Abstract
Introduction
Post-traumatic stress disorder (PTSD) is a prevalent and severe psychiatric disorder. Repetitive transcranial magnetic stimulation (rTMS) targeting the dorsolateral prefrontal cortex provides limited relief for symptoms of PTSD. This study will be conducted to validate the efficacy of MRI-guided rTMS in targeting the sites most closely associated with the amygdala for patients with PTSD. We hypothesise that the intervention will improve clinical symptoms by decreasing amygdala activity in patients.
Methods and analysis
A randomised, double-blind, sham-controlled trial will be conducted. Forty-eight eligible patients with PTSD will be randomly assigned to receive either active or sham MRI-guided rTMS for 10 consecutive days after the initial MRI scans. MRI scans will be recollected at the end of the intervention. Clinical assessments will be performed at baseline, treatment day 5, treatment day 10, and 2 weeks, 4 weeks, 8 weeks after completion of the intervention to monitor changes in clinical symptoms. The primary assessment outcome is the change in PTSD symptoms between baseline and treatment day 10, as measured by the PTSD Checklist for DSM-5. Repeated measures analysis of variance will be performed using statistical software SPSS V.26.0. The significance level will be set at 0.05.
Ethics and dissemination
Ethical approval has been obtained from the Ethics Committee of Xijing Hospital in Xi'an, China (KY20222176-X-1), and the trial has been registered on ClinicalTrials.gov. The findings of this trial will be disseminated at academic conferences or published in peer-reviewed scientific journals.
Trial registration number
Keywords: transcranial magnetic stimulation, psychiatry, neurology
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This is a randomised controlled clinical trial to investigate the efficacy of MRI-guided repetitive transcranial magnetic stimulation (rTMS) for the treatment of post-traumatic stress disorder (PTSD).
Patients will be randomly assigned to the active or sham stimulation group while patients and assessors will be blinded to this condition.
The efficacy will be monitored with an 8-week follow-up after the treatment.
A limitation of this study is that rTMS will be administered in combination with medication, making it difficult to verify the efficacy of rTMS as a monotherapy for PTSD.
Introduction
Post-traumatic stress disorder (PTSD) is a severe psychiatric disorder characterised by recurrent intrusive re-experiencing, nightmares, hyperarousal, avoidance behaviour and altered cognition or mood.1 PTSD seriously impairs work ability and quality of life, which causes a heavy burden on families and society. The WHO reported that the lifetime prevalence of PTSD reached 3.9% in a sample of 71 083 respondents, with nearly half of them exhibiting persistent symptoms.2 Currently, the treatment for PTSD primarily includes medication and psychotherapy. However, a significant number of patients still do not get relief after treatment.3 Additionally, almost 25% of patients with PTSD did not experience recovery within a 10-year period.4
Transcranial magnetic stimulation (TMS) is a non-invasive physical therapy by directly stimulating the cerebral cortex to alter brain activity. Repetitive TMS (rTMS) is commonly used in clinical practice. High-frequency stimulation increases cortical excitability, while low-frequency stimulation inhibits excitability.5 A number of studies have investigated the efficacy of rTMS for PTSD and preliminary findings indicate that targeting either the left or right dorsolateral prefrontal cortex (dlPFC) can partially alleviate PTSD symptoms.6–8 According to rTMS guidelines, high-frequency rTMS targeting the right dlPFC is considered a ‘Level B’ for the treatment of PTSD.9 Besides, intermittent theta burst stimulation (iTBS) is a novel rTMS protocol in which high-frequency (50 Hz) pulse clusters are delivered at 5 Hz for 2 s, and the next cluster is repeated with an 8 s interval.10 iTBS can produce a quicker and longer-lasting effect on the cortex in a shorter time than conventional rTMS patterns.11 Philip et al 12 applied iTBS to the right dlPFC in patients with PTSD and found that partial clinical improvement can be observed after short-term interventions.
However, there is still a significant proportion of patients with PTSD without remission of clinical symptoms after rTMS treatment, which may be primarily attributed to the stimulation target.13 14 Most rTMS targets the dlPFC, which may not be a critical brain region in the pathogenesis of PTSD. Currently, numerous evidence supports the notion that the amygdala plays a crucial role in the development and persistence of PTSD. The amygdala, located in the depths of the dorsomedial temporal cortex, is a brain region closely associated with fear conditioning.15 Meanwhile, PTSD is also recognised as a disorder of dysfunction in fear conditioning, in which abnormalities in the amygdala are particularly prominent. Patients with PTSD exhibit a smaller volume in the amygdala16 17 and often show hyperactivation in response to negative emotional stimuli as compared with the healthy group.18 19 The amygdala is also significantly overactive, even in the resting state.20 Current research suggests that hyperactivity of the amygdala is an important pathogenetic mechanism in PTSD and contributes to the core clinical symptoms.21 Furthermore, there is a positive correlation between the level of amygdala activity and the clinical severity of the disorder.22–24 The clinical symptoms of patients with PTSD can be significantly improved by inhibiting the function of the amygdala.25 Therefore, the efficacy of rTMS for PTSD may be significantly enhanced by reducing the activity of the amygdala.
