Abstract
Cardiometabolic diseases, including cardiovascular disease (CVD) and type 2 diabetes (T2D), are the leading cause of death globally. Because T2D and obesity are strongly associated, weight loss is the cornerstone of treatment. However, weight loss is rarely sustained, which may lead to weight cycling, which is associated with increased mortality risk in patients with T2D. Meta-analyses show that weight loss is not generally associated with reduced mortality risk in T2D, whereas weight cycling is associated with increased all-cause and CVD mortality. This may be attributable in part to increased variability in CVD risk factors that often accompany weight cycling, which studies show is consistently associated with adverse CVD outcomes in patients with T2D. The inconsistent associations between weight loss and mortality risk in T2D, and consistent findings of elevated mortality risk associated with weight cycling, present a conundrum for a weight-loss focused T2D prevention and treatment strategy. This is further complicated by the findings that among patients with T2D, mortality risk is lowest in the body mass index (BMI) range of ~25–35 kg/. Because this “obesity paradox” has been consistently demonstrated in 7 meta-analyses, the lower mortality risk for individuals with T2D in this BMI range may not be all that paradoxical. Physical activity (PA), cardiorespiratory fitness (CRF), and muscular fitness (MF) are all associated with reduced risk of T2D, and lower risk of CVD and all-cause mortality in individuals with T2D. Reducing sedentary behavior, independent of PA status, also is strongly associated with reduced risk of T2D. Improvements in cardiometabolic risk factors with exercise training are comparable to those observed in weight loss interventions, and are largely independent of weight loss. To minimize risks associated with weight cycling, it may be prudent to adopt a weight-neutral approach for prevention and treatment of individuals with obesity and T2D by focusing on increasing PA and improving CRF and MF without a specific weight loss goal.
Keywords: obesity, metabolic syndrome, cardiorespiratory, cardiovascular disease, exercise, weight fluctuation, body weight variability
1. Introduction
Cardiometabolic diseases, including cardiovascular disease (CVD) and type 2 diabetes (T2D), are the leading cause of death globally [1]. An estimated 463 million people have T2D, and this number is projected to increase by 25% in 2030 and by 51% in 2045 [2]. Obesity is associated with increased risk of CVD and T2D, although lifestyle factors, such as physical activity and diet, are considered important to reduce risk of CVD and T2D [3, 4, 5, 6]. Because T2D and obesity are strongly associated, weight loss is the cornerstone of treatment [7]. However, weight loss is rarely sustained [8, 9, 10]. During the past 4 decades, worldwide obesity prevalence has doubled in 70 countries [11], and has tripled in the United States [12]. During this same period of time, the prevalence of weight loss attempts has increased substantially, and it is estimated that ~40%–50% of US adults attempt weight loss annually [13, 14]. Data from 2013–2016 National Health and Nutrition Examination Surveys indicated that two-thirds of adults with obesity tried to lose weight within the preceding year [13]. Thus, it could be argued that weight loss strategies have been largely unsuccessful at reducing obesity prevalence.
Due to the transient success of weight loss attempts, weight cycling is common, and is associated with health risks [14, 15, 16]. For example, the magnitude of the mortality risk associated with weight cycling [17, 18, 19] is comparable to, or greater than, that reported for obesity [20, 21, 22]. An important question is whether the risks of weight cycling outweigh the risks associated with obesity. This is especially relevant to individuals with T2D and obesity because weight loss is routinely advocated as a treatment strategy. Although obesity greatly increases the risk of T2D [23], the benefits of weight loss need to be considered in the context of potential risks associated with repeated episodes of weight regain that could lead to chronic weight cycling. Of additional consideration is the well documented finding of an obesity paradox in patients with T2D, which consistently shows that the body mass index (BMI, kg/) associated with lowest mortality is in the BMI categories defined as overweight or moderately obese (i.e., BMI ~25–35 kg/) [24, 25, 26, 27, 28, 29, 30]. Accordingly, it has been suggested that weight loss strategies that minimize weight cycling should be advocated [31, 32]. Given the poor success of weight loss attempts over the past several decades, such an approach may be impracticable.
Physical activity (PA), cardiorespiratory fitness (CRF), and muscular fitness (MF) also influence the risk associated with obesity and T2D [33, 34, 35, 36, 37, 38, 39, 40, 41]. PA is defined as any bodily movement produced by skeletal muscles that results in energy expenditure, and can categorized into occupational, sports, conditioning, leisure-time, or household activities [42]. CRF is a measure of maximal aerobic capacity and is usually assessed by an exercise test to volitional exhaustion [43]. MF generally reflects the integrated status of muscular strength and endurance [42], but in epidemiological studies is most frequently defined by assessing maximum force generation while performing a specific task (e.g., leg press, chest press, handgrip strength). Exercise training has well documented health benefits independent of weight loss [4, 5, 6], which is notable because exercise training alone rarely results in appreciable weight loss [44, 45, 46, 47]. This has implications for treatment because published data on the association between intentional weight loss and mortality risk in patients with T2D is sparse and inconsistent [48].
One of the objectives of this review was to examine the published data on mortality and CVD morbidity risks associated with weight loss and weight cycling in individuals with T2D. Another was to review published data on T2D incidence associated with PA, CRF, and MF, and the mortality risks associated with PA and CRF in persons with T2D. Comparison of associated risks may help to inform decisions about treatment strategies for individuals with T2D. This review relied primarily on data from prospective cohort studies and, when possible, meta-analyses of cohort studies.
2. Weight Loss and Mortality Risk in T2D
Although weight loss is routinely advocated for treating individuals with obesity, especially with comorbidities such as CVD and T2D, intentional weight loss is not consistently associated with reduced mortality risk [4]. This is particularly true for individuals with T2D. A meta-analysis of 3 observational cohort studies indicated that intentional weight loss in overweight or obese individuals with T2D was not associated with significantly reduced all-cause mortality risk (relative risk, RR = 0.90; 95% confidence interval, CI, 0.67–1.22) [48]. It is important to note that this meta-analysis exhibited considerable heterogeneity in risk estimates across the 3 cohort studies.
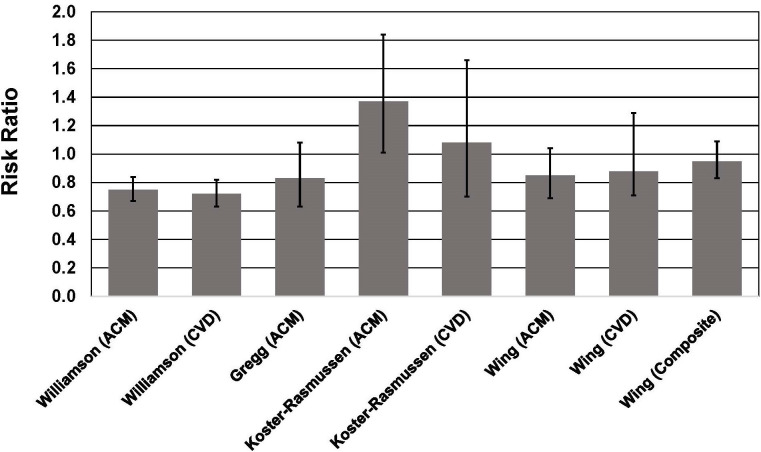
For example, in the American Cancer Society’s Cancer Prevention Study I [49], self-reported intentional weight loss among men and women with T2D and BMI 27 kg/ was associated with a 25% lower risk of all-cause mortality (RR = 0.75, 95% CI, 0.67–0.83) and 28% lower risk of CVD mortality (RR = 0.72, 95% CI, 0.63–0.82) (Fig. 1, Ref. [50]). Data on individuals with T2D and BMI 25 kg/ in the National Health Interview Survey [51] showed that self-reported intentional weight loss was not associated with lower risk of mortality during 9 years of follow-up (Hazard Ratio, HR = 0.83, 95% CI, 0.63–1.08). Interestingly, just “trying to lose weight” but failing to do so was associated with a 23% lower risk of mortality (HR = 0.72, 95% CI, 0.55–0.96) (Fig. 1). These results suggest that the behaviors (e.g., exercise and diet) may be more important for reducing mortality risk than weight loss per se.
Fig. 1.
Association between intentional weight loss and mortality risk in individuals with type 2 diabetes. See text for description of studies. Vertical bars = 95% confidence intervals. ACM, All-cause mortality; CVD, cardiovascular disease mortality. In the study by Wing et al. [50], composite = death from cardiovascular causes, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for angina.
By contrast, among patients in the intervention arm of the Diabetes Care in General Practice randomized clinical trial [52], intentional weight loss was generally associated with higher mortality risk (Fig. 1). This result was primarily driven by patients with T2D and BMI 30 kg/. During 13 years of follow-up, those with BMI 30 kg/ in the “intention to lose weight group” had a 37% higher all-cause mortality risk (HR = 1.37, 95% CI, 1.01–1.84) for each 1-kg weight loss per year during a 6-year monitoring period. For patients with BMI 30 kg/, intentional weight loss was not associated with mortality risk. In contrast to studies in which weight loss intention and amount were self-reported [49, 51], subjects in this study were weighed regularly during the physician-supervised 6-year monitoring period, with a median of 13 weights recorded during the monitoring period. Lowest mortality was observed in patients who maintained their weight during the follow-up period.
The findings of the Diabetes Care in General Practice study are consistent with the results of the Look AHEAD trial that found no benefit of an intensive lifestyle intervention that resulted in significant weight loss in adults with T2D and obesity [50]. During a median follow-up of 9.6 years, patients receiving the intensive lifestyle intervention had a HR (0.95, 95% CI, 0.83–1.09) for the primary outcome (death from cardiovascular causes, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for angina) that was not different from the control group receiving diabetes support and education, despite achieving significantly greater weight loss throughout the study and greater reductions in hemoglobin A1c (HbA1c) (Fig. 1).
3. Weight Cycling and Mortality Risk in T2D
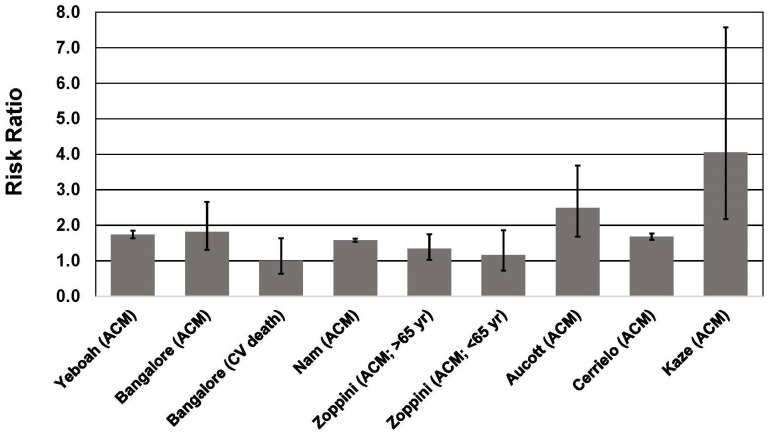
Several meta-analyses have shown that weight cycling is associated with a ~41%–53% higher risk of all-cause mortality [17, 18, 19] and a 36% higher risk of cardiovascular disease mortality [19]. The 36% higher risk of CVD mortality is consistent with a 35% higher risk of hypertension and 49% higher risk of CVD morbidity associated with weight cycling [19]. Higher morbidity and mortality risk associated with weight cycling has been well documented in T2D [53, 54, 55, 56, 57, 58, 59, 60, 61] (Fig. 2 Ref. [55], Fig. 3). A recent meta-analysis that included 6 studies of individuals with T2D, indicated that weight cycling was associated with higher risk of all-cause mortality [62]. Regardless of how weight cycling was defined (e.g., average successive variability of body weight; coefficient of variation of body weight; standard deviation of body weight), fluctuation in body weight was associated with a 50%–58% higher risk of all-cause mortality in patients with T2D. Results from these six studies [53, 55, 56, 58, 59, 61], and three additional studies [54, 57, 60], are described below and presented in Figs. 2,3.
