Many of the common cardiovascular disorders (especially in elderly people) are linked to thrombosis—such as ischaemic heart disease, atrial fibrillation, valve disease, hypertension, and atherosclerotic vascular disease—requiring the use of antithrombotic therapy. This raises questions regarding the appropriate use of antithrombotic therapy in older people, especially because strategies such as anticoagulation with warfarin need regular monitoring of the international normalised ratio (INR), a measure of the induced haemorrhagic tendency, and carry a risk of bleeding. The presence of concomitant physical and medical problems increases the interactions and risks associated with warfarin, and anticoagulation in elderly patients often needs an assessment of the overall risk:benefit ratio.
Questions to ask when considering oral anticoagulation
Is there a definite indication (such as atrial fibrillation)?
Is there a high risk of bleeding or strong contraindication against anticoagulation?
Will concurrent medication or disease states increase bleeding risk or interfere with anticoagulation control?
Is drug compliance and attendance at anticoagulant clinic for monitoring likely to be a problem?
Will there be regular review of the patient, especially with regard to risks and benefits of anticoagulation?
 ISI=international sensitivity ratio. The mean normal prothrombin time is often generated from samples from local healthy subjects or a commercially available standard. The exact value of the ISI depends on the thromboplastin used in the prothrombin time method
ISI=international sensitivity ratio. The mean normal prothrombin time is often generated from samples from local healthy subjects or a commercially available standard. The exact value of the ISI depends on the thromboplastin used in the prothrombin time method
Physical frailty in elderly people may reduce access to anticoagulant clinics for INR monitoring. The decline in cognitive function in some elderly patients also may reduce compliance with anticoagulation and the appreciation of bleeding risks and drug interactions. However, in recent studies of anticoagulation in elderly people, no significant associations of anticoagulant control were found with age, sex, social circumstances, mobility, domicillary supervision of medication, or indications for anticoagulation.
Warfarin
Bleeding is the most serious and common complication of warfarin treatment. For any given patient, the potential benefit from prevention of thromboembolic disease needs to be balanced against the potential harm from induced haemorrhagic side effects.
Minor bleeds
Most bleeding problems are clinically minor, although patients are unlikely to view such bleeds in these terms. The problems include nose bleeds, bruising, and excessive bleeding after minor injury such as shaving. Patients should be made aware of these common problems and be reassured that these events are expected in patients receiving warfarin treatment. Menorrhagia is surprisingly rare as a major clinical problem, even though it can be severe.
More serious problems
Patients need access to medical care if they have serious problems. Such problems are generally due to a high INR. Usually, spontaneous bruising, any bleeding that is difficult to arrest, frank haematuria, any evidence of gastrointestinal bleeding, and haemoptysis, need urgent assessment. The definition of minor or major bleeding lacks clarity: in many cases the patient presents with a concern that may need follow up, and a minor bleed can only be defined as such in retrospect. In most cases, evidence of bleeding suggests some underlying pathology but may also be due to drug interactions. For example, a patient with recurrent haemoptysis may be found to have hereditary telangectasia. Further investigation of the cause of bleeding should always be considered, particularly if the bleeding is recurrent. It is also important in these instances to check for concomitant drug use, particularly drugs received over the counter. Patients should be aware that aspirin and non-steroidal anti-inflammatory drugs are particularly dangerous in combination with warfarin; however, even supposedly safe drugs such as paracetamol can affect a patient's bleeding tendency.
Sudden, unexplained changes to the efficacy of warfarin may be caused by the consumption of over the counter multivitamin tablets or foodstuffs that contain vitamin K
Patients at high risk of bleeding with warfarin
Age >75 years
History of uncontrolled hypertension (defined as systolic blood pressure >180mm Hg or diastolic blood pressure >100 mm Hg)
Alcohol excess (acute or chronic), liver disease
Poor drug compliance or clinic attendance
Bleeding lesions (especially gastrointestinal blood loss, such as peptic ulcer disease, or recent cerebral haemorrhage)
Bleeding tendency (including coagulation defects, thrombocytopenia) or concomitant use of non-steroidal anti-inflammatory drugs and antibiotics
Instability of INR control and INR >3
Incidence of bleeding problems
The incidence of severe bleeding problems that may bring patients to an accident and emergency unit has probably been overestimated. The annual incidence of fatality caused by warfarin administration has been estimated to be 1%. However, this is based on old data, and, although difficult to prove, the overall improvement in anticoagulation control in the past 10-15 years means that a more realistic figure is about 0.2%. Methodological problems have hampered the interpretation of previously reported data, particularly with regard to definitions of major and minor bleeding episodes, with some investigators accepting hospital admission for transfusion of up to 4 units of blood as being “minor.” Certainly, the most serious “major” bleed is an intracranial haemorrhage. Reviews of observational and experimental studies showed annual bleeding rates of 0-4.8% for fatal bleeding and 2.4-8.1% for major bleeds. Minor bleeds are reported more often, with about 15% of patients having at least one minor event a year.