In addition, the stimulation coils frequently used in clinics can only affect cortical activity about 2–5.5 cm below the scalp, which results in rTMS failing to directly modulate the activity of the amygdala. However, the effects of rTMS are not only limited to the stimulation region but also induce subsequent changes in other brain regions that are closely connected to it.26 MRI-guided rTMS can accurately affect deep brain regions by selecting stimulation targets based on functional connectivity.27 28 The ventrolateral PFC (vlPFC) may be the target region of MRI-guided rTMS that can significantly affect the activity of the amygdala. The vlPFC has significant functional connectivity with the amygdala, which is enhanced in patients after effective treatment,29 30 and it is also the only brain region in the PFC that can directly receive rTMS while having relatively more amygdala projections.31 32 Sydnor et al 33 found that selecting the most functionally relevant sites of the vlPFC as TMS targets for the amygdala can significantly reduce amygdala activity. They also discovered that a higher density of white matter pathways connecting the vlPFC and amygdala is associated with greater changes in amygdala activity.
To summarise, the efficacy of rTMS for PTSD may be improved if these findings are used to inform the implementation of rTMS. Therefore, we plan to conduct a randomised controlled study aimed at validating the efficacy of MRI-guided rTMS in the treatment of PTSD by indirectly modulating the activity of the amygdala.
Study objective
The amygdala is hyperactive in patients with PTSD, and MRI-guided rTMS can indirectly decrease amygdala activity through the functional and structural connectivity of each individual.33 Presumably, MRI-guided rTMS in patients with PTSD would reduce amygdala activity and significantly improve symptoms of PTSD. Therefore, in this randomised double-blind controlled study, we will analyse the degree of structural and functional connectivity of each participant, identifying the sites that are most closely linked to the amygdala as stimulation targets, and assess the effect of MRI-guided rTMS on clinical symptoms and brain activity.
We hypothesised that patients with PTSD who receive active stimulation will show more significant decreases in symptom severity after the intervention compared with patients who receive sham stimulation. We further hypothesise that active rTMS can significantly reduce amygdala activity, and that the extent of reduction is correlated with symptom improvement.
Methods and analysis
Study design
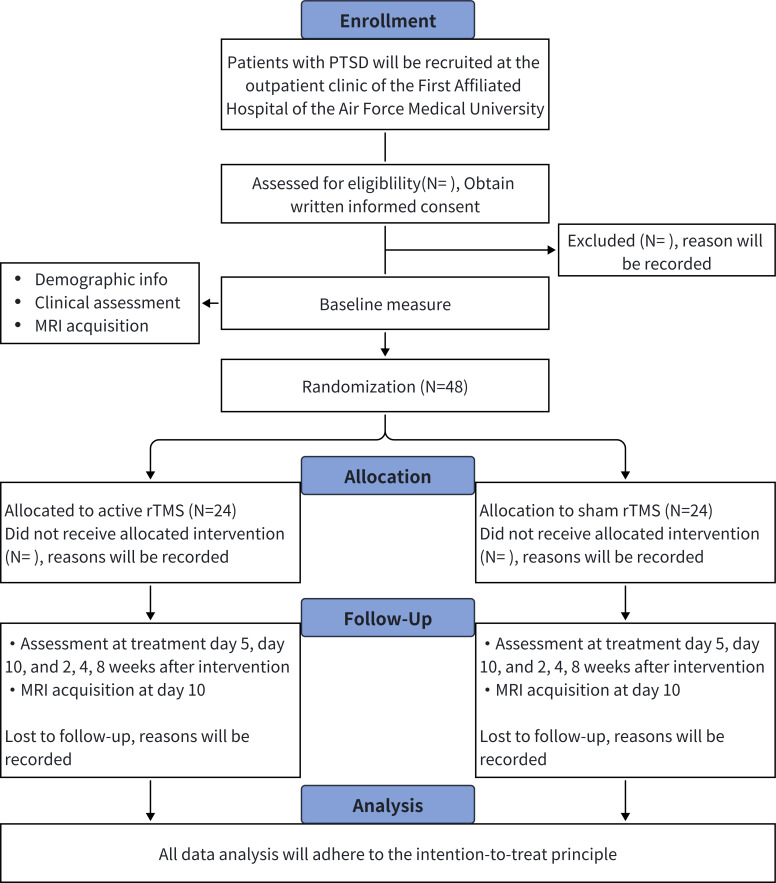
This study protocol is designed in accordance with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) statement. The process of this study is shown in figure 1. Patients with PTSD will be randomly assigned to either the active rTMS group or the sham rTMS group using the block group randomisation method. MRI scans will be performed on participants to identify target sites, then rTMS will be administered for 10 consecutive days. Participants will undergo additional MRI scans after the treatment to investigate changes in brain function before and after the treatment. Meanwhile, clinical symptom assessments will be conducted at baseline, treatment day 5, treatment day 10, and 2 weeks, 4 weeks, 8 weeks post-treatment to explore the improvement of PTSD symptoms by rTMS. This trial started in September 2023 and is expected to be completed in December 2024.
