Abstract
Introduction
E-cigarette and cannabis use by adolescents are risk factors for smoking initiation. We hypothesised that increasingly common dual use of e-cigarette and cannabis in adolescence leads to more frequent cigarette smoking in young adulthood.
Methods
Data are from a prospective cohort study in Southern California, where 1164 participants who ever used nicotine products in their lifetime completed surveys in 12th grade (T1:2016), and at 24-month (T2) and 42-month (T3) follow-ups. Past 30-day use (number of days: range=0–30) of cigarettes, e-cigarettes and cannabis, and nicotine dependence, were assessed in each survey. Nicotine dependence for cigarettes and e-cigarettes was assessed using original and modified (for e-cigarette) Hooked on Nicotine Checklists (number of dependent products: range=0–2). Path analysis examined the mediation process via nicotine dependence linking baseline e-cigarette and cannabis use to subsequent increased cigarette use.
Results
Baseline exclusive use of e-cigarettes (baseline prevalence, 2.5%) was associated with 2.61-fold increase in frequency of smoking days at T3 (95% CI 1.04 to 13.1), exclusive cannabis use (26.0%) with 2.58-fold increase (95% CI 1.43 to 4.98), and dual use (7.4%) with 5.84-fold increase (95% CI 3.16 to 12.81), compared with baseline non-users. Nicotine dependence at T2 mediated 10.5% (95% CI 6.3 to 14.7) and 23.2% (95% CI 9.6 to 36.3) of the association of cannabis and dual use, respectively, with increased smoking at T3.
Discussion
Adolescent e-cigarette and cannabis use was associated with more frequent smoking during young adulthood, with larger effects of dual use. Associations were partially mediated through nicotine dependence. Dual use of cannabis and e-cigarettes may contribute to the development of nicotine dependence and increased use of combustible cigarettes.
INTRODUCTION
Cigarette smoking among high school students has declined for several decades in the USA. However, a new pattern of nicotine and cannabis use related behaviour characterised by high prevalence of e-cigarette vaping and cannabis use has emerged among adolescents and young adults over the last two decades.1–3 The annual prevalence of cannabis use among 12th graders declined in the USA from a peak in 1979 (prevalence rate:51%) until 1992 (prevalence rate:22%). Since then the annual prevalence of cannabis use increased to 35.9% in 2018.1 This increase in cannabis use co-occurred with increases in e-cigarette use in the USA. According to the 2019 Youth Risk Behavior Survey (YRBS), the prevalence of past 30-day use of e-cigarettes, cannabis and cigarettes was 33%, 22% and 6%, respectively, among 9th–12th graders.4 The prevalence of past 30-day exclusive use of e-cigarettes and cannabis was 14% and 4%, respectively, and the prevalence of dual use of e-cigarettes and cannabis was 13%. The high prevalence of e-cigarette and cannabis dual use among high school children is concerning given the well-established relationship between cannabis and smoking.5 Cannabis use has been associated with smoking initiation among non-smokers and with difficulty in quitting among smokers,6 effects that might be due to cannabis-facilitated nicotine dependence.5
There is a large body of evidence that e-cigarette use is also associated with subsequent use of combustible cigarettes.7 In a meta-analysis, Yoong et al identified 25 studies through systematic review, 13 of which were from the USA. The adjusted pooled risk ratio of the 17 studies investigating the relationship between ever use of e-cigarettes and subsequent ever use of combustible cigarettes was 3.01 (95% CI 2.37 to 3.82). Six studies investigated the association between ever use of e-cigarettes ‘at baseline’ and subsequent ‘current’ (past 30-day) use of combustible cigarettes; the pooled adjusted risk ratio was 2.56 (95% CI 1.61 to 4.07). The progression from e-cigarette use to smoking potentially can be explained by two major possible pathways: the intention pathway and the addiction pathway.8 9 A recent study exploring the possible role of intention pathway (e-cigarette use leads to higher intention to smoke) noted that, although ‘intent to smoke’ is a strong risk factor for smoking initiation following e-cigarette use among adolescents,10 it cannot explain the total effect. Their finding suggests that the progression from e-cigarette use to smoking may also involve other pathways, like the ‘addiction pathway’ (e-cigarette leads to nicotine dependence, leading to smoking initiation). E-cigarettes deliver nicotine that is rapidly absorbed and in amounts that can result in nicotine dependence.11 Potential addictiveness of e-cigarette use has been observed in multiple studies.8 9 11 12 A recent study reported that the prevalence of nicotine dependence did not vary between e-cigarette and combustible cigarette users, although urinary cotinine levels were lower among e-cigarette users compared with combustible cigarette users.13
There is a growing body of evidence that e-cigarette-induced nicotine dependence can be potentiated with co-use of cannabis.14 15 At the molecular level, the actions of both nicotine and δ-9-tetrahydrocannabinol (THC), directly or indirectly, involve the dopaminergic pathway15 that is central to reward-seeking and reinforcing behaviour, and to drug use and dependence.16 The simultaneous upregulation and desensitisation of the nicotinic acetylcholine receptors is purported to be related to nicotinic disorder as they modulate both dopaminergic and glutaminergic pathways.17 THC, the main psychoactive ingredient of cannabis, is an agonist of cannabinoid type-1 receptors (CB1Rs) that modulate neurotransmitter release.14 Activation of CB1Rs by THC leads to increased activity of dopaminergic neurons in the mesolimbic region. Besides sharing similar neurobiological pathways with THC, nicotine is known to interact with CB1Rs.18 Furthermore, the cholinergic (nicotine induced) and endocannaboid (cannabis induced) systems are known to interact in reward-related processes.19 In animal studies, selective blocking of CB1R has been shown to diminish the rewarding properties of nicotine.20
Currently little is known regarding the effect of e-cigarette and cannabis dual use by adolescents on smoking behaviour and nicotine dependence in young adulthood. Based on the associations of e-cigarette and cannabis use with smoking progression and on the neurobiology of addiction to nicotine and cannabis, we hypothesised that dual use of e-cigarettes and cannabis among high school adolescents will lead to greater use of cigarettes during young adulthood, and the prospective associations will be mediated through increased level of nicotine dependence (the addiction pathway). We explored our hypothesis in a prospective cohort study of 12th grade students who were followed into young adulthood.
