Abstract
Whole genome duplication is frequently observed in cancer, and its prevalence in our prior analysis of end-stage, homologous recombination deficient high grade serous ovarian cancer (almost 80% of samples) supports the notion that whole genome duplication provides a fitness advantage under the selection pressure of therapy. Here, we therefore aim to identify potential therapeutic vulnerabilities in primary high grade serous ovarian cancer with whole genome duplication by assessing differentially expressed genes and pathways in 79 samples. We observe that MHC-II expression is lowest in tumors which have acquired whole genome duplication early in tumor evolution, and further demonstrate that reduced MHC-II expression occurs in subsets of tumor cells rather than in canonical antigen-presenting cells. Early whole genome duplication is also associated with worse patient survival outcomes. Our results suggest an association between the timing of whole genome duplication, MHC-II expression and clinical outcome in high grade serous ovarian cancer that warrants further investigation for therapeutic targeting.
Subject terms: Cancer genomics, Ovarian cancer, Tumour immunology
There is high prevalence of whole genome duplication (WGD) in high grade serous ovarian cancer. Here, the authors compare tumours with and without WGD and find that those that acquired WGD early during tumour evolution are associated with worse survival and have the lowest expression of MHC-II.
Introduction
Whole genome duplication (WGD) is frequently observed in many cancer types, including high grade serous ovarian cancer (HGSC)1,2. WGD serves as a buffer to tolerate acquisition of deleterious mutations and consequently is positively selected for under certain conditions, despite a fitness cost to cells3. WGD has been observed in 50–60% of primary ovarian cancers4,5, yet we observed a higher proportion in our study of end-stage homologous recombination (HR) deficient HGSC (79.6% of tumours), suggesting that WGD continues to be acquired after diagnosis6. There are multiple genomic events that occur in HGSC which can predispose toward polyploidy and WGD such as TP53 mutations, and PIK3CA and CCNE1 alterations1,7–9. Both its frequency and continued acquisition under the selection pressure of therapy indicate that WGD is advantageous in HGSC1,4,10.
HGSC confers a poor prognosis, with a 5-year survival approaching 50%11–13, and is rarely cured once diagnosed, even in those with a good initial response to treatment. Our previous work starkly illustrated that the mechanisms of resistance are diverse6, and targeted treatments do not exist for many of these in mainstream clinical practice. New treatments have been sought for HGSC, however the response to immune checkpoint inhibitor (ICI) therapy has been poor, despite evidence that the immune milieu has an important role in ovarian cancer control and survival14–16. This may be due to a lack of tumour or stromal immune cell infiltration, and specific mechanisms of immune escape17. While immune escape related to reduced neoantigen presentation has been largely described with regard to MHC-I in HGSC and other cancer types17–19, there is increasing suggestion that MHC-II expression also plays a prominent role20. Canonical antigen presenting cells, including macrophages, dendritic cells and B cells, as well as cancer cells, can express MHC-II and present neoantigens20,21. The presence of MHC-II on cancer cells can even predict response to ICI20,22. Additionally, across tumour types, aneuploidy and response to ICI have been linked23.
We hypothesized that WGD might drive unique transcriptional processes in HGSC that may contribute to disease recurrence and treatment resistance. Therefore, if these could be targeted early in cancer evolution, then development of resistance could be abrogated.
In this work, we aim to elucidate the characteristics of primary HGSC which have undergone WGD that may represent therapeutic vulnerabilities, and demonstrate here an association between the timing of WGD and MHC-II expression in HGSC, as well as with clinical outcomes.
Results
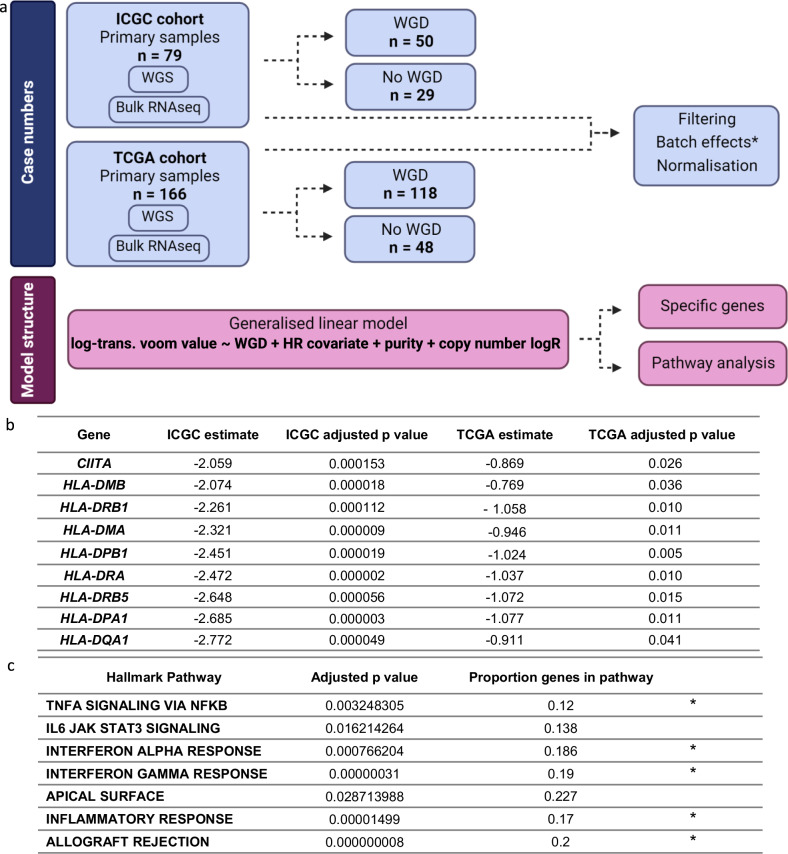
MHC-II pathway expression is reduced in tumours with WGD
Whole genome sequencing (WGS) data from seventy-nine primary HGSC tumour samples in the International Cancer Genome Consortium (ICGC) study, described previously by Patch et al.24, was analysed for whole genome duplication (WGD) status. WGD was defined as the tumour having >50% of the autosomal genome with a major copy number (MCN) ≥ 21. Fifty of these tumours had WGD and 29 did not. To identify genes where expression differed between cases with and without WGD, a differential gene expression (DGE) analysis was performed using the matched RNA sequencing data and a generalised linear model (GLM) (Fig. 1a). This included covariates of purity as well as gene specific copy number inferred from FACETS25 for each sample, since by definition tumours with WGD are likely to have a greater number of copy number amplifications potentially affecting gene expression. The coefficient estimate generated by the GLM was used as the magnitude of difference in place of log fold change, since this model needed to account for per gene, per sample covariates, unlike standard DGE analysis tools, and log fold change is not determined by the model. The median tumour purity estimated by FACETS was 68.7% in tumours without WGD and 62% in tumours with WGD (Supplementary Table 1). Of the 16,375 genes input into the model, 82 were significantly upregulated and 593 significantly downregulated using a coefficient estimate threshold of ±1.5 and a p value < 0.05. The higher number of down-regulated compared to up-regulated genes in tumours with WGD is likely due to the fact that the model accounts for copy number log ratio as a covariate, since by definition tumours with WGD will have higher total copy number per gene.
Fig. 1. Differential gene expression analysis workflow and key results.
a Schematic demonstrating (top) case numbers for the International Cancer Genome Consortium (ICGC) discovery and The Cancer Genome Atlas (TCGA) validation cohort and workflow, and (bottom) the differential gene expression (DGE) generalised linear model structure. *The TCGA validation cohort was processed in the same manner, however batch correction was not possible since batch information is not given. Whole genome duplication (WGD), homologous recombination deficiency (HRD). Created with BioRender.com. b Key DGE results derived from generalised linear model for CIITA and MHC-II related genes with significantly lower expression in both the discovery and validation cohorts in WGD samples. c Overrepresented pathways derived by integrating discovery and validation DGE results through ActivePathways35 (ranked hypergeometric test) using the differentially expressed geness with significantly lower expression in WGD samples. Asterisks denote pathways involved in immune response. Source data are provided as a Source Data file and Supplementary Table 2. P values are adjusted for multiple comparisons.
Interestingly, we noted that 13 MHC-II genes had a statistically significant coefficient estimate <−1.5 in tumours with WGD compared to those without. Despite these genes being located on chromosome 6, this did not appear to be driven by a consistent chromosomal arm loss occurring in the tumours with WGD (Supplementary Fig. 1a). Similarly, comparing the segment copy number there was no significant difference in the segment mean between MHC-II genes and other genes in the same region (6p21.32–6p25.3; p = 0.09; Supplementary Fig. 1b). In addition, by comparing the coefficient estimates from the model for all genes within the region on 6p where these genes are located, we observed that the low expression specifically affected the MHC-II genes rather than being common to all genes in the region (p < 0.001, Wilcoxon’s test; Supplementary Fig. 1c). CD74, which encodes the invariant chain that binds to the MHC alpha and beta chains and is located on chromosome 5, also had significantly lower expression (coeff. est. −1.95, p < 0.001), supporting our observation that there is specific downregulation of MHC-II-related genes in the tumours with WGD and this is independent of chromosomal loci. Finally, we re-ran our model without copy number as a covariate, producing similar results (Supplementary Tables 2, 3). This indicates that the transcriptional differences observed are independent of gene specific copy number status.
