Postherpetic neuralgia after herpes zoster can considerably affect quality of life. The current treatment options are discussed here
Herpes zoster (shingles) affects up to half of all people who live to 85 years of age and can lead to long term morbidity. Appropriate treatment controls acute symptoms and reduces the risk of longer term complications. The most common complication in immunocompetent patients is distressing and sometimes intractable chronic pain. Prevention and treatment should be priorities. Most cases of zoster can be managed in primary care and a full understanding of the condition is essential. A previous BMJ editorial focused on variability of estimates of prevalence.1 Here we present an update on the treatment of herpes zoster and postherpetic neuralgia.
Summary points
Appropriate treatment of herpes zoster can control acute symptoms and reduce the risk of longer term complications
Knowledge of risk factors for postherpetic neuralgia can provide a rationale for their prevention
Most cases of zoster and postherpetic neuralgia can be managed in primary care
What is herpes zoster?
Herpes zoster results from recrudescence of latent varicella zoster virus from dorsal root or cranial nerve ganglia, present since primary infection with varicella (chicken pox).2 After the primary infection the virus is probably often reactivated, but competent cell mediated immunity prevents clinical disease. These asymptomatic reactivations and contact with people with varicella may enhance immunity.3 In temperate climates varicella is usually a childhood disease, but in tropical climates, particularly in isolated communities, it is more common in adolescents or adults; in either case zoster may follow. The incidence of zoster in community samples ranges from 1.2-3.4 per 1000 person years.4 At an incidence of 2/1000, about 500 000 cases annually would occur in the United States and about half this number in the United Kingdom.2 The incidence rises steeply with age, being less than 1 per 1000 person years in children and as much as 12 per 1000 person years in those aged over 65 years.4
The commonest cause of viral recrudescence is decline in cell mediated immunity related to age. Reduced immunity associated with some malignancies (such as lymphoma), treatment of malignancy (chemotherapy or radiotherapy), HIV infection, and use of immunosuppressant drugs after organ transplant surgery or for disease management (such as steroids) are also risk factors. As the age of the population and many of these illnesses and treatments will increase in the future we expect that the incidence of zoster will rise. Childhood vaccination against varicella with a live attenuated vaccine is now common in the United States and may be introduced elsewhere. Because the vaccine virus may be less likely to establish latency and reactivate, vaccination may ultimately reduce the incidence of zoster.5 Until this occurs, however, zoster may actually increase as less childhood varicella in the population provides fewer opportunities for boosting specific immunity and thereby limits the contribution such boosting may make to maintaining latency. Vaccination of older adults who have had varicella is being investigated, and this may also prevent or attenuate zoster.6
Management of acute disease
Although there are several serious complications of zoster (ophthalmic, splanchnic, cerebral, motor), the most common in immunocompetent adults is postherpetic neuralgia—pain that continues months or years after the rash has healed. Although postherpetic neuralgia has been defined in different ways, recent data support the distinction between acute herpetic neuralgia (within 30 days of rash onset), subacute herpetic neuralgia (30-120 days after rash onset), and postherpetic neuralgia (defined as pain lasting at least 120 days from rash onset).7,8 The most well established risk factors for postherpetic neuralgia are older age, greater severity of acute pain during zoster, more severe rash, and a prodrome of dermatomal pain before onset of the rash.4 Patients with all of these risk factors may have as much as a 50-75% risk of persisting pain six months after rash onset.
Long term prognosis and treatment
Patients with herpes zoster should receive treatment to control acute symptoms and prevent complications. Severity of the acute symptoms and risk factors for complications must be considered in the assessment of the risk:cost:benefit ratio of different strategies. Patients over the age of 50, irrespective of other risk factors, are at much greater risk of developing postherpetic neuralgia and should be offered treatment. By inhibiting replication of varicella zoster virus, the antiviral agents acyclovir, famciclovir, and valaciclovir attenuate the severity of zoster—specifically, the duration of viral shedding is decreased, rash healing is hastened, and the severity and duration of acute pain are reduced.2 Attenuation of the severity of the acute infection and the neural damage it causes should reduce the likelihood of postherpetic neuralgia. Randomised controlled trials and meta-analyses have shown that antiviral therapy in zoster significantly reduces the risk of prolonged pain. For example, the summary odds ratio for the incidence of pain at six months in zoster patients treated with acyclovir was 0.54 (95% confidence interval 0.36 to 0.81) in a meta-analysis of five placebo controlled trials.9 Although the results of the antiviral trials taken singly can be challenged, the consistency of the findings provides strong support for the use of an antiviral agent. In clinical practice the prodrugs valaciclovir and famciclovir may be more effective than acyclovir (which has poor bioavailability after oral administration) because patients are more likely to comply with treatment (with three rather than five doses a day).
