Abstract
Background
Women experiencing problematic menopausal symptoms report lower health-related quality of life and greater healthcare use than women without symptoms. Not all women want to or are able to take hormone replacement therapy. Strengthening the evidence for menopause symptom-management options, including physical activity, improves agency for women.
Aim
This overview assesses effectiveness of physical activity and exercise interventions targeting women experiencing menopause symptoms.
Methods
Medline, Embase, CINAHL, Scopus, The Cochrane Database of Systematic Reviews and Social Science Citation Index were searched (June 2023) for systematic reviews of physical activity and exercise interventions targeting women experiencing menopause. Reviews were assessed using AMSTAR-2 and a best-evidence approach to synthesis without meta-analysis (SWIM) was adopted. The protocol was registered on PROSPERO (CRD42022298908).
Results
Seventeen reviews included 80 unique relevant primary studies with 8983 participants. There is evidence showing improvement of physical, urogenital, and total symptoms following yoga interventions. Evidence for vasomotor and psychological symptoms was inconclusive. Findings for aerobic exercise were inconclusive although there were some examples of beneficial effects on total and vasomotor symptoms. Evidence was very limited for other types of physical activity and impact on physical, sexual and urogenital symptoms.
Conclusion
There is some evidence that yoga, and to lesser extent, aerobic exercise may be beneficial for some menopause symptoms, but there is insufficient evidence to recommend a particular form of exercise. Current reviews categorise women on menopause status; broadening this to include ethnicity, income status, employment and other factors will allow better understanding of context for successful interventions.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12905-024-03243-4.
Keywords: Menopause, Symptom management, Physical activity/Exercise, Quality of life, Overview of reviews
Introduction
The menopause - defined as cessation of menstrual periods - is a gradual, naturally occurring process for women that typically occurs between 42 and 55 years of age [1]. Problems ‘below the waist’ are often unattractive topics for public or political discourse; the UK Government’s recent publication of the Women’s Health Strategy [2] and establishment of the Menopause Task Force [3] have increased attention in the UK.
Many women (around 80%) experience sometimes debilitating symptoms associated with oestrogen and testosterone depletion for an average of four (but up to 12) years. These include hot flushes, night sweats, sleep disruption, fatigue, difficulty concentrating, depression and anxiety, mood swings, irritability, and loss of confidence [1]. Women experiencing problematic menopausal symptoms report lower levels of health-related quality of life and greater use of healthcare than women without symptoms. Prolonged lack of oestrogen impacts the cardiovascular system and can increase risk of long-term conditions including osteoporosis [4]. Although many women experience problematic menopause symptoms, many fewer use Hormone Replacement Treatment (HRT) [5].
Emerging evidence suggests physical activity may be beneficial [6] for alleviating some menopausal symptoms and helping prevent diseases with increased risk during menopause. Physical activity can be categorised into occupational, sports, conditioning, household, or other activities. Exercise is physical activity that is planned, structured, and repetitive and has improvement or maintenance of physical fitness as an objective [7]. There is strong evidence that, throughout life, physical activity is protective against chronic conditions including coronary heart disease, obesity, type 2 diabetes, and mental health problems [8]. UK recommendations are clear about the benefits of physical activity, importance of strength training, and amount of recommended weekly activity [9].
However, women may reduce physical activity during menopause transition [10]. In England 38% of women aged 45–54 years do less than the weekly recommended 150 min moderate activity, and 60% of adult women do less than twice weekly strength training [11]. The ‘Women in Sport’ report [10] found that, although physical activity levels were low, menopausal women’s desire to be more active was high, and increased when recommended by a health professional. Many women with menopause symptoms may seek medical advice from their GP. However, not all women want to, or are able to take, or access, HRT. Strengthening the evidence-base for all intervention options may improve agency over menopause symptom management for women [5].
Aim
This overview aims to assess the effectiveness of physical activity and exercise interventions targeting women experiencing menopause. There are multiple recent and ongoing systematic reviews in this area, but no existing overview [12–14].
Methods
The overview protocol was registered on PROSPERO (CRD42022298908) [15] which is an international prospective register of systematic reviews. This platform allows authors to view systematic reviews in progress and also improves accountability for authors to justify any decisions made to change their original published protocol. It was conducted using guidance from the Cochrane Handbook for Systematic Reviews of Interventions [16] and reported following the Preferred Reporting Items for Overviews of Reviews (PRIOR) [17].
Inclusion criteria
The PICO (population, intervention, comparator, outcomes) inclusion criteria are provided in Box 1.
Box 1.
Inclusion criteria for systematic reviews
| Population |
We included women with spontaneous or surgical menopause, in the peri-menopausal or postmenopausal period. Perimenopause is the interval in which a woman has irregular cycles of ovulation and menstruation before the menopause. Postmenopausal women are defined as those with surgical or spontaneous menopause and amenorrhoea for longer than 12 months. |
| Interventions | We included systematic reviews that evaluated physical activity or exercise interventions undertaken to reduce menopausal symptoms in women. Physical activity or exercise is defined as any bodily movement produced by skeletal muscles that results in energy expenditure. We placed no limits on how the activity is delivered and included both instructor-led or self-led programmes, accepting review authors’ definitions of activity. The types of interventions included, but were not limited to: Yoga; Resistance or strength training; Aerobic exercise; Walking; Flexibility or stretching training (including Pilates, Tai Chi, Qi Gong). |
| Comparator | We included systematic reviews that compared any type of exercise or physical activity with no active treatment, another type of exercise or physical activity, or with other treatments such as HRT as controls. |
| Outcomes |
We included both menopause symptoms as a class, and specific types of symptoms. Types of menopause symptoms were broadly categorised as follows: vasomotor (hot flushes and night sweats), physical (musculoskeletal pain, headaches, palpitations, sleep problems, reduced muscle mass), urogenital symptoms (vaginal dryness), sexual difficulties (low sexual desire), psychological (low mood / anxiety, concentration problems) [1]. We also included a category for ‘total’ symptoms (i.e. vasomotor plus physical plus urogenital plus sexual plus psychological) which is the same term used in the MENQOL instrument [18, 19] and includes quality of life. We considered all symptom outcomes to be equally important. Improvement in menopause symptoms had to be assessed by one or more of a range of validated tools for both the intervention and the control groups. These could be generic or menopause specific instruments and included the following: Global QoL [20]; 36-item Short Form Health Survey (SF-36) [21]; World Health Organization QoL [22]; Utian QoL [23], Menopause-specific QoL [18, 19]; International Incontinence questionnaire [24]; Sexual Activity questionnaire [25]; Greene Climacteric scale [26]; Women’s health questionnaire [27]; Hot Flash Related Daily Interference Scale [28]. |
Types of studies
We included systematic reviews (with or without meta-analysis). Systematic reviews were defined using criteria from the Database of Abstracts of Reviews of Effects [29]. Reviews had to have: clear inclusion/exclusion criteria; adequate search strategy; synthesis of studies; and quality assessment of studies. Reviews reported only as conference abstracts, or not published in English, and review protocols were excluded.
