Summary:
Incorporation of new technologies to assist the liposuction procedure is becoming increasingly common. These technologies allow for a softer technique, balanced shaping, elimination of excess adipose tissue, and skin tightening. Some of these technologies include ultrasound (US; US-assisted liposculpture, VASER-assisted liposuction), power suction (power-assisted liposuction), radiofrequency (RF; RF-assisted lipolysis), and laser (laser-assisted liposuction). In addition, some of these devices have been shown to reduce the incidence of hematomas/inflammation and shorten recovery time. We report our experience in high-definition liposculpture of the arms in addition to new technologies to improve skin retraction, comparing their results in terms of complications, satisfaction score, and aesthetic outcomes. We included patients with mild-to-moderate arm dermatochalasis (Duncan classification) fat deposits in the upper extremities who were considered candidates for third-generation US-assisted liposculpture, power-assisted liposuction, RF-assisted lipolysis/skin tightening, and laser-assisted liposuction. A total of 683 consecutive patients met the inclusion criteria for the study. Most of them were women (n = 605, 88%). Fat grafting was performed in 80 patients (11.7%). A significant portion of the patients were secondary cases (n = 223, 33%). Age ranged from 18 to 70 years (median = 38 years). BMI ranged from 17.8 to 34.8 kg/m2 (mean = 24.3 kg/m2). RF-assisted and laser-assisted high-definition liposculpture of the arms are both effective and reproducible techniques for patients who seek an athletic and slim arm contour. A low rate of complications and high satisfaction index support our findings.
Takeaways
Question: What are the benefits of using new technologies for liposculpture of the arms?
Findings: Patients with arm dermatochalasis and adipose deposits underwent arm liposculpture using different technologies such as vibration amplification of sound energy at resonance, power liposuction devices, laser, and/or radiofrequency. Results showed high satisfaction scores and a lower rate of complications among a cohort of 683 patients. Combination of ultrasound, MicroAire, and radiofrequency demonstrated both safety and effectiveness in enhancing the contour of the arms.
Meaning: New technologies enhance the aesthetic outcomes after arm liposculpture. Our study affirms their safety and reliability.
INTRODUCTION
Currently, liposculpture is the most commonly performed aesthetic procedure worldwide, yet addressing the arms remains a significant challenge for some plastic surgeons.1 Achieving a natural and defined contour in this area requires considering various anatomic structures such as adipose and muscular layers, deep noble structures, and skin laxity.2–4 Additionally, individual patient characteristics, including sex, degree of dermatochalasis, previous surgery, and skin quality (thickness, moisture, recoil, among others) are essential factors in overcoming this challenge.5 To aid in achieving optimal results, the incorporation of new technologies to assist the liposuction procedure is becoming increasingly common. These technologies allow for a softer technique, balanced shaping, elimination of excess adipose tissue, and skin tightening. To mention some of these technologies: ultrasound (US; US-assisted liposculpture, VASER-assisted liposuction), power suction [power-assisted liposuction (PAL)], radiofrequency (RF; RF-assisted lipolysis), and laser (laser-assisted liposuction). Most of these devices are designed to improve skin quality by actively contracting subdermal collagen fibers and reducing the loose skin in the posterior arm, without the need for additional surgical incisions.5–8
PAL relies on either cannula enhanced closed-suction device (Power X, VASER Lipo System 2021 Solta Medical; Bausch Health Companies Inc., Bothell, Wash.) or cannula oscillating and vibrating movement to accelerate fat removal (MicroAire Liposuction System 2020; MicroAire Surgical Instruments, LLC).4 US-assisted liposuction (VASER Lipo System 2021 Solta Medical; Bausch Health Companies Inc.) uses US wave energy to break up supportive tissue from fat cells, emulsify some fat cells while protecting other structures such as vessels, lymphatics and nerves.5,7 Other devices with growing popularity are RF-based technologies (BodyTite and Morpheus-8; INMODE Aesthetics Ltd., Lake Forest, Calif.) and lasers. RF generates electromagnetic energy that promotes tissue lipolysis, promotes neocollagenesis, and retracts mature collagen fibers. This aids liposuction procedures by improving skin tone and elasticity.5,8,9 Lasers selectively cause photothermolysis, breaking down adipocytes without affecting surrounding structures. They effectively emulsify fat to ease extraction; however, they disrupt the fat cells to a level that might not be suitable for autologous lipoinjection.5,10 The latter is a true downside of laser, as high-definition liposculpture (HDL) entails per se, fat grafting to certain areas.11
Considering the growing demand for arm liposuction and the current shift toward more conservative techniques, we present a compilation of experiences from various surgeons in different centers, using diverse technologies for skin tightening following arm high-definition liposuction.2,4
Anatomy