Risk factors for bleeding
Age is the main factor that increases risk of bleeding. One study showed a 32% increase in all bleeding and a 46% increase in major bleeding for every 10 year increase above the age of 40.
Early studies suggested an increased risk with increasing target INR, but the data were difficult to interpret because results were reported in both INR and prothrombin time. The actual risk of bleeding should be taken into account as well as the degree of anticoagulation (as measured by the INR). One study which achieved point prevalence of therapeutic INRs of 77% reported no association between bleeding episodes and target INR.
Data from an Italian study in 2745 patients with 2011 patient years of follow up reported much lower bleeding rates, with an overall rate of 7.6 per 100 patient years. The reported rates for fatal, major, and minor bleeds were 0.25, 1.1, and 6.2 per 100 patient years respectively. This study confirmed an increased risk with age and found a significantly increased risk during the first 90 days of treatment. Peripheral vascular and cerebrovascular disease carried a higher relative risk of bleeding, and target INR was strongly associated with bleeding with a relative risk of 7.9 (95% confidence interval 5.4 to11.5, P<0.0001) when the most recent INR recorded was >4.5. Data from a trial in a UK community showed 39.8 minor, 0.4 major, and no fatal haemorrhagic events per 100 patient years for the total study population, with 3.9 serious thromboembolic events per 100 patient years, of which 0.79 were fatal.
Warfarin is therefore a relatively safe drug, particularly if therapeutic monitoring is performed well. Analogies are often made between therapeutic monitoring of warfarin and monitoring of blood glucose for diabetic patients. Given the increase in numbers of patients receiving warfarin, particularly for atrial fibrillation, the scale of the problem is likely to be the same. There is no reason why warfarin monitoring cannot become as routine as glucose monitoring in diabetes: relevant small machines are available for generating an INR (with associated standards and quality control).
Risk of bleeding associated with warfarin treatment
Rate of bleeding episodes associated in the general patient population is decreasing (possibly due to better management)
Risk increases with age
Risk of bleeding is directly related to the achieved intensity of INR rather than the target INR (a clear dose-response effect)
Temporal association between measured INR and risk of bleeding
Relative risk of bleeding is increased in patients with cerebrovascular disease and venous thrombosis
Overanticoagulation
Excessive anticoagulation without bleeding or with only minor bleeding can be remedied by dose reduction or discontinuation. The risk of bleeding is decreased dramatically by lowering the intended INR from 3-4.5 down to 2-3, although this increases the risk of thrombosis. If bleeding becomes substantial, 2-5 mg of oral or subcutaneous vitamin K may be needed. In patients with prosthetic valves, vitamin K should perhaps be avoided because of the risk of valve thrombosis unless there is life threatening intracranial bleeding. Alternatives to vitamin K include a concentrate of the prothrombin group of coagulation factors including II, IX, and X, fresh frozen plasma 15 ml/kg, and recombinant factor VIIa.
Aspirin
Aspirin has little effect in terms of bruising but can cause serious gastrointestinal bleeding. The risk of gastrointestinal bleeding is related to dose and should not be problematic at doses of 75 mg/day given as thromboprophylaxis. There is currently no consensus as to optimal dose of aspirin for stroke prevention in atrial fibrillation. A meta-analysis of randomised controlled trials using aspirin showed that a mean dose of 273 mg/day, increased absolute risk of haemorrhagic stroke to 12 events per 10 000 people. This relatively small increase must be weighed against the reduced risk of myocardial infarction (to 137 events per 10 000) and ischaemic stroke (to 39 events per 10 000). However, in one trial of patients with well controlled hypertension, use of aspirin 75 mg prevented 1.5 myocardial infarctions per 1000 patients a year, which was in addition to the benefit achieved by lowering the blood pressure, with no effect on stroke. Although there was no increase in the number of fatal bleeding events (seven in patients taking aspirin, compared with eight in the placebo group), there was a 1.8% increase in non-fatal, major bleeding events (129 events in patients taking aspirin, compared with 70 in the placebo group) and minor bleeds (156 and 87, respectively).
