the Vineland Adaptive Behavior Scales-3rd Ed. (VABS-3) domain-level form communication standard score (Sparrow et al., 2016). Caregivers indicate the frequency with which their child completes items. Item-level scores provide a standard score (M = 100, SD = 15), with higher scores indicating higher skills.
Analysis
Two trained research assistants independently scored and checked language measures. The first author and research assistants discussed all disagreements until consensus was reached. NVIQ, autism traits, and communication were each auto-scored within their testing platforms. Next, data were checked for missingness. Missing data were: (a) language and NVIQ scores (n = 1; did not complete assessment); (b) SRS-2 scores (n = 2; n = 1 missing form, n = 1 did not complete the SRS-2); and (c) social drivers of health measures (n = 2 did not complete). Missing data were replaced using predictive mean matching with one imputation in SPSS 29 (IBM Corp., 2023; Little & Rubin, 2019). PPVT-5, EVT-3, and SRT scores were z-scored and averaged.
Prior to analysis, data were checked for multicollinearity, linearity, homoscedasticity, and normality. Multicollinearity was assessed using variance inflation factors (VIF), with a cutoff of ≥4 and α of .05 for removing variables from analysis. No VIF was ≥ 4. For the first research question, analysis tested for differences between participants with and without LI in communicative outcomes and social drivers of health using Wald χ2 statistics and covarying NVIQ band. For the second research question, given sample size, Spearman (1904) correlations tested for significant relationships between language, NVIQ, social drivers of health, and communicative outcomes. Interpretation of effect sizes was 0.25 as small, 0.40 as moderate, and 0.65 as large (Gaeta & Brydges, 2020), with significant effects ≥0.25 entered into the model. As communicative outcome variables were not normally distributed, separate generalized linear mixed effects models estimated the extent to which individual differences in language and NVIQ and social drivers of health predicted VABS-3 communication domain standard scores and SRS-2 social communication impairment t-scores. Models were fit with GLMM procedures in SPSS 29 (IBM Corp., 2023), with fixed effects of predictors and by-participant random intercepts. Model fit was assessed using information criteria and likelihood ratio tests.
Community Involvement
This study used a community-based participatory approach (Wallerstein & Duran, 2006), with partners choosing their role and opting to join the team at all study stages. Community partners co-developed the research questions and design, including methods, outcome measures, interpretation of the data, and dissemination (e.g., community-driven workshops). While the research team included diverse individuals with lived, personal, and professional experiences pertaining to autism, team members did not know participants in this study.
Results
Communicative Outcomes by Language Impairment Status, Accounting for NVIQ Band
Over 50% of the sample met criteria for LI; see Table 1. Classifying participants on the basis of LI and NVIQ band resulted in six groups: 1) NVIQ < 75 without LI (n = 1); 2) NVIQ < 75 with LI (n = 10); 3) NVIQ of 75 to 84 without LI (n = 2); 4) NVIQ of 75 to 84 with LI (n = 8); 5) NVIQ ≥ 85 without LI (n = 29); and 6) NVIQ ≥ 85 with LI (n = 22). Fisher’s exact test revealed an association between LI status and NVIQ bands, p = .002, but LI status and NVIQ dissociated in over one-third of participants. Three (4.11%) had NVIQ < 84 but not LI, and 22 (30.14%) had NVIQ ≥ 85 plus LI.
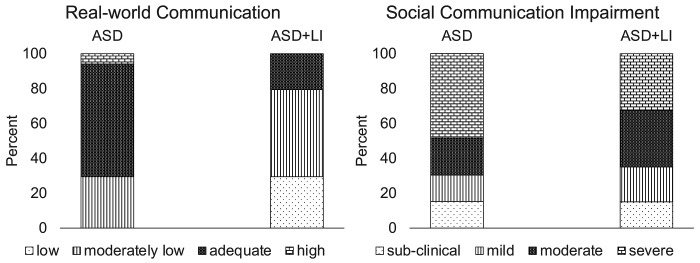
Given NVIQ band, LI status did not significantly differentiate participants in social communication impairment or social drivers of health; see Table 2. However, group estimated marginal means for VABS-3 communication differed in clinical descriptions: adequate for those without LI and moderately low for those with LI (88.15 versus 76.43), but this difference was not significant at the adjusted α of < .01 (p = .014). Descriptively, over two-thirds of participants with LI had low or moderately low communication scores versus roughly one-third of those without LI; see Figure 1. Sample SRS-2 social communication impairment t-scores ranged from 50 to ≥90, with most showing moderate or high levels of autism traits. Group estimated marginal means indicated a moderate level of autism traits (71.1 versus 74.1). Sample unmet service needs (range: 0-14) and barriers to services (range: 0-11) varied, with similar group estimated marginal means for unmet service needs (3.31 versus 3.64) and barriers (5.13 versus 6.01). Sense of community ranged from between strongly disagree and disagree to strongly agree (1.38-5), and group estimated marginal means corresponded to roughly neither agree to disagree (2.90 versus 3.04). In all, there was no one-to-one ratio between levels of language and NVIQ, and LI only differentiated participants in real-world communication skills.
Table 2.
Group Communicative Outcomes and Social Drivers of Health (N = 73)
| Variable | ASD | ASD+LI | Wald χ2 | df | p | ||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| EMM | 95% CI | EMM | 95% CI | ||||
| Unmet service needs | 3.31 | [2.28, 4.82] | 3.64 | [2.72, 4.87] | 0.16 | 1 | .693 |
| Barriers to services | 5.13 | [3.90, 6.74] | 6.01 | [5.01, 7.21] | 1.14 | 1 | .285 |
| Sense of community | 2.9 | [2.54, 3.26] | 3.04 | [2.72, 3.37] | 0.51 | 1 | .473 |
| SRS-2 SCI t-score | 74.1 | [69.34, 79.18] | 71.1 | [67.62, 74.63] | 1.26 | 1 | .261 |
| VABS-3 communication | 88.02 | [79.15, 97.89] | 76.3 | [71, 81.95] | 6.10 | 1 | .014 |
Note. LI = language impairment. EMM = estimated marginal means. Models fit with maximum likelihood estimation and robust covariance. Unmet service needs fit with negative binomial distribution and log link. Barriers to services fit with a Poisson distribution and log link. Sense of community and VABS-3 communication scores fit with Gaussian distribution and identity link. SRS-2 SCI t-scores fit with Tweedie distribution and identity link. Wald χ2 statistics and EMM control for NVIQ of < 75, 75 to 84, and ≥ 85. Data corrected for multiple comparisons using Holm-Bonferroni method (Holm, 1979). Sense of community = Brief Sense of Community Scale overall score (Peterson et al., 2008). Unmet service needs and barriers to services = National Longitudinal Transition Survey-2 items (Newman et al., 2011), per Taylor & Henninger (2015). SRS-2 SCI = Social Responsiveness Scale-2nd Ed. social communication & interaction (Constantino, 2012).