The skin of the arm is highly susceptible to premature wrinkles and cording due to, its skin thinness compared with other body areas.12 The subcutaneous fat layer in the arm consists of two components: the superficial (areolar) layer and the deep (lamellar) layer. The areolar layer is composed of vertically arranged cells separated by arches of connective tissue, blood vessels, and secondary lymphatic vessels. On the other hand, the lamellar layer contains larger adipose cells, connective tissue, and primary blood vessels/lymphatics. The posterior-external and anteroexternal parts of the arm are particularly prone to fat deposition in the lamellar layer.2,12 The superficial fascial system separates these layers and blends medially with the clavipectoral and axillary fascial systems. With aging and excessive weight loss, such fascial systems may deteriorate, leading to significant arm ptosis. The deep fascial system covers the muscles (deltoid, biceps, and triceps) and important structures. The contour and shape of the arm are influenced by muscular development and the patient’s gender.12–14 The medial brachial cutaneous nerve and medial antebrachial cutaneous nerve originate from the medial fascicle of the lower trunk of the brachial plexus. They provide superficial and deep sensation to the elbow, proximal forearm, and the upper third of the arm. The deep brachial artery and the cephalic vein run alongside the medial brachial cutaneous nerve, all of which border the ulnar nerve. The lymphatics follow the venous system, converging and draining at the axillary region, specifically in the axillary ganglia. Recognizing and understanding the anatomical structures is crucial to performing a precise superficial technique and avoiding injury during the procedure.12
MATERIALS AND METHODS
We carried out a retrospective review of medical records from the senior authors (L.C.C.U. and R.B.) and looked for patients with brachial dermatochalasis stages 1, 2a, and 2b, according to Duncan’s classification15 who underwent arm liposculpture between January 2018 and December 2022. Inclusion and exclusion criteria are described in Table 1. We also performed a bibliographic search with terms “arm liposculpture” AND “technologies” AND “device-based liposuction” in the following databases: PubMed, ClinicalKey, Science Direct, and OMIM. This allowed us to broaden our discussion to find updated information about new technologies involved in arm contouring surgery.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion criteria |
| - Age between 18 and 60 y old - ASA I and ASA II patients - BMI ≤ 35 kg/m2 - Mild-to-moderate brachial dermatochalasis including stages 1, 2A, 2B (Duncan*) |
| Exclusion criteria |
| - Pregnant or breast-feeding women - Severe dermatochalasis and/or patients requiring brachioplasty - BMI > 35 kg/m2 - Postbariatric patients - Active users of: pacemakers, internal defibrillators, or any other active electromagnetic implant - Patients with plates, metal pins, silicone implants, or any filler substance in the arms - Any active skin condition at area of treatment - Isotretinoin use or any derivative (Accutane, Roaccutane) within 6 mo before surgery - Prior use of: hyaluronic acid, fractional CO2 laser, micro needling, morpheus, or any other skin retraction technologies at the area of treatment - Presence of any of the following comorbidities: History of skin cancer or premalignant lesions; cardiac disorders, epilepsy, uncontrolled hypertension, diabetes mellitus, thyroid dysfunction, liver, or kidney disease; hemorrhagic coagulopathies or use of anticoagulants; any condition or drug use that might lead to an immunosuppressive state (eg, AIDS, HIV, medications) - Any allergic or hypersensitivity reaction to conductive gel |
Duncan classification of skin dermatochalasis.
ASA, American Society of Anesthesiologists physical status classification.
Surgery
Landmarking for the surgery is conducted with the patient in a standing position. [See Video 1 (online), which shows markings.] Just before patient preparation, we mark the areas of fat deposits, negative spaces, and lines for muscular definition. The patients are initially positioned in a prone position and then shifted to a supine position for the arm liposuction procedure. The arms are positioned in 90-degree abduction at a neutral position, with external and internal rotation, and 90-degree elbow flexion. We make three access incisions: one anterior, one posterior over the axillary folds, and one at the elbow. The liposuction is performed using a traditional three-step approach: (1) infiltration with tumescent solution (1000 mL of saline and 1 mg of 1:1000 epinephrine + lidocaine 10 mg/kg, and 250 mg tranexamic acid); (2) vibration amplification of sound energy at resonance (VASER)-assisted fat emulsification in intermittent mode at 40%–50% power; (3) PAL using the MicroAire liposuction system with 3- and 4-mm straight Mercedes cannulas. [See Video 2 (online), which shows surgery—variable energy and ultrasound arms.] We follow our markings for HDL and address the dynamic zones at the distal, proximal, and mid arms. The muscular definition is tailored according to the patient’s preferences and body phenotype.16
Video 1. This video shows: Arm positioning: 90º abduction at the shoulder in neutral flexion, internal rotation to 90º and elbow flexed at 90º. Marking: Deltoid area is marked with black, surrounding the posterior and intermediate fascicles of the muscle. The proximal shadow limits the liposuction over the teres muscles, while also addresses the deltoid insertion (humerus tuberosity) and the dynamic zone between the triceps and the deltoid, by internal and external rotation of the shoulder joint at 90º abduction. Negative spaces and fat deposits are marked with green, as well as the posterior axis of the arm, which will guide the posterior projection.
Video 2. This video shows a classic three-step approach for arms liposculpture: 1. Infiltration; 2. VASER emulsification; 3. Liposculpture.
After liposculpture, we used either one of the four different technologies (BodyTite, Morpheus-8, Renuvion, Lumiia Diode Laser) to improve skin tightening in patients with some or any grade of arm ptosis. All patients underwent general anesthesia, which included a combination of IV medication (propofol, dexmedetomidine, and remifentanil) plus inhaled anesthetics (sevoflurane). Additional IV medications were antibiotic prophylaxis with Cefazolin (2 g IV, 60 minutes before incision), dexamethasone 8 mg, metoclopramide 10 mg, diclofenac 50 mg, and ranitidine 50 mg. Patients were kept in normothermia by means of an air-inflated blanket (preoperative and postoperative) and an electric-heated blanket (during surgery). We took medical-grade photographs before and during follow-up appointments at 2 days and 1, 3, 6, and 12 months after surgery.