Figure 1.
Flow chart of the study design. PTSD, post-traumatic stress disorder; rTMS, repetitive transcranial magnetic stimulation.
Participants
Patients with PTSD will be recruited at the outpatient clinic of the First Affiliated Hospital of the Air Force Medical University, China, from March 2023 to June 2024. Recruitment information will also be made into a poster and disseminated through social media in order to recruit patients. These have been approved by the hospital Ethics Committee. Participants who meet the following inclusion and exclusion criteria are eligible for this study. At the screening, participants will be informed by the investigator about the study procedures, risks and benefits and the voluntary nature of participation. Meanwhile, written informed consent will be obtained from all participants prior to their participation in the study (online supplemental file 1).
bmjopen-2023-081751supp001.pdf (68.2KB, pdf)
Inclusion criteria
Between the ages of 18 and 65 years.
Meeting the criteria of the DSM-5 for PTSD, which will be assessed by two professional psychiatrists.
With a score greater than 33 on the PTSD Checklist for DSM-5 (PCL-5).
Not receive any medication or psychotherapy for PTSD before entering the study.
Exclusion criteria
Significant medical illnesses or diseases that may affect the central nervous system.
Abnormal EEG or MRI evidence of brain abnormalities.
Contraindications to MRI scans or TMS including metal or electronic implants, claustrophobia, and so on.
Alcohol and drug abuse.
Strong suicidal ideation or a history of previous suicidal behaviour.
Pregnancy, lactation, or planning pregnancy during the trial period.
Patient and public involvement
Patients and the public were not involved in the design of the study.
Sample size
Sample size is calculated using PASS software V.2021. We used the results of a previous randomised controlled study on PTSD conducted by our research team, which shares a similar study design with the current study.34 The effect size of PCL scale scores after rTMS treatment in the previous study is 0.82. The significance level is set at 0.05 (two-tailed test) and the statistical power is set at 80%. It has been calculated that 38 participants are needed. Assuming a dropout rate of 20%, the sample size is expanded to 48 participants (24 participants per group).
Allocation and blinding
Participants will be randomly assigned to either the active rTMS group or the sham rTMS group in a 1:1 ratio, following a randomisation sequence. The sequence has been formulated by a specialised investigator (YM) before the trial. The allocation details of each participant will be sequentially sealed in opaque envelopes.35 When participants enter the study, the researcher will open the envelopes in sequence and inform the therapist of the appropriate treatment.
Participants, their families and the raters conducting the clinical assessments are blinded to the group assignment. Participant ID and subgroup information will be anonymised to ensure that the blinding remains in effect until the study is completed. If severe adverse events occur, unblinding will be performed after consultation with the principal investigator.
MRI data acquisition and identifying targets
Neuroimaging data will be acquired at Xi'an YunYing Image Medical Diagnosis Center using a 3T uMR 780 scanner (Shanghai United Imaging Healthcare Co, Ltd, China). MRI data will include T1-weighted structural MRI, resting-state functional MRI and diffusion tensor imaging sequences. The acquisition parameters are as follows: (1) T1-weighted structural MRI: thickness=1 mm, slices=200, repetition time=7.24 ms, echo time=3.10 ms, inversion time=750 ms, field of view=256×256 mm2, inversion time=750 ms, flip angle=10°, voxel size=1×1×1 mm3; (2) resting-state functional MRI: thickness=4 mm, slices=8400, repetition time=2000 ms, echo time=30 ms, field of view=224×224 mm2, flip angle=90°, voxel size=3.5×3.5×4.0 mm3; (3) diffusion tensor imaging: thickness=2 mm, slices=2475, repetition time=12 676 ms, echo time=88.6 ms, field of view=224×224 mm2, flip angle=90°, voxel size=2×2×2 mm3, b-value=1000 s/mm². During the scan, participants will be asked to close their eyes, relax, not think intentionally, and not fall asleep.
