Gall stones are common but often do not give rise to symptoms. Pain arising from the gall bladder may be typical of biliary colic, but a wide variety of atypical presentations can make the diagnosis challenging. After a period of uncertainty in the 1980s, when operative techniques were challenged by drug treatment and lithotripsy, it is now widely accepted that symptomatic gallbladder stones should be treated by laparoscopic cholecystectomy. Clinical judgment and local expertise will greatly influence the management of bile duct stones, particularly if cholecystectomy is also required.
Asymptomatic gall stones are common and require no treatmentTypical symptoms include biliary colic—right upper quadrant pain, radiating to the back, and lasting less than 12 hoursSymptomatic gall stones are usually treated by laparoscopic cholecystectomy
Epidemiology of gall stones
In the United Kingdom about 8% of the population aged over 40 years have gall stones, which rises to over 20% in those aged over 60. Fortunately, 90% of these stones remain asymptomatic, but cholecystectomy is the most commonly performed abdominal procedure.
Risk factors for gall stones
Cholesterol stones
Obesity
High fat diet
Oestrogens (female, pregnancy, oral contraception)
Hereditary
Loss of bile salts (Crohn's disease, terminal ileal resection)
Impaired gall bladder emptying (such as truncal vagotomy, type 1 diabetes, octreotide, parenteral nutrition, and starvation or rapid voluntary weight loss)
Pigment stones
Haemolytic disease
Biliary stasis
Biliary infection
The incidence of gall stones varies widely, being greatly influenced by dietary intake, particularly of fat. For example, in Saudi Arabia gallstone disease was virtually unheard of 50 years ago, but, with increasing affluence and a Western type diet, gall stones are now as common there as in many Western countries. Genetic factors also contribute. The native Indian populations of Chile and Peru are highly susceptible, with a close to 100% lifetime risk of gall stones in their female population. Several risk factors have been identified, which relate to the two major stone types, cholesterol stones and pigment stones.
Pathogenesis
Gall stones form when the solubility of bilirubin or cholesterol is exceeded. Pigment stones arise in the gall bladder when there has been increased bilirubin production from breakdown of haemoglobin. Mixed stones contain both bilirubin and cholesterol and may be calcified. Precipitated bilirubin may form a nidus for subsequent cholesterol deposition.
Secondary pigment stones form in the bile duct as a consequence of obstruction or by accumulation around a small primary stone. These stones are associated with bacterial infection and arise by bacterial deconjugation of the bilirubin-glucuronide complex.
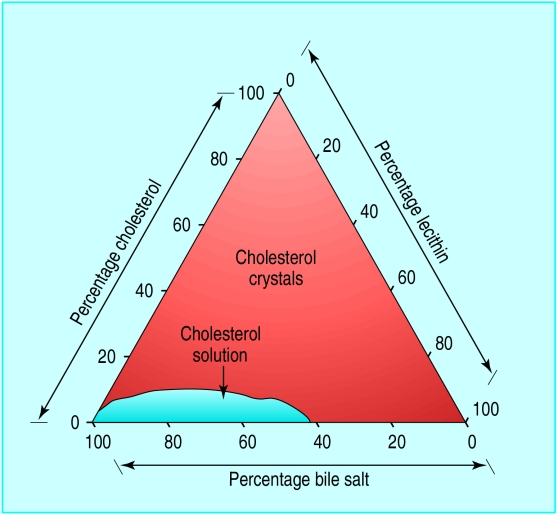
Cholesterol stones arise because of an imbalance in the mechanisms maintaining cholesterol in solution. Cholesterol is a hydrophobic molecule and is dispersed in micelles by the combined action of bile salts and lecithin. The risk of precipitation is directly related to cholesterol concentration and inversely to the concentrations of bile salts and lecithin, giving rise to a triangular coordinate. Increased cholesterol excretion is largely of dietary origin but may also result from changes in steroid metabolism associated with pregnancy, oral contraceptives, and obesity.
