Abstract
INTRODUCTION
The intersection of ageing and spinal cord injury (SCI) is of global concern. Two scenarios have been described: 1) “SCI with ageing,” an increase in the average age of SCI onset, and 2) “ageing with SCI,” an increase in post-injury life expectancy. These scenarios entail complex health care and rehabilitation needs due to the accumulation of comorbidities, ageing-related and SCI-induced physiological changes, and post-SCI secondary health conditions. We systematically reviewed Clinical Practice Guidelines (CPGs) with the objective of identifying the extent to which SCI CPGs include recommendations for the rehabilitation and management of people who are “ageing with SCI” or who have acquired an “SCI with ageing”. We termed these as “ageing-related recommendations”. We also aimed to describe them and identify gaps.
EVIDENCE ACQUISITION
We searched PubMed (NCBI), CINAHL Complete (EBSCOhost) and Embase (Elsevier) for relevant CPGs between 28 December 2022 and 5 January 2023. Included CPGs were evidence-based and had at least one ageing-related recommendation for SCI rehabilitation and management. We used the two core sets of the International Classification of Functioning, Disability and Health (ICF) to identify gaps.
EVIDENCE SYNTHESIS
Only 16 (30%) of the 52 identified CPGs included ageing-related recommendations. Most were recent US or European publications and lacked specific chapters on ageing. These CPGs included 40 ageing-related recommendations, mostly “strong” but based on “low” to “very low” quality of evidence. The overall quality of the development process was low and did not consider the values and preferences of stakeholders and patients. Common topics included cardiovascular, bone, metabolic, bowel, bladder, and skin health. The recommendations could be linked to 30 ICF categories which represented only 18% of the ICF categories included in the comprehensive versions of two ICF Core Sets. Key gaps were found in mobility, interpersonal interactions, and relationships, neuromusculoskeletal and movement-related, mental, sensory and pain functions.
CONCLUSIONS
There is a notable lack of high-quality ageing-related recommendations for SCI management and rehabilitation. Future research should prioritize the generation of high-quality evidence to develop age-sensitive CPGs. Future SCI CPGs need to address the complex challenges at the interface of ageing and SCI, considering patient and stakeholder preferences.
Key words: Spinal cord injuries, Aging, Practice guideline
European Journal of Physical and Rehabilitation Medicine 2024 June;60(3):433-44
DOI: 10.23736/S1973-9087.24.08244-3
© 2024 THE AUTHORS
SYSTEMATIC REVIEW
(Cite this article as: Seijas V, Schrepfer L, Posada AM, Spir MA, Machado B, Sigrist-Nix D, et al. Evidence-based recommendations for the rehabilitation and management of the ageing population with spinal cord injury: a systematic review of clinical practice guidelines. Eur J Phys Rehabil Med 2024;60:433-44. DOI: 10.23736/S1973-9087.24.08244-3)
Introduction
Global attention is increasingly focused on the intersection of ageing and disability.1 Verbrugge and Yang described two distinct paradigms: 1) “ageing with disability,” which refers to individuals with pre-existing health conditions who benefit from increased life expectancy due to advances in social and health services; and 2) “disability with ageing,” which describes those who experience disability primarily as a result of age-related conditions.2 In spinal cord injury (SCI), the spinal cord’s anatomical structures and physiological functions are damaged by various causes, such as trauma, inflammation, or tumors. As a result, motor, sensory and autonomic functions are impaired below the level of injury.3 Whether due to traumatic or non-traumatic causes, SCI is generally irreversible and a chronic health condition with rather low global incidence and prevalence but a very high disability burden.4, 5 As with other chronic disabling conditions, the intersection of ageing and SCI is of global concern.6-10
Similarly to the general “ageing and disability” paradigm, two scenarios have been described about the association between ageing and SCI: 1) “SCI with ageing” namely an increase in the average age of SCI onset; and 2) “ageing with SCI” namely an increase in life expectancy after the injury.11 A rising proportion of older people in societies correlates with increased incidence and prevalence of both traumatic and non-traumatic SCI, predominantly attributable to falls and neoplasms9, 11, 12 while advancements in acute management, effective rehabilitation strategies, and responsive long-term care have increased life expectancy for individuals with SCI.9, 11, 13, 14 Consequently, a growing proportion of the SCI population now exceeds the age of 65.9 Both scenarios are associated with complex health care and rehabilitation needs arising from the accumulation of comorbidities, ageing-related and SCI-induced physiological changes, and the emergence of post-SCI secondary health conditions.9, 11, 15, 16 Frequent comorbidities include cardiovascular disease, obesity, diabetes, and cancer.9, 11, 16, 17 Ageing-related post-SCI secondary health conditions commonly include osteoporosis, chronic pain, neurogenic bowel and bladder dysfunction, urinary tract infections, pressure injuries, depression, and upper extremity musculoskeletal wear and tear.9, 11, 16, 17 This accumulation of health conditions negatively affects the overall functioning of SCI patients, affecting not only the individual’s well-being but also that of their families and caregivers.9, 11, 15, 16 Individuals who sustain SCI over the age of 65 demonstrate increased dependency on caregivers and experience the highest annual mortality rates within the SCI population.6 Older age at SCI is also associated with increased daily nursing care and reduced independence at discharge.18
The access of persons with SCI to evidence-based acute care, rehabilitation and long-term care is therefore essential. As is usual in evidence-based medicine (EBM), decisions about which interventions to provide to the person with SCI should be based on the available scientific evidence, patients’ preferences and clinical expertise, ideally using Clinical Practice Guidelines (CPGs).19 CPGs guide clinicians in their decision-making process and include “recommendations intended to optimize patient care that are informed by systematic reviews of evidence and an assessment of the benefits and harms of alternative care options”20. The implementation of CPGs by healthcare professionals is essential to ensure that quality and state-of-the-art treatment is consistently provided. By improving the delivery of more efficient care, the use of GPCs ultimately leads to better health outcomes for individuals and to a reduction in avoidable costs to the healthcare system.20 In the context of ageing with SCI, CPGs for rehabilitation and long-term follow-up and management are particularly important.
