Graphical Abstract
Graphical Abstract.
In this issue of the journal, Aksu et al.1 report the results of a retrospective multicentre registry evaluating cardioneuroablation (CNA) for the treatment of atrioventricular block (AVB). Included patients had second- or higher-degree diurnal AVB, excluding Mobitz II type, deemed to be vagally induced. Atrioventricular block was persistent in 11% of cases, and on top of non-specific symptoms, all the patients except five had experienced syncope. The ablation procedure involved the right or left ganglia was guided by electroanatomical mapping and used extracardiac vagal stimulation in some cases. The primary endpoint was the absence of syncope and elimination of second- or higher-degree diurnal AVB during follow-up. The study population was relatively young: a total of 130 patients were included, with a median age of 34 years. Ablation procedures were effective in 96.2% of cases, with no major procedure-related complications. Of the five patients who failed to achieve the periprocedural result i.e. abortion of AV block, all received or already had a pacemaker. Median follow-up was 300 days. Recurrences were observed, despite achieving immediate success criteria, in 14% of cases. The use of intraprocedural vagal stimulation did not influence the primary endpoint. There was a tendency to achieve an immediate post-procedural success more often when the operator was more experienced. The existence of persistent AVB, older age, and comorbidities including atrial fibrillation, hypertension, and coronary artery disease was associated with the negative primary outcome i.e. syncope or higher-degree AV block recurrence.
The use of CNA for the treatment of AVB had been raised by earlier publications and merited multicentre evaluation.2,3 An increasing interest in this topic exists among electrophysiologists as CNA has shown promising results in treating very symptomatic patients with cardioinhibitory reflex syncope.4,5 The results of this relatively large registry therefore worth our attention. Nevertheless, as it stands, this report may generate ideas, but its outcomes should be treated with caution and cannot form the basis for expanded CNA recommendations.
Main reasons for being careful about PIRECNA registry results are related to the methodology of the present registry as follows:
It is a retrospective, multicentre registry involving 20 centres. The population, the inclusion criteria, the methodology of CNA, the accuracy in the assessment of symptoms, and the documentation of AVB before and during the follow-up are extremely heterogeneous and questionable, making interpretation of results uncertain. In particular, the reader has not been offered any adequate information about possible traumatic incidents, and symptom impact on the quality of life prior to decision to perform CNA. Further, the reason for ablation was non-specific symptoms including fatigue, irritability, lassitude, inability to concentrate, lack of interest, forgetfulness, dizziness feeling of warmth, light-headedness, dizziness, nausea, and sweating. These symptoms are hardly explained by intermittent AV block. In clinical practice, these patients do not appear to be common, and there is a risk of significant over-interpretation of such non-specific symptoms and their possible association with an intermittent conduction disorder often seen in otherwise young and trained people.
There is a discrepancy between the inclusion criteria, i.e. 2nd degree or advanced AV block and symptoms of ‘fatigue, irritability, lassitude, inability to concentrate, lack of interest, forgetfulness, dizziness feeling of warmth, light-headedness, dizziness, nausea, sweating, or syncope’, and the primary outcome, i.e. freedom from syncope and of any symptomatic diurnal AVB. The primary endpoint should have been consistent with the criteria used for patient inclusion, i.e. not only to demonstrate the disappearance of AV block but also to assess the improvement of subjective symptoms that led to decision to perform the procedure. In the absence of proven symptom improvement, CNA may cure the ECG, but not the patient.
From a pathophysiological point of view, it is very difficult to exclude an underlying intrinsic abnormality of AV node conduction. The normal outcome of electrophysiological study and the improvement of AV conduction after atropine infusion are not sufficient to exclude an intrinsic abnormality. An alternative and likely explanation is that vagal output simply unmasks an underlying AV node disease. This reasoning has important clinical consequences. Cardioneuroablation does not eliminate a conduction system disease, but rather eliminates the ECG manifestations of a concealed intrinsic AV node disease that remain as it is and will likely progress in the future to more severe forms.