Risk of bleeding
There have been conflicting results concerning the role of age as an independent risk factor for haemorrhage induced by anticoagulants. Advanced age (>75 years), intensity of anticoagulation (especially INR >4), history of cerebral vascular disease (recent or remote), and concomitant use of drugs that interfere with haemostasis (aspirin or non-steroidal anti-inflammatory drugs) are probably the most important variables determining patients' risk of major life threatening bleeding complications while they are receiving anticoagulation treatment.
Variables that influence the risk of bleeding in elderly people
Increased sensitivity to the effect of anticoagulation, perhaps due to increased receptor affinity or lower dietary vitamin K intake
Concurrent use of drugs that increase bleeding risk
Associated comorbidity and other diseases that decrease compliance and increase the risk of bleeding
Generally elderly people have increased sensitivity to the anticoagulant effect of warfarin, and require a lower mean daily dose to achieve a given anticoagulant intensity. For example, patients aged >75 years need less than half the daily warfarin dose of patients aged <35 for an equivalent level of anticoagulation. Whatever the mechanism it is clear that warfarin therapy needs careful justification for being given to elderly patients, and the dose needs modification and careful monitoring.
As there is an exponential increase in bleeding risk with a linear increase in anticoagulant effect, there will be a substantial increase in bleeding risk with overanticoagulation. For example, the annual risk of bleeding rises from 1.6% in elderly people not treated with anticoagulant drugs (based on the “Sixty-Plus” study), to 5% (relative risk 3) at an INR of 2.5, and to 50% (relative risk 30) at an INR of 4. In another study, total bleeding events were 39% in a group of 31 patients with an INR of 7 compared with 13% in a group of 100 with a stable INR (odds ratio 5.4, 95% CI 2.1-13.9). The greatest risk factor for being in this group was (apart from having a high target INR) antibiotic therapy in the preceding four weeks.
Reasons for increased sensitivity to anticoagulation in elderly people
Lower body weight
Differences in pharmacokinetics, with a tendency towards reduced drug clearance in the elderly either due to decreases in renal or hepatic blood flow and function with age per se or disease processes
Change in receptor sensitivity
Lower dietary vitamin K intake in the elderly may perhaps be the more important cause
Multiple drug therapy or polypharmacy is quite common, with the consequence of adverse drug interactions, the risk of which rises exponentially with the number of drugs given simultaneously and with concurrent diseases. Typical drug interactions include changes in absorption across intestinal mucosae and hepatic metabolism. Patients should be cautioned about the risk of warfarin-drug interactions when their medication list is altered. The decline in cognitive function in some elderly patients may mean they do not realise that some drugs can interact with anticoagulants and so they do not mention their use of oral anticoagulants to doctors or pharmacists. However, elderly patients are likely to attend clinic less often than younger patients, suggesting a greater degree of INR stability.
