Although it is not clear whether Dr Sylvius (above) was describing his teaching method in relation to a group of students or to a succession of individual students, he understood the essential features of clinical education. He understood, for example, the need for active learning in an authentic clinical setting.
Wards, operating theatres, general practice, and community clinics provide a context for active learning
“My method (is) to lead my students by hand to the practice of medicine, taking them every day to see patients in the public hospital, that they may hear the patients' symptoms and see their physical findings. Then I question the students as to what they have noted in the patients and about their thoughts and perceptions regarding the cause of the illness and the principles of treatment”Dr Franciscus de la Boe Sylvius, 17th century professor of medicine at the University of Leyden, Netherlands
Dr Sylvius also understood another important feature of one to one teaching—close behavioural observation (of each other, teacher and learner). No other setting provides the same opportunity for this. Dr Sylvius led his students “by [the] hand.” He cared about his role as a teacher. In the closely observed one to one relationship your unguarded statements, your reactions under pressure, and your opinions about other people and the world at large are all magnified.
As a teacher, you are an important role model whether you wish it or not
What's different about one to one teaching?
| Lecture | Seminar | PBL group | Clinical tutorial | One to one clinical attachment | |
| Efficiency* | High | Medium | Low | Low | Very low |
| Active learning | Low (usually) | Variable | High | Medium to high | Very high |
| Mutual feedback | Low | Medium | High | Medium to high | Very high |
| Modelling behaviour in real life setting | Low | Low | Medium | High | Very high |
PBL=problem based learning.
*Based on student numbers.
Just as you cannot hide from the learner, so the learner's knowledge, skills, and attitudes will become apparent to you. Provided that you have created a trusting relationship, you can discuss his or her personal and professional attitudes and values in a way that is seldom possible in a larger group. This is perhaps one of the key benefits of one to one teaching.
Another feature of one to one teaching is the opportunity to adjust what you teach to the learner's needs—“customise” your teaching. In 1978 Ausubel and colleagues suggested that the secret of education is to find out what the learner already knows and teach accordingly. In a lecture, tutorial, or seminar you cannot hope to diagnose and respond to every individual's learning needs, but a one to one relationship provides an opportunity to match the learning experience to the learner.
One to one teaching is perhaps one of the most powerful ways of “influencing students.” You can create opportunities for active learning in authentic clinical settings while modelling desirable personal and professional attributes.
Stott and Davis in 1979 promoted the idea that one to one primary care consultations offer exceptional but often unrealised potential. The principles used in primary care consultations can be applied to one to one teaching, and the secret is forethought and planning.
Plan ahead—ask yourself some important questions
What is the main purpose of the one to one attachment?
Do you know why it is part of the learning programme?
What are the learner's needs?
How will you gauge how effectively you have met the learner's needs?
How would you like this learner to describe the experience to a peer?
Exceptional potential of one to one teaching
It tackles current learning needs
It promotes autonomy and self directed learning
It links prior knowledge with new clinical experiences
It enables opportunistic teaching
Provide an orientation
Most of us recall clinical teachers whose social skills amounted to a brief glance and a grunt. Times have changed, or should have. Find out and remember the learner's name—a simple but important courtesy. Outline the special opportunities and benefits that the attachment can provide. Ask the learner to prepare a learning plan and then compare the learner's plan to your own expectations. Once the plan has been agreed, don't shelve it—refer to it during the attachment and modify as necessary.
Agree on the ground rules
Ground rules are both practical (punctuality, dress, access to patient records) and philosophical (respect for patients and colleagues, confidentiality, consent, openness to different points of view). If these have been spelled out on day 1, you won't be caught out later. Make sure that the learner knows how much time you will be able to spend in observing, teaching, and giving feedback and what you expect in return.
Ask helpful questions
Open ended questions are generally better than closed questions at the beginning of the exchange. A small number of closed questions later in the conversation help you to “diagnose” just how much the learner knows and understands. Avoid questions that require nothing but recall. Try to formulate questions that assume an appropriate amount of knowledge, but build in higher order thinking and/or higher order skills. You might ask the learner, for example, to explain to you (as if you were the patient) the mechanisms behind a condition such as asthma or hypertension. This simulates clinical interface with a patient—testing recall, understanding, and communications skills all at once.
Skilful teaching is not unlike skilful history taking
“If musicians learned to play their instruments as physicians learn to interview patients, the procedure would consist of presenting in lectures or maybe in a demonstration or two the theory and mechanisms of the music-producing ability of the instrument and telling him to produce a melody. The instructor of course, would not be present to observe or listen to the student's efforts, but would be satisfied with the student's subsequent verbal report of what came out of the instrument.”George Engel, after visiting 70 medical schools in North America
Give feedback
Learners value feedback highly, and valid feedback is based on observation. Deal with observable behaviours and be practical, timely, and concrete. The one to one relationship enables you to give feedback with sensitivity and in private. Begin by asking the learner to tell you what he or she feels confident of having done well and what he or she would like to improve. Follow up with your own observations of what was done well (be specific), and then outline one or two points that could help the student to improve.
Encourage reflection
Just as many learning opportunities are wasted if they are not accompanied by feedback from an observer, so too are they wasted if the learner cannot reflect honestly on his or her performance. One to one teaching is ideally suited to encouraging reflective practice, because you can model the way a reflective practitioner behaves. Two key skills are (a) “unpacking” your clinical reasoning and decision making processes and (b) describing and discussing the ethical values and beliefs that guide you in patient care.