METHODS
Sample and procedure
Participants in this analysis were a subsample (n=1164) of an ongoing prospective cohort study on mental health and health behaviours originally recruited as 9th grade students in 2013 from 10 Southern California high schools (see online supplemental figure S1).21 Paper-and-pencil surveys were administered at baseline on-site at participating high schools, and follow-up surveys were conducted remotely via the internet. Of the 3396 participants in the original cohort, 3168 completed surveys during 12th grade (the baseline survey for this analysis). As we hypothesised that cannabis and e-cigarette use lead to increased cigarette use through nicotine dependence, we restricted the current analysis to the 1164 participants who had ever used any nicotine products (eg, combustible cigarettes, e-cigarettes) at least once in 12th grade or at subsequent surveys. (Only ever nicotine users were asked about nicotine dependence in the study, see online supplemental figure S1.). The study sample included data from participants who completed surveys at baseline (T1; Fall 2016, 12th grade, mean age (SD) = 17.5 (0.4) years) and two follow-ups after high school graduation (T2 (24-month follow-up; October 2018 to October 2019); mean age (SD) = 19.7 (0.4) and T3 (42-month follow-up; May to October 2020); mean age(SD) = 21.2 (0.4)). All participants provided informed consent.
Measures
E-cigarette and cannabis use
At baseline, participants reported past 30-day use of e-cigarettes (with nicotine) and cannabis products using questions derived from validated national survey items.22 23 Cannabis products included ‘(1) combustible cannabis (eg, pot, weed, hash, reefer, or bud); (2) blunts (ie, cannabis rolled in tobacco leaf or cigar casing); (3) electronic device to vape cannabis or hash oil (eg, liquid pot, weed pen) [vaporised cannabis]; (4) cannabis or THC food or drinks (eg, pot brownies, edibles, butter, oil) [edible cannabis]; and (5) dabbing (eg, wax, shatter, budder, butane hash oil /BHO) [cannabis concentrate]’. Both e-cigarette use and cannabis products use variables were dichotomously coded (0=no use; 1=any use), and a dual use status variable was created using these two dichotomous variables (0=no use; 1=any cannabis product use only; 3=e-cigarette use only; and 4=dual use of cannabis products and e-cigarettes).
Combustible cigarette use
Across baseline and follow-up assessments, frequency (ie, number of days) of combustible cigarette use in the past 30 days was assessed by an ordinal item with seven options. These response categories were recoded into quantitative count variables by taking the mean value of each ordinal category (ie, rounding up to the nearest integer) for use in negative binomial regression models as follows: 0 days (0 days), 2 days (1–2 days), 4 days (3–5 days), 8 days (6–9 days), 15 days (10–19 days), 25 days (20–29 days) and 30 days (all 30 days). As an alternative outcome for sensitivity analyses, participants were also asked how many cigarettes, on average, were smoked daily. We also calculated ‘cigarettes used per day’ based on number of cigarettes smoked per smoking day in the last 30 days.
Nicotine dependence
At all time points, tobacco product dependence symptoms were measured using the Hooked on Nicotine Checklist (HONC), a validated self-report measure for use among youth, who commonly have mild dependence.24–26 Students reported whether they had ever experienced each of 10 dependence symptoms for e-cigarettes and for combustible cigarettes. E-cigarette and combustible cigarette dependence items were identically worded, except for substitution of e-cigarette and vaping terms for cigarette and smoking. Endorsing ≥1 symptoms indicated that the participant screened positive for dependence.12 24 A nicotine dependence variable for e-cigarettes and cigarettes was then coded as 0 (neither), 1 (to either product) or 2 (to both products).
Covariates
Past 30-day use of tobacco, cannabis use and other tobacco products (ie, any use of cigars/cigarillos or hookah) at baseline (T1; during high school years), and sociodemographic characteristics including gender, age, race/ethnicity, parental education level, and school free/reduced lunch were treated as covariates in the analysis. Participants’ enrolment in a 4-year college programme, living with parents, and personal and family financial situation were assessed at the first follow-up survey (T2) after (grade 12) high school graduation. Response categories for each covariate are presented in table 1.
Table 1.
Descriptive statistics*
| Variables | Mean (SD)/N (%) |
|---|---|
| Female gender (vs male), N (%) | 655 (56.3) |
| Age, mean (SD), year | 17.49 (0.41) |
| Race/ethnicity, N (%) | |
| Hispanic | 609 (53.6) |
| Asian | 127 (11.2) |
| African American | 46 (4.0) |
| Non-Hispanic white | 191 (16.8) |
| Other† | 163 (14.3) |
| Parents graduated from college, N (%) | 446 (38.3) |
| Free/reduced school lunch, N (%) | 517 (54.0) |
| In 4-year college enrolment, N (%)‡ | 585 (57.4) |
| Live with parents), N (%)‡ | 743 (73.3) |
| Financial situation-self, N (%)‡ | |
| Live comfortable | 429 (42.5) |
| Meet needs with a little left | 266 (26.4) |
| Meet basic expenses | 245 (24.3) |
| Do not meet basic expenses | 69 (6.8) |
| Financial situation-family, N (%)‡ | |
| Live comfortable | 208 (20.6) |
| Meet needs with a little left | 504 (49.8) |
| Meet basic expenses | 172 (17.0) |
| Do not meet basic expenses | 128 (12.6) |
| Cigarette use (past 30 days), N (%) | 101 (8.7) |
| Number of days of cigarette smoking (past 30 days), mean (SD) | 0.73 (3.7) |
| Other tobacco product use (past 30 days), N (%)§ | 68 (5.8) |
| Nicotine dependence, mean (SD) | 0.15 (0.42) |
| Dual use status (past 30 days), N (%) | |
| No use | 745 (64.0) |
| Exclusive cannabis use | 304 (26.1) |
| Exclusive e-cigarette use | 29 (2.5) |
| Dual use | 86 (7.4) |
Analytical sample n=1164.
Other race/ethnicity includes respondents who selected ‘American Indian/Alaska Native’, ‘Native Hawaiian/Pacific Islander’, ‘multi-ethnic/multi-racial’ or ‘other’ options for the forced-choice race/ethnicity question.
Collected from the participants at T2 after high school graduation. All other variables collected at baseline (T1).
Other tobacco products include cigars/cigarillos and hookah.