We hypothesized that altered expression of a transcription factor or upstream regulator may explain this MHC-II depletion. Consistent with this notion, we found that the Class II Major Histocompatibility Complex Transactivator (CIITA) gene, known as the master-regulator of MHC-II activity26, was also significantly downregulated in tumours with WGD (coeff. est. = −2.06, p < 0.001). These DGE results were then verified in the independent TCGA dataset, specifically in a cohort of 166 HGSC tumours for which complete clinical information, copy number, tumour purity and RNAseq data was available. The intersect of genes between the 2 datasets that were differentially expressed at any magnitude was assessed (n = 689 genes with copy number covariate, Supplementary Table 2; n = 550 without copy number covariate, Supplementary Table 3). In this way, CIITA and 8 of the 13 MHC-II genes were also confirmed to be significantly more lowly expressed in the WGD samples of the TCGA validation set, albeit by a smaller magnitude (Fig. 1b).
We sought determinants of the difference in CIITA expression between samples with or without WGD. Though MHC-II is constitutively expressed by canonical antigen-presenting cells, it can also be inducibly expressed by other cells including tumour cells27–29. CIITA expression is typically controlled by methylation of four context-specific promoters21,30–32. Using our previously generated methylation array data6,24 it was only possible to identify 1 probe likely to correspond to a CIITA promoter region; however, no samples were hypermethylated at this probe. We also did not find evidence of CIITA hypermethylation in the TCGA data. Upstream signalling factors reported to regulate the expression of CIITA include IFNγ, JAK1, STAT1, IRF1 and FBXO1121,33,34, however none of these were significantly differentially expressed across both the discovery and validation datasets. There was however a moderate correlation between IRF1 (a positive regulator of CIITA) and CIITA expression in both datasets (ICGC R = 0.53, p < 0.001; TCGA R = 0.51, p < 0.001, Spearman’s test; Supplementary Fig. 2a, b).
Pathway analysis reveals depletion of immune response in WGD
Pathway enrichment analysis was conducted using the most highly and lowly expressed genes from the DGE results for the ICGC discovery and TCGA validation cohorts using ActivePathways35, which integrates results from multiple datasets, to identify significantly enriched Hallmark pathways. Seven downregulated and no upregulated pathways were identified as being associated with presence of WGD (Fig. 1c). Notably, the significantly depleted processes largely related to the immune response. Downregulated pathways were similar to those described in a pan-cancer analysis of differentially expressed pathways between cancers with and without WGD, which found Allograft rejection, Inflammatory response and Interferon gamma response to be downregulated in samples with WGD3.
Timing of WGD is associated with MHC-II gene expression
In pan-cancer studies, WGD has been described as occurring early in tumorigenesis or comparatively ‘later’, around the time of diagnosis2; WGD may also occur after diagnosis. We hypothesised that MHC-II expression and other biological processes highlighted by our pathway analysis might be affected by the timing of WGD acquisition, and therefore used the method described by Dewhurst et al. to categorise WGD as ‘early’ or ‘late’36. Their method uses genomic regions with a total copy number of 2 to categorise tumours with more heterozygous regions as having undergone genome duplication before the majority of losses (early), and tumours with more homozygous regions classified as having undergone WGD after the majority of losses (late). While this is acknowledged to be heuristic, our findings were concordant with the previous analysis by Gerstung et al.2 for the 36 ICGC samples with WGD analysed by both methods (Supplementary Fig. 2c).
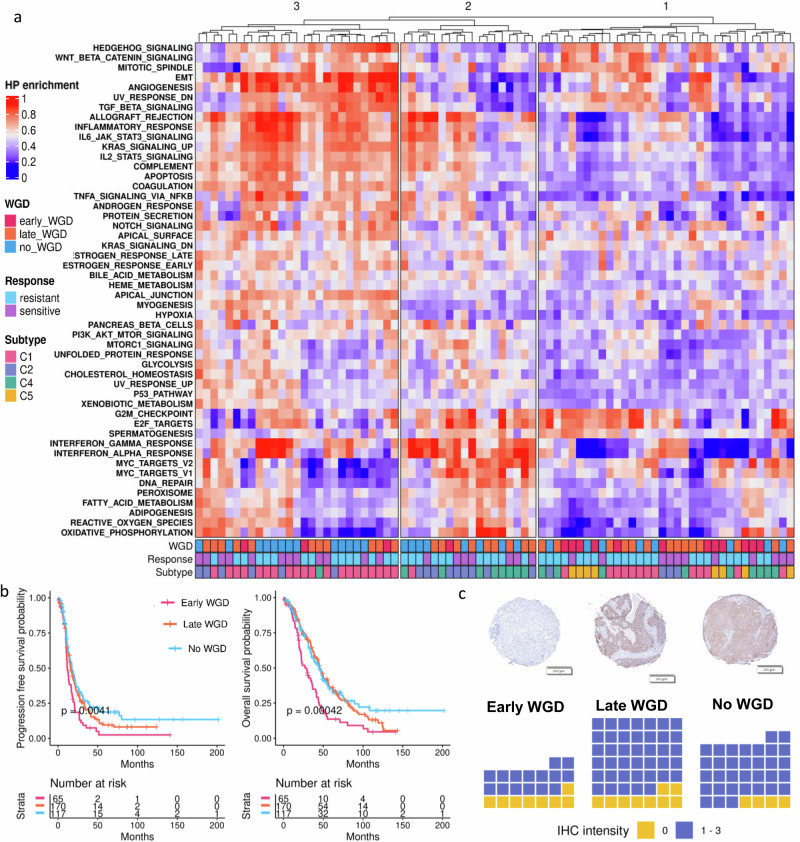
Using the ICGC discovery dataset, we observed that Hallmark pathway enrichment scores clustered by timing of WGD (Fig. 2a). Clade 1, with downregulation of pathways related to immune response identified in the analysis by ActivePathways (Interferon Gamma response, Interferon Alpha response, Inflammatory response, Allograft rejection, and TNF signalling via NF-KB), was enriched for tumours with early WGD (p = 0.04, Chi squared test). This pattern of enrichment was similar in the TCGA dataset but was not statistically significant (p = 0.14, Chi squared test; Supplementary Table 4). As HGSC molecular subtypes are associated with the extent of epithelial and stromal immune cell infiltration and patient response to treatment37, we also annotated each sample for these. Notably, C5 (proliferative) samples, which are immune depleted38, exclusively fell into this clade. In keeping with this we observed that LIN28B, which is highly expressed in C5 tumours39, was one of most significantly upregulated genes in WGD samples (Supplementary Tables 2, 3). In contrast, the second and third clades, enriched for tumours with late WGD and tumours without WGD respectively, generally displayed enrichment of immune related pathways. Clade 3 was notably enriched for the C1 (mesenchymal) subtype.
Fig. 2. Differences in gene expression and clinical outcomes by timing of WGD.
a Hierarchical clustering of Hallmark pathway enrichment scores in the discovery ICGC cohort. n = 79. Heatmap is annotated by timing of whole genome duplication (WGD), clinical response to first line therapy and molecular subtype (C1,C2,C4,C5). b Two-sided Kaplan–Meier analysis of overall survival (top) and progression free survival (bottom) by presence and timing of WGD in 352 patients (ICGC and TCGA cohorts combined). c Top: Representative image of core stained with anti-HLA DR + DP + DQ for each WGD category; scale bar is 200 μm. Bottom: Waffle plots depicting immunohistochemistry (IHC) results, coloured by zero (yellow) versus any (lilac) staining with anti-HLA DR + DP + DQ, separated by WGD status. Early WGD n = 23 cores; Late WGD n = 49 cores; No WGD n = 37 cores. Source data are provided as a Source Data file.
Tumours with early WGD had significantly lower expression of CIITA compared to those with late or no WGD (p = 0.04, Kruskal-Wallis test, ICGC dataset, Supplementary Fig. 2d). The same pattern was observed for the 8 MHC-II genes that had been identified as significantly differentially expressed across both the ICGC and TCGA cohorts. Expression of these genes was lowest in the tumours with early WGD, though only 4 of 8 genes were statistically significant after adjustment for multiple testing (Supplementary Fig. 2d). Taken together, reduced CIITA and MHC-II gene expression was more strongly associated with early WGD, rather than just WGD generally. We hypothesized then that reduced MHC-II expression might contribute to immune evasion in patients with tumours which have undergone early WGD, and that therefore patients with early WGD might have poorer survival outcomes. In order to have sufficient power to detect survival differences by WGD timing we examined patient survival in a combined cohort (79 ICGC cases and 166 TCGA cases, plus 107 additional TCGA cases for which WGS and survival information were accessible; total of 352 patients). Strikingly, both progression free survival (PFS) and overall survival (OS) were significantly worse for cases with early WGD, with little separation between those with late or no WGD (Fig. 2b). This remained significant in multivariate analysis with both age and stage at diagnosis, using Cox proportional hazards for both OS (p = 0.002 late WGD, p = 0.03 no WGD) and PFS (p = 0.01 late WGD, p = 0.003 no WGD; Supplementary Fig. 2e,f).
