Abstract
Lateral ankle sprain (LAS) is one of the most common types of injury in professional football (soccer) players with high risk of recurrence. The rehabilitation after LAS in professional football players is often still time-based and relies on anecdotal experience of clinicans. There is still a lack of utilization of criteria-based rehabilitation concepts after LAS in professional football. The aims of this clinical commentary are (1) to critically discuss the need for criteria-based rehabilitation concepts after LAS in professional football players, (2) to highlight the current lack of these approaches and (3) to present a novel clinical guideline-based rehabilitation algorithm. Short time-loss (15 days) and high recurrence rate (17%) raise the question of trivialization of LAS in professional football. Despite consequences for many stakeholders involved (players, teams, clubs, insurers), there is still a lack of of criteria-based, step-by-step approaches. The use of a criteria-based rehabilitation approach might reduce the high recurrence rate after LAS in professional football players and will lead, in turn, to increased long-term player availability. Practical experiences of he authors demonstrate the feasibility of such an approach. The effectiveness of this novel rehabilitation algorithm remains to be evaluated in future studies.
Level of Evidence: 5
Keywords: lateral ankle sprains, rehabilitation algorithm, professional football (soccer), decision-making, progression
INTRODUCTION
Injury to the ankle is considered to be the third most common type of injury in elite football (soccer) players.1 Fourteen to eighteen percent of all injuries occurring in professional football affect the ankle.2–4 The ligamentous apparatus is the most frequently injured anatomical structure of the ankle with 67-81% of all ankle injuries affecting the lateral ligament complex (LLC). With more than three fourths of ligament injuries affecting the lateral ligament complex,5,6 the lateral ankle sprain (LAS) is the most common isolated type of ankle injury.6 Up to 40% of all athletes have residual symptoms and develop chronic impairments after the initial LAS.5,7
Rehabilitation of LAS is often conducted in a time-based manner, with a reliance on clinicians’ anecdotal experience. The American Physical Therapy Association (APTA) appointed an expert panel to review the literature and identify recommendations and updates on the 2013 Clinical Practice Guidelines.8,9 The review8 collated and updated ankle injury management recommendations and their appropriate outcome measures. Contrary to other types of injuries (e.g. groin, Anterior Cruciate Ligament [ACL]), there are still no evidence-based step-by-step approaches to rehabilitation after LAS.10–13 Individual recommendations for the rehabilitation of ankle sprain injuries14 and broad consensus on their implementation do exist,15,16 but there is no published consensus that combines all recommendations into an evidence-based step-by-step approach.10 First return to competition (RTC) recommendations based on expert opinions exist,16–18 but there are no rehabilitation concepts that provide tests and criteria for progression within the rehabilitation phase. This lack of standardized rehabilitation approaches seems all the more surprising given the high prevalence, incidence, and recurrence rate of 6% up to 41% of LAS in professional football players,6,19 especially since the idea of criteria-based rehabilitation has already been established for rehabilitation after other types of injury (including ACL).11
Premature RTC and inadequate rehabilitation are considered to be one of the most important risk factors for a recurrent ankle sprain injury.16 High incidence and recurrence rates cause consequences for many stakeholders involved (players, teams, clubs, insurers) in terms of personal athletic development, the club´s financial burden, and treatment costs. A comprehensive testing and criteria-based approach aims to optimize the rehabilitation process while achieving the overall goal of reducing the recurrence rate of LAS in professional football players.
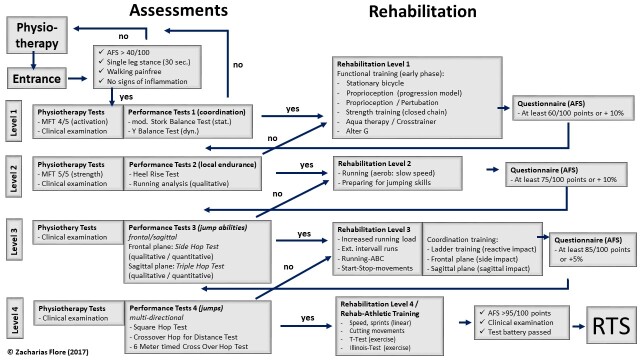
For this reason, the authors have developed a rehabilitation algorithm (Supplementary Material 1) that determines progression within rehabilitation by ensuring athletes pass specific standardized clinical examinations, performance tests, and achieve a specific questionnaire score (Ankle Function Score, AFS) defined for each rehabilitation level. The most current CPG assessments have been integrated into a step-by-step approach within the acute and subacute phase. However, there is still a lack of a CPG or recommended assessments within the ongoing RTS phases until RTC.
The primary aim of this clinical commentary is to critically discuss the need for criteria-based rehabilitation concepts after LAS in professional football. The secondary aim is to highlight the lack of theses approaches. The third aim is to present a criteria-based rehabilitation algorithm following lateral ankle sprains in professional football players through the rehabilitation phase until final clearance for return to competition.
LACK OF APPLICATION OF CONCEPTS AND THE NEED FOR CRITERIA-BASED REHABILITATION
While criteria-based approaches have been developed in recent decades for different body regions (knee, groin, thigh) and various types of injury (ACL, adductor injuries),11,12 rehabilitation after LAS commonly remains time-based and relies on the anecdotal experience of clinicians.13,16 Missing criteria for phase-sensitive progression within the rehabilitation phase as well as missing final test criteria for release to RTC may increase the risk of premature sports participation.13 The average time-loss after LAS in elite football players is 15 days and is thus often below the recovery time required for physiological ligament healing.20,21 This means that elite football players may return to competition too soon with incompletely healed ligaments.22 Premature RTC is considered to be one of the highest risk factors for re-injury.16 The recurrence rate after LAS in elite football players averages 17%.20 which is one of the highest recurrence rates of all sports injuries.13,16 The short time-loss (15 days) and high recurrence rate (17%) raise the question of trivialization of LAS injuries in elite footballers. A criteria-based rehabilitation program could manage rehabilitation and get the athlete back on the pitch as safely as possible, rather than as quickly as possible. The overall goal should be to lower the recurrence rate and reduce the risk of possible long-term consequences.13 Tassignon13 could not detect any study that included a criteria-based rehabilitation concept. There is a need to develop phase-sensitive and -specific multifactorial assessments and decision-making models.10,13 LAS is still trivialised and injured athletes are expected to return to competition as quickly as possible. The scientific evaluation of these concepts, in particular the objective assessment of their effectiveness in reduced risk of reinjury, could bring about a shift in coaches’ thinking regarding the risk of long-term sporting and health consequences for the athlete (Supplementary Material 2).
