Abstract
In the United States, racial disparities in adverse maternal health outcomes remain a pressing issue, with Black women experiencing a 3–4 times higher risk of maternal mortality and a 2–3 times higher risk of severe maternal morbidity. Despite recent encouraging efforts, fundamental determinants of these alarming inequities (e.g. structural racism) remain understudied. Approaches that address these structural drivers are needed to then intervene upon root causes of adverse maternal outcomes and their disparities, and to ultimately improve maternal health across the U.S. In this paper, we offer a conceptual framework for future studies of structural racism and maternal health disparities and systematically synthesize the current empirical epidemiologic literature on the links between structural racism measures and adverse maternal health outcomes. For the systematic review, we searched electronic databases (Pubmed, Web of Science, and EMBASE) to identify peer reviewed U.S. based quantitative articles published between 1990 and 2021 that assessed the link between measures of structural racism and indicators of maternal morbidity/mortality. Our search yielded 2,394 studies and after removing duplicates, 1408 were included in the title and abstract screening, of which 18 were included in the full text screening. Only 6 studies met all the specified inclusion criteria for this review. Results revealed that depending on population sub-group analyzed, measures used, and covariates considered, there was evidence that structural racism may increase the risk of adverse maternal health outcomes. This review also highlighted several areas for methodological and theoretical development in this body of work. Future work should more comprehensively assess structural racism in a way that informs policy and interventions that can ameliorate its negative consequences on racial/ethnic disparities in maternal morbidity/mortality.
Keywords: structural racism, maternal health, maternal outcomes, health inequities
1. Introduction
Pregnancy-related complications are urgent public health crises in the United States.1 The U.S. has more than twice the rate of maternal deaths compared to any other high-resource nation.2 Even more alarming are the stark racial differences in maternal mortality. Between 2007–2016, at 40.8 per 100,000 live births, Black women had the highest pregnancy-related mortality rate than any other racial group.3 Paralleling this trend, for every mother that dies due to pregnancy, there are 100 mothers who suffer a severe maternal morbidity (SMM) event.1,4–6 SMM is the occurrence of life-threatening physiologic conditions during childbirth and/or postpartum, which have serious implications for the long- and short- term outcomes of a birthing person, including survival. It comprises of severe dysfunctions (e.g. heart failure), which are common precursors to maternal mortality.7 SMM has seen increases in prevalence throughout the past few decades, with persistent and widening racial/ethnic disparities. Each year SMM affects more than 50,000 women in the U.S., and Black women face a 2-fold higher risk of SMM compared with White women.8,9 Prior research has also documented alarming racial/ethnic disparities in the prevalence of leading causes of maternal mortality such as hypertensive disorders of pregnancy.10 Addressing this dire maternal health crisis requires a close examination of root causes behind maternal morbidity and mortality, and their racial/ethnic disparities.11,12
Studies investigating the underlying factors contributing to racial disparities in pregnancy-related complications primarily focus on individual-level explanations, such as health-related behaviors (“lifestyle factors”) and clinical comorbidities (“biomedical risks”).13–17 However, stark racial/ethnic differences in maternal morbidity and mortality persist even after accounting for numerous individual-level factors. This work has also been insufficient in explaining the increased prevalence of these adverse maternal health outcomes and their racial/ethnic gaps.14,18–20 Hence, there is a pressing need to examine contextual factors that influence disease risk. The Ecosocial theory posits that addressing structural health determinants with attention to history and power is key in improving population health, as failing to do so reproduces health inequities and maintains the uneven distribution of disease.17,21 Thus, it is increasingly important to focus on socio-political forces, such as structural racism, that disproportionately disenfranchise racially/ethnically marginalized individuals.
Structural racism has received increasing attention as the main driver of racial health inequities.22 Scholars have documented its ill health-effects and how it may shape racial health inequities across a wide-range of health outcomes.23 However, the links between structural racism and adverse maternal health outcomes are severely under-investigated, and there are theoretical and methodological gaps that have yet to be addressed.24 We begin this paper by defining structural racism, describing mechanisms by which it determines health outcomes broadly, and by offering a conceptual framework that outlines the pathways through which structural racism influences pregnancy-related outcomes. We then systematically synthesize the current literature on the links between place-based measures of structural racism and maternal morbidity/mortality and identify areas of theoretical and methodological advancement for future research.
A note on language:
Throughout this manuscript, we use gendered language (e.g. “maternal,” “mothers,”, “women”) and gender-inclusive language (e.g. “people”) interchangeably with the acknowledgement that not all people who give birth are women. These terms in this paper are intended to be inclusive of all birthing persons including cisgender, transgender, queer, non-binary, and gender-diverse individuals.
1.1. Structural racism: definition and health implications
Structural racism, a legacy of settler colonialism and African slavery in the Americas, is recognized as a fundamental driver of racial/ethnic health inequities.25–28 It is defined as the totality of ways by which intrinsically linked and mutually reinforcing cultural domains and social/political institutions work in concert to disenfranchise racially/ethnically marginalized populations.23,28 These institutions, including but not limited to, the criminal legal system, housing, education, health care, and employment, together reinforce hierarchies, while perpetuating inequitable policies/practices and discriminatory social norms based on a socially ascribed identity used to subordinate members of specific racial/ethnic groups—“race.”25,26,29,30 Structural racism transcends interpersonal prejudice and bias and internalized racism, other key dimensions of racism.31 It is an upstream determinant of such norms, whose roots are embedded within the very policies, laws, and institutions that constitute the social fabric of the U.S. and consequently the everyday contexts that surround individuals.32,33
In addition to outright hate crime and violence targeted towards racially/ethnically minoritized populations in the U.S., there have been/are multiple instances of historic and contemporary state-sponsored discriminatory laws/practices that continue to harm the health and well-being of racially/ethnically marginalized people. Through restrictive housing covenants and redlining practices, Black and other people of color were unfairly denied housing and loans, were prohibited from attaining wealth in the form of homeownership, and their neighborhoods were deemed unworthy of investment.34 Federal economic subsidies that excluded Black and other people of color, together with educational and occupational segregation, denied racially/ethnically marginalized individuals access to socio-economic mobility and hindered the beneficial health rewards that come from it.35,36 Structural racism also patterns the types of hospitals where racially/ethnically marginalized individuals receive care. Despite the integration of hospitals in the wake of the civil rights movement, segregated medical care still persists—pushing Black and Brown individuals to seek treatment in lower-quality facilities and receive poor care due to provider bias.37,38 School discipline policies that disproportionately target Black and Brown youth, not only interrupt educational trajectories and hence influence health, but also directly contribute to the large/growing prison population in the U.S., which incarcerates more people per capita than any other nation.39–43 Law-enforcement violence is yet another manifestation of structural racism that causes death and injury to thousands of individuals every year, with Black individuals bearing the greatest burden.44 Specific instances of police/state violence also lead entire Black communities to experience vicarious violence and trauma.45 Mass incarceration, aided by governmental campaigns, such as the war-on-drugs and harsh mandatory sentencing laws, is another important axis of structural racism that continues to institutionalize millions of Black and Brown Americans and tear-apart countless families, depleting community resources and dismantling social fabrics.46 It is also critical to note the role that intersectionality plays in how structural racism shapes health inequities.47 Structural racism interacts with and is fueled by other forms of marginalization, including sexism, classism, ableism, homophobia, transphobia, xenophobia etc, to create new forms of social adversities, which collectively are greater than the sum of each individual source of oppression.32,48,49
1.2. Pathways linking structural racism and adverse pregnancy-related outcomes
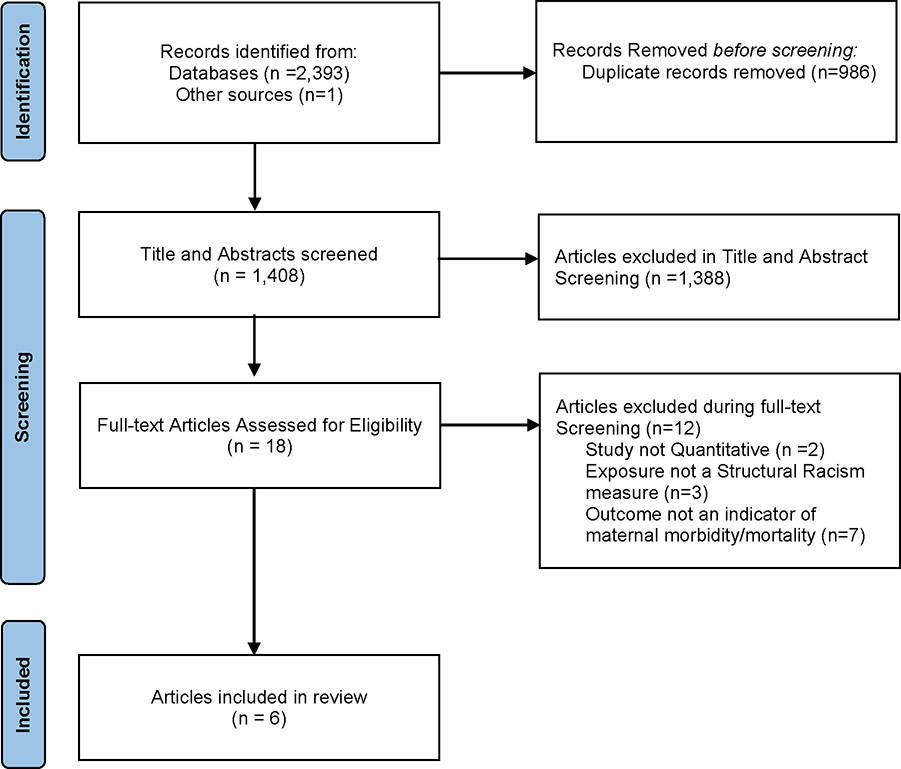
The compounding of these deeply intertwined policies, practices, and norms that exist within multiple societal/institutional domains, perpetuates racial/ethnic inequities in maternal health outcomes through multiple mechanisms.22 Figure 1 outlines the proposed pathways by which structural racism across the life-course influences uneven risk of maternal morbidity/mortality.