Search strategy
In June 2023 we searched Medline, Embase (both OvidSP), CINAHL (EBSCO), Scopus (Elsevier), The Cochrane Database of Systematic Reviews and Social Science Citation Index (Clarivate); reference lists were also searched. These databases were chosen based on previous reviews on a similar topic. Date limitation (2000 onwards) was used because a Medline search produced no prior results and because validated tools and instruments were not previously routinely used for menopause symptoms [30]. The strategy combined keywords relating to physical activity, exercise, menopausal symptoms and study design (see Supplementary Table 3 for example search strategy). Only reviews written in the English language were included.
Selection criteria
Two independent reviewers (AM and DH/AMK) used the systematic review organisational web tool, Rayyan [31] to review both abstracts and full text articles of potentially relevant studies. This ensures robust screening of papers and reduces the risk of bias as papers are blinded until screening is complete. At each stage disagreements were resolved through discussion with a third reviewer (CET).
Data extraction and management
A data extraction table was created based on Cochrane guidance for overview of reviews [16]. Two reviewers (AM and AMK/DH) extracted data including: review methods and characteristics; participants and interventions; outcome data; and demographic characteristics in line with PROGRESSplus which is a validated list of characteristics known to affect health outcomes and equity [32]. PROGRESS refers to Place of residence; Race/ethnicity/culture/language; Occupation; Gender/sex; Religion; Education; Socioeconomic status; Social capital and PLUS refers to: (1) personal characteristics associated with discrimination (e.g. age, disability) (2) features of relationships (e.g. smoking parents, excluded from school 3) time-dependent relationships (e.g. leaving the hospital, respite care, other instances where a person may be temporarily at a disadvantage).
Methodological quality
Two reviewers (AM and AMK) independently assessed reviews using the AMSTAR-2 [33] (Assessing the Methodological Quality of Systematic Reviews) tool to generate overall ratings of ‘high’, ‘moderate’, ‘low’ or ‘critically low’ based on 16 questions/items, of which seven are deemed critical. The review team discussed critical domain weaknesses to produce consensus judgements. This tool was chosen as it is appropriate for systematic reviews that include both randomised and non-randomised trials.
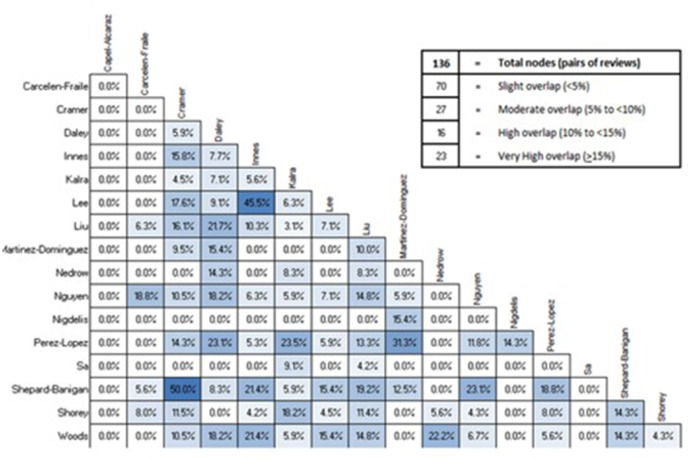
Overlap
To assess overlap in included primary studies between reviews, the corrected covered area (CCA) [34] was calculated using GROOVE (Graphical Representation of Overlap for Overviews). This software calculates the percentage of studies that appear in two reviews. This was to ensure primary studies were not counted more than once which would potentially give false weighting to a result. A CCA score or > 15% indicates very high overlap.
Synthesis
We used an approach guided by the SWiM [35] (synthesis without meta-analysis) methodology, and key aspects of this approach are as follows. We considered two main types of comparison: physical activity versus no intervention and comparisons between two different types of activity. The synthesis was further grouped by activity type and then by symptoms. We used a best-evidence approach to focus on reviews with high-quality AMSTAR-2 ratings published within the past 10 years. Guided by GRADE domains, we also considered risk of bias, imprecision and inconsistency of evidence within each review and overall [36].
Results
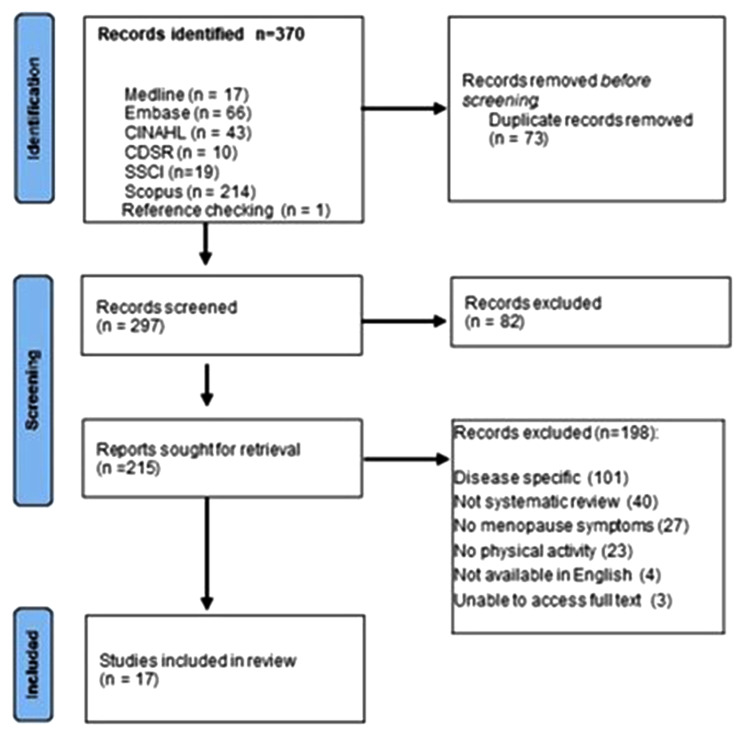
We identified 370 records (Fig. 1). Following deduplication, we assessed 297 abstracts and 215 full texts, and included seventeen systematic reviews [6, 14, 37–51].
Fig. 1.
PRISMA flowchart of data selection
Description of included reviews
Main review characteristics are presented in Table 1. From these reviews we extracted 80 unique studies (71 RCTs) and 8983 participants once overlap has been accounted for; study overlap is shown in Fig. 2. Reporting on demographic characteristics in line with PROGRESSPlus [32] guidance was limited.
Table 1.