Ethical Considerations
Each patient was informed of the purpose, methods, sources of funding, any possible conflicts of interest, institutional affiliations of the authors, anticipated benefits, potential risks of our study and the discomfort it may entail, poststudy provisions and outcomes according to the Declaration of Helsinki (Fortaleza 2013), and Resolutions 8430 of 1993 and 2378 of 2008 of the Ministry of Health and Social Protection of Colombia. They were also informed of the right to refuse to participate in the study or to withdraw consent to participate at any time without reprisal. A freely given informed consent was signed for each patient participating in our report.
Outcome Evaluation
Patients were asked to complete a nonstandardized survey to evaluate postoperative outcomes between 3 and 6 months after the surgery. The survey consisted of questions formulated in a Likert-based model, and the results were evaluated accordingly.
Statistical Analysis
For continuous variables with normal distribution, unpaired two-sided t tests were conducted, and Mann–Whitney U tests for nonnormal distribution to determine if the two groups were equal. Wilcoxon signed-rank test was used if no normal distribution was found. Categorical variable significance was tested with chi-square test; dichotomous variables were tested with Fisher exact test. Outcomes were tested to a significance level of 5% (P ≤ 0.05). Jamovi (version 2.3, computer software, retrieved from https://www.jamovi.org) was used for statistical analysis.
RESULTS
We identified a total of 683 consecutive patients who met the inclusion criteria for the study. However, seven of these patients underwent brachioplasty and were therefore excluded from the analysis. The majority of the included patients were woman (n = 605, 88%). Fat grafting was performed in 80 patients (11.7%), predominantly targeting the deltoids and biceps muscles. The duration of surgery was not specifically evaluated, as arm liposuction is commonly performed in conjunction with a 360-degree body sculpting procedure. A significant portion of the patients were secondary cases (n = 223, 33%). The age of the patients ranged from 18 to 70 years, with a median age of 38. The BMI ranged from 17.8 to 34.8 kg/m2, with a mean of 24.3. Additional demographic data can be found in Tables 2 and 3.
Table 2.
Patient Demographics (Descriptive Categorical)
| Level | Count | Proportion, % | |
|---|---|---|---|
| Sex | Female | 605 | 88.6 |
| Male | 78 | 11.4 | |
| Type of surgery | Lipo + brachioplasty | 7 | 1.0 |
| Lipo + FG | 80 | 11.7 | |
| Liposuction | 596 | 87.3 | |
| Deltoids FG | No | 660 | 96.6 |
| Yes | 23 | 3.4 | |
| Biceps FG | No | 664 | 97.2 |
| Yes | 19 | 2.8 | |
| Prior surgery | 1 | 427 | 62.5 |
| 2 | 223 | 32.7 | |
| 3 | 33 | 4.8 | |
| Complications | Asymmetry | 4 | 0.6 |
| Cording | 30 | 4.4 | |
| Dehiscence | 6 | 0.9 | |
| Edema | 58 | 8.5 | |
| Hematoma | 1 | 0.1 | |
| Infection | 1 | 0.1 | |
| No | 583 | 85.4 | |
| Power X | No | 585 | 85.7 |
| Yes | 98 | 14.3 | |
| VASER | No | 14 | 2.0 |
| Yes | 669 | 98.0 | |
| MicroAire | No | 39 | 5.7 |
| Yes | 644 | 94.3 | |
| Renuvion | No | 588 | 86.1 |
| Yes | 95 | 13.9 | |
| BodyTite | No | 656 | 96.0 |
| Yes | 27 | 4.0 | |
| Laser | No | 449 | 65.7 |
| Yes | 234 | 34.3 |
FG, fat grafting.
Table 3.
Patient Demographics (Descriptive Continuous)
| Age | Weight | BMI | Year | |
|---|---|---|---|---|
| n | 683 | 683 | 683 | 683 |
| Missing | 10 | 10 | 10 | 10 |
| Mean | 40 | 63.9 | 24.3 | 2021 |
| Median | 38 | 63 | 23.9 | 2022 |
| SD | 9.48 | 8.13 | 2.64 | 1.22 |
| Minimum | 18 | 39 | 17.8 | 2018 |
| Maximum | 70 | 105 | 34.8 | 2022 |
The most frequently used technologies included VASER + MicroAire and VASER + MicroAire + Laser, each accounting for 34.7% and 34.3% of the cases, respectively. Additional information can be found in Table 4.
Table 4.