Figure 1.
Communicative outcomes by group. LI = language impairment.
Predictive Effects of Communicative Outcomes
There were significant associations between social drivers of health and communicative outcomes; see Table 3. Higher real-world communication was associated with fewer unmet service needs and barriers, as well as higher language and NVIQ. Lower social communication impairment was associated with fewer unmet service needs and barriers, as well as higher sense of community. Thus, environmental responsiveness to individual needs, as indicated by services, and sociocultural capital, as indicated by sense of community, seemed to be important for communicative outcomes. Communicative outcomes showed small to moderate associations with one another, as did individual differences and social drivers of health, indicating no one-to-one ratio between measures. Higher language was associated with higher NVIQ and fewer unmet service needs. More unmet service needs and barriers were associated with one another and lower sense of community. These patterns signify sense of community, unmet services, and barriers to services as potentially useful predictors for social communication impairment, as well as language, NVIQ, unmet service needs, and barriers to services for real-world communication.
Table 3.
Spearman’s Correlation Coefficients of Social Drivers of Health, Language, NVIQ, and Communicative Outcomes
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Language z-scores | - | ||||||
| 2. NVIQ | .61** | - | |||||
| 3. Unmet service needs | .31** | −.14 | - | ||||
| 4. Barriers to services | −.19 | −.08 | .50** | - | |||
| 5. Sense of community | .03 | .12 | −.43** | −.27* | - | ||
| 6. Social communication impairment | −.04 | −.03 | −.48** | .31** | −.47** | - | |
| 7. Real-world communication | .60** . | .50** | −.41** | −.35* | .23 | −.48** | - |
Note. Language z-scores = average of receptive vocabulary, expressive vocabulary, and nonword repetition. Unmet service needs and barriers to services = National Longitudinal Transition Survey-2 items (Newman et al., 2011), as in Taylor & Henninger (2015). Sense of community = Brief Sense of Community Scale overall score (Peterson et al., 2008). Social communication impairment = Social Responsiveness Scale-2nd Ed. social communication & interaction t-score (Constantino, 2012). Real-world communication = Vineland Adaptive Behavior Scales-3rd Ed. domain-level communication standard score (Sparrow et al., 2016).
= p < .05.
= p < .01.
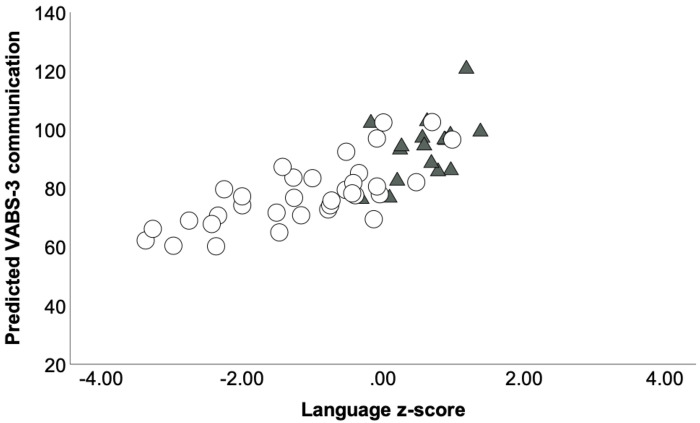
Generalized linear mixed modeling with a normal distribution and identity link function examined to what extent language, NVIQ, unmet services, and barriers to services predicted real-world communication skills; see Table 4. To facilitate interpretation, NVIQ was centered on 100 (Hoffman & Walters, 2022). In the null model, VABS-3 communication scores significantly varied across participants, τ2 = 151.06, z = 2.55, p = .012. The expected score was 83.20, corresponding to moderately low real-world communication skills. When including fixed effects, intercept variance remained significant, τ = 94.38, z = 2.40, p = .016. However, model fit improved, χ2(4) = 30.21, p < .0001. AIC and BIC were smaller, and marginal pseudo-R2 increased to 40.5%, indicating the variance explained for by fixed effects. Given a language z-score of zero, an NVIQ of 100, and no unmet service needs or barriers to services, the expected VABS-3 communication score was 95.08, corresponding to “adequate.” Relative to the intercept and holding all other variables constant, for every unit increase in language z-scores, VABS-3 communication scores were expected to be 5.54 times higher; see Figure 2. Language skills, but not NVIQ, unmet service needs, and barriers to services, predicted real-world communication, while controlling for individual variation.
Table 4.
Model Results of Real-World Communication
| Parameter | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| β | SE | 95% CI | β | SE | 95% CI | |
| Intercept | 83.20** | 2.41 | [78.36, 88.04] | 95.08** | 4.12 | [86.79, 103.37] |
| Language z-scores | 5.44** | 1.67 | [1.94, 8.93] | |||
| NVIQ centered on 100 | .16 | .11 | [−.07, .40] | |||
| Unmet service needs | −.65 | .66 | [−2.00, .71] | |||
| Barriers to services | −.96 | .69 | [−2.34, .43] | |||
| AIC | 435.62 | 405.44 | ||||
| BIC | 439.19 | 408.82 | ||||
| Marginal pseudo-R2 | .000 | .405 | ||||
| Conditional pseudo-R2 | .500 | .702 | ||||
| −2 LL | 431.37 | 401.16 | ||||
| df | 2 | 6 | ||||
| LRT | 30.21 | |||||
Note. Language z-scores = average of receptive vocabulary, expressive vocabulary, and nonword repetition. Unmet service needs and barriers to services = National Longitudinal Transition Survey-2 items (Newman et al., 2011), as in Taylor & Henninger (2015). Models fit with a Gaussian distribution and identity link function, with a random intercept, variance components structure, Satterthwaite approximation, and robust covariance estimation.
= p < .05.
p < .01.
Figure 2.
Observed language z-scores by Vineland Adaptive Behavior Scales-3rd Ed. communication standard scores, predicted from language z-scores, NVIQ, unmet service needs, and barriers to services. Circles = autism plus language impairment. Triangles = autism without language impairment. Language z-scores = average of receptive vocabulary, expressive vocabulary, and nonword repetition accuracy.
