All medical practice should be governed by basic ethical principles, and intensive care medicine is no exception. Indeed, because of the nature of intensive care ethical issues are addressed almost daily.
Ethical principles of medical care
Autonomy
Beneficence
Non-maleficence
Distributive justice
Why withdraw treatment?
Withdrawal of treatment is an issue in intensive care medicine because it is now possible to maintain life for long periods without any hope of recovery. Intensive care is usually a process of supporting organ systems, but it does not necessarily offer a cure. Prolonging the process of dying is not in the patient’s best interests as it goes against the ethical principles of beneficence and non-maleficence. However, withdrawal of treatment does not equate with withdrawal of care. Care to ensure the comfort of a dying patient is as important as the preceding attempts to achieve cure.
Dr A decides to continue but not increase the level of vasoactive drug support or inspired oxygen concentration given to a man with multiple organ failure who has been in intensive care for 16 days. Over the next 5 days the patient improves; noradrenaline is discontinued and ventilatory support reduced, and he begins to rouse. He then develops a probable catheter related sepsis and deteriorates. Should Dr A abide by his previous decision of non-escalation? If not, why did he make the decision in the first place? What would he do if treatment was restarted but a similar situation occurred a week later? It would be appropriate (although it might be viewed as inconsistent) to review each requirement for treatment in the light of the patient’s current condition
It is often easier to withhold a treatment than to withdraw it once it has been instituted. Ethically, however, there is no difference between withdrawing a treatment that is felt to offer no benefit and withholding one that is not indicated. The common practice of offering a short period of aggressive intensive care in an attempt to gain improvement, followed by review, will inevitably mean that treatment is withdrawn for patients who have not improved and for whom death is felt to be inevitable.
An 18 year old patient has chemotherapy and bone marrow transplantation for leukaemia. While waiting for marrow recovery she develops respiratory failure and needs mechanical ventilation with 100% oxygen. Shortly after she requires increasing doses of noradrenaline and progresses to anuric renal failure. The intensive care team suggest that treatment should be withdrawn as her chances of survival are remote, but the haematologists argue that her renal, respiratory, and cardiovascular failure are potentially reversible if the bone marrow is given time to recover. After discussion with the family it is agreed that treatment should be withdrawn on the grounds of futility
About 70% of deaths in intensive care occur after withdrawal of treatment. This is not euthanasia. The cause of death remains the underlying disease process, and treatment is withdrawn as it has become futile. However, the timing of withdrawal, the treatments withdrawn, and the manner of withdrawal may vary considerably, not only from country to country but also between intensive care units in the same country.
Patient autonomy
Autonomy is another of the basic precepts of ethical practice, but there are problems with its implementation in the intensive care unit. Most critically ill patients are not competent to participate in discussion because of sedation or their illness. In some American states a designated chain of surrogacy exists. However, in the United Kingdom relatives do not have legal rights of decision making. Recent cases of conflict in the United States between healthcare providers and families have shown that the use of surrogates does not necessarily increase the chances of best care for the patient. Families may also find the concept of futile care difficult to accept. Furthermore, data on which prognoses are based are statistical and cannot necessarily be applied to an individual patient.
An Asian man is brought into hospital in a coma after a massive subarachnoid haemorrhage, which is confirmed by computed tomography. Despite full intensive care he becomes brain dead. The doctors approach the family about the possibility of organ donation, but they refuse on cultural grounds. They also refuse to permit withdrawal of support as their religion does not accept brain death. Should the family’s wishes be respected or should support be withdrawn regardless? It was decided to maintain full support until the patient died 5 days later
Another difficult issue occurs when a patient may survive but with a poor quality of life. The concept of “relative futility” is dangerous as it introduces an unknown and potentially highly variable factor—namely, a doctor’s judgment on the patient’s quality of life. Substitution of the word “reasonable” for “relative” has been argued to give doctors more latitude in deciding whether a treatment is ethically justifiable.
When to withdraw treatment
In general, treatment is withdrawn when death is felt to be inevitable despite continued treatment. This would typically be when dysfunction in three or more organ systems persists or worsens despite active treatment or in cases such as multiple organ failure in patients with failed bone marrow transplantation. These decisions remain difficult because of the paucity of data on different clinical scenarios.