The authors have developed a criteria-based rehabilitation algorithm based on specific test and progression criteria. Due to the need for and the lack of criteria-based rehabilitation concepts after LAS in professional football, the algorithm was developed in 2017. The methology of its development is presented in supplemental material (Supplementary Material 3). This algorithm is presented in full step-by-step detail in the supplementary material. Progression through rehabilitation levels is controlled by passing predefined assessments. Superordinate domains which should be included in test batteries for decision-making of RTC based on expert opinions and consensus are already described.15,16,18 However, there is still a lack of tests and criteria to guide rehabilitation. Tassignon13 recommends integrating phase-sensitive domains in a dynamic rehabilitation model. Specific tests and criteria for secure phase transition are defined from a multitude of described assessments (Supplementary Material 1), which potentially correspond to the biomechanical requirements of the subsequent rehabilitation level and take into account the status of physiological ligament healing. The patient’s perspective is also taken into account by integrating a patient reported outcome/questionnaire (AFS) and a standardized clinical examination based on recommended clinical examination standards (ROM, strength, manual joint tests including the Anterior Drawer Test [ADT], Talar Tilt Test [TLT]; circumferential measurement). Players are progressed by integrating phase-specific functional performance tests (FPT). The FPTs represent the expected biomechanical requirements of the subsequent rehabilitation level and should thus ensure safe rehabilitation training (Supplementary Material 4 and 5). With this approach, the authors combine the individual assessments for the first time in an arrangement under progressive aspects and under consideration of physiological ligament healing. The rehabilitation algorithm is an evidence-based concept. It takes into account the current scientific recommendations derived from clinical practice guidelines23 and considers the application in everyday practice in professional football.
INTRODUCTION OF A NOVEL CRITERIA-BASED REHABILITATION ALGORITHM
Rehabilitation algorithm within the post-injury pyramid
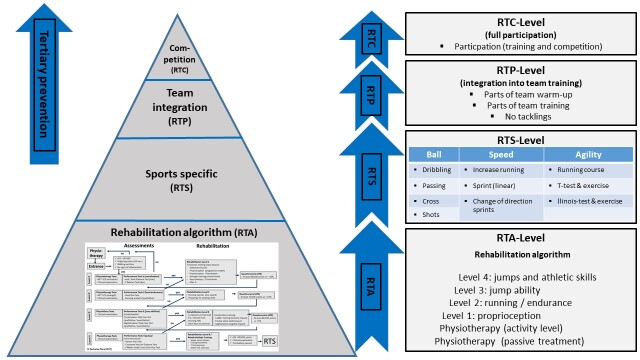
The rehabilitation algorithm is a concept consisting of four levels (Figure 1). As part of a post-injury phase (rehabilitation process), it forms the lowermost differentiated part of a post-injury pyramid (Figure 2). The prerequisite for progressing to a subsequent rehabilitation level is passing three assessments (achieving a level-dependent score in the patient reported outcome measure, passing a standardised clinical examination, and passing performance tests). The athlete remains at a rehabilitation level until each assessment for progression to the next level is passed.
The entire rehabilitation phase consists of four macro-phases (Return to Activity [RTA], Return to Sports [RTS], Return to Play [RTP], Return to Competition [RTC]). In the RTA phase, the greatest differentiation takes place in the entire rehabilitation process, taking into account the time-dependent wound healing phases. Sport-specific (football) training forms are the focus in the RTS phase. After the integration into team training (RTP), the athlete is released for unrestricted participation in competition (RTC).
Within the RTA level, each individual test battery for the phase transition and training form is in itself progressively structured. The approach respects the anatomical nature and biomechanical alignment of the ligament structures, the load tolerance at the respective stages of wound healing, and the load stimuli necessary for optimal healing (e.g. collagen synthesis through dosed tensile stimuli).
Figure 1. Rehabilitation algorithm.
Figure 2. Post injury pyramid.