Tumour-specific CIITA and MHC-II gene expression
We next sought to determine whether the reduced MHC-II expression seen in bulk sequencing data from tumour samples with WGD was due to altered expression by tumour or antigen-presenting cells. While canonical antigen-presenting cells such as dendritic cells, macrophages and B cells are typically the source of MHC-II expression, tumour cell specific MHC-II expression has been shown in ovarian cancer as well as other cancer types28,29,40, where it predicts response to immune checkpoint inhibition22,41. Using CIBERSORTx immune cell imputations, we did not observe a difference in proportion of B cells, dendritic cells nor macrophages by timing of WGD (Supplementary Tables 5, 6), hence we hypothesised that differences in MHC-II expression were caused by inducible expression in tumour cells, as has been suggested in other studies29,40. To ascertain the cell types expressing MHC-II, we evaluated protein expression of MHC-II by immunohistochemistry (IHC) using an anti-HLA DR + DP + DQ antibody. Sixty-one of the 79 ICGC tumours were tested (13 with early WGD, 27 with late WGD and 21 without WGD). Review of the IHC by a gynaecologic pathologist determined that MHC-II was expressed in the tumour cells as well as immune cells. MHC-II IHC staining intensity was reduced in tumour cells from cases with early WGD compared to either late or no WGD (p = 0.049, glmm, Supplementary Fig. 3). In contrast, neither tumour-infiltrating lymphocytes nor stromal lymphocytes displayed a significant difference in MHC-II staining intensity by timing of WGD. Overall, there were proportionally more tumours with a complete absence of MHC-II expression in the group with early WGD, yet this did not reach statistical significance (p = 0.06, Chi squared test, Fig. 2c).
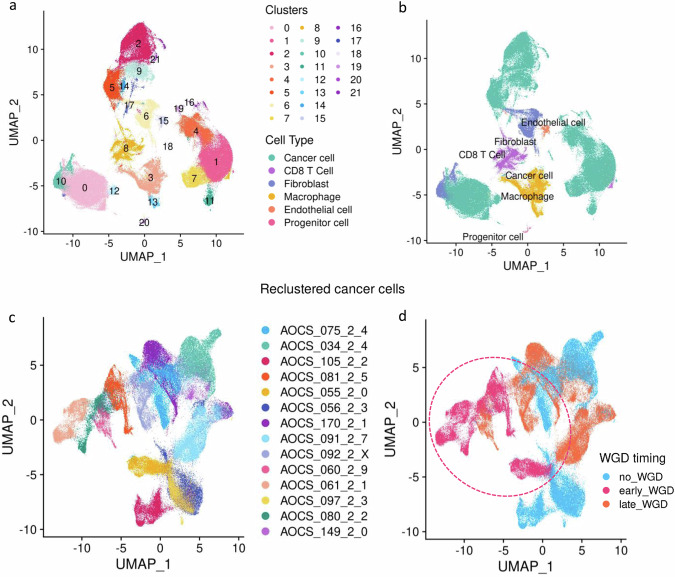
To address which cells are expressing CIITA and to examine the intercellular MHC-II signalling associated with this, we performed single nuclei RNA sequencing (snRNAseq) of 5 patient samples each with either early, or late or no WGD (n = 15, Supplementary Table 7). For one sample, sufficient nuclei could not be extracted at the lysis step and was not processed further, hence a total of 195,712 single nuclei from tumour samples from 14 patients were sequenced and passed quality control. Following filtering and transformation, principal component analysis and UMAP analysis generated 22 clusters from 177,801 nuclei. Cells were annotated using a consensus method of cancer cell markers and marker-based annotation with ScType42, and assessed for aneuploidy prediction using CopyKAT (Fig. 3a, b, Supplementary Table 8).
Fig. 3. Single nuclei RNA sequencing.
a UMAP plots of all cells coloured by Seurat clusters. b UMAP plots of all cells coloured by cell types. c UMAP of reclustered cancer cells coloured by patient. d UMAP of reclustered cancer cells coloured by whole genome duplication (WGD) timing (inferred per patient from bulk WGS). Ellipse highlights early WGD clustering. For a and b: Early WGD n = 4 patients, 33,965 nuclei; Late WGD n = 5 patients, 63,156 nuclei; No WGD n = 5 patients, 80,680 nuclei. c, d Early WGD n = 4 patients, 31,479 nuclei; Late WGD n = 5 patients, 48,685 nuclei; No WGD n = 5 patients, 60,602 nuclei.
Fifteen cancer cell clusters were identified through cell type annotation. These were then re-clustered separately to assess cancer cell-specific differences (Fig. 3c, d). Annotated by WGD status, this demonstrated a macro-cluster of cancer cells from tumours with early WGD, separate from cancer cells with late or no WGD (Fig. 3d).
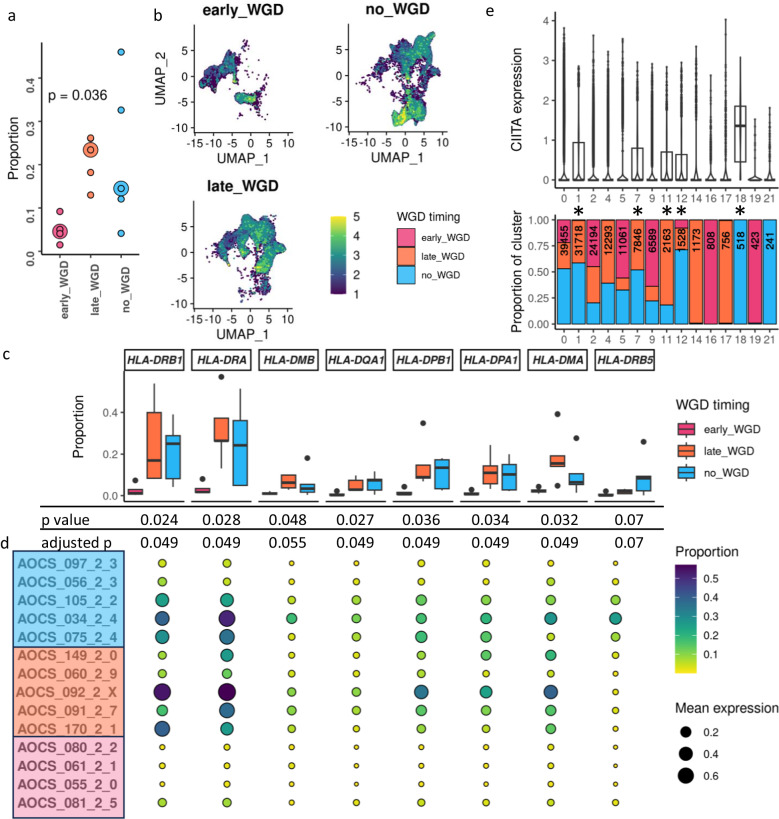
We confirmed that CIITA was expressed in proportionally fewer cancer cells within each patient sample in tumours with early WGD, compared to those with late or no WGD (p = 0.04, Fig. 4a). Comparison of the level of CIITA expression across all cancer cell clusters confirmed that CIITA was also significantly more lowly expressed in early WGD tumours (coeff. est. = 4.91 late WGD, p value < 0.001, coeff. est. = 4.18 no WGD, p value < 0.001, glmm; Fig. 4b). This was also reflected in the proportions of cancer cells expressing MHC-II genes across and within cases (Fig. 4c, d, Supplementary Fig. 4). Further analysis revealed that CIITA expression levels in cancer cells was not uniform; interrogating the individual clusters revealed that CIITA was substantially expressed in only 5 of the 15 cancer cell clusters (Fig. 4e). These 5 clusters were strongly enriched for cells from tumours with late or no WGD (p = <0.001, Chi squared test), with only 1.0% of cancer cells from patients with early WGD falling into these 5 clusters, compared to 38.6% and 40.7% of late and no WGD cancer cells respectively. Having seen a moderate correlation between CIITA and IRF1 in the bulk RNAseq data, we examined this in the snRNAseq, but found a more modest correlation between CIITA and IRF1 expression within cancer cells (R = 0.26, p < 0.001, CS-CORE, Supplementary Fig. 5a). All MHC-II genes which were statistically significant in the bulk RNAseq DGE analysis also had a statistically significant correlation with CIITA expression within cancer cells in the snRNAseq data (Supplementary Fig. 5a).
Fig. 4. CIITA and MHC-II gene expression in snRNAseq.
a Proportion of cancer cells expressing CIITA. Each small dot represents an individual patient. Large dot represents median for that category. Early WGD n = 4 patients; Late WGD n = 5 patients; No WGD n = 5 patients. Large dot represents median for that category. p = 0.036, Kruskal–Wallis test. b Feature UMAP plots of CIITA expression within cancer cells only, split by whole genome duplication (WGD) status. Cells are visualised in each plot from lowest to highest expression and numerical expression depicted as a relative scale to enable visualisation. c Boxplots summarising the proportion of cancer cells per patient expressing each MHC-II gene that was significant in the bulk DGE analysis. P values (Kruskal–Wallis test) and adjusted p values are depicted below. Early WGD n = 4 patients, 31,479 nuclei; Late WGD n = 5 patients, 48,685 nuclei; No WGD n = 5 patients, 60,602 nuclei. d Proportion of cancer cells expressing each gene shown for each patient individually, grouped by WGD timing. Mean expression denoted by size of circle (see legend). e Violin plots overlaying boxplots of CIITA expression in cancer cells by original Seurat cluster (top), annotated by proportion of cells from each WGD status category (bottom). Asterisks denote clusters designated to have substantial expression. For all boxplots: Left and right whiskers terminate at the minimum and maximum values no further than 1.5× interquartile range; centre line represents median (50th percentile); left and right boundaries of box represent the first (25th percentile) and third (75th percentile) quartiles, respectively; outlying values are plotted as individual points beyond whiskers. Source data are provided as a Source Data file.