Based on the MRI data of each participant, we will identify sites in the right vlPFC that are structurally and functionally strongly associated with the right amygdala. These sites will be targeted for subsequent rTMS. The right hemisphere is chosen as the target for rTMS because previous studies have suggested that it may be more effective than the left hemisphere.36 The target calculation process is as follows: first, the resting-state data will be preprocessed with reslicing and head motion correction, alignment and Gaussian smoothing processing. Then, the right vlPFC will be divided into several subregions, and their subnucleolar concentrations, subnucleolar sizes and functional connectivity coefficients with the right amygdala will be comprehensively analysed to identify the sites that are functionally closely connected to the amygdala. Finally, the white matter fibre connections between these sites and the amygdala will be detected, and the optimal stimulation target will be selected by combining the functional connections and white matter fibre connections between them.
Interventions
The MRI-guided rTMS will be delivered by the Black Dolphin Transcranial Magnetic Robot (Spirit Dolphin, SLD-YXRJ-V1.0) from Xi'an Solide Brain Control Medical Technology Co, which is equipped with a figure-of-eight coil (Yingchi Tech, Shenzhen, China). The robot is equipped with a positioning navigation system based on neuroimaging, which allows it to manipulate the coil alignment and accurately place it on pre-explored targets. The position of the coil can be adjusted in real time during treatment to ensure that stimuli are consistently applied to the same target area. MRI-based positioning is currently the most accurate method for placing the TMS coil at the target site.37 Preliminary results have shown that using this positioning generates greater clinical efficacy compared with traditional scalp measurements.38
A figure-of-eight coil will be used in the treatment of this study. Twenty sessions will be performed over 10 consecutive days, with two iTBS sessions per day at 50 min intervals (intensity of 90% motor threshold, each containing 1800 pulses for 10 min). The 10 min iTBS session has been shown to significantly improve symptoms of PTSD after up to 20 sessions. Our study will employ the iTBS protocol, which will be applied twice a day to expedite the treatment duration. The 50 min interval is based on a previous iTBS study on iTBS, which suggests that intervals of 50 min or more can have a stronger cumulative effect on nerve fibres.39 40 In the sham stimulation group, the coil will be turned 90° and placed in contact with the scalp, producing the same stimulation sound and some degree of scalp sensation. This approach does not induce significant changes in cortical activity and has been used in many randomised controlled studies of rTMS.10 41 The treatment will be conducted by a trained technician in a separate treatment room. Participants will be prohibited from communicating with each other during the treatment intervals to prevent the cohort effect. In addition, each participant will take paroxetine (20 mg/day) concurrently with rTMS treatment, in accordance with ethical guidelines. This is because paroxetine is currently the first-line medication for PTSD in clinical settings.42 MRI and rTMS will be provided free of charge for participants.
Outcomes
General information, including gender, age, type of trauma and comorbidities, will be collected at baseline. Clinical symptoms will be monitored using self-rated and physician-rated clinical scales assessed at baseline, treatment day 5, treatment day 5, and 2 weeks, 4 weeks, 8 weeks after the end of treatment. MRI scans will also be performed at baseline and after the last session to observe the effects of rTMS on brain activity in patients with PTSD. In addition, any adverse events will be promptly recorded during the entire study period.
Primary outcome
The PTSD Checklist for DSM-5 (PCL-5) is a self-report scale commonly used to assess the severity of core PTSD symptoms. PCL-5 scores of 31–33 are optimal for efficiently diagnosing PTSD, with higher scores indicating more severe symptoms of PTSD.43 The change from baseline to the 10-day treatment post of PCL-5 will be the primary measure as it can effectively reflect the effect of the intervention on PTSD symptoms.
Secondary outcomes
The change in PCL-5 scale total score at baseline compared with 2, 4 and 8 weeks after the end of treatment will be used to investigate the long-term efficacy of rTMS on symptoms of PTSD.
The 17-item Hamilton Depression Rating Scale (HAMD-17) and the Beck Depression Inventory (BDI) are clinician-rated and self-rated scales used to assess depressive symptoms, respectively.44 45 Higher total scores on these scales indicate more severe depressive symptoms. The change in total scores of the HAMD-17 and BDI from baseline to each of the other time points will be used to assess the efficacy of rTMS on depressive symptoms.