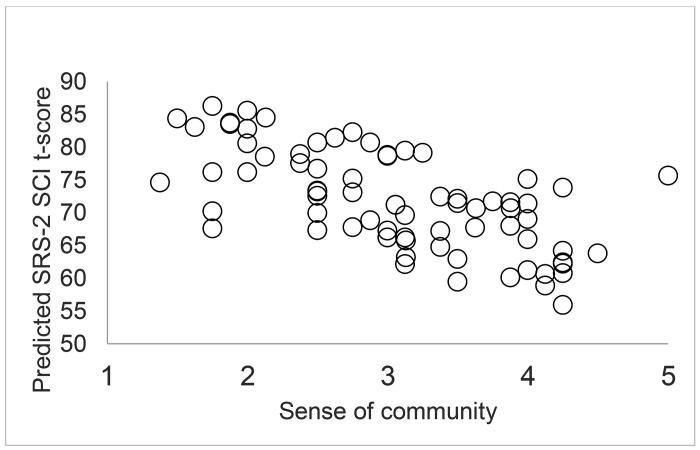
A separate generalized linear mixed model with a normal distribution and identity link function examined the predictive effects of unmet service needs, barriers to services, and sense of community on social communication impairment; see Table 5. In the null model, SRS-2 social communication impairment t-scores significantly varied among participants, τ2 = 61.65, z = 3.04, p = .002. The expected baseline score was 71.88, corresponding to a moderate level of impairment. When including fixed effects, intercept variance remained significant, τ2 = 46.21, z = 2.94, p = .003, but model fit improved, χ2(3) = 26.05, p < .0001. AIC and BIC decreased, and variance explained for by fixed effects increased to 27.3%. For a participant with no unmet service needs or barriers to services, and holding sense of community constant, the expected SRS-2 social communication impairment t-score was 79.50, corresponding to a high level of impairment. Holding all other variables constant, for every one-unit increase in sense of community, SRS-2 social communication impairment t-scores were expected to be 4.18 times lower relative to the intercept; see Figure 3. Given individual variation, sense of community – but not unmet service needs or barriers – predicted lower social communication impairment.
Table 5.
Model Results of Social Communication Impairment
| Parameter | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| β | SE | 95% CI | β | SE | 95% CI | |
| Intercept | 71.88** | 1.29 | [69.30, 74.45] | 79.50** | 5.51 | [68.51, 90.50] |
| Sense of community | −4.18** | 1.50 | [−7.17, −1.19] | |||
| Unmet service needs | .77 | .45 | [−.13, 1.67] | |||
| Barriers to services | .47 | .39 | [−.32, 1.25] | |||
| AIC | 559.45 | 533.40 | ||||
| BIC | 563.83 | 537.69 | ||||
| Marginal pseudo-R2 | .000 | .273 | ||||
| Conditional pseudo-R2 | .500 | .637 | ||||
| −2 LL | 555.27 | 529.22 | ||||
| df | 2 | 5 | ||||
| LRT | 26.05 | |||||
Note. Sense of community = Brief Sense of Community Scale overall score (Peterson et al., 2008). Unmet service needs and barriers to services = National Longitudinal Transition Survey-2 items (Newman et al., 2011), as in Taylor & Henninger (2015). Models fit with a Gaussian distribution and identity link function, with a random intercept, variance components structure, Satterthwaite approximation, and robust covariance estimation.
= p < .05.
p < .01.
Figure 3.
Observed sense of community by Social Responsiveness Scale-2nd Ed. social communication impairment t-score, predicted from sense of community, unmet service needs, and barriers to services.
Discussion
This report is the first step in understanding the experiences and impact of social drivers of health, including sense of community, in minoritized autistic adolescents and adults ranging widely in language and nonverbal cognitive skills. A salient finding is that even when accounting for individual differences in NVIQ, relative structural language levels in terms of LI did not differentiate participants in social drivers of health or social communication impairment. These findings have implications for supporting the transition to adulthood.
Contextualizing Communicative Outcomes
Communicative outcomes reflected individual differences in language and environmental factors. LI did not differentiate participants in real-world communication scores and an adjusted α of < .01. However, group differences were significant at α < .05, and over two twice as many participants without LI had “adequate” communication scores than those with LI. Further, language z-scores predicted an increase in real-world communication scores by 5.44. Whether this effect is clinically significant, though, is unknown. Minimally clinically important differences on the Vineland-II communication range from 2.8 to 5.4 by age and estimation method (Chatham et al., 2018), but concordance with the VABS-3 is limited (Farmer et al., 2020). In contrast, LI did not differentiate participants in social communication impairment, nor did language z-scores predict social communication impairment. These patterns are consistent with prior work in autistic and nonautistic adults with and without LI (Johnson et al., 1999), where real-world communication – but not quality of life or social support networks – differed. As an indicator of language use (Sparrow et al., 2016), effects of language z-scores on real-world communication may reflect interactions between autistic individuals and environments versus individual language skills (Cheang et al., 2024).
This account is consistent with a social-ecological model of factors affecting health (Bronfenbrenner, 1977), as well as with study results. Here, sense of community predicted social communication impairment. Further, though not significant predictors, unmet services and barriers to services were significantly associated with social communication impairment. This finding brings to light the importance of contextualizing the transition to adulthood. Complex experiences of socialization in terms of race and ethnicity influence sense of community (Lardier Jr et al., 2022), as does disability (Bolick, 2008). Given race and disability (Annamma et al., 2018), if minoritized autistic individuals (or families) do not feel like a given space is meant for them, they may have reduced access to environments in which to communicate or pursue communication goals (Lewis & Oyserman, 2016). As effects of other social drivers of health were nonsignificant, sense of community might mediate the relationship between unmet service needs and barriers to services in social communication impairment.
In this sample, there was significant by-participant intercept variance. Though not a primary outcome, such variation may indicate two things. First, consistent with conceptual approaches to diversity (Plaut, 2010), there was no one-to-one correspondence between being racially or ethnically minoritized and experiences. Thus, without theoretical and empirical justification, such as knowledge of culturally bound perceptions about disability and community (Kim et al., 2022), there is not adequate motivation for blanket comparisons of racial and ethnic groups. Second, this variation underlines the importance of precision-based approaches to developing supports. Social drivers of health with known epigenetic influences, such as discrimination, socioeconomic deprivation, and community disinvestment (Martin et al., 2022), are necessary targets for intervention and key to improving outcomes.
Findings have implications for autistic individuals themselves. Though there is growing awareness of the ways in which language and cognitive skills can vary across the autism spectrum (Bal et al., 2016; Butler et al., 2023; Manenti et al., 2024), documenting this heterogeneity is important for advocacy and equity in terms of appreciating multiple facets of profiles versus unilaterally assigning labels on the basis of too little information (Kover & Abbeduto, 2023). In addition, assessing unmet service needs, barriers to services, and sense of community using person-centered measures is critical for evidence-based practice (Burns et al., 2011), as well as for changing the narrative of developmental outcomes in the transition to adulthood. Given findings of self-blame and stigma among autistic adults (Han et al., 2023; Muniandy et al., 2023), documenting the extent to which environmental factors shape experiences and outcomes is important. Consistent with recent calls (Anderson et al., 2018a), results indicate that assessing interpersonal and community social drivers of health in autistic adolescents and adults is conceptually and practically relevant.