Immunocompromised individuals are at greater risk of complications and may require intravenous acyclovir. Zoster affecting the first division of the trigeminal nerve, particularly if the nasociliary branch is affected (lesions near the tip of the nose), may lead to acute damage to one or more components of the eye and permanent complications that threaten sight. It requires ophthalmic opinion and antiviral therapy. Corticosteroids used alone are not recommended for the treatment of herpes zoster, but in combination with antiviral therapy they may hasten return to premorbid quality of life in patients at high risk for postherpetic neuralgia.2 Acute pain will be reduced by antiviral drugs but patients will also require analgesics, sometimes strong opioids.
Long term prognosis
Unfortunately, some patients with zoster still experience prolonged pain despite adequate antiviral therapy. In patients over 50 years, 20% continue to report pain six months after the onset of the rash despite treatment with valaciclovir or famciclovir.4 Amitriptyline commenced during zoster may reduce the risk of postherpetic neuralgia, as may opioid analgesics and gabapentin.10 Invasive therapy during acute zoster, such as somatic or sympathetic nerve block, however, remains controversial.11 Several peer reviewed guidelines for the management of zoster exist.12 Early return to normal social and domestic activities should be encouraged.
Established postherpetic neuralgia may be intractable and lead to considerable disability and suffering in an elderly patient's final years of life. First line therapy includes attention to psychosocial factors as well as medical treatment. Patients need clear advice on measures such as use of natural fibre clothing and maintenance of social and physical activities. If appropriate dosages of a tricyclic antidepressant (preferably nortriptyline) or gabapentin do not provide adequate relief, strong opioids such as oxycodone, morphine, or methadone may be required. The number needed to treat for tricyclics or gabapentin is about 3. Combination therapy is common, and the multiple putative mechanisms of neuropathic pain provide a rationale for this approach, but studies have not been conducted to examine its efficacy. All these medications should be used with close monitoring as there are considerable risks in elderly patients.10,13 Oral medication is often associated with side effects, and patients are more likely to comply with treatment if these are explained and doses are adjusted. Some side effects may be controllable—for example, artificial saliva spray for dry mouth secondary to treatment with tricyclic antidepressants.
A local anaesthetic (lidocaine 5%) patch can provide pain relief with minimal side effects and, where it is available, is often used in combination with oral medications.10,13 Some patients can benefit from other techniques, including topical capsaicin and topical application of aspirin suspended in a volatile substance such as acetone.13 A highly controversial therapy for patients failing to respond to conventional management involves intrathecal injection of methylprednisolone. Although results seemed good and complications few, the risk of serious complications may preclude use of this treatment until well designed studies have confirmed efficacy and lack of morbidity.14
Recent guidelines, with supporting evidence, and further information
International Herpes Management Forum (IHMF) www.IHMF.org
Varicella Zoster Virus Research Foundation (VZVRF) www.vzvfoundation.org
Early treatment in postherpetic neuralgia may be more effective than later treatment.15 Although additional research is needed to confirm this, it is clearly desirable to relieve chronic pain as early in its course as possible. The primary care provider can often achieve effective pain control in patients with either herpes zoster or postherpetic neuralgia. However, when either the acute pain of herpes zoster or the chronic pain of postherpetic neuralgia is not rapidly and effectively controlled in primary care with the first line medications discussed above, referral to a pain specialist or pain management centre should be considered to reduce pain and to improve the patient's quality of life.
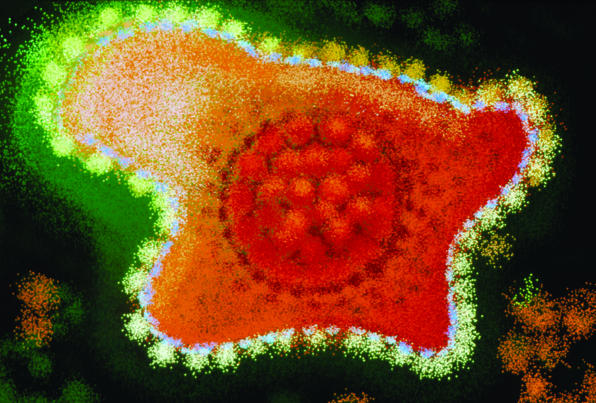
Figure.
BSIP VEM/SPL
Transmission electron micrograph of varicella zoster virus
Figure.