Further reading
Blann AD, Hewitt J, Siddique F, Bareford D. Racial background is a determinant of average warfarin dose required to maintain the INR between 2.0 and 3.0. Br J Haematol 1999;10:207-9
Erhardtsten E, Nony P, Dechavanne M, Ffrench P, Boissel JP, Hedner U. The effect of recombinant factor VIIa (NovoSevenTM) in healthy volunteers receiving acenocoumarol to an International Normalized Ratio above 2.0. Blood Coag Fibrin 1998;9:741-8
Fitzmaurice DA, Hobbs FDR, Murray ET, Hodder, RL, Allan TF, Rose, PE. Oral anticoagulation management in primary care with the use of computerised decision support and near-patient testing. A randomised controlled trial. Arch Intern Med 2000;160:2323-48
Gurwitz JH, Goldberg RJ, Holden A, Knapic N, Ansell J. Age-related risks of long term oral anticoagulant therapy. Arch Intern Med 1988;148:1733-6
He J, Whelton PK, Vu B, Klag MJ. Aspirin and risk of haemorrhagic stroke. JAMA 1998;280:1930-5
Haemostasis and Thrombosis Task Force of the British Society for Haematology. Guidelines on oral anticoagulation: third edition. Br J Haematol 1998;101:374-87
Landefeld CS, Beyth RJ. Anticoagulant related bleeding: clinical epidemiology, prediction, and prevention. Am J Med 1993;95:315-28
Levine MN, Hirsh J, Landefeld CS, Raskob G. Haemorrhagic complications of anticoagulant treatment. Chest 1992;102:352-63S
Panneerselvan S, Baglin C, Lefort W, Baglin T. Analysis of risk factors for over-anticoagulation in patients receiving long-term warfarin. Br J Haematol 1998;103:422-4
Palareti G, Leali N, Coccheri S, Poggi M, Manotti C, D'Angelo A, et al. Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Lancet 1996;348:423-8
van der Meer FJM, Rosendaal FR, Vandenbroucke, Briet E. Bleeding complications in oral anticoagulant therapy. Arch Int Med 1993;153:1557-62
Many diseases associated with stroke and thromboembolism are more common with increasing age. Older patients are often at highest risk, and appropriate anticoagulation therapy reduces morbidity and mortality. Careful and continuing evaluation of patients is necessary to ensure that the risks of bleeding do not outweigh the benefits from anticoagulation.
Figure.
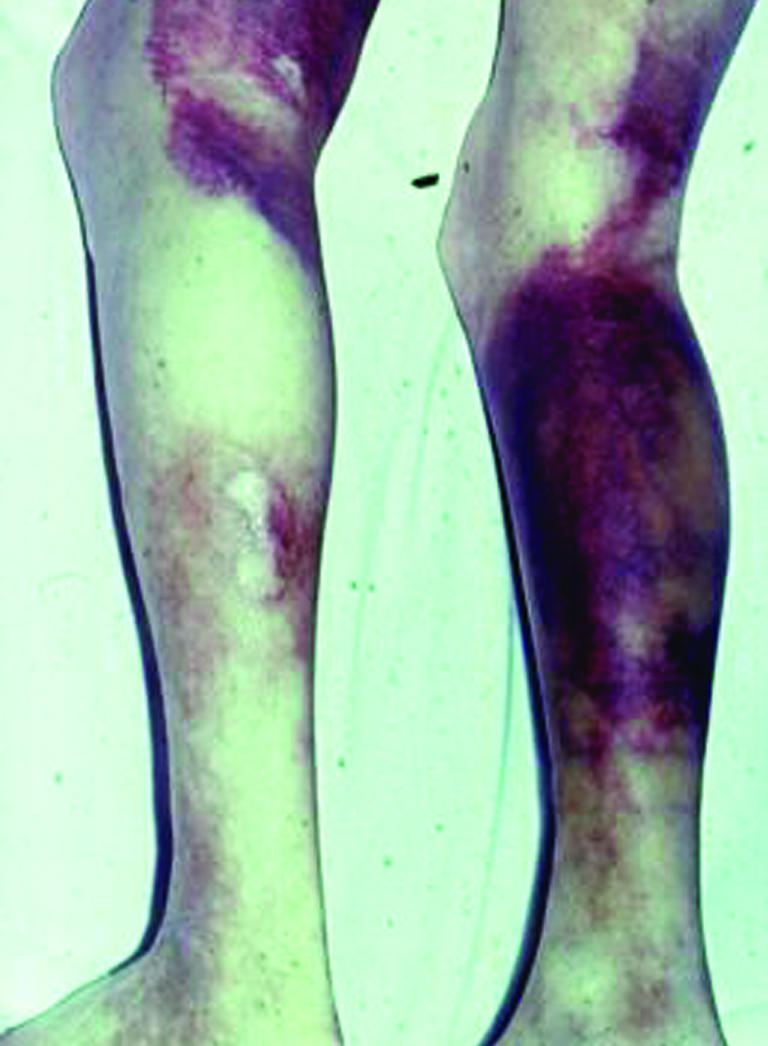
Purpura, petechiae, and haematoma secondary to overcoagulation
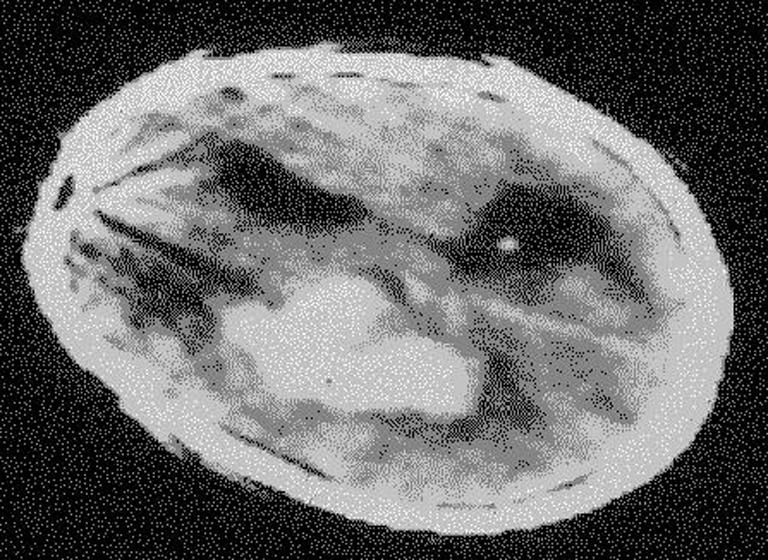
Figure.