CPGs should address key issues faced by persons with SCI. The International Classification of Functioning, Disability and Health (ICF)21 coined the concept of “functioning,” encompassing all body functions and structures.22 The ICF has been widely used to comprehensively describe the lived experience of health.22 The ICF Core Sets have been developed to comprehensively and consistently capture the most relevant aspects of functioning in specific health conditions.23 For SCI, two comprehensive Core Sets exist, one for post-acute care24 and one for long-term care.25 The extent to which existing SCI CPGs cover the aspects listed in these core sets, especially the long-term care one, may reflect their suitability to guide clinicians and health professionals.
Given the complexity of the association between ageing and SCI, it is essential that CPGs address the needs of this population. However, to the best of our knowledge, no CPGs have been developed specifically to address the rehabilitation and long-term management needs of people who are “ageing with SCI” or who have acquired an “SCI with ageing.” Although several CPGs address a variety of health issues relevant to people with SCI and focus on rehabilitation and management, the extent to which these CPGs include specific recommendations for people who are “ageing with SCI” or who have acquired an “SCI with ageing”, hereafter referred to as “ageing-related recommendations,” is unknown. We, therefore, conducted a systematic review of CPGs with the following objectives: 1) to assess the extent to which evidence-based guidelines for the rehabilitation and management of adults with SCI include age-related recommendations, 2) to provide a detailed description of age-related recommendations, including their methodological quality, and c) to identify areas of functioning covered by current ageing-related recommendations and gaps. This review aims to guide future research and CPGs development in the field of ageing and SCI.
Evidence acquisition
Study design
We conducted a systematic review of CPGs following the state-of-the-art methods,26 and used the Preferred Reporting Items for Systematic Reviews (PRISMA 2020).27 We registered the protocol of the systematic review with the International Prospective Register of Systematic Reviews (PROSPERO) on 15th January 2023 (registration ID: CRD42023387878).
Eligibility criteria
We defined eligibility criteria using the population, intervention, attributes of eligible CPGs and recommendation characteristics from the PICAR framework, developed to guide systematic reviews of CPGs.26 We included CPGs that were based on evidence and had at least one ageing-related recommendation for the rehabilitation and management of people with traumatic or non-traumatic SCI. Recommendations were considered ageing-related if they referred to people who had SCI at a young age and who had lived with the injury for a long time, or “ageing with SCI,” or to people who had SCI at an older age, or “SCI with ageing.” We have deliberately refrained from specifying chronological age cut-offs for both populations, as previous studies have shown that the health status associated with a given age can vary considerably depending on the country of residence,28 and others have shown that defining ageing cut-offs for SCI is even more difficult than for the general population due to the interference of SCI with the “normal” ageing process.10 We restricted inclusion to the latest versions of CPGs published in English and German from 2012 to 2022. A flow diagram was developed to guide the team members in the application of the eligibility criteria (Supplementary Digital Material 1: Supplementary Table I).
Information sources and search strategy
We searched PubMed (NCBI), CINAHL Complete (EBSCOhost) and Embase (Elsevier) for relevant CPGs between 28th December 2022 and 5th January 2023. We used database-specific controlled vocabulary for the terms “spinal cord injury” and “clinical practice guideline” and filtered for results in English and German published between 2012 and 2022. An example search strategy is provided in Supplementary Digital Material 2 (Supplementary Table II). We also searched five guideline repositories: Guidelines International Network (GIN), National Institute for Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN), Alliance for the Implementation of CPGs (AiCPG), and the Association of the Scientific Medical Societies in Germany (AWMF). In addition, we searched three SCI-specific websites: American Spinal Injury Association (ASIA), Spinal Cord Injury Research Evidence (SCIRE), and Paralyzed Veterans of America (PVA). Furthermore, we conducted an unstructured search in Google Scholar using the terms “spinal cord injury” and “guideline.” We screened the results of the first 10 pages. Finally, we conducted a snowball search by screening the reference lists of eligible CPGs as well as articles that were not CPGs but included CPGs (e.g. a systematic review of CPGs).
CPGs selection process
Three reviewers (L.S., B.M., and V.S.) used a three-stage screening process, which is summarized in a flow chart in Supplementary Table I. First, L.S. and V.S. independently screened titles and abstracts. Second, full texts were assessed for eligibility. Decisions were compared and disagreements were resolved by discussion. Finally, in a third step, L.S. and B.M. reviewed guidelines for the inclusion of at least one ageing-related recommendation. Decisions were compared and disagreements were resolved by discussion with a V.S. For German CPGs, the three-step screening process was only applied by the L.S. In case of doubt, the respective parts were translated with the help of DeepL Translator29 and discussed with V.S., who is not proficient in German. The web application Rayyan (https://www.rayyan.ai/) was used throughout the process.
Data collection process
Three authors (L.S., B.M., and V.S.) participated in the data extraction process. Prior to pilot testing the data extraction, the following information was retrieved using a standardized data extraction form in MS Excel: title, year of publication, author(s), country of guideline development, whether or not a peer review process was undertaken, guideline objectives, whether the guideline was comprehensive or focused on a single topic (e.g. pressure injuries), target user and population, continuum of care, care setting, and whether or not the guideline included a chapter specific to older people. The following aspects of the included recommendations: word(s) “cueing” to “older people” as a target population, the strength of recommendation, quality of recommendation, intended target user, chapter and page, and health problems addressed.
Study risk of bias assessment
Two co-authors (A.M.P. and M.A.S.) used the Recommendation Excellence (AGREE-REX)30 tool to assess the quality of recommendations. The AGREE-REX tool includes nine items: 1) evidence; applicability to 2) target users and 3) patients/populations; values and preferences of 4) target users, 5) patients/populations, 6) policy/decision-makers and 7) guideline developers; 8) purpose; 9) application and adoption, categorized into three domains: clinical applicability, values and preferences, and implementability. We rated the overall quality of each item. The broader assessment – both the suitability of specific recommendations and the overall quality of the included CPGs – was beyond our research scope and therefore not pursued.
Synthesis methods
The synthesis included descriptive quantitative analysis (e.g., frequencies) of guideline and recommendation characteristics, and qualitative analysis to identify commonalities and group recommendations by health issues of interest. Two SCI-specific comprehensive ICF Core Sets, post-acute24 and long-term25 were used as reference frameworks to identify areas of functioning covered by current ageing-related recommendations and to signal gaps in recommendations. The ICF Core Sets included altogether 142 ICF categories. Using standardized ICF linking rules,31 two co-authors (L.S. and V.S.) linked the health issues addressed by ageing-related recommendations to the ICF categories of the ICF Core Sets. If areas covered by the recommendations could not be linked to the ICF categories, they were linked to the corresponding ICF category of the full ICF.21 We used the GRADE system32 to homogenize the reporting of CPGs grading systems for the strength of recommendations and quality of evidence.