Distribution of Frequencies among Different Types of Technologies per Procedure
| Level | Count | Proportion, % |
|---|---|---|
| Power X | 8 | 1.2 |
| Renuvion | 1 | 0.1 |
| VASER + MicroAire | 237 | 34.7 |
| VASER + Power X | 24 | 3.5 |
| VASER + Renuvion | 1 | 0.1 |
| VASER + Power X + MicroAire | 57 | 8.3 |
| VASER + MicroAire + BodyTite | 22 | 3.2 |
| VASER + MicroAire + LASER | 234 | 34.3 |
| VASER + MicroAire + Renuvion | 81 | 11.9 |
| VASER + Power X + MicroAire + BodyTite | 1 | 0.1 |
| VASER + Power X + MicroAire + Renuvion | 8 | 1.2 |
| VASER + MicroAire + Renuvion + BodyTite | 4 | 0.6 |
Complications were reported in 14.6% of the cases, as outlined in Tables 2 and 5. The majority of these complications were considered minor and occurred during the early postoperative period, including edema and cording (8.5% and 4.4%, respectively). Treatment for cording involved subcutaneous medication and intermittent sessions of external US and RF. Only one infection of the posterior arm was reported in our cohort, which was successfully managed with a 7-day course of oral antibiotics, wound irrigation, and dressings. No major complications were reported.
Table 5.
Distribution of Technologies per Procedure and Their Relationship with Number of Complications
| Complications | ||||||||
|---|---|---|---|---|---|---|---|---|
| Technologies per procedure |
Asymmetry | Cording | Dehiscence | Edema | Hematoma | Infection | Total | |
| VASER + MicroAire | n | 1 | 8 | 1 | 29 | 1 | 1 | 41 |
| % | 0.1 | 1.2 | 0.1 | 4.2 | 0.1 | 0.1 | 6.0 | |
| VASER + Power X | n | 1 | 0 | 0 | 2 | 0 | 0 | 3 |
| % | 0.1 | 0.0 | 0.0 | 0.3 | 0.0 | 0.0 | 0.4 | |
| VASER + Power X + MicroAire | n | 0 | 1 | 2 | 6 | 0 | 0 | 9 |
| % | 0.0 | 0.1 | 0.3 | 0.9 | 0.0 | 0.0 | 1.3 | |
| VASER + Power X + MicroAire + Renuvion | n | 0 | 0 | 1 | 1 | 0 | 0 | 2 |
| % | 0.0 | 0.0 | 0.1 | 0.1 | 0.0 | 0.0 | 0.3 | |
| VASER + MicroAire + BodyTite | n | 0 | 2 | 0 | 7 | 0 | 0 | 9 |
| % | 0.0 | 0.3 | 0.0 | 1.0 | 0.0 | 0.0 | 1.3 | |
| VASER + MicroAire + Renuvion + BodyTite | n | 0 | 0 | 0 | 3 | 0 | 0 | 3 |
| % | 0.0 | 0.0 | 0.0 | 0.4 | 0.0 | 0.0 | 0.5 | |
| VASER + MicroAire + LASER | n | 0 | 12 | 1 | 2 | 0 | 0 | 15 |
| % | 0.0 | 1.8 | 0.1 | 0.3 | 0.0 | 0.0 | 2.2 | |
| VASER + MicroAire + BodyTite | n | 0 | 0 | e0 | 0 | 0 | 0 | 0 |
| % | 0.0 | 0.0 % | 0.0 % | 0.0 % | 0.0 % | 0.0 % | 0.0 % | |
| VASER + MicroAire + Renuvion | n | 2 | 6 | 1 | 8 | 0 | 0 | 17 |
| % | 0.3 | 0.9 | 0.1 | 1.2 | 0.0 | 0.0 | 2.5 | |
| Renuvion | n | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| % | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| VASER + Power X | n | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| % | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| VASER + Renuvion | n | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| % | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | |
| MicroAire | n | 0 | 0 | 0 | 0 | 0 | 0 | 5 |
| % | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Power X | n | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| % | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| VASER + Power X + MicroAire + BodyTite | n | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| % | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Total | n | 4 | 30 | 6 | 58 | 1 | 1 | 100 |
| % | 0.6 | 4.4 | 0.9 | 8.5 | 0.1 | 0.1 | 14.6 | |
Analysis of our survey was conducted using scores ranging from 1 to 10, where scores of 1–3 were considered detrimental results and scores of 7–10 were considered good/optimal (Table 6). The majority of patients (87%) expressed satisfaction with the procedure, with a significant number of them assigning a perfect score (55%). Stratified analysis revealed a statistical difference with lower complication rates in patients undergoing laser and BodyTite therapies. However, after weighting the data and considering the practical significance (effect size, ε2), no associations were found between complications and the different technologies used (Table 7). Similarly, stratified analysis showed a statistical difference with higher scores in patients undergoing VASER, Laser, and Renuvion procedures. However, once again, after weighting the data (ε2), no associations were found between complications and the various technologies utilized (Table 8).
Table 6.
Distribution of Technologies per Procedure and Their Relationship with the Satisfaction Score
| Satisfaction Score | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Technologies per procedure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total |
| VASER + MicroAire | 1 | 3 | 3 | 0 | 8 | 6 | 25 | 75 | 17 | 75 | 213 |
| VASER + Power X | 0 | 0 | 0 | 0 | 1 | 1 | 4 | 5 | 2 | 7 | 20 |
| VASER + Power X + MicroAire | 0 | 1 | 0 | 0 | 2 | 7 | 9 | 12 | 4 | 16 | 51 |
| VASER + Power X + MicroAire + Renuvion | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 4 | 8 |
| VASER + MicroAire + BodyTite | 0 | 0 | 0 | 0 | 2 | 1 | 2 | 8 | 1 | 7 | 21 |
| VASER + MicroAire + RENUVION + BodyTite | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 4 |
| VASER + MicroAire + LASER | 0 | 0 | 1 | 2 | 19 | 2 | 32 | 39 | 0 | 134 | 229 |
| VASER + MicroAire + BodyTite | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| VASER + MicroAire + Renuvion | 0 | 0 | 1 | 2 | 4 | 5 | 7 | 26 | 6 | 23 | 74 |
| RENUVION | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| VASER + Power X | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 2 |
| VASER + Renuvion | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| MicroAire | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 4 |
| Power X | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 4 | 8 |
| VASER + Power X + MicroAire + BodyTite | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Total | 1 | 4 | 5 | 6 | 37 | 25 | 82 | 169 | 35 | 272 | 636 |
Table 7.