The tumour microenvironment and its interactions with cancer cells
In the snRNAseq data immune cells were observed in lower proportions in tumours with early WGD compared to those with late or no WGD, but this did not reach statistical significance (p = 0.07, Kruskal–Wallis test, Supplementary Fig. 5b, Supplementary Table 9).
We conducted a non-comparative examination of intercellular communications, identifying expression of statistically significant ligand-receptor pairs in the snRNAseq data between the cell clusters identified by Seurat using CellChat43; Supplementary Fig. 5c, Supplementary Table 10). Similarities across the three WGD categories were noted; for example, cancer-associated fibroblasts (Fibroblast_6) were the source of strong outgoing communications with both immune and cancer cells across all 3 WGD groups (Supplementary Fig. 5d), suggesting that they are a substantial contributor to modulation of the tumour microenvironment. Cancer cell_0, the largest cluster of cancer cells (28%), had few outgoing signals, little inter-cluster communication, and multiple but weak incoming signals. Conversely, many other cancer cell clusters such as Cancer cell_1 demonstrated multiple incoming and outgoing communications. These differences suggest that the individual cancer cell clusters represent unique populations of cancer cells, whereby some are relatively autonomous and less affected by the surrounding environment, whereas others are strongly modulated by communication with malignant and non-malignant cells.
In a descriptive analysis of interactions between cell subsets in the different WGD categories, tumours with early WGD had markedly low MHC-II signalling (Fig. 5). Only macrophages displayed any MHC-II signalling in tumours with early WGD; in contrast, extensive intercellular MHC-II signalling between macrophages and both cancer and non-malignant cells was observed in tumours with late or no WGD. While this is a non-comparative observation, this was also reflected in the per-gene pattern of MHC-II gene expression between WGD categories in cancer cells (Fig. 4c, d).
Fig. 5. Ligand-receptor pair communication predictions between cell clusters.
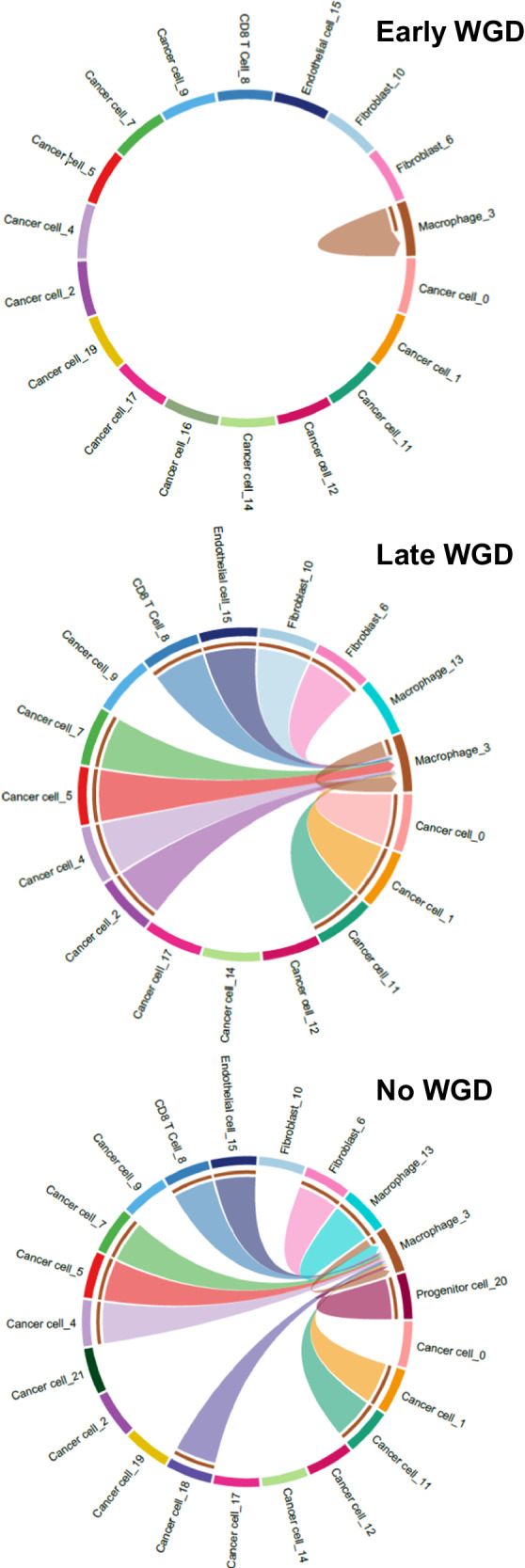
Circle plots visualising the presence or absence of statistically significant interactions between and within cell groups for MHC-II (KEGG pathway hsa04514). The whole genome duplication (WGD) subgroups (early, late and no WGD) are individually depicted and not directly compared. Source data are provided in Supplementary Table 10.
Discussion
WGD is a frequent event in HGSC, yet its impact on tumour evolution is not well understood. Our findings suggest that early acquisition of WGD sculpts the molecular landscape of the tumour, resulting in decreased MHC-II expression compared to cancer cells with late or no WGD. Separately, we identified an association between the timing of WGD and patient survival outcomes. Together, these findings indicate a possible relationship between timing of WGD, MHC-II expression and clinical outcome in HGSC. While prior work has suggested there are worse outcomes in HGSC and other tumour types with WGD compared to those without, including more advanced stage at diagnosis and survival1,5,44, the clinical relevance of WGD timing in HGSC has not previously been examined. Although we have not demonstrated a causative link between MHC-II expression and survival, it is plausible that they are directly related, given the strong association of immune cell infiltration and survival in HGSC, which has been recognised for many years14. We also identified cancer cell heterogeneity, with only a subset of cancer cells expressing MHC-II, likely driven by inducible CIITA expression, and that these cells are rare in cancers with early WGD.
Neoantigen expression is required to generate anti-tumour CD8 and CD4 T cell responses. Though loss of MHC-class I expression has been more strongly linked to cancer as a mechanism of immune escape17,19, our findings demonstrate compelling evidence of tumour-specific MHC-class II dependent activity in HGSC and a potential pathway to immune escape in HGSC with early WGD. As cancer cells with WGD are genomically unstable and generally have a higher mutation burden than those without WGD45,46, WGD is likely to result in more immunogenicity due to a higher neoantigen burden and reduced MHC-II expression may be especially advantageous for survival of cancer cells with WGD. This is supported by observations of a relationship between aneuploidy or WGD and correlates of immune evasion in patient cohorts3,23. Furthermore, Davoli et al. described lower expression of pathways related to interferon gamma and immune regulation in tumours with high somatic copy number alterations across tumour types by GSEA analysis, including significantly lower CIITA expression23. Importantly they identified a relationship between high levels of aneuploidy and poor response to CTLA4 inhibition in patients with melanoma.
We did not identify a definite determinant of CIITA transcriptional control in this study. This is a topic which has been studied extensively in other tumour types26,30,32,47. It remains quite possible that hypermethylation of the pIV promoter of CIITA controls tumour-specific MHC-II expression, however we could not demonstrate this here, due to the limitations of genome-wide methylation arrays used in the included studies. Other limitations of this study include the inability to accurately evaluate tumours for their MHC-II specific neoantigen expression. In contrast to MHC-I, current methods of bioinformatically assessing neoantigens are suboptimal for MHC-II, in part due to the promiscuity of MHC-II molecules48. Additionally, it is unclear whether early acquisition of WGD occurs via a different mechanism to WGD acquired later and that this might explain the differences in patient survival and expression of CIITA and MHC class II genes between the groups. Alternatively, early WGD may simply reflect more time for the evolution of immune escape between WGD and the timing of sampling. Our findings illuminate an important gap in our knowledge of the immune response in HGSC.
Since the presence of tumour-specific MHC-II-expressing cancer cells is a predictor of ICI response in melanoma and triple negative breast cancer20,22,49, our findings may have implications for therapeutic intervention in HGSC. Modest responses to ICI have been observed to date in ovarian cancer, but this may be due to the unselected nature of the ICI trials, and that they were used in later lines of treatment, by which time tumours have often evolved to become immune depleted5,44. The possibility of successful immune targeting agents with more MHC-II ligand specificity, such as LAG3 or TIM3, may be more fruitful in HGSC27,50,51. Since inducible CIITA expression is controlled epigenetically, hypomethylating agents may be able to reverse hypermethylation and abrogate the reduced CIITA and MHC-II expression in early WGD HGSC tumours40,52. It is clear from our previous work6 that targeting resistance mechanisms earlier in the clinical course is vital to stem the development of a heterogenous cancer landscape with numerous resistance mechanisms that cannot all be plausibly targeted. Identifying early features of HGSC which are therapeutically targetable such as this is therefore clearly attractive and warrants further investigation.
Methods
This research study was approved by the Peter MacCallum Cancer Centre Human Research Ethics Committee (15/84).
Patient cohorts
ICGC discovery cohort
Copy number from WGS, bulk RNA sequencing (RNAseq), methylation arrays and clinical data from 79 primary HGSC samples from the ICGC dataset, which are described in Patch et al.24, were utilised.