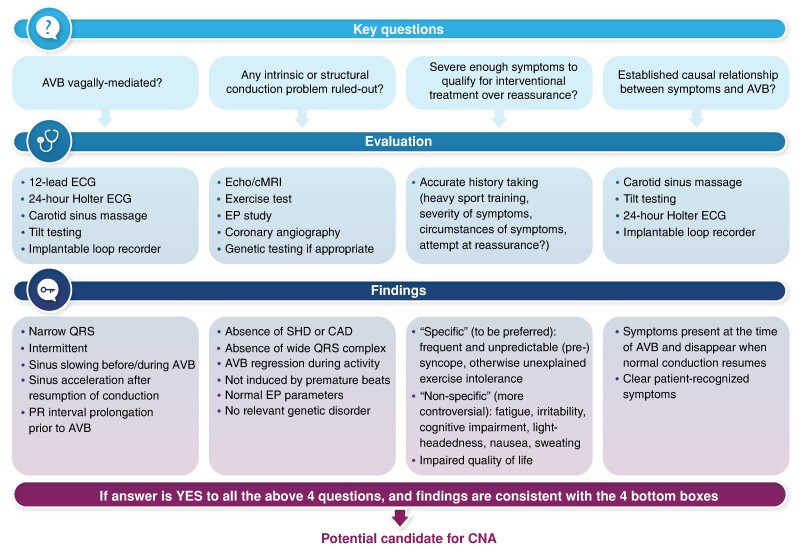
Considering the risk of a widespread use of this method in patients with undefined AV block aetiology and non-specific symptoms, we recommend following a clear diagnostic pathway for adequate selection of CNA candidates (Graphical Abstract). The aim of this pathway is to make it highly probable that the conductive disorder is vagal in nature, and that it is involved in severe symptoms with a clear cause-and-effect relationship.
Demonstration of the direct involvement of the parasympathetic system in the conduction disturbance is key. The characteristics of AVB episodes must be carefully analysed either during spontaneous episodes captured by prolonged ECG monitoring or during provocative tests. It is clear that a high vagal tone may be a cause of bradycardia, particularly in young and trained individuals.6–8 In these patients, there is usually permanent sinus bradycardia, on top of which episodes of paroxysmal first- or second-degree AVB of the Mobitz 1 type, or even more advanced second degree and complete AV block may occur. The analysis of sinus rate before the occurrence of the AV block is the clue for differentiating vagal AVB from intrinsic AVB.6,7,9 Slowing of the sinus node rate characterizes vagal AVB while the intrinsic form is generally precipitated by an increase in sinus rate and/or premature ventricular contractions. An increase of PR interval before the occurrence of blocked P waves is also the rule to follow before episodes can be classified as vagal AV block. The improvement of the AV node conduction properties after administration of atropine is well known and does not really help in decision-taking from a clinical point of view since vagal AVB is usually transient making the evaluation of the effect of atropine on the block unreliable as a clinical indicator.10 Intrinsic nodal AVB also respond to atropine, although a lesser extent, and there is no clear cut-off between intrinsic and extrinsic AVB. The most recent guidelines on cardiac pacing clearly advocate for pacing in Mobitz I AV block when symptoms are related to the AVB or the localization of the conduction disturbance is below the AV node. In fact, in more advanced AV block, vagal AV block should be recognized to avoid pacing.6,7
Any intrinsic or structural conduction problem should be ruled out by using the most appropriate tests. Rarely, vagal syncope or other types of reflex syncope are accompanied by paroxysmal AVB.11 If we were to consider an intervention for paroxysmal AVB, the characteristics in favour of vagal AVB are generally considered as indicatory for a non-interventional management.6,7,9,12
The symptoms must be severe enough to qualify for interventional therapy. Since hospital- and home-monitoring systems are on the rise, we see a danger in treating conduction abnormalities that are not related to a serious disease and are associated with non-specific symptoms. We recommend relying on symptoms that are specific of bradycardia rather than on non-specific symptoms. Quality of life should be clearly impaired.
Symptoms should be clearly related to the electrocardiographic abnormality. Due to the episodic nature of conduction disturbances, provocative tests are recommended as the first step like in the evaluation of unexplained syncope.13,14 The role of implantable loop recorder is important in inconclusive cases and should probably be part of the evaluation in most patients before decision to embark on interventional pathway.15
Conclusion
Since vagally induced AV block is often a benign condition, its interventional therapy should be aimed at symptom improvement in severely affected patients, in whom a clear cause–effect relationship can be established. Although the long-term effects of CNA are unknown, this method may seem attractive. However, well-designed trials should be performed before it is recommended for wider use. Until the results of such studies are available, we recommend to follow the official position of a recent joint document16 issued by the principal arrhythmia societies that state: ‘in patients with extrinsic (functional) sinus node disease and AV block, CNA should be treated as investigational, and if considered in severely symptomatic patients, after proven failure of non-invasive conventional therapies, it requires the setting of controlled trials’.
Contributor Information
Jean-Claude Deharo, Assistance Publique—Hôpitaux de Marseille, Centre Hospitalier Universitaire La Timone, Service de Cardiologie, France and Aix Marseille Université, C2VN, Cardiologie—Hôpital La Timone, Boulevard Jean Moulin, 13005 Marseille, France.