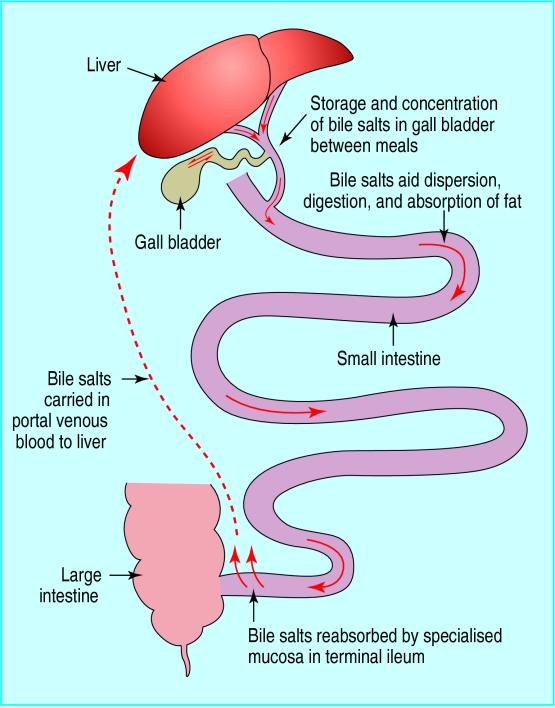
Bile salts are retrieved from the gut by the terminal ileum, and this enterohepatic circulation is essential for maintenance of the bile salt pool. The endogenous synthesis of bile salt is rate limited at a level much lower than its normal daily excretion by the liver. Many gastrointestinal diseases affect bile salt metabolism—in particular, Crohn's disease and surgical resection of the terminal ileum predispose people to gall stones.
Impaired gallbladder emptying predisposes to gall stones by increasing the time that material stays in the gall bladder, allowing excessive crystal growth. In addition, the dilating and flushing effect of fresh hepatic bile is lost when the gall bladder contracts poorly.
Symptoms associated with gall stones
Biliary colic is usually felt as a severe gripping or gnawing pain in the right upper quadrant. It may radiate to the epigastrium, or around the lower ribs, or directly through to the back. It may be referred to the lower pole of the scapula or the right lower ribs posteriorly. However, many variations on this pattern have been described, including retrosternal pain and abdominal pain only in the epigastrium or on the left side. Such symptoms, in the presence of gallbladder stones, merit consideration of cholecystectomy.
There may be difficulty when symptoms are less clear. In a year about 25% of the adult population consults a general practitioner for dyspeptic symptoms. As nearly 8% of these individuals will have asymptomatic gall stones, many patients with dyspeptic symptoms are given the label “gallstone dyspepsia.” A pattern of symptoms supposedly associated with gall stones has been described, but several careful studies of patients before and after cholecystectomy have failed to show any clear association with either a good or poor outcome. Since asymptomatic gall stones and dyspepsia are so common in the general populations, they often coexist. Dyspeptic symptoms may be too readily attributed to the presence of gall stones, leading to inappropriate and ineffective surgery. Not surprisingly, therefore, symptoms may persist in up to 20% of patients after cholecystectomy.
Symptoms associated with gall stones
Biliary colic
Right subcostal or epigastric pain radiating to back or lower pole of scapula lasting for 20 minutes to 6 hours
Associated with vomiting brought on by (any) food
May disturb sleep
Acute cholecystitis
Severe pain and tenderness in right subcostal region for >12 hours
Fever and leucocytosis
Complications
Gallbladder stones may be complicated by acute cholecystitis, mucocele, or empyema. These are difficult to distinguish clinically; a patient may present with an episode of acute cholecystitis that fails to resolve and at operation is found to have an empyema or a mucocele. In addition to symptoms of biliary colic, such patients have pain that is constant and lasts for more than 12 hours; they also have tenderness over the gall bladder, which may be palpable, and may have a fever and leucocytosis.
Symptoms of dyspepsia not associated with gall stones
| • Repeated belching | • Fullness after normal meals |
| • Inability to finish normal meals | • Abdominal distension (bloating) |
| • Fluid regurgitation | • Epigastric or retrosternal burning |
| • Nausea | • Vomiting (without biliary colic) |
Complications of bile duct stones include obstructive jaundice and acute pancreatitis.