Fig. 1.
Structural Racism and Racial Health Inequities in Maternal Health: A Conceptual Framework.
Through the aforementioned historical and contemporary discriminatory policies and practices, structural racism has led to the concentration of poverty and unhealthy social and physical environments within racially/ethnically segregated neighborhoods in which people of color primarily reside.50,51 Such neighborhoods may lack healthy amenities, e.g. healthy grocery stores and parks, which are important predictors of health-related behaviors, preconception health, and consequently a healthy pregnancy/childbirth.52–54 Consistent with this framing, research has documented links between racial residential segregation, poor neighborhood environments, and pregnancy-related outcomes.55–58 The limited availability of safe and secure housing, and the physical proximity to sources of environmental toxins and pollutants is also another pathway through which structural racism shapes maternal health outcomes. Research has shown that historically redlined neighborhoods have increased concentration of air pollution, given that these neighborhoods are the mainstays for industrial plants, railroads, and other generators of environmental pollutants.59 As such, structural racism predisposes birthing people to respiratory illnesses, such as asthma, which have been linked with pregnancy-related complications.60
Poor educational opportunities and low-wage jobs are other important manifestations of structural racism, which hinder upward social mobility among racially/ethnically marginalized individuals. Structural racism patterns the distribution of health-promoting material goods/resources and socioeconomic opportunities, including access to quality and timely health care, health literacy, disposable income, and social capital. Both before and during pregnancy, these resources can be utilized to promote/maintain health, and to avoid pregnancy-related complications. Therefore, socioeconomic resources have been linked to health behaviors such as delayed prenatal care initiation, and consequently adverse maternal health outcomes and their clinical precursors (e.g. pregnancy-induced hypertension).21,22,61,62
Structural racism also shapes the distribution of psychosocial stressors and assets that influence risk of pregnancy-related complications.63 Inter-personal experiences of racism in every-day contexts have been linked with multiple mental and physical health outcomes, as well as subclinical indicators of disease, which may increase risk of adverse pregnancy-related complications.25 Stress also arises from contending with social disorder, crimes, and heightened vigilance against aggressive policing in neighborhoods negatively impacted by structural racism.45,64–66 Being chronically exposed to such stressors across the life-course triggers a cascade of maladaptive physiologic stress responses, dysregulating and compromising a large range of organ-systems and accelerating premature biological aging.67 This physiological wear and tear can then heighten a mother’s likelihood of experiencing complications during pregnancy and/or childbirth.56 By limiting the availability of community-based resources such as social support networks and neighborhood social cohesion, that may buffer the negative health consequences of stressful experiences, structural racism also leaves mothers vulnerable to adverse pregnancy outcomes.68 The biological embodiment of structural racism through stress pathways over and above material resources is also evident in research documenting that higher socio-economic status does not produce the same level of health benefits for Black individuals as it does for White individuals.69,70 There is evidence indicating adverse outcomes among upwardly-mobile Black individuals, as they may contend with additional racism-related stress due to prejudiced treatment from their colleagues in higher paying jobs and/or neighbors in more affluent neighborhoods.71 Consistent with this phenomenon, research shows that racial disparities in adverse birthing outcomes persist regardless of high socio-economic status, with Black women bearing a disproportionate risk.72,73
Partially influenced by racial and economic segregation and referral patterns, Black individuals have been found to disproportionally receive care in a concentrated set of hospitals that generally provide lower quality of care across multiple indicators.37,74,75 Prior research has documented greater risk of pregnancy-related complications associated with giving birth in primarily Black-serving hospitals, and such hospitals have also been shown to mainly serve populations whose clinical profile is at a higher risk for adverse maternal outcomes.76,77 Implicit and explicit interpersonal bias in medical care settings is another pathway through which structural racism influences adverse maternal outcomes. Black women are often given less attention and dismissed when expressing concerns about their well-being, with several examples of Black birthing individuals whose health has been compromised because of medical provider bias (including refusal to listen), regardless of their individual socioeconomic status.78,79
2. Methods:
2.1. Search strategy
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.80 We searched Pubmed, Web of Sciences, and EMBASE databases for peer-reviewed journal articles published between 1990 and September 14th, 2021. Search terms were constructed in consultation with a campus public health librarian and based on prior literature (Appendix 1 & 2). We searched for studies that assessed structural racism in relation to maternal morbidity and mortality using title, abstract, and author key words. For the structural racism-related terms, we additionally included words that indicate some of the specific measures used to assess structural racism such as “redlining” and “index of concentration at the extremes”. For the maternal morbidity and mortality terms, we also included words that indicate pregnancy-induced illnesses that are considered significant precursors of severe maternal morbidity and mortality such as preeclampsia and gestational diabetes.81,82
2.2. Study selection process
Studies were included in the review if they met the following inclusion criteria: (a) published in English, (b) based in the U.S., (c) quantitative empirical study, (d) exposure includes a measure of structural racism, and (e) outcome includes an indicator of maternal morbidity and mortality. Studies that did not assess measures of racism at the area-level (place-based measures of racial/ethnic inequities) explicitly and those that only assessed infant and birth-related outcomes such as pre-term birth were not included in the study. Two researchers (E.M.H. and S.R.M.) independently reviewed titles and abstracts as well as full text articles using Covidence 83 and conflicts were resolved during regular team meetings.
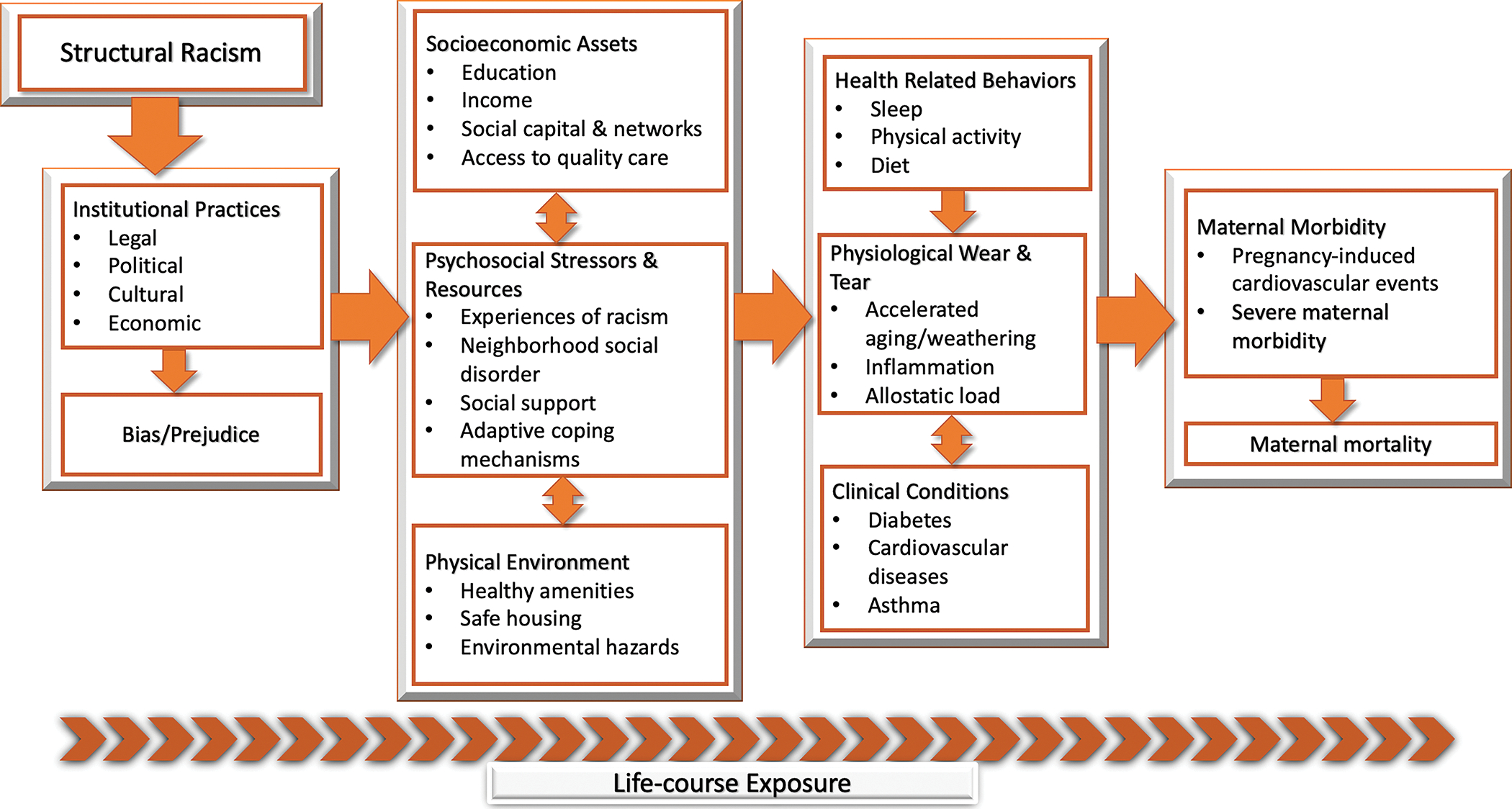
The formal search criteria identified 2,393 studies, of which 986 were removed because they were duplicates. We identified one additional study published after the formal search was conducted. This left 1408 studies to be screened for title and abstract. Of these, 18 studies advanced into the full text review and only 6 studies met all the specified inclusion criteria (Figure 2).