Statistical analysis
Preliminary analyses involved calculating descriptive statistics for study covariates and combustible cigarette use levels across follow-ups by baseline e-cigarette and cannabis dual use status. We examined a path model to evaluate the total direct effect of past 30-day e-cigarette and cannabis dual use at baseline on past 30-day combustible cigarette use outcome at T3 after controlling for sociodemographic factors, nicotine dependence, cigarette use and other tobacco product use at T1. Using the path analysis, we then tested mediation pathways linking baseline past 30-day e-cigarette and cannabis dual use status to past 30-day combustible cigarette use outcome at T3 via nicotine dependence and combustible cigarette use at T2. Estimates on pathways linking baseline dual use status to mediators (ie, nicotine dependence and number of smoking days at T2) were presented by unstandardised regression coefficients (bs). Also, considering the distribution of the past 30-day combustible cigarette use frequency outcome variable at T3 (ie, non-negative integers showing positive skewness with evidence of overdispersion), negative binomial regression modelling was used.27 The negative binomial regression coefficients (bs) were exponentiated to obtain rate ratios (RRs) with 95% CIs. Indirect effects were tested via bootstrapping, and effect sizes were calculated based on the proportion of indirect effect to the total effect using a protocol of a regression-based model.28
Sensitivity analyses
We restricted the analysis to study participants who were not past 30-day cigarette smokers at T1 (n=1057) to investigate whether the observed associations were similar (online supplemental figure S2). We also assessed whether having excluded participants who reported ‘no lifetime’ use of nicotine products at baseline (n=1439) could have resulted in selection bias; we conducted a sensitivity analysis including all participants who provided valid data at baseline and at least one follow-up (n=2603, online supplemental figure S3). We also assessed whether the key mediational pathways in the primary analysis were also observed in an analysis using an alternative cigarette use outcome, the number of cigarettes smoked per smoking day (online supplemental figure S4).
All analyses were conducted in Mplus V.8.29 As respondents were clustered within schools at baseline, a complex analysis was used to adjust parameter SEs for interdependence in the data (ie, the error terms of regression models were not independent) to avoid an underestimation of SEs. Statistical significance was set at p=0.05 (two-tailed). Full information maximum likelihood estimation was used to account for missing data.
RESULTS
Study population
Among total 3168 high school students who completed the baseline survey, the analytical sample included 1164 participants who were identified as lifetime nicotine product users and provided valid data for key study variables at baseline and at ≥1 follow-ups (online supplemental figure S1). The study population was sociodemographically heterogenous (56.3% female, 53.6% Hispanic, 11.2% Asian, 4.0% black, 16.8% non-Hispanic white), with a mean (SD) age of 17.5 years (0.4) at baseline, 19.7 (0.4) at T2 and 21.2 (0.4) at T3. At T2, the first follow-up time point after high school graduation, 57.4% of the analytical sample was enrolled in a 4-year college programme, and 73.3% of respondents reported living with a parent (table 1). The 1439 who completed the survey at baseline (12th grade) but never used any nicotine products at baseline or at any of the follow ups did not differ from the analytical sample in age (see online supplemental table S1) but were more likely to be Asian and have college graduate parents, and less likely to be Hispanic.
Nicotine and cannabis use
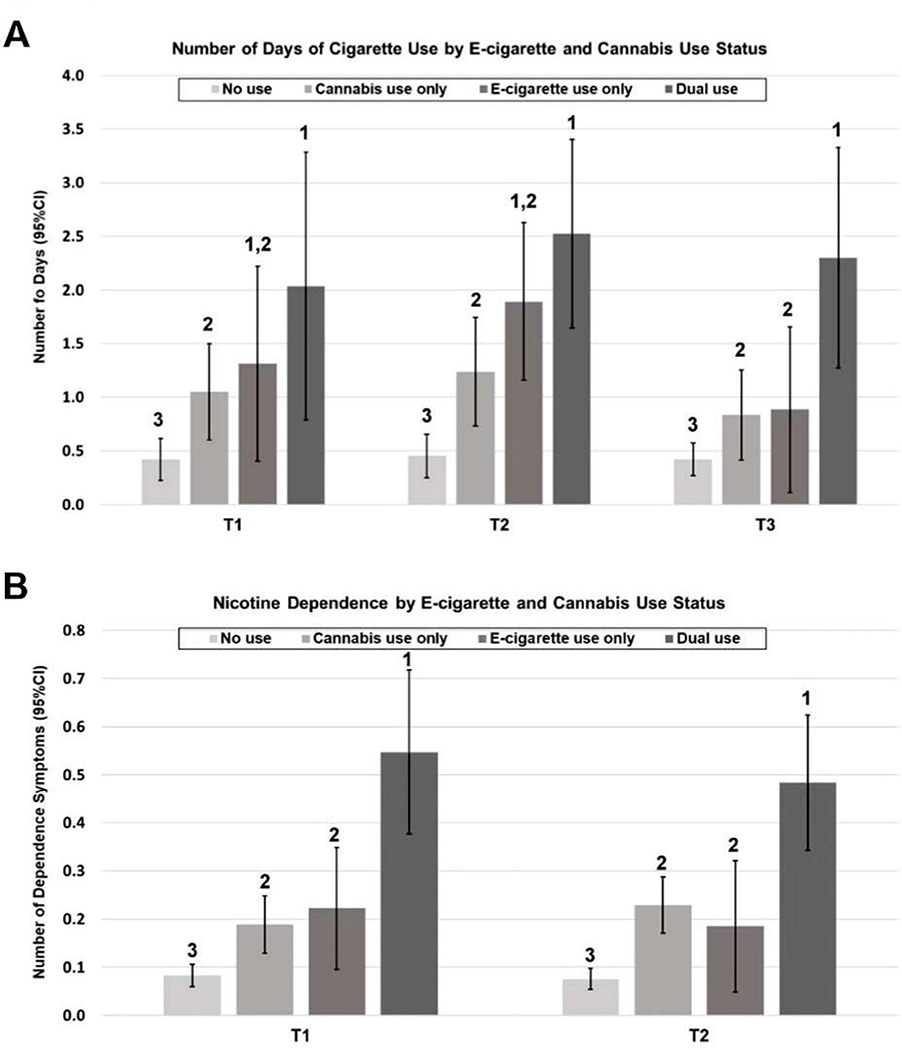
There were 8.7% of study participants who smoked cigarettes int the past 30 days at baseline. The average number of days of cigarette use in the past 30 days was 0.73 (SD=3.7) at T1, 0.85 (SD=3.7) at T2 and 0.66 (SD=2.87) at T3. Among the analytical sample, 26% used cannabis exclusively; only 2.5% used e-cigarettes exclusively; and 7.4% were dual users (used e-cigarettes and cannabis). Among the e-cigarette and cannabis dual users at baseline (T1), the average days of cigarette use were consistent over time (mean difference test values of p≥0.95): 2.0 days at T1, 2.5 days at T2 and 2.3 days at T3, respectively. The past 30-day cigarette smoking days were not statistically significantly different over the study period (T1,T2 and T3; values of p≥0.09) for any of the e-cigarette and cannabis use status at baseline (figure 1A). The average number of days of cigarette smoking was significantly higher among dual users compared with exclusive cannabis users (values of p<0.03), or with non-users (values of p<0.001), at each of the time points (T1–T3; figure 1A). Average number of days of smoking were not statistically significantly different between exclusive cannabis and exclusive e-cigarette users at each time point. Respondents reporting exclusive e-cigarette or cannabis use at T1, T2 and T3 also had higher past 30-day smoking frequency than those who reported no past 30-day use of either e-cigarette or cannabis (values of p<0.05).