Limitations
This study was not without its limitations and had tradeoffs, given its aim to provide new insight on social drivers of health. First, the sample was small and included individuals who used primarily language to communicate (Hughes et al., 2023), limiting the generalizability of findings. In addition, this study utilized different respondents on questionnaires, depending on availability. Although scores only differed on sense of community, this difference is a source of variance. This study also did not comprehensively assess social drivers of health, such as the extent of unmet service needs or barriers to services (Burke et al., 2023) or all domains, such as economic stability or discrimination (CDC, 2021). Similarly, this study did not assess individual differences, such as co-occurring psychiatric diagnoses, or language measures that might reveal greater heterogeneity, such as natural language sampling (Butler et al., 2023). Last, minimally clinically significant differences are unknown for communicative outcomes and social drivers of health (Chatham et al., 2018). Similarly, it is unknown how these communicative outcomes compare to person-centered goals for communication, if any.
Future Directions
Amid growing attention to social drivers of health in outcomes in autism (Schendel et al., 2022), study findings and limitations lay groundwork for future research. While this study examined select social drivers of health, they may differ from the screening items used in routine care settings, such as economic stability or family factors (Sokol et al., 2019). A next step is to understand how social drivers of health of this study compare to measures used in settings where autistic adults access care. Second, future work is needed to merge clinical measures to assess communication with person-centered outcome measures (Choi et al., 2022; Cummins et al., 2020), as well as with outcome measures across other domains to more fully evaluate the role of social drivers of health in communicative outcomes. Third, understanding the desired benefits and outcomes of assessing social drivers of health from multiple perspectives (Mazurek et al., 2021), with the goal of improving environments for autistic adolescents and adults, is important. Autistic adults may face communicative challenges in accessing routine care given inadequate environmental supports or preparation of practitioners to interact with them (Doherty et al., 2022). Integrating information from different relevant parties, from minoritized autistic adolescents and adults to caregivers and healthcare providers, is critical to translate empirical findings into action (Field et al., 2014).
Conclusions
In examining a racially and ethnically minoritized sample of autistic adolescents and adults ranging in language skills and NVIQ, this study documented relationships between social drivers of health and communicative outcomes. Effects of language on real-world communication and of sense of community on social communication impairment provide evidence for communicative outcomes as arising from interactions of individual with environment. These findings should inform characterization of developmental trajectories by placing emphasis on the fundamental role of sense of community in social communication impairment. In turn, findings should inform development of supports by adopting a holistic approach to clinical assessment and planning.
Acknowledgements:
TG was supported by an American Speech-Language-Hearing Foundation New Investigators Research Grant (PI: Girolamo) and NIDCD T32 DC001703 (PI: Eigsti).
Footnotes
Conflicting Interests Statement: The authors have no conflicts of interest.
References
- American Association on Intellectual and Developmental Disabilities. (2024). Defining criteria for intellectual disability. Author. Retrieved June 2 from https://www.aaidd.org/intellectual-disability/definition [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. [Google Scholar]
- Americans with Disabilities Act of 1990, §§ 12101 et seq. U.S.C. (2008). https://www.ada.gov/pubs/adastatute08.htm
- Anderson C., & Butt C. (2018). Young adults on the autism spectrum: The struggle for appropriate services. Journal of Autism and Developmental Disorders, 48(11), 3912–3925. 10.1007/s10803-018-3673-z [DOI] [PubMed] [Google Scholar]
- Anderson D. K., Liang J. W., & Lord C. (2014). Predicting young adult outcome among more and less cognitively able individuals with autism spectrum disorders. Journal of Child Psychology and Psychiatry, 55(5), 485–494. 10.1111/jcpp.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson K. A., Roux A. M., Kuo A., & Shattuck P. T. (2018a). Social-ecological correlates in adult autism outcome studies: A scoping review. Pediatrics, 141(Supplement 4), S306–S317. 10.1542/peds.2016-4300H [DOI] [PubMed] [Google Scholar]
- Anderson K. A., Sosnowy C., Kuo A. A., & Shattuck P. T. (2018b). Transition of individuals with autism to adulthood: A review of qualitative studies. Pediatrics, 141(Supplement 4), S318–S327. 10.1542/peds.2016-4300I [DOI] [PubMed] [Google Scholar]
- Annamma S. A., Connor D., & Ferri B. (2013). Dis/ability critical race studies (DisCrit): Theorizing at the intersections of race and dis/ability. Race Ethnicity and Education, 16(1), 1–31. 10.1080/13613324.2012.730511 [DOI] [Google Scholar]
- Annamma S. A., Ferri B. A., & Connor D. J. (2018). Disability critical race theory: Exploring the intersectional lineage, emergence, and potential futures of DisCrit in education. Review of Research in Education, 42(1), 46–71. 10.3102/0091732X18759041 [DOI] [Google Scholar]
- Bal V. H., Katz T., Bishop S. L., & Krasileva K. (2016). Understanding definitions of minimally verbal across instruments: Evidence for subgroups within minimally verbal children and adolescents with autism spectrum disorder. Journal of Child Psychology and Psychiatry, 57(12), 1424–1433. 10.1111/jcpp.12609 [DOI] [PubMed] [Google Scholar]
- Bal V. H., Kim S.-H., Fok M., & Lord C. (2019). Autism spectrum disorder symptoms from ages 2 to 19 years: Implications for diagnosing adolescents and young adults. Autism Research, 12(1), 89–99. 10.1002/aur.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billstedt E., Carina Gillberg I., & Gillberg C. (2007). Autism in adults: symptom patterns and early childhood predictors. Use of the DISCO in a community sample followed from childhood. Journal of Child Psychology and Psychiatry, 48(11), 1102–1110. 10.1111/j.1469-7610.2007.01774.x [DOI] [PubMed] [Google Scholar]
- Billstedt E., Gillberg I. C., & Gillberg C. (2010). Aspects of quality of life in adults diagnosed with autism in childhood: A population-based study. Autism, 1362361309346066. 10.1177/1362361309346066 [DOI] [PubMed] [Google Scholar]