Monitor progress
Identify deficiencies
Ask the learner, half way through the attachment, to do a self assessment of how things are going. If both you and the learner can identify deficiencies within a safe learning environment, you can work together to tackle them well before the attachment ends
If you have serious concerns, you have an obligation to make them known to the learner and to the medical school or training authority
It is not appropriate to diagnose serious problems and hand the learner on to the next stage of training in the hope that the problems will somehow be correct themselves
Use other one to one teachers
Senior medical students, junior doctors, registrars, nurses, and allied health professionals are all potential teachers. When junior colleagues interact with a learner, you can encourage them with positive feedback on their teaching.
Every patient interview and every physical examination places the learner in a privileged relationship with a patient. We all have patients whom we especially admire—particularly people who have coped bravely with a chronic illness or a major disability, a disaster such as war, or other misfortunes. Such patients activate an emotional response in the learner, imprinting a enriched memory of the patient and the patient's illness.
Promote active learning
Time is limited in most clinical setting, and it can be tempting to revert to a passive observational teaching model
Think about strategies to promote active learning
Brief students to observe specific features of a consultation or procedure
Ask patients for permission for the learner to carry out all or part of the physical examination or a procedure while you observe
If space is available, allow students to interview patients in a separate room or cubicle before presenting them to you
If possible videotape consultations for a debriefing session at a more convenient time
Arrange for the learner to see the same patient over time, or in another context, such as a home visit
Points to remember
Do
Welcome
Set shared achievable goals
Put yourself in the learner's shoes
Ask interesting questions
Monitor progress and give feedback
Encourage
Don't
Appear unprepared
Be vague about your expectations
Confine the learner to passive roles
Be “nit-picking”
Leave feedback to the final assessment
Humiliate
Reap the rewards
The role of the teacher is frequently undervalued, and yet teaching is potentially rewarding and enjoyable. It is also one of the defining features of a profession. Without teaching to ensure the transmission of knowledge, medicine becomes just another “job.”
Further reading
Parsell G, Bligh J. Recent perspectives on clinical teaching. Med Educ 2001;35:409-14
Paulman PM, Susman JL, Abboud CA, eds. Precepting medical students in the office. London: Johns Hopkins University Press, 2000.
Westberg J, Jason H. Collaborative clinical education: the foundation of effective health care. New York: Springer, 1993.
Whitehouse C, Roland M, Campion P, eds. Teaching medicine in the community: a guide for undergraduate education. New York: Oxford University Press, 1997.
Stott N, Davis R. The exceptional potential in each primary care consultation. J R Coll Gen Pract 1979;29:201-5
Ausubel D, Novak J, Hanesian H. Educational psychology: a cognitive view. New York: Rinehart and Winston, 1978.
One to one teaching inevitably exposes you to evaluation by the learner. If the learner trusts you, he or she will be able to tell you what has worked well, and what could be improved. Respond to feedback by reflecting rather than by explaining, excusing, or offering counter arguments to defend your particular style. Openness to feedback is another professional attribute that is best modelled one to one.
Learners for whom you have been a role model and mentor are likely to repay you many times over. Sometimes you have the opportunity to observe their personal and professional development long after the one to one attachment has finished. Dr Sylvius knew how to do it, and Cicero understood its rejuvenating qualities.
Figure.
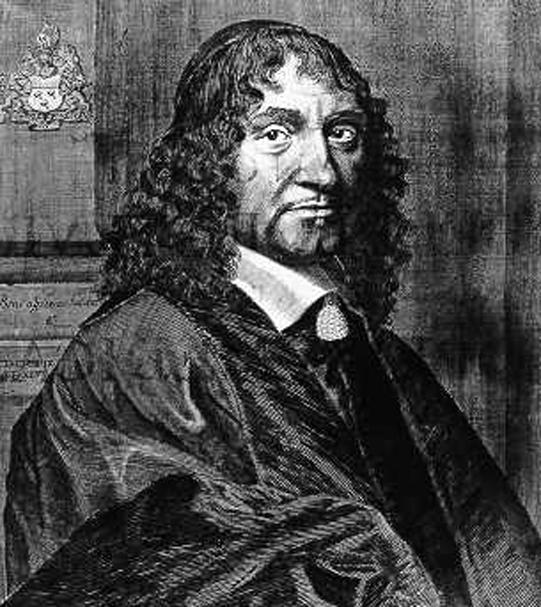
Dr Franciscus de la Boe Sylvius
Figure.
Find out and remember the learner's name—a simple but important courtesy
Figure.
“Cultivate the society of the young, remain interested and never stop learning” (Cicero)
Acknowledgments
The illustration on p 544 is reproduced with permission from Jake Wyman/Photonica.
The illustration of the young Cicero reading (by Vicenzo Foppa) is reproduced with permission from the Bridgeman Art Library.
Footnotes
The ABC of learning and teaching in medicine is edited by Peter Cantillon, senior lecturer in medical informatics and medical education, National University of Ireland, Galway, Republic of Ireland; Linda Hutchinson, director of education and workforce development and consultant paediatrician, University Hospital Lewisham; and Diana F Wood, deputy dean for education and consultant endocrinologist, Barts and the London, Queen Mary's School of Medicine and Dentistry, Queen Mary, University of London. The series will be published as a book in late spring.
Jill Gordon is associate professor in the department of medical education at the University of Sydney, Australia.