Figure 2:
Study inclusion PRISMA flowchart
2.3. Data extraction
Data from the studies included was extracted using a template constructed according to PRISMA guidelines on Covidence.83 In addition to study settings and characteristics, we evaluated the articles included in this review for the measures of structural racism utilized, the geographic level at which structural racism was assessed, the data sources used to measure structural racism, the pregnancy-related outcomes examined, and subsequent associations estimated. We also evaluated articles for how race/ethnicity was operationalized in the analysis/interpretation of findings and the theoretical framings and pathways highlighted on the relationship between structural racism and pregnancy-related complications.
3. Results
3.1. Study settings, population, and design
The majority of studies (66.7%) were based on samples from the North East region of the U.S. 84–87 Sample sizes ranged from 4,788 to 316,600, with half of the studies including more than 100,000 observations (Table 1). 85,86,88 All studies utilized registry-based data from either electronic health or birth records.
Table 1:
Summary of Study Characteristics
| N (%) | Reference | |
|---|---|---|
|
| ||
| Study Design | ||
| Cross-sectional | 3 (50.0) | Janevic 202085, Liu 201986, Grady 200887 |
| Retrospective Cohort | 3 (50.0) | Dyer 202188, Hollenbach 202184, Mayne 201889 |
| Sample Size | ||
| ≤10,000 | 1 (16.7) | Mayne 201889 |
| 10,000–100,000 | 2 (33.3) | Hollenbach 202184, Grady 200887 |
| >100,000 | 3 (50.0) | Dyer 202188, Janevic 202085, Liu 201986 |
| U.S. Region | ||
| North-East | 4 (66.7) | Hollenbach 202184, Janevic 202085, Liu 201986, Grady 200887 |
| Mid-West | 1 (16.7) | Mayne 201889 |
| West | - | - |
| South | 1 (16.7) | Dyer 202188 |
| Exposure Geographic level | ||
| Census-tract | 3 (50.0) | Dyer 202188, Mayne 201889, Grady 200887 |
| Zip Code | 2 (33.3) | Hollenbach 202184, Janevic 202085 |
| County | 1 (16.7) | Liu 201986 |
| Race/Ethnicity Variable Consideration | ||
| Within-Group Analysis | 1 (16.7) | Mayne 201889 |
| Covariate | 4 (66.7) | Dyer 202188, Hollenbach 202184, Janevic 202085, Liu 201986 |
| Effect Measure Modifier | 4 (66.7) | Dyer 202188, Janevic 202085, Liu 201986, Grady 200887 |
3.2. Outcomes:
Two studies assessed SMM as defined by the Center for Disease Control and Prevention 21 criteria as their outcome of interest.85,86 A study by Dyer et al examined all pregnancy-related deaths up to one year postpartum (Table 2).88 Two additional studies examined hypertensive disorders of pregnancy, which was defined as the presence of gestational hypertension or pre-eclampsia (Table 2).84,89 Lastly, Grady et al examined the relationship between residential segregation and hypertensive disorders of pregnancy, gestational diabetes, and eclampsia as precursors to low birth weight (Table 2).87
Table 2:
Summary of study findings
| Author & Publication Year | Measure of Structural Racism | Outcome | Sample Size | Study Region & Years of Observation | Racial/Ethnic Groups Analyzed | Findings |
|---|---|---|---|---|---|---|
|
| ||||||
| Dyer 202188 | Index of Concentration at the Extremes (ICE) Race and Income combined [Census-tract level] |
Pregnancy associated mortality Assessment: Maternal death records |
101,596 | Louisiana 2016–2017 | Non-Hispanic Black, Non-Hispanic White, Hispanic/Multiple/“Other” |
Concentrated deprivation (ICE tertile 1)
vs concentrated privilege (ICE tertile 3) Overall population: aRR=1.73, 95% CI: 1.02–2.93 aRR adjusted for Maternal Race=1.17, 95% CI: 0.62–2.19 Race/ethnicity-Specific: NA Moderate deprivation (ICE tertile 2) vs concentrated privilege (ICE tertile 3) Overall population: aRR=1.22, 95% CI: 0.71–2.07 aRR adjusted for Maternal Race=1.10, 95% CI: 0.63–1.92 Race/ethnicity-Specific: NA |
| Hollenbach 202184 | Historical Redlining [Zip code level] |
Pregnancy-associated hypertension Assessment: Electronic birth certificate database |
64,804 | New York State 2005–2018 | Not shown |
“Hazardous”
vs “Best” neighborhoods Overall population: OR(unadjusted)=1.26, 95% CI: 1.03–1.52 Race/ethnicity-specific: NA |
| Janevic 202085 | Index of Concentration at the Extremes (ICE) Race, income, and race and income combined [Zip code level] |
Severe Maternal Morbidity Assessment: CDC SMM Indicator Index 7 from hospital discharge records |
316,600 | New York City 2012–2014 | Black, Latinx, White, Asian |
ICE Race highest (Quintile 1)
vs lowest (Quintile 5) relative deprivation;* Overall population: aRD cases/100=0.3, 95%CI: 0.1–0.6 Black women: RD(unadjusted) cases/100=1.6, 95%CI: 0.4–2.9 Latinx women: RD(unadjusted) cases/100=1.3, 95%CI: 0.6–2.1 White women: RD(unadjusted) cases/100=0, 95%CI: −0.4–0.5 Asian women: RD(unadjusted) cases/100=0.9, 95%CI: 0.2–1.6 ICE Income highest (Quintile 1) vs lowest (Quintile 5) relative deprivation;* Overall population: aRD cases/100=0.4, 95% CI: 0.2– 0.6 Black women: RD(unadjusted) cases/100=1.1, 95%CI: 0.1–2.1 Latinx women: RD(unadjusted) cases/100=1.4, 95%CI: 0.8–2.0 White women: RD(unadjusted) cases/100=−0.2, 95%CI: −0.7–0.3 Asian women: RD(unadjusted) cases/100=−0.3, 95%CI: −0.8–0.2 ICE Race and Income combined highest (Quintile 1) vs lowest (Quintile 5) relative deprivation;* Overall population: aRD cases/100=0.4, 95% CI: 0.2–0.6 Black women: RD(unadjusted) cases/100=1.6, 95%CI: 0.4–2.9 Latinx women: RD(unadjusted) cases/100=1.6, 95%CI: 1.0–2.1 White women: RD(unadjusted) cases/100=0.3, 95%CI: 0.3–0.8 Asian women: RD(unadjusted) cases/100=1.0, 95%CI: 0.3–1.6 |
| Liu 201986 | Ratio of Black and white female unemployment rates, Ratio of Black and white female 4-year college education rates, Ratio of Black and white total incarcerated people [County level] |
Severe Maternal Morbidity Assessment: CDC SMM Indicator Index 7 from hospital discharge records |
244,854 | New York State 2011–2013 | Black, White |
High vs low employment inequity; Overall population: aOR=1.06, 95% CI:0.95–1.17 Race/ethnicity Specific: NA High vs low educational inequity; Overall population: aOR=1.47, 95%:1.17–1.85 Race/ethnicity Specific: NA High vs low incarceration inequity; Overall population: aOR=1.07, 95% CI: 0.90–1.27 Race/ethnicity Specific: NA |
| Mayne 201889 | Racial Residential Segregation (Gi* statistic) [Census-tract level] |
Hypertensive Disorder of Pregnancy Assessment: Electronic Health Records |
4,748 | Chicago, IL 2009–2013 | Black |
High vs low segregation; Black women: aOR=1.10, 95% CI: 0.82–1.46 Other racial/ethnic groups: NA Medium vs low segregation; Black women: aOR=1.09, 95% CI: 0.77–1.54 Other racial/ethnic groups: NA Associations moderated by neighborhood poverty (p(χ2)=0.002) [estimates not shown] |
| Grady 200887 | Racial residential segregation (local spatial segregation) [Census-tract level] |
Pregnancy-related diabetes Pregnancy-related hypertension Preeclampsia, eclampsia Assessment: Vital statistics birth records |
91,748 | New York City 2000 | Black, White |
A standard deviation increase in segregation; Black women: Pregnancy Related Hypertension aOR=1.10, 95% CI: 1.01–1.20 Difference in relative odds=1.45 White women: Estimates not shown [not statistically significant] Other racial/ethnic groups: NA |
aRR=Adjusted Risk Ratio; RD=Risk Difference; OR=Odds Ratio; aOR=Adjusted Odds ratio; aRD=Adjusted Risk Difference; CI=Confidence Interval
Results presented for extreme categories
3.3. Measures of structural racism
3.3.1. Index of Concentration at the Extremes
Two studies used the Index of Concentration at the Extremes (ICE) using data from the American Community Survey to assess spatial racial and economic polarization.85,88 Janevic et al assessed ICE-race, ICE-income, and ICE-race and income combined at the zip code level, while Dyer et al used the combined race and income ICE measure at the census tract level. ICE quantifies the degree to which individuals with extreme deprivation and privilege may concentrate within geographic units.90,91 ICE measures can assess the concentration of low-income versus high-income residents (ICE-income), racially marginalized (e.g. Black) versus most privileged (i.e. White) residents (ICE-race), and/or the combination of both—i.e. the concentration of low-income Black individuals versus high-income white residents (ICE-race and income combined). ICE measures range between −1 and 1, where values closer to −1 indicate that most/all residents in the given area are mostly deprived and values closer to 1 indicate that most/all residents in the given area are mostly privileged. ICE has been recommended for public health monitoring of structural inequities within places, as it captures the clustering of extreme deprivation/privilege.91
3.3.2. Historical redlining