Summary of included systematic reviews
| Author/Year | No. of studies included in overview* (Population) | Intervention type | Duration / Frequency / Session Length | Symptom category | AMSTAR2 |
|---|---|---|---|---|---|
| Carcelen-Fraile et al. (2020) [37] | 11 studies: 8 RCTs, 1 feasibility, 1 prospective, 1 pre-post study (1548) |
Pelvic floor muscle training (PFM) Aerobic exercise Yoga Mind-body therapy. |
Duration 12 weeks (range = 8 weeks - 24 months) Frequency: 1-5 times per week Length: 30–120 min |
Total Vasomotor Physical Sexual |
Low |
| Capel-Alcaraz et al. (2023) [49] | 4 RCTs (274) | Resistance training |
Duration: 12 – 52 weeks Frequency: 1-3 times per week Length: 55–60 min |
Vasomotor Total |
Low |
| Cramer et al. (2018) [38] | 13 RCTs (1306) | Yoga |
Duration: 4–16 (median 12) weeks, Frequency: 1–14 (median 2) times per week, Length: 20–120 (median 60) minutes per session |
Total Vasomotor Psychological Physical Urogenital |
High |
| Daley et al. (2014) [6] | 5 RCTs (733) | Aerobic exercise |
Duration: 3-6 months Frequency: 3-7 times per week Length: 40–60 min |
Vasomotor | High |
| Innes et al. (2010) [39] | 9 studies: 3 RCTs, 5 uncontrolled clinical trials, 1 nonrandomised controlled trial (484) |
Mind-body therapy Yoga |
Duration: 16-week programme (Tai Chi) Frequency: 1/2 - 5 sessions/week Length: 60–150 min |
Total Vasomotor Psychological Physical |
Moderate |
| Kalra et al. (2022) [40] | 10 RCTs (833) |
Aerobic exercise Yoga Resistance training Mind-body therapy |
Duration: 6-52 weeks Frequency: 2-3 per week Length: 40–60 min |
Total Psychological Physical |
Critically low |
| Lee et al. (2009) [41] | 7 studies, 3 RCTs, 1 controlled clinical trial, 3 uncontrolled clinical trial (470) | Yoga |
Duration: 8-12 weeks Frequency: 2-3 times per week Length: 60–90 min |
Total Vasomotor Psychological Physical |
Low |
| Liu et al. (2022) [51] | 21 RCTs (2884) |
Aerobic exercise Yoga Resistance training Mind-body therapy |
Duration: 3-48 weeks Frequency: 1-7 sessions a week Length: 30–120 min |
Vasomotor | High |
| Martinez-dominguez et al. (2018) [48] | 10 RCTs (1463) |
Yoga Aerobic exercise Resistance training Moderate-high intensity Low intensity Medium-term Long-term |
Duration ranged from 12 weeks to 14 months. ‘Mid-term exercise intervention’ (MTEI) = 12 weeks - 4 months ‘Long-term exercise intervention’ (LTEI) = 6-14 months |
Psychological | High |
| Nedrow et al. (2006) [42] | 3 RCTs (284) | Aerobic exercise |
Duration: 6-52 weeks Frequency: 3 per week or 225 min per week. Length: Not reported |
Total Vasomotor Psychological Physical |
Moderate |
| Nguyen et al. (2020) [14] | 9 RCTs (882) |
Pelvic floor muscle training (PFM) Yoga Aerobic exercise |
Duration: 4 weeks – 6 months, Frequency: 1-7 times per week Length: 20–90 min |
Total Vasomotor Psychological Physical Sexual Urogenital |
High |
| Nigdelis et al. (2018) [43] | 5 RCTs (2112) |
Aerobic exercise Resistance training Mind-body therapy Medium-term exercise Long-term exercise Moderate-high intensity Low intensity |
Duration: 6 - 24 months Frequency: 3-5 per week Length: 30–60 min |
Vasomotor Psychological Physical |
Critically low |
| Perez-Lopez et al. (2017) [44] | 11 RCTs (1943) |
Medium-term exercise Long-term exercise |
Duration: 6 weeks - 12 months (MTEI = 12 weeks - 4 months & LTEI = 6-12mths) Frequency: 2-5 per week Length: 40–90 min |
Psychological | Low |
| Sa et al. (2022) [50] | 2 RCTs (94) |
Resistance training Aerobic exercise |
Duration: 8 weeks & 15 weeks Frequency: 3 per week Length: Not reported |
Vasomotor | High |
| Shepherd-Banigan et al. (2017) [45] | 8 RCTs (927) |
Yoga Mind-body therapy |
Duration: 10-13 weeks Frequency: 1-7 per week Length: 15–90 min |
Vasomotor Psychological |
High |
| Shorey et al. (2020) [46] | 15 RCTs (1337) |
Mind-body therapy Aerobic exercise Resistance training Yoga |
Duration: 1-24 weeks Frequency: Not reported Length: Not reported |
Total Vasomotor |
High |
| Woods et al. (2014) [47] | 7 RCTs (1056) |
Yoga Mind-body therapy Aerobic exercise |
Duration: 3 weeks - 12 months Frequency: 1-5 weeks Length: 20–60 min |
Vasomotor Psychological Physical |
Critically low |
*Prior to overlap correction (CCA)
Fig. 2.
Corrected Coverage Area (CCA) for included reviews
Interventions included: aerobic exercise (11 reviews); yoga (11 reviews); other forms of mind-body therapy, such as stretching and relaxation, Tai Chi and Qi Gong (eight reviews); resistance/strength exercises (seven reviews); and pelvic floor muscle training (two reviews). Yoga is categorised separately to mind-body therapy due to the large number of reviews focusing solely on yoga. Intervention durations varied from one week to 24 months. Session length ranged from 20 to 120 min and frequency from 0.5 to 7 times per week. Comparators included: no active treatment, wait-list controls, health education or alternative exercise. Two RCTs in the reviews used HRT as a comparator but this was not reported at review level. Table 2 shows assessed comparisons and symptoms reported.
Table 2.
Evidence map by symptom category and comparison
Eight reviews were rated high quality [6, 14, 38, 45, 46, 48, 50, 51] via AMSTAR-2, the remainder were moderate [39, 42], low [37, 41, 44, 49] or critically low quality [40, 43, 47] (Supplementary Table 2). The most common issues were lack of protocol before conducting the search, not justifying exclusion decisions, and not considering bias assessment in discussion of individual results. We summarise only the high-quality effectiveness evidence here; detailed results including effect estimates are in Table 3. Detailed results of moderate, low, and critically low-quality evidence are summarised in Supplementary Table 1.
Table 3.