Any patient with suspected complications of either gallbladder or bile duct stones should be referred for urgent specialist assessment and may well require immediate admission to hospital.
Diagnosis
Ultrasonography has replaced cholecystography as the diagnostic test for gall stones. About 95% of gallbladder stones will be detected by ultrasonography, which is cheap, quick, and harmless. If strong clinical suspicion of gall stones exist, and ultrasonography does not show stones, the test should be repeated. Other diagnostic tests are less sensitive and are rarely indicated.
Management
The management of gall stones depends on their position, either in the gall bladder or bile duct.
Gallbladder stones
The management of gallbladder stones is now relatively straightforward. Asymptomatic gallstones require no intervention as the risks of any procedure outweigh the potential benefits.
Options for treatment of symptomatic gallbladder disease
Laparoscopic cholecystectomy—Safe in specialist hands, rapid recovery,permanently effective, current gold standard
Open cholecystectomy—Traditional, painful, prolonged recovery, scar
Alternative therapies
Extracorporeal shock wave lithotripsy—Complex
Bile salt dissolution—Expensive
Percutaneous cholecyslithotomy—Leaves abnormal gall bladder in situ,high recurrence rate, suitable only for a few selected patients
In the 1980s dissatisfaction with the outcome of open cholecystectomy led to several alternative therapies such as extracorporeal shock wave lithotripsy and bile salt dissolution therapy. These treatments were restricted in their applicability and have been almost completely superseded by laparoscopic cholecystectomy. This procedure offers a more rapid recovery and return to work, much less abdominal scarring, and at least as good long term relief of symptoms as open cholecystectomy. In specialist hands almost all uncomplicated gallbladder stones can be dealt with laparoscopically, with minimal risk of injury to the bile duct.
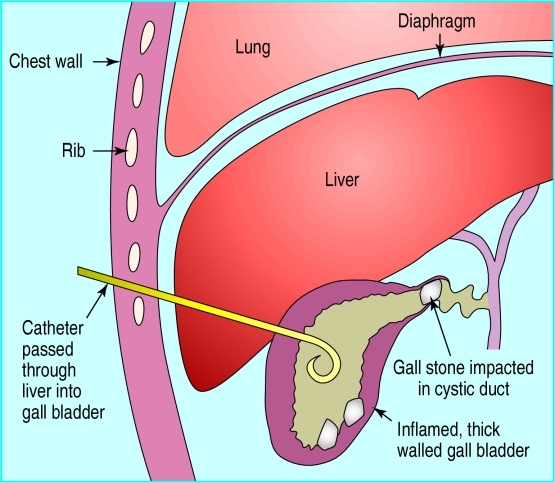
Complicated gallbladder stones—If complications arise (such as acute cholecystitis, mucocele, or empyema) cholecystectomy is performed. This will usually be by the laparoscopic approach, but up to 10% of operations have to be converted to laparotomy. In some elderly patients with acute presentation, percutaneous cholecystostomy is performed under ultrasound control to relieve the infection and avoid the morbidity of an emergency operation. Subsequently, the stones may be extracted percutaneously, leaving the gall bladder in place, or, if appropriate, cholecystectomy is performed.
Stones in the bile duct
Stones may migrate from the gall bladder into the bile duct. Cholangiography is performed before, during, or immediately after cholecystectomy to demonstrate the presence or absence of bile duct stones in patients with known risk factors. A cholangiogram may be obtained endoscopically, at operation, or by means of magnetic resonance imaging. Uncomplicated bile duct stones should be removed when they are detected, because of the high risk of complications such as acute pancreatitis, obstructive jaundice, or cholangitis if they are left in situ.
The management of asymptomatic duct stones is controversial. The traditional approach of open cholecystectomy with exploration of the common bile duct offers simplicity and widespread applicability and avoids exposing the patient to the risk of procedure related pancreatitis. Alternatives are laparoscopic cholecystectomy with endoscopic sphincterotomy and stone extraction either before or after cholecystectomy, or else laparoscopic exploration of the common bile duct. Currently practice varies according to the expertise available locally.