Fig. 2.
Association between body weight fluctuation (weight cycling) and mortality risk in individuals with type 2 diabetes. See text for description of studies. Vertical bars = 95% confidence intervals. ACM, All-cause mortality; CV, cardiovascular. In the study of Kaze et al. [55], a 15.28-fold higher risk of CVD mortality is not shown for purposes of maintaining scale on the y-axis.
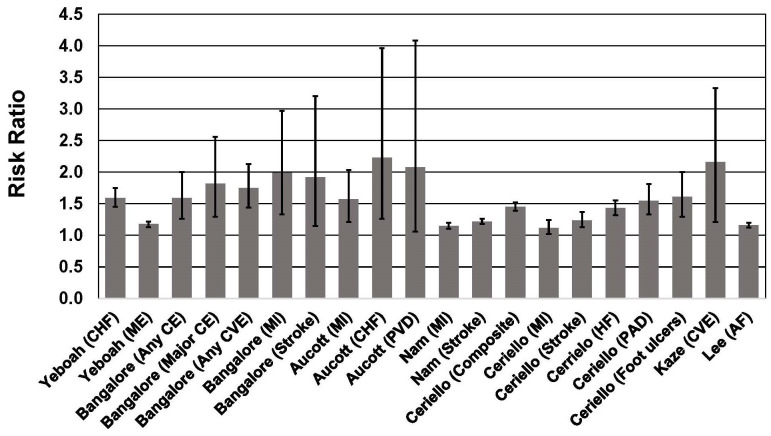
Fig. 3.
Association between body weight fluctuation (weight cycling) and risk of adverse cardiovascular outcomes in individuals with type 2 diabetes. See text for description of studies. Vertical bars = 95% confidence intervals. AF, atrial fibrillation; CE, coronary event; CHF, congestive heart failure; Composite, Nonfatal myocardial infarction, nonfatal stroke, and all-cause mortality; CVE, cardiovascular event; HF, heart failure; ME, microvascular events; MI, myocardial infarction; PAD, peripheral artery disease; PVD, peripheral vascular disease.
In the ACCORD trial (Action to Control Cardiovascular Risk Factors in Diabetes), which included 10,251 participants with T2D, body weight variability during a mean 3.5 years of follow-up was associated with a 25% higher risk of the primary outcome (nonfatal myocardial infarction or stroke, or CVD death), 59% higher risk of heart failure, 74% higher risk all-cause mortality, and an 18% higher risk of microvascular events [56]. These associations were significant even after adjusting for BMI. The ACCORD trial is a multicenter factorial randomized controlled trial (RCT) designed to compare intensive blood pressure, glycemic, and lipid treatment with standard care in patients with T2D, ~91% with BMI 25 kg/, and 62% with BMI 30 kg/. The ACCORD trial was not a weight loss intervention; thus it is not known if weight variability was the result of intentional or unintentional weight loss. In this trial, higher BMI was also associated with higher risk of heart failure and all-cause mortality, but body weight variability appeared to be associated with greater risk. For example, compared with patients with BMI 30 kg/ who were in the lowest quartile of body weight variability, patients with BMI 25 kg/ at baseline but who were in the highest quartile of body weight variability had a 191% higher risk of CVD events (HR = 2.91, 95% CI, 1.35–6.28).
Among 6408 patients with T2D participating in one of three clinical trials of statins [53], weight cycling was associated with a significant increase of a composite endpoint that included coronary heart disease, death, myocardial infarction, resuscitated cardiac arrest, coronary revascularization, and unstable or new-onset angina. Subjects had a median of 12 body weight assessments during the interventions and follow-up periods of between 3.9 and 4.9 years. Body weight variability was calculated as the average absolute difference between successive body weight measurements. When expressed as a continuous variable, each 1 standard deviation (SD) increase in body weight variability was associated with an ~8%–21% higher risk of coronary and cardiovascular events, including mortality. Compared with patients in the lowest quintile of body weight variability, patients in the highest quintile of body weight variability had a 59% higher risk of any coronary event, 84% higher risk of major coronary event, 75% higher risk of any cardiovascular event, 82% higher risk of death, 99% higher risk of MI, and 92% higher risk of stroke. These associations were independent of traditional CVD risk factors, mean body weight, and weight change. Importantly, the associations between body weight variability and CVD risk increased with BMI. Consequently, the CV risks associated with weight cycling among patients with T2D were disproportionately observed in those with the highest BMI. Since weight cycling is more prevalent among individuals with high BMI [63, 64], it is plausible that higher risk associated with obesity may be in part due to adverse health effects of weight cycling.
Among 624,237 Korean adults with T2D, body weight variability over a 5-year period was associated with a 58% higher risk of all-cause mortality, a 22% higher risk of stroke, and a 15% higher risk of myocardial infarction during a follow-up period of 7–8 years [59]. The results were unchanged after adjustment for traditional CVD risk factors, and were observed in all age groups and both sexes. Higher mortality risk was observed in individuals with low and high BMI, although the HR was higher for BMI 25 kg/ (53%) compared to BMI 25 kg/ (36%). The higher mortality risk associated with weight variability was also significant (and similar) among individuals who experienced a weight loss of 5%, weight gain of 5%, or had a weight change of 5% during the 5-year period in which body weights were measured. These results indicate that body weight trajectory during the study did not affect adverse outcomes associated with weight cycling.
In a study of 1319 patients with T2D in the Verona Diabetes Study [60], variability in BMI during a 3-year period was associated with a 34% higher risk of mortality during a 10-year follow-up in adults ages 65 years, but was not associated with significantly higher mortality in adults 65 years (HR = 1.16, 95% CI, 0.72–1.86).
Among 29,316 adults with T2D in Scotland [58], weight variability based on multiple measurements over a 5-year period was associated with increased risk of all-cause mortality, myocardial infarction, and congestive heart failure during a mean follow-up of 5.2 years. Risk increased with higher degrees of weight variability. For example, the all-cause mortality HR for the subjects in the quartile with the highest coefficient of variation (CV) of body weight was 2.49 (95% CI, 1.68–3.68) compared to the quartile with the lowest CV of body weight. For congestive heart failure, quartiles 2–4 all had significantly increased risk (68%–123% higher) compared with the referent group with the lowest CV in body weight.
In the Swedish National Diabetes Register [61], which included 100,576 adults with T2D, increasing body weight variability over a 3-year period was associated with a 45% higher risk of the primary outcome (non-fatal MI or stroke; all-cause mortality) during a subsequent 5-year follow-up. For the highest quartile of body weight variability, all-cause mortality risk was 68% higher compared to the quartile with the lowest body weight variability.
The Look AHEAD trial reported that weight fluctuation was associated with increased mortality risk in the control group but not the intensive lifestyle intervention group [55]. In the control group, participants in the highest quartile of CV of BMI had a 4.06-fold greater risk of all-cause mortality, a 15.28-fold higher risk of CVD mortality, and a 2.16-fold higher risk of cardiovascular events. The highest quartile of CV for waist circumference (WC) was also significantly associated with a 1.84-fold higher risk of all-cause mortality and a 6.46-fold higher risk of CVD mortality. By contrast, CV for BMI and WC were not associated with higher risk for any outcome measure in the intervention group. The authors speculated that the lack of association in the intervention group could possibly be attributed to the exercise component of the intervention. Even partial weight regain after weight-loss interventions has been shown to result in reversal of cardiometabolic improvements that occurred during the weight-loss intervention [65], and exercise during a period of controlled weight regain can counter the adverse effects of weight regain on cardiometabolic risk markers [66, 67]. It is also worth noting that accumulation of visceral abdominal fat following liposuction can be entirely eliminated by exercise training [68]. Thus it is possible that the exercise component of the Look AHEAD intensive lifestyle intervention helped offset the deleterious impact of multiple episodes of weight regain following weight loss that could have occurred during the 6.7 years of follow-up.
The mechanisms underlying the higher risk associated with weight cycling are not well understood, although fluctuations in CVD risk factors, which could accompany repeated cycles of weight loss/weight gain, have been shown to be associated with higher mortality risk, especially CVD mortality [14, 31, 32]. Weight fluctuation is associated with increased risk of hyperinsulinemia and insulin resistance, elevated blood glucose and glycemic variability, dyslipidemia, and hypertension [14, 15, 31, 32, 69]. All of these could help explain the elevated risk of adverse CVD outcomes associated with weight cycling (Fig. 2).
In addition to the increased risk of mortality and adverse CVD outcomes associated with weight cycling, it is important to note that weight cycling is also associated with T2D incidence. Two meta-analyses indicated that weight cycling was associated with a 21% [19] and 33% [70] higher risk of T2D incidence. Additionally, among 6 million Korean adults, weight cycling was associated with a 26.3% higher risk of T2D and a 17.5% higher risk of hypertension [71]. Thus, in addition to increasing mortality risk among individuals with T2D, weight cycling may also increase risk of developing the disease.
A limitation of the studies on weight cycling is that weight loss intention was not assessed, and unintentional weight loss is more frequently associated with higher mortality risk compared with intentional weight loss [72]. However, given the high prevalence of weight loss attempts worldwide, and the fact that weight loss is routinely recommended for individuals with T2D and obesity, it is plausible that much of the weight cycling is a result of intentional weight loss attempts that inevitably lead to weight regain [8, 9, 10].
4. Obesity, T2D, and Mortality: Paradox, or Not?
The relationship between BMI and mortality is complex, and is influenced by fitness and physical activity [4, 37, 73]. An obesity paradox has been demonstrated for numerous chronic health conditions, in which lowest mortality is typically observed in individuals with BMI 25 kg/. With no exceptions, seven meta-analyses have documented the existence of an obesity paradox in T2D, with lowest mortality risk associated with BMI in the range of ~25–35 kg/ [24, 25, 26, 27, 28, 29, 30]. Reasons for the obesity paradox remain obscure, but it is worth noting that among healthy adults, some studies [74, 75, 76], including meta-analyses [21, 77, 78, 79], have shown that the lowest mortality risk in apparently healthy populations is in a similar BMI range as that associated with lowest mortality in adults with T2D. Thus, the relatively lower mortality risk associated with overweight and moderate obesity in T2D, as is consistently shown in meta-analyses, may not be all that paradoxical. Accordingly, Flegal and Ioannidis [80] recommended that the term “obesity paradox” be abandoned because it has no precise definition and that labeling counterintuitive findings a paradox adds no value.
It is also important to note that none of the cohort studies used in these meta-analyses included any measure of CRF, which is strongly inversely associated with mortality risk across all BMI strata in patients with T2D [33, 34, 35]. In the Henry Ford Exercise Testing Project (FIT Project), which included 8528 patients with T2D, after a 10-year mean follow-up, subjects with obesity had a 30% lower mortality rate compared to patients with BMI 25 kg/. This was most evident among patients with the lowest CRF. Within each BMI group, there was a strong inverse association between CRF and mortality rate. Overall, compared to those in the lowest category of CRF (6 METs), those with higher CRF (6–9.9 METs) had a ~50% lower mortality rate and those with the highest levels of CRF (10 METs) had a 70% lower mortality rate. The lowest mortality rate was observed among individuals with BMI 30 kg/ and high CRF (10 METs). In this cohort, the lower mortality associated with CRF was independent of CVD risk factors, including hypertension, hyperlipidemia, diabetes, and smoking. In fact, an individual with a CRF 10 METs and 3 CVD risk factors had ~60% lower mortality rate compared to an individual with zero risk factors but a CRF 6 METs. These results highlight the importance of CRF, and especially of maintaining moderate-to-high CRF even in the presence of multiple CVD risk factors. The results also suggest that the absence of traditional CVD risk factors does not confer mortality benefit among individuals with T2D and low CRF.