Summary of findings (high quality reviews only)
| Outcome | Review | SMD | 95%CI | I² | RCTs | Participants | ROB | |||
|---|---|---|---|---|---|---|---|---|---|---|
| High | Low | Unclear | ||||||||
| Aerobic exercise vs. no intervention | ||||||||||
| Total | Nguyen | 0.23 | -0.1 to 0.56 | 59% | 5 | 441 | 1 | X | 4 | |
| Shorey | -0.69 | -1.09 to –0.28 | 0% | 2 | 101 | X | 1 | 1 | ||
| Vasomotor | Daley | -0.10 | -0.33 to 0.13 | 30% | 3 | 454 | 1 | X | 2 | |
| Nguyen | -0.14 | -0.42 to 0.15 | 63% | 5 | 602 | 1 | X | 4 | ||
| Shorey | -0.26 | -0.70 to 0.17 | 76% | 4 | 358 | X | 2 | 2 | ||
| Liu (Frequency) | 0.14 | -0.03 to 0.31 | 35% | 7 | 940 | 4 | 2 | 10 | ||
| Liu (Severity) | 0.25 | 0.04 to 0.47 | 72% | 11 | 1425 | 4 | 2 | 10 | ||
| Liu (Severity index) | 0.67 | 0.17 to 1.17 | 46% | 3 | 127 | 4 | 2 | 10 | ||
| Psychological | Nguyen | 0.56 | -0.04 to 1.15 | 93% | 6 | 812 | 1 | X | 5 | |
| Physical | Nguyen | 0.89 | -0.11 to 1.89 | 97% | 5 | 660 | 1 | X | 4 | |
| Urogenital | Nguyen | -0.79 | -1.92 to 0.34 | 85% | 2 | 204 | X | X | 2 | |
| Sexual | Nguyen | -0.19 | -0.43 to 0.04 | 36% | 4 | 494 | 1 | X | 3 | |
| Low intensity exercise vs. no intervention | ||||||||||
| Psychological | Martinez-Dominguez | -0.58 | -1.39 to 0.24 | 93% | 4 | 460 | X | 2 | 2 | |
| Moderate to high intensity exercise vs. no intervention | ||||||||||
| Psychological | Martinez-Dominguez | -0.06 | -0.22 to 0.09 | 41% | 7 | 1250 | X | X | 7 | |
| Short to medium term exercise vs. no intervention | ||||||||||
| Total | Shorey | -0.70 | -1.22 to -0.18 | 76% | 5 | 282 | X | 2 | 3 | |
| Psychological | Martinez-Dominguez | -0.42 | -0.81 to -0.02 | 87% | 7 | 939 | X | 2 | 5 | |
| Long term exercise vs. no intervention | ||||||||||
| Psychological | Martinez-Dominguez | -0.03 | -0.18 to 0.13 | 29% | 5 | 1013 | X | X | 5 | |
| Yoga vs. no intervention | ||||||||||
| Total | Cramer | -1.05 | -1.57 to -0.53 | 88% | 8 | 671 | Bias not reported at primary study level. | |||
| Vasomotor | Cramer | -0.76 | -1.27 to -0.25 | 85% | 8 | 548 | Bias not reported at primary study level. | |||
| Nguyen | -0.37 | -1.15 to 0.4 | 82% | 3 | 179 | Bias not reported at primary study level. | ||||
| Shepherd-Banigan | -0.34 | -0.92 to 0.25 | 0% | 3 | 204 | Bias not reported at primary study level. | ||||
| Psychological | Cramer | -0.75 | -1.17 to -0.34 | 84% | 10 | 756 | Bias not reported at primary study level. | |||
| Nguyen | 0.76 | -0.30 to 1.81 | 95% | 4 | 433 | 1 | X | 3 | ||
| Shepherd-Banigan | -0.32 | -0.47 to -0.17 | 0% | 6 | 707 | 4 | 1 | 1 | ||
| Physical | Cramer | -0.65 | -1.05 to -0.25 | 82% | 9 | 718 | Bias not reported at primary study level. | |||
| Nguyen | 1.39 | 0.19 to 2.59 | 93% | 3 | 333 | X | X | 3 | ||
| Urogenital | Cramer | -0.53 | -0.81 to -0.25 | 61% | 7 | 661 | Bias not reported at primary study level. | |||
| Sexual | Nguyen | -0.36 | -1.18 to 0.46 | 81% | 2 | 150 | X | X | 2 | |
| Mind-body therapies vs. no intervention | ||||||||||
| Total | Shorey | -1.51 | -2.64 to -0.37 | 78% | 2 | 92 | X | 1 | 1 | |
| Resistance training vs. no intervention | ||||||||||
| Total | Shorey | -0.67 | -1.51 to 0.18 | NA | 1 | 23 | X | X | 1 | |
| Pelvic floor training vs. no intervention | ||||||||||
| Total | Nguyen | 0.76 | -0.40 to 1.92 | 78% | 2 | 59 | X | X | 2 | |
| Aerobic exercise vs. yoga | ||||||||||
| Total | Cramer | -0.21 | -0.66 to 0.25 | 77% | 4 | 386 | Bias not reported at primary study level. | |||
| Vasomotor | Cramer | -0.45 | -0.87 to -0.04 | 72% | 3 | 373 | Bias not reported at primary study level. | |||
| Daley | -0.03 | -0.45 to 0.38 | 61% | 2 | 279 | 1 | X | 1 | ||
| Shepherd-Banigan (1 of 2 RCTs not combined within review) | -0.40 | -0.78 to -0.02 | NA | 1 | 108 | 1 | X | X | ||
| Shepherd-Banigan (2 of 2 RCTs not combined within review) | -0.15 | -0.41 to 0.11 | NA | 1 | 233 | X | X | 1 | ||
| Liu | 0.15 | -0.06 to 0.35 | 13% | 3 | 432 | 1 | 1 | 1 | ||
| Psychological | Cramer | -0.09 | -0.47 to 0.28 | 76% | 5 | 526 | Bias not reported at primary study level. | |||
| Physical | Cramer | -0.15 | -0.55 to 0.26 | 79% | 4 | 483 | Bias not reported at primary study level. | |||
| Urogenital | Cramer | -0.12 | -0.53 to 0.3 | 74% | 3 | 376 | Bias not reported at primary study level. | |||
| Aerobic vs. resistance | ||||||||||
| Vasomotor | Sa | -2.60 | -9.01 to 3.81 | NA | 1 | 36 | 1 | X | X | |
| Physical | Sa | -5.90 | -16.17 to 4.37 | NA | 1 | 36 | 1 | X | X | |
| Psychological | Sa | -2.90 | -8.24 to 2.44 | NA | 1 | 36 | 1 | X | X | |
| Sexual | Sa | 0.40 | -4.37 to 5.17 | NA | 1 | 36 | 1 | X | X | |
Comparison 1 – Exercise vs. no intervention
Aerobic exercise vs. no intervention
Total menopause symptoms
Two recent, high-quality reviews [14, 46] assessed the effect of aerobic exercise on total menopause symptoms (seven RCTs, 542 participants). There is no primary study overlap between these high-quality reviews because of different inclusion criteria. One review [46] (two RCTs, 101 participants), showed a beneficial effect of aerobic exercise, the second review [14] (five RCTs, 441 participants) reported no effect of interventions.