The Hamilton Anxiety Scale and the Zung Self-Rating Anxiety Scale are commonly used in clinical practice to assess anxiety symptoms. In the present study, these scales will be used to assess the effectiveness of the intervention in reducing anxiety symptoms.
The Insomnia Severity Index (ISI) is a widely used questionnaire for screening insomnia. The measure is brief, consisting of only seven items. Each item is scored from 0 to 4, with higher scores indicating greater sleep disturbance. In this study, the ISI will be used to assess the efficacy of the intervention on insomnia and sleep disturbances related to insomnia.
Resting-state functional MRI reflects the spontaneous neural activity in different brain regions. Amplitude of the low-frequency fluctuation (ALFF) and regional homogeneity (ReHo) provide different perspectives for assessing the level of spontaneous activity in a single voxel of the brain.46 47 In the present study, we will calculate the ALFF and ReHo values of the right amygdala before and after treatment, respectively, and compare their differences to explore the effect of rTMS on amygdala activity. The relationship between these changes and clinical outcomes will also be explored.
The incidence of adverse events during treatment and the retention rates in each group will be used to assess the safety and acceptability of the 10-day MRI-guided rTMS.
Data collection and management
Assessment data will be collected by two psychiatrists who are blinded to the allocation and not involved in patient treatment. Assessors have extensive work experience and will receive specific training to ensure consistency in assessment results among them. Participants will be available for phone interviews to facilitate the completion of follow-up visits.
Personal information and clinical outcomes of participants will be initially stored in paper case report forms, and on the last day of each week, the data will be electronically saved in an Excel database, which will be maintained on a separate computer at the research centre. Data containing personally identifiable information will be stored in a separate Excel file, and each item will be assigned a specific code that will be used to refer to the participant in other databases. MRI scans will be performed at a specialised imaging facility. MRI scans of each participant will initially be stored on a CD, which will then be uploaded to the image database by the research staff. All paper documents and image CDs will be stored in a secure filing cabinet in the study centre, while the computer and Excel database will be password-protected to ensure participant privacy. In addition, data from rTMS, including intensity thresholds, treatment progress and any adverse events that occur during treatment, will be collected and independently stored by the therapist. This data will then be added to the total Excel file after the study.
Participant safety
Prior to enrolment, participants with contraindications to MRI, such as metal implants in the body and claustrophobia, will be excluded. A specialised examiner will be responsible for conducting the MRI scans. They will also ensure that there are no relevant contraindications prior to the examination and provide earmuffs to mitigate the noise.
rTMS has been shown to be safe and well-tolerated in most clinical situations. Common adverse events include headaches and localised abnormal sensations, which are often mild and typically resolve within an hour after rTMS. However, rTMS has a low risk of inducing seizures, with an incidence rate of approximately 0.01%–0.1%. Therefore, we will exclude participants who have a history of seizures or show abnormal EEG during screening. rTMS will be administered by experienced therapists to ensure that participants are promptly treated in case of adverse events. If any serious adverse events occur during the study, the participant will be taken by the investigator to either the emergency department or the specialist clinic. The sponsor is responsible for covering the cost of treatment and providing financial compensation to participants who suffer trial-related harm or death. Adverse events and study progress will be periodically reviewed by the Ethics Committee.
Participants will be discontinued from the study if (1) serious adverse events occur (eg, seizure and suicide); (2) the participant does not wish to continue; (3) the participant is unable to tolerate the discomfort produced by rTMS; and (4) serious violations of the treatment protocol occur, such as interruptions of treatment for 2 days or more.
Statistical analysis
All data analysis will adhere to the intention-to-treat principle. Basic information and clinical scores of all participants will be analysed using IBM SPSS Statistics for Windows V.26.0. Continuous variables will be expressed as means and SD, while categorical variables will be presented as frequencies and percentages. The independent samples t-test or χ2 test will be used to verify homogeneity between groups. One-way repeated measures analysis of variance (ANOVA) will be used to compare the outcome variables at different time points within each group. Two-way repeated measures ANOVA will be used to test the interaction effect of 'intervention' and 'time' on the outcome variables at different periods between the two groups. Multiple comparisons will then be performed using the Bonferroni test to identify specific significant differences. If there are significant differences in baseline characteristics, the analysis of covariance (ANCOVA) model will be used to analyse the differences between groups. If there is missing data, it will be processed using the multiple imputation method.
The MRI data before and after treatment will be processed and analysed using the SPM12 software package in Matlab R2019b. The Restplus V1.2 toolbox will be used to preprocess and calculate the ALFF and ReHo. Then, paired samples t-tests will be used to examine the differences before and after treatment within each group, and independent samples t-tests will be used to compare the differences after treatment between groups.