The Look AHEAD trial is also instructive with regard to the associations between CRF, BMI, and mortality in adults with T2D and BMI 25 kg/. In a secondary analysis of 4773 adults, ages 45–76 years, after a mean follow-up of 9.2 years, all-cause mortality rate was 30% lower per SD higher MET level (1 MET = 3.5 mL /kg/min). Also, for each SD higher MET level, CVD mortality was reduced by 55%, and a composite CV outcome was reduced by 28% [81]. These reductions were evident with and without BMI in basic multivariate model. By contrast, when adjusted for CRF, BMI was not associated with all-cause or CVD mortality, or higher risk of MI, stroke, angina, or heart failure. In fact, BMI was protective from stroke, MI and composite CVD outcomes when adjusted for CRF.
5. Fitness, Physical Activity, Sedentary Behavior, and Prevention of T2D
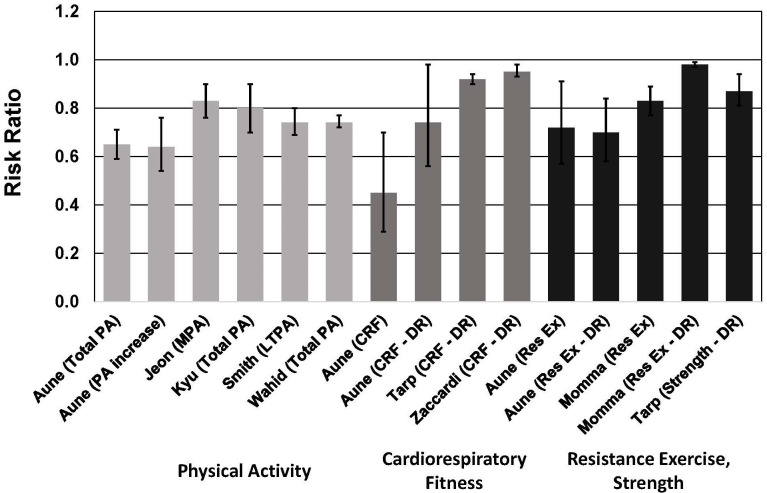
Five meta-analyses have been published on the association between PA and risk of T2D. These meta-analyses consistently show lower risk associated with higher PA, with the highest PA levels corresponding to a 13% to 35% lower risk of T2D [82, 83, 84, 85, 86] (Fig. 4). These meta-analyses included data from 67 publications (not including duplications), with a total of ~2,160,445 men and women. Most of the cohorts were from the United States, China, Japan, South Korea, Australia, and 11 European countries. In two of the meta-analyses [82, 83], all of the included studies (59 of the 67 total across all five meta-analyses) were judged to have scores of 7–9 (high quality) on the 9-point Newcastle-Ottawa Scale (NOS) for quality assessment [87]. In one meta-analysis [84], 17 of 28 studies had NOS scores 7, and only 1 had a score 4. In the smallest meta-analysis [85], with only 3 studies, 2 had NOS scores 7 and 1 had a score of 4. One meta-analysis did not report whether the authors rated the quality of studies [86], but all of the studies included in this meta-analysis were also included in one or more of the other four meta-analyses. Thus, most of the studies included in these meta-analyses were assessed as high quality. Heterogeneity was only significant in one of the meta-analyses [84]. It is important to note that all of the 27 relative risks included in this meta-analysis were 1.0, with heterogeneity largely due to the large range in differences in relative risks (0.34 to 0.96). Significant publication bias was evident in two of the meta-analyses [82, 83].
Fig. 4.
Meta-analyses of cohort studies on the association between risk of type 2 diabetes and physical activity, cardiorespiratory fitness, resistance exercise and muscular strength. See text for description of meta-analyses. Vertical bars = 95% confidence intervals. PA, physical activity; MPA, moderate-intensity physical activity; LTPA, leisure time physical activity; CRF, cardiorespiratory fitness; Res Ex, resistance exercise; DR, dose-response. In Aune et al. [82], DR = per 20 mL /kg/min (~5.7 METs) for CRF and per 5 hours/week of resistance exercise; in Tarp et al. [39] and Zaccardi et al. [36], DR = per 1 MET (3.5 mL /kg/min) higher cardiorespiratory fitness; in Momma et al. [89], DR = per 10 min/week of resistance exercise training; in Tarp et al. [39], DR = per 1 standard deviation in muscular strength.
Four of these meta-analyses demonstrated nonlinear dose-response associations, with steeper risk reductions associated with lower levels of PA [82, 83, 84, 85]. In two meta-analyses, PA equal to 11.25 MET-hour/week was associated with a 26% lower risk of T2D [84, 85]. This amount of PA corresponds to ~150 min/week of moderate-intensity PA (e.g., for a 4.5-MET activity such as walking at ~3.5 mph). These observations are important because the majority of adults with T2D do not meet the minimum PA guidelines [88].
The results of one meta-analysis highlighted the importance of increasing PA from a baseline sedentary level. For individuals who increased their PA from a low level to a moderate or high level, risk of T2D was reduced by 36% [82]. This was comparable to the 41% lower risk for individuals who had a consistently high level of moderate-to-vigorous PA (MVPA).
In addition to PA, CRF [36, 39, 82] and MF [39, 82, 89] are also associated with lower risk of T2D (Fig. 4). These meta-analyses included data from 17 publications for CRF and 15 publications for MF (not including duplications), with a total of ~1.6 million men and women in the CRF studies and ~1.9 million men and women in the MF studies. The majority of these participants consisted of ~1.5 million male military conscripts from Sweden [90], and were included in only one of the meta-analyses [39]. Cohorts from the United States, Canada, Finland, Sweden, Denmark, England, Switzerland, and Japan were included, as well as 17 countries in the Prospective Urban Rural Epidemiology (PURE) study. In two of the three meta-analyses on CRF [36, 82], all of the included studies (13 of the 17 total across all three meta-analyses) were assigned NOS scores of 7. In the other meta-analysis [39], 4 of 10 studies were assigned NOS scores 7 and the other 6 studies had NOS scores of 5 or 6. All three of the meta-analyses reported significant heterogeneity [36, 39, 82]. However, this was largely due to the wide range in relative risks reported (0.09 to 1.02), and it is important to note that all but 1 of the relative risks in these 17 studies were 1.0. Significant publication bias was evident in only one of the meta-analyses [82], and that was due to 1 study.
For CRF, each 1-MET (3.5 mL/kg/min) higher level of CRF was associated with a ~5%–8% lower risk of T2D [36, 39, 82]. The risk reduction estimates in these meta-analyses included adjustments for BMI. In support of these observations are results from the Coronary Artery Risk Development in Young Adults cohort, which indicated that a decrease in CRF over a 7-year period was associated with a 22% higher risk of T2D in women and a 45% higher risk of T2D in men during the 20 years of the study [91]. These findings highlight the importance of CRF for reducing risk of T2D, and are consistent with the finding that CRF is positively correlated with pancreatic beta cell function, independent of fatness in individuals with the metabolic syndrome [92].
For the meta-analyses on MF, one reported that all included studies had NOS scores 7 [82], one reported that 4 studies had NOS scores 7 and 6 studies had NOS scores between 4–6 [39], and one reported that all 5 studies included in the meta-analysis had NOS scores between 4–6 [89]. Only one of the meta-analyses reported significant heterogeneity [39], and none reported significant publication bias.
Three meta-analyses demonstrated that muscular strength was associated with a 13%–28% lower risk of T2D [39, 82, 89]. In categorical analyses, the highest strength group had a 17%–28% lower risk of T2D [82, 89]. In dose-response analyses, each 1-SD increase in muscular strength was associated with a 13% lower risk of T2D [39], and each 10 min/week of strengthening exercises was associated with a 2% lower risk of T2D [89]. In the latter dose-response study, risk decreased markedly until about 60 min/week of strengthening exercises.
On the opposite end of the PA continuum, it has also been shown that sedentary behavior, such as sitting time and watching television, increases risk of T2D [93, 94, 95, 96]. Although PA attenuates this relationship, sitting time and sedentary behavior are significantly associated with T2D risk independent of PA [93, 95]. A meta-analysis of 5 cohort studies indicated that, compared to the group with the lowest amount of sitting time, individuals with the highest amount of daily sitting time had a 13% higher risk of T2D [93]. Even when adjusting for PA, a high amount of daily sitting was associated with a 10% higher T2D risk. In another meta-analysis of 5 studies, the highest amount of total daily sedentary time was associated with a 91% higher risk of T2D [94]. Thus, reducing risk of T2D requires both increasing PA and fitness, as well as reducing time spent in sedentary activities.
It must be acknowledged that intensive lifestyle interventions accompanied by significant weight loss have also been documented to reduce T2D incidence [3]. However, when looking at the various intensive lifestyle interventions to prevent T2D, it is not apparent that significant weight loss is obligatory to achieve benefit. In a systematic review and meta-analysis of 7 large lifestyle interventions, T2D risk reduction across all interventions were similar, ranging between 48% and 57%, yet weight reduction among the studies varied considerably, with some of interventions showing minimal, if any, weight loss [3].
6. Increasing Physical Activity and Fitness to Reduce Mortality Risk in T2D
PA [97, 98, 99, 100], CRF [101, 102], and MF [103, 104, 105, 106] are all inversely associated with all-cause and CVD mortality, and these associations are independent of BMI. Among individuals with T2D, data from three meta-analyses demonstrate that higher PA is associated with lower all-cause mortality risk [107, 108, 109] (Fig. 5, Ref. [107, 108]). These meta-analyses included data from 20 publications (not including duplications), with a total of 47,467 men and women. The cohorts were from the United States, Japan, and 11 European countries. Only one of the meta-analyses assessed study quality with the NOS [109], in which 8 of the 12 included studies were assigned a score of 7, and 4 were assigned a score of 6. One meta-analysis did not report quality assessment [108], and one [107] used the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach to assess certainty of evidence [110]. This meta-analysis of 6 studies graded the certainty of evidence as “low”. All three meta-analyses reported significant heterogeneity. Only one of the meta-analyses reported evidence of publication bias [108]. As discussed above, the significant heterogeneity was attributable to the large range of relative risks for lower mortality risk associated with higher CRF, with all but 1 of the studies reporting a relative risk 1.0.
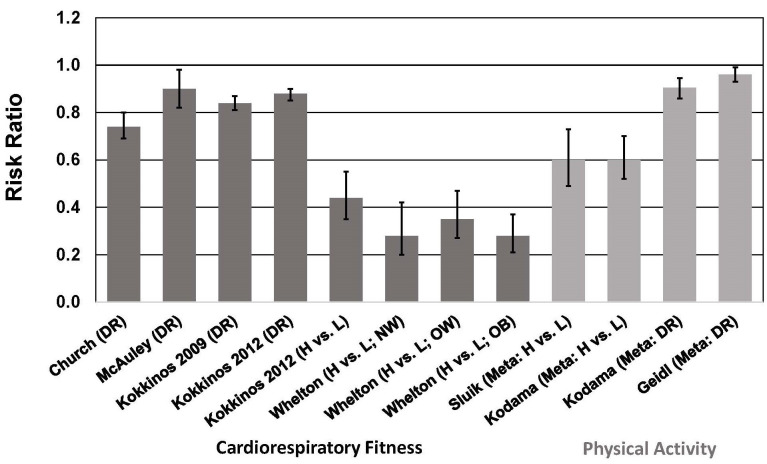
Fig. 5.