Stratified Analysis of Complications per Technology (Independently)
| Technology | χ² | df | P | ε² |
|---|---|---|---|---|
| Power X | 9.92 | 6 | 0.128 | 0.01455 |
| VASER | 2.45 | 6 | 0.874 | 0.00359 |
| MicroAire | 4.2 | 6 | 0.649 | 0.00616 |
| Renuvion | 12.18 | 6 | 0.058 | 0.01786 |
| BodyTite | 30.93 | 6 | <0.001 | 0.04535 |
| Laser | 31.62 | 6 | <0.001 | 0.04636 |
Table 8.
Stratified Analysis of Satisfaction Score per Technology (Independently)
| Technology | χ² | df | P | ε² |
|---|---|---|---|---|
| Power X | 16 | 9 | 0.067 | 0.0252 |
| VASER | 23.9 | 9 | 0.005 | 0.0376 |
| MicroAire | 12.2 | 9 | 0.203 | 0.0192 |
| Renuvion | 19 | 9 | 0.025 | 0.0299 |
| BodyTite | 11.8 | 9 | 0.227 | 0.0185 |
| Laser | 68.6 | 9 | <0.001 | 0.108 |
DISCUSSION
When it comes to liposculpture, the arms remain a challenging area to treat.4 The complex subdermal anatomy, redundant skin, and variations in adipose tissue distribution based on sex and ethnicity have prompted various authors to propose different classifications for liposuction.1–3,12,15,17–23 Some of these classifications have focused on avoiding the need for brachioplasty. For instance, Appelt et al24 reported their experience with a classification based on the specific location of laxity and recommended a certain type of brachioplasty for patients in each category. Chia et al,1 Dayan et al,25 and Theodorou et al6,26 classified arms according to their skin laxity and quality while also providing great evidence of the efficacy of RF to improve skin retraction of the arms skin. Khatib27 measured the vertical height of hanging skin, caudal to the bicipital groove, to evaluate the degree of brachial ptosis in 2007. After that, Duncan15 presented a modified classification including concepts from Khatib,27 Teimourian and Malekzadeh,3 in which he categorized the degree of skin laxity and lipodystrophy in various stages, and has become the most widely used classification for arm contouring. We used Duncan classification to asses our patients preoperatively and guided surgery based on HDL premises (Figs. 1–3).
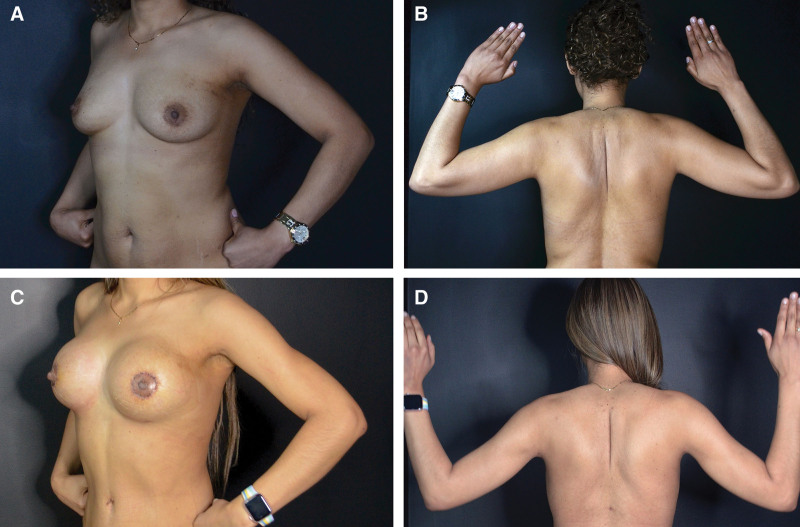
Fig. 1.
A 31-year-old female patient. Preoperative BMI: 24.5 kg/m2. Postoperative BMI: 23.1 kg/m2. Procedure: HDL including arms and thighs + abdominoplasty + buttocks fat grafting (500 mL/side). Lipoaspirate: 6800 mL. Technologies for variable energy and ultrasound arms: VASER, MicroAire, BodyTite. Preoperative pictures show a stage 2a posterior arm ptosis with moderate fat deposits (A and B), whereas the postoperative photographs (8 weeks) show a younger appearance and athletic definition of the arms with a proper skin retraction without resection procedures (C and D).