Figure 1.
Number of days of past 30-day smoking (A) and nicotine dependence score (B), by e-cigarette and cannabis use status at baseline. Analytic sample N=1164. Post-hoc pairwise comparisons were tested using ANOVA least significant difference (p<0.05). Groups not sharing numerals are significantly different (p<0.05) in ANOVA Least Significant Difference.
A similar pattern was observed for nicotine dependence; dual users showed the highest number of symptoms for nicotine dependence than other use statuses (figure 1B). At baseline, in the past 30 days, only 1% of the participants used e-cigarette all 30 days, while it was 3.3% for cannabis use (online supplemental table S2)
Primary results of path analyses
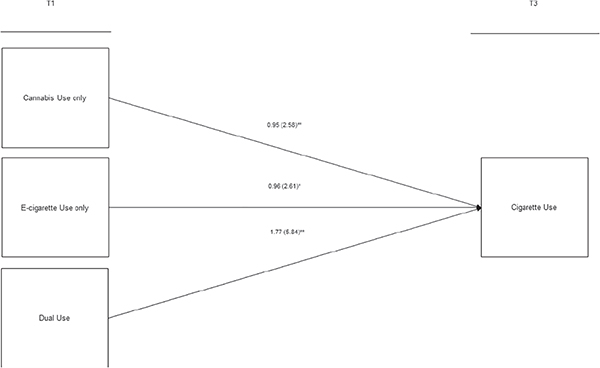
A path model was first conducted to evaluate the total effect of e-cigarette and cannabis use at baseline on past 30-day combustible cigarette use outcome at T3. We then performed a mediational path analysis to examine associations linking e-cigarette and cannabis use (T1) to cigarette use (T3) via cigarette use and nicotine dependence (T2). After controlling for baseline combustible cigarette use and other covariates, exclusive cannabis use (b=0.95; 95% CI 0.36 to 1.61/RR=2.58; 95% CI 1.43 to 4.98) in the past 30 days at T1 (12th grade), compared with no use, was significantly associated with increases in past 30-day combustible cigarette use at T3 (ie, total effect; figure 2).
Figure 2.
Total main effect model. Analytic sample N=1164. Negative binomial regression model in path analysis adjusting for all sociodemographic factors (eg, age, gender, race/ethnicity, and socioeconomic status) and baseline past 30-day cigarette use or other tobacco products, and nicotine dependence. Reference group of joint cannabis and e-cigarette use status at T1 was ‘No use’. Rate ratios (RRs) are shown (95% confidence intervals [95%CIs] are presented in online supplemental table S1). **p<0.001; *p<0.05 (two-tailed).
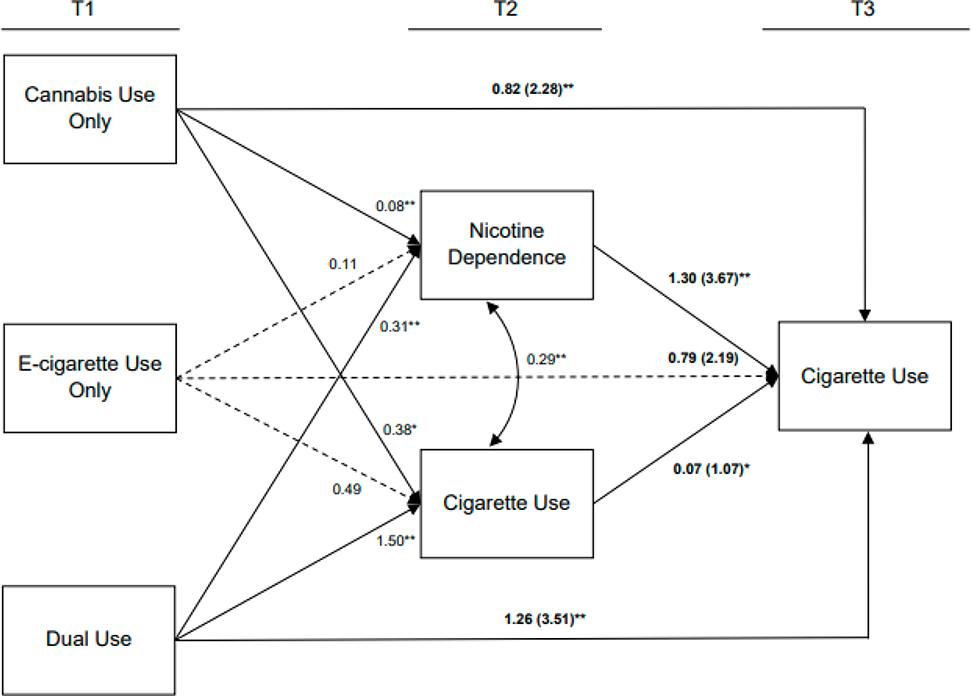
This total effect was mediated by nicotine dependence at T2 in the mediational path analysis model simultaneously adjusting for the concurrent mediational process of cigarette use at T2 (figure 3). Compared with no use, exclusive cannabis use in 12th grade was positively associated with increases in nicotine dependence (b=0.08; 95% CI 0.05 to 0.11) and cigarette use (b=0.38; 95% CI 0.18 to 0.57) at T2, which in turn were significantly related to greater number of smoking days at T3 (b=1.30; 95% CI 0.84 to 1.79/RR=3.67; 95% CI 2.32 to 6.01 and b=0.07; 95% CI 0.02 to 0.12/RR=1.07; 95% CI 1.02 to 1.13, respectively). The remaining direct effect of cannabis only use at T1 on increases in cigarette use at T3 was significant (b=0.82; 95% CI 0.28 to 1.36/RR=2.28; 95% CI 1.33 to 3.88) but reduced compared with the total effect (table 2 and online supplemental table S3).