Association between cardiorespiratory fitness (cohort studies) and physical activity (meta-analyses) and all-cause mortality risk in individuals with type 2 diabetes. See text for description of studies. Vertical bars = 95% confidence intervals. ACM, all-cause mortality; DR, dose-response; H, highest category of CRF or PA; L, Lowest category of CRF or PA; Meta, meta-analysis; NW, normal weight, BMI = 18.5–25 kg/; OW, overweight, BMI = 25–30 kg/; OB, obese, BMI 30 kg/. In all CRF studies, DR = per 1 MET (3.5 mL /kg/min) higher CRF. In Kodama et al. [108], DR = per 1 MET-hour/day higher PA level; in Geidl et al. [107], DR = per 10 MET-hour/week higher PA level.
In meta-analyses that included a total of 12 cohort studies of individuals with T2D, total PA, leisure-time PA, and walking were associated with a ~40% lower risk of all-cause and CVD mortality when comparing highest vs. lowest categories of PA [109] (Fig. 5). These risk reductions are similar to those reported in another meta-analysis showing a 40% lower risk of all-cause mortality (13 studies) when comparing highest vs. lowest categories of PA [108]. In a dose-response analysis, this study showed that each 1 MET-hour/day (~70–140 min/week of moderate-intensity PA, depending on MET level) increase in PA was associated with a 9.5% lower risk of all-cause mortality (Fig. 5). This meta-analysis also showed a 29% lower risk of CVD risk when comparing highest vs. lowest categories of PA, and a 7.9% lower risk of CVD per 1 MET-hour/day increase in PA in a dose-response analysis [108]. A more recent dose-response meta-analysis indicated that each 10 MET-hour/week (~100–200 min/week of moderate-intensity PA, depending on MET level) increase in PA was associated with a 4% lower risk of all-cause mortality [107]. The reason for the marked difference in risk reduction between the two dose-response meta-analyses is not apparent. The more recent meta-analysis included only 6 studies (3 of which were not included in the earlier meta-analysis), which makes comparisons difficult.
No meta-analyses have been published on the association between CRF and mortality in patients with T2D. However, several cohort studies have been published to confirm this association in T2D, and that the inverse association between CRF and mortality is independent of BMI [33, 34, 35, 40, 41]. Among men with T2D in the Aerobics Center Longitudinal Study [40], male veterans with T2D [33, 34, 35], and men and women in the Henry Ford Exercise Testing Project [41], higher CRF was associated with lower risk of all-cause mortality, and this association was observed in all BMI strata. Each 1-MET increase in CRF was associated with a 10%–18% survival benefit [33, 34, 35], which is comparable to the 11% lower all-cause mortality risk associated with a 1-MET higher CRF level reported in a recent meta-analysis of 37 cohort studies involving more than 2.2 million participants [111].
These data from cohort studies based on single point assessments of PA or CRF suggest that increasing PA and/or CRF would reduce mortality risk in individuals with T2D. Abundant evidence in healthy populations shows that increasing PA [112, 113, 114, 115, 116, 117, 118, 119] or improving CRF [120, 121, 122, 123, 124, 125, 126, 127] (determined by 2 or more assessments over time) is associated with reduced risk of all-cause and CVD mortality. Risk reductions for increasing PA are in the range of 15%–50% [4], whereas those associated with improvements in CRF are even greater. Moving from “low fit” to a higher fitness category is associated with a 30%–60% reduction in mortality risk [4], and in dose-response analyses, each 1-MET increase in CRF is associated with a 14%–29% reduction in all-cause mortality [4].
Unfortunately, there are limited data on individuals with T2D with regard to mortality risk reductions associated with either increasing PA or improving CRF. Among persons with T2D in the European Prospective Investigation into Cancer and Nutrition Study, changes in cycling behavior was associated with mortality risk [128]. Information on PA and cycling behavior was obtained at two time periods, 5 years apart. Compared with people who reported no cycling at baseline, during a mean follow-up of 7.7 years, those who took up cycling experienced a 35% lower risk of all-cause mortality and a 51% lower risk of CVD mortality. These risk reductions were independent of other PA. These results are consistent with previous reports showing that PA is associated with lower mortality rates in T2D [107, 108, 109]. These results on individuals with T2D are similar to those from a study of Danish adults which showed that taking up cycling was associated with a 22% lower risk of all-cause mortality during a follow-up of ~10–13 years [116]. It is worth noting that in this Danish population, cycling was not associated with weight loss or a reduction in the incidence of overweight or obesity during the follow-up [129].
The reduced mortality rate in persons with T2D who have high levels of PA and/or CRF could be due to many factors, including improved vascular endothelial function [130, 131, 132], reductions in visceral abdominal and ectopic fat [133, 134], and molecular adaptations in fat cells that improve “metabolic fitness” of adipose tissue [135, 136, 137]. These exercise-induced adaptations occur with little, if any, loss of total body fat [4]. Lower mortality risk in physically active persons with T2D may also be attributable in part to the beneficial effect of exercise on heart rate variability (HRV) [138]. Low HRV is associated with increased mortality risk [139], and HRV is reduced in patients with T2D [140]. A systematic review of 15 exercise intervention studies in patients with T2D showed that exercise training increased HRV [138]. Risk reduction may also be attributable to improvements in CVD risk factors, as described in the next section.
7. Exercise Training, Weight Loss, and CVD Risk Factors
Weight loss is associated with improvements in risk factors for CVD and T2D, as consistently documented in meta-analyses of RCTs [141, 142, 143, 144, 145, 146, 147, 148]. Weight loss in these studies was typically achieved by energy-restriction, either alone or in combination with exercise, and in one meta-analysis by medication [143]. Thus it is difficult to distinguish whether the improvements in risk factors are attributable to weight loss per se, or to changes in diet quality and/or exercise. As discussed below, improvements in CVD risk factors with exercise training are similar in magnitude to those reported in weight loss studies.
Weight loss interventions have been shown to reduce HbA1c by ~0.2% to 0.9% [141, 144, 147]. These reductions are similar to the reductions of ~0.2%–0.8% reported for exercise intervention studies [149, 150, 151, 152]. In the exercise RCTs, it is unlikely that weight loss accounted for the reductions in HbA1c because either weight loss did not occur with exercise training [149] or the magnitude of weight loss with exercise training was unrelated to the magnitude of reduction in HbA1c [152].
Increases in blood concentrations of high-density lipoprotein cholesterol with exercise training (2–5 mg/dL) [153, 154, 155, 156, 157] are comparable to those for weight loss interventions (1–4 mg/dL) [141, 142, 143, 144, 148], and reductions in low-density lipoprotein cholesterol for exercise training (3–10 mg/dL) [153, 155, 158] are similar to those reported for weight loss interventions (1–15 mg/dL) [141, 142, 143, 147, 148]. Reductions in blood triglyceride concentrations tend to be greater with weight loss interventions (11–58 mg/dL) [141, 147, 148] compared to exercise training (5–26 mg/dL) [153, 155, 157, 159].
Systolic and diastolic blood pressure reductions with exercise training (2–5 mmHg) [160, 161, 162, 163, 164, 165] are also similar to those reported in weight loss studies (1–5 mmHg) [141, 143, 144, 145, 146, 147]. Even though some weight loss may occur with exercise training, correlations between changes in blood pressures and body weight are 0.10 [166].
As mentioned above, these results must be interpreted with caution because the weight loss studies used diet and/or exercise in combination, or weight loss medications. Since diet alone and exercise alone can improve CVD risk factors in the absence of weight loss [4, 5], conclusions about the independent effects of weight loss must be considered in this context.
8. Summary and Conclusions
Prevalence of obesity and incidence of T2D have increased steadily during the past 40 years, and are projected to increase further in the next few decades. Although weight loss remains the cornerstone of treatment, empirical evidence strongly suggests that weight loss strategies have been largely ineffective in the long-term because obesity prevalence continues to grow despite an ever-increasing number of weight loss attempts. Moreover, despite documented improvements in cardiometabolic risk factors with weight loss, clear evidence for a survival benefit associated with intentional weight loss in patients with T2D is lacking. This may be due in large part to higher mortality risk associated with weight cycling in this population. Body weight fluctuation can lead to CVD risk factor variability, and both are associated with adverse cardiovascular outcomes. Higher all-cause mortality and CVD morbidity associated with weight cycling in patients with T2D was consistent across all studies, especially CVD morbidity. Further complicating the issue is the consistent finding of lower mortality risk associated with higher BMI in individuals with T2D. These observations present a conundrum for treatment and prevention strategies that focus primarily on weight loss.
Exercise training interventions typically improve cardiometabolic risk factors by a magnitude comparable to that shown in weight-loss interventions. Even more importantly, PA and CRF are consistently and strongly associated with lower T2D incidence and mortality among those with obesity and T2D. Thus, focusing on increasing PA and improving fitness (both cardiorespiratory and muscular) might be a more straightforward approach to prevention and treatment of T2D. Because dose-response studies show that the steepest risk reductions for T2D are observed when sedentary, low-fit individuals become more active, even modest increases in PA and fitness could have considerable impact in reducing morbidity and mortality risk. A focus on increasing PA and improving fitness, without a specific weight loss target, may also help to minimize weight cycling associated sequelae.
Acknowledgment
Not applicable.
Footnotes
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author Contributions
GAG is the sole author and is responsible for conceptualization; content design; writing original draft; review and editing; approval of the published version of the manuscript.
Ethics Approval and Consent to Participate
Not applicable.
Funding
This research received no external funding.
Conflict of Interest
The author declares no conflict of interest.