Artur Fedorowski, Department of Cardiology, Karolinska University Hospital, Stockholm, Sweden; Department of Medicine, Karolinska Institute, 171 64 Stockholm, Sweden; Department of Clinical Sciences, Lund University, 214 28 Malmö, Sweden.
Michele Brignole, Department of Cardiology, IRCCS Istituto Auxologico Italiano, Faint and Fall Research Centre, S. Luca Hospital, Piazzale Brescia 20, 20149 Milano, Italy.
References
- 1. Aksu T, Piotrowski R, Tung R, De Potter T, Markman TM, du Fay de Lavallaz J et al. Procedural and intermediate-term results of electroanatomical-guided CardioNeuroablation for treatment of suprahisian second or advanced-degree atrioventricular block: PIRECNA multicenter registry. Europace 2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pachon JC, Pachon EI, Pachon JC, Lobo TJ, Pachon MZ, Vargas RN et al. “Cardioneuroablation”—new treatment for neurocardiogenic syncope, functional AV block and sinus dysfunction using catheter RF-ablation. Europace 2005;7:1–13. [DOI] [PubMed] [Google Scholar]
- 3. Pachon-M JC, Ortencio FA, Pachon-M EI, Lobo T, Santillana-P TG, Pachon CT et al. Treatment of symptomatic functional atrioventricular block by cardioneuroablation as an alternative to pacemaker implantation. JACC Case Rep 2022;4:990–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Piotrowski R, Baran J, Sikorska A, Krynski T, Kulakowski P. Cardioneuroablation for reflex syncope: efficacy and effects on autonomic cardiac regulation—a prospective randomized trial. JACC Clin Electrophysiol 2023;9:85–95. [DOI] [PubMed] [Google Scholar]
- 5. Brignole M, Aksu T, Calò L, Debruyne P, Deharo JC, Fanciulli A et al. Clinical controversy: methodology and indications of cardioneuroablation for reflex syncope. Europace 2023;25:euad033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: developed by the task force on cardiac pacing and cardiac resynchronization therapy of the European Society of Cardiology (ESC) with the special contribution of the European Heart Rhythm Association (EHRA). Europace 2022;24:71–164. [DOI] [PubMed] [Google Scholar]
- 7. Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2019;74:e51–156. [DOI] [PubMed] [Google Scholar]
- 8. McClaskey D, Lee D, Buch E. Outcomes among athletes with arrhythmias and electrocardiographic abnormalities: implications for ECG interpretation. Sports Med 2013;43:979–91. [DOI] [PubMed] [Google Scholar]
- 9. Alboni P, Holz A, Brignole M. Vagally mediated atrioventricular block: pathophysiology and diagnosis. Heart 2013;99:904–8. [DOI] [PubMed] [Google Scholar]
- 10. Akhtar M, Damato AN, Caracta AR, Batsford WP, Josephson ME, Lau SH. Electrophysiologic effects of atropine on atrioventricular conduction studied by His bundle electrogram. Am J Cardiol 1974;33:333–43. [DOI] [PubMed] [Google Scholar]
- 11. Barra SNC, Providencia R, Paiva L, Nascimento J, Marques AL. A review on advanced atrioventricular block in young or middle-aged adults. Pacing Clin Electrophysiol 2012;35:1395–405. [DOI] [PubMed] [Google Scholar]
- 12. Brignole M, Arabia F, Ammirati F, Tomaino M, Quartieri F, Rafanelli M et al. Standardized algorithm for cardiac pacing in older patients affected by severe unpredictable reflex syncope: 3-year insights from the Syncope Unit Project 2 (SUP 2) study. Europace 2016;18:1427–33. [DOI] [PubMed] [Google Scholar]
- 13. Brignole M, Ammirati F, Arabia F, Quartieri F, Tomaino M, Ungar A et al. Assessment of a standardized algorithm for cardiac pacing in older patients affected by severe unpredictable reflex syncopes. Eur Heart J 2015;36:1529–35. [DOI] [PubMed] [Google Scholar]
- 14. Brignole M, Moya A, De Lange FJ, Deharo J-C, Elliott PM, Fanciulli A et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Kardiol Pol 2018;76:1119–98. [DOI] [PubMed] [Google Scholar]
- 15. Brignole M. Different electrocardiographic manifestations of the cardioinhibitory vasovagal reflex. Europace 2009;11:144–6. [DOI] [PubMed] [Google Scholar]
- 16. Aksu T, Brignole M, Calò L, Debrruyne P, Di Biase l, Deharo JC, et al. Joint document cardioneuroablation for the treatment of reflex syncope and functional bradyarrhythmias. A scientific statement of the European Heart Rhythm Association (EHRA) of the ESC, the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Society (APHRS) and the Latin American Heart Rhythm Society (LAHRS). Europace 2024. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]