Single nuclei RNAseq was performed on 15 of the snap frozen primary tumour samples that were part of the ICGC study, described further below. Patients had previously given written informed consent through the Australian Ovarian Cancer Study (AOCS), approved by the Peter MacCallum Cancer Centre HREC (01/60). The samples were chosen based on the WGD timing determined from the WGS, the availability of tissue and tumour cellularity. All participants in this study were female, and participants in AOCS were not provided with compensation.
TCGA validation cohort
TCGA data used in this paper, generated by the TCGA Research Network53, was downloaded using the R package TCGAbiolinks (RRID:SCR_017683) v2.20.0 for RNA and copy number data, and v2.31.2 for Illumina Infinium HumanMethylation27 array data. ABSOLUTE purity estimates were downloaded directly from supplementary information from Aran et al., and copy number signatures from Steele et al.54,55.
Bulk RNAseq analysis
HTseq values from both cohorts were processed using edgeR (RRID:SCR_012802) v3.34.0 to generate trimmed mean of M values (TMM)56,57. Limma::voom (RRID:SCR_010943) v3.50.358 was used to generate normalised and log-transformed values for input into differential gene expression.
Copy number and whole genome duplication analysis
Tumour purity and copy number log ratio were inferred from the ICGC WGS data by FACETS25. Whole genome duplication (WGD), defined by percentage of the autosomal genome with a major copy number of 2 or more, was calculated as per the method described by Bielski et al.1. The median tumour purity was 62% and 68.7% in those with and without WGD respectively, however we noted that cases excluded by our purity threshold of 0.3 were preferentially those without WGD. It is possible that this may therefore result in a proportionally higher frequency of WGD in our cohort, but does not bias the classification or analysis itself. Both copy number and RNAseq data had been aligned to reference genome GRCh37 for ICGC. TCGA harmonised GRCh38 data was downloaded as using TCGAbiolinks v2.20.0. and gene expression annotated to GRCh38. Timing of WGD was inferred using the method described by Dewhurst et al.36.
Differential gene expression analysis
Covariates
Gene expression can be affected by a number of technical factors, which should reasonably be considered in RNAseq analysis3. Technical factors, library preparation batch and sequencing run were considered as potential effects however these contributed little to bias and were not included. Accounting for copy number was particularly important, because, by definition, the genome-doubled samples were expected to have on average higher copy number and therefore gene expression, and this was done using the copy number log ratio.
Homologous recombination (HR) status can be quantified in a number of ways: HR gene annotation (BRCA1/2 annotation of somatic and germline variants), COSMIC SBS signature 3, HRDsum, Classifier of Homologous Recombination Deficiency (CHORD) and copy number signature 17 (associated with HRD)55,59–61. Having tested models encompassing each of these classifiers on a subset of genes spanning all chromosomes for efficient comparison, all models were found to fit better with a HR covariate than without, and there was little difference between Akaike Information Criterion (AIC) and F statistics between models. The model was therefore run with copy number signature 17, as the HR-deficiency covariate as complete information was available for both datasets.
Model
In order to account for copy number in the DGE analysis, which is a per-gene and per-sample value, standard tools such as edgeR or limma::voom could not be used for DGE analysis. Therefore, a GLM was used, using HR status, copy number at that gene segment and tumour purity as covariates, with a gaussian distribution, using the R packages foreach v1.5.2 and doParallel v1.0.1762 in the format:
P values were adjusted for multiple hypothesis testing using the Benjami–Hochberg method. The coefficient estimate was used as the measure of magnitude of effect.
Because the models were run iteratively per gene, rather than as one, diagnostics could not be applied to the entire model. As an alternative, three genes were randomly picked (genes falling at tertiles) and their individual models assessed using DHARMa63. Model fit was assessed using DHARMa (RRID:SCR_022136) v0.4.5, specifically assessing for Kolmogorov-Smirnov goodness-of-fit test, outliers and dispersion.
Pathway analysis
ActivePathways v1.1.1, which detects overrepresentation of genes using a ranked hypergeometric test, was used for pathway analysis, due to its advantage of being able to integrate a discovery and validation dataset35. A coefficient estimate of >±1 was used for the ICGC dataset, but a less stringent threshold of ±0.5 for the TCGA dataset, to enable inclusion of a sufficient number of genes.
CIBERSORTx
The CIBERSORTx web-based pipeline (RRID:SCR_016955) was previously used to infer immune cell estimations from RNA sequencing, described in Burdett et al.6,64. Briefly, this was performed with batch correction enabled, B-mode, quantile normalisation was disabled, absolute mode and 500 permutations, and the LM22 signature matrix was employed for immune cell deconvolution. No further processing was performed.
Methylation data
Methylation array data was generated in our previous work6,24. This included all 79 cases described here and no further processing was done6. Probes corresponding to promoter regions were identified as per our previous work, assessing for probes within 2000bp of the transcription start site and an inverse spearman correlation of ≤−0.3. Beta values of ≥0.8 were considered to be hypermethylated.
Single nuclei RNA sequencing
RNA pre-processing
Single nuclei were isolated from snap frozen tumour samples using the protocol established by Martelotto et al.65, with minor modification as summarised: snap frozen samples were sectioned at 100 μm and chilled salty EZ lysis buffer (supplemented with RNase inhibitor) was added. The samples were homogenised using a douncer then filtered using a 70 μm strainer mesh, to remove the undigested and fatty tissues. The nuclei were then centrifuged at 500 × g for 5 min at 4 °C. To clean up the nuclei suspension, gradient solution was used and centrifuged 3200 × g, for 20 min at 4 °C. The nuclei were washed in Wash Buffer 2 (10 mM Tris-HCl pH 7.5, 10 mM NaCl, 3 mM MgCl2, 1% BSA, 0.2–1 U/uL Protector RNAse Inhibitor (Roche; cat# 3335399001) and passed through 40 μm strainer mesh. The nuclei were resuspended in Wash Buffer 1 (1× PBS, 1% BSA, 0.2–1 U/μL Protector RNAse Inhibitor).
The 10× Chromium platform was used to generate single nuclei RNAseq (snRNAseq) libraries using the 10x Genomics single cells 3‘ reagent kit v3.1 (cat# 1000123). Libraries were sequenced on the Illumina NovaSeq6000 (paired end 150 bp reads, 40,000 reads per cell).
Data and processing
snRNAseq data for 14 samples was aligned to the reference genome GRCh38 using CellRanger (RRID:SCR_023221)66. Seurat (RRID:SCR_016341) v4.1.1 was used to process, scale and normalise the data, with default filters (min.cells = 3, min.features = 200). More advanced filtering removed low quality cells, multiplets, dead cells and those with a high mitochondrial RNA content (filtered to <15%).
Further transformation and downstream analyses were performed using Seurat v4.3.0.1. Threshold based filtering was applied, to remove the most extreme (and improbable) values, so that Seurat nFeature and nCount parameters more than ±2.5 standard deviations from the mean were excluded.
Data was then processed using SCTransform on individual samples, scaled and then batch-corrected using Harmony (RRID:SCR_022206) v0.1.067,68. Correction factors used were processing batch and sequencing run. Seurat was also used to run UMAP, with 25 dimensions.
Cell annotation, copy number variation and cell-cell communication
Choice of cell annotation methods may have a strong impact on results and subsequent conclusions. A consensus method was therefore used: first, ScType was used with two separate datasets chosen for their respective strengths. The internally curated set of immune markers within ScType performed well to annotate non-cancer cells, and the markers relevant to an ovarian cancer context identified by69. performed well to identify cancer cells and provide further weight to in-built ScType annotations. Independently, expression of marker genes for both cancer and non-malignant cell types (such as EPCAM, PAX8, MUC16, WT1 for cancer cells and COL1A1 for fibroblasts) were examined per cluster to assess the fidelity of these calls. A consensus based on the 3 annotations was then taken.
Cells were further classified using predictions of whether the cells were diploid or aneuploid using an integrative Bayesian segmentation approach via CopyKAT (RRID:SCR_024512)70. Specifically, cell clusters annotated as cancer or non-malignant cells were assessed for the proportion of cells predicted to be aneuploid or diploid, with cells classified as ‘not defined’ excluded. Cancer cells were then reprocessed, using the NormalizeData function with Seurat, since we found that SCTransform is valuable for cell type inference but yields data which has a continuous yet binned structure which is difficult for downstream statistical analyses on gene expression. Data was then batch-corrected for processing and sequencing batch with Harmony and UMAP rerun with 18 dimensions.
CellChat (RRID:SCR_021946) was used to analyse ligand-receptor pairs and predict incoming and outgoing signals between cell subsets43.
Statistics
All analysis and statistics were performed in RStudio (RRID:SCR_000432, v4.1.0). The type of numeric statistical tests used are indicated in text. Analyses were run with ggpubr (RRID:SCR_021139, v0.4.0) for data which did not include multiple samples/cells from the same patient. All comparisons of means are two-sided. For statistical analysis of gene expression in cancer cells in snRNAseq data, a generalised linear mixed model with the ‘tweedie’ distribution was used71,72.
Mixed models were conducted using glmmTMB (v1.1.3) and fit assessed with DHARMa (v0.4.5). Categorical tests were run using Chi square test (stats v4.1.0). To address the issue of sparse matrices, correlations on snRNAseq were performed with CS-CORE73 (v1.0.1).