References
- [1].World Health Organization Cardiovascular Diseases (CVDs) 2021. [(Accessed: 25 May 2022)]. Available at: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- [2].Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Research and Clinical Practice . 2019;157:107843. doi: 10.1016/j.diabres.2019.107843. [DOI] [PubMed] [Google Scholar]
- [3].Uusitupa M, Khan TA, Viguiliouk E, Kahleova H, Rivellese AA, Hermansen K, et al. Prevention of Type 2 Diabetes by Lifestyle Changes: A Systematic Review and Meta-Nnalysis. Nutrients . 2019;11:2611. doi: 10.3390/nu11112611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gaesser GA, Angadi SS. Obesity treatment: Weight loss versus increasing fitness and physical activity for reducing health risks. iScience . 2021;24:102995. doi: 10.1016/j.isci.2021.102995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Gaesser GA, Angadi SS, Sawyer BJ. Exercise and diet, independent of weight loss, improve cardiometabolic risk profile in overweight and obese individuals. The Physician and Sportsmedicine . 2011;39:87–97. doi: 10.3810/psm.2011.05.1898. [DOI] [PubMed] [Google Scholar]
- [6].Ross R, Blair S, de Lannoy L, Després J-P, Lavie CJ. Changing the endpoints for determining effective obesity management. Progress in Cardiovascular Diseases . 2015;57:330–336. doi: 10.1016/j.pcad.2014.10.002. [DOI] [PubMed] [Google Scholar]
- [7].Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet . 2022;399:394–405. doi: 10.1016/S0140-6736(21)01919-X. [DOI] [PubMed] [Google Scholar]
- [8].Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. The American Journal of Clinical Nutrition . 2001;74:579–584. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- [9].Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM. Meta-analysis: the effect of dietary counseling for weight loss. Annals of Internal Medicine . 2007;147:41–50. doi: 10.7326/0003-4819-147-1-200707030-00007. [DOI] [PubMed] [Google Scholar]
- [10].Sumithran P, Proietto J. The defence of body weight: a physiological basis for weight regain after weight loss. Clinical Science . 2013;124:231–241. doi: 10.1042/CS20120223. [DOI] [PubMed] [Google Scholar]
- [11].Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. The New England Journal of Medicine . 2017;377:13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hruby A, Hu FB. The Epidemiology of Obesity: a Big Picture. PharmacoEconomics . 2015;33:673–689. doi: 10.1007/s40273-014-0243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Martin CB, Herrick KA, Sarafrazi N, Ogden CL. Attempts to Lose Weight Among Adults in the United States, 2013–2016. NCHS Data Brief . 2018:1–8. [PubMed] [Google Scholar]
- [14].Montani J-, Schutz Y, Dulloo AG. Dieting and weight cycling as risk factors for cardiometabolic diseases: who is really at risk. Obesity Reviews . 2015;16:7–18. doi: 10.1111/obr.12251. [DOI] [PubMed] [Google Scholar]
- [15].Montani JP, Viecelli AK, Prevot A, Dulloo AG. Weight cycling during growth and beyond as a risk factor for later cardiovascular diseases: the ‘repeated overshoot’ theory. International Journal of Obesity . 2006;30:S58–S66. doi: 10.1038/sj.ijo.0803520. [DOI] [PubMed] [Google Scholar]
- [16].Strohacker K, Carpenter KC, McFarlin BK. Consequences of Weight Cycling: An Increase in Disease Risk. International Journal of Exercise Science . 2009;2:191–201. doi: 10.70252/ASAQ8961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cheng FW, Gao X, Jensen GL. Weight Change and All-Cause Mortality in Older Adults: A Meta-Analysis. Journal of Nutrition in Gerontology and Geriatrics . 2015;34:343–368. doi: 10.1080/21551197.2015.1090362. [DOI] [PubMed] [Google Scholar]
- [18].Zhang Y, Hou F, Li J, Yu H, Li L, Hu S, et al. The association between weight fluctuation and all-cause mortality: A systematic review and meta-analysis. Medicine . 2019;98:e17513. doi: 10.1097/MD.0000000000017513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Zou H, Yin P, Liu L, Liu W, Zhang Z, Yang Y, et al. Body-Weight Fluctuation Was Associated With Increased Risk for Cardiovascular Disease, All-Cause and Cardiovascular Mortality: A Systematic Review and Meta-Analysis. Frontiers in Endocrinology . 2019;10:728. doi: 10.3389/fendo.2019.00728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. British Medical Journal . 2016;353:i2156. doi: 10.1136/bmj.i2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. The Journal of the American Medical Association . 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Di Angelantonio E, Bhupathiraju Sh N, Wormser D, Gao P, Kaptoge S, Berrington de Gonzalez A, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet . 2016;388:776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Klein S, Gastaldelli A, Yki-Jarvinen H, Scherer PE. Why does obesity cause diabetes. Cell Metabolism . 2022;34:11–20. doi: 10.1016/j.cmet.2021.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Carnethon MR, De Chavez PJD, Biggs ML, Lewis CE, Pankow JS, Bertoni AG, et al. Association of Weight Status with Mortality in Adults with Incident Diabetes. The Journal of the American Medical Association . 2012;308:581–590. doi: 10.1001/jama.2012.9282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Chang H, Li Y, Hsieh C, Liu P, Lin G. Association of body mass index with all-cause mortality in patients with diabetes: a systemic review and meta-analysis. Cardiovascular Diagnosis and Therapy . 2016;6:109–119. doi: 10.21037/cdt.2015.12.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Gao F, Wang ZJ, Shen H, Yang SW, Nie B, Zhou YJ. Impact of obesity on mortality in patients with diabetes: Meta-analysis of 20 studies including 250,016 patients. Journal of Diabetes Investigation . 2018;9:44–54. doi: 10.1111/jdi.12677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kwon Y, Kim HJ, Park S, Park YG, Cho KH. Body Mass Index-Related Mortality in Patients with Type 2 Diabetes and Heterogeneity in Obesity Paradox Studies: A Dose-Response Meta-Analysis. PLoS ONE . 2017;12:e0168247. doi: 10.1371/journal.pone.0168247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Liu XM, Liu YJ, Zhan J, He QQ. Overweight, obesity and risk of all-cause and cardiovascular mortality in patients with type 2 diabetes mellitus: a dose-response meta-analysis of prospective cohort studies. European Journal of Epidemiology . 2015;30:35–45. doi: 10.1007/s10654-014-9973-5. [DOI] [PubMed] [Google Scholar]
- [29].Zaccardi F, Dhalwani NN, Papamargaritis D, Webb DR, Murphy GJ, Davies MJ, et al. Nonlinear association of BMI with all-cause and cardiovascular mortality in type 2 diabetes mellitus: a systematic review and meta-analysis of 414,587 participants in prospective studies. Diabetologia . 2017;60:240–248. doi: 10.1007/s00125-016-4162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Zhao Y, Qie R, Han M, Huang S, Wu X, Zhang Y, et al. Association of BMI with cardiovascular disease incidence and mortality in patients with type 2 diabetes mellitus: a systematic review and dose–response meta-analysis of cohort studies. Nutrition, Metabolism and Cardiovascular Diseases . 2021;31:1976–1984. doi: 10.1016/j.numecd.2021.03.003. [DOI] [PubMed] [Google Scholar]
- [31].Messerli FH, Hofstetter L, Rimoldi SF, Rexhaj E, Bangalore S. Risk Factor Variability and Cardiovascular Outcome: JACC Review Topic of the Week. Journal of the American College of Cardiology . 2019;73:2596–2603. doi: 10.1016/j.jacc.2019.02.063. [DOI] [PubMed] [Google Scholar]
- [32].Barnett MP, Bangalore S. Cardiovascular Risk Factors: It’s Time to Focus on Variability. Journal of Lipid and Atherosclerosis . 2020;9:255–267. doi: 10.12997/jla.2020.9.2.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kokkinos P, Myers J, Faselis C, Doumas M, Kheirbek R, Nylen E. BMI–Mortality Paradox and Fitness in African American and Caucasian Men with Type 2 Diabetes. Diabetes Care . 2012;35:1021–1027. doi: 10.2337/dc11-2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Kokkinos P, Myers J, Nylen E, Panagiotakos DB, Manolis A, Pittaras A, et al. Exercise Capacity and all-Cause Mortality in African American and Caucasian Men with Type 2 Diabetes. Diabetes Care . 2009;32:623–628. doi: 10.2337/dc08-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].McAuley PA, Myers JN, Abella JP, Tan SY, Froelicher VF. Exercise Capacity and Body Mass as Predictors of Mortality among Male Veterans with Type 2 Diabetes. Diabetes Care . 2007;30:1539–1543. doi: 10.2337/dc06-2397. [DOI] [PubMed] [Google Scholar]
- [36].Zaccardi F, O’Donovan G, Webb DR, Yates T, Kurl S, Khunti K, et al. Cardiorespiratory fitness and risk of type 2 diabetes mellitus: a 23-year cohort study and a meta-analysis of prospective studies. Atherosclerosis . 2015;243:131–137. doi: 10.1016/j.atherosclerosis.2015.09.016. [DOI] [PubMed] [Google Scholar]
- [37].Fogelholm M. Physical activity, fitness and fatness: relations to mortality, morbidity and disease risk factors. A systematic review. Obesity Reviews . 2010;11:202–221. doi: 10.1111/j.1467-789X.2009.00653.x. [DOI] [PubMed] [Google Scholar]
- [38].Lee D, Sui X, Church TS, Lee I-, Blair SN. Associations of Cardiorespiratory Fitness and Obesity with Risks of Impaired Fasting Glucose and Type 2 Diabetes in Men. Diabetes Care . 2009;32:257–262. doi: 10.2337/dc08-1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Tarp J, Støle AP, Blond K, Grøntved A. Cardiorespiratory fitness, muscular strength and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetologia . 2019;62:1129–1142. doi: 10.1007/s00125-019-4867-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Church TS, Cheng YJ, Earnest CP, Barlow CE, Gibbons LW, Priest EL, et al. Exercise Capacity and Body Composition as Predictors of Mortality among Men with Diabetes. Diabetes Care . 2004;27:83–88. doi: 10.2337/diacare.27.1.83. [DOI] [PubMed] [Google Scholar]
- [41].Whelton SP, McAuley PA, Dardari Z, Orimoloye OA, Brawner CA, Ehrman JK, et al. Association of BMI, Fitness, and Mortality in Patients with Diabetes: Evaluating the Obesity Paradox in the Henry Ford Exercise Testing Project (FIT Project) Cohort. Diabetes Care . 2020;43:677–682. doi: 10.2337/dc19-1673. [DOI] [PubMed] [Google Scholar]
- [42].Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Reports . 1985;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- [43].Ross R, Blair SN, Arena R, Church TS, Després J, Franklin BA, et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: a Case for Fitness as a Clinical Vital Sign: a Scientific Statement from the American Heart Association. Circulation . 2016;134:e653–e699. doi: 10.1161/CIR.0000000000000461. [DOI] [PubMed] [Google Scholar]
- [44].Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Medicine and Science in Sports and Exercise . 2009;41:459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- [45].Donnelly JE, Smith BK. Is exercise effective for weight loss with ad libitum diet? Energy balance, compensation, and gender differences. Exercise and Sport Sciences Reviews . 2005;33:169–174. doi: 10.1097/00003677-200510000-00004. [DOI] [PubMed] [Google Scholar]
- [46].Foright RM, Presby DM, Sherk VD, Kahn D, Checkley LA, Giles ED, et al. Is regular exercise an effective strategy for weight loss maintenance. Physiology and Behavior . 2018;188:86–93. doi: 10.1016/j.physbeh.2018.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Thorogood A, Mottillo S, Shimony A, Filion KB, Joseph L, Genest J, et al. Isolated Aerobic Exercise and Weight Loss: a Systematic Review and Meta-Analysis of Randomized Controlled Trials. The American Journal of Medicine . 2011;124:747–755. doi: 10.1016/j.amjmed.2011.02.037. [DOI] [PubMed] [Google Scholar]