We did not assess reporting bias or certainty of assessment in the body of evidence for an outcome, as this was outside the scope of our review.
Data availability
All data generated or analyzed during this study are included in this published article.
Evidence synthesis
CPGs selection
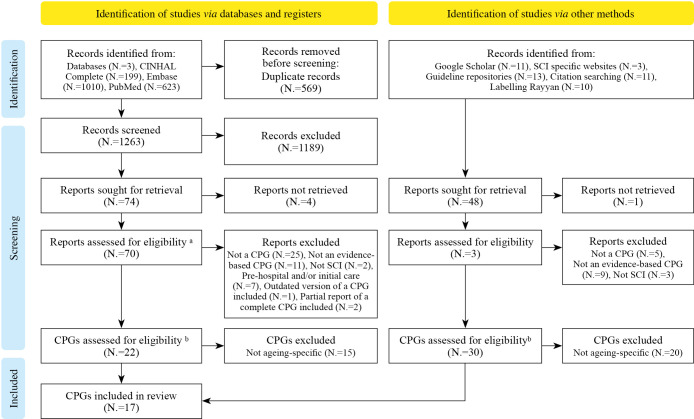
Of 1263 database hits and 48 documents from the grey literature search, 122 were selected for full-text review. Of these, five were not accessible and requests to the authors remained unanswered. Of the remaining 117 CPGs, 65 were excluded. Finally, 52 eligible CPGs were screened for ageing-related recommendations, resulting in the inclusion of 16 CPGs (31% of eligible CPGs) (Figure 1). The list of the 52 identified CPGs is available in Supplementary Digital Material 3 (Supplementary Table III).
Figure 1.
—Adjusted PRISMA flow chart. a In this step, the eligibility of the first 4 steps from the flow diagram (broadly speaking the methodology) was assessed; b In this step, the eligible CPGs were assessed on whether they include at least one ageing specific recommendation or not (step 5).
Characteristics of included CPGs
Of the 16 included CPGs (Supplementary Digital Material 4: Supplementary Table IV), 12 (75%) were published in the last 5 years. Most of the included CPGs were developed in the USA by the Paralyzed Veterans of America (N.=6, 37%) or in Europe (N.=5, 31%). Of the 16 CPGs, 12 (75%) were topic-specific: three focused on urinary functions,33-35 two on bowel management,36, 37 two on pressure injury prevention and management,38, 39 and one each on bone health,40 autonomic dysreflexia,41 weight management,42 cardiometabolic risk,43 and venous thromboembolism.44 The two CPGs with the most ageing-related recommendations were generic and recently published in 2022: “Rehabilitation after traumatic injury” published by the National Institute for Health and Care Excellence (NICE)45 and “Lifelong follow-up care for people with SCI”46 published by the German Speaking Society of Paraplegia, each one with 8 ageing-related recommendations. None of the CPGs had a specific chapter on ageing (Supplementary Table IV).
Recommendation characteristics
Supplementary Digital Material 5 (Supplementary Table V) shows the main characteristics of included recommendations. The result of the standardization of the grading systems of the CPGs is available in Supplementary Digital Material 6 (Supplementary Table VI). The 16 included CPGs provided a total of 40 recommendations, the majority of which were “strong in favor” (N.=29, 72.5%), with ‘low’ to ‘very low’ quality of evidence (N.=35, 87.5%). The target population indicator was very heterogeneous, but ‘older persons/people/adults’ was the most common, followed by age ranges. Most recommendations were very specific, addressing one health issue and making one suggestion at a time (e.g. recommendations 1, 2 and 7), while others were more complex, addressing many health issues and suggesting several interventions at a time (e.g. recommendations 9, 34 and 39). Seven recommendations referred to other CPGs for additional information (recommendations 2, 3, 6, 7, 15 and 29). Three recommendations (17, 31 and 32) adapted recommendations originally developed for the general population. Finally, some recommendations were highly unspecific (e.g., recommendations 12, 14, 24) or only raised awareness of a health problem but did not provide any suggestion for treatment or rehabilitation (e.g., recommendation 4).
Quality of the recommendations
The result of the quality assessment using the AGRE-REX tools is available in Supplementary Digital Material 7 (Supplementary Table VII). The overall quality of the recommendations was low. The lowest average scores were assigned to item 6 (mean 1.6), which assesses whether the values and preferences of policy and decision makers were considered in the development of the recommendations, and item 4 (mean 1.9), which assesses whether the values and preferences of target users were considered. The search strategies used to find evidence to support the recommendations in most guidelines were general searches, not specific to the recommendations, which made it difficult to apply AGRE REX because the outcomes of each recommendation were not pre-defined. Most of the included guidelines did not have a chapter dedicated to the implementation of the guidelines. Most recommendations did not use GRADE32 criteria and terminology such as consistency, precision and indirectness to report their results.
Content of the recommendations
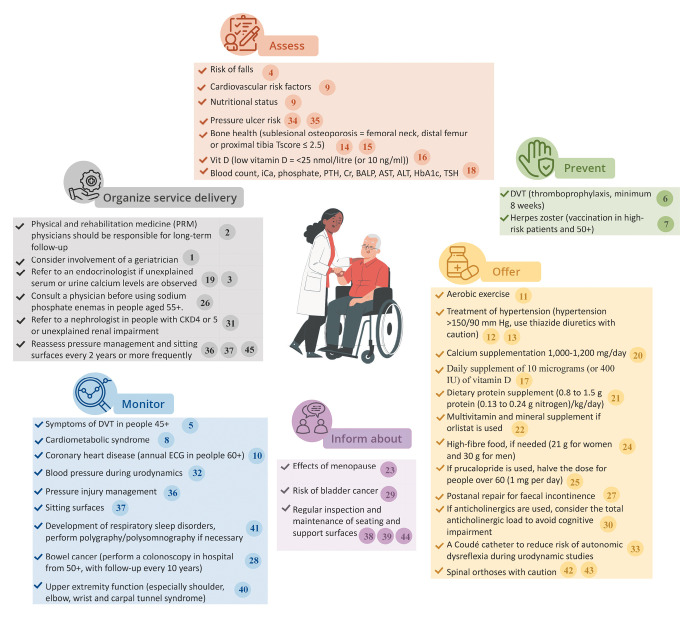
To facilitate the reader’s understanding of the grouping of recommendations by health problem of interest and the linking to ICF codes, the recommendations have been further summarized and ‘complex’ recommendations have been split so that they can address a single health problem and/or suggest a single intervention at a time. Supplementary Digital Material 8 (Supplementary Table VIII) shows the summarized and simplified recommendations organized by health topic and linked to relevant ICF codes. The most frequently addressed topics were cardiovascular, bone, metabolic, bowel, bladder, and skin health. In Figure 2, we provide a summary of available ageing-related recommendations by key areas of practice, including assessment, prevention, treatment, education, monitoring, and service organization. Diagnostic criteria, indication for treatment, warnings about side effects and regularity of interventions were the most common adaptations of ageing-related recommendations.