P MARAZZI/SPL
Blisters on skin caused by herpes zoster infection
Footnotes
Funding: None.
Competing interests: RWJ has undertaken research for Pfizer on gabapentin and pregabalin. He has acted as adviser to GlaxoSmithKline, Pfizer, and Johnson and Johnson in the past. He is a board member of the International Herpes Management Forum, which has received unrestricted educational grants from several commercial organisations. RHD has received research support from, served as a consultant to, and been on the speakers bureau for AstraZeneca, Elan Pharmaceuticals, King Pharmaceuticals, National Institute of Health, NeurogesX, Novartis, Ortho-McNeil Pharmaceutical, Pfizer, Reliant Pharmaceuticals, UCB Pharma, US Department of Defense, and US Food and Drug Administration.
References
- 1.Cunningham AL, Dworkin RH. The management of post-herpetic neuralgia. BMJ. 2000;321:778–779. doi: 10.1136/bmj.321.7264.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gnann JW, Jr, Whitley RJ. Herpes zoster. N Engl J Med. 2002;347:340–346. doi: 10.1056/NEJMcp013211. [DOI] [PubMed] [Google Scholar]
- 3.Thomas SL, Wheeler JG, Hall AJ. Contacts with varicella or with children and protection against herpes zoster in adults: a case-control study. Lancet. 2002;360:678–682. doi: 10.1016/S0140-6736(02)09837-9. [DOI] [PubMed] [Google Scholar]
- 4.Dworkin RH, Schmader KE. Epidemiology and natural history of herpes zoster and postherpetic neuralgia. In: Watson CPN, Gershon AA, editors. Herpes zoster and postherpetic neuralgia. 2nd ed. New York: Elsevier Press; 2001. pp. 39–64. [Google Scholar]
- 5.Gershon AA. Live-attenuated varicella vaccine. Infect Dis Clin North Am. 2001;15:65–81. doi: 10.1016/s0891-5520(05)70268-3. [DOI] [PubMed] [Google Scholar]
- 6.Levin MJ. Use of varicella vaccines to prevent herpes zoster in older individuals. Arch Virol. 2001;suppl 17:151–160. doi: 10.1007/978-3-7091-6259-0_16. [DOI] [PubMed] [Google Scholar]
- 7.Dworkin RH, Portenoy RK. Proposed classification of herpes zoster pain. Lancet. 1994;343:1648. doi: 10.1016/s0140-6736(94)93106-2. [DOI] [PubMed] [Google Scholar]
- 8.Desmond RA, Weiss HL, Arani RB, Soong SJ, Wood MJ, Fiddian PA, et al. Clinical applications for change-point analysis of herpes zoster pain. J Pain Symptom Manage. 2002;23:510–516. doi: 10.1016/s0885-3924(02)00393-7. [DOI] [PubMed] [Google Scholar]
- 9.Jackson JL, Gibbons R, Meyer G, Inouye L. The effect of treating herpes zoster with oral acyclvir in preventing postherpetic neuralgia: a meta-analysis. Arch Intern Med. 1997;157:909–912. [PubMed] [Google Scholar]
- 10. Dworkin RH, Schmader KE. Treatment and prevention of postherpetic neuralgia. Clin Infect Dis 2003 (in press). [DOI] [PubMed]
- 11.Wu CL, Marsh A, Dworkin RH. The role of sympathetic nerve blocks in herpes zoster and postherpetic neuralgia. Pain. 2000;87:121–129. doi: 10.1016/S0304-3959(00)00230-X. [DOI] [PubMed] [Google Scholar]
- 12.Johnson RW, Mandal BK. Guidelines for the management of shingles: report of a working group of the British Society for the Study of Infection. J Infect. 1995;30:193–200. [PubMed] [Google Scholar]
- 13.Kanazi GE, Johnson RW, Dworkin RH. Treatment of postherpetic neuralgia: an update. Drugs. 2000;59:1113–1126. doi: 10.2165/00003495-200059050-00007. [DOI] [PubMed] [Google Scholar]
- 14.Kotani N, Kushikata T, Hashimoto H, Kimura F, Muraoka M, Yodono M, et al. Intrathecal methylprednisolone for intractable postherpetic neuralgia. N Engl J Med. 2000;343:1514–1519. doi: 10.1056/NEJM200011233432102. [DOI] [PubMed] [Google Scholar]
- 15.Bowsher D. Postherpetic neuralgia and its treatment: a retrospective survey of 191 patients. J Pain Symptom Manage. 1996;12:290–299. doi: 10.1016/s0885-3924(96)00180-7. [DOI] [PubMed] [Google Scholar]