Vasomotor symptoms
Four high-quality reviews reported vasomotor symptoms [6, 14, 46, 51] (21 RCTs, 2219 participants). Three reviews consistently reported no clear effect of aerobic exercise. Evidence from all three reviews [6, 14, 46] is impacted by imprecision, one review’s GRADE assessment was low certainty evidence [6]. One review separately analysed frequency and severity of vasomotor symptoms, finding no clear effect on frequency but a beneficial effect of aerobic exercise on severity [51].
Other symptoms
One high-quality review [14] found no clear effect for the four following symptom categories: psychological, physical, urogenital, sexual. For each outcome there was high heterogeneity, at least one study at high risk of bias, or both (Table 3).
Exercise intensity: low
Psychological symptoms
Three reviews assessed low intensity exercise (including walking and yoga) [43, 44, 48] one was high-quality [48]. The high-quality review found no clear effect based on four RCTs (460 participants). The evidence was impacted by imprecision.
Exercise intensity: moderate-high
Psychological symptoms
Three reviews assessed moderate to high intensity exercise for psychological symptoms [43, 44, 48] one was high-quality [48]. Moderate intensity exercise was consistently defined across all three reviews; aerobic and cardiovascular activity were considered moderately intense. The high-quality review found no clear effect based on seven RCTs (1250 participants).
Exercise duration
Both ‘short to medium term exercise’ and ‘long term exercise’ versus no intervention were assessed by four reviews [43, 44, 46, 48] two were high quality [46, 48].
Short to medium-term exercise (up to 6 months)
Total symptoms
One high-quality review [46] assessed between one and 24 weeks exercise and found a benefit based on five RCTs (282 participants).
Psychological symptoms
The second high-quality review [48] assessed up to 12 weeks of exercise for psychological symptoms and found a benefit based on seven RCTs (939 participants).
Long-term exercise (over 6 months)
Psychological symptoms
One high-quality review [48] assessed long-term exercise for psychological symptoms (five RCTs, 1013 participants) and found no effect. The evidence is impacted by high risk of bias.
Yoga versus no intervention
Total symptoms
One high-quality review [38] (eight RCTs, 671 participants) found a benefit on total menopause symptoms. This review included some studies at high risk of bias, but it was unclear how many such studies contributed to the effect.
Vasomotor symptoms
Three high-quality reviews [14, 38, 45] found differing results. One review [38] (eight RCTs, 548 participants), found a benefit of yoga. Two reviews [14, 45] (eleven RCTs and 383 participants) found no effect of interventions.
Psychological symptoms
Three high-quality reviews [14, 38, 45] included ten, four and six RCTs respectively when assessing the impact of yoga on psychological symptoms but the number of unique RCTs and participants is unclear. One review [45] showed a benefit of yoga; the other reviews found no clear effects [14, 38]. All reviews were impacted by high risk of bias in studies with substantial numbers of participants.
Physical symptoms
Two high-quality reviews [14, 38] (11 RCTs, unclear number of participants), found a benefit of yoga. Symptoms included were sleep, joint pain and fatigue. One review [38] included some high risk of bias studies but their relevance to this outcome is unclear.
Urogenital symptoms
One high-quality review [38] found a benefit of yoga from a meta-analysis of seven RCTs (661 participants). Review authors reported moderate heterogeneity (61%) and some high risk of bias.
Sexual symptoms
One high-quality review [14] found no effect of interventions from two RCTs (150 participants). This is strongly impacted by imprecision because of small numbers of participants.
Mind-body therapy versus no intervention
Total symptoms
One high-quality review [46] found a positive effect favouring mind-body therapy based on two RCTs (92 participants). This review is impacted by high levels of imprecision because of the small number of participants.
Resistance exercise versus no intervention
In both total and vasomotor symptoms evidence is very limited despite high-quality reviews.
Total symptoms
One high-quality review [46] included a single very small study (23 participants) which found no effect on total menopause symptoms. Very high levels of imprecision limit the certainty of this finding.
Vasomotor symptoms
One high-quality review [50] reported a benefit of resistance training on incidence of moderate or severe hot flash episodes. This is based on a single, very small RCT (58 participants) and the effect estimate reflects high levels of imprecision.
Pelvic floor training versus no intervention
Total symptoms
One high-quality review [14] found no effect based on two RCTs (59 participants). Again, small numbers of participants mean evidence is very imprecise.
Comparison 2: Different types of exercise compared with each other
Aerobic exercise versus yoga
Total symptoms
One high-quality review [38] found no difference between aerobic exercise and yoga based on four RCTs (386 participants). While the review included some studies with high risk of bias it is unclear how many of these contributed to this evidence.
Vasomotor symptoms
Four high-quality reviews [6, 38, 45, 51] had mixed findings. One review [38] (three RCTs, 373 participants) found an effect in favour of yoga. This review included some studies at high risk of bias, but it was unclear how many contributed to the effect. Two reviews [6, 51] (two RCTs, 279 participants and three RCTs, 432 participants) each found no clear differences between aerobic exercise and yoga. A fourth review did not pool the two included RCTs (432 participants); one of these showed a benefit of yoga [45].
Other symptoms
One high-quality review [38] assessed aerobic exercise versus yoga on psychological (five RCTs, 526 participants), physical (four RCTs, 483 participants) and urogenital symptoms (three RCTs, 376 participants). There were no clear differences between the groups for any symptoms. This review included some high risk of bias studies, but it was unclear how many contributed to the effect estimates.
Aerobic exercise versus resistance training
Total symptoms
One high-quality review [50] included one RCT (36 participants) comparing aerobic versus resistance training for 8 weeks. No differences were observed in total menopause quality-of-life domains. This result is subject to a high level of imprecision due to the small sample size.
Vasomotor symptoms
One high-quality [50] review reported an effect favouring resistance training over aerobic exercise on frequency of hot flash symptoms based on one RCT (36 participants). Due to the small sample size, this result is subject to a high level of imprecision.
Discussion
This overview identified seventeen systematic reviews which included 80 relevant primary studies (8983 unique participants). Eight high-quality reviews evaluated various forms of physical activity. Fifteen reviews compared an activity to no intervention, eleven reviews researched aerobic exercise and eleven reviews researched yoga interventions, with limited evidence for other interventions. Nine reviews related to total symptom measures, vasomotor and psychological symptoms, with very limited evidence for physical, sexual, urogenital symptoms. Key limitations of the evidence from high-quality reviews were high risk of bias in primary studies, differences between review findings and heterogeneity between studies within reviews, and in some instances very high levels of imprecision due to few studies with very small numbers of participants. All of these reduce our confidence in the evidence.