Figure 2.
—Summary of ageing-related recommendations.47 The numbers make references to key actions listed on Supplementary Table III. iCa: Ionized Calcium; PTH: Parathyroid hormone; Cr: Creatinine; BALP: Bone-specific alkaline phosphatase; AST: Serum aspartate transaminase; ALT: Serum alanine transaminase; HbAlc: Hemoglobin Alc; TSH: thyroid stimulating hormone.
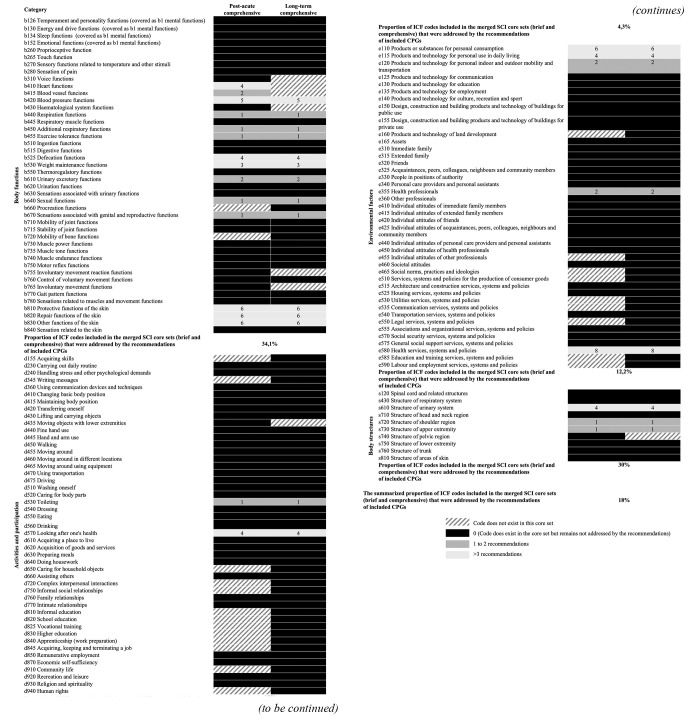
Areas of functioning addressed and not addressed by ageing-related recommendations
The content of all but one of the recommendations (Recommendation No. 3 on assessing fall risk) could be linked to ICF categories. The 39 linked recommendations related to 30 ICF categories, of which 17 related to body functions, two to activities and participation, five to environmental factors and six to body structures. The 87% (26) of the ICF categories identified are part of the two ICF Core Sets for SCI post-acute24 and long-term.25 However, they represent only 18% of all ICF Core Set categories.
The ICF domain with the highest proportion of unaddressed areas was “Activities and participation,” with less than 5% of categories covered by at least one recommendation. Although there were recommendations on wheelchairs and seating surfaces, the recommendations addressed the regular assessment or pressure injury prevention, but there were no specific recommendations on, for example, the characteristics that these technologies need to meet to serve the ageing population well, or how the training process needs to be carried out. Therefore, no recommendations were linked to the common ICF categories related to mobility (d455 Moving around, d460 Moving around in different locations, d465 Moving around using equipment). Similarly, no recommendation was linked to d7 interpersonal interactions and relationships. Only 34% of body functions categories were addressed, and none of the categories related to b1 mental functions, b2 sensory functions and pain, or b7 neuromusculoskeletal and movement-related functions were addressed. For the mapping of the ICF categories (Figure 3).
Figure 3.
—Mapping of the ICF categories.
Discussion
We conducted a systematic review of CPGs to identify to what extent these included recommendations for the rehabilitation and management of people who are “ageing with SCI” or who have acquired an “SCI with ageing,” which we termed “ageing-related recommendations.” Out of the 52 identified CPGs, only 16 (30%) included at least one ageing-related recommendation. Most of the 16 included guidelines were published within the last 5 years in the USA or Europe and none had a chapter devoted exclusively to ageing. These 16 CPGs included 40 ageing-related recommendations, most of which were ‘strong’ but based on ‘low’ to ‘very low’ quality of evidence. The overall quality of the recommendations’ formulation process was low. The most common topics addressed were cardiovascular, bone, metabolic, bowel, bladder, and skin health. The recommendations could be linked to 30 ICF categories, the majority of which were body functions and represented only 18% of the ICF categories included in the comprehensive versions of two ICF Core Sets for SCI (post-acute24 and long-term).25 Significant gaps were found in areas related to activities and participation, such as mobility and interpersonal interactions and relationships, and other body functions, such as neuromusculoskeletal and movement-related, mental, sensory and pain functions.
Despite high-income countries (HICs) facing greater needs around ageing, most of their SCI rehabilitation and management CPGs lack ageing-related recommendations
HICs are urgently confronted with rapidly ageing societies and therefore in a greater need of ageing-specific evidence and recommendations to guide clinical practice.5 Indeed, population ageing is associated with an increase in the number of SCI cases, resulting for instance from falls.48 Consistently, all CPGs containing ageing-related recommendations were developed in HICs, as classified by World Bank49 and in countries where the most research on SCI is produced.50 Nevertheless, only 30% of the identified CPGs in this review included ageing-related recommendations. Research on ageing with SCI has highlighted cardiovascular disease, obesity, diabetes, osteoporosis, pressure injury, bowel management, urinary incontinence and infection, musculoskeletal system and chronic pain as the predominant issues requiring action.9, 11, 16, 17 None of these were found to be comprehensively addressed in the included guidelines. In addition, we found no recommendations for diabetes, urinary tract infections or chronic pain, and ageing-related recommendations covered less than one-fifth of the ICF categories included in two ICF Core Sets for SCI (post-acute24 and long-term).25 Although we have summarized key recommendations for the ageing population with SCI in Figure 2, guidance is lacking to fully address the needs of those who are “ageing with SCI” or who have acquired an “SCI with ageing”.