Figure 3.
Mediational path analysis model. Analytic sample N=1164. Negative binomial regression model in path analysis adjusting for all sociodemographic factors (eg, age, gender, race/ethnicity, and socio-economic status) and baseline past 30-day cigarette use or other tobacco products and nicotine dependence) presented in table 1. Reference group of joint cannabis and e-cigarette use status at T1 was ‘No use’. Estimates on pathways linking T1 to T2 were unstandardised regression coefficients. Estimates on pathways (bold text) linking T1/T2 to T3 were rate ratios (RRs; 95%CIs are presented in online supplemental table S2). **p<0.001; *p<0.05 (two-tailed).
Table 2.
Indirect effects of mediational paths linking baseline dual use to cigarette use at T3 via nicotine dependence and cigarette use at T2*
| Total main effect model† | Mediational path analysis model‡ | |||||
|---|---|---|---|---|---|---|
| Dual use status T1 → Cigarette use T3 | Dual use status T1 → Cigarette use T3 | Dual use status T1 → Cigarette use T2 → Cigarette use T3 | Dual use status T1 → Nicotine dependence T2 → Cigarette use T3 | |||
| Total effects | Direct effects | Indirect effects§ | Proportion mediated | Indirect effects§ | Proportion mediated | |
| Dual use status Tl | b (95% Cl) | b (95% Cl) | b (95% Cl) | % (95% Cl) | b (95% Cl) | % (95% Cl) |
| No use | REF | REF | REF | - | REF | - |
| Cannabis use only | 0.95 (0.36 to 1.61) | 0.82 (0.28 to 1.36) | 0.03 (0.01 to 0.05) | 3.2 (1.1 to 5.3) | 0.10 (0.06 to 0.14) | 10.5 (6.3 to 14.7) |
| E-cigarette use only | 0.96 (0.04 to 2.57) | 0.79 (−0.02 to 2.46) | 0.03 (−0.01 to 0.13) | - | 0.14 (−0.02 to 0.45) | - |
| Dual use | 1.77 (1.15 to 2.55) | 1.26 (0.11 to 2.31) | 0.10 (0.03 to 0.18) | 5.7 (1.7 to 10.2} | 0.41 (0.17 to 0.64) | 23.3 (9.6 to 36.3) |
Analytical sample n=1164. All models were adjusted for past 30-day cigarette use or other tobacco products and nicotine dependence at T1 and age, sex, race/ethnicity and socioeconomic status.
Total main effect model presented in figure 2.
Mediational path onlays is model presented in figure 3.
Indirect effect estimates (path coefficients between T1 and T2 x path coefficients between T2 and T3; b (95% Cl) and effect size (proportion mediated: the proportion of indirect effect to the total effect) were calculated based on the mediational path model presented in figure 3. Unstandardised path coefficient (b) and 95% Cl are presented.
For dual use, the main effect model found the significant association between dual cannabis/e-cigarette use at T1 and cigarette smoking at T3 (b=1.77; 95% CI 1.15 to 2.55/RR=5.84; 95% CI 3.16 to 12.81); figure 2. Compared with participants with no e-cigarette or cannabis use at baseline, who reported (unadjusted) average 0.4 days of smoking at T3, dual users at baseline reported average 2.3 days of smoking at T3 (figure 1A). In the subsequent mediational path analysis, baseline dual users showed increased levels of nicotine dependence (b=0.31; 95% CI 0.19 to 0.43) and combustible cigarette use (b=1.50; 95% CI 0.97 to 2.03) after high school graduation (T2), which in turn were positively associated with the number of smoking days at T3. After accounting for these mediational paths, baseline dual use was significantly associated with increases in past 30-day cigarette use (b=1.26; 95% CI 0.11 to 2.31/RR=3.51; 95% CI 1.12 to 10.01) as remaining direct effects (figure 3 and table 2).
Compared with no use of e-cigarette and cannabis at T1, exclusive e-cigarette use at T1 was associated with increases in number of cigarette smoking days at T3 (b=0.96; 95% CI 0.04 to 2.57/RR=2.61; 95% CI 1.04 to 13.07); figure 2 (total main effect). However, exclusive e-cigarette use at T1 was not significantly associated through meditational paths of nicotine dependence and cigarette use at T2 with cigarette use at T3 (figure 3 and table 2).
Test of indirect effects
In the primary mediation path analysis, nicotine dependence and combustible cigarette use simultaneously mediated the prospective associations of exclusive cannabis use and dual use with combustible cigarette use. As presented in table 2, the indirect effect of exclusive cannabis use at T1 → Nicotine dependence T2 → Cigarette use T3 was significant (b=0.10; 95% CI 0.06 to 0.14), and nicotine dependence at T2 mediated 10.5% (95% CI 6.3% to 14.7%) of total effects of exclusive cannabis use at T1 on increases in cigarette use at T3. The indirect effect of Dual use T1→ Nicotine dependence T2 → Cigarette use at T3 was significant, and the proportion of this indirect effect of the total effect was 23.3% (95% CI 9.6% to 36.3%). Cigarette use at T2 significantly mediated 3.2% (95% CI 1.1% to 5.3%) of the associations of exclusive cannabis use at T1 with cigarette use at T3, and 5.7% (95% CI 1.7% to 10.2%) of total effects of dual use on cigarette use at T3.