- [48].Chen Y, Yang X, Wang J, Li Y, Ying D, Yuan H. Weight loss increases all-cause mortality in overweight or obese patients with diabetes: A meta-analysis. Medicine . 2018;97:e12075. doi: 10.1097/MD.0000000000012075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Williamson DF, Thompson TJ, Thun M, Flanders D, Pamuk E, Byers T. Intentional weight loss and mortality among overweight individuals with diabetes. Diabetes Care . 2000;23:1499–1504. doi: 10.2337/diacare.23.10.1499. [DOI] [PubMed] [Google Scholar]
- [50].Wing RR, Bolin P, Brancati FL, Bray GA, Clark JM, Coday M, et al. Cardiovascular Effects of Intensive Lifestyle Intervention in Type 2 Diabetes. New England Journal of Medicine . 2013;369:145–154. doi: 10.1056/NEJMoa1212914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Gregg EW, Gerzoff RB, Thompson TJ, Williamson DF. Trying to lose weight, losing weight, and 9-year mortality in overweight U.S. adults with diabetes. Diabetes Care . 2004;27:657–662. doi: 10.2337/diacare.27.3.657. [DOI] [PubMed] [Google Scholar]
- [52].Koster-Rasmussen R, Simonsen MK, Siersma V, Henriksen JE, Heitmann BL, de Fine Olivarius N. Intentional Weight Loss and Longevity in Overweight Patients with Type 2 Diabetes: A Population-Based Cohort Study. PLoS ONE . 2016;11:e0146889. doi: 10.1371/journal.pone.0146889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Bangalore S, Fayyad R, DeMicco DA, Colhoun HM, Waters DD. Body Weight Variability and Cardiovascular Outcomes in Patients with Type 2 Diabetes Mellitus. Circulation: Cardiovascular Quality and Outcomes . 2018;11:e004724. doi: 10.1161/CIRCOUTCOMES.118.004724. [DOI] [PubMed] [Google Scholar]
- [54].Kaze AD, Erqou S, Santhanam P, Bertoni AG, Ahima RS, Fonarow GC, et al. Variability of adiposity indices and incident heart failure among adults with type 2 diabetes. Cardiovascular Diabetology . 2022;21:16. doi: 10.1186/s12933-021-01440-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Kaze AD, Santhanam P, Erqou S, Ahima RS, Bertoni AG, Echouffo-Tcheugui JB. Body Weight Variability and Risk of Cardiovascular Outcomes and Death in the Context of Weight Loss Intervention among Patients with Type 2 Diabetes. JAMA Network Open . 2022;5:e220055. doi: 10.1001/jamanetworkopen.2022.0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Yeboah P, Hsu F, Bertoni AG, Yeboah J. Body Mass Index, Change in Weight, Body Weight Variability and Outcomes in Type 2 Diabetes Mellitus (from the ACCORD Trial) The American Journal of Cardiology . 2019;123:576–581. doi: 10.1016/j.amjcard.2018.11.016. [DOI] [PubMed] [Google Scholar]
- [57].Lee HJ, Choi EK, Han KD, Kim DH, Lee E, Lee SR, et al. High variability in bodyweight is associated with an increased risk of atrial fibrillation in patients with type 2 diabetes mellitus: a nationwide cohort study. Cardiovascular Diabetology . 2020;19:78. doi: 10.1186/s12933-020-01059-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Aucott LS, Philip S, Avenell A, Afolabi E, Sattar N, Wild S, et al. Patterns of weight change after the diagnosis of type 2 diabetes in Scotland and their relationship with glycaemic control, mortality and cardiovascular outcomes: a retrospective cohort study. BMJ Open . 2016;6:e010836. doi: 10.1136/bmjopen-2015-010836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Nam GE, Kim W, Han K, Lee C, Kwon Y, Han B, et al. Body Weight Variability and the Risk of Cardiovascular Outcomes and Mortality in Patients with Type 2 Diabetes: a Nationwide Cohort Study. Diabetes Care . 2020;43:2234–2241. doi: 10.2337/dc19-2552. [DOI] [PubMed] [Google Scholar]
- [60].Zoppini G, Verlato G, Targher G, Bonora E, Trombetta M, Muggeo M. Variability of body weight, pulse pressure and glycaemia strongly predict total mortality in elderly type 2 diabetic patients. The Verona Diabetes Study. Diabetes/Metabolism Research and Reviews . 2008;24:624–628. doi: 10.1002/dmrr.897. [DOI] [PubMed] [Google Scholar]
- [61].Ceriello A, Lucisano G, Prattichizzo F, Eliasson B, Franzen S, Svensson AM, et al. Variability in body weight and the risk of cardiovascular complications in type 2 diabetes: results from the Swedish National Diabetes Register. Cardiovascular Diabetology . 2021;20:173. doi: 10.1186/s12933-021-01360-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Huang S, Shi K, Ren Y, Wang J, Yan WF, Qian WL, et al. Association of magnitude of weight loss and weight variability with mortality and major cardiovascular events among individuals with type 2 diabetes mellitus: a systematic review and meta-analysis. Cardiovascular Diabetology . 2022;21:78. doi: 10.1186/s12933-022-01503-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Fildes A, Charlton J, Rudisill C, Littlejohns P, Prevost AT, Gulliford MC. Probability of an Obese Person Attaining Normal Body Weight: Cohort Study Using Electronic Health Records. American Journal of Public Health . 2015;105:e54–e59. doi: 10.2105/AJPH.2015.302773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Syngal S, Coakley EH, Willett WC, Byers T, Williamson DF, Colditz GA. Long-term weight patterns and risk for cholecystectomy in women. Annals of Internal Medicine . 1999;130:471–477. doi: 10.7326/0003-4819-130-6-199903160-00003. [DOI] [PubMed] [Google Scholar]
- [65].Kroeger CM, Hoddy KK, Varady KA. Impact of Weight Regain on Metabolic Disease Risk: a Review of Human Trials. Journal of Obesity . 2014;2014:614519. doi: 10.1155/2014/614519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Thomas TR, Warner SO, Dellsperger KC, Hinton PS, Whaley-Connell AT, Rector RS, et al. Exercise and the metabolic syndrome with weight regain. Journal of Applied Physiology . 2010;109:3–10. doi: 10.1152/japplphysiol.01361.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Warner SO, Linden MA, Liu Y, Harvey BR, Thyfault JP, Whaley-Connell AT, et al. The effects of resistance training on metabolic health with weight regain. Journal of Clinical Hypertension . 2010;12:64–72. doi: 10.1111/j.1751-7176.2009.00209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Benatti F, Solis M, Artioli G, Montag E, Painelli V, Saito F, et al. Liposuction induces a compensatory increase of visceral fat which is effectively counteracted by physical activity: a randomized trial. The Journal of Clinical Endocrinology and Metabolism . 2012;97:2388–2395. doi: 10.1210/jc.2012-1012. [DOI] [PubMed] [Google Scholar]
- [69].Rhee E. Weight Cycling and its Cardiometabolic Impact. Journal of Obesity and Metabolic Syndrome . 2017;26:237–242. doi: 10.7570/jomes.2017.26.4.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Kodama S, Fujihara K, Ishiguro H, Horikawa C, Ohara N, Yachi Y, et al. Unstable bodyweight and incident type 2 diabetes mellitus: a meta-analysis. Journal of Diabetes Investigation . 2017;8:501–509. doi: 10.1111/jdi.12623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Kim SH, Kwak JS, Kim SP, Choi SH, Yoon HJ. The association between diabetes and hypertension with the number and extent of weight cycles determined from 6 million participants. Scientific Reports . 2022;12:5235. doi: 10.1038/s41598-022-09221-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Harrington M, Gibson S, Cottrell RC. A review and meta-analysis of the effect of weight loss on all-cause mortality risk. Nutrition Research Reviews . 2009;22:93–108. doi: 10.1017/S0954422409990035. [DOI] [PubMed] [Google Scholar]
- [73].Lavie CJ, Carbone S, Kachur S, OʼKeefe EL, Elagizi A. Effects of Physical Activity, Exercise, and Fitness on Obesity-Related Morbidity and Mortality. Current Sports Medicine Reports . 2019;18:292–298. doi: 10.1249/JSR.0000000000000623. [DOI] [PubMed] [Google Scholar]
- [74].Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. The Journal of the American Medical Association . 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- [75].Fontaine KR, McCubrey R, Mehta T, Pajewski NM, Keith SW, Bangalore SS, et al. Body mass index and mortality rate among Hispanic adults: a pooled analysis of multiple epidemiologic data sets. International Journal of Obesity . 2012;36:1121–1126. doi: 10.1038/ijo.2011.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Yi S, Ohrr H, Shin S, Yi J. Sex-age-specific association of body mass index with all-cause mortality among 12.8 million Korean adults: a prospective cohort study. International Journal of Epidemiology . 2015;44:1696–1705. doi: 10.1093/ije/dyv138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].McGee DL, Diverse Populations Collaborations Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Annals of Epidemiology . 2005;15:87–97. doi: 10.1016/j.annepidem.2004.05.012. [DOI] [PubMed] [Google Scholar]
- [78].Winter JE, MacInnis RJ, Nowson CA. The Influence of Age the BMI and All-Cause Mortality Association: A Meta-Analysis. The Journal of Nutrition, Health & Aging . 2017;21:1254–1258. doi: 10.1007/s12603-016-0837-4. [DOI] [PubMed] [Google Scholar]
- [79].Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA. BMI and all-cause mortality in older adults: a meta-analysis. The American Journal of Clinical Nutrition . 2014;99:875–890. doi: 10.3945/ajcn.113.068122. [DOI] [PubMed] [Google Scholar]
- [80].Flegal KM, Ioannidis JPA. The Obesity Paradox: a Misleading Term that should be Abandoned. Obesity . 2018;26:629–630. doi: 10.1002/oby.22140. [DOI] [PubMed] [Google Scholar]
- [81].Wills AC, Vazquez Arreola E, Olaiya MT, Curtis JM, Hellgren MI, Hanson RL, et al. Cardiorespiratory Fitness, BMI, Mortality, and Cardiovascular Disease in Adults with Overweight/Obesity and Type 2 Diabetes. Medicine and Science in Sports and Exercise . 2022;54:994–1001. doi: 10.1249/MSS.0000000000002873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Aune D, Norat T, Leitzmann M, Tonstad S, Vatten LJ. Physical activity and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis. European Journal of Epidemiology . 2015;30:529–542. doi: 10.1007/s10654-015-0056-z. [DOI] [PubMed] [Google Scholar]
- [83].Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. British Medical Journal . 2016;354:i3857. doi: 10.1136/bmj.i3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Smith AD, Crippa A, Woodcock J, Brage S. Physical activity and incident type 2 diabetes mellitus: a systematic review and dose–response meta-analysis of prospective cohort studies. Diabetologia . 2016;59:2527–2545. doi: 10.1007/s00125-016-4079-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Wahid A, Manek N, Nichols M, Kelly P, Foster C, Webster P, et al. Quantifying the Association between Physical Activity and Cardiovascular Disease and Diabetes: a Systematic Review and Meta‐Analysis. Journal of the American Heart Association . 2016;5 doi: 10.1161/JAHA.115.002495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical Activity of Moderate Intensity and Risk of Type 2 Diabetes: a systematic review. Diabetes Care . 2007;30:744–752. doi: 10.2337/dc06-1842. [DOI] [PubMed] [Google Scholar]
- [87].Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute. 2011. [(Accessed: 25 July 2022)]. Available at: https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp.