The lack of robust research on ageing and SCI may explain the paucity of recommendations
A global bibliometric analysis examining the volume of research produced for the field of SCI shows a steady increase over the years, with 995 articles published in 1999 and 3159 in 2018.50 Searching the PubMed database for the combination of the terms “ageing OR aging” and “spinal cord injury” shows that the evidence about ageing in SCI is also steadily increasing, with a somewhat steeper increase in the years 2012, 2014, 2019, but especially from 2021 onwards. However, even though most of the included guidelines were recently published (between 2018 and 2022), 87% of the ageing-related recommendations identified were of low or very low quality. One reason for the poor quality could be the presence of the first form of indirectness “when the interventions described in the recommendations are derived from other target populations,”51 such as the general elderly population or the young population with SCI, leading to a downgrading of their quality52 or, in some cases, hindering the development of a recommendation altogether. For example, recommendations for colorectal cancer screening,46 hypertension treatment,43 and vaccination46 were mostly based on recommendations for the general population and were rated as very low quality. On the other hand, the Paralyzed Veterans of America guideline on bone health and osteoporosis presented evidence of the effectiveness of osteoporosis treatments for postmenopausal women and the elderly population without SCI but was unable to derive a recommendation for the population with SCI. In addition, research may be needed to characterize the different groups that result from the intersection of ageing and SCI in order to better guide clinical practice. For example, accelerated ageing has been described in people with SCI,13 but when do age-related needs begin in this population? Ten, 20, 30 years after injury? Is the time since injury the best indicator of this process, or how can the onset of this process be identified, or even better, slowed down? On the other hand, those injured at an older age may have different characteristics and needs. Older people have different physiological reserves and different responses to trauma due to premorbid frailty, comorbidities, and prescribed medications.53 Furthermore, the exact age at which a trauma patient should be considered an older adult and the differences between the needs and outcomes of frail older trauma patients and healthy older trauma patients remain controversial.54, 55
Several guidelines have highlighted the lack of evidence in ageing and SCI and made ‘research recommendations’
Other reasons for the lack of evidence on SCI and ageing include the relatively low incidence and prevalence of SCI, resulting in small sample sizes, and the heterogeneity within this population, which makes it difficult for researchers to study complex interventions.56 The comorbidities associated with ageing further increase the heterogeneity of the SCI population, and it is well-known that older people are often excluded from RCTs, leading to a lack of high-quality evidence.56 When study samples are small, more evidence on the topic is needed to support CPG recommendations.56 Research recommendations have been included in CPGs, for example on the use of spinal orthoses45 and the management of osteoporosis in postmenopausal women with SCI.40 However, on a positive note, the strength of recommendations was rated as strong in 50% of them, which may indicate that even when the quality of evidence is low, expert confidence in the recommendations is high.
Still, the development of high-quality and ageing-sensitive CPGs and recommendations that include the views of stakeholders and people with SCI is urgently needed
The health issues faced by the ageing population with SCI have been sufficiently highlighted in research,9, 11, 16, 17 but there appears to be a lack of specific research on how to treat, manage and rehabilitate the problems of the ageing population. Evidence coming from the younger population with SCI cannot be simply extrapolated to the ageing population. For example, there is strong evidence favoring the use of spinal orthoses in the young population, however, according to the guideline developing group’s experts, these orthoses are poorly tolerated by the ageing and adverse effects are frequent.45 Other examples relate to the comorbidities faced by the ageing population which change the treatments of choice due to an increased prevalence of polypharmacy and side effects, such as in the case of the use of thiazide diuretics,43 Orlistat,42 prucalopride,36 sodium phosphate enemas36 and anticholinergics.33 Unfortunately, we did not find any age-specific CPGs or CPGs with specific chapters on ageing, and the overall quality of the development of the identified recommendations was low. Consideration of stakeholders’ and patients’ values and preferences in the development of recommendations was particularly poor, although this is considered to be a key element in the successful implementation of CPGs.57
Limitations of the study
Our systematic review has several limitations. First, the criteria for categorizing a recommendation as ‘ageing-related’ were somewhat arbitrary. For example, recommendations targeting “chronic SCI,” defined as ≥2 years post-injury,40 were excluded. However, the word chronic could have been used by some authors to describe people with a long duration of injury or ageing with SCI, and this might have resulted in a loss of information. In addition, some recommendations were included if they justified ageing in their rationale, but this aspect was not systematically checked in all rationales. Secondly, there is disagreement in the literature about the definition of CPGs and different approaches to their development.32, 58 We used a two-criteria approach to identify guidelines: 1) the recommendations were based on a systematic search for evidence and 2) the methods used to formulate the recommendations were described. We may have included or excluded a few guidelines that would or would not be considered evidence-based guidelines by other researchers. Finally, we focused only on assessing the quality of individual recommendations within CPGs, rather than the overall quality of the CPGs themselves. This methodology may introduce bias by treating high- and low-quality guidelines as equivalent. Similarly, we did not use the results of our quality assessment to determine the eligibility of recommendations.59
Conclusions
In conclusion, despite the increasing share of persons who are “ageing with SCI” or who have acquired an “SCI with ageing,” particularly in HICs, there is a noticeable lack of high-quality ageing-related recommendations for SCI management and rehabilitation. While the literature has underscored the health challenges arising from the intersection of ageing and SCI, there appears to be a lack of specific research on how to manage and rehabilitate the problems of this population, and none of their priority issues have been comprehensively addressed in any of the included CPGs. Future research should focus on generating high-quality evidence to support the development of high-quality and ageing-sensitive CPGs. Future CPGs in SCI should address the unique and complex issues arising from the intersection of ageing and SCI, considering the values and preferences of patients and stakeholders in the development process.
Supplementary Digital Material 1
Supplementary Table I
Eligibility criteria
Supplementary Digital Material 2
Supplementary Table II
Exemplary search strategy for PubMed.