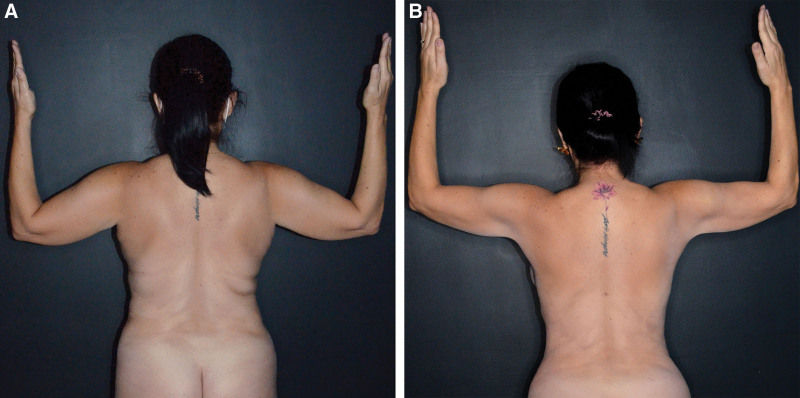
Fig. 3.
A 49-year-old female patient with moderate-to-severe brachial dermatochalasis underwent high-definition liposuction and RF treatment with BodyTite on her arms. The 3-month postoperative photograph (B) reveals a newly rejuvenated arm, in contrast to the preoperative photograph (A) depicting severe skin sagging and adipose deposits.
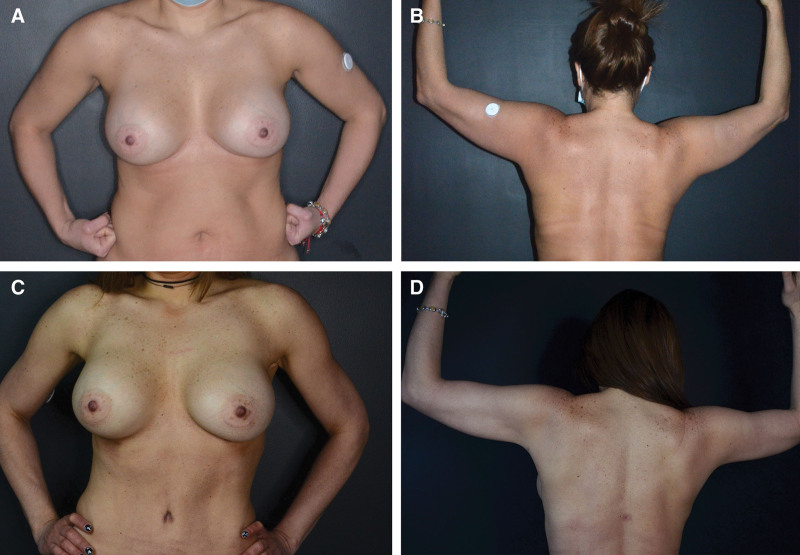
Fig. 2.
A 46-year-old female patient. Medical history: Maturity-onset diabetes of the young diabetes mellitus. Preoperative BMI: 27.7 kg/m2. Postoperative BMI: 24.2 kg/m2. Procedure: HDL including arms + abdominoplasty + Buttocks fat grafting (500 mL/side). Lipoaspirate: 3400 mL. Technologies for variable energy and ultrasound arms: VASER, MicroAire, BodyTite (abdomen), and Morpheus-8 (arms). Preoperative pictures show a stage 2b posterior arm ptosis with a bulky look due to moderate fat deposits (A and B). Outstanding skin retraction and a new muscular definition is evident in these 2-month postoperative photographs (C and D).
Our study aimed to investigate potential differences in outcomes between different technologies used for skin tightening following arm HDL.2,4 Although the data revealed a skewed distribution favoring laser liposuction [which was utilized in 95% of cases by one of the authors (R.B.)], the combination of VASER and MicroAire demonstrated comparable rates of complications and satisfaction indices, as determined through effect size comparison (ε2). This finding further supports the significant benefits of both technologies for arm contouring and muscular definition.2,4,12,19,28 Interestingly, the use of any technology in addition to VASER and MicroAire (such as Renuvion, BodyTite, or Laser) was associated with a higher incidence of complications (P < 0.05). However, after considering the practical significance (effect size), only BodyTite and laser showed a slightly different yet not statistically significant rate of complications, which can be attributed to the skewed distribution toward these specific devices (most patients underwent either of these two technologies).
Stratified analysis of the satisfaction score showed a lack of statistical difference only for laser technology after effect size comparison, which could mean that its actual benefits might be related to the use of VASER and MicroAire, rather than the use of laser diode itself. Although our study did not specifically analyze outcomes related to skin retraction for each technology, the high satisfaction index observed indirectly suggests that these technologies may indeed be effective for achieving desirable skin retraction outcomes. [See figure, Supplemental Digital Content 1, which shows a 32-year-old female patient with moderate-to-severe brachial dermatochalasis who underwent BodyTite RF treatment of the arm in addition to HDL (using VASER and MicroAire), http://links.lww.com/PRSGO/D90.] [See figure, Supplemental Digital Content 2, which shows a 30-year-old woman who presented with moderate brachial dermatochalasis. She underwent HDL (using VASER, MicroAire, and Power X) and received Renuvion treatment for her arms, http://links.lww.com/PRSGO/D91.] Only a small subset of patients (n = 13, 2%) underwent the combination of four different technologies, including MicroAire, VASER, Power X, Renuvion, and/or BodyTite. Interestingly, no increase in complications or alterations in satisfaction scores were observed when compared with the use of other technologies individually.