Acalculous biliary pain
The symptoms of biliary colic are characteristic but may occur in the absence of gall stones. In such cases a specialist must decide whether an operation to remove the gall bladder is appropriate, in the belief that symptoms are due to microscopic crystals (microlithiasis) or to a structural abnormality of the cystic duct.
Risk factors suggesting presence of bile duct stones at cholecystectomy for symptomatic gallbladder stones
Common bile duct dilated (>6 mm on ultrasound)
Recent abnormal levels of liver enzymes or bilirubin
History of acute pancreatitis
History of obstructive jaundice
Occasionally, biliary colic seems to be associated with a high pressure sphincter of Oddi, and symptoms may resolve after endoscopic sphincterotomy. Alternative explanations for so called acalculous biliary pain include irritable bowel syndrome with upper gastrointestinal manifestations (see previous article). Chronic pancreatitis must also be carefully excluded. Any decision to carry out a cholecystectomy for this condition should be made by a hepatobiliary specialist.
Gallbladder cancer
Gallbladder cancer is rare and usually asymptomatic until at an advanced stage. Usually it is associated with gall stones and may be discovered incidentally at operation. Suspicious features in a patient with biliary symptoms include weight loss, anaemia, persistent vomiting, and a palpable mass in the right upper quadrant. Such patients require urgent investigation. The prognosis is good if the disease is diagnosed at an early stage, but complete resection is often not possible because of the advanced stage at presentation.
Figure.
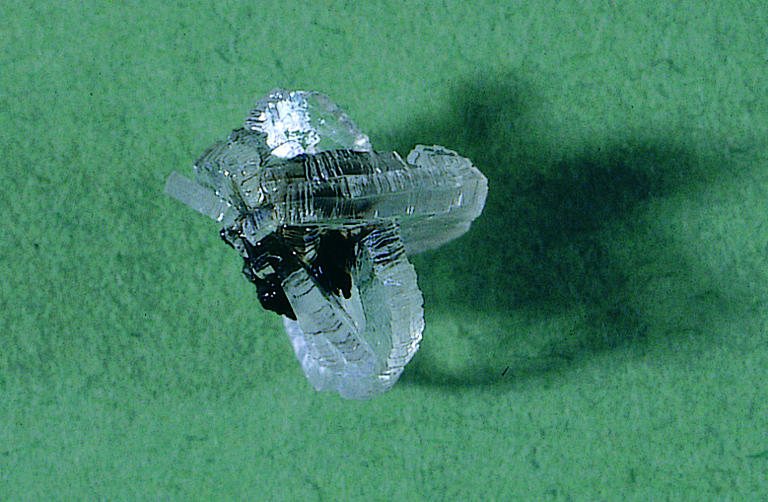
Mixed gall stone with bilirubin nucleus and attached clear cholesterol crystals
Figure.
Triangular coordinates relating solubility of cholesterol with concentrations of cholesterol, bile salts, and lecithin
Figure.
Enterohepatic circulation of bile salts. Each molecule circulates at least once for each meal
Figure.