Supplementary Digital Material 3
Supplementary Table III
List of all identified Clinical Practice Guidelines.
Supplementary Digital Material 4
Supplementary Table IV
Characteristics of included clinical practice guidelines.
Supplementary Digital Material 5
Supplementary Table V
Ageing-related recommendations.
Supplementary Digital Material 6
Supplementary Table VI
Standardization of the Clinical Practice Guidelines grading system.
Supplementary Digital Material 7
Supplementary Table VII
Standardization of the Clinical Practice Guidelines grading system.
Supplementary Digital Material 8
Supplementary Table VIII
Summary from recommendations organized by areas of interest and linked with relevant ICF codes.
Footnotes
Conflicts of interest: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript. Inge Eriks-Hoogland was also an author of one of the included CPGs. However, she was not involved in eligibility or quality assessment.
References
- 1.Pili R, Gaviano L, Pili L, Petretto DR. Ageing, Disability, and Spinal Cord Injury: Some Issues of Analysis. Curr Gerontol Geriatr Res 2018;2018:4017858. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30581466&dopt=Abstract 10.1155/2018/4017858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verbrugge LM, Yang Ls. Aging with disability and disability with aging. J Disabil Policy Stud 2002;12:253–67. 10.1177/104420730201200405 [DOI] [Google Scholar]
- 3.Ge L, Arul K, Ikpeze T, Baldwin A, Nickels JL, Mesfin A. Traumatic and nontraumatic spinal cord injuries. World Neurosurg 2018;111:e142–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29253698&dopt=Abstract 10.1016/j.wneu.2017.12.008 [DOI] [PubMed] [Google Scholar]
- 4.Holmes D. Spinal-cord injury: spurring regrowth. Nature 2017;552:S49. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29239374&dopt=Abstract 10.1038/d41586-017-07550-9 [DOI] [PubMed] [Google Scholar]
- 5.Ding W, Hu S, Wang P, Kang H, Peng R, Dong Y, et al. Spinal Cord Injury: The Global Incidence, Prevalence, and Disability From the Global Burden of Disease Study 2019. Spine 2022;47:1532–40. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35857624&dopt=Abstract 10.1097/BRS.0000000000004417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kern SB, Hunter LN, Sims AC, Berzins D, Riekena H, Andrews ML, et al. Understanding the Changing Health Care Needs of Individuals Aging With Spinal Cord Injury. Top Spinal Cord Inj Rehabil 2019;25:62–73. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30774290&dopt=Abstract 10.1310/sci2501-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krause JS, Bozard JL. Natural course of life changes after spinal cord injury: a 35-year longitudinal study. Spinal Cord 2012;50:227–31. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21946444&dopt=Abstract 10.1038/sc.2011.106 [DOI] [PubMed] [Google Scholar]
- 8.Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord 2012;50:365–72. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22270188&dopt=Abstract 10.1038/sc.2011.178 [DOI] [PubMed] [Google Scholar]
- 9.Groah SL, Charlifue S, Tate D, Jensen MP, Molton IR, Forchheimer M, et al. Spinal cord injury and aging: challenges and recommendations for future research. Am J Phys Med Rehabil 2012;91:80–93. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21681060&dopt=Abstract 10.1097/PHM.0b013e31821f70bc [DOI] [PubMed] [Google Scholar]
- 10.Sabariego C, Ehrmann C, Bickenbach J, Pacheco Barzallo D, Schedin Leiulfsrud A, Strøm V, et al. Ageing, functioning patterns and their environmental determinants in the spinal cord injury (SCI) population: A comparative analysis across eleven European countries implementing the International Spinal Cord Injury Community Survey. PLoS One 2023;18:e0284420. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=37079622&dopt=Abstract 10.1371/journal.pone.0284420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pili R, Gaviano L, Pili L, Petretto DR. Ageing, disability, and spinal cord injury: some issues of analysis. Curr Gerontol Geriatr Res 2018;2018:4017858. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30581466&dopt=Abstract 10.1155/2018/4017858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson JR, Cronin S, Fehlings MG, Kwon BK, Badhiwala JH, Ginsberg HJ, et al. Epidemiology and impact of spinal cord injury in the elderly: results of a fifteen-year population-based cohort study. J Neurotrauma 2020;37:1740–51. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32292120&dopt=Abstract 10.1089/neu.2020.6985 [DOI] [PubMed] [Google Scholar]
- 13.Hitzig SL, Eng JJ, Miller WC, Sakakibara BM, SCIRE Research Team . An evidence-based review of aging of the body systems following spinal cord injury. Spinal Cord 2011;49:684–701. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21151191&dopt=Abstract 10.1038/sc.2010.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization, International Spinal Cord Society. International perspectives on spinal cord injury. World Health Organization; 2013. [Google Scholar]
- 15.Hill M, Jörgensen S, Levi R. [Spinal cord injury rehabilitation]. Lakartidningen 2021;118:20231–20231. [Swedish]. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34498238&dopt=Abstract [PubMed] [Google Scholar]
- 16.Jensen MP, Molton IR, Groah SL, Campbell ML, Charlifue S, Chiodo A, et al. Secondary health conditions in individuals aging with SCI: terminology, concepts and analytic approaches. Spinal Cord 2012;50:373–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22143678&dopt=Abstract 10.1038/sc.2011.150 [DOI] [PubMed] [Google Scholar]
- 17.Jörgensen S, Iwarsson S, Lexell J. Secondary health conditions, activity limitations, and life satisfaction in older adults with long-term spinal cord injury. PM R 2017;9:356–66. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27647215&dopt=Abstract 10.1016/j.pmrj.2016.09.004 [DOI] [PubMed] [Google Scholar]
- 18.Keusen P, Vuilliomenet T, Friedli M, Widmer M. Age at Onset of Spinal Cord Injury is Associated with Increased Inpatient Care Needs, Reduced Independence at Discharge and a Higher Risk of Institutionalization after Primary Inpatient Rehabilitation. J Rehabil Med 2023;55:jrm00353. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36306176&dopt=Abstract 10.2340/jrm.v54.4468 [DOI] [PMC free article] [PubMed]
- 19.Bragge P, Guy S, Boulet M, Ghafoori E, Goodwin D, Wright B. A systematic review of the content and quality of clinical practice guidelines for management of the neurogenic bladder following spinal cord injury. Spinal Cord 2019;57:540–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30971756&dopt=Abstract 10.1038/s41393-019-0278-0 [DOI] [PubMed] [Google Scholar]
- 20.Steinberg E, Greenfield S, Wolman DM. Clinical practice guidelines we can trust. National Academies Press; 2011. [PubMed] [Google Scholar]
- 21.World Health Organization. International Classification of Functioning, Disability and Health (ICF); 2001 [Internet]. Available from: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health [cited 2024, Feb 27].