Yoga was the intervention with most evidence (11 reviews) in terms of numbers of primary studies. There is evidence showing improvement of physical, urogenital, and total symptoms following yoga interventions two to three times weekly. Evidence for vasomotor and psychological symptoms was inconclusive. Session lengths and intervention durations varied, ranging from 20 to 120 mins and from three weeks to 24 months respectively. Findings for aerobic exercise were inconclusive although there were some examples of beneficial effects on total and vasomotor symptoms. Findings directly comparing yoga with aerobic exercise varied; it is unclear whether their effects differ. Evidence for resistance training was very limited. Based on the evidence synthesised in this overview, there is insufficient good quality evidence to recommend one form of exercise over any other. There is clear need for further high quality RCTs in this area to identify efficacious exercise interventions.
Strengths and limitations
This overview systematically appraised the evidence for the effects of a wide range of physical activity on menopausal symptoms although interventions were predominantly structured forms of exercise rather than general activity. We used a comprehensive search and rigorous systematic review method; our synthesis focused on the highest-quality evidence. Identified reviews included primarily RCTs meaning most evidence originates from studies designed to answer questions of intervention efficacy. A risk with undertaking an overview is that included reviews may not be up to date with the most recent RCTs. An overview review also depends on existing systematic reviews including salient activities and outcomes. These limitations are to some degree mitigated by the relatively recent search dates and wide scope of included reviews, which should capture most interventions and outcomes. Limited impact was observed for our date and language restrictions: no reviews were excluded due to our post-2000 restriction; four reviews were excluded due to language limitations.
Overviews risk multiple counting of primary studies and participants due to overlap. Good reporting in included reviews allowed us to map overlap and determine the number of unique RCTs and participants contributing to each symptom assessment for most comparisons. This means we are confident we have not over-estimated the evidence base.
Overviews necessarily rely on the decisions and judgements of authors of included reviews which are sometimes poorly reported or unreliable. We have mitigated this by focusing on reviews assessed as high quality and by considering, wherever possible, the consistency and precision of their included evidence as well as risk of bias. We have noted where this was unclear. Activities were generally not well or systematically described (there was no use of TIDieR) [52] and many exercise interventions were simply classed as ‘aerobic’; further research should clearly delineate exercise categories to permit greater understanding of the impact of exercise type, intensity, and duration. A narrative review on walking as a potential benefit for menopause symptoms [53] previously highlighted this difficulty in navigating the variations in exercise duration and frequency as a challenge for researchers with respect to agreement on beneficial outcome.
Reporting of factors relating to equity was also limited, making the relevance of evidence to disadvantaged groups unclear. Current reviews categorise women on menopause status; broadening this to include ethnicity, income status, employment type and other PROGRESSPlus [32] factors will allow better understanding of the context in which an intervention is most effective.
Evaluation of HRT as a comparator was lacking; only seen in two reviews [6, 42]. Each review included a single RCT comparing this with exercise; findings were inconsistent with evidence strongly favouring HRT over physical activity for hot flashes [6] but a benefit of physical activity over HRT on menopause-specific quality of life was evidenced [42]. Reporting of complementary use of HRT was also limited. Since many women use exercise as an alternative to or complement of HRT, the comparison between and intersection of the two approaches could usefully be explored. HRT prescribing is unequal; in the UK women from lower socio-economic groups are around 30% less likely to be prescribed HRT than those from more affluent areas [54]. Communities with higher Black and minority ethnic populations are more likely to have lower socio-economic profiles, so multiple equity indicators are likely involved in prescribing [55, 56]. Strengthening evidence for all menopause management options available to women may support equity and accessibility of useful treatments.
Further research
Reviews frequently reported there was no evidence of a difference between exercise groups and controls, or between different types of exercise, but it should be noted that most included RCTs were underpowered. Thus findings of no difference between different types of exercise do not indicate that either exercise would have no effect relative to no intervention; but an assessment of appropriate transitivity would need to be undertaken in order proceed with a network meta-analysis of all available trials to fully utilise the data for this. Direct comparisons indicate that both yoga and aerobic exercise may sometimes be effective relative to no intervention. In many cases included trials were too small and too few to identify effects; optimal information sizes were not calculated but would likely not be met. It is therefore important that reviews, and our synthesis, are not interpreted as evidence of no effect; but rather as evidence that more adequately powered studies are needed.
We have identified several research gaps via this overview. More research on resistance training and high intensity aerobic exercise is needed, as is research on the impact of exercise on physical, sexual, and urogenital symptoms. Beyond this, a comprehensive review and network meta-analysis would enable full use of all the available RCT evidence to identify where new trials are most urgently needed. Any future RCTs should be adequately powered, rigorously designed, and clearly reported. This includes clear description of interventions using TIDieR domains [52] and clear reporting of PROGRESSPlus participant characteristics [32].
Conclusion
There is some evidence that both yoga, and to a lesser extent, aerobic exercise may be beneficial for some menopause symptoms, but there is insufficient evidence to recommend a particular form of exercise for specific symptom management. Exercise benefits for general health are well documented; both aerobic and resistance training are generally recommended [9]. These recommendations, together with the personal preferences of women, are currently likely to be most important in guiding exercise choice and clinical prescription.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
Conceptualisation, AM, CT; methodology, AM, AMK, GN, CT; formal analysis, AM, AMK, GN, CET, DH; data curation, AM, AMK, GN, CET, DH; writing—original draft preparation, AM, AMK, GN; writing— review and editing, AM, AMK, GN, CET, DH, JM, CT; funding acquisition, CT. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the National Institute for Health and Care Research, Applied Research Collaboration-Greater Manchester (NIHR200174), Centre for Ageing Better, and a NIHR Senior Investigator Award to Prof Todd (NIHR200299). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, the Department of Health and Social Care, or its partner organisations.
Data availability
This overview includes only previously published data. Further information on aspects of the overview process not included in the supplementary information (I.e., lists of excluded studies) are available on request from the authors; please email Annemarie Money annemarie.money@manchester.ac.uk.
Declarations
Ethics approval and consent to participate
The paper is a review of reviews, using publicly available data published in systematic reviews, therefore it does not involve human participants and does not require ethical approval.
Consent for publication
The paper is a review of reviews, using publicly available data published in systematic reviews, therefore it does not involve human participants and does not require ethical approval.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Institute for Health and Care Management. Menopause: Diagnosis and Management (NG 23) [Internet]. 2019. Report No.: NG23. https://www.nice.org.uk/guidance/ng23.