Criteria-driven tests and examinations
The integration of three test tools (the AFS, clinical examination, performance tests) may help to ensure readiness for phase transition from multiple perspectives. The integration of a questionnaire (patient reported outcome measure) is generally recommended as a complement to performance testing.11,13,24 In so doing, subjective feedback is provided by the patient which can support the decision-making process alongside objective functional tests.25 A validated questionnaire can bridge the gap between subjective patient assessment and objective measurement parameters in the RTS process and should be part of a criteria-guided rehabilitation process.11 Integrating a standardized clinical examination ensures the testing of clinical criteria (range of motion (ROM), joint stability, signs of inflammation, muscle function tests, assessment of swelling) and enables progress monitoring during rehabilitation. Performance tests (proprioception and hop tests) are established standards for guiding rehabilitation and for final testing of readiness for RTC.26–28 Hop tests are frequently used performance measures.29–31 Functional performace tests are practical, cost-efficient, and can be applied quickly and easily in almost any clinical setting without much equipment.29,30,32,33
The Ankle Function Score (AFS)
One method for patient-centred assessment of readiness to return to sport is the use of patient reported outcomes /questionnaires.11,25 Most questionnaires only test the athlete’s physical or psychological readiness at the end of rehabilitation before the RTC. Hence, they are outcome measures and not designed for process evaluation.34 The AFS is a questionnaire consisting of five items (pain, instability, weight bearing, swelling, gait pattern). In total 100 points can be scored.35 Because of its scoring system, the AFS may enable objective and comparable sustainable progress monitoring to control the progression within rehabilitation. Therefore, the AFS is evaluative36 and can be used as an additional tool to the clinical examination and performance tests to assist in guiding and evaluating the rehabilitation process.37 The AFS is simple to use, quick to complete, and to evaluate. Therefore, it is suitable for daily practice, especially in competitive sports, to manage rehabilitation and process assessment.37
Clinical examination
Passing a standardized clinical examination is an essential component when it comes to making decisions on progression to a subsequent rehabilitation phase. Clinical Practice Guidelines find moderate evidence to classify LAS based on clinical findings of function, ligament laxity, pain, swelling, hemorrhaging, point tenderness and ankle motion.8 The clinical examination consists of manual ankle tests: Anterior Drawer Test (ADT) and Talar Tilt Test (TLT), manual muscle function tests [MFT], circumference measurement, as well as range of motion (ROM) assessments. The ADT and TLT are specific stability tests to examine the integrity and mechanical stability of the lateral ligaments. Moreover, they are also used in clinical examinations to monitor progress7,28 with high sensitivity from post injury day five.15,38 Muscle function tests (MFT) are suitable for determining muscle strength status and can also be used to monitor progress toward regaining strength abilities.39 They are standard tests of isometric muscle strength.28,40 A near full ROM is a prerequisite for subsequent training and movement sequences. As ROM restrictions (especially in the anterior direction)41,42 remain one of the most common deficits after LAS gradual improvement of ROM is an essential part of the clinical progression. Side to side difference in ROM should be less than 10 degrees of dorsiflexion to pass the clinical examination for Levels 1 and 2. Furthermore, ROM should be the same compared to the non-injured ankle to pass the criteria for progression to the ongoing levels. ROM is often hindered by persistent swelling. Swelling can negatively affect muscle, joint, and proprioception function18,43 and should be controlled especially in the early functional phase. The swelling should not be more than +1% compared to the previous measurement to check possible irritant reactions.
Functional performance tests
Functional performance tests (FPT), especially proprioception and hop tests, are established standards for assessing rehabilitation after sports injuries.29,31,44 FPT can objectively guide progression through rehabilitation and determine release for unrestricted participation.32,33,45 In the proposed algorithm, tests are arranged progressively, taking into account the phases of wound healing, loading capacities, and objectives of the training exercises of the subordinate training levels. Level 1 aims to train proprioceptive skills (sensory perception, afferentiation, “joint sense”) while avoiding biomechanical impulse stress on the lateral ligament complex. Thus, passing proprioception tests including the static modified Stork Balance Test and dynamic Y-Balance Test is a prerequisite for release into Level 1. The aim of Level 2 is a return to running. The heel rise test and qualitative running analysis are part of the functional testing for entering the second level. Taking into account the time-dependent progression of wound healing and integrity of the ligaments, the performance tests in Level 3 are increasingly more dynamic and include the Side Hop Test (SHT) and Triple Hop Test (THD). Passing highly dynamic multi-directional hop tests (Square Hop Test, Crossover Hop Test, modified 6m timed Crossover) is required for release into Level 4. The test sequence is designed to be progressive so that combined sagittal and frontal hops are performed first under high control (Square Hop Test), progressing to reduced control (Crossover Hop Test), and then under time pressure conditions (modified 6m timed Crossover). Because of familiarization aspects, the testing of high-dynamic jump tests in Levels 3 and 4 is initially conducted qualitatively. In this way, the quality of movement and the pain response can be assessed prior to quantitative testing and, if necessary, a potentially damaging/injurious quantitative test can be avoided. Passing the functional performance tests is determined by a Limb Symmetry Index (LSI) of the injured leg greater than 90% compared to the uninjured leg. The LSI is a useful and easy to perform assessment of lower limb function using the uninjured limb as a control.29
Table 1. Progression criteria and training exercises (examples, SM_ Fig. 3+4).
| Level | Progression criteria into the level | Training exercise (examples) |
|---|---|---|
| 1: Proprioception |
|
|
| 2: Running |
|
|
| 3: Jump abilities |
|
|
| 4: athletic skills (rehabilitation) |
|
|
| RTS: football-specific |
|
|
| RTP: re-integration (team training) |
|
|
| RTC: team training |
|
|
Only new exercises for each level added. Exercises from previous levels can be applied.
AFS, Ankle Function Score; RTP, Return to Play; RTS, Return to Sports; VBG,Verwaltungs Berufsgenossenschaft (German elite sports insurance)
DISCUSSION ON SPECIFIC COMPONENTS OF THE REHABILITATION ALGORITHM
Clinical Practice Guidelines within the algorithm
CPGs can be used to integrate the best evidence into clinical rehabilitation of LAS as they are an important move toward developing specific rehabilitation approaches. Relevant tests and assessments were used as progression criteria. While the CPGs summarize the best evidence of clinical assessments, the rehabilitation algorithm brings this best evidence together in how it is practically applied. The table (Supplementary Material 6) summarizes similarities and differences between the most recent CPG (2021) and the rehabilitation algorithm presented herein, and demonstrates the justification for it´s integration.
Questionnaires / AFS
The AFS is an evaluative instrument that can guide the course of rehabilitation.36,37 Specific benchmarks were set at each phase transition (40, 60, 75, 85, 95) based on our experience in accordance with the literature. The AFS was not explicitly developed for process evaluation after LAS injuries in elite football, but it is particularly suitable for daily use in professional sports. The authors recommend the evaluation of the use of the AFS as a prognostic and evaluative tool for process control after LAS injury in elite football players.