One study included in this review used Home Owner’s Loan Corporation (HOLC) redlining maps from the 1930s at the zip code level.84 Redlining was a practice of grading neighborhoods where Black, other people of color, immigrant, and low-income individuals resided as “hazardous” and thus financially “risky”, while primarily White neighborhoods were regarded as “safe/best” for mortgage insuring, refinancing, and lending. 34 HOLC was a New Deal era initiative enacted to introduce economic recovery by providing economic assistance such as low-interest mortgages to homeowners at risk of foreclosure. In order to assess the condition of the homes in maintaining their financial value, HOLC commissioned local real estate agents to appraise properties within neighborhoods of every major city in the U.S., where they created color-coded “Residential Security” maps that rated neighborhoods into four grades; A-“Best”, B-“Still Desirable”, C-“Definitely Declining”, D-“Hazardous.”92 Neighborhoods labeled “hazardous” were colored red, while the “Best” neighborhoods were colored in green.34 This practice, subsequently adopted by both the Federal Housing Agency and the Department of Veteran Affairs, promoted and maintained racial residential segregation and extreme disinvestment of neighborhoods with a high proportion of minoritized residents.34,92,93
3.3.3. Racial residential segregation
Two of the studies included in the review assessed racial residential segregation as a proxy of structural racism.87,89 Mayne et al used the Getis-Ord Gi*statistic while Grady et al used a measure of local spatial segregation index to assess racial isolation.87,89 Both of these studies utilized data from the U.S. Census to construct their measures at the census tract level. The Gi*statistic is a z-score that signifies how the racial composition of a smaller geographic unit and its neighboring areas (e.g. census tract) differs from that of the average racial composition of the larger geographic unit within which they are contained (e.g. metropolitan statistical area).94 Z-scores greater than 1.96 indicate a statistically significant higher concentration of a racial group, whereas z-scores lower than −1.96 indicate a statistically significant absence of racial concentration within the smaller area, all compared to the larger geographic entity. The local spatial segregation index assesses segregation by measuring the degree to which a member of a racial group will interact with another racial group within their own or adjacent neighborhood.95 The lack of potential interaction indicates the presence of segregation. This measure is typically standardized and ranges from 0–1, with 0 indicating 100% potential interaction and 1 indicating 100% absence of potential interaction. Residential segregation is considered a prominent marker of structural racism that influences the social/physical/socioeconomic environments within neighborhoods where marginalized people reside.50,51
3.3.4. Other area-level measures of racial inequities
Only one study assessed multiple measures of structural racism at the county level.86 This study leveraged the American Community Survey and the Vera Institute of Justice In Our Own Backyard dataset 42 to quantify the racial inequities in female educational attainment, female employment, and incarceration (male and female combined) rates based on the Black to White population ratios in these county-level indicators. These measures indicate how structural racism shapes the differential distribution of power and privilege across multiple societal domains.96
3.4. Summary of findings
3.4.1. Links between structural racism and maternal outcomes
Across studies included, there was a general pattern that structural racism measures were associated with maternal morbidity and mortality. Findings depended on operationalization of structural racism, population-subgroups assessed, and covariates included in models. Below we describe associations in more detail.
One study from Louisiana found that higher spatial racial and economic polarization at the census-tract level, as defined by ICE-race and income combined, was associated with increased risk of pregnancy-associated mortality in partially adjusted models that accounted for maternal age, educational attainment, census tract-level percent of families living below poverty, and rurality (Table 2).88 However, the association was no longer significant with the inclusion of maternal race/ethnicity.88 Similarly, another study found that residing in zip codes with the highest relative deprivation using ICE-race, -income, and -race and income combined was associated with higher risk of SMM (Table 2).85 These associations were partially explained by hospital site of delivery, comorbidities, and socioeconomic factors.
A study assessing the link between racial residential segregation using the Gi* statistic and hypertensive disorders of pregnancy (HDP) found no significant associations when accounting for maternal characteristics and neighborhood poverty, but observed that for women living in socioeconomically deprived neighborhoods, greater racial residential segregation was associated with greater odds of HDP (Table 2).89 On the other hand, in neighborhoods with less deprivation, segregation was associated with lower odds of HDP. Another study examining racial residential segregation measured using the local spatial segregation index found that only among African American individuals, segregation was linked with higher odds of pregnancy-related hypertension after accounting for individual-level risk factors as well as neighborhood poverty (Table 2).87 These findings are supported by the results of another study in this review that documented significant associations between residing in historically redlined neighborhoods and increased odds of pregnancy-induced hypertension.84 However, associations reported in this study were not adjusted for any covariates (Table 2).
A study that examined multiple indicators of area-level structural racism reveled that among the measures used, only Black-White inequity in female educational attainment was associated with increased odds of SMM after accounting for individual and hospital-level characteristics (Table 2).86
3.4.2. Consideration of race/ethnicity in analyses and subsequent differential findings
Half of the studies in this review considered the birthing person’s race/ethnicity both as a control variable as well as an effect measure modifier.85,86,88 In assessing the degree to which ICE-race contributed to racial/ethnic inequities in risk of pregnancy-related mortality, Dyer et al found no differences.88 Similarly, Liu et al found no statistically significant interactions between county-level measures of structural racism and race/ethnicity in predicting SMM.86 On the other hand, Janevic et al found that in unadjusted models, risk differences associated with high relative deprivation proxied using ICE and SMM were the largest for Black and Latina women, compared to White individuals.85 Further analyses disentangling associations within Latina identified women revealed that Black Latina women had higher risk differences of SMM associated with ICE measures. In their investigation of the links between residing in historically redlined neighborhoods and pregnancy-related hypertension, Hollenbach et al only reported estimates that do not account for any covariates.84 However, for the primary outcome they considered (preterm birth), they controlled for both maternal and paternal race, and findings were only slightly attenuated. Finally, Mayne et al conducted a within-group analyses and examined relationships only among Black birthing people, while Grady et al used race/ethnicity stratified models to assess associations among Black and White women separately.87,89
3.4.3. Theoretical frameworks, pathways, and mechanisms discussed
Although not always explicitly stated, the majority of the studies included in this review contextualized structural racism as a fundamental cause of disease.28,85–89 Studies outlined that the impact of structural racism on these disparate health outcomes may be facilitated through multiple pathways. One such pathway discussed is the role it plays in shaping neighborhood environments and chronic stress burden to impact the distribution of clinical risk factors of adverse birthing outcomes. Such studies named historical discriminatory mortgage lending policies and redlining practices as the root of contemporary racial residential segregation.15,84,87–89 More specifically, Grady et al underscored that racial residential segregation is one “geospatial manifestation of racism,” which harms health by leading to concentrated poverty, systematic disinvestment, and poor physical and social attributes within racially segregated neighborhoods.87 Grady, Dyer, Mayne and Janevic et al also pointed to how in these neighborhoods, chronic stress arising from to exposure to physical/social disorder may cause physiological deterioration, elevating the risk of adverse birthing events.85–89 Grady et al and Dyer et al also highlighted that structural racism influences discriminatory social norms.87,88 A few of the studies made reference to the weathering hypothesis as one mechanism through which structural racism is embodied to influence racial/ethnic disparities in adverse maternal health outcomes.87,89,97 This hypothesis highlights how accumulation of racism-related stress throughout the life-course may lead to pre-mature biological aging among Black birthing people, exacerbating Black-White disparities in birthing outcomes.