- 2.Women’s. Health Strategy for England. August 2022. 2022.
- 3.Department for Health and Social Care. Nation unite to tackle menopause taskforce [Internet]. 2022. https://www.gov.uk/government/news/nations-unite-to-tackle-menopause-taskforce.
- 4.Lewiecki EM, Leader D, Weiss R, Williams SA. Challenges in osteoporosis awareness and management: results from a survey of US postmenopausal women. J Drug Assess. 2019;8(1):25–31. doi: 10.1080/21556660.2019.1579728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newson LR. Best practice for HRT: unpicking the evidence. Br J Gen Pract. 2016;66(653):597–8. doi: 10.3399/bjgp16X687097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daley A, Stokes-Lampard H, Thomas A, MacArthur C. Exercise for vasomotor menopausal symptoms. Cochrane Gynaecology and Fertility Group, editor. Cochrane Database Syst Rev [Internet]. 2014 Nov 28 [cited 2024 Jun 18];2014(11). 10.1002/14651858.CD006108.pub4. [DOI] [PMC free article] [PubMed]
- 7.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep Wash DC 1974. 1985;100(2):126–31. [PMC free article] [PubMed] [Google Scholar]
- 8.Almeida OP, Khan KM, Hankey GJ, Yeap BB, Golledge J, Flicker L. 150 minutes of vigorous physical activity per week predicts survival and successful ageing: a population-based 11-year longitudinal study of 12 201 older Australian men. Br J Sports Med. 2014;48(3):220–5. doi: 10.1136/bjsports-2013-092814. [DOI] [PubMed] [Google Scholar]
- 9.Department for Health and Social Care. UK Chief Medical Officers’ Physical Activity Guidelines [Internet]. 2019 Sep. https://assets.publishing.service.gov.uk/media/5d839543ed915d52428dc134/uk-chief-medical-officers-physical-activity-guidelines.pdf.
- 10.Sport, England. Women in Sport. Silver Linings – Understanding women’s relationship with sport and physical activity in later life [Internet]. 2017. https://womeninsport.org/wp-content/uploads/2017/10/Silver-Linings-report.pdf.
- 11.Sport England. Active Lives data [Internet]. 2021 2022. https://www.sportengland.org/research-and-data/data/active-lives/active-lives-data-tables.
- 12.Mansikkamäki K, Raitanen J, Malila N, Sarkeala T, Männistö S, Fredman J, et al. Physical activity and menopause-related quality of life – a population-based cross-sectional study. Maturitas. 2015;80(1):69–74. doi: 10.1016/j.maturitas.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 13.Mansikkamäki K, Raitanen J, Nygård CH, Tomás E, Rutanen R, Luoto R. Long-term effect of physical activity on health-related quality of life among menopausal women: a 4-year follow-up study to a randomised controlled trial. BMJ Open. 2015;5(9):e008232. doi: 10.1136/bmjopen-2015-008232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen TM, Do TTT, Tran TN, Kim JH. Exercise and Quality of Life in Women with menopausal symptoms: a systematic review and Meta-analysis of Randomized controlled trials. Int J Environ Res Public Health. 2020;17(19):7049. doi: 10.3390/ijerph17197049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Money A, McDermott J, Eost-Telling C, Harris D, Littlewood A, Todd C. The impact of physical activity interventions on improvements to symptoms for women experiencing menopause transition symptoms: review of reviews. Prospero [Internet]. 2022; https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=298908.
- 16.Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L, Chapter V. Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. In: Cochrane Handbook for Systematic Reviews of Interventions [Internet]. www.training.cochrane.org/handbook.
- 17.Pollock M, Fernandes RM, Pieper D, Tricco AC, Gates M, Gates A, et al. Preferred reporting items for overviews of reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):335. doi: 10.1186/s13643-019-1252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, et al. A menopause-specific quality of life questionnaire: development and psychometric properties. Maturitas. 1996;24(3):161–75. doi: 10.1016/S0378-5122(96)82006-8. [DOI] [PubMed] [Google Scholar]
- 19.Lewis JE, Hilditch JR, Wong CJ. Further psychometric property development of the menopause-specific quality of life questionnaire and development of a modified version, MENQOL-Intervention questionnaire. Maturitas. 2005;50(3):209–21. doi: 10.1016/j.maturitas.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 20.Hyland ME, Sodergren SC. Development of a new type of global quality of life scale, and comparison of performance and preference for 12 global scales. Qual Life Res. 1996;5(5):469–80. doi: 10.1007/BF00540019. [DOI] [PubMed] [Google Scholar]
- 21.Hooker SA. SF-36. In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine [Internet]. New York, NY: Springer New York; 2013 [cited 2024 Jun 18]. pp. 1784–6. http://link.springer.com/10.1007/978-1-4419-1005-9_1597.
- 22.World Health Organization, Division of Mental Health. WHOQOL-BREF: introduction, administration, scoring and generic version of the assessment : field trial version. [Internet]. 1996. https://iris.who.int/handle/10665/63529.
- 23.Utian WH, Janata JW, Kingsberg SA, Schluchter M, Hamilton JC. The Utian Quality of Life (UQOL) Scale: development and validation of an instrument to quantify quality of life through and beyond menopause. Menopause. 2002;9(6):402–10. doi: 10.1097/00042192-200211000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Abrams P, Cardozo L, Wein A. 3rd international consultation on incontinence—research society 2011. Neurourol Urodyn. 2012;31(3):291–2. doi: 10.1002/nau.22221. [DOI] [PubMed] [Google Scholar]
- 25.Thirlaway K, Fallowfield L, Cuzick J. The sexual activity questionnaire: a measure of women’s sexual functioning. Qual Life Res. 1996;5(1):81–90. doi: 10.1007/BF00435972. [DOI] [PubMed] [Google Scholar]
- 26.Greene JG. Constructing a standard climacteric scale. Maturitas. 1998;29(1):25–31. doi: 10.1016/S0378-5122(98)00025-5. [DOI] [PubMed] [Google Scholar]
- 27.Hunter M. Womens Health Questionnaire. Qual Life Res. 2000;9(6suppl):733–8. doi: 10.1023/A:1008973822876. [DOI] [Google Scholar]
- 28.Carpenter JS. The Hot Flash Related Daily Interference Scale. J Pain Symptom Manage. 2001;22(6):979–89. doi: 10.1016/S0885-3924(01)00353-0. [DOI] [PubMed] [Google Scholar]
- 29.Centre for Reviews and Dissemination (UK). Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. 1995. https://www.ncbi.nlm.nih.gov/books/NBK285222/.