Clinical examination
A standardized clinical examination consists of both ROM and muscle strength assessments and measurements of effusion and laxity. ROM is often limited after LAS injury and should be restored within two weeks post-injury.46,47 Manual therapy is recommended to restore ROM.48 Unrestricted ROM is required for testing and training.
The integration of muscle strength tests is recommended due to impairments in muscle function (strength, reaction time), especially of the peroneal muscles.38,49 Reduced muscle functioning of the peroneus muscles may affect the risk of re-injury due to its ankle protection function.38 It is recommended to test muscle function with a dynamometer in order to produce objective outcomes.15,50 However, manual muscle testing procedures are used by the authors for practical reasons. Dynamometers are expensive and not available in every clinical setting. A manual muscle test can offer an alternative to objective measurement of progression.39 Various cut-offs are proposed to check different strength abilities at each level.
In addition, the ADT and TLT are used to assess ligament integration, stability, and laxity of the ankle. The ADT and TLT are manual ankle tests to assess Anterior Talo-Fibular Ligament (ATFL) [ADT] and Calcaneo-Fibular Ligament (CFL) [TLT], the most commonly injured ligaments in the ankle joint.7,13 The ADT and TLT are recommended to be integrated in an ankle assessment7,28 with specifity of 0.67-1.00 and sensitivity of 0.50-0.97, respectively.15,38,51–53 Current clinical guidelines recommend the use of the Reverse anterolateral drawer test (RALDT) and anterolateral talar palpation in addition to the ADT. Even though it has limited accuracy and reliability the ADT is still one of the most commonly utilized tests for ankle sprain assessment.8 The ADT shows the most accuracy when assessed five days post injury.15,38 For this reason, the authors are integrating ADT and TLT for the first time after the acute phase as a complementary assessment tool for transition to Level 1. The authors use a (+) system to objectively assess the laxity during the rehabilitation progression similar to Johnson,54 based on recommendations of grading of Rammelt.55
Functional Performance Tests (FPT)
The integration of functional performance tests (FPT) to assess lower limb function after injury has been recommended elsewhere.29,31–33,45,56 Functional performance tests are aimed at the basic (fundamental) requirements that an athlete must meet in order to perform their sports.26 Noyes56 described the principle of functional rehabilitation using a jump test battery in the early 1990s. Since then, a variety of functional tests have been developed and evaluated.
Proprioception tests assess general somato-sensory abilities (postural control, balance), while hop tests assess motor control in a more dynamic (multidirectional) environment. While Read52 describes the general comparability of test results due to inconsistent implementation and standards, Davies57 criticizes the ability of individual jump tests to measure performance and outcome of rehabilitation and refers to the lack of biomechanical evaluation studies.57,58 Kotsifaki investigated the biomechanical loads in different joints for common hop tests which is fundamental work to specify the inclusion of hop tests in specific rehabilitation programs due to biomechanical loads which affect individual joints.59,60 Future studies will have to evaluate which loads or directions affect the ankle and its lateral ligament complex in the tests that are used in this algorithm, and whether they exceed the current load capacity (status of healing).
In this algorighm, FPTs are mostly used as criteria for a final test battery at the end of rehabilitation as a decision aid for clearance to RTC.17 The use of phase-sensitive FPTs lacks or phase-sensitive tests have not been evaluated in terms of their phase-specific use (sensitivity; specifity).13 The authors integrate phase-specific FPTs that test the biomechanical requirements of the rehabilitation level to be entered, taking into account time-dependent physiological healing. The training forms of the rehabilitation levels also follow the principle of physiological healing. The tests check the ability to perform the upcoming training skills in advance to ensure safe training.
For example, proprioception tests in Level 1 check somato-sensory abilities. These abilities are fundamental and should be restored as soon as possible for the further course of rehabilitation.14 Proprioception testing and training are low-impact and can therefore be included early in functional training.
Level 2 marks the transition from closed-chain training (e.g. weight-bearing) to open-chain running training. The HRT is a closed-chain test for assessing the calf-muscle strength and endurance61 whilst the qualitative running analysis assesses the ability to run in an open-chain manner. Running is a fundamental movement pattern and is therefore an essential part (milestone) of rehabilitation. A qualitative running analysis is recommended to assess lower limb injury function11,15 and therefore integrated into the rehabilitation algorithm.
The authors integrate several hop tests in Levels 3 and 4. These are valid individually to assess the management of lower limb injuries with a reliability and specificity of 0.66-0.97 and 0.80-0.92 respectively.26,30,58,62 The hop direction is chronological from frontal (SHT), to sagittal (THD), to multidirectional under progressing conditions. The arrangement of the hop tests takes into account the anatomical location of the most frequently injured ligament structures (ATFL, CFL) of the ankle as well as the status of physiological healing.63
Some of the utilzed FPTs are modified. These are intended to improve the tests for the ankle sprain rehabilitation setting. A modification of FPTs in terms of their targeted use is recommended by Caffrey.45
Limb Symmetry Index
The LSI is a simple method to obtain a prediction of the side-to-side difference in the lower limbs in FPTs. Several authors emphasize the advantages of the methodology in the clinical setting, as it is practical and can be used without software calculation.29,64 The LSI is increasingly discussed critically as it underestimates potential performance deficits, evokes questions about the accuracy of the methology and overlooks “true deficits” in supposedly easy performance tests.44 The use of LSI for quantifying the results of performance tests has mainly been evaluated in ACL patients or healthy individuals. Few LSI results are reported for performance testing after ankle injuries, which highlights both the need for normative data for performance testing in elite football players after ankle injuries and their LSI results. The authors integrate the LSI into the assessment of the performance tests, especially because of its applicability as a simple tool to quantify the test results, while being aware (and mindful) of its limitations. Ultimately, the use of LSI remains debatable for assessing lateral differences in the lower limbs after injury.