Studies also highlighted how structural racism may lead to limited social support systems and depleted community resources, hindering the availability of protective resources against psychosocial stressors, and consequently increasing risk of adverse pregnancy-related outcomes.87,88 They also underscored that structural racism may determine both access to and the quality of the health facilities where pregnant people of color may receive care and give birth.85,87 Grady et al additionally outlined how structural racism may impact health through limited access to social mobility and that it may result in heightened police surveillance/violence within segregated neighborhoods.87
4. Discussion
This systematic review aimed to synthesize quantitative empirical studies that have assessed the link between measures of structural racism and adverse pregnancy-related outcomes in the United States. Studies identified and reviewed in the study add to our understanding of how structural racism shapes racial/ethnic disparities in maternal morbidity and mortality. One of the main findings of this review is the dearth of literature examining the relationship between structural racism and maternal morbidity/mortality, as only six studies qualified for the review. This indicates the degree to which these links are severely understudied in the epidemiologic literature, warranting the need of future studies that more comprehensively interrogate structural racism as the driver of racial/ethnic inequities in these outcomes. In addition to the limited number of studies included, due to heterogeneities in operationalizing structural racism, differences in the analytical strategies used, and variety of outcomes assessed, drawing solid conclusions regarding the relationship between structural racism and maternal morbidity/mortality is challenging. However, this review does confirm that depending on measures used and population sub-groups assessed, evidence suggests that structural racism has detrimental associations with adverse maternal health outcomes. It also highlights several theoretical and methodological considerations that should be addressed in future studies. Scholars have argued that theory is required to conduct sound epidemiology, and this is even more apparent when assessing health impacts of structural racism.16,17,21
Policy implications should be one of the main take-ways from studies that examine structural racism and its health-related consequences. Not engaging in this type of interpretation may result in reifying racial inequities as “natural,” inexorable, or beyond human control (despite the reality that racial inequity has been created by humans, e.g., through policies mentioned above). However, studies included in this review minimally discussed how the measures they used may inform long-term structural change. First, a majority of the studies included used indicators such as racial residential segregation using neighborhood compositional measures from administrative sources. Although racial residential segregation has been shown to be a fundamental driver of health inequities, scholars have argued that using compositional measures to indicate contextual factors may ignore the specific racist policies and processes through which racism continues to function.50,98,99 It has also been argued that since neighborhood compositional measures themselves are consequences of racism, they may be insufficient at proxying the construct as a whole.100 In recent years, studies have begun to investigate historical racist practices such as concentration of slavery 101 and redlining 61 in relation to present-day health outcomes. However, these encouraging efforts are limited in number, as only one study in this review assessed historical redlining as a measure of structural racism.84 The reliance on compositional measures to proxy structural racism may be due to the lack of historical data and policy databases that can be linked with individual-level health data. Thus, it is imperative that public health allocate resources to create policy databases, such as one recently introduced by Agenor et al and examine them in relation to health.102 It is also important to note that manifestations of structural racism may not always be explicitly spatial. As mentioned above, structural racism is embedded within various social, political, and cultural institutions, which makes it challenging to study using traditional place-based measures. Additionally, the mechanisms by which structural racism influences population health outcomes are complex and may also exceed geographic boundaries. Hence, it is crucial that epidemiologists collectively consider the different arms of structural racism that may or may not have spatial implications.
Second, in the studies included, there doesn’t appear to be a consensus nor discussion about how the level of geography at which racism is assessed may be more/less applicable to policy transformation. More granular geographic entities, such as census tracts, may allow researchers to examine the proximal environments surrounding individuals and generate evidence for local community-based interventions. However, since structural racism is entrenched within multiple policies and practices at several levels of geography, studies examining its manifestation at the city, county, and state levels may prove essential in dismantling its deeply ingrained nature.98,99 For example, recent high-profile murders of Black and Brown individuals at the hands of police and the subsequent public outcries condemning these killings have highlighted the role that local governing bodies, including city council, play in reinforcing police violence via practices such as budget allocation. Police abolition movements have shown how city budget dedicated to law-enforcement agencies often trump funds earmarked towards other essential sectors such as health services by several fold.103,104 Although seemingly race-neutral, it is evident that these budget allocations directly aide the disproportionate hyper-surveillance of communities of color, while depriving these same communities of essential health-promoting resources. Identifying this wide disparity in funding and its consequences, activists and advocates have identified reallocation of these funds towards community solutions as a sustainable way to reimagine community safety as well as to mitigate the negative health impacts of policing.105 However, the empirical evidence surrounding how such city-level policies that may contribute to racist practices are related to racial disparities in maternal health outcomes is virtually non-existent. Thus, future work should assess how specific laws and strategies at various levels of governance that disproportionately influence communities of color are related to adverse maternal health outcomes.
Addressing the ubiquity and multi-dimensionality of structural racism is another methodological challenge that has been minimally addressed in the studies included in the review. Single markers of structural racism, such as racial residential segregation are known to co-occur with other dimensions of structural racism such as socio-economic disenfranchisement, police violence, and mass incarceration.23,99,106 In fact, racially marginalized individuals, particularly Black people, bear the clustering of these indicators and may be multiply disadvantaged across the several domains within which structural racism manifests.106,107 In this review, only one study simultaneously investigated multiple markers of structural racism, while two others considered spatial polarization due to both race/ethnicity and income.85,86,88 Assessing only one dimension of structural racism may potentially underestimate the totality of ways that it influences adverse health outcomes through its different axes. It is also important to examine and address the ways through which these different dimensions of structural racism may work together and interact with one another to shape health outcomes. Relatedly, research must additionally assess the degree to which commonly used statistical frameworks are able to evaluate structural racism as a multi-dimensional construct. The one study that assessed multiple markers of structural racism used separate models to estimate the associations between these indicators and SMM.86 However, separately modeling the relationship between different dimensions of structural racism and health may severely underestimate its total impact on health. Assessing several markers together in the same model could also lead to violations such as multi-collinearity. Thus, it is important that future research consider novel methodological approaches, such as the recently proposed latent class structural racism measure by Chantarat et al, for a more comprehensive assessment of multiple indicators of structural racism.99,108
Discussion of proposed pathways through which structural racism gets biologically embedded to influence adverse maternal health outcomes was also minimal in the studies included. Particularly, most studies did not address how intersectionality may influence the embodiment of structural racism. Intersectionality, a term originating from Black feminist thought leaders and legal scholars, explicates how the intertwined nature of multiple axes of oppression such as racism, sexism, classism, ableism, homophobia, etc create unique sets of marginalization that are greater than their additive compilation.47–49,109 These interacting forces shape the availability of material and psychosocial resources that can protect against the adverse consequences of structural racism.110,111 They also influence the distribution of additional sources of adversity that may exacerbate its negative health impacts.112 One related example is the differential accruement of health benefits associated with socio-economic advancement among racially/ethnically marginalized individuals. The diminishing returns hypothesis states that due to racism, Black individuals do not receive the same degree of health improvement from higher socioeconomic status as do White people.70 Hence, given the complex within-group heterogeneities that may exist, the several processes that may moderate and/or mediate the embodiment of structural racism, and the intersectional nature of racial/ethnic disparities in maternal health, it is imperative that studies consider the role of interacting social inequities. In this review, only one study explicitly addressed intersectionality and gendered racism by using county-level indicators of Black-White inequities in female unemployment and educational attainment to proxy structural racism.86 This may also be because of the lack of data, especially from administrative sources measuring intersectional discrimination and individual-level stress/resilience. It could also be due to the lack of consensus on which quantitative approaches are adequate enough to represent how structural racism, along with other sources of social inequities influences adverse maternal health outcomes. This underscores the need for improved data sources and statistical approaches to more closely investigate how interacting social adversities and psychosocial mechanisms shape the health effects of structural racism.
Across the studies included, there was a lack of agreement on how to operationalize race/ethnicity as well as other covariates in regression models. Half of the studies included in this study considered race/ethnicity both as a control variable and as an effect measure modifier. A majority of the studies that included race/ethnicity in their models as an adjustment variable commented on the degree to which main-effect associations changed with the inclusion of this covariate. Studies that conceptualized race/ethnicity as an effect measure modifier examined the presence of a statistically significant interaction between race/ethnicity and the measure of racism used. One study exclusively assessed associations only among Black birthing people, while a second study used race/ethnicity stratified models to conduct within-group analyses.87,89 While there may be different theoretical/methodological justifications for choosing any one of these analytical strategies, it is important to explicitly state why investigators are choosing to control for race/ethnicity and/or treat it as an effect measure modifier. Studies should explain the theoretical basis for such analytic decisions, especially given increasing awareness of the socio-political construction of race within the racial health disparities literature.29 Similarly, there does not seem to be a consensus on whether behavioral and clinical risk factors should be included in models assessing the link between structural racism and maternal morbidity/mortality. Although not always explicitly stated, studies included in the review acknowledged that these risk factors are consequences of structural racism and precede the adverse maternal health outcomes considered. However, studies continue to statistically adjust for these factors in their models, which may underestimate the effect of structural racism on adverse maternal outcomes mediated through these indicators. Future studies should explicitly state the conceptualization and theory behind controlling for such variables within the context of similar investigations.