The threshold for statistical significance across all analyses was p < 0.05. For CellChat, the default number of permutations (M = 100) was used, with a p value of <0.05 considered significant. CellChat internally uses bonferonni correction for multiple testing correction for differential interaction analysis. The final p values are not corrected again after the permutation as per the authors’ documentation.
All other multiple testing corrections were performed using Benjamini–Hochberg method. Joint p values from glmms were calculated using emmeans package (v1.7.5).
Immunohistochemistry
Immunohistochemistry (IHC) was performed using the anti-HLA DR + DP + DQ antibody [clone CR3/43] (Abcam Cat# ab7856 lot# GR3434335-1; RRID:AB_306142). Following optimization on ovarian tumour tissue and non-malignant tonsil sections, the IHC was performed on 2 tissue microarrays (TMAs) comprising two cores per primary tumour from 82 patients from the ICGC study.
TMAs were incubated at 56 °C for 30 min to deparaffinize them. Slides were dewaxed in histolene, then passed through 100% ethanol, and then passed through 70% ethanol for 1 min, and finally deionized water for 5 min. Slides were transferred to a pressure cooker to undergo heat-mediated antigen retrieval, by heating to 125 °C for 3 min in sodium citrate buffer (pH 6.0). Slides were then washed in deionized water. Endogenous peroxidase activity was quenched by submerging slides in 3% hydrogen peroxide and deionized water. Slides were rinsed in Tris-buffered saline with 0.1% Tween 20 detergent (TBST), then blocked using 1X Antibody Diluent/Block (Akoya Biosciences, ARD1001) for 5 min at room temperature. The primary antibody was used at a dilution of 1:150. 100 µL of the prepared dilution was added to each slide and incubated for 60 min at room temperature. Slides were then washed three times for 2 min in TBST. Slides were then incubated for 30 min with the secondary antibody (Anti-Mouse Immunoglobulin Anti-HLA, Vector Laboratories, catalogue number MP-7401-15), then rinsed three times for 2 min with TBST at room temperature. Next, slides were incubated in chromagen substrate solution (25 µL/1 drop 3,3’-Diaminobenzidine (DAB) (Agilent, K3467) with 1 mL substrate K3468), until desired stain intensity developed, at <1 min. Slides were rinsed in deionized water and counterstained with haematoxylin.
Reporting of slides was performed by an external pathologist trained in gynaecological oncology, with scoring parameters summarised in Table 1.
Table 1.
Immunohistochemistry scoring
| Parameter | Options |
|---|---|
| Cell type stained |
Stromal lymphocytes (L) Tumour infiltrating lymphocytes (TIL) Tumour cells (T) |
| Intensity | Positive: 1–3+ |
| Percentage of assessed cells staining | Numerical percentage |
Each tumour sample was represented on a TMA in duplicate; after staining only 45 of the cases had 2 cores (one had been sampled twice resulting in 46 pairs, with a total of 109 cores).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Source data
Acknowledgements
We acknowledge the statistical input of Madawa Jayawardana with regard to complex model fitting. We thank Peter MacCallum Cancer Centre Molecular Genomics Core facility, supported by the Australian Cancer Research Foundation. The Australian Ovarian Cancer Study (AOCS) acknowledges the cooperation of the participating institutions in Australia and acknowledges the contribution of the study nurses, research assistants and all clinical and scientific collaborators to the study. The complete AOCS Study Group can be found at www.aocstudy.org. We would like to thank all of the women who participated in these research programs. This research was financially supported by grants from Department of Health and Human Services through the National Health and Medical Research Council of Australia (NHMRC, APP1189939 to N.L.B., APP1161198 to D.D.L.B. and E.L.C.) and the Victorian Cancer Agency (VCA MCRF21004 to E.L.C.). The AOCS Group was supported by the U.S. Army Medical Research and Materiel Command under DAMD17-01-1-0729, The Cancer Council Victoria, Queensland Cancer Fund, The Cancer Council New South Wales, The Cancer Council South Australia, The Cancer Council Tasmania and The Cancer Foundation of Western Australia (Multi-State Applications 191, 211 and 182) and NHMRC (ID199600; ID400413 and ID400281). The Australian Ovarian Cancer Study gratefully acknowledges additional support from Ovarian Cancer Australia and the Peter MacCallum Cancer Foundation. Figure 1a was created with BioRender.com released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license.
Author contributions
Using CRediT (Contribution Roles Taxonomy) N.L.B.—conceptualization, formal analysis, investigation, software, visualization, writing original draft, writing—review/editing M.O.W.—investigation, writing—review/editing A.P.—software, formal analysis, writing—review/editing L.T.—software, formal analysis, writing—review/editing S.A.—investigation, writing—review/editing AOCS—data curation, resources, writing—review/editing D.D.L.B.—conceptualization, resources, funding acquisition, writing—review/editing E.L.C.—conceptualization, funding acquisition, supervision, writing original draft, writing—review/editing.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Data availability
All bulk RNAseq, whole genome sequencing and methylation data used in this study has previously been published. The ICGC publicly available data24,74 used in this study are available in the European Genome-Phenome archive under accession code EGAD00001000877. The TCGA publicly available data53 used in this study are available from https://portal.gdc.cancer.gov/. Due to the sensitive nature of these patient datasets, access is subject to approval from the ICGC Data Access Compliance Office (https://docs.icgc.org/download/data-access/). ICGC methylation data sets have been deposited into the Gene Expression Omnibus (GEO; https://www.ncbi.nlm.nih.gov/geo/) under accession code GSE65821, without access restrictions. ICGC gene count level transcriptomic data has been deposited into the GEO under accession code GSE209964. ABSOLUTE purity estimates and copy number signatures were downloaded directly from supplementary information54,55. The snRNAseq raw data generated in this study have been deposited in the European Genome-Phenome archive under the accession code EGAD50000000364. Due to the sensitive nature of these patient datasets, the data is available under restricted access, which can be obtained by contacting DGO@petermac.org. Responses to data requests aim to be provided within two weeks. Access will be granted for appropriate research use, which are in line with the original consent provided through AOCS. Duration of data access once granted is not restricted. Processed data are available in Supplementary Tables. The remaining data are available within the Article, Supplementary Information or Source Data file. Source data are provided with this paper.
Code availability
This study uses existing R packages for all analyses and no novel/custom code was developed. The code to generate figures and GLM has been uploaded to synapse.org at https://www.synapse.org/Synapse:syn52673607 (free Synapse account is required) and is available on request to corresponding author.
Competing interests
D.D.L.B. reports research support grants from Roche-Genentech, AstraZeneca, and personal consulting fees from Exo Therapeutics, none of which are related to this work. E.L.C reports research grant funding from AstraZeneca which is not related to this work. The remaining authors declare no potential conflicts of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Deceased: A Ferrier.
Deceased: A McCartney.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Elizabeth L. Christie, Email: liz.christie@petermac.org
Australian Ovarian Cancer Study Group:
D. Bowtell, G. Chenevix-Trench, A. Green, P. Webb, A. DeFazio, D. Gertig, N. Traficante, S. Fereday, S. Moore, J. Hung, K. Harrap, T. Sadkowsky, N. Pandeya, L. Bowes, L. Galletta, D. Giles, J. Hendley, K. Alsop, B. Alexander, P. Ashover, S. Brown, T. Corrish, L. Green, L. Jackman, K. Ferguson, K. Martin, A. Martyn, B. Ranieri, M. Malt, Y. E. Chiew, A. Stenlake, H. Sullivan, A. Mellon, R. Robertson, T. Vanden Bergh, M. Jones, P. Mackenzie, J. Maidens, K. Nattress, J. White, V. Jayde, P. Mamers, T. Schmidt, H. Shirley, S. Viduka, H. Tran, S. Bilic, L. Glavinas, C. Ball, C. Young, J. Brooks, L. Mileshkin, G. Au-Yeung, K. Phillips, D. Rischin, N. Burdett, R. Delahunty, E. Christie, D. Garsed, S. Fox, D. Johnson, S. Lade, M. Loughrey, N. O’Callaghan, W. Murray, D. Purdie, D. Whiteman, A. Proietto, S. Braye, G. Otton, C. Camaris, R. Crouch, L. Edwards, N. Hacker, D. Marsden, G. Robertson, D. Bell, S. Baron-Hay, A. Ferrier, G. Gard, D. Nevell, N. Pavlakis, S. Valmadre, B. Young, P. Beale, J. Beith, J. Carter, C. Dalrymple, R. Houghton, P. Russell, M. Davy, M. K. Oehler, C. Hall, T. Dodd, P. Blomfield, D. Challis, R. McIntosh, A. Parker, D. Healy, T. Jobling, T. Manolitsas, J. McNealage, P. Rogers, B. Susil, E. Sumithran, I. Simpson, N. Zeps, I. Hammond, Y. Leung, A. McCartney, R. Stuart-Harris, F. Kirsten, J. Rutovitz, P. Clingan, J. Shannon, T. Bonaventura, J. Stewart, S. Begbie, A. Glasgow, M. Friedlander, M. Links, J. Grygiel, J. Hill, A. Brand, K. Byth, P. Harnett, G. Wain, R. Jaworski, R. Sharma, B. Ward, D. Papadimos, A. Crandon, M. Cummings, K. Horwood, A. Obermair, L. Perrin, D. Wyld, J. Nicklin, T. Healy, K. Pittman, D. Henderson, J. Miller, J. Pierdes, B. Brown, R. Rome, D. Allen, P. Grant, S. Hyde, R. Laurie, M. Robbie, P. Waring, V. Billson, J. Pyman, D. Neesham, M. Quinn, C. Underhill, R. Bell, L. F. Ng, R. Blum, V. Ganju, M. Buck, and I. Haviv
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-024-50137-y.