- 22.Stucki G, Bickenbach J. 1.1 Basic Concepts, Definitions and Models. J Int Soc Phys Rehabil Med 2019;2: [Google Scholar]
- 23.Bickenbach J, Cieza A, Rauch A, et al. ICF core sets: manual for clinical practice for the ICF research branch, in cooperation with the WHO collaborating centre for the family of international classifications in Germany (DIMDI): Hogrefe Publishing GmbH; 2012. [Google Scholar]
- 24.Kirchberger I, Cieza A, Biering-Sørensen F, Baumberger M, Charlifue S, Post MW, et al. ICF Core Sets for individuals with spinal cord injury in the early post-acute context. Spinal Cord 2010;48:297–304. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19786973&dopt=Abstract 10.1038/sc.2009.128 [DOI] [PubMed] [Google Scholar]
- 25.Cieza A, Kirchberger I, Biering-Sørensen F, Baumberger M, Charlifue S, Post MW, et al. ICF Core Sets for individuals with spinal cord injury in the long-term context. Spinal Cord 2010;48:305–12. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20065984&dopt=Abstract 10.1038/sc.2009.183 [DOI] [PubMed] [Google Scholar]
- 26.Johnston A, Kelly SE, Hsieh SC, Skidmore B, Wells GA. Systematic reviews of clinical practice guidelines: a methodological guide. J Clin Epidemiol 2019;108:64–76. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30529647&dopt=Abstract 10.1016/j.jclinepi.2018.11.030 [DOI] [PubMed] [Google Scholar]
- 27.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88:105906. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33789826&dopt=Abstract 10.1016/j.ijsu.2021.105906 [DOI] [PubMed] [Google Scholar]
- 28.Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health 2019;4:e159–67. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30851869&dopt=Abstract 10.1016/S2468-2667(19)30019-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deep L, editor. 2022 [Internet]. Available from: https://www.deepl.com/translator [cited 2024, Feb 27].
- 30.Brouwers MC, Spithoff K, Kerkvliet K, Alonso-Coello P, Burgers J, Cluzeau F, et al. Development and Validation of a Tool to Assess the Quality of Clinical Practice Guideline Recommendations. JAMA Netw Open 2020;3:e205535. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32459354&dopt=Abstract 10.1001/jamanetworkopen.2020.5535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cieza A, Fayed N, Bickenbach J, Prodinger B. Refinements of the ICF Linking Rules to strengthen their potential for establishing comparability of health information. Disabil Rehabil 2019;41:574–83. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26984720&dopt=Abstract 10.3109/09638288.2016.1145258 [DOI] [PubMed] [Google Scholar]
- 32.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE Working Group . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18436948&dopt=Abstract 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sekido N, Igawa Y, Kakizaki H, Kitta T, Sengoku A, Takahashi S, et al. Clinical guidelines for the diagnosis and treatment of lower urinary tract dysfunction in patients with spinal cord injury. Int J Urol 2020;27:276–88. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32077161&dopt=Abstract 10.1111/iju.14186 [DOI] [PubMed] [Google Scholar]
- 34.Schurch B, Iacovelli V, Averbeck MA, Stefano C, Altaweel W, Finazzi Agrò E. Urodynamics in patients with spinal cord injury: A clinical review and best practice paper by a working group of The International Continence Society Urodynamics Committee. Neurourol Urodyn 2018;37:581–91. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28762566&dopt=Abstract 10.1002/nau.23369 [DOI] [PubMed] [Google Scholar]
- 35.UK National Institute for Health and Care Excellence (NICE). Urinary incontinence in neurological disease: Assessment and management; 2012 [Internet]. Available from: https://www.nice.org.uk/guidance/cg148 [cited 2024, Feb 27]. [PubMed]
- 36.Johns J, Krogh K, Rodriguez GM, Eng J, Haller E, Heinen M, et al. Management of neurogenic bowel dysfunction in adults after spinal cord injury: clinical practice guideline for health care providers. Top Spinal Cord Inj Rehabil 2021;27:75–151. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34108835&dopt=Abstract 10.46292/sci2702-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cotterill N, Madersbacher H, Wyndaele JJ, Apostolidis A, Drake MJ, Gajewski J, et al. Neurogenic bowel dysfunction: Clinical management recommendations of the Neurologic Incontinence Committee of the Fifth International Consultation on Incontinence 2013. Neurourol Urodyn 2018;37:46–53. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28640977&dopt=Abstract 10.1002/nau.23289 [DOI] [PubMed] [Google Scholar]
- 38.Consortium for Spinal Cord Medicine Member Organizations. Pressure ulcer prevention and treatment following spinal cord injury: A clinical practice guideline for health-care professionals; 2014 [Internet]. Available from: https://www.mascip.co.uk/wp-content/uploads/2015/05/CPG_Pressure-Ulcer.pdf [cited 2024, Feb 27]. [DOI] [PubMed]
- 39.Houghton PE, Campbell K. Canadian best practice guidelines for the prevention and management of pressure ulcers in people with Spinal Cord Injury: a resource handbook for clinicians: Ontario Neurotrauma Foundation; 2013 [Internet]. Available from: https://www.woundscanada.ca/docman/public/wound-care-canada-magazine/2013-vol-11-no-2/489-wcc-fall-2013-v11n2-best-practice/file [cited 2024, Feb 27].
- 40.Paralyzed Veterans of America, Consortium for Spinal Cord Medicine. Bone health and osteoporosis management in individuals with spinal cord injury; 2022 [Internet]. Available from: https://pva.org/wp-content/uploads/2022/05/CPG_Spinal-Cord-Medicine_2022_FINAL.pdf [cited 2024, Feb 27].