Sensitivity analyses
After restricting the analysis to study participants who were not past 30-day cigarette smokers at T1 (n=1057), exclusive cannabis use and dual use of e-cigarettes and cannabis at T1 were still associated with increased cigarette use at T3, and the associations were mediated through nicotine dependence and cigarette smoking at T2 (see online supplemental figure S2). Thus, the pattern of associations was consistent, although the estimates of associations of nicotine dependence and cigarette use at T2 with cigarette use at T3 were attenuated. In the sensitivity analysis including all participants who provided valid data at baseline and at least at one follow-up (n=2603, figure 1), the overall associations were similar to results in the primary analysis (see online supplemental figure S3). Using the supplemental outcome of cigarette use quantity per day in the past 30 days (ie, number of cigarettes smoked per smoking day; range=0–20 cigarettes), we consistently found significant results in the key mediating pathways of dual use T1→ Nicotine dependence T2→ Cigarettes smoked per smoking day T3 (see online supplemental figure S4).
DISCUSSION
As e-cigarette and cannabis use among adolescents is common, it is important to understand how these exposures affect cigarette smoking habits into young adulthood. To the best of our knowledge this is the first study exploring the dual effect of e-cigarette and cannabis use among adolescents on subsequent cigarette smoking among young adults via the mediational process of nicotine dependence using longitudinal data, which were available over a follow-up period of 42 months. Using mediational analysis, we show that cannabis and e-cigarette use during 12th grade was prospectively associated with higher frequency of combustible cigarette use at 42-month follow-up after high school graduation and that the estimated effect was partially mediated through nicotine dependence and cigarette use assessed at 24-month follow-up. Prevalence of combustible cigarette use at the conclusion of follow-up was most prominent among adolescents who were dual users of e-cigarette and cannabis (2.3 average smoking days (figure 1a), 31.4% past-month smokers among dual users (online supplemental table S4)). The effect of dual use of cannabis and e-cigarettes with subsequent smoking has not been explored in previous longitudinal studies. Thus, the association of both cannabis and e-cigarette use leading to a large increased risk of monthly smoking days, with a substantial proportion of this increase mediated through nicotine dependence and cigarette use in the intervening period is a unique contribution to our understanding of the trajectory of smoking increase in young adults.
Previous studies have shown that the ‘intention pathway’—higher intention to smoke cigarettes—only partially explains the risk of subsequent smoking among e-cigarette users.10 A recent study exploring the possible role of the intention pathway found that although smoking initiation was higher among adolescents who intended to smoke, adolescents who were never smokers and had no intention to smoke but used e-cigarettes were more than four times more likely to smoke in subsequent years than adolescents who did not use e-cigarette.10 The authors concluded that this might be due to the role of the ‘addictive pathway’ above and beyond the ‘intention pathway’ among e-cigarette users. Our group has previously reported that adolescents were more likely to have symptoms of e-cigarette dependence if they vaped in the last 30 days, compared with those who did not vape in last 30 days.12 The current observation that dual use of cannabis and e-cigarettes markedly augmented nicotine dependence, leading to higher frequency of subsequent smoking, is biologically plausible based on similar effects of cannabis and e-cigarettes on dopaminergic pathways of addiction.
Results are consistent with previous studies showing associations of e-cigarette and cannabis use with nicotine dependence.30–34 Strengths of this study are to demonstrate that the strong association of dual e-cigarette and cannabis use with subsequent frequency of days of cigarettes smoked and to show that these associations were partially mediated through nicotine dependence and cigarette use; the estimated mediational effect of nicotine dependence on subsequent frequency of cigarette smoking was larger than the mediational effect of cigarette smoking, indicating that nicotine dependence is central to understanding the effects of e-cigarette and cannabis use on smoking progression. In addition, dual use of e-cigarette and cannabis among adolescents had substantial associations with nicotine dependence; the estimated effect of dual use on subsequent smoking frequency was substantially larger than the effect of either alone. This effect of dual use of e-cigarette and cannabis, potentially due to interactions within neurological pathways of addiction shared by nicotine and cannabis5 14 18 warrants further investigation in animal and human studies. Additional research is also needed to differentiate the roles of the ‘intention pathway’ and ‘addiction pathway’ in cigarette uptake associated with the dual use of e-cigarette and cannabis. Although the mediational pathways of combustible cigarette use at T2 were simultaneously modelled with nicotine dependence to consider the consistency of smoking behaviours over time, this does not control for the ‘intention pathway’, because it reflects effects of both intentions to smoke and addiction effects at T1.
Associations of cannabis use with cigarette smoking have been observed among adults.35 In a large cohort (age 18+ years, n=26 341), those who used cannabis were at much greater risk of subsequent smoking initiation. Furthermore, smokers who also used cannabis were substantially less likely to quit smoking (OR=0.36; 95% CI 0.20 to 0.65) compared with smokers who did not use cannabis. In another study of participants age 12+ years, cigarette dependence was highest among daily users of cannabis than among non-daily or never users.36 Our results extend these previous studies in a young adult population in a longitudinal analytical framework demonstrating the role of nicotine dependence and an increasing trajectory of cigarette use mediating cannabis associations. The study strengthens the evidence that cannabis use increases smoking across adolescence into adult life.
The association of exclusive e-cigarette use with subsequent smoking frequency is consistent with previous studies.7 Unlike exclusive cannabis and dual use, we did not find statistically significant mediation effects by nicotine dependence or cigarette smoking, although the mediational effect estimates of exclusive e-cigarette use were consistently larger than those of exclusive cannabis use. The sample of exclusive e-cigarette users at baseline (2.5%) was much smaller than the 26.1% prevalence of cannabis users. Thus, statistical power to identify statistically significant mediational effects was limited. We identified no other previous studies that differentiated between mediational effects associated with exclusive e-cigarette use and dual use of e-cigarettes and cannabis.7
Among caveats to the study, the absolute number of cigarette smoking days and level of nicotine dependence was low in this sample of adolescents and youth. The HONC Scale identifies the mild symptoms of nicotine dependence more commonly in youth than the established nicotine dependence observed among adult heavy smokers. Further follow-up will assess whether dual use of e-cigarettes and cannabis will result in progression to heavy regular smoking and the role of dependence. Also, we couldn’t explore whether the observed association varied by mode of cannabis intake as 92.8% of our participants used combustible cannabis (see online supplemental table S5). However, our study supports the hypothesis, suggested by preclinical neuropharmacological studies, that THC augments nicotine dependence such that dual use of cannabis and e-cigarettes results in greater cigarette smoking.