- [88].Morrato EH, Hill JO, Wyatt HR, Ghushchyan V, Sullivan PW. Physical Activity in U.S. Adults with Diabetes and at Risk for Developing Diabetes, 2003. Diabetes Care . 2007;30:203–209. doi: 10.2337/dc06-1128. [DOI] [PubMed] [Google Scholar]
- [89].Momma H, Kawakami R, Honda T, Sawada SS. Muscle-strengthening activities are associated with lower risk and mortality in major non-communicable diseases: a systematic review and meta-analysis of cohort studies. British Journal of Sports Medicine . 2022;56:755–763. doi: 10.1136/bjsports-2021-105061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Crump C, Sundquist J, Winkleby MA, Sieh W, Sundquist K. Physical Fitness among Swedish Military Conscripts and Long-Term Risk for Type 2 Diabetes Mellitus: A Cohort Study. Annals of Internal Medicine . 2016;164:577–584. doi: 10.7326/M15-2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Carnethon MR, Sternfeld B, Schreiner PJ, Jacobs DR, Lewis CE, Liu K, et al. Association of 20-Year Changes in Cardiorespiratory Fitness with Incident Type 2 Diabetes: the coronary artery risk development in young adults (CARDIA) fitness study. Diabetes Care . 2009;32:1284–1288. doi: 10.2337/dc08-1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Ramos JS, Dalleck LC, Borrani F, Fassett RG, Coombes JS. Cardiorespiratory fitness is positively associated with increased pancreatic beta cell function independent of fatness in individuals with the metabolic syndrome: Fitness versus fatness. Journal of Science and Medicine in Sport . 2017;20:45–49. doi: 10.1016/j.jsams.2016.04.007. [DOI] [PubMed] [Google Scholar]
- [93].Bailey DP, Hewson DJ, Champion RB, Sayegh SM. Sitting Time and Risk of Cardiovascular Disease and Diabetes: a Systematic Review and Meta-Analysis. American Journal of Preventive Medicine . 2019;57:408–416. doi: 10.1016/j.amepre.2019.04.015. [DOI] [PubMed] [Google Scholar]
- [94].Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary Time and its Association with Risk for Disease Incidence, Mortality, and Hospitalization in Adults: a systematic review and meta-analysis. Annals of Internal Medicine . 2015;162:123–132. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- [95].Patterson R, McNamara E, Tainio M, de Sá TH, Smith AD, Sharp SJ, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. European Journal of Epidemiology . 2018;33:811–829. doi: 10.1007/s10654-018-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Guo C, Zhou Q, Zhang D, Qin P, Li Q, Tian G, et al. Association of total sedentary behaviour and television viewing with risk of overweight/obesity, type 2 diabetes and hypertension: a dose–response meta‐analysis. Diabetes, Obesity and Metabolism . 2020;22:79–90. doi: 10.1111/dom.13867. [DOI] [PubMed] [Google Scholar]
- [97].Bellocco R, Jia C, Ye W, Lagerros YT. Effects of physical activity, body mass index, waist-to-hip ratio and waist circumference on total mortality risk in the Swedish National March Cohort. European Journal of Epidemiology . 2010;25:777–788. doi: 10.1007/s10654-010-9497-6. [DOI] [PubMed] [Google Scholar]
- [98].Crespo C, Palmieri MR, Perdomo RP, McGee DL, Smit E, Sempos CT, et al. The Relationship of Physical Activity and Body Weight with all-Cause Mortality Results from the Puerto Rico Heart Health Program. Annals of Epidemiology . 2002;12:543–552. doi: 10.1016/s1047-2797(01)00296-4. [DOI] [PubMed] [Google Scholar]
- [99].Hu G, Tuomilehto J, Silventoinen K, Barengo NC, Peltonen M, Jousilahti P. The effects of physical activity and body mass index on cardiovascular, cancer and all-cause mortality among 47 212 middle-aged Finnish men and women. International Journal of Obesity . 2005;29:894–902. doi: 10.1038/sj.ijo.0802870. [DOI] [PubMed] [Google Scholar]
- [100].Zhang X, Cash RE, Bower JK, Focht BC, Paskett ED. Physical activity and risk of cardiovascular disease by weight status among U.S adults. PLoS ONE . 2020;15:e0232893. doi: 10.1371/journal.pone.0232893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN. Fitness vs. Fatness on all-Cause Mortality: a Meta-Analysis. Progress in Cardiovascular Diseases . 2014;56:382–390. doi: 10.1016/j.pcad.2013.09.002. [DOI] [PubMed] [Google Scholar]
- [102].Barry VW, Caputo JL, Kang M. The Joint Association of Fitness and Fatness on Cardiovascular Disease Mortality: a Meta-Analysis. Progress in Cardiovascular Diseases . 2018;61:136–141. doi: 10.1016/j.pcad.2018.07.004. [DOI] [PubMed] [Google Scholar]
- [103].Carbone S, Kirkman DL, Garten RS, Rodriguez-Miguelez P, Artero EG, Lee DC, et al. Muscular Strength and Cardiovascular Disease: AN UPDATED STATE-OF-THE-ART NARRATIVE REVIEW. Journal of Cardiopulmonary Rehabilitation and Prevention . 2020;40:302–309. doi: 10.1097/HCR.0000000000000525. [DOI] [PubMed] [Google Scholar]
- [104].García-Hermoso A, Cavero-Redondo I, Ramírez-Vélez R, Ruiz JR, Ortega FB, Lee D, et al. Muscular Strength as a Predictor of all-Cause Mortality in an Apparently Healthy Population: a Systematic Review and Meta-Analysis of Data from Approximately 2 Million Men and Women. Archives of Physical Medicine and Rehabilitation . 2018;99:2100–2113.e5. doi: 10.1016/j.apmr.2018.01.008. [DOI] [PubMed] [Google Scholar]
- [105].Kim Y, Wijndaele K, Lee DC, Sharp SJ, Wareham N, Brage S. Independent and joint associations of grip strength and adiposity with all-cause and cardiovascular disease mortality in 403,199 adults: the UK Biobank study. The American Journal of Clinical Nutrition . 2017;106:773–782. doi: 10.3945/ajcn.117.156851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Saeidifard F, Medina-Inojosa JR, West CP, Olson TP, Somers VK, Bonikowske AR, et al. The association of resistance training with mortality: a systematic review and meta-analysis. European Journal of Preventive Cardiology . 2019;26:1647–1665. doi: 10.1177/2047487319850718. [DOI] [PubMed] [Google Scholar]
- [107].Geidl W, Schlesinger S, Mino E, Miranda L, Pfeifer K. Dose–response relationship between physical activity and mortality in adults with noncommunicable diseases: a systematic review and meta-analysis of prospective observational studies. International Journal of Behavioral Nutrition and Physical Activity . 2020;17:109. doi: 10.1186/s12966-020-01007-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Kodama S, Tanaka S, Heianza Y, Fujihara K, Horikawa C, Shimano H, et al. Association between Physical Activity and Risk of all-Cause Mortality and Cardiovascular Disease in Patients with Diabetes: a meta-analysis. Diabetes Care . 2013;36:471–479. doi: 10.2337/dc12-0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Sluik D, Buijsse B, Muckelbauer R, Kaaks R, Teucher B, Johnsen NF, et al. Physical Activity and Mortality in Individuals with Diabetes Mellitus: A Prospective Study and Meta-analysis. Archives of Internal Medicine . 2012;172:1285. doi: 10.1001/archinternmed.2012.3130. [DOI] [PubMed] [Google Scholar]
- [110].Schunemann H, Brozek J, Guyett G, Oxman A. The GRADE Working Group. GRADE handbook for grading quality of evidence and strength of recommendations. McMaster University and Evidence Prime Inc. 2013. [(Accessed: 25 July 2022)]. Available at: https://gdt.guidelinedevelopment.org/app/handbook/handbook.html.
- [111].Laukkanen JA, Isiozor NM, Kunutsor SK. Objectively Assessed Cardiorespiratory Fitness and all-Cause Mortality Risk: An Updated Meta-analysis of 37 Cohort Studies Involving 2,258,029 Participants. Mayo Clinic Proceedings . 2022;97:1054–1073. doi: 10.1016/j.mayocp.2022.02.029. [DOI] [PubMed] [Google Scholar]
- [112].Aggio D, Papachristou E, Papacosta O, Lennon LT, Ash S, Whincup P, et al. Trajectories of physical activity from midlife to old age and associations with subsequent cardiovascular disease and all-cause mortality. Journal of Epidemiology and Community Health . 2020;74:130–136. doi: 10.1136/jech-2019-212706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Gregg EW, Cauley JA, Stone K, Thompson TJ, Bauer DC, Cummings SR, et al. Relationship of Changes in Physical Activity and Mortality among Older Women. The Journal of the American Medical Association . 2003;289:2379. doi: 10.1001/jama.289.18.2379. [DOI] [PubMed] [Google Scholar]
- [114].Kieffer SK, Croci I, Wisløff U, Nauman J. Temporal Changes in a Novel Metric of Physical Activity Tracking (Personal Activity Intelligence) and Mortality: the HUNT Study, Norway. Progress in Cardiovascular Diseases . 2019;62:186–192. doi: 10.1016/j.pcad.2018.09.002. [DOI] [PubMed] [Google Scholar]
- [115].Mok A, Khaw KT, Luben R, Wareham N, Brage S. Physical activity trajectories and mortality: population based cohort study. British Medical Journal . 2019;365:l2323. doi: 10.1136/bmj.l2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Østergaard L, Jensen MK, Overvad K, Tjønneland A, Grøntved A. Associations between Changes in Cycling and all-Cause Mortality Risk. American Journal of Preventive Medicine . 2018;55:615–623. doi: 10.1016/j.amepre.2018.06.009. [DOI] [PubMed] [Google Scholar]
- [117].Paffenbarger RS, Hyde RT, Wing AL, Lee I, Jung DL, Kampert JB. The Association of Changes in Physical-Activity Level and other Lifestyle Characteristics with Mortality among Men. New England Journal of Medicine . 1993;328:538–545. doi: 10.1056/NEJM199302253280804. [DOI] [PubMed] [Google Scholar]
- [118].Petersen CB, Gronbaek M, Helge JW, Thygesen LC, Schnohr P, Tolstrup JS. Changes in physical activity in leisure time and the risk of myocardial infarction, ischemic heart disease, and all-cause mortality. European Journal of Epidemiology . 2012;27:91–99. doi: 10.1007/s10654-012-9656-z. [DOI] [PubMed] [Google Scholar]
- [119].Wannamethee SG, Shaper AG, Walker M. Changes in physical activity, mortality, and incidence of coronary heart disease in older men. The Lancet . 1998;351:1603–1608. doi: 10.1016/S0140-6736(97)12355-8. [DOI] [PubMed] [Google Scholar]
- [120].Blair SN, Kohl HW, Barlow CE, Paffenbarger RS, Gibbons LW, Macera CA. Changes in Physical Fitness and all-Cause Mortality. A prospective study of healthy and unhealthy men. The Journal of the American Medical Association . 1995;273:1093–1098. [PubMed] [Google Scholar]
- [121].Ehrman JK, Brawner CA, Al-Mallah MH, Qureshi WT, Blaha MJ, Keteyian SJ. Cardiorespiratory Fitness Change and Mortality Risk Among Black and White Patients: Henry Ford Exercise Testing (FIT) Project. The American Journal of Medicine . 2017;130:1177–1183. doi: 10.1016/j.amjmed.2017.02.036. [DOI] [PubMed] [Google Scholar]
- [122].Erikssen G. Physical Fitness and Changes in Mortality: the survival of the fittest. Sports Medicine . 2001;31:571–576. doi: 10.2165/00007256-200131080-00001. [DOI] [PubMed] [Google Scholar]
- [123].Imboden MT, Harber MP, Whaley MH, Finch WH, Bishop DA, Fleenor BS, et al. The Influence of Change in Cardiorespiratory Fitness With Short-Term Exercise Training on Mortality Risk From The Ball State Adult Fitness Longitudinal Lifestyle Study. Mayo Clinic Proceedings . 2019;94:1406–1414. doi: 10.1016/j.mayocp.2019.01.049. [DOI] [PubMed] [Google Scholar]
- [124].Imboden MT, Harber MP, Whaley MH, Finch WH, Bishop DL, Fleenor BS, et al. The Association between the Change in Directly Measured Cardiorespiratory Fitness across Time and Mortality Risk. Progress in Cardiovascular Diseases . 2019;62:157–162. doi: 10.1016/j.pcad.2018.12.003. [DOI] [PubMed] [Google Scholar]
- [125].Kokkinos P, Myers J, Faselis C, Panagiotakos DB, Doumas M, Pittaras A, et al. Exercise Capacity and Mortality in Older Men: a 20-year follow-up study. Circulation . 2010;122:790–797. doi: 10.1161/CIRCULATIONAHA.110.938852. [DOI] [PubMed] [Google Scholar]