- Bolick T. (2008). “It takes a community”: Social capital, autism spectrum disorders, and the real world. Topics in Language Disorders, 28(4). 10.1097/01.TLD.0000341130.39275.fa [DOI] [Google Scholar]
- Botting N. (2020). Language, literacy and cognitive skills of young adults with developmental language disorder (DLD). International Journal of Language & Communication Disorders, 55(2), 255–265. 10.1111/1460-6984.12518 [DOI] [PubMed] [Google Scholar]
- Boucher J. (2012). Research review: structural language in autistic spectrum disorder–characteristics and causes. Journal of Child Psychology and Psychiatry, 53(3), 219–233. [DOI] [PubMed] [Google Scholar]
- Braveman P., & Gottlieb L. (2014). The social determinants of health: it’s time to consider the causes of the causes. Public Health Reports, 129(Supplement 2), 19–31. 10.1177/00333549141291s206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brignell A., Morgan A. T., Woolfenden S., Klopper F., May T., Sarkozy V., & Williams K. (2018). A systematic review and meta-analysis of the prognosis of language outcomes for individuals with autism spectrum disorder. Autism & Developmental Language Impairments, 3, 2396941518767610. 10.1177/2396941518767610 [DOI] [Google Scholar]
- Bronfenbrenner U. (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513–531. 10.1037/0003-066X.32.7.513 [DOI] [Google Scholar]
- Burke M. M., Cheung W. C., Best M., DaWalt L. S., & Taylor J. L. (2024). Measuring what matters: Considerations for the measurement of services for individuals with autism. Journal of Developmental and Physical Disabilities, 36, 423–439. 10.1007/s10882-023-09916-6 [DOI] [Google Scholar]
- Burns P. B., Rohrich R. J., & Chung K. C. (2011). The levels of evidence and their role in evidence-based medicine. Plastic and Reconstructive Surgery, 128(1), 305–310. 10.1097/PRS.0b013e318219c171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler L. K., Shen L., Chenausky K. V., La Valle C., Schwartz S., & Tager-Flusberg H. (2023). Lexical and morphosyntactic profiles of autistic youth with minimal or low spoken language skills. American Journal of Speech-Language Pathology, 32(2), 733–747. 10.1044/2022_AJSLP-22-00098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calder S. D., Brennan-Jones C. G., Robinson M., Whitehouse A., & Hill E. (2023). How we measure language skills of children at scale: A call to move beyond domain-specific tests as a proxy for language. International Journal of Speech-Language Pathology, 25(3), 440–448. 10.1080/17549507.2023.2171488 [DOI] [PubMed] [Google Scholar]
- Cameron L. A., Borland R. L., Tonge B. J., & Gray K. M. (2022). Community participation in adults with autism: A systematic review. Journal of Applied Research in Intellectual Disabilities, 35(2), 421–447. 10.1111/jar.12970 [DOI] [PubMed] [Google Scholar]
- Cardenas I., Steiner J. J., & Peterson N. A. (2021). Measurement invariance of the Brief Sense of Community Scale across non-Hispanic, Black and Hispanic college students. Journal of Community Psychology, 49(6), 2106–2121. 10.1002/jcop.22640 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2021). Social determinants of health: Know what affects health. Retrieved March 5, from https://www.cdc.gov/socialdeterminants/index.htm
- Chatham C., Taylor K., Charman T., Liogier D’Ardhuy X., Eule E., Fedele A., Hardan A., Loth E., Murtagh L., & del Valle Rubido M. (2018). Adaptive behavior in autism: Minimal clinically important differences on the Vineland II. Autism Research, 11(2), 270–283. 10.1002/aur.1874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheang R. T., Skjevling M., Blakemore A. I., Kumari V., & Puzzo I. (2024). Do you feel me? Autism, empathic accuracy and the double empathy problem. Autism, 13623613241252320. 10.1177/13623613241252320 [DOI] [PubMed] [Google Scholar]
- Chen Y.-J., Duku E., Zaidman-Zait A., Szatmari P., Smith I. M., Ungar W. J., Zwaigenbaum L., Vaillancourt T., Kerns C., Bennett T., Elsabbagh M., Thompson A., & Georgiades S. (2023). Variable patterns of daily activity participation across settings in autistic youth: A latent profile transition analysis. Autism, 27(8), 2241–2255. 10.1177/13623613231154729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K. R., Lotfizadah A. D., Bhakta B., Pompa-Craven P., & Coleman K. J. (2022). Concordance between patient-centered and adaptive behavior outcome measures after applied behavior analysis for autism. BMC Pediatrics, 22(1), 314. 10.1186/s12887-022-03383-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clegg J., Crawford E., Spencer S., & Matthews D. (2021). Developmental Language Disorder (DLD) in young people leaving care in England: A study profiling the language, literacy and communication abilities of young people transitioning from care to independence. International Journal of Environmental Research and Public Health, 18(8), 4107. 10.3390/ijerph18084107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commission on Social Determinants of Health. (2008). Closing the gap in a generation: health equity through action on the social determinants of health: final report of the commission on social determinants of health (9241563702). World Health Organization. [Google Scholar]
- Constantino J. N. (2012). Social Responsiveness Scale, Second Edition. Western Psychological Services. [Google Scholar]
- Cummins C., Pellicano E., & Crane L. (2020). Autistic adults’ views of their communication skills and needs. International Journal of Language & Communication Disorders, 55(5), 678–689. 10.1111/1460-6984.12552 [DOI] [PubMed] [Google Scholar]
- Doherty M., Neilson S., O’Sullivan J., Carravallah L., Johnson M., Cullen W., & Shaw S. C. K. (2022). Barriers to healthcare and self-reported adverse outcomes for autistic adults: a cross-sectional study. BMJ Open, 12(2), e056904. 10.1136/bmjopen-2021-056904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn D. M. (2019). Peabody Picture Vocabulary Test, Fifth Edition: Manual. Pearson. [Google Scholar]
- Eilenberg J. S., Paff M., Harrison A. J., & Long K. A. (2019). Disparities based on race, ethnicity, and socioeconomic status over the transition to adulthood among adolescents and young adults on the autism spectrum: A systematic review. Current Psychiatry Reports, 21(5), 32. 10.1007/s11920-019-1016-1 [DOI] [PubMed] [Google Scholar]
- Every Student Succeeds Act, Pub. L. No. 114-95, § 1001-1605 (2015). [Google Scholar]
- Farmer C., Adedipe D., Bal V. H., Chlebowski C., & Thurm A. (2020). Concordance of the Vineland Adaptive Behavior Scales, second and third editions. Journal of Intellectual Disability Research, 64(1), 18–26. 10.1111/jir.12691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidler L. J., Plante E., & Vance R. (2011). Identification of adults with developmental language impairments. American Journal of Speech-Language Pathology 20(1), 2–13. 10.1044/1058-0360(2010/09-0096) [DOI] [PubMed] [Google Scholar]