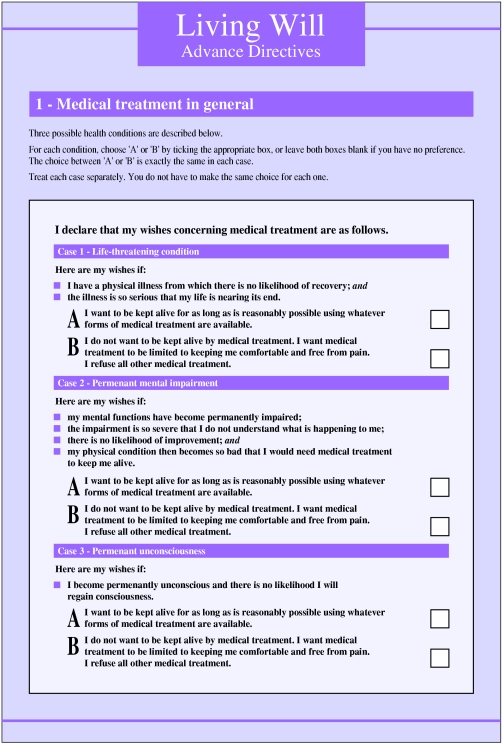
Whatever the definition of futility used the carers must act as advocates for the patient. This requirement has, however, been criticised as paternalistic. Advance directives are uncommon in the United Kingdom. The advance refusal of treatment is legally binding provided certain conditions are met. The BMA has issued a statement supporting the use of living wills. A problem still exists unless they are precisely worded.
Caring for families
Regardless of whether families are involved in the decision making process, they are affected by the behaviour of the carers. Families who feel excluded from discussion, who have had the burden of decision making placed on them, or in cases where there was delay or excess haste in enacting decisions express negative feelings towards the process of withdrawing treatment. Communication with the family is a vital part of the general care of intensive care patients. Relatives must be kept fully informed about the patient’s condition, in particular regarding issues of limiting and withdrawing treatment. Although decisions rest with the medical staff, it is unwise to limit or withdraw treatment without the agreement of the relatives.
Process of withdrawal
Approaches to the withdrawal of treatment vary with the attitudes of the intensive care doctors. Some doctors are prepared only to withhold treatment rather than to withdraw it despite the lack of ethical distinction. This approach can create difficulties once the threshold for the withheld treatment is reached.
Once a decision has been made to withdraw treatment and agreement has been obtained from the family and admitting team, inotropes and vasopressors are discontinued, sedation may be increased, and the inspired oxygen concentration reduced to room air. Other supportive treatments such as renal replacement therapy are also removed. Death usually follows shortly afterwards. Only rarely is ventilation discontinued.
In general, it is better for the family if the patient is not moved from intensive care once the decision is made. It is unfair to expose the family to unfamiliar staff at this distressing time, especially if they have built up a rapport with nursing and medical staff. Most units have rooms where the family can be with the patient.
Problems
Problems arising from decisions to withdraw treatment can be divided into four types.
The referring team request continued futile therapy
This can usually be resolved by explaining the rationale and offering a second opinion from another intensive care consultant. If conflict still remains, treatment cannot be withdrawn. The family should not be informed of a decision to withdraw that is then rescinded because of interteam conflicts. It will reduce their faith in subsequent decisions and undermine confidence in the predicted outcome.
The patient’s family requests continued futile therapy
Guilt usually plays a part in the family’s request to continue treatment, although religious and cultural factors may also contribute. Agreement can usually be obtained by explaining the rationale again and offering a second opinion from within or outside the intensive care team. It is best not to withdraw treatment if there is conflict. However, the final decision rests with the intensive care team. This underlines the need for good communication.
A 65 year old man is admitted to intensive care after a laparotomy for faecal peritonitis secondary to a perforated diverticulum. He needs mechanical ventilation, haemofiltration, and noradrenaline. Two days later his children (the next of kin) request discontinuation of treatment as they feel that their father would not wish to be put through this suffering and had strongly expressed such views. However, he shows evidence of clinical improvement and his requirements for noradrenaline and oxygen are significantly reduced. The intensive care team therefore felt that treatment should not be withdrawn. The man recovered and was discharged from hospital. It was later discovered that his family had apportioned his possessions while he was in intensive care
The family requests inappropriate discontinuation of therapy
The rationale behind the therapy and the reasons why continuing treatment is thought appropriate should be explained. The duty of care is to the patient, not the family. Again, a second opinion can be offered.
The patient requests discontinuation of therapy.
Explain to the patient the rationale for the treatment and that, in the opinion of the intensive care team, a chance of recovery exists. It may be appropriate to offer a short term contract for treatment (for example, 48 hours then review). Ultimately, the competent patient has the right to refuse treatment even if that treatment is life saving.
Figure.
Living wills enable people to have a say in their treatment when they are incapable of taking part in decision making
Figure.
Talking to patients’ relatives is best done in a quiet room of the unit
Acknowledgments
The living will was provided by Terence Higgins Trust and King’s College London.
Footnotes
Bob Winter is consultant in intensive care, University Hospital, Nottingham, and Simon Cohen is senior lecturer in intensive care, University College London Hospitals, London.
The ABC of intensive care is edited by Mervyn Singer, reader in intensive care medicine, Bloomsbury Institute of Intensive Care Medicine, University College London and Ian Grant, director of intensive care, Western Infirmary, Edinburgh. The series was conceived and planned by the Intensive Care Society’s council and research committee.