Patient safety and satisfaction have been key factors driving the design and innovation of various body contouring alternatives in terms of technology. In 1994, Apfelberg et al29 demonstrated that incorporating a laser fiber within a standard liposuction cannula reduced blood loss and improved postoperative recovery.5 Subsequent studies revealed that direct application of laser energy to subcutaneous tissue destroyed adipocyte structure, converting fatty tissue into an emulsion that could be absorbed or lipoaspirated.30 Comparatively, RF-assisted liposuction and lipolysis revolutionized the field by incorporating benefits of subdermal tissue retraction and collagen remodeling.1,6,26,31,32 In fact, we recently published the effects of RF on collagen synthesis and fibroblast activity in a biopsy and molecular-based article.8
The operative techniques that we are reporting align with the current concepts and premises of high-definition arm contouring described by Hoyos and Perez.2,4 However, we incorporate new technologies for skin tightening to embrace more conservative approaches, as suggested by Hoyos et al33 in their recent work on excisional body contouring surgery. Our results support the benefits of both RF-assisted lipolysis and laser-assisted liposuction with similar outcomes and reproducible techniques. VASER, MicroAire, BodyTite, and Diode Laser are all technologies that complement HDL to achieve well-defined, athletic arms.
Nevertheless, fibrotic cords pose a significant challenge for surgeons (4.4% in our cohort), as they are often associated with both technique and patient skin quality. Excessive trauma and the subsequent superficial injury to the lymphatic vessels usually end up with internal scarring, secondary disordered accumulation of collagen fibers and, ultimately, skin cords. Most postoperative cording solves without further treatment apart from local massages and stretching exercises. However, those that remain after initial treatment are the ones that usually require intralesional injection of enzymatic/anti-inflammatory medication and extensive follow-up.1,19,20,24,28,34 Other complications of arm contouring include overresection, burns, asymmetry, and contour defects, all of which can be treated with reoperative procedures (lipoinjection, liposhifting, and equalization).
Limitations
Failure to objectively evaluate the degree of skin retraction among devices is definitely a shortcoming of our article. Skewed data also make difficult a proper analysis even after weighting data. Clinical trials comparing technologies are required to further support our findings.
CONCLUSIONS
RF-assisted and laser-assisted HDL of the arms are both effective and reproducible techniques for patients who seek an athletic and slim arm contour. Addition of RF- and laser-based devices to improve skin retraction allow the surgeon to move into more conservative techniques for arm contouring. A low rate of complications and high satisfaction support our findings.
DISCLOSURES
The authors did not have financial interest or receive any financial support of the products or devices mentioned in this article. Dr. Cala serves as a consultant and receives royalties by performing as a speaker from INMODE aesthetics (InMode Ltd. 2022, Lake Forest, Calif.). INMODE is manufacturer and owner from BodyTite and Morpheus-8 devices. The other authors have no financial interest to declare.
Supplementary Material
Footnotes
Published online 19 March 2024.
Presented at the 4th annual meeting of the Moroccan Society of Aesthetic Plastic Surgeons, SOMCEP, Variable Energy and Ultrasound Arms, Marrakech, Morocco, October 29, 2022.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Chia CT, Theodorou SJ, Hoyos AE, et al. Radiofrequency-assisted liposuction compared with aggressive superficial, subdermal liposuction of the arms. Plast Reconstr Surg Glob Open. 2015;3:e459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoyos A, Perez M. Arm dynamic definition by liposculpture and fat grafting. Aesthet Surg J. 2012;32:974–987. [DOI] [PubMed] [Google Scholar]
- 3.Teimourian B, Malekzadeh S. Rejuvenation of the upper arm. Plast Reconstr Surg. 1998;102:545–551; discussion 552. [DOI] [PubMed] [Google Scholar]
- 4.Hoyos A. Arms. In: Perez M, ed. Total Definer: Atlas of Body Sculpting. 1st ed. New York: Thieme; 2023:251–298. [Google Scholar]
- 5.Shridharani S, Broyles J, Matarasso A. Liposuction devices: technology update. Med Devices. 2014;7:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Theodorou SJ, Del Vecchio D, Chia CT. Soft tissue contraction in body contouring with radiofrequency-assisted liposuction: a treatment gap solution. Aesthet Surg J. 2018;38:S74–S83. [DOI] [PubMed] [Google Scholar]
- 7.Hoyos A, Millard J. VASER-assisted high-definition liposculpture. Aesthet Surg J. 2007;27:594–604. [DOI] [PubMed] [Google Scholar]
- 8.Cala Uribe LC, Perez Pachon ME, Zannin Ferrero A, et al. Effects of bipolar radiofrequency on collagen synthesis from patients with brachial ptosis. Plast Reconstr Surg Glob Open. 2023;11:e4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaplan H, Gat A. Clinical and histopathological results following TriPollarTM radiofrequency skin treatments. J Cosmet Laser Ther. 2009;11:78–84. [DOI] [PubMed] [Google Scholar]
- 10.Badin A, Moraes L, Gondek L, et al. Laser lipolysis: flaccidity under control. Aesthetic Plast Surg. 2002;26:335–339. [DOI] [PubMed] [Google Scholar]
- 11.Coleman SR. Structural fat grafting: more than a permanent filler. Plast Reconstr Surg. 2006;118(3 Suppl):108S–120S. [DOI] [PubMed] [Google Scholar]
- 12.Miotto G, Ortiz-Pomales Y. Arm contouring: review and current concepts. Aesthet Surg J. 2018;38:850–860. [DOI] [PubMed] [Google Scholar]
- 13.Lockwood T. Brachioplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96:912–920. [DOI] [PubMed] [Google Scholar]
- 14.Gusenoff JA, Coon D, Rubin JP. Brachioplasty and concomitant procedures after massive weight loss: a statistical analysis from a prospective registry. Plast Reconstr Surg. 2008;122:595–603. [DOI] [PubMed] [Google Scholar]
- 15.Duncan DI. Improving outcomes in upper arm liposuction: adding radiofrequency-assisted liposuction to induce skin contraction. Aesthet Surg J. 2012;32:84–95. [DOI] [PubMed] [Google Scholar]
- 16.Hoyos AE, Perez ME, Domínguez-Millán R. Variable sculpting in dynamic definition body contouring: procedure selection and management algorithm. Aesthet Surg J. 2021;41:318–332. [DOI] [PubMed] [Google Scholar]
- 17.Schlesinger SL. Suction-assisted lipectomy of the upper arm: a four-cannula technique. Aesthetic Plast Surg. 1990;14:271–274. [DOI] [PubMed] [Google Scholar]
- 18.Dudelzak J, Hussain M, Goldberg DJ. Laser lipolysis of the arm, with and without suction aspiration: clinical and histologic changes. J Cosmet Laser Ther. 2009;11:70–73. [DOI] [PubMed] [Google Scholar]
- 19.Boeni R. Circumferential liposuction of the female arm. Am J Cosmet Surg. 2019;36:125–129. [Google Scholar]
- 20.Gilliland MD, Lyos AT. CAST Liposuction of the arm improves aesthetic results. Aesthetic Plast Surg. 1997;21:225–229. [DOI] [PubMed] [Google Scholar]
- 21.Hong YG, Sim HB, Lee MY, et al. Three-dimensional circumferential liposuction of the overweight or obese upper arm. Aesthetic Plast Surg. 2012;36:497–503. [DOI] [PubMed] [Google Scholar]
- 22.Di Pietro V, Colicchia G, Cervelli V, et al. Arm contouring after massive weight loss: liposuction-assisted brachioplasty versus standard technique. J Cutan Aesthet Surg. 2018;11:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brightman L, Weiss E, Chapas AM, et al. Improvement in arm and post-partum abdominal and flank subcutaneous fat deposits and skin laxity using a bipolar radiofrequency, infrared, vacuum and mechanical massage device. Lasers Surg Med. 2009;41:791–798. [DOI] [PubMed] [Google Scholar]
- 24.Appelt EA, Janis JE, Rohrich RJ. An algorithmic approach to upper arm contouring. Plast Reconstr Surg. 2006;118:237–246. [DOI] [PubMed] [Google Scholar]
- 25.Dayan E, Chia C, Burns AJ, et al. Adjustable depth fractional radiofrequency combined with bipolar radiofrequency: a minimally invasive combination treatment for skin laxity. Aesthet Surg J. 2019;39(Suppl_3):S112–S119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Theodorou SJ, Paresi RJ, Chia CT. Radiofrequency-assisted liposuction device for body contouring: 97 patients under local anesthesia. Aesthetic Plast Surg. 2012;36:767–779. [DOI] [PubMed] [Google Scholar]
- 27.Khatib HAE. Classification of brachial ptosis: strategy for treatment. Plast Reconstr Surg. 2007;119:1337–1342. [DOI] [PubMed] [Google Scholar]
- 28.Hoyos AE, Stefanelli M, Perez ME, et al. Adipose tissue transfer in dynamic definition liposculpture PART III. The arms: biceps, triceps, and deltoids. Plast Reconstr Surg Glob Open. 2023;11:e4651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Apfelberg DB, Rosenthal S, Hunstad JP, et al. Progress report on multicenter study of laser-assisted liposuction. Aesthetic Plast Surg. 1994;18:259–264. [DOI] [PubMed] [Google Scholar]
- 30.Leclère FM, Alcolea JM, Vogt P, et al. Laser-assisted lipolysis for arm contouring in Teimourian grades I and II: a prospective study of 45 patients. Lasers Med Sci. 2015;30:1053–1059. [DOI] [PubMed] [Google Scholar]
- 31.Mulholland RS. BodyTite: the science and art of radiofrequency assisted lipocoagulation (RFAL) in body contouring surgery. The Art of Body Contouring. IntechOpen; 2019. Available at: 10.5772/intechopen.83446 [DOI] [Google Scholar]
- 32.Mulholland RS. Radio frequency energy for non-invasive and minimally invasive skin tightening. Clin Plast Surg. 2011;38:437–448, vi. [DOI] [PubMed] [Google Scholar]
- 33.Hoyos AE, Perez ME, Mogollon IR, et al. Decision-making algorithm for advanced excisional body contouring: dynamic definition solutions for skin laxity. Plast Reconstr Surg. 2022;150:1248–1259. [DOI] [PubMed] [Google Scholar]
- 34.Lim SYD, Cheng WNS. Axillary web syndrome complicating dermatologic surgery. Dermatol Surg. 2022;48:150–152. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.