The pattern of cannabis and e-cigarette use in the study population markedly differed from what is observed in a nationally representative population of US youth (9th–12th graders) of the YRBS.4 The prevalence of exclusive use of e-cigarette was lower (2.5% vs 14%) and cannabis was higher (22% vs 4%) than the nationally representative rates. However, the study population differed from the YRBS in multiple aspects: unlike the YRBS population, the study population was exclusively from southern California, it included only 12th grade students at baseline and had a lower proportion of non-Hispanic whites (17% vs 52%), factors that can affect both e-cigarette and cannabis use. Our findings may not be generalisable to dissimilar populations across the USA.
One concern is whether restricting the study sample to participants with reported use of any nicotine product over the course of the study could have introduced selection bias. Study participants who never used any nicotine product (n=1439) were less likely to be Hispanic and more likely to be Asian and have parents with a college degree compared with those included in the study analysis (from online supplemental table S1). However, all analytical models were adjusted for age, sex, race/ethnicity and socioeconomic status. Furthermore, in a sensitivity analysis, when we included all participants who provided valid data at study baseline and at least one of the follow-ups (n=2603), the overall pattern of effect estimates were similar to those in the analytical sample (see online supplemental figure S3). Therefore, selection bias seems unlikely to explain the observed associations.
Given the known relationship between cigarette smoking and nicotine dependence, which can lead to greater use of cigarettes,37 38 one explanation for the observed associations could be cigarette use and nicotine dependence at T1. We adjusted for current cigarette smoking and nicotine dependence at T1 in the primary analyses to control for this possibility. Furthermore, as a sensitivity analysis we restricted the mediational analysis to those who had not smoked in the past 30 days at T1 (see online supplemental figure S2). The pattern of associations of cannabis and e-cigarettes with subsequent smoking and of mediation pathways in this restricted population was similar to the results in the primary analysis. Therefore, we conclude that observed associations are not an artefact of cigarette use and nicotine dependence at T1.
Another concern could be measurement error in exposure and outcome variables due to self-reported use of e-cigarette, cannabis and cigarettes, and to self-reported nicotine dependence. However, assessment of exposure to nicotine and cannabis products used standardised survey questionnaires (or adaptations)22 23 that have been shown to have good reliability39 and to have adequate psychometric properties.23 Like many previous studies assessing e-cigarette nicotine dependence among adolescents, we used a modified version of HONC.12 24 Therefore, it is unlikely that the robust pattern of observed associations is explained by measurement error.
CONCLUSION
This longitudinal study provides evidence that dual use of e-cigarettes and cannabis, which is common in adolescents in our sample, is associated with more frequent cigarette smoking during young adulthood and that this prospective relationship is partially mediated by increased nicotine dependence. This suggests a likely causal pathway linking e-cigarette, cannabis and dual use, to increasing cigarette use. The results fulfil several criteria for causation in observational studies: temporality, biological plausibility and large effect sizes. Cannabis use was highly prevalent among adolescents in this study, while dual use was common. Therefore, this study provides a rationale for regulatory and other interventions to prevent both e-cigarette and cannabis use in adolescents in order to curb cigarette smoking in young adults. In California and other states in which cannabis use has been legalised, the implications for increased cannabis use in adolescents leading to heavier cigarette use in young adults warrants further investigation and regulatory scrutiny.40
Supplementary Material
WHAT IS ALREADY KNOWN ON THIS TOPIC
Independently, e-cigarette and cannabis use is associated with smoking initiation and nicotine dependence. However, little is known about the effect of dual use of e-cigarette and cannabis on cigarette smoking behaviour among adolescents, among whom the dual use of e-cigarette and cannabis is common.
WHAT THIS STUDY ADDS
This prospective study shows that dual use of e-cigarette and cannabis among high school children is associated with increased smoking over a 42-month period, compared with non-users; and this effect was partially mediated through nicotine dependence. The study provides a potential causal pathway between dual use of e-cigarette and cannabis during adolescence leading to higher frequency of smoking and heavier smoking during young adulthood.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
As cannabis is being legalised in many states in the USA, research is needed to understand the relationship to cigarette use. Interventions targeting both e-cigarette and cannabis use among adolescents may be needed to curb cigarette uptake and use as young adults.
Funding
The study was supported by the National Institutes of Health (grants U54CA180905, R21HD084812, P30ES007048 and 5P30CA014089).
Footnotes
Competing interests None declared.
Patient consent for publication Not applicable.
Ethics approval This study involves human participants and was approved by the institutional review board of the University of Southern California (HS-18–00706). Written informed consent was obtained for all participants prior to data collection. Participants gave informed consent to participate in the study before taking part.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
REFERENCES
- 1.Johnston LD, Miech RA, O’Malley PM. MONITORING THE FUTURE NATIONAL SURVEY RESULTS ON DRUG USE 1975. 2018. Available: http://www.monitoringthefuture.org//pubs/monographs/mtf-overview2018.pdf
- 2.Wang TW, Gentzke AS, Creamer MR, et al. Tobacco product use and associated factors among middle and high school students-United States, 2019. MMWR Surveill Summ 2019;68:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamilton AD, Jang JB, Patrick ME, et al. Age, period and cohort effects in frequent cannabis use among US students: 1991–2018. Addiction 2019;114:1763–72. 10.1111/add.14665 Available: https://onlinelibrary.wiley.com/toc/13600443/114/10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wills TA, Leventhal AM, Sargent JD, et al. Concurrent use of e-cigarettes, combustible cigarettes, and marijuana. Pediatrics 2021;148:e2021050749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lemyre A, Poliakova N, Bélanger RE. The relationship between tobacco and cannabis use: a review. Subst Use Misuse 2019;54:130–45. [DOI] [PubMed] [Google Scholar]