The need for longitudinal and prospective studies was another methodological issue highlighted in this review. Studies included in this study were primarily cross-sectional in design, which limits the ability to establish temporality. One study included in this review did use redlining maps from the 1930s to assess how racism was related to present-day obstetric complications.84 Such studies alleviate concerns around temporality and generate evidence on the far-reaching health impacts of racist policies. The use of cross-sectional data also raises a challenge in fully capturing the cumulative impact of structural racism across a birthing person’s lifespan and its subsequent implications for pregnancy and childbirth. Although some studies did make references to the weathering hypothesis and the accumulation of racism-related stress across the life-course, studies did not explicitly address this context in their analyses. In the broader literature and in this review, there are virtually no studies that examine how structural racism may shape adverse birth outcomes through the dysregulation of pre-conception health. Furthermore, only half of the studies included in this review analytically considered the health of birthing people prior to their pregnancies.85, 86 and 89 Given the extant theoretical explanations on the sensitivity of this particular period, it is imperative that future studies closely investigate the interplay between racism, preconception health, and adverse maternal health outcomes.113–117
This review has several limitations. First, there were only a few studies that met the inclusion criteria of this review. Additionally, given the complexity of structural racism and the vast list of possible search terms that may have been used to indicate its proxies, there may have been some articles that were not included in the screening and review process. Second, there was significant heterogeneity in the measures used to assess both structural racism and adverse maternal health outcomes. Third, it is possible that studies that found null associations between structural racism measures and maternal morbidity/mortality have not been published. Hence, it is not possible to make conclusive inference about the evidence on the link between racism and maternal morbidity/mortality. Lastly, this manuscript is focused on how structural racism operates within the U.S. to influence adverse maternal health outcomes. However, structural racism is not unique to the U.S. and is a global issue that continues negatively impact the health and well-being of marginalized individuals world-wide. Thus, future studies should assess how structural racism operates differently across various countries to influence population health outcomes.
Conclusion
Structural racism is a critical determinant of racial/ethnic disparities in adverse pregnancy-related complications. It influences the distribution of material and psychosocial stressors/resources, including healthy neighborhood amenities, safe, stable, and secure housing, chronic stress due to obvert and subvert discrimination, community resources, and social support networks, all of which directly and indirectly influence the degree to which racially/ethnically marginalized individuals are able to have healthy pregnancies and childbirth. This review highlighted the state of the empirical quantitative literature on structural racism and maternal morbidity/mortality. We outline proposed pathways, theoretical, and methodological considerations, as well as implications for future research, and offer a comprehensive conceptual framework which can be utilized in future studies.
Supplementary Material
Highlights:
Structural racism is the root cause of racial/ethnic health inequities.
Research on structural racism and maternal morbidity/mortality remains limited.
We offer a conceptual framework and conduct a systematic review on the links between structural racism and adverse maternal health outcomes.
Results show that structural racism has harmful implications for maternal morbidity/mortality.
Future research focusing on policy implications and interventions is needed.
Funding Statement:
This work was supported by the National Institute of Nursing Research (grant numbers 5R01NR017020–04 and 1R01NR020335–01).
Footnotes
Conflict of Interest Statement: The authors have no conflict of interest to disclose.
References:
- 1.Howell EA. Reducing Disparities in Severe Maternal Morbidity and Mortality. Clin Obstet Gynecol. 2018. doi: 10.1097/GRF.0000000000000349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tikkanen R, Gunja MZ, Fitzgerald M, Zephyrin L. Maternal Mortality and Maternity Care in the United States Compared to 10 Other Developed Countries; 2020. https://www.commonwealthfund.org/publications/issue-briefs/2020/nov/maternal-mortality-maternity-care-us-compared-10-countries.
- 3.Petersen EE, Davis NL, Goodman D, et al. Racial/Ethnic Disparities in Pregnancy-Related Deaths — United States, 2007–2016. MMWR Morb Mortal Wkly Rep. 2019;68(35):762–765. doi: 10.15585/mmwr.mm6835a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leonard SA, Main EK, Scott KA, Profit J, Carmichael SL. Racial and ethnic disparities in severe maternal morbidity prevalence and trends. Ann Epidemiol. 2019;33:30–36. doi: 10.1016/j.annepidem.2019.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirshberg A, Srinivas SK. Epidemiology of maternal morbidity and mortality. Semin Perinatol. 2017;41(6):332–337. doi: 10.1053/j.semperi.2017.07.007 [DOI] [PubMed] [Google Scholar]
- 6.Metcalfe A, Wick J, Ronksley P. Racial disparities in comorbidity and severe maternal morbidity/mortality in the United States: an analysis of temporal trends. Acta Obstet Gynecol Scand. 2018;97(1):89–96. doi: 10.1111/aogs.13245 [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Prevention and Control. Severe Maternal Morbidity in the United States.
- 8.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120(5):1029–1036. doi: 10.1097/AOG.0b013e31826d60c5 [DOI] [PubMed] [Google Scholar]
- 9.Creanga AA, Bateman BT, Kuklina EV, Callaghan WM. Racial and ethnic disparities in severe maternal morbidity: A multistate analysis, 2008–2010. Am J Obstet Gynecol. 2014;210(5):435.e1–435.e8. doi: 10.1016/j.ajog.2013.11.039 [DOI] [PubMed] [Google Scholar]
- 10.Ford ND, Cox S, Ko JY, et al. Hypertensive Disorders in Pregnancy and Mortality at Delivery Hospitalization — United States, 2017–2019. MMWR Morb Mortal Wkly Rep. 2022;71(17):585–591. doi: 10.15585/mmwr.mm7117a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain J, Moroz L. Strategies to reduce disparities in maternal morbidity and mortality: Patient and provider education. Semin Perinatol. 2017;41(5):323–328. doi: 10.1053/j.semperi.2017.04.010 [DOI] [PubMed] [Google Scholar]
- 12.Jain JA, Temming LA, D’Alton ME, et al. SMFM Special Report: Putting the “M” back in MFM: Reducing racial and ethnic disparities in maternal morbidity and mortality: A call to action. Am J Obstet Gynecol. 2018;218(2):B9–B17. doi: 10.1016/j.ajog.2017.11.591 [DOI] [PubMed] [Google Scholar]
- 13.Lindquist A, Knight M, Kurinczuk JJ. Variation in severe maternal morbidity according to socioeconomic position: A UK national case-control study. BMJ Open. 2013;3(6):1–8. doi: 10.1136/bmjopen-2013-002742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howland RE, Angley M, Won SH, et al. Determinants of Severe Maternal Morbidity and Its Racial/Ethnic Disparities in New York City, 2008–2012. Matern Child Health J. 2019;23(3):346–355. doi: 10.1007/s10995-018-2682-z [DOI] [PubMed] [Google Scholar]
- 15.Wang E, Glazer KB, Howell EA, Janevic TM. Social Determinants of Pregnancy-Related Mortality and Morbidity in the United States: A Systematic Review. Obstet Gynecol. 2020;135(4):896–915. doi: 10.1097/AOG.0000000000003762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krieger N. Epidemiology and the People’s Health: Theory and Context. New York: Oxford University Press; 2011. [Google Scholar]
- 17.Krieger N. Epidemiology and the web of causation: Has anyone seen the spider? Soc Sci Med. 1994. doi: 10.1016/0277-9536(94)90202-X [DOI] [PubMed] [Google Scholar]
- 18.Creanga AA, Bateman BT, Mhyre JM, Kuklina E, Shilkrut A, Callaghan WM. Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. Am J Obstet Gynecol. 2014;211(6):647.e1–647.e16. doi: 10.1016/j.ajog.2014.06.006 [DOI] [PubMed] [Google Scholar]
- 19.Guglielminotti J, Landau R, Wong CA, Li G. Patient-, Hospital-, and Neighborhood-Level Factors Associated with Severe Maternal Morbidity During Childbirth: A Cross-Sectional Study in New York State 2013–2014. Matern Child Health J. 2019;23(1):82–91. doi: 10.1007/s10995-018-2596-9 [DOI] [PubMed] [Google Scholar]
- 20.Carmichael SL, Abrams B, El Ayadi A, et al. Ways Forward in Preventing Severe Maternal Morbidity and Maternal Health Inequities: Conceptual Frameworks, Definitions, and Data, from a Population Health Perspective. Women’s Heal Issues. 2021:1–6. doi: 10.1016/j.whi.2021.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krieger N. Theories for social epidemiology in the 21st century: An ecosocial perspective. Int J Epidemiol. 2001. doi: 10.1093/ije/30.4.668 [DOI] [PubMed] [Google Scholar]
- 22.Williams DR, & Mohammed SA. Racism and health I: Pathways and scientific evidence. Am Behav Sci. 2013;57(8):1152–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 24.Alson JG, Robinson WR, Pittman L, Doll KM. Incorporating measures of structural racism into population studies of reproductive health in the United States: A Narrative Review. Heal Equity. 2021;5(1):49–58. doi: 10.1089/heq.2020.0081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams DR, Lawrence JA, Davis BA. Racism and Health: Evidence and Needed Research. Annu Rev Public Health. 2019;40(1):105–125. doi: 10.1146/annurev-publhealth-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gee GC, Ford CL. Structural racism and health inequities: Old Issues, New Directions. Du Bois Rev. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cogburn CD. Culture, Race, and Health: Implications for Racial Inequities and Population Health. Milbank Q. 2019;97(3). doi: 10.1111/1468-0009.12411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Phelan JC, Link BG. Is Racism a Fundamental Cause of Inequalities in Health? Annu Rev Sociol. 2015. doi: 10.1146/annurev-soc-073014-112305 [DOI] [Google Scholar]
- 29.Roberts DE. Fatal Invention : How Science, Politics, and Big Business Re-Create Race in the Twenty-First Century. New York: New Press; 2011. [Google Scholar]