- [126].Lee D, Sui X, Artero EG, Lee I, Church TS, McAuley PA, et al. Long-Term Effects of Changes in Cardiorespiratory Fitness and Body Mass Index on all-Cause and Cardiovascular Disease Mortality in Men: the Aerobics Center Longitudinal Study. Circulation . 2011;124:2483–2490. doi: 10.1161/CIRCULATIONAHA.111.038422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Prestgaard E, Mariampillai J, Engeseth K, Erikssen J, Bodegard J, Liestol K, et al. Change in Cardiorespiratory Fitness and Risk of Stroke and Death. Stroke . 2018;50:155–161. doi: 10.1161/STROKEAHA.118.021798. [DOI] [PubMed] [Google Scholar]
- [128].Ried-Larsen M, Rasmussen MG, Blond K, Overvad TF, Overvad K, Steindorf K, et al. Association of Cycling with all-Cause and Cardiovascular Disease Mortality among Persons with Diabetes: The European Prospective Investigation Into Cancer and Nutrition (EPIC) Study. JAMA Internal Medicine . 2021;181:1196–1205. doi: 10.1001/jamainternmed.2021.3836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [129].Rasmussen MG, Overvad K, Tjønneland A, Jensen MK, Østergaard L, Grøntved A. Changes in Cycling and Incidence of Overweight and Obesity among Danish Men and Women. Medicine and Science in Sports and Exercise . 2018;50:1413–1421. doi: 10.1249/MSS.0000000000001577. [DOI] [PubMed] [Google Scholar]
- [130].Early KS, Stewart A, Johannsen N, Lavie CJ, Thomas JR, Welsch M. The Effects of Exercise Training on Brachial Artery Flow-Mediated Dilation: A Meta-analysis. Journal of Cardiopulmonary Rehabilitation and Prevention . 2017;37:77–89. doi: 10.1097/HCR.0000000000000206. [DOI] [PubMed] [Google Scholar]
- [131].Pearson MJ, Smart NA. Effect of exercise training on endothelial function in heart failure patients: A systematic review meta-analysis. International Journal of Cardiology . 2017;231:234–243. doi: 10.1016/j.ijcard.2016.12.145. [DOI] [PubMed] [Google Scholar]
- [132].Ramos JS, Dalleck LC, Tjonna AE, Beetham KS, Coombes JS. The Impact of High-Intensity Interval Training Versus Moderate-Intensity Continuous Training on Vascular Function: a Systematic Review and Meta-Analysis. Sports Medicine . 2015;45:679–692. doi: 10.1007/s40279-015-0321-z. [DOI] [PubMed] [Google Scholar]
- [133].Sabag A, Way KL, Keating SE, Sultana RN, O’Connor HT, Baker MK, et al. Exercise and ectopic fat in type 2 diabetes: a systematic review and meta-analysis. Diabetes and Metabolism . 2017;43:195–210. doi: 10.1016/j.diabet.2016.12.006. [DOI] [PubMed] [Google Scholar]
- [134].Verheggen RJ, Maessen MF, Green DJ, Hermus AR, Hopman MT, Thijssen DH. A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: distinct effects on body weight and visceral adipose tissue. Obesity Reviews . 2016;17:664–690. doi: 10.1111/obr.12406. [DOI] [PubMed] [Google Scholar]
- [135].Dollet L, Zierath JR. Interplay between diet, exercise and the molecular circadian clock in orchestrating metabolic adaptations of adipose tissue. The Journal of Physiology . 2019;597:1439–1450. doi: 10.1113/JP276488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Stanford KI, Goodyear LJ. Muscle-Adipose Tissue Cross Talk. Cold Spring Harbor Perspectives in Medicine . 2018;8:a029801. doi: 10.1101/cshperspect.a029801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Townsend LK, Knuth CM, Wright DC. Cycling our way to fit fat. Physiological Reports . 2017;5:e13247. doi: 10.14814/phy2.13247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Villafaina S, Collado-Mateo D, Fuentes JP, Merellano-Navarro E, Gusi N. Physical Exercise Improves Heart Rate Variability in Patients with Type 2 Diabetes: a Systematic Review. Current Diabetes Reports . 2017;17:110. doi: 10.1007/s11892-017-0941-9. [DOI] [PubMed] [Google Scholar]
- [139].Dekker JM, Crow RS, Folsom AR, Hannan PJ, Liao D, Swenne CA, et al. Low Heart Rate Variability in a 2-Minute Rhythm Strip Predicts Risk of Coronary Heart Disease and Mortality from several Causes: the ARIC Study. Atherosclerosis Risk In Communities. Circulation . 2000;102:1239–1244. doi: 10.1161/01.cir.102.11.1239. [DOI] [PubMed] [Google Scholar]
- [140].Benichou T, Pereira B, Mermillod M, Tauveron I, Pfabigan D, Maqdasy S, et al. Heart rate variability in type 2 diabetes mellitus: A systematic review and meta-analysis. PLoS ONE . 2018;13:e0195166. doi: 10.1371/journal.pone.0195166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Franz MJ, Boucher JL, Rutten-Ramos S, VanWormer JJ. Lifestyle Weight-Loss Intervention Outcomes in Overweight and Obese Adults with Type 2 Diabetes: a Systematic Review and Meta-Analysis of Randomized Clinical Trials. Journal of the Academy of Nutrition and Dietetics . 2015;115:1447–1463. doi: 10.1016/j.jand.2015.02.031. [DOI] [PubMed] [Google Scholar]
- [142].Hasan B, Nayfeh T, Alzuabi M, Wang Z, Kuchkuntla AR, Prokop LJ, et al. Weight Loss and Serum Lipids in Overweight and Obese Adults: a Systematic Review and Meta-Analysis. The Journal of Clinical Endocrinology and Metabolism . 2020;105:3695–3703. doi: 10.1210/clinem/dgaa673. [DOI] [PubMed] [Google Scholar]
- [143].Khera R, Pandey A, Chandar AK, Murad MH, Prokop LJ, Neeland IJ, et al. Effects of Weight-Loss Medications on Cardiometabolic Risk Profiles: A Systematic Review and Network Meta-analysis. Gastroenterology . 2018;154:1309–1319.e7. doi: 10.1053/j.gastro.2017.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Mudaliar U, Zabetian A, Goodman M, Echouffo-Tcheugui JB, Albright AL, Gregg EW, et al. Cardiometabolic Risk Factor Changes Observed in Diabetes Prevention Programs in US Settings: A Systematic Review and Meta-analysis. PLoS Medicine . 2016;13:e1002095. doi: 10.1371/journal.pmed.1002095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [145].Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of Weight Reduction on Blood Pressure: a meta-analysis of randomized controlled trials. Hypertension . 2003;42:878–884. doi: 10.1161/01.HYP.0000094221.86888.AE. [DOI] [PubMed] [Google Scholar]
- [146].Semlitsch T, Krenn C, Jeitler K, Berghold A, Horvath K, Siebenhofer A. Long-term effects of weight-reducing diets in people with hypertension. The Cochrane Database of Systematic Reviews . 2021;2:CD008274. doi: 10.1002/14651858.CD008274.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Zomer E, Gurusamy K, Leach R, Trimmer C, Lobstein T, Morris S, et al. Interventions that cause weight loss and the impact on cardiovascular risk factors: a systematic review and meta-analysis. Obesity Reviews . 2016;17:1001–1011. doi: 10.1111/obr.12433. [DOI] [PubMed] [Google Scholar]
- [148].Dattilo AM, Kris-Etherton PM. Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. The American Journal of Clinical Nutrition . 1992;56:320–328. doi: 10.1093/ajcn/56.2.320. [DOI] [PubMed] [Google Scholar]
- [149].Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of Exercise on Glycemic Control and Body Mass in Type 2 Diabetes Mellitus: a meta-analysis of controlled clinical trials. The Journal of the American Medical Association . 2001;286:1218. doi: 10.1001/jama.286.10.1218. [DOI] [PubMed] [Google Scholar]
- [150].Jelleyman C, Yates T, O’Donovan G, Gray LJ, King JA, Khunti K, et al. The effects of high-intensity interval training on glucose regulation and insulin resistance: a meta-analysis. Obesity Reviews . 2015;16:942–961. doi: 10.1111/obr.12317. [DOI] [PubMed] [Google Scholar]
- [151].Liu J, Zhu L, Li P, Li N, Xu Y. Effectiveness of high-intensity interval training on glycemic control and cardiorespiratory fitness in patients with type 2 diabetes: a systematic review and meta-analysis. Aging Clinical and Experimental Research . 2019;31:575–593. doi: 10.1007/s40520-018-1012-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].Snowling NJ, Hopkins WG. Effects of Different Modes of Exercise Training on Glucose Control and Risk Factors for Complications in Type 2 Diabetic Patients: a meta-analysis. Diabetes Care . 2006;29:2518–2527. doi: 10.2337/dc06-1317. [DOI] [PubMed] [Google Scholar]
- [153].Igarashi Y, Nogami Y. Response of Lipids and Lipoproteins to Regular Aquatic Endurance Exercise: a Meta-Analysis of Randomized Controlled Trials. Journal of Atherosclerosis and Thrombosis . 2019;26:14–30. doi: 10.5551/jat.42937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [154].Kodama S, Tanaka S, Saito K, Shu M, Sone Y, Onitake F, et al. Effect of Aerobic Exercise Training on Serum Levels of High-Density Lipoprotein Cholesterol: a meta-analysis. Archives of Internal Medicine . 2007;167:999–1008. doi: 10.1001/archinte.167.10.999. [DOI] [PubMed] [Google Scholar]
- [155].Lin X, Zhang X, Guo J, Roberts CK, McKenzie S, Wu W, et al. Effects of Exercise Training on Cardiorespiratory Fitness and Biomarkers of Cardiometabolic Health: a Systematic Review and Meta‐Analysis of Randomized Controlled Trials. Journal of the American Heart Association . 2015;4:e002014. doi: 10.1161/JAHA.115.002014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [156].Pattyn N, Cornelissen VA, Eshghi SRT, Vanhees L. The Effect of Exercise on the Cardiovascular Risk Factors Constituting the Metabolic Syndrome: a meta-analysis of controlled trials. Sports Medicine . 2013;43:121–133. doi: 10.1007/s40279-012-0003-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [157].Wewege MA, Thom JM, Rye KA, Parmenter BJ. Aerobic, resistance or combined training: A systematic review and meta-analysis of exercise to reduce cardiovascular risk in adults with metabolic syndrome. Atherosclerosis . 2018;274:162–171. doi: 10.1016/j.atherosclerosis.2018.05.002. [DOI] [PubMed] [Google Scholar]
- [158].Halbert JA, Silagy CA, Finucane P, Withers RT, Hamdorf PA. Exercise training and blood lipids in hyperlipidemic and normolipidemic adults: a meta-analysis of randomized, controlled trials. European Journal of Clinical Nutrition . 1999;53:514–522. doi: 10.1038/sj.ejcn.1600784. [DOI] [PubMed] [Google Scholar]
- [159].Osman AF, Mehra MR, Lavie CJ, Nunez E, Milani RV. The incremental prognostic importance of body fat adjusted peak oxygen consumption in chronic heart failure. Journal of the American College of Cardiology . 2000;36:2126–2131. doi: 10.1016/s0735-1097(00)00985-2. [DOI] [PubMed] [Google Scholar]
- [160].Ashton RE, Tew GA, Aning JJ, Gilbert SE, Lewis L, Saxton JM. Effects of short-term, medium-term and long-term resistance exercise training on cardiometabolic health outcomes in adults: systematic review with meta-analysis. British Journal of Sports Medicine . 2020;54:341–348. doi: 10.1136/bjsports-2017-098970. [DOI] [PubMed] [Google Scholar]
- [161].Cornelissen VA, Fagard RH. Effects of Endurance Training on Blood Pressure, Blood Pressure-Regulating Mechanisms, and Cardiovascular Risk Factors. Hypertension . 2005;46:667–675. doi: 10.1161/01.HYP.0000184225.05629.51. [DOI] [PubMed] [Google Scholar]
- [162].Cornelissen VA, Fagard RH. Effect of resistance training on resting blood pressure: a meta-analysis of randomized controlled trials. Journal of Hypertension . 2005;23:251–259. doi: 10.1097/00004872-200502000-00003. [DOI] [PubMed] [Google Scholar]
- [163].Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of Resistance Training on Blood Pressure and other Cardiovascular Risk Factors: a meta-analysis of randomized, controlled trials. Hypertension . 2011;58:950–958. doi: 10.1161/HYPERTENSIONAHA.111.177071. [DOI] [PubMed] [Google Scholar]
- [164].Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. Journal of the American Heart Association . 2013;2:e004473. doi: 10.1161/JAHA.112.004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [165].Incollingo Rodriguez AC, Rodriguez A, Callahan LC, Saxbe D, Tomiyama AJ. The buddy system: A randomized controlled experiment of the benefits and costs of dieting in pairs. Journal of Health Psychology . 2019;24:1945–1954. doi: 10.1177/1359105317709514. [DOI] [PubMed] [Google Scholar]
- [166].Fagard RH. Exercise characteristics and the blood pressure response to dynamic physical training. Medicine and Science in Sports and Exercise . 2001;33:S484–S494. doi: 10.1097/00005768-200106001-00018. [DOI] [PubMed] [Google Scholar]