- Field B., Booth A., Ilott I., & Gerrish K. (2014). Using the Knowledge to Action Framework in practice: A citation analysis and systematic review. Implementation Science, 9(1), 172. 10.1186/s13012-014-0172-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaeta L., & Brydges C. R. (2020). An examination of effect sizes and statistical power in speech, language, and hearing research. Journal of Speech, Language, and Hearing Research, 63(5), 1572–1580. 10.1044/2020JSLHR-19-00299 [DOI] [PubMed] [Google Scholar]
- Gillespie-Lynch K., Sepeta L., Wang Y., Marshall S., Gomez L., Sigman M., & Hutman T. (2012). Early childhood predictors of the social competence of adults with autism. Journal of Autism and Developmental Disorders, 42(2), 161–174. 10.1007/s10803-011-1222-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girolamo T., Shen L., Monroe Gulick A., Rice M. L., & Eigsti I. M. (2023). Studies assessing domains pertaining to structural language in autism vary in reporting practices and approaches to assessment: A systematic review. Autism, 13623613231216155. 10.1177/13623613231216155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grondhuis S. N., Lecavalier L., Arnold L. E., Handen B. L., Scahill L., McDougle C. J., & Aman M. G. (2018). Differences in verbal and nonverbal IQ test scores in children with autism spectrum disorder. Research in Autism Spectrum Disorders, 49, 47–55. 10.1016/j.rasd.2018.02.001 [DOI] [Google Scholar]
- Han E., Scior K., Heath E., Umagami K., & Crane L. (2023). Development of stigma-related support for autistic adults: Insights from the autism community. Autism, 27(6), 1676–1689. 10.1177/13623613221143590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman L., & Walters R. W. (2022). Catching up on multilevel modeling. Annual review of psychology, 73, 659–689. 10.1146/annurev-psych-020821-103525 [DOI] [PubMed] [Google Scholar]
- Howlin P. (2021). Adults with autism: Changes in understanding since DSM-111. Journal of Autism and Developmental Disorders, 51(12), 4291–4308. 10.1007/s10803-020-04847-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P., Moss P., Savage S., & Rutter M. (2013). Social outcomes in mid-to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. Journal of the American Academy of Child & Adolescent Psychiatry, 52(6), 572–581.e571. [DOI] [PubMed] [Google Scholar]
- Howlin P., & Taylor J. L. (2015). Addressing the need for high quality research on autism in adulthood. Autism, 19(7), 771–773. [DOI] [PubMed] [Google Scholar]
- Hughes M. M., Shaw K. A., DiRienzo M., Durkin M. S., Esler A., Hall-Lande J., Wiggins L., Zahorodny W., Singer A., & Maenner M. J. (2023). The prevalence and characteristics of children with profound autism, 15 sites, United States, 2000-2016. Public Health Reports, 138(6), 971–980. 10.1177/00333549231163551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. (2023). IBM SPSS Statistics for Macintosh. In (Version 29.0.2.0) IBM Corp. [Google Scholar]
- Individuals with Disabilities Education Act, U.S.C. § 1400 (2004). [Google Scholar]
- Ishler K. J., Berg K. A., Olgac T., Obeid R., & Biegel D. E. (2023). Barriers to service and unmet need among autistic adolescents and young adults. Autism, 27(7), 1997–2010. 10.1177/13623613221150569 [DOI] [PubMed] [Google Scholar]
- Johnson C. J., Beitchman J. H., & Brownlie E. (2010). Twenty-year follow-up of children with and without speech-language impairments: Family, educational, occupational, and quality of life outcomes. American Journal of Speech-Language Pathology, 19(1), 51–65. 10.1044/1058-0360(2009/08-0083) [DOI] [PubMed] [Google Scholar]
- Johnson C. J., Beitchman J. H., Young A., Escobar M., Atkinson L., Wilson B., Brownlie E. B., Douglas L., Taback N., & Lam I. (1999). Fourteen-year follow-up of children with and without speech/language impairments: Speech/language stability and outcomes. Journal of Speech, Language, and Hearing Research, 42(3), 744–760. 10.1044/jslhr.4203.744 [DOI] [PubMed] [Google Scholar]
- Kim S. Y., Cheon J. E., Gillespie-Lynch K., & Kim Y.-H. (2022). Is autism stigma higher in South Korea than the United States? Examining cultural tightness, intergroup bias, and concerns about heredity as contributors to heightened autism stigma. Autism, 26(2), 460–472. 10.1177/13623613211029520 [DOI] [PubMed] [Google Scholar]
- Kover S. T., & Abbeduto L. (2023). Toward equity in research on intellectual and developmental disabilities. American Journal on Intellectual and Developmental Disabilities, 128(5), 350–370. 10.1352/1944-7558-128.5.350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai M.-C., Anagnostou E., Wiznitzer M., Allison C., & Baron-Cohen S. (2020). Evidence-based support for autistic people across the lifespan: Maximising potential, minimising barriers, and optimising the person–environment fit. The Lancet Neurology, 19(5), 434–451. 10.1016/S1474-4422(20)30034-X [DOI] [PubMed] [Google Scholar]
- Lardier D. T. Jr, Opara I., Cantu I., Garcia-Reid P., & Reid R. J. (2022). The brief sense of community scale: Testing dimensionality and measurement invariance by gender among Hispanic/Latinx youth. Journal of Community Psychology, 50(1), 409–425. 10.1002/jcop.22585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lardier D. T. Jr, Reid R. J., & Garcia-Reid P. (2018). Validation of the Brief Sense of Community Scale among youth of color from an underserved urban community. Journal of Community Psychology, 46(8), 1062–1074. 10.1002/jcop.22091 [DOI] [PubMed] [Google Scholar]
- Laxman D. J., Taylor J. L., DaWalt L. S., Greenberg J. S., & Mailick M. R. (2019). Loss in services precedes high school exit for teens with autism spectrum disorder: A longitudinal study. Autism Research, 12(6), 911–921. 10.1002/aur.2113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy A., & Perry A. (2011). Outcomes in adolescents and adults with autism: A review of the literature. Research in Autism Spectrum Disorders, 5(4), 1271–1282. 10.1016/j.rasd.2011.01.023 [DOI] [Google Scholar]
- Lewis N. A., & Oyserman D. (2016). Using identity-based motivation to improve the nation–s health without breaking the bank. Behavioral Science & Policy, 2(2), 24–38. 10.1353/bsp.2016.0013 [DOI] [Google Scholar]
- Little R. J., & Rubin D. B. (2019). Statistical analysis with missing data (Vol. 793). John Wiley & Sons. [Google Scholar]