RTS-Level: Interval Kicking Progression (IKP)
Arundale65 has recommended a return to ball training at the earliest possible point of time for football players. Returning to the ball after injury can have a motivating effect and support the rehabilitation process.65 However, it must be considered that not every injured body site can be evaluated in the same way: As football is played with the feet, the ball training directly impacts the injured structure. Therefore, special attention should be devoted to a patient wth an ankle sprain during ball training. Impacts of several thousand Newtons can be generated on the foot/ankle during kicks.66–68 Incorrectly hit balls, especially under fatigued conditions at the end of a training session, can hyperextend the capsular ligamentous apparatus and lead to renewed microtrauma. The authors suggest using different ball types (e.g. volley ball, soft ball) to allow ball training without affecting the healing status negatively. Impacts on the foot/ankle during kicking have been described in several studies.66–68 So far, there are no step-by-step approaches for specific types of injury taking into account biomechanical impacts.65 For this reason, we recommend orientation to an IKP with attention to clinical responses after rehabilitation training. This makes the standardized clinical examination, which is also part of the rehabilitation algorithm for this reason, all the more important. The authors view a too-soon return to ball training after LAS injury critically.
RTP phase: lack of criteria in the end stage of rehabilitation
While the rehabilitation algorithm can steer the rehabilitation in the acute and sub-acute phase (RTA level) well through its differentiated approach by phase-sensitive testing, taking into account the temporal wound healing phases and load stability of the tissue and ligaments, the standardization of the rehabilitation during the RTS phase is made significantly more difficult by the start of ball training. Currently, there are no football-specific (kicking) tests, nor criteria for football-specific stress progression. Therefore, rehabilitation from this point on until reintegration into team training (RTC) remains anecdotal or experience-based despite all efforts to make it as objective as possible. The difficulty of objectification beyond this phase is made evident by the lack of Clinical Practice Guidelines beyond the subacute phase.8 Taking into account biomechanical impacts and their integration into a progressive rehabilitation program, kicking test batteries could be an important component of future RTC concepts and could close the currently existing gap between the subacute phase (RTA/RTS level) and the return to unrestricted team training (RTC).
CONCLUSIONS & KEY POINTS
The high recurrence rate (17%) with short time-loss (15 days) after LAS in elite football players raises the question of trivialization and highlights the need for criteria-based rehabilitation concepts rather than traditional time-based approaches. There is still a lack of criteria-based step-by-step approaches to guide rehabilitation. However, CPGs lack sport-specific tests and assessments especially in the subacute and ongoing phase for RTC decision-making.
The presented rehabilitation algorithm is the first to attempt to correlate individual assessments and combine them into a self-contained progressive approach taking into account evidence-based CPGs. Early utilization of this algorithm demonstrate its feasibility. The extent to which this rehabilitation algorithm can sustainably reduce the recurrence rate after LAS in elite football players remains to be evaluated in future studies.
Corresponding author
Zacharias Flore
University of Kent, School of Sport and Exercise Sciences
Kapellenstraße 8a
39104 Magdeburg, Germany
zf43@kent.ac.uk
+4915203090096
Supplementary Material
References
- Epidemiology of injuries in professional football: a systematic review and meta-analysis. López-Valenciano A., Ruiz-Pérez I., Garcia-Gómez A.., et al. 2020Br J Sports Med. 54(12):711–718. doi: 10.1136/bjsports-2018-099577. doi: 10.1136/bjsports-2018-099577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Injury incidence and injury patterns in professional football: the UEFA injury study. Ekstrand J., Hägglund M., Waldén M. 2011Br J Sports Med. 45(7):553–558. doi: 10.1136/bjsm.2009.060582. doi: 10.1136/bjsm.2009.060582. [DOI] [PubMed] [Google Scholar]
- A prospective epidemiological study of injuries in four English professional football clubs. Hawkins R. D., Fuller C. W. 1999Br J Sports Med. 33(3):196. doi: 10.1136/bjsm.33.3.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An examination of injuries in major league soccer. The inaugural season. Morgan B.E., Oberlander M.A. 2001Am J Sports Med. 29:426–430. doi: 10.1177/03635465010290040701. [DOI] [PubMed] [Google Scholar]
- Return to play after a lateral ligament ankle sprain. D'Hooghe P., Cruz F., Alkhelaifi K. 2020Curr Rev Musculoskelet Med. 13(3):281–288. doi: 10.1007/s12178-020-09631-1. doi: 10.1007/s12178-020-09631-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Time-trends and circumstances surrounding ankle injuries in men's professional football: an 11-year follow-up of the UEFA Champions League injury study. Waldén M., Hägglund M., Ekstrand J. 2013Br J Sports Med. 47(12):748–753. doi: 10.1136/bjsports-2013-092223. doi: 10.1136/bjsports-2013-092223. [DOI] [PubMed] [Google Scholar]