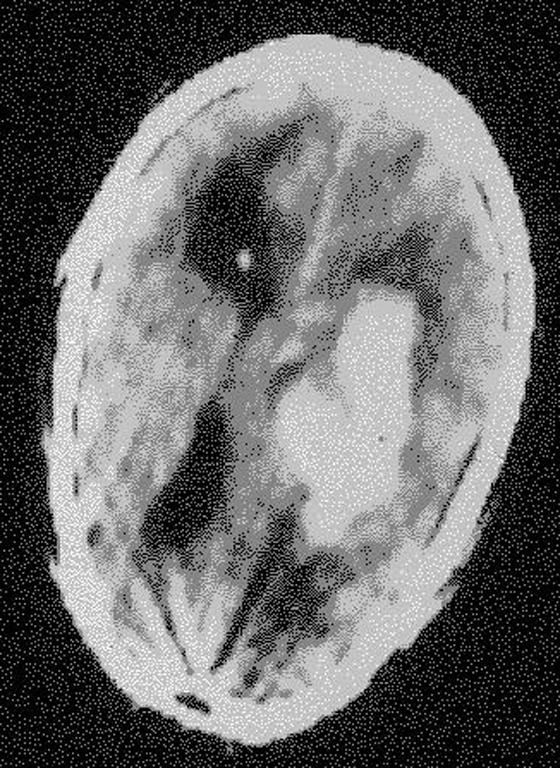
Computed tomography scan showing intracerebral haemorrhage
Figure.
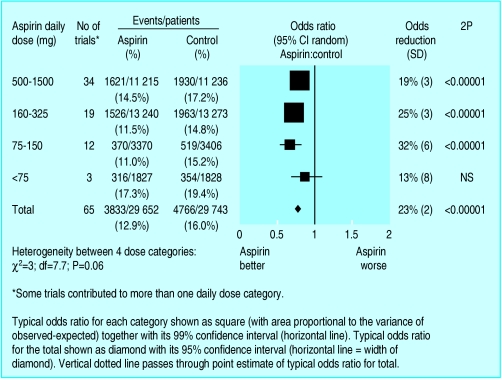
Myocardial infarction, stroke, and bleeding in hypertension optimal trial (HOT) (ASP=aspirin, PLA=placebo)
Figure.
Effect of different doses of aspirin in secondary prevention of vascular events
Acknowledgments
The diagram showing the results of the hypertension optimal trial is adapted from Hansson L, et al. Lancet 1998;351:1755-62. The figure showing the effect of different doses of aspirin in secondary prevention of vascular events is reproduced from Clinical Evidence (June issue 7), BMJ Publishing Group, 2002.
Footnotes
David Fitzmaurice is reader in primary care and general practice at the University of Birmingham. Andrew D Blann is senior lecturer in medicine, and Gregory Y H Lip is professor of cardiovascular medicine, both at the haemostasis thrombosis and vascular biology unit, university department of medicine, Cith Hospital, Birmingham.
The ABC of antithrombotic therapy is edited by Gregory Y H Lip and Andrew D Blann. The series will be published as a book in spring 2003.