Ethics and dissemination
The study will be conducted in accordance with the Declaration of Helsinki and the study protocol. Ethical permission has been obtained from the Ethics Committee of the First Affiliated Hospital of Air Force Military Medical University (Grant No. KY20222176-X-1), and the study has been registered with ClinicalTrials.gov. All participants will be informed of the study details and will be asked to sign a written informed consent before participating in the study.
The efficacy of the intervention will be disseminated at international and national academic conferences or published in peer-reviewed scientific journals.
Strengths and limitations
The present trial has the following strengths: first, to our knowledge, this study is the first randomised double-blind sham-controlled study using MRI-guided rTMS for the treatment of PTSD; second, the target selected in this study is vlPFC, a region currently not intervened in TMS clinical treatment. Therefore, our results may enrich target selection for future TMS treatment; third, the present study aims to inhibit amygdala activity, and neuroimages will be acquired before and after treatment, which will probably reveal PTSD-related therapeutic mechanisms. This study also has some limitations: first, due to ethical requirements, patients will take the medication while receiving TMS, which may mask the differences in efficacy between the two groups. However, it usually takes about a month for medications to begin to show efficacy in treating PTSD, so the influence of medication on the primary outcome may have been limited. Second, the lack of objective observations to measure changes in PTSD symptoms is also a limitation of this study.
Supplementary Material
Footnotes
Contributors: All authors contributed to the initiation of this study. YCZ, MC, NT and HW were involved in the conception and design of the study. HW provided technical support for MRI analysis and rTMS. YCZ, YYZ, YM drafted the manuscript. ZP, NL and RL reviewed and revised the manuscript. All authors have read and approved the final manuscript.
Funding: This work is supported by National Natural Science Foundation of China (82330043).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. N Engl J Med 2017;376:2459–69. 10.1056/NEJMra1612499 [DOI] [PubMed] [Google Scholar]
- 2. Rosellini AJ, Liu H, Petukhova MV, et al. Recovery from DSM-IV post-traumatic stress disorder in the WHO world mental health surveys. Psychol Med 2018;48:437–50. 10.1017/S0033291717001817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: A review of randomized clinical trials. JAMA 2015;314:489–500. 10.1001/jama.2015.8370 [DOI] [PubMed] [Google Scholar]
- 4. Rosellini AJ, Fayyad J, Koenen KC. Patterns and Predictors of the Course of Posttraumatic Stress Disorder[J]. Trauma and Posttraumatic Stress Disorder: Global Perspectives from the WHO World Mental Health Surveys. New York, NY: Cambridge University Press, 2018:240–52. [Google Scholar]
- 5. Jannati A, Oberman LM, Rotenberg A, et al. Assessing the mechanisms of brain plasticity by transcranial magnetic stimulation. Neuropsychopharmacology 2023;48:191–208. 10.1038/s41386-022-01453-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ahmadizadeh MJ, Rezaei M. Unilateral right and bilateral Dorsolateral Prefrontal cortex transcranial magnetic stimulation in treatment post-traumatic stress disorder: A randomized controlled study. Brain Res Bull 2018;140:334–40. 10.1016/j.brainresbull.2018.06.001 [DOI] [PubMed] [Google Scholar]
- 7. Woodside DB, Colton P, Lam E, et al. Dorsomedial Prefrontal cortex repetitive transcranial magnetic stimulation treatment of Posttraumatic stress disorder in eating disorders: an open-label case series. Int J Eat Disord 2017;50:1231–4. 10.1002/eat.22764 [DOI] [PubMed] [Google Scholar]
- 8. Watts BV, Landon B, Groft A, et al. A sham controlled study of repetitive transcranial magnetic stimulation for Posttraumatic stress disorder. Brain Stimul 2012;5:38–43. 10.1016/j.brs.2011.02.002 [DOI] [PubMed] [Google Scholar]
- 9. Lefaucheur J-P, André-Obadia N, Antal A, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): an update. Clin Neurophysiol 2014;125:2150–206. 10.1016/j.clinph.2014.05.021 [DOI] [PubMed] [Google Scholar]
- 10. Blumberger DM, Vila-Rodriguez F, Thorpe KE, et al. Effectiveness of Theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet 2018;391:1683–92. 10.1016/S0140-6736(18)30295-2 [DOI] [PubMed] [Google Scholar]