References
- 1.Bielski CM, et al. Genome doubling shapes the evolution and prognosis of advanced cancers. Nat. Genet. 2018;50:1189–1195. doi: 10.1038/s41588-018-0165-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gerstung M, et al. The evolutionary history of 2,658 cancers. Nature. 2020;578:122–128. doi: 10.1038/s41586-019-1907-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quinton RJ, et al. Whole-genome doubling confers unique genetic vulnerabilities on tumour cells. Nature. 2021;590:492–497. doi: 10.1038/s41586-020-03133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Priestley P, et al. Pan-cancer whole-genome analyses of metastatic solid tumours. Nature. 2019;575:210–216. doi: 10.1038/s41586-019-1689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carter SL, et al. Absolute quantification of somatic DNA alterations in human cancer. Nat. Biotechnol. 2012;30:413–421. doi: 10.1038/nbt.2203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burdett NL, et al. Multiomic analysis of homologous recombination-deficient end-stage high-grade serous ovarian cancer. Nat. Genet. 2023;55:437–450. doi: 10.1038/s41588-023-01320-2. [DOI] [PubMed] [Google Scholar]
- 7.Etemadmoghadam D, et al. Resistance to CDK2 Inhibitors Is Associated with Selection of Polyploid Cells in CCNE1-Amplified Ovarian CancerResistance to CDK2 Inhibitors in CCNE1-Amplified Cancer. Clin. Cancer Res. 2013;19:5960–5971. doi: 10.1158/1078-0432.CCR-13-1337. [DOI] [PubMed] [Google Scholar]
- 8.Zeng J, Hills SA, Ozono E, Diffley JF. Cyclin E-induced replicative stress drives p53-dependent whole-genome duplication. Cell. 2023;186:528–542.e14. doi: 10.1016/j.cell.2022.12.036. [DOI] [PubMed] [Google Scholar]
- 9.Berenjeno IM, et al. Oncogenic PIK3CA induces centrosome amplification and tolerance to genome doubling. Nat. Commun. 2017;8:1–15. doi: 10.1038/s41467-017-02002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martínez-Jiménez, F., et al. Genetic immune escape landscape in primary and metastatic cancer. Nat. Genet.55, 820–831 (2023). [DOI] [PMC free article] [PubMed]
- 11.Health AIo, Welfare. Cancer data in Australia. (AIHW, 2023).
- 12.Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. Ca Cancer J. Clin. 2023;73:17–48. doi: 10.3322/caac.21763. [DOI] [PubMed] [Google Scholar]
- 13.Cancer Survival in England, cancers diagnosed 2015 to 2019, followed up to 2020. NHS Digital. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/cancer-survival-in-england/cancers-diagnosed-2015-to-2019-followed-up-to-2020#summary (2022).
- 14.Zhang L, et al. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N. Engl. J. Med. 2003;348:203–213. doi: 10.1056/NEJMoa020177. [DOI] [PubMed] [Google Scholar]
- 15.Disis ML, et al. Efficacy and safety of avelumab for patients with recurrent or refractory ovarian cancer: phase 1b results from the JAVELIN solid tumor trial. JAMA Oncol. 2019;5:393–401. doi: 10.1001/jamaoncol.2018.6258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zamarin D, et al. Randomized phase II trial of nivolumab versus nivolumab and ipilimumab for recurrent or persistent ovarian cancer: an NRG oncology study. J. Clin. Oncol. 2020;38:1814. doi: 10.1200/JCO.19.02059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang AW, et al. Interfaces of malignant and immunologic clonal dynamics in ovarian cancer. Cell. 2018;173:1755–69. e22. doi: 10.1016/j.cell.2018.03.073. [DOI] [PubMed] [Google Scholar]
- 18.Montesion M, et al. Somatic HLA Class I Loss Is a Widespread Mechanism of Immune Evasion Which Refines the Use of Tumor Mutational Burden as a Biomarker of Checkpoint Inhibitor ResponsePan-Cancer Analysis of HLA LOH as a Method of Immune Evasion. Cancer Discov. 2021;11:282–292. doi: 10.1158/2159-8290.CD-20-0672. [DOI] [PubMed] [Google Scholar]
- 19.McGranahan N, et al. Allele-specific HLA loss and immune escape in lung cancer evolution. Cell. 2017;171:1259–71. e11. doi: 10.1016/j.cell.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang, X. Q., et al. Spatial predictors of immunotherapy response in triple-negative breast cancer. Nature621, 868–876 (2023). [DOI] [PMC free article] [PubMed]
- 21.Axelrod ML, Cook RS, Johnson DB, Balko JM. Biological Consequences of MHC-II Expression by Tumor Cells in CancerBiological Consequences of MHC-II Expression by Tumor Cells. Clin. Cancer Res. 2019;25:2392–2402. doi: 10.1158/1078-0432.CCR-18-3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson DB, et al. Melanoma-specific MHC-II expression represents a tumour-autonomous phenotype and predicts response to anti-PD-1/PD-L1 therapy. Nat. Commun. 2016;7:1–10. doi: 10.1038/ncomms10582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davoli T, Uno H, Wooten EC, Elledge SJ. Tumor aneuploidy correlates with markers of immune evasion and with reduced response to immunotherapy. Science. 2017;355:eaaf8399. doi: 10.1126/science.aaf8399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patch A-M, et al. Whole–genome characterization of chemoresistant ovarian cancer. Nature. 2015;521:489–494. doi: 10.1038/nature14410. [DOI] [PubMed] [Google Scholar]
- 25.Shen R, Seshan VE. FACETS: allele-specific copy number and clonal heterogeneity analysis tool for high-throughput DNA sequencing. Nucleic Acids Res. 2016;44:e131. doi: 10.1093/nar/gkw520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steimle V, Siegrist C-A, Mottet A, Lisowska-Grospierre B, Mach B. Regulation of MHC class II expression by interferon-γ mediated by the transactivator gene CIITA. Science. 1994;265:106–109. doi: 10.1126/science.8016643. [DOI] [PubMed] [Google Scholar]
- 27.Johnson DB, et al. Tumor-specific MHC-II expression drives a unique pattern of resistance to immunotherapy via LAG-3/FCRL6 engagement. JCI insight. 2018;3:e120360. doi: 10.1172/jci.insight.120360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson AM, et al. Cancer cell–intrinsic expression of MHC Class II regulates the immune microenvironment and response to Anti–PD-1 therapy in lung adenocarcinoma. J. Immunol. 2020;204:2295–2307. doi: 10.4049/jimmunol.1900778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Callahan MJ, et al. Increased HLA-DMB expression in the tumor epithelium is associated with increased CTL infiltration and improved prognosis in advanced-stage serous ovarian cancer. Clin. Cancer Res. 2008;14:7667–7673. doi: 10.1158/1078-0432.CCR-08-0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muhlethaler-Mottet A, Otten LA, Steimle V, Mach B. Expression of MHC class II molecules in different cellular and functional compartments is controlled by differential usage of multiple promoters of the transactivator CIITA. EMBO J. 1997;16:2851–2860. doi: 10.1093/emboj/16.10.2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pennini ME, Pai RK, Schultz DC, Boom WH, Harding CV. Mycobacterium tuberculosis 19-kDa lipoprotein inhibits IFN-γ-induced chromatin remodeling of MHC2TA by TLR2 and MAPK signaling. J. Immunol. 2006;176:4323–4330. doi: 10.4049/jimmunol.176.7.4323. [DOI] [PubMed] [Google Scholar]
- 32.Waldburger J-M, Suter T, Fontana A, Acha-Orbea H, Reith W. Selective abrogation of major histocompatibility complex class II expression on extrahematopoietic cells in mice lacking promoter IV of the class II transactivator gene. J. Exp. Med. 2001;194:393–406. doi: 10.1084/jem.194.4.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chan KL, et al. Inhibition of the CtBP complex and FBXO11 enhances MHC class II expression and anti-cancer immune responses. Cancer Cell. 2022;40:1190–206. e9. doi: 10.1016/j.ccell.2022.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chang C-H, Fontes JD, Peterlin M, Flavell RA. Class II transactivator (CIITA) is sufficient for the inducible expression of major histocompatibility complex class II genes. J. Exp. Med. 1994;180:1367–1374. doi: 10.1084/jem.180.4.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paczkowska M, et al. Integrative pathway enrichment analysis of multivariate omics data. Nat. Commun. 2020;11:1–16. doi: 10.1038/s41467-019-13983-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dewhurst SM, et al. Tolerance of whole-genome doubling propagates chromosomal instability and accelerates cancer genome evolution. Cancer Discov. 2014;4:175–185. doi: 10.1158/2159-8290.CD-13-0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tothill RW, et al. Novel molecular subtypes of serous and endometrioid ovarian cancer linked to clinical outcome. Clin. Cancer Res. 2008;14:5198–5208. doi: 10.1158/1078-0432.CCR-08-0196. [DOI] [PubMed] [Google Scholar]