- Understanding acute ankle ligamentous sprain injury in sports. Fong D. T., Chan Y. Y., Mok K. M., Yung P. S., Chan K. M. 2009Sports Med Arthrosc Rehabil Ther Technol. 1(14):14. doi: 10.1186/1758-2555-1-14. doi: 10.1186/1758-2555-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ankle stability and movement coordination impairments: Lateral ankle ligament sprains Revision 2021. Martin R. L., Davenport T. E., Fraser J. J.., et al. 2021J Orthop Sports Phys Ther. 51(4):CPG1–CPG80. doi: 10.2519/jospt.2021.0302. doi: 10.2519/jospt.2021.0302. [DOI] [PubMed] [Google Scholar]
- Ankle stability and movement coordination impairments: ankle ligament sprains. Martin R. L., Davenport T. E., Paulseth S., Wukich D. K., Godges J. J., Orthopaedic Section American Physical Therapy Association 2013J Orthop Sports Phys Ther. 43(9):A1–A40. doi: 10.2519/jospt.2013.0305. doi: 10.2519/jospt.2013.0305. [DOI] [PubMed] [Google Scholar]
- Acute Ankle sprain management: An umbrella review of systematic reviews. Gaddi D., Mosca A., Piatti M.., et al. Jul 7;2022 Front Med (Lausanne) 9:868474. doi: 10.3389/fmed.2022.868474. doi: 10.3389/fmed.2022.868474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. Myer G.D., Paterno M.V., Ford K.R., Quatman C.E., Hewett T.E. 2006J Orthop Sports Phys Ther. 36(6):385–402. doi: 10.2519/jospt.2006.2222. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- Return to sport after criteria-based rehabilitation of acute adductor injuries in male athletes: A prospective cohort study. Serner A., Weir A., Tol J. L.., et al. 2020Orthopaedic Journal of Sports Medicine. 8(1):12. doi: 10.1177/2325967119897247. doi: 10.1177/2325967119897247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Criteria-based return to sport decision-making following lateral ankle sprain injury: a systematic review and narrative synthesis. Tassignon B., Verschueren J., Delahunt E.., et al. 2019Sports Med. 49(4):601–619. doi: 10.1007/s40279-019-01071-3. [DOI] [PubMed] [Google Scholar]
- Rehabilitation of the ankle after acute sprain or chronic instability. Mattacola C. G., Dwyer M. K. 2002J Athl Train. 37(4):413–429. [PMC free article] [PubMed] [Google Scholar]
- Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Delahunt E., Bleakley C. M., Bossard D. S., et al. 2018Br J Sports Med. 52(20):1304–1310. doi: 10.1136/bjsports-2017-098885. doi: 10.1136/bjsports-2017-098885. [DOI] [PubMed] [Google Scholar]
- Lack of consensus on return-to-sport criteria following lateral ankle sprain: A systematic review of expert opinions. Wikstrom E. A., Mueller C., Cain M. S. 2020J Sport Rehabil. 29(2):231–237. doi: 10.1123/jsr.2019-0038. doi: 10.1123/jsr.2019-0038. [DOI] [PubMed] [Google Scholar]
- Bloch H., Klein C., Kühn N., Luig P. Return to competition – Test manual for assessment of the ability to play after an acute lateral ankle sprain injury. VBG; Hamburg: [Google Scholar]
- Return to sport decisions after an acute lateral ankle sprain injury: introducing the PAASS framework-an international multidisciplinary consensus. Smith M.D., Vicenzino B., Bahr R.., et al. 2021Br J Sports Med. 55(22):1270–1276. doi: 10.1136/bjsports-2021-104087. doi: 10.1136/bjsports-2021-104087. [DOI] [PubMed] [Google Scholar]
- Prevalence and risk factors of ankle sprain among male soccer players in Tabuk, Saudi Arabia: A cross-sectional study. Amer H., Mohamed S. 2020The Open Sports Sciences Journal. 13(19):27–33. doi: 10.2174/1875399X02013010027. doi: 10.2174/1875399X02013010027. [DOI] [Google Scholar]
- Time-loss and recurrence of lateral ligament ankle sprains in male elite football: A systematic review and meta-analysis. Flore Z., Hambly K., De Coninck K., Welsch G. 2022Scand J Med Sci Sports. 32(12):1690–1709. doi: 10.1111/sms.14217. doi: 10.1111/sms.14217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soft tissue healing and its impact on rehabilitation. Houglum P. 1992J Sport Rehabil. 1(1):19–39. doi: 10.1123/jsr.1.1.19. [DOI] [Google Scholar]
- Epidemiology of injuries in male and female youth football players: A systematic review and meta-analysis. Robles-Palazón F. J., López-Valenciano A., De Ste Croix M., et al. 2022J Sport Health Sci. 11(6):681–695. doi: 10.1016/j.jshs.2021.10.002. doi: 10.1016/j.jshs.2021.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Which functional tests and self-reported questionnaires can help clinicians make valid return to sport decisions in patients with chronic ankle instability? A narrative review and expert opinion. Picot B., Hardy A., Terrier R., Tassignon B., Lopes R., Fourchet F. May 26;2022 Front Sports Act Living. 4:902886. doi: 10.3389/fspor.2022.902886. doi: 10.3389/fspor.2022.902886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Return to play after an ankle sprain: guidelines for the podiatric physician. Richie D.H., Izadi F.E. 2015Clin Podiatr Med Surg. 32(2):195–215. doi: 10.1016/j.cpm.2014.11.003. doi: 10.1016/j.cpm.2014.11.003. [DOI] [PubMed] [Google Scholar]