- 11. Huang Y-Z, Edwards MJ, Rounis E, et al. Theta burst stimulation of the human motor cortex. Neuron 2005;45:201–6. 10.1016/j.neuron.2004.12.033 [DOI] [PubMed] [Google Scholar]
- 12. Philip NS, Barredo J, Aiken E, et al. Theta-burst transcranial magnetic stimulation for Posttraumatic stress disorder. Am J Psychiatry 2019;176:939–48. 10.1176/appi.ajp.2019.18101160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harris A, Reece J. Transcranial magnetic stimulation as a treatment for Posttraumatic stress disorder: A meta-analysis. J Affect Disord 2021;289:55–65. 10.1016/j.jad.2021.04.003 [DOI] [PubMed] [Google Scholar]
- 14. van Rooij SJH, Sippel LM, McDonald WM, et al. Defining focal brain stimulation targets for PTSD using neuroimaging. Depress Anxiety 2021. 10.1002/da.23159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Janak PH, Tye KM. From circuits to behaviour in the amygdala. Nature 2015;517:284–92. 10.1038/nature14188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Del Casale A, Ferracuti S, Barbetti AS, et al. Grey matter volume reductions of the left hippocampus and amygdala in PTSD: A coordinate-based meta-analysis of magnetic resonance imaging studies. Neuropsychobiology 2022;81:257–64. 10.1159/000522003 [DOI] [PubMed] [Google Scholar]
- 17. Bromis K, Calem M, Reinders AATS, et al. Meta-analysis of 89 structural MRI studies in Posttraumatic stress disorder and comparison with major depressive disorder. Am J Psychiatry 2018;175:989–98. 10.1176/appi.ajp.2018.17111199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stevens JS, Kim YJ, Galatzer-Levy IR, et al. Amygdala reactivity and anterior cingulate habituation predict Posttraumatic stress disorder symptom maintenance after acute civilian trauma. Biol Psychiatry 2017;81:1023–9. 10.1016/j.biopsych.2016.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stevens JS, Jovanovic T, Fani N, et al. Disrupted amygdala-Prefrontal functional Connectivity in civilian women with Posttraumatic stress disorder. J Psychiatr Res 2013;47:1469–78. 10.1016/j.jpsychires.2013.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Koch SBJ, van Zuiden M, Nawijn L, et al. Aberrant resting-state brain activity in Posttraumatic stress disorder: a meta-analysis and systematic review. Depress Anxiety 2016;33:592–605. 10.1002/da.22478 [DOI] [PubMed] [Google Scholar]
- 21. Fenster RJ, Lebois LAM, Ressler KJ, et al. Brain circuit dysfunction in post-traumatic stress disorder: from Mouse to man. Nat Rev Neurosci 2018;19:535–51. 10.1038/s41583-018-0039-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sun D, Gold AL, Swanson CA, et al. Threat-induced anxiety during goal pursuit disrupts amygdala-Prefrontal cortex Connectivity in Posttraumatic stress disorder. Transl Psychiatry 2020;10:61. 10.1038/s41398-020-0739-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Liu T, Ke J, Qi R, et al. Altered functional Connectivity of the amygdala and its Subregions in Typhoon-related post-traumatic stress disorder. Brain Behav 2021;11:e01952. 10.1002/brb3.1952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mehta ND, Stevens JS, Li Z, et al. Inflammation, amygdala-ventromedial Prefrontal functional Connectivity and symptoms of anxiety and PTSD in African American women recruited from an inner-city hospital: preliminary results. Brain Behav Immun 2022;105:122–30. 10.1016/j.bbi.2022.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bijanki KR, van Rooij SJH, Ely TD, et al. Case series: unilateral amygdala ablation ameliorates post-traumatic stress disorder symptoms and biomarkers. Neurosurgery 2020;87:796–802. 10.1093/neuros/nyaa051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Legrand M, Troubat R, Brizard B, et al. Prefrontal cortex rTMS reverses behavioral impairments and Differentially activates C-Fos in a mouse model of post-traumatic stress disorder. Brain Stimul 2019;12:87–95. 10.1016/j.brs.2018.09.003 [DOI] [PubMed] [Google Scholar]