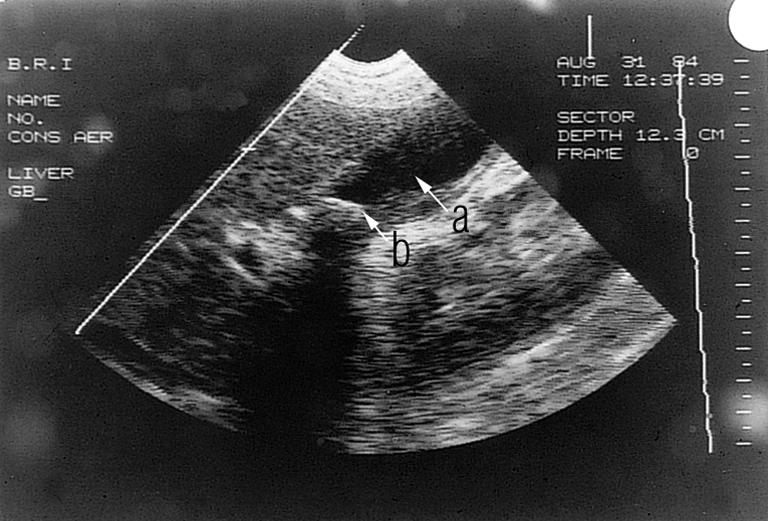
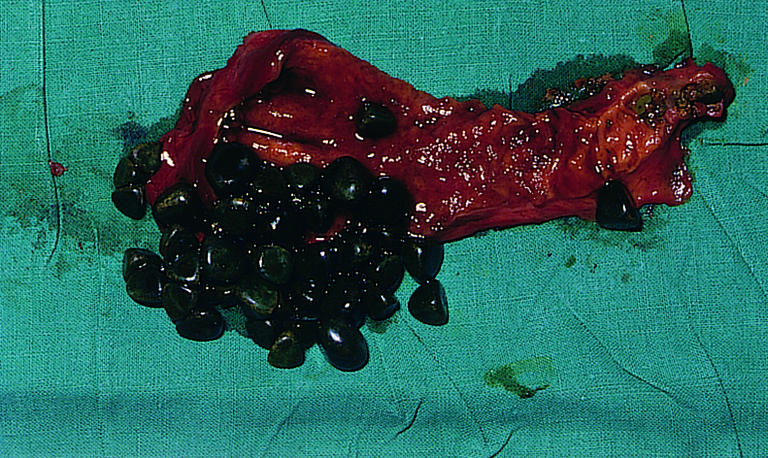
Top: Ultrasound image of gall bladder with dark area (a) representing gall bladder and multiple white echoes (b) representing stones. Bottom: The gall bladder after cholecystectomy with multiple small stones
Figure.
Percutaneous cholecystostomy for acute cholecystitis. Percutaneous drainage relieves the acute phase, allowing subsequent stone extraction via the drain track or cholecystectomy when inflammation has resolved
Figure.

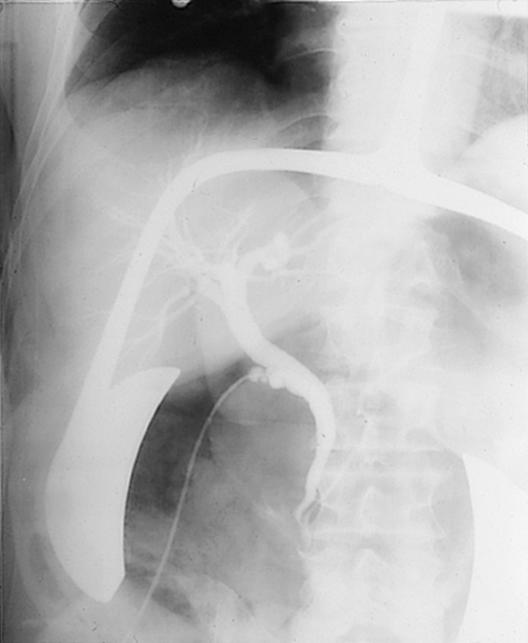

Cholangiography for duct stones. Top left: Endoscopic retrograde cholangiogram showing two stones in the bile duct (arrows). Top right: Operative cholangiogram (no stones). Bottom: Magnetic resonance cholangiogram obtained by 3-D reconstruction from a single breath hold acquisition
Acknowledgments
The diagram of triangular coordinates relating cholesterol solubility with bile salts and lecithin is adapted from Admirand WH, Small DM. J Clin Invest 1968;47:1043-52. The magnetic resonance cholangiogram was kindly provided by Dr C N Hacking.
Footnotes
C D Johnson is reader in surgery at the University Surgical Unit (816), Southampton General Hospital, Southampton.
The ABC of upper gastrointestinal tract is edited by Robert Logan, senior lecturer in the division of gastroenterology, University Hospital, Nottingham; Adam Harris, consultant physician and gastroenterologist, Kent and Sussex Hospital, Tunbridge Wells; J J Misiewicz, honorary consultant physician and joint director of the department of gastroenterology and nutrition, Central Middlesex Hospital, London; and J H Baron, honorary professorial lecturer at Mount Sinai School of Medicine, New York, USA, and former consultant gastroenterologist, St Mary's Hospital, London.