- National Athletic Trainers' Association position statement: conservative management and prevention of ankle sprains in athletes. Kaminski T.W., Hertel J., Amendola N., Manske 2013J Athl Train. 48(4):528–545. doi: 10.4085/1062-6050-48.4.02. doi: 10.4085/1062-6050-48.4.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triple-hop distance as a valid predictor of lower limb strength and power. Hamilton R. T., Shultz S. J., Schmitz R. J., Perrin D. H. 2008J Athl Train. 43(2):144–151. doi: 10.4085/1062-6050-43.2.144. doi: 10.4085/1062-6050-43.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Functional performance testing for power and return to sports. Manske R., Reiman M. 2013Sports Health. 5(3):244–250. doi: 10.1177/1941738113479925. doi: 10.1177/1941738113479925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Analysis of muscle activity and ankle joint movement during the side-hop test. Yoshida M., Taniguchi K., Katayose M. 2011J Strength Cond Res. 25(8):2255–2264. doi: 10.1519/JSC.0b013e3181ec86d5. doi: 10.1519/JSC.0b013e3181ec86d5. [DOI] [PubMed] [Google Scholar]
- Functional performance testing following knee ligament injury. Clark N. C. 2001Physical Therapy in Sport. 2(2):91–105. doi: 10.1054/ptsp.2001.0035. [DOI] [Google Scholar]
- Knee stability and movement coordination impairments: knee ligament sprain. Logerstedt D. S., Snyder-Mackler L., Ritter R. C., Axe M. J., Godges J. J., Orthopaedic Section of the American Physical Therapist Association 2010J Orthop Sports Phys Ther. 40(4):A1–A37. doi: 10.2519/jospt.2010.0303. doi: 10.2519/jospt.2010.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The non-injured leg can be used as a reference for the injured leg in single-legged hop tests. Vereijken A., van Trijffel E., Aerts I., Tassignon B., Verschueren J., Meeusen R. Jul 1;2021 Int J Sports Phys Ther. 16(4):1052–1066. doi: 10.26603/001c.25758. doi: 10.26603/001c.25758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reliability of lower extremity functional performance tests. Bolgla L. A., Keskula D. R. 1997J Orthop Sports Phys Ther. 26(3):138–142. doi: 10.2519/jospt.1997.26.3.138. doi: 10.2519/jospt.1997.26.3.138. [DOI] [PubMed] [Google Scholar]
- Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Reid A., Birmingham T. B., Stratford P. W., Alcock G. K., Giffin J. R. 2007Phys Ther. 87(3):337–349. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- Validity and responsiveness of the ankle function score after acute ankle injury. van der Wees P., Hendriks E., van Beers H., van Rijn R., Dekker J., de Bie R. 2012Scand J Med Sci Sports. 22(2):170–174. doi: 10.1111/j.1600-0838.2010.01243.x. doi: 10.1111/j.1600-0838.2010.01243.x. [DOI] [PubMed] [Google Scholar]
- The prognosis of ankle sprains. de Bie R. A., de Vet H. C., van den Wildenberg F. A., Lenssen T., Knipschild P. G. 1997Int J Sports Med. 18(4):285–289. doi: 10.1055/s-2007-972635. [DOI] [PubMed] [Google Scholar]
- Sprunggelenksinstabilität. Rehabilitation. Rückkehr zum Sport. et al. 2012GOTS-Expertenmeeting: Sprunggelenksinstabilität :79–84. https://sport-ortho.de/files/Bilder-und-Dokumente/Dokumente/GOTS-Expertenmeeting%202012_PE.pdf
- van der Wees P. J. Evaluation of evidence-based clinical guidelines in physical therapy : ankle sprain as case example. Datawyse / Universitaire Pers Maastricht; [DOI] [Google Scholar]
- Acute ankle sprain in athletes: Clinical aspects and algorithmic approach. Halabchi F., Hassabi M. Dec 18;2020 World J Orthop. 11(12):534–558. doi: 10.5312/wjo.v11.i12.534. doi: 10.5312/wjo.v11.i12.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wieben K. Muskelfunktion. Prüfung und klinische Bedeutung. Thieme Verlag; Stuttgart: [Google Scholar]
- The standing heel-rise test for ankle plantar flexion: criterion for normal. Lunsford B. R., Perry J. 1995Phys Ther. 75(8):694–698. doi: 10.1093/ptj/75.8.694. doi: 10.1093/ptj/75.8.694. [DOI] [PubMed] [Google Scholar]
- Systematic review of motor control and somatosensation assessment tests for the ankle. Bertrand-Charette M., Dambreville C., Bouyer L. J., Roy J. S. Jul 6;2020 BMJ Open Sport Exerc Med. 6(1):e000685. doi: 10.1136/bmjsem-2019-000685. doi: 10.1136/bmjsem-2019-000685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. Gribble P. A., Hertel J., Plisky P. 2012J Athl Train. 47(3):339–357. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effect of peripheral afferent alteration of the lateral ankle ligaments on dynamic stability. Myers J. B., Riemann B. L., Hwang J. H., Fu F. H., Lephart S. M. 2003Am J Sports Med. 31(4):498–506. doi: 10.1177/03635465030310040401. [DOI] [PubMed] [Google Scholar]
- A critical analysis of limb symmetry indices of hop tests in athletes after anterior cruciate ligament reconstruction: A case control study. Gokeler A., Welling W., Benjaminse A., Lemmink K., Seil R., Zaffagnini S. 2017Orthop Traumatol Surg Res. 103(6):947–951. doi: 10.1016/j.otsr.2017.02.015. doi: 10.1016/j.otsr.2017.02.015. [DOI] [PubMed] [Google Scholar]
- The ability of 4 single-limb hopping tests to detect functional performance deficits in individuals with functional ankle instability. Caffrey C., Docherty C. L., Schrader J., Klossner J. 2009J Orthop Sports Phys Ther. 39(11):799–806. doi: 10.2519/jospt.2009.3042. doi: 10.2519/jospt.2009.3042. [DOI] [PubMed] [Google Scholar]
- Aktuelle und neue konzepte in der behandlung akuter außenbandverletzungen des sprunggelenkes - current and new concepts in the treatment of lateral ligament sprains in ankle sistorsions. Best R., Brüggemann P., Petersen W., Rembitzki I., Ellermann A., Gösele-Koppenburg A., Liebau C. 2011Deutsche Zeitschrift für Sportmedizin. 62(3):57–62. [Google Scholar]
- Some conservative strategies are effective when added to controlled mobilisation with external support after acute ankle sprain: a systematic review. Bleakley C. M., McDonough S. M., MacAuley D. C. 2008Aust J Physiother. 54(1):7–20. doi: 10.1016/s0004-9514(08)70061-8. doi: 10.1016/s0004-9514(08)70061-8. [DOI] [PubMed] [Google Scholar]