- Littman D. M. (2022). Third places, social capital, and sense of community as mechanisms of adaptive responding for young people who experience social marginalization. American Journal of Community Psychology, 69(3-4), 436–450. 10.1002/ajcp.12531 [DOI] [PubMed] [Google Scholar]
- Liu B. M., Paskov K., Kent J., McNealis M., Sutaria S., Dods O., Harjadi C., Stockham N., Ostrovsky A., & Wall D. P. (2023). Racial and ethnic disparities in geographic access to autism resources across the US. JAMA Network Open, 6(1), e2251182. 10.1001/jamanetworkopen.2022.51182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C., McCauley J. B., Pepa L. A., Huerta M., & Pickles A. (2020). Work, living, and the pursuit of happiness: Vocational and psychosocial outcomes for young adults with autism. Autism, 24(7), 1691–1703. 10.1177/1362361320919246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magiati I., Tay X. W., & Howlin P. (2014). Cognitive, language, social and behavioural outcomes in adults with autism spectrum disorders: A systematic review of longitudinal follow-up studies in adulthood. Clinical Psychology Review, 34(1), 73–86. 10.1016/j.cpr.2013.11.002 [DOI] [PubMed] [Google Scholar]
- Mahmoudi Farahani L. (2016). The value of the sense of community and neighbouring. Housing, Theory and Society, 33(3), 357–376. 10.1080/14036096.2016.1155480 [DOI] [Google Scholar]
- Manenti M., Ferré S., Tuller L., Houy-Durand E., Bonnet-Brilhault F., & Prevost P. (2024). Profiles of structural language and nonverbal intellectual abilities in verbal autistic adults. Research in Autism Spectrum Disorders, 114, 102361. 10.1016/j.lingua.2023.103598 [DOI] [Google Scholar]
- Martin C. L., Ghastine L., Lodge E. K., Dhingra R., & Ward-Caviness C. K. (2022). Understanding health inequalities through the lens of social epigenetics. Annual Review of Public Health, 43, 235–254. 10.1146/annurev-publhealth-052020-105613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason D., Capp S. J., Stewart G. R., Kempton M. J., Glaser K., Howlin P., & Happé F. (2021). A meta-analysis of outcome studies of autistic adults: Quantifying effect size, quality, and meta-regression. Journal of Autism and Developmental Disorders, 51, 3165–3179. 10.1007/s10803-020-04763-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews N. L., Smith C. J., Pollard E., Ober-Reynolds S., Kirwan J., & Malligo A. (2015). Adaptive functioning in autism spectrum disorder during the transition to adulthood. Journal of Autism and Developmental Disorders, 45(8), 2349–2360. 10.1007/s10803-015-2400-2 [DOI] [PubMed] [Google Scholar]
- Maye M., Boyd B. A., Martínez-Pedraza F., Halladay A., Thurm A., & Mandell D. S. (2021). Biases, barriers, and possible solutions: Steps towards addressing autism researchers under-engagement with racially, ethnically, and socioeconomically diverse communities. Journal of Autism and Developmental Disorders, 1–6. 10.1007/s10803-021-05250-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurek M. O., Sadikova E., Cheak-Zamora N., Hardin A., Huerta I., Sohl K., & Malow B. A. (2021). They deserve the “same level of care that any other person deserves”: Caregiver perspectives on healthcare for adults on the autism spectrum. Research in Autism Spectrum Disorders, 89, 101862. 10.1016/j.rasd.2021.101862 [DOI] [Google Scholar]
- McCauley J. B., Pickles A., Huerta M., & Lord C. (2020). Defining positive outcomes in more and less cognitively able autistic adults. Autism Research, 13(9), 1548–1560. 10.1002/aur.2359 [DOI] [PubMed] [Google Scholar]
- McMillan D. W., & Chavis D. M. (1986). Sense of community: A definition and theory. Journal of Community Psychology, 14(1), 6–23. [DOI] [Google Scholar]
- Morrison K. E., DeBrabander K. M., Jones D. R., Ackerman R. A., & Sasson N. J. (2020a). Social cognition, social skill, and social motivation minimally predict social interaction outcomes for autistic and non-autistic adults. Frontiers in Psychology, 11, 591100. 10.3389/fpsyg.2020.591100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison K. E., DeBrabander K. M., Jones D. R., Faso D. J., Ackerman R. A., & Sasson N. J. (2020b). Outcomes of real-world social interaction for autistic adults paired with autistic compared to typically developing partners. Autism, 24(5), 1067–1080. 10.1177/1362361319892701 [DOI] [PubMed] [Google Scholar]
- Müller E., & Cannon L. (2016). Parent perspectives on outcomes and satisfaction levels of young adults with autism and cognitive impairments. Focus on Autism and Other Developmental Disabilities, 31(2), 92–103. 10.1177/1088357614528800 [DOI] [Google Scholar]
- Muniandy M., Richdale A. L., Arnold S. R. C., Trollor J. N., & Lawson L. P. (2023). Brief report: Longitudinal role of coping strategies on mental health outcomes in autistic youth and adults. Journal of Autism and Developmental Disorders. 10.1007/s10803-023-05953-4 [DOI] [PubMed] [Google Scholar]
- National Institutes of Health. (2021). NIH-wide strategic plan for fiscal years 2021–2025. https://www.nih.gov/sites/default/files/about-nih/strategic-plan-fy2021-2025-508.pdf
- Newman L., Wagner M., Knokey A. M., Marder C., Nagle K., Shaver D., Wei X., Cameto R., Contreras E., Ferguson K., Greene S., & Schwarting M. (2011). The post-high school outcomes of young adults with disabilities up to 8 years after high school: A report from the National Longitudinal Transition Study-2 (NLTS2) SRI International. https://ies.ed.gov/ncser/pubs/20113005/pdf/20113005.pdf [Google Scholar]
- Office of Management and Budget. (2024). Revisions fo OMB’s Statistical Policy Directive No. 15: Standards for Maintaining, Collecting, and Presenting Federal Data on Race and Ethnicity,. (89 FR 22182). Federal Register Notice: Office of Information and Regulatory Affairs, Office of Management and Budget, Executive Office of the President, Retrieved from https://obamawhitehouse.archives.gov/omb/fedreg_1997standards [Google Scholar]
- Orsmond G. I., Shattuck P. T., Cooper B. P., Sterzing P. R., & Anderson K. A. (2013). Social participation among young adults with an autism spectrum disorder. Journal of Autism and Developmental Disorders, 43, 2710–2719. 10.1007/s10803-013-1833-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson. (2023). Staying connected through telepractice. Author. Retrieved April 3 from https://www.pearsonassessments.com/professional-assessments/digital-solutions/telepractice/about.html [Google Scholar]
- Peterson N. A., Speer P. W., & McMillan D. W. (2008). Validation of a brief sense of community scale: Confirmation of the principal theory of sense of community. Journal of Community Psychology, 36(1), 61–73. 10.1002/jcop.20217 [DOI] [Google Scholar]
- Plaut V. C. (2010). Diversity science: Why and how difference makes a difference. Psychological Inquiry, 21(2), 77–99. 10.1080/10478401003676501 [DOI] [Google Scholar]