- 41.Krassioukov A, Linsenmeyer TA, Beck LA, Elliott S, Gorman P, Kirshblum S, et al. Evaluation and management of autonomic dysreflexia and other autonomic dysfunctions: preventing the highs and lows. Management of blood pressure, sweating, and temperature dysfunction. Top Spinal Cord Inj Rehabil 2021;27:225–90. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34108837&dopt=Abstract 10.46292/sci2702-225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wong S, O’Connor L, Twist A, Moseley G, Langan R, Smith É, et al. Multidisciplinary Association for Spinal Cord Injury Professions (MASCIP) Guidelines for Weight-Management in Individuals with Spinal Cord Injury; 2019 [Internet]. https://www.mascip.co.uk/wp-content/uploads/2019/10/03-May-2018-Wong-et-al-MASCIP-Weight-Management-Guidelines-for-People-with-a-Spinal-Cord-Injury.pdf [cited 2024, Feb 27].
- 43.Nash MS, Groah SL, Gater DR, Jr, Dyson-Hudson TA, Lieberman JA, Myers J, et al. Consortium for Spinal Cord Medicine . Identification and management of cardiometabolic risk after spinal cord injury: clinical practice guideline for health care providers. Top Spinal Cord Inj Rehabil 2018;24:379–423. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30459501&dopt=Abstract 10.1310/sci2404-379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Consortium for Spinal Cord Medicine . Prevention of venous thromboembolism in individuals with spinal cord injury: clinical practice guidelines for health care providers. Top Spinal Cord Inj Rehabil 2016;22:209–40. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29339863&dopt=Abstract 10.1310/sci2203-209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.National Institute for Health and Care Excellence. Rehabilitation after traumatic injury (NICE Guideline 211); 2022 [Internet]. Available from: https://www.nice.org.uk/guidance/ng211 [cited 2024, Feb 27]. [PubMed]
- 46.Deutschsprachige Medizinische Gesellschaft für Paraplegiologie. Lebenslange Nachsorge für Menschen mit Querschnittlähmung; 2022 [Internet]. Available from: https://register.awmf.org/assets/guidelines/179-014l_S2k_Lebenslange-Nachsorge-fuer-Menschen-mit-Querschnittlaehmung_2022-12.pdf [cited 2024, Feb 27].
- 47.Free vector humanization concept illustration. Image by Storyset on Freepik; 2024 [Internet]. Available from: https://www.freepik.com/free-vector/humanization-concept-illustration_37452257.htm [cited 2024, Feb 27].
- 48.Feigin VL, Nichols E, Alam T, et al. ; GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019;18:459–80. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30879893&dopt=Abstract 10.1016/S1474-4422(18)30499-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.World Bank. New World Bank country classifications by income level: 2022-2023; 2022 [Internet]. Available from: https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2022-2023 [cited 2024, Feb 27].
- 50.Li Y, Wei B, Zhong Y, Feng H, Wu H. A bibliometric analysis of global research on spinal cord injury: 1999-2019. Spinal Cord 2022;60:281–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34497380&dopt=Abstract 10.1038/s41393-021-00691-9 [DOI] [PubMed] [Google Scholar]
- 51.Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE Working Group . GRADE guidelines: 8. Rating the quality of evidence—indirectness. J Clin Epidemiol 2011;64:1303–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21802903&dopt=Abstract 10.1016/j.jclinepi.2011.04.014 [DOI] [PubMed] [Google Scholar]
- 52.Petrisor BA, Keating J, Schemitsch E. Grading the evidence: levels of evidence and grades of recommendation. Injury 2006;37:321–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16488417&dopt=Abstract 10.1016/j.injury.2006.02.001 [DOI] [PubMed] [Google Scholar]
- 53.Atinga A, Shekkeris A, Fertleman M, Batrick N, Kashef E, Dick E. Trauma in the elderly patient. Br J Radiol 2018;91:20170739. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29509505&dopt=Abstract 10.1259/bjr.20170739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rohollahi F, Farahbakhsh F, Kankam SB, Mohammadi M, Mohammadi A, Korkorian R, et al. Role of Frailty Status in Prediction of Clinical Outcomes of Traumatic Spinal Injury: A Systematic Review and Meta-Analysis. J Neurotrauma 2023;40:2453–68. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=37432902&dopt=Abstract 10.1089/neu.2023.0008 [DOI] [PubMed] [Google Scholar]
- 55.Shakil H, Jaja BN, Zhang PF, Jaffe RH, Malhotra AK, Harrington EM, et al. Assessment of the incremental prognostic value from the modified frailty index-5 in complete traumatic cervical spinal cord injury. Sci Rep 2023;13:7578. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=37165004&dopt=Abstract 10.1038/s41598-023-34708-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Patsakos EM, Bayley MT, Kua A, Cheng C, Eng J, Ho C, et al. Can-SCIP Guideline Expert Panel . Development of the Canadian Spinal Cord Injury Best Practice (Can-SCIP) Guideline: methods and overview. J Spinal Cord Med 2021;44(Suppl 1):S52–68. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34779719&dopt=Abstract 10.1080/10790268.2021.1953312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim C, Armstrong MJ, Berta WB, Gagliardi AR. How to identify, incorporate and report patient preferences in clinical guidelines: A scoping review. Health Expect 2020;23:1028–36. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32656807&dopt=Abstract 10.1111/hex.13099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Institute for Quality and Efficiency in Health Care (IQWiG). What are clinical practice guidelines? Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006. [Google Scholar]
- 59.Rapidi CA, Tederko P, Moslavac S, Popa D, Branco CA, Kiekens C, et al. Professional Practice Committee of the UEMS-PRM Section . Evidence-based position paper on Physical and Rehabilitation Medicine (PRM) professional practice for persons with spinal cord injury. The European PRM position (UEMS PRM Section). Eur J Phys Rehabil Med 2018;54:797–807. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29952157&dopt=Abstract 10.23736/S1973-9087.18.05374-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table I
Eligibility criteria
Supplementary Table II
Exemplary search strategy for PubMed.
Supplementary Table III
List of all identified Clinical Practice Guidelines.
Supplementary Table IV
Characteristics of included clinical practice guidelines.
Supplementary Table V
Ageing-related recommendations.
Supplementary Table VI
Standardization of the Clinical Practice Guidelines grading system.
Supplementary Table VII
Standardization of the Clinical Practice Guidelines grading system.
Supplementary Table VIII
Summary from recommendations organized by areas of interest and linked with relevant ICF codes.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.