- 30.Bonilla-silva E. Rethinking Racism: Toward a Structural Interpretation. Am Sociol Rev. 1997;62(3):465–480. [Google Scholar]
- 31.Jones CP. Levels of racism: A theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212–1215. doi: 10.2105/AJPH.90.8.1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crenshaw K, Gotanda NP, Peller G, Thomas K. Critical Race Theory: The Key Writings That Formed the Movement. New York: The New Press; 1995. [Google Scholar]
- 33.Bailey ZD, Feldman JM, Bassett MT. How Structural Racism Works — Racist Policies as a Root Cause of U.S. Racial Health Inequities. N Engl J Med. 2021. doi: 10.1056/nejmms2025396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rothstein R. The Color of Law: A Forgotten History of How Our Government Segregated America. First. New York; London: Liveright Publishing Corporation, a division of W.W. Norton & Company; 2017. [Google Scholar]
- 35.Johnson R. Children of the Dream: Why School Integration Works. New York: Hachette Book Group; 2019. [Google Scholar]
- 36.O’Brien R, Neman T, Seltzer N, Evans L, Venkataramani A. Structural racism, economic opportunity and racial health disparities: Evidence from U.S. counties. SSM - Popul Heal. 2020. doi: 10.1016/j.ssmph.2020.100564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ly DP, Lopez L, Isaac T, Jha AK. How Do Black-Serving Hospitals Perform on Patient Safety Indicators? Med Care. 2010;48(12):1133–1137. doi: 10.1097/mlr.0b013e3181f81c7e [DOI] [PubMed] [Google Scholar]
- 38.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (with CD). National Academies Press; 2003. doi: 10.17226/12875 [DOI] [PubMed] [Google Scholar]
- 39.Vable AM, Duarte CDP, Cohen AK, Maria Glymour M, Ream RK, Yen IH. Does the type and timing of educational attainment influence physical health? a novel application of sequence analysis. Am J Epidemiol. 2020. doi: 10.1093/aje/kwaa150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Duarte CDP, Salas-Hernández L, Griffin JS. Policy Determinants of Inequitable Exposure to the Criminal Legal System and Their Health Consequences among Young People. Am J Public Health. 2020. doi: 10.2105/AJPH.2019.305440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Skiba RJ, Michael RS, Nardo AC, Peterson RL. The color of discipline: Sources of racial and gender disproportionality in school punishment. Urban Rev. 2002. doi: 10.1023/A:1021320817372 [DOI] [Google Scholar]
- 42.Subramanian R, Henrichson C, Kang-Brown J. In Our Own Backyard: Confronting Growth and Disparities in American Jails.
- 43.Widra E, Herring T, 2021. States of Incarceration: the Global Context. Prison Policy Initiative. [Google Scholar]
- 44.Bor J, Venkataramani AS, Williams DR, Tsai AC. Police killings and their spillover effects on the mental health of black Americans: a population-based, quasi-experimental study. Lancet. 2018. doi: 10.1016/S0140-6736(18)31130-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alang S, McAlpine D, McCreedy E, Hardeman R. Police brutality and black health: Setting the agenda for public health scholars. Am J Public Health. 2017;107(5):662–665. doi: 10.2105/AJPH.2017.303691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alexander M. The New Jim Crow: Mass Incarceration in the Age of Colorblindness. New York: The New Press; 2010. [Google Scholar]
- 47.Crenshaw K. Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics. Univ Chic Leg Forum. 1989:139–167. [Google Scholar]
- 48.Crenshaw K. Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color. Stanford Law Rev. 1991. doi: 10.2307/1229039 [DOI] [Google Scholar]
- 49.Lorde A. Sister Outsider: Essays and Speeches. Trumansburg, NY: Crossing Press; 1984. [Google Scholar]
- 50.Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Rep. 2001. doi: 10.1016/S0033-3549(04)50068-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31(1):178–194. doi: 10.1093/epirev/mxp001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Diez Roux A V. Neighborhoods and health: where are we and were do we go from here? Rev Epidemiol Sante Publique. 2007. doi: 10.1016/j.respe.2006.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vinikoor-Imler LC, Messer LC, Evenson KR, Laraia BA. Neighborhood conditions are associated with maternal health behaviors and pregnancy outcomes. Soc Sci Med. 2011;73(9):1302–1311. doi: 10.1016/j.socscimed.2011.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.O’Campo P, Burke JG, Culhane J, et al. Neighborhood deprivation and preterm birth among non-Hispanic Black and white women in eight geographic areas in the United States. Am J Epidemiol. 2008. doi: 10.1093/aje/kwm277 [DOI] [PubMed] [Google Scholar]
- 55.Mehra R, Boyd LM, Ickovics JR. Racial residential segregation and adverse birth outcomes: A systematic review and meta-analysis. Soc Sci Med. 2017. doi: 10.1016/j.socscimed.2017.09.018 [DOI] [PubMed] [Google Scholar]
- 56.Mendez DD, Hogan VK, Culhane JF. Institutional racism, neighborhood factors, stress, and preterm birth. Ethn Heal. 2014. doi: 10.1080/13557858.2013.846300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mendez DD, Thorpe RJ, Amutah N, et al. Neighborhood racial composition and poverty in association with pre-pregnancy weight and gestational weight gain. SSM - Popul Heal. 2016;2(April):692–699. doi: 10.1016/j.ssmph.2016.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pickett KE, Collins JW, Masi CM, Wilkinson RG. The effects of racial density and income incongruity on pregnancy outcomes. Soc Sci Med. 2005;60(10):2229–2238. doi: 10.1016/j.socscimed.2004.10.023 [DOI] [PubMed] [Google Scholar]
- 59.Lane HM, Morello-frosch R, Marshall JD, Apte JS. Historical Redlining Is Associated with Present-Day Air Pollution Disparities in U.S. Cities. 2022. doi: 10.1021/acs.estlett.1c01012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Miranda ML, Maxson P, Edwards S. Environmental contributions to disparities in pregnancy outcomes. Epidemiol Rev. 2009;31(1):67–83. doi: 10.1093/epirev/mxp011 [DOI] [PubMed] [Google Scholar]
- 61.Krieger N, van Wye G, Huynh M, et al. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017. Am J Public Health. 2020. doi: 10.2105/AJPH.2020.305656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gazmararian JA, Adams MM, Pamuk ER. Associations between measures of socioeconomic status and maternal health behavior. Am J Prev Med. 1996. doi: 10.1016/s0749-3797(18)30353-2 [DOI] [PubMed] [Google Scholar]
- 63.Clark R, Anderson NB, Clark VR, & Williams DR. Racism as a stressor for African Americans. Am Psychol. 1999;54(10):805–816. [DOI] [PubMed] [Google Scholar]
- 64.Jahn JL, Krieger N, Agénor M, et al. Gestational exposure to fatal police violence and pregnancy loss in US core based statistical areas, 2013–2015. EClinicalMedicine. 2021;36. doi: 10.1016/j.eclinm.2021.100901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Goin DE, Gomez AM, Farkas K, et al. Occurrence of fatal police violence during pregnancy and hazard of preterm birth in California. Paediatr Perinat Epidemiol. 2021;35(4):469–478. doi: 10.1111/ppe.12753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hardeman RR, Chantarat T, Smith ML, Karbeah J, Van Riper DC, Mendez DD. Association of Residence in High-Police Contact Neighborhoods with Preterm Birth among Black and White Individuals in Minneapolis. JAMA Netw Open. 2021;4(12):1–12. doi: 10.1001/jamanetworkopen.2021.30290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Brondolo E, Gallo LC, Myers HF. Race, racism and health: Disparities, mechanisms, and interventions. J Behav Med. 2009;32(1):1–8. doi: 10.1007/s10865-008-9190-3 [DOI] [PubMed] [Google Scholar]
- 69.Williams DR and Collins C. US Socioeconomic and Racial Differences in Health: Patterns and Explanations, Annu Rev Sociol. 1995; 21(1), pp. 349–386. [Google Scholar]
- 70.Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60(1):191–204. doi: 10.1016/j.socscimed.2004.04.026 [DOI] [PubMed] [Google Scholar]
- 71.Hudson D, Sacks T, Irani K, Asher A. The price of the ticket: Health costs of upward mobility among African Americans. Int J Environ Res Public Health. 2020. doi: 10.3390/ijerph17041179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Johnson JD, Green CA, Vladutiu CJ, Manuck TA. Racial disparities in prematurity persist among women of high socioeconomic status. Am J Obstet Gynecol MFM. 2020;2(3):1–15. doi: 10.1016/j.ajogmf.2020.100104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brase P, MacCallum-Bridges C, Margerison CE. Racial inequity in preterm delivery among college-educated women: The role of racism. Paediatr Perinat Epidemiol. 2021;35(4):482–490. doi: 10.1111/ppe.12772 [DOI] [PubMed] [Google Scholar]
- 74.López L, Jha AK. Outcomes for whites and blacks at hospitals that disproportionately care for black medicare beneficiaries. Health Serv Res. 2013;48(1):114–128. doi: 10.1111/j.1475-6773.2012.01445.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167(11):1177–1182. doi: 10.1001/archinte.167.11.1177 [DOI] [PubMed] [Google Scholar]
- 76.Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016;215(2):143–152. doi: 10.1016/j.ajog.2016.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ona S, Huang Y, Ananth CV, Gyamfi-Bannerman C, Wen T, Wright JD, D’Alton ME and Friedman AM Services and payer mix of Black-serving hospitals and related severe maternal morbidity. Am J Obstet Gynecol. 221; 224(6), pp.605–e1. [DOI] [PubMed] [Google Scholar]
- 78.Sacks TK. Invisible Visits: Black Middle-Class Women in the American Healthcare System. Oxford University Press; 2019. [Google Scholar]
- 79.Saluja B, Bryant Z. How Implicit Bias Contributes to Racial Disparities in Maternal Morbidity and Mortality in the United States. J Women’s Heal. 2021;30(2):270–273. doi: 10.1089/jwh.2020.8874 [DOI] [PubMed] [Google Scholar]
- 80.Mena E, Bolte G. Intersectionality-based quantitative health research and sex/gender sensitivity: A scoping review. Int J Equity Health. 2019;18(1):1–11. doi: 10.1186/s12939-019-1098-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kuklina E V, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the united states. Obstet Gynecol. 2009;113(6):1299–1306. doi: 10.1097/AOG.0b013e3181a45b25 [DOI] [PubMed] [Google Scholar]
- 82.Davidson AJF, Park AL, Berger H, et al. Risk of severe maternal morbidity or death in relation to elevated hemoglobin A1c preconception, and in early pregnancy: A population-based cohort study. PLoS Med. 2020;17(5):1–18. doi: 10.1371/journal.pmed.1003104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Veritas Health Innovation. Covidence Systematic Review Software. 2016.