- 38.Chen GM, et al. Consensus on molecular subtypes of high-grade serous ovarian carcinoma. Clin. Cancer Res. 2018;24:5037–5047. doi: 10.1158/1078-0432.CCR-18-0784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Helland Å, et al. Deregulation of MYCN, LIN28B and LET7 in a molecular subtype of aggressive high-grade serous ovarian cancers. PloS One. 2011;6:e18064. doi: 10.1371/journal.pone.0018064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Turner TB, et al. Epigenetic modifiers upregulate MHC II and impede ovarian cancer tumor growth. Oncotarget. 2017;8:44159. doi: 10.18632/oncotarget.17395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roemer MG, et al. Major histocompatibility complex class II and programmed death ligand 1 expression predict outcome after programmed death 1 blockade in classic Hodgkin lymphoma. J. Clin. Oncol. 2018;36:942. doi: 10.1200/JCO.2017.77.3994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ianevski A, Giri AK, Aittokallio T. Fully-automated and ultra-fast cell-type identification using specific marker combinations from single-cell transcriptomic data. Nat. Commun. 2022;13:1246. doi: 10.1038/s41467-022-28803-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jin S, et al. Inference and analysis of cell-cell communication using CellChat. Nat. Commun. 2021;12:1088. doi: 10.1038/s41467-021-21246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cheng Z, et al. The genomic landscape of early-stage ovarian high grade serous carcinoma. Clin. Cancer Res. 2022;28:2911–2922. doi: 10.1158/1078-0432.CCR-21-1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu C-H, et al. Differential whole-genome doubling and homologous recombination deficiencies across breast cancer subtypes from the Taiwanese population. Commun. Biol. 2021;4:1–12. doi: 10.1038/s42003-021-02597-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.López S, et al. Interplay between whole-genome doubling and the accumulation of deleterious alterations in cancer evolution. Nat. Genet. 2020;52:283–293. doi: 10.1038/s41588-020-0584-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang XP, et al. Class II transactivator knockdown limits major histocompatibility complex II expression, diminishes immune rejection, and improves survival of allogeneic bone marrow stem cells in the infarcted heart. FASEB J. 2016;30:3069–3082. doi: 10.1096/fj.201600331R. [DOI] [PubMed] [Google Scholar]
- 48.Chen B, et al. Predicting HLA class II antigen presentation through integrated deep learning. Nat. Biotechnol. 2019;37:1332–1343. doi: 10.1038/s41587-019-0280-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gonzalez-Ericsson PI, et al. Tumor-specific major histocompatibility-II expression predicts benefit to anti–PD-1/L1 therapy in patients with HER2-negative primary breast cancer. Clin. Cancer Res. 2021;27:5299–5306. doi: 10.1158/1078-0432.CCR-21-0607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Uboha, N. V., et al. Phase II study of spartalizumab (PDR001) and LAG525 in advanced solid tumors and hematologic malignancies. Am. Soc. Clin. Oncol. 37, 2553–2553 (2019).
- 51.Kozłowski M, Borzyszkowska D, Cymbaluk-Płoska A. The Role of TIM-3 and LAG-3 in the Microenvironment and Immunotherapy of Ovarian Cancer. Biomedicines. 2022;10:2826. doi: 10.3390/biomedicines10112826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cycon KA, Mulvaney K, Rimsza LM, Persky D, Murphy SP. Histone deacetylase inhibitors activate CIITA and MHC class II antigen expression in diffuse large B‐cell lymphoma. Immunology. 2013;140:259–272. doi: 10.1111/imm.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.TCGAR Network WeinsteinJ, Collisson EA, et al. “The cancer genome atlas pan-cancer analysis project,”. Nat. Genet. 2013;45:1113–1120. doi: 10.1038/ng.2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aran D, Sirota M, Butte AJ. Systematic pan-cancer analysis of tumour purity. Nat. Commun. 2015;6:1–12. doi: 10.1038/ncomms9971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Steele CD, et al. Signatures of copy number alterations in human cancer. Nature. 2022;606:984–991. doi: 10.1038/s41586-022-04738-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Robinson MD, McCarthy DJ, Smyth GK. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. 2010;26:139–140. doi: 10.1093/bioinformatics/btp616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Robinson MD, Oshlack A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol. 2010;11:1–9. doi: 10.1186/gb-2010-11-3-r25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Law CW, Chen Y, Shi W, Smyth GK. voom: Precision weights unlock linear model analysis tools for RNA-seq read counts. Genome Biol. 2014;15:1–17. doi: 10.1186/gb-2014-15-2-r29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alexandrov LB, et al. The repertoire of mutational signatures in human cancer. Nature. 2020;578:94–101. doi: 10.1038/s41586-020-1943-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Telli ML, et al. Homologous Recombination Deficiency (HRD) Score Predicts Response to Platinum-Containing Neoadjuvant Chemotherapy in Patients with Triple-Negative Breast CancerHRD Predicts Response to Platinum Therapy in TNBC. Clin. Cancer Res. 2016;22:3764–3773. doi: 10.1158/1078-0432.CCR-15-2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nguyen, L., Martens, J., Van Hoeck, A., Cuppen, E. Pan-cancer landscape of homologous recombination deficiency. Nat. Commun.11, 5584 (2020). [DOI] [PMC free article] [PubMed]
- 62.Weston, S., Calaway, R. Getting Started with doParallel and foreach. Available on https://cran.r-project.org/web/packages/doParallel/vignettes/gettingstartedParallel.pdf (2015).
- 63.Hartig F. DHARMa: residual diagnostics for hierarchical (multi-level/mixed) regression models. R package version 0.4.5. https://CRAN.R-project.org/package=DHARMa (2022)
- 64.Newman AM, et al. Determining cell type abundance and expression from bulk tissues with digital cytometry. Nat. Biotechnol. 2019;37:773–782. doi: 10.1038/s41587-019-0114-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martelotto, L. G. Protocol for nuclei isolation from fresh and frozen tissues using Salty-Ez10 or Salty-Ez50 buffer: compatible with snRNA-Seq and Multiome workflows from 10x Genomics doi.org/10.17504/protocols.io.bx64prgw (2021).
- 66.Zheng GX, et al. Massively parallel digital transcriptional profiling of single cells. Nat. Commun. 2017;8:14049. doi: 10.1038/ncomms14049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Korsunsky I, et al. Fast, sensitive and accurate integration of single-cell data with Harmony. Nat. Methods. 2019;16:1289–1296. doi: 10.1038/s41592-019-0619-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tran HTN, et al. A benchmark of batch-effect correction methods for single-cell RNA sequencing data. Genome Biol. 2020;21:1–32. doi: 10.1186/s13059-019-1850-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vázquez-García, I. et al. Ovarian cancer mutational processes drive site-specific immune evasion. Nature612, 778–786 (2022). [DOI] [PMC free article] [PubMed]
- 70.Gao R, et al. Delineating copy number and clonal substructure in human tumors from single-cell transcriptomes. Nat. Biotechnol. 2021;39:599–608. doi: 10.1038/s41587-020-00795-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brooks ME, et al. glmmTMB balances speed and flexibility among packages for zero-inflated generalized linear mixed modeling. R. J. 2017;9:378–400. doi: 10.32614/RJ-2017-066. [DOI] [Google Scholar]
- 72.Dunn, P. K., Smyth, G. K. Generalized Linear Models With Examples in R (Springer, 2018).
- 73.Su CXZ, Shan X, Cai B, Zhao H, Zhang J. Cell-type-specific co-expression inference from single cell RNA-sequencing data. Nat. Commun. 2023;14:4846. doi: 10.1038/s41467-023-40503-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Consortium ICG. International network of cancer genome projects. Nature. 2010;464:993–998. doi: 10.1038/nature08987. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
All bulk RNAseq, whole genome sequencing and methylation data used in this study has previously been published. The ICGC publicly available data24,74 used in this study are available in the European Genome-Phenome archive under accession code EGAD00001000877. The TCGA publicly available data53 used in this study are available from https://portal.gdc.cancer.gov/. Due to the sensitive nature of these patient datasets, access is subject to approval from the ICGC Data Access Compliance Office (https://docs.icgc.org/download/data-access/). ICGC methylation data sets have been deposited into the Gene Expression Omnibus (GEO; https://www.ncbi.nlm.nih.gov/geo/) under accession code GSE65821, without access restrictions. ICGC gene count level transcriptomic data has been deposited into the GEO under accession code GSE209964. ABSOLUTE purity estimates and copy number signatures were downloaded directly from supplementary information54,55. The snRNAseq raw data generated in this study have been deposited in the European Genome-Phenome archive under the accession code EGAD50000000364. Due to the sensitive nature of these patient datasets, the data is available under restricted access, which can be obtained by contacting DGO@petermac.org. Responses to data requests aim to be provided within two weeks. Access will be granted for appropriate research use, which are in line with the original consent provided through AOCS. Duration of data access once granted is not restricted. Processed data are available in Supplementary Tables. The remaining data are available within the Article, Supplementary Information or Source Data file. Source data are provided with this paper.
This study uses existing R packages for all analyses and no novel/custom code was developed. The code to generate figures and GLM has been uploaded to synapse.org at https://www.synapse.org/Synapse:syn52673607 (free Synapse account is required) and is available on request to corresponding author.