- Effectiveness of exercise therapy and manual mobilisation in ankle sprain and functional instability: a systematic review. van der Wees P. J., Lenssen A. F., Hendriks E. J., Stomp D. J., Dekker J., de Bie R. A. 2006Aust J Physiother. 52(1):27–37. doi: 10.1016/s0004-9514(06)70059-9. doi: 10.1016/s0004-9514(06)70059-9. [DOI] [PubMed] [Google Scholar]
- Eccentric plantar-flexor torque deficits in participants with functional ankle instability. Fox J., Docherty C. L., Schrader J., Applegate T. 2008J Athl Train. 43(1):51–54. doi: 10.4085/1062-6050-43.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manual muscle testing: does it meet the standards of an adequate screening test? Bohannon R. W. 2005Clin Rehabil. 19(6):662–667. doi: 10.1191/0269215505cr873oa. doi: 10.1191/0269215505cr873oa. [DOI] [PubMed] [Google Scholar]
- Anterolateral talar palpation: A complementary test for ankle instability. Gomes J. L. E., Soares A. F., Bastiani C. E., de Castro J. V. 2018Foot Ankle Surg. 24(6):486–489. doi: 10.1016/j.fas.2017.05.006. [DOI] [PubMed] [Google Scholar]
- Evaluating and differentiating ankle instability. Gribble P. A. 2019J Athl Train. 54(6):617–627. doi: 10.4085/1062-6050-484-17. doi: 10.4085/1062-6050-484-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An accuracy evaluation of clinical, arthrometric, and stress-sonographic acute ankle instability examinations. Wiebking U., Pacha T.O., Jagodzinski M. 2015Foot Ankle Surg. 21(1):42–48. doi: 10.1016/j.fas.2014.09.006. doi: 10.1016/j.fas.2014.09.006. [DOI] [PubMed] [Google Scholar]
- Comparison of a lateral hop test versus a forward hop test for functional evaluation of lateral ankle sprains. Johnson M. R., Stoneman P. D. 2007J Foot Ankle Surg. 46(3):162–174. doi: 10.1053/j.jfas.2006.12.007. doi: 10.1053/j.jfas.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Frische außenbandruptur am oberen sprunggelenk. Rammelt S., Richter M., Walther M. 2017Leitlinien Unfallchirurgie. AWMF(012-022):22. [Google Scholar]
- Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Noyes F.R., Barber S.D., Mangine R.E. 1991Am J Sports Med. 19(5):513–518. doi: 10.1177/036354659101900518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- Is it time we better understood the tests we are using for return to sport decision making following ACL reconstruction? A critical review of the hop tests. Davies W. T., Myer G. D., Read P. J. 2020Sports Med. 50(3):485–495. doi: 10.1007/s40279-019-01221-7. doi: 10.1007/s40279-019-01221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Better reporting standards are needed to enhance the quality of hop testing in the setting of ACL return to sport decisions: a narrative review. Read P., Mc Auliffe S., Wilson M.G., Myer G.D. 2021Br J Sports Med. 55(1):23–29. doi: 10.1136/bjsports-2019-101245. doi: 10.1136/bjsports-2019-101245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vertical and horizontal hop performance: Contributions of the hip, knee, and ankle. Kotsifaki A., Korakakis V., Graham-Smith P., Sideris V., Whiteley R. 2021Sports Health. 13(2):128–135. doi: 10.1177/1941738120976363. doi: 10.1177/1941738120976363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Single leg vertical jump performance identifies knee function deficits at return to sport after ACL reconstruction in male athletes. Kotsifaki A., Van Rossom S., Whiteley R.., et al. 2022Br J Sports Med. 56(9):490–498. doi: 10.1136/bjsports-2021-104692. doi: 10.1136/bjsports-2021-104692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Test-retest reliability of the standing heel-rise test. Ross M.D., Fontenot E.G. 2000Sport Rehabil. 9:117–123. doi: 10.1123/jsr.9.2.117. [DOI] [Google Scholar]
- Predictive factors for ankle syndesmosis injury in football players: a prospective study. Sman A. D., Hiller C. E., Rae K.., et al. 2014J Sci Med Sport. 17(6):586–590. doi: 10.1016/j.jsams.2013.12.009. doi: 10.1016/j.jsams.2013.12.009. [DOI] [PubMed] [Google Scholar]
- The jump shot - a biomechanical analysis focused on lateral ankle ligaments. Lindner M., Kotschwar A., Zsoldos R.R., Groesel M., Peham C. 2012J Biomech. 45(1):202–206. doi: 10.1016/j.jbiomech.2011.09.012. doi: 10.1016/j.jbiomech.2011.09.012. [DOI] [PubMed] [Google Scholar]
- Test-retest and interrater reliability of the functional lower extremity evaluation. Haitz K., Shultz R., Hodgins M., Matheson G. O. 2014J Orthop Sports Phys Ther. 44(12):947–954. doi: 10.2519/jospt.2014.4809. doi: 10.2519/jospt.2014.4809. [DOI] [PubMed] [Google Scholar]
- An interval kicking progression for return to soccer following lower extremity injury. Arundale A., Silvers H., Logerstedt D., Rojas J., Snyder-Mackler L. 2015Int J Sports Phys Ther. 10(1):114–127. [PMC free article] [PubMed] [Google Scholar]
- The biomechanics of kicking in soccer: a review. Lees A., Asai T., Andersen T. B., Nunome H., Sterzing T. 2010J Sports Sci. 28(8):805–817. doi: 10.1080/02640414.2010.481305. [DOI] [PubMed] [Google Scholar]
- Ball impact dynamics of instep soccer kicking. Shinkai H., Nunome H., Isokawa M., Ikegami Y. 2009Med Sci Sports Exerc. 41(4):889–897. doi: 10.1249/MSS.0b013e31818e8044. doi: 10.1249/MSS.0b013e31818e8044. [DOI] [PubMed] [Google Scholar]
- The relationship of the kicking action in soccer and anterior ankle impingement syndrome. A biomechanical analysis. Tol J.L., Slim E., van Soest A.J., van Dijk C.N. 2002Am J Sports Med. 30(1):45–50. doi: 10.1177/03635465020300012101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.