- 6.Weinberger AH, Platt J, Copeland J, et al. Is cannabis use associated with increased risk of cigarette smoking initiation, persistence, and relapse? longitudinal data from a representative sample of US adults. J Clin Psychiatry 2018;79:17m11522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoong SL, Hall A, Turon H, et al. Association between electronic nicotine delivery systems and electronic non-nicotine delivery systems with initiation of tobacco use in individuals aged. [DOI] [PMC free article] [PubMed]
- 8.Goldenson NI, Leventhal AM, Stone MD, et al. Associations of electronic cigarette nicotine concentration with subsequent cigarette smoking and vaping levels in adolescents. JAMA Pediatr 2017;171:1192–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Primack BA, Soneji S, Stoolmiller M, et al. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatr 2015;169:1018–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Owotomo O, Stritzel H, McCabe SE, et al. Smoking intention and progression from e-cigarette use to cigarette smoking. Pediatrics 2020;146:e2020002881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jankowski M, Krzystanek M, Zejda JE, et al. E-Cigarettes are more addictive than traditional cigarettes-A study in highly educated young people. Int J Environ Res Public Health 2019;16:2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vogel EA, Cho J, McConnell RS, et al. Prevalence of electronic cigarette dependence among youth and its association with future use. JAMA Netw Open 2020;3:e1921513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rudasingwa G, Kim Y, Lee C, et al. Comparison of nicotine dependence and biomarker levels among traditional cigarette, heat-not-burn cigarette, and liquid e-cigarette users: results from the think study. Int J Environ Res Public Health 2021;18:4777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zehra A, Burns J, Liu CK, et al. Cannabis addiction and the brain: a review. J Neuroimmune Pharmacol 2018;13:438–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rabin RA, George TP. A review of co-morbid tobacco and cannabis use disorders: possible mechanisms to explain high rates of co-use. Am J Addict 2015;24:105–16. [DOI] [PubMed] [Google Scholar]
- 16.Dani JA. Roles of dopamine signaling in nicotine addiction. Mol Psychiatry 2003;8:255–6. [DOI] [PubMed] [Google Scholar]
- 17.Laviolette SR, van der Kooy D. The neurobiology of nicotine addiction: bridging the gap from molecules to behaviour. Nat Rev Neurosci 2004;5:55–65. [DOI] [PubMed] [Google Scholar]
- 18.Ren M, Lotfipour S. Nicotine gateway effects on adolescent substance use. West J Emerg Med 2019;20:696–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Valjent E, Mitchell JM, Besson MJ, et al. Behavioural and biochemical evidence for interactions between delta 9-tetrahydrocannabinol and nicotine. Br J Pharmacol 2002;135:564–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen C, Perrault G, Voltz C, et al. Sr141716, a central cannabinoid (CB (1)) receptor antagonist, blocks the motivational and dopamine-releasing effects of nicotine in rats. Behav Pharmacol 2002;13:451–63. [DOI] [PubMed] [Google Scholar]
- 21.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA 2015;314:700–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance-United States, 2009. MMWR Surveill Summ 2010;59:1–142. [PubMed] [Google Scholar]
- 23.Johnston LD, O’Malley PM, Miech RA, et al. Monitoring the future national survey results on drug use 1975–2014: overview: key findings on adolescent drug use. In: Ann Arbor. MI: Institute for Social Research, The University of Michigan, 2015. [Google Scholar]
- 24.DiFranza JR, Savageau JA, Fletcher K, et al. Measuring the loss of autonomy over nicotine use in adolescents: the DANDY (development and assessment of nicotine dependence in youths) study. Arch Pediatr Adolesc Med 2002;156:397–403. [DOI] [PubMed] [Google Scholar]
- 25.Mantey DS, Case KR, Omega-Njemnobi O, et al. Use frequency and symptoms of nicotine dependence among adolescent e-cigarette users: comparison of JUUL and non-JUUL users. Drug and Alcohol Dependence 2021;228:109078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tackett AP, Hébert ET, Smith CE, et al. Youth use of e-cigarettes: does dependence vary by device type? Addict Behav 2021;119:106918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hilbe JM. Negative binomial regression. Negative Binomial Regression 2 ed. Cambridge: Cambridge University Press, 17 March 2011. [Google Scholar]
- 28.Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychol Methods 2011;16:93–115. [DOI] [PubMed] [Google Scholar]
- 29.Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles, CA: Muthen & Muthen, 2017. [Google Scholar]
- 30.Rycroft N, Hogarth L, MacKillop J, et al. Vapers exhibit similar subjective nicotine dependence but lower nicotine reinforcing value compared to smokers. Addict Behav 2021;115:106737. [DOI] [PubMed] [Google Scholar]
- 31.Kechter A, Cho J, Miech RA, et al. Nicotine dependence symptoms in U.S. youth who use JUUL e-cigarettes. Drug Alcohol Depend 2021;227:108941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xi Z-X, Muldoon P, Wang X-F, et al. Δ8 -tetrahydrocannabivarin has potent anti-nicotine effects in several rodent models of nicotine dependence. Br J Pharmacol 2019;176:4773–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.González Roz A, Secades Villa R, Weidberg S. Evaluating nicotine dependence levels in e-cigarette users. Adicciones 2017;29:136–8. [DOI] [PubMed] [Google Scholar]
- 34.Agrawal A, Lynskey MT, Pergadia ML, et al. Early cannabis use and DSM-IV nicotine dependence: a twin study. Addiction 2008;103:1896–904. 10.1111/j.1360-0443.2008.02354.x Available: http://blackwell-synergy.com/doi/abs/10.1111/add.2008.103.issue-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weinberger AH, Delnevo CD, Wyka K, et al. Cannabis use is associated with increased risk of cigarette smoking initiation, persistence, and relapse among adults in the United States. Nicotine Tob Res 2020;22:1404–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weinberger AH, Dierker L, Zhu J, et al. Cigarette dependence is more prevalent and increasing among US adolescents and adults who use cannabis, 2002–2019. Tob Control 2021:tobaccocontrol-2021–056723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Notley C, Ward E, Dawkins L, et al. User pathways of e-cigarette use to support long term tobacco smoking relapse prevention: a qualitative analysis. Addiction 2021;116:596–605. 10.1111/add.15226 Available: https://onlinelibrary.wiley.com/toc/13600443/116/3 [DOI] [PubMed] [Google Scholar]
- 38.Cougle JR, Hakes JK, Macatee RJ, et al. Probability and correlates of dependence among regular users of alcohol, nicotine, cannabis, and cocaine: concurrent and prospective analyses of the National epidemiologic survey on alcohol and related conditions. J Clin Psychiatry 2016;77:e444–50. [DOI] [PubMed] [Google Scholar]
- 39.Brener ND, Kann L, McManus T, et al. Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health 2002;31:336–42. [DOI] [PubMed] [Google Scholar]
- 40.Weinberger AH, Wyka K, Goodwin RD. Impact of cannabis Legalization in the United States on trends in cannabis use and daily cannabis use among individuals who smoke cigarettes. Drug Alcohol Depend 2022;238:109563. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.