- 30.Shin H, Shin HS. Measurement of quality of life in Menopausal women: a systematic review. West J Nurs Res. 2012;34(4):475–503. doi: 10.1177/0193945911402848. [DOI] [PubMed] [Google Scholar]
- 31.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol. 2014;67(1):56–64. doi: 10.1016/j.jclinepi.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 33.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;j4008. [DOI] [PMC free article] [PubMed]
- 34.Bracchiglione J, Meza N, Bangdiwala SI, Niño de Guzmán E, Urrútia G, Bonfill X, et al. Graphical representation of overlap for OVErviews: GROOVE tool. Res Synth Methods. 2022;13(3):381–8. doi: 10.1002/jrsm.1557. [DOI] [PubMed] [Google Scholar]
- 35.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;l6890. [DOI] [PMC free article] [PubMed]
- 36.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carcelén-Fraile M, del Aibar-Almazán C, Martínez-Amat A, Cruz-Díaz A, Díaz-Mohedo D, Redecillas-Peiró E. Effects of Physical Exercise on sexual function and quality of sexual life related to menopausal symptoms in Peri- and Postmenopausal women: a systematic review. Int J Environ Res Public Health. 2020;17(8):2680. doi: 10.3390/ijerph17082680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cramer H, Peng W, Lauche R. Yoga for menopausal symptoms—A systematic review and meta-analysis. Maturitas. 2018;109:13–25. doi: 10.1016/j.maturitas.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 39.Innes KE, Selfe TK, Vishnu A. Mind-body therapies for menopausal symptoms: a systematic review. Maturitas. 2010;66(2):135–49. doi: 10.1016/j.maturitas.2010.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kalra S, Yadav J, Ajmera P, Sindhu B, Pal S. Impact of Physical Activity on Physical and Mental Health of Postmenopausal Women: A Systematic Review. J Clin Diagn Res [Internet]. 2022 [cited 2024 Jun 19]; https://www.jcdr.net/article_fulltext.asp?issn=0973-709x&year=2022&month=February&volume=16&issue=2&page=YE01-YE08&id=15974
- 41.Lee MS, Kim JI, Ha JY, Boddy K, Ernst E. Yoga for menopausal symptoms: a systematic review. Menopause. 2009;16(3):602–8. doi: 10.1097/gme.0b013e31818ffe39. [DOI] [PubMed] [Google Scholar]
- 42.Nedrow A, Miller J, Walker M, Nygren P, Huffman LH, Nelson HD. Complementary and alternative therapies for the management of menopause-related symptoms: a systematic evidence review. Arch Intern Med. 2006;166(14):1453. doi: 10.1001/archinte.166.14.1453. [DOI] [PubMed] [Google Scholar]
- 43.Nigdelis MP, Martínez-Domínguez SJ, Goulis DG, Pérez-López FR. Effect of programmed exercise on perceived stress in middle-aged and old women: a meta-analysis of randomized trials. Maturitas. 2018;114:1–8. doi: 10.1016/j.maturitas.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 44.Pérez-López FR, Martínez-Domínguez SJ, Lajusticia H, Chedraui P. Effects of programmed exercise on depressive symptoms in midlife and older women: a meta-analysis of randomized controlled trials. Maturitas. 2017;106:38–47. doi: 10.1016/j.maturitas.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 45.Shepherd-Banigan M, Goldstein KM, Coeytaux RR, McDuffie JR, Goode AP, Kosinski AS, et al. Improving vasomotor symptoms; psychological symptoms; and health-related quality of life in peri- or post-menopausal women through yoga: an umbrella systematic review and meta-analysis. Complement Ther Med. 2017;34:156–64. doi: 10.1016/j.ctim.2017.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shorey S, Ang L, Lau Y. Efficacy of mind–body therapies and exercise-based interventions on menopausal‐related outcomes among Asian perimenopause women: a systematic review, meta‐analysis, and synthesis without a meta‐analysis. J Adv Nurs. 2020;76(5):1098–110. doi: 10.1111/jan.14304. [DOI] [PubMed] [Google Scholar]
- 47.Woods NF, Mitchell ES, Schnall JG, Cray L, Ismail R, Taylor-Swanson L, et al. Effects of mind–body therapies on symptom clusters during the menopausal transition. Climacteric. 2014;17(1):10–22. doi: 10.3109/13697137.2013.828198. [DOI] [PubMed] [Google Scholar]
- 48.Martínez-Domínguez SJ, Lajusticia H, Chedraui P, Pérez-López FR, for the Health outcomes and systematic analyses (HOUSSAY) Project. The effect of programmed exercise over anxiety symptoms in midlife and older women: a meta-analysis of randomized controlled trials. Climacteric. 2018;21(2):123–31. doi: 10.1080/13697137.2017.1415321. [DOI] [PubMed] [Google Scholar]
- 49.Capel-Alcaraz AM, García-López H, Castro-Sánchez AM, Fernández-Sánchez M, Lara-Palomo IC. The efficacy of Strength exercises for reducing the symptoms of menopause: a systematic review. J Clin Med. 2023;12(2):548. doi: 10.3390/jcm12020548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sá KMM, da Silva GR, Martins UK, Colovati MES, Crizol GR, Riera R, et al. Resistance training for postmenopausal women: systematic review and meta-analysis. Menopause. 2023;30(1):108–16. doi: 10.1097/GME.0000000000002079. [DOI] [PubMed] [Google Scholar]
- 51.Liu T, Chen S, Mielke GI, McCarthy AL, Bailey TG. Effects of exercise on vasomotor symptoms in menopausal women: a systematic review and meta-analysis. Climacteric. 2022;25(6):552–61. doi: 10.1080/13697137.2022.2097865. [DOI] [PubMed] [Google Scholar]
- 52.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348(mar07 3):g1687–1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 53.Sydora BC, Turner C, Malley A, Davenport M, Yuksel N, Shandro T, et al. Can walking exercise programs improve health for women in menopause transition and postmenopausal? Findings from a scoping review. Menopause. 2020;27(8):952–63. doi: 10.1097/GME.0000000000001554. [DOI] [PubMed] [Google Scholar]
- 54.Hillman S, Shantikumar S, Ridha A, Todkill D, Dale J. Socioeconomic status and HRT prescribing: a study of practice-level data in England. Br J Gen Pract. 2020;70(700):e772–7. doi: 10.3399/bjgp20X713045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Phillipa Stroud, Legatum Institute Foundation. Measuring Poverty report [Internet]. 2020. https://socialmetricscommission.org.uk/wp-content/uploads/2020/06/Measuring-Poverty-2020-Web.pdf.
- 56.National Institute for Health and Care Management. British National Formulary (BNF) [Internet]. 2020. https://bnf.nice.org.uk/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This overview includes only previously published data. Further information on aspects of the overview process not included in the supplementary information (I.e., lists of excluded studies) are available on request from the authors; please email Annemarie Money annemarie.money@manchester.ac.uk.