- 27. Oathes DJ, Zimmerman JP, Duprat R, et al. Resting fMRI-guided TMS results in subcortical and brain network modulation indexed by Interleaved TMS/fMRI. Exp Brain Res 2021;239:1165–78. 10.1007/s00221-021-06036-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Raij T, Nummenmaa A, Marin M-F, et al. Prefrontal cortex stimulation enhances fear extinction memory in humans. Biol Psychiatry 2018;84:129–37. 10.1016/j.biopsych.2017.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Silvers JA, Insel C, Powers A, et al. vlPFC-vmPFC-amygdala interactions underlie age-related differences in cognitive regulation of emotion. Cereb Cortex 2017;27:3502–14. 10.1093/cercor/bhw073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lu L, Mills JA, Li H, et al. Acute Neurofunctional effects of Escitalopram in pediatric anxiety: A double-blind, placebo-controlled trial. J Am Acad Child Adolesc Psychiatry 2021;60:1309–18. 10.1016/j.jaac.2020.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ghashghaei HT, Hilgetag CC, Barbas H. Sequence of information processing for emotions based on the anatomic dialogue between Prefrontal cortex and amygdala. Neuroimage 2007;34:905–23. 10.1016/j.neuroimage.2006.09.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ray RD, Zald DH. Anatomical insights into the interaction of emotion and cognition in the Prefrontal cortex. Neurosci Biobehav Rev 2012;36:479–501. 10.1016/j.neubiorev.2011.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sydnor VJ, Cieslak M, Duprat R, et al. Cortical-subcortical structural connections support transcranial magnetic stimulation engagement of the amygdala. Sci Adv 2022;8:eabn5803. 10.1126/sciadv.abn5803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhou P, Zhang Y, Tan QR. Effect of repetitive transcranial magnetic stimulation (rTMS) combined with paroxetine in the treatment of Posttraumatic stress disorder. J Psychiatry (Chinese Ed) 2016;29:89–92. [Google Scholar]
- 35. Lai D, Wang D, McGillivray M, et al. Assessing the quality of randomization methods in randomized control trials. Healthcare 2021;9:100570. 10.1016/j.hjdsi.2021.100570 [DOI] [PubMed] [Google Scholar]
- 36. Kan RLD, Zhang BBB, Zhang JJQ, et al. Non-invasive brain stimulation for Posttraumatic stress disorder: a systematic review and meta-analysis. Transl Psychiatry 2020;10:168. 10.1038/s41398-020-0851-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cash RFH, Weigand A, Zalesky A, et al. Using brain imaging to improve spatial targeting of transcranial magnetic stimulation for depression. Biol Psychiatry 2021;90:689–700. 10.1016/j.biopsych.2020.05.033 [DOI] [PubMed] [Google Scholar]
- 38. Cole EJ, Stimpson KH, Bentzley BS, et al. Stanford accelerated intelligent Neuromodulation therapy for treatment-resistant depression. Am J Psychiatry 2020;177:716–26. 10.1176/appi.ajp.2019.19070720 [DOI] [PubMed] [Google Scholar]
- 39. Lynch G, Kramár EA, Babayan AH, et al. Differences between synaptic plasticity thresholds result in New timing rules for maximizing long-term potentiation. Neuropharmacology 2013;64:27–36. 10.1016/j.neuropharm.2012.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Smolen P, Zhang Y, Byrne JH. The right time to learn: mechanisms and optimization of spaced learning. Nat Rev Neurosci 2016;17:77–88. 10.1038/nrn.2015.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pan F, Mou T, Shao J, et al. Effects of Neuronavigation-guided rTMS on serum BDNF, Trkb and VGF levels in depressive patients with suicidal Ideation. J Affect Disord 2023;323:617–23. 10.1016/j.jad.2022.11.059 [DOI] [PubMed] [Google Scholar]
- 42. Abdallah CG, Averill LA, Akiki TJ, et al. The Neurobiology and Pharmacotherapy of Posttraumatic stress disorder. Annu Rev Pharmacol Toxicol 2019;59:171–89. 10.1146/annurev-pharmtox-010818-021701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bovin MJ, Marx BP, Weathers FW, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical Manual of mental disorders-fifth edition (PCL-5) in veterans. Psychol Assess 2016;28:1379–91. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- 44. Furukawa TA, Reijnders M, Kishimoto S, et al. Translating the BDI and BDI-II into the HAMD and vice versa with Equipercentile linking. Epidemiol Psychiatr Sci 2019;29:e24. 10.1017/S2045796019000088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lin CH, Park C, McIntyre RS. Early improvement in HAMD-17 and HAMD-7 scores predict response and remission in depressed patients treated with fluoxetine or electroconvulsive therapy. J Affect Disord 2019;253:154–61. 10.1016/j.jad.2019.04.082 [DOI] [PubMed] [Google Scholar]
- 46. Zang Y-F, He Y, Zhu C-Z, et al. Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain Dev 2007;29:83–91. 10.1016/j.braindev.2006.07.002 [DOI] [PubMed] [Google Scholar]
- 47. Zang Y, Jiang T, Lu Y, et al. Regional homogeneity approach to fMRI data analysis. Neuroimage 2004;22:394–400. 10.1016/j.neuroimage.2003.12.030 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-081751supp001.pdf (68.2KB, pdf)