- 84.Hollenbach SJ, Thornburg LL, Glantz JC, Hill E. Associations between Historically Redlined Districts and Racial Disparities in Current Obstetric Outcomes. JAMA Netw Open. 2021;4(9):1–9. doi: 10.1001/jamanetworkopen.2021.26707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Janevic T, Zeitlin J, Egorova N, Hebert PL, Balbierz A, Howell EA. Neighborhood Racial And Economic Polarization, Hospital Of Delivery, And Severe Maternal Morbidity. Health Aff (Millwood). 2020;39(5):768–776. doi: 10.1377/hlthaff.2019.00735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Liu SY, Fiorentini C, Bailey ZD, Huynh M, McVeigh K, Kapan D. Structural Racism and Severe Maternal Morbidity in New York State. Clin Med Insights Women’s Heal. 2019;12(1–8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Grady SC, Ramírez IJ. Mediating medical risk factors in the residential segregation and low birthweight relationship by race in New York City. Heal Place. 2008;14(4):661–677. doi: 10.1016/j.healthplace.2007.10.011 [DOI] [PubMed] [Google Scholar]
- 88.Dyer L, Chambers BD, Crear-Perry J, Theall KP, Wallace M. The Index of Concentration at the Extremes (ICE) and Pregnancy-Associated Mortality in Louisiana, 2016–2017. Matern Child Health J. 2021. doi: 10.1007/s10995-021-03189-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mayne SL, Yellayi D, Pool LR, Grobman WA, Kershaw KN. Racial Residential Segregation and Hypertensive Disorder of Pregnancy among Women in Chicago: Analysis of Electronic Health Record Data. Am J Hypertens. 2018;31(11):1221–1227. doi: 10.1093/ajh/hpy112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Massey D. The Prodigal Paradigm Returns: Ecology Comes Back to Sociology. In: Does It Take A Village?: Community Effects on Children, Adolescents, and Families. ; 2001. [Google Scholar]
- 91.Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, Van Wye G. Public health monitoring of privilege and deprivation with the index of concentration at the extremes. Am J Public Health. 2016. doi: 10.2105/AJPH.2015.302955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nelson RK, Winling L, Marciano R, Connolly N. Mapping Inequality: Redlining in New Deal America.
- 93.Mitchell B, Franco J. HOLC “Redlining” Maps: The Persistent Structure of Segregation and Economic Inequality; 2018. [Google Scholar]
- 94.Getis A, Ord JK. The Analysis of Spatial Association by Use of Distance Statistics. Geogr Anal. 1992;24(3):189–206. doi: 10.1111/j.1538-4632.1992.tb00261.x [DOI] [Google Scholar]
- 95.Wong DWS. Modeling local segregation: A spatial interaction approach. Geogr Environ Model. 2002;6(1):81–97. doi: 10.1080/13615930220127305 [DOI] [Google Scholar]
- 96.Lukachko A, Hatzenbuehler ML, Keyes KM. Structural racism and myocardial infarction in the United States. Soc Sci Med. 2014;103:42–50. doi: 10.1016/j.socscimed.2013.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: A population-based test of the weathering hypothesis. Soc Sci Med. 1996. doi: 10.1016/0277-9536(95)00159–X [DOI] [PubMed] [Google Scholar]
- 98.Riley AR. Neighborhood Disadvantage, Residential Segregation, and Beyond—Lessons for Studying Structural Racism and Health. J Racial Ethn Heal Disparities. 2018;5(2):357–365. doi: 10.1007/s40615-017-0378-5 [DOI] [PubMed] [Google Scholar]
- 99.Hardeman RR, Homan PA, Chantarat T, Davis BA, Brown TH. Improving The Measurement Of Structural Racism To Achieve Antiracist Health Policy. Health Aff 2022;41(2):179–186. doi: 10.1377/hlthaff.2021.01489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sewell AA. The Racism-Race Reification Process. Sociol Race Ethn. 2016;2(4):402–432. doi: 10.1177/2332649215626936 [DOI] [Google Scholar]
- 101.Kramer MR, Black NC, Matthews SA, James SA. The legacy of slavery and contemporary declines in heart disease mortality in the U.S. South. SSM - Popul Heal. 2017;3(February):609–617. doi: 10.1016/j.ssmph.2017.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Agénor M, Perkins C, Stamoulis C, et al. Developing a Database of Structural Racism–Related State Laws for Health Equity Research and Practice in the United States. Public Health Rep. 2021;136(4):428–440. doi: 10.1177/0033354920984168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Vitale AS. The End of Policing. Brooklyn, NY; 2017. [Google Scholar]
- 104.Fassler E. 10 Largest US Cities Will Spend More on Police Than Public Health This Year. TRUTHOUT. 2021. [Google Scholar]
- 105.American Public Health Association. Addressing Law Enforcement Violence as a Public Health Issue.; 2018.
- 106.Lukachko A, Hatzenbuehler ML, Keyes KM. Structural racism and myocardial infarction in the United States. Soc Sci Med. 2014;103:42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chambers BD, Erausquin JT, Tanner AE, Nichols TR, Brown-Jeffy S. Testing the Association Between Traditional and Novel Indicators of County-Level Structural Racism and Birth Outcomes among Black and White Women. J Racial Ethn Heal Disparities. 2018;5(5):966–977. doi: 10.1007/s40615-017-0444-z [DOI] [PubMed] [Google Scholar]
- 108.Chantarat T, Van Riper DC, Hardeman RR. The intricacy of structural racism measurement: A pilot development of a latent-class multidimensional measure. eClinicalMedicine. 2021;40:1–7. doi: 10.1016/j.eclinm.2021.101092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Combahee River Collective, 1977. The Combahee River Collective Statement.
- 110.Ford CL, Airhihenbuwa CO. The public health critical race methodology: Praxis for antiracism research. Soc Sci Med. 2010;71(8):1390–1398. doi: 10.1016/j.socscimed.2010.07.030 [DOI] [PubMed] [Google Scholar]
- 111.Collins PH, Bilge S, 2016. Intersectionality (Key Concepts). Polity Press, Cambridge, UK. [Google Scholar]
- 112.Bowleg L. The problem with the phrase women and minorities: Intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. doi: 10.2105/AJPH.2012.300750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kramer MR, Hogue CJ, Dunlop AL, Menon R. Preconceptional stress and racial disparities in preterm birth: An overview. Acta Obstet Gynecol Scand. 2011. doi: 10.1111/j.1600-0412.2011.01136.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Entringer S, Buss C, Shirtcliff EA, et al. Attenuation of maternal psychophysiological stress responses and the maternal cortisol awakening response over the course of human pregnancy. Stress. 2010. doi: 10.3109/10253890903349501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30. doi: 10.1023/A:1022537516969 [DOI] [PubMed] [Google Scholar]
- 116.Mahrer NE, Guardino CM, Hobel C, Dunkel Schetter C. Maternal Stress before Conception Is Associated with Shorter Gestation. Ann Behav Med. 2021;55(3):242–252. doi: 10.1093/abm/kaaa047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Class QA, Khashan AS, Lichtenstein P, Långström N, D’Onofrio BM. Maternal Stress and Infant Mortality: The Importance of the Preconception Period. Psychol Sci. 2013. doi: 10.1177/0956797612468010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.