- Pooley J. A., Cohen L., & Pike L. T. (2005). Can sense of community inform social capital? The Social Science Journal, 42(1), 71–79. 10.1016/j.soscij.2004.11.006 [DOI] [Google Scholar]
- Powell J. A. (2012). Racing to justice: Transforming our conceptions of self and other to build an inclusive society. Indiana University Press. [Google Scholar]
- Rast J. E., Fernandes S. J., Schott W., & Shea L. L. (2023). Disparities by race and ethnicity in inpatient hospitalizations among autistic adults. Journal of Autism and Developmental Disorders. 10.1007/s10803-023-05911-0 [DOI] [PubMed] [Google Scholar]
- Raven J., Rust J., Chan F., & Zhou X. (2018). Raven’s 2 Progressive Matrices, Clinical Edition. Pearson. [Google Scholar]
- Rehabilitation Act of 1973, §§ 790 et seq. U.S.C. § 504 (1973). [Google Scholar]
- Schaeffer J., Abd El-Raziq M., Castroviejo E., Durrleman S., Ferré S., Grama I., Hendriks P., Kissine M., Manenti M., Marinis T., Meir N., Novogrodsky R., Perovic A., Panzeri F., Silleresi S., Sukenik N., Vicente A., Zebib R., Prevost P., & Tuller L. (2023). Language in autism: Domains, profiles and co-occurring conditions. Journal of Neural Transmission, 130(3), 433–457. 10.1007/s00702-023-02592-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schendel D., Roux A. M., McGhee Hassrick E., Lyall K., Shea L., Vivanti G., Wieckowski A. T., Newschaffer C., & Robins D. L. (2022). Applying a public health approach to autism research: A framework for action. Autism Research, 15(4), 592–601. 10.1002/aur.2689 [DOI] [PubMed] [Google Scholar]
- Schott W., Nonnemacher S., & Shea L. (2021). Service use and unmet needs among adults with autism awaiting home- and community-based Medicaid services. Journal of Autism and Developmental Disorders, 51(4), 1188–1200. 10.1007/s10803-020-04593-2 [DOI] [PubMed] [Google Scholar]
- Schott W., Tao S., & Shea L. (2022). Co-occurring conditions and racial-ethnic disparities: Medicaid enrolled adults on the autism spectrum. Autism Research, 15(1), 70–85. 10.1002/aur.2644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selin C. M., Rice M. L., Girolamo T. M., & Wang C. J. (2022). Work setting effects on speech-language pathology practice: Implications for Identification of children with specific language impairment. American Journal of Speech-Language Pathology, 31(2), 854–880. 10.1044/2021_AJSLP-21-00024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck P. T., Garfield T., Roux A. M., Rast J. E., Anderson K., Hassrick E. M., & Kuo A. (2020). Services for adults with autism spectrum disorder: A systems perspective. Current Psychiatry Reports, 22(3), 13. 10.1007/s11920-020-1136-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg L. D., Lohmeier H. L., Campbell T. F., Dollaghan C. A., Green J. R., & Moore C. A. (2009). A nonword repetition task for speakers with misarticulations: The Syllable Repetition Task (SRT). Journal of Speech, Language & Hearing Research,, 52(5), 1189–1212. 10.1044/1092-4388(2009/08-0047) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg L. D., & Mabie H. L. (2017). Speech and motor speech assessment findings in eight complex neurodevelopmental disorders (24). www.waisman.wisc.edu/phonology/techreports/TREP24.PDF
- Silleresi S. (2023). Intelligence profiles in autism spectrum disorder. In Developmental profiles in autism spectrum disorder: Theoretical and methodological implications (pp. 127–157). John Benjamins. 10.1075/lald.68 [DOI] [Google Scholar]
- Sokol R., Austin A., Chandler C., Byrum E., Bousquette J., Lancaster C., Doss G., Dotson A., Urbaeva V., & Singichetti B. (2019). Screening children for social determinants of health: A systematic review. Pediatrics, 144(4), e20191622. 10.1542/peds.2019-1622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow S. S., Cicchetti D. V., & Saulnier C. A. (2016). Vineland Adaptive Behavior Scales-Third Ed. Pearson. [Google Scholar]
- Spearman C. (1904). The proof and measurement of association between two things. The American Journal of Psychology, 15(1), 72–101. [PubMed] [Google Scholar]
- Taló C., Mannarini T., & Rochira A. (2014). Sense of community and community participation: A meta-analytic review. Social Indicators Research, 117(1), 1–28. 10.1007/s11205-013-0347-2 [DOI] [Google Scholar]
- Tamm L., Day H. A., & Duncan A. (2022). Comparison of adaptive functioning measures in adolescents with autism spectrum disorder wiithout intellectual disability. Journal of Autism and Developmental Disorders, 52(3), 1247–1256. 10.1007/s10803-021-05013-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J. L., & Henninger N. A. (2015). Frequency and correlates of service access among youth with autism transitioning to adulthood. Journal of Autism and Developmental Disorders, 45(1), 179–191. 10.1007/s10803-014-2203-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin M. C., Drager K. D. R., & Richardson L. F. (2014). A systematic review of social participation for adults with autism spectrum disorders: Support, social functioning, and quality of life. Research in Autism Spectrum Disorders, 8(3), 214–229. 10.1016/j.rasd.2013.12.002 [DOI] [Google Scholar]
- Tomblin J. B., Records N. L., Buckwalter P., Zhang X., Smith E., & O’Brien M. (1997). Prevalence of specific language impairment in kindergarten children. Journal of Speech, Language, and Hearing Research, 40(6), 1245–1260. 10.1044/jslhr.4006.1245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turcotte P., Mathew M., Shea L. L., Brusilovskiy E., & Nonnemacher S. L. (2016). Service needs across the lifespan for individuals with autism. Journal of Autism and Developmental Disorders, 46(7), 2480–2489. 10.1007/s10803-016-2787-4 [DOI] [PubMed] [Google Scholar]
- Turnbull H. R. III, Turnbull A. P., Stowe M., & Huerta N. (2006). Free appropriate public education: The law and children with disabilities (75h ed.). Love Publishing Company. [Google Scholar]
- Wallerstein N. B., & Duran B. (2006). Using community-based participatory research to address health disparities. Health Promotion Practice, 7(3), 312–323. 10.1177/1524839906289376 [DOI] [PubMed] [Google Scholar]
- Wiig E. H., Semel E., & Secord W. (2013). Clinical Evaluation of Language Fundamentals-5th Ed. [Google Scholar]
- Williams K. T. (2019). Expressive Vocabulary Test-Third Edition: Manual. Pearson. [Google Scholar]
- World Health Organization. (2022). International Classification of Diseases (ICD)-11. https://icd.who.int/en [Google Scholar]
- Zidrou C., Kleisiaris C., & Adamakidou T. (2021). Associations between disability in activities of daily living and social capital aspects among older adults: A scoping review. Journal of Frailty, Sarcopenia & Falls,, 6(3), 119–130. 10.22540/jfsf-06-119 [DOI] [PMC free article] [PubMed] [Google Scholar]