Abstract
Background
Intracranial arachnoid cysts are benign collections of cerebrospinal fluid that are often asymptomatic and discovered incidentally. An interhemispheric location of these lesions is rare, with only a few such cases reported in the literature. Though spontaneous regression of arachnoid cysts has been described in other locations, to date this phenomenon has not been reported in interhemispheric fissure cysts.
Observations
In this report, we describe a patient with a large, multiloculated interhemispheric arachnoid cyst diagnosed on prenatal ultrasound. She did not exhibit neurologic deficits or signs of increased intracranial pressure and was observed with serial imaging. After several years of observation, imaging revealed spontaneous and progressive decrease in the cyst size.
Lessons
We illustrate a case of regression of an interhemispheric arachnoid cyst in a pediatric patient. To our knowledge, this is the first reported case of spontaneous shrinkage of an arachnoid cyst in this location. Although the current presentation is rare, this reporting adds to the current understanding of natural history of arachnoid cysts and provides an example of radiographical improvement without intervention of a cyst located within the interhemispheric fissure.
Keywords: Arachnoid cyst, Interhemispheric cyst, Spontaneous regression, Pediatric
Introduction
Intracranial arachnoid cysts are congenital, benign collections of cerebrospinal fluid surrounded by an arachnoid membrane that are often asymptomatic [1, 2]. Interhemispheric location of these cysts is uncommon, with only a few cases reported in the literature [3–5]. Interestingly, several reports have detailed cases of cyst shrinkage or disappearance without intervention in locations other than the interhemispheric region. The literature for interhemispheric cysts in the pediatric population focuses primarily on their surgical management [4, 6–9].
Here, we report a case of a large interhemispheric cyst that spontaneously decreased in size after conservative management. To the authors’ knowledge, this is the first description of spontaneous reduction of an interhemispheric arachnoid cyst.
Illustrative Case
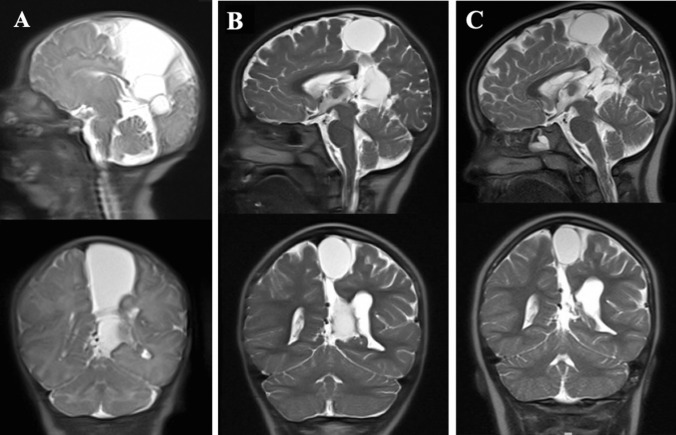
This female patient had an unremarkable medical history aside from a multiloculated interhemispheric arachnoid cyst that was discovered during routine prenatal ultrasound. Subsequent ultrasounds in utero demonstrated stability in size of the cystic mass. She was born at 38 weeks via C-section due to arrest of descent. Delivery was also notable for prolonged rupture of membranes (22 h) with chorioamnionitis, for which her mother was treated with ampicillin and gentamicin. Head circumference at birth was in the 75th percentile, and the baby’s fontanelle was soft and compressible. Fast sequence magnetic resonance imaging (MRI) was obtained on day 2 of life to establish a baseline, which demonstrated a large cluster of extra-axial cystic structures within the interhemispheric space, with associated hypoplastic posterior corpus callosum (Fig. 1A). No intervention was planned at that time as the baby did not show any signs of increased intracranial pressure (ICP) or neurological deficit from the cyst. She was discharged on day 4 of life, and outpatient neurosurgical follow-up was arranged. Repeat cranial imaging was obtained at her first follow-up at age 3 weeks, which showed unchanged size of the interhemispheric cyst and stable hypoplasia of the splenium of the corpus collosum. Head circumference at this time was near the 50th percentile. Imaging at follow-up over the next 5 years revealed stability of cyst size. Head circumference over that time did increase to approximately the 80–90th percentile, which also remained stable thereafter. She did not exhibit motor deficits, experience headaches, or have symptoms of increased ICP such as papilledema throughout this time. Brain MRI at her follow-up at age 6 years showed significant reduction in the cyst size compared to prior (Fig. 1B). Further decrease in cyst size was revealed on MRI at her 8-year follow-up visit (Fig. 1C), after which follow-up was planned on an as-needed basis. She continued to do well clinically and did not exhibit any neurologic deficit.
Fig. 1.
A Sagittal (upper) and coronal (lower) brain fast sequence magnetic resonance imaging (MRI) on day 2 of life, demonstrating a large cluster of extra-axial cystic structures at the medial aspect of the left parietal lobe extending inferior to the quadrigeminal cistern with mass effect on the adjacent brain and left lateral ventricle, as well as hypoplastic posterior corpus callosum. B Sagittal (upper) and coronal (lower) brain fast sequence MRI at 6 years of age, showing decrease in size of the cyst. C Sagittal (upper) and coronal (lower) brain fast sequence MRI at 8 years of age, which showed further decrease in size in the cyst
Discussion
Observations
As interhemispheric arachnoid cysts are rare lesions, information regarding their natural course and optimal management is limited. It is estimated that interhemispheric location of arachnoid cysts comprises approximately 5% of all cases [10]. One retrospective study of arachnoid cyst prevalence in children found that of 309 incidentally detected cysts, only 4 were located in the interhemispheric region [11]. In children, these lesions are typically concomitant with developmental anomalies of midline structures, such as partial or complete agenesis of the corpus callosum [3, 6–9]. Our patient demonstrated dysplastic appearance of the splenium of the corpus callosum, aligning with this association. In spite of the large dimensions these lesions can attain, clinical manifestations may be subtle or absent. With the increased utilization of ultrasound prenatally, more of these lesions have been diagnosed prior to birth [12, 13], as was the case in our patient.
Arachnoid cysts associated with neurological symptoms or increased ICP can be managed surgically with craniotomy for cyst resection, endoscopic fenestration, or cystoperitoneal shunting. There have been several prior case series on the surgical management of interhemispheric cysts using such techniques [2, 6, 7, 9, 10]. This literature demonstrates that when encountered, interhemispheric cysts are often treated operatively.
Regression or disappearance of arachnoid cysts has been reported in prior literature. There have been several cited instances of cyst disappearance following head injury, in which cysts found in association with subdural or epidural hematomas following trauma decrease in size as the hematoma subsides [14–16]. One proposed mechanism of this phenomenon is that cranial trauma may cause rupture of the outer membrane of the cyst, thus leading to cyst fluid drainage into the subarachnoid space [17]. Thereby, cysts found incidentally on imaging done after trauma are found to decrease in size on subsequent imaging. Other types of intracranial irritation aside from trauma, such as meningitis, have also been associated with cyst disappearance [18]. In the absence of trauma or other notable irritating event, some have suggested that a communication between the cyst and subarachnoid space can be created by sudden, transient increases in ICP during Valsalva maneuver [19]. Numerous cases of seemingly spontaneous regression of arachnoid cysts have been discussed in the literature in both children and adults [20–26]. The most common locations of these reported disappearing arachnoid cysts are the middle cranial fossa, posterior cranial fossa, temporal/temporo-frontal region, suprasellar region, and prepontine region [19]. To date, there has been no cited case of spontaneously regressing interhemispheric cyst.
In the current case, we describe a pediatric patient with a multiloculated arachnoid cyst diagnosed in utero that was followed with serial imaging for several years and subsequently demonstrated spontaneous shrinkage. She did not have cranial trauma nor other intracranial irritation or pathology that preceded cyst regression. Of note, during the period of observation of the cyst, the patient experienced a fall from her tricycle without consequent loss of consciousness or neurological change. However, this occurred after radiological evidence of decrease in cyst size. As such, this fall likely was not the inciting event that led to cyst regression.
In cases of asymptomatic arachnoid cysts, most opt for conservative treatment with observation and serial imaging. Reports of shrinkage of these lesions are clinically relevant when counseling patients and families on the potential outcomes of arachnoid cysts. The currently reported case is the first cited description of such a shrinkage of an arachnoid cyst located within the interhemispheric fissure, adding to the collective knowledge of possible clinical course of a cyst in this specific location.
Author contributions
A.F. and J.J. wrote the main manuscript text. A.F. prepared figure 1. All authors reviewed the manuscript.
Funding
No funds, grants, or other support was received.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kotil K, Balci N, Bilge T (2007) Intracranial symptomatic giant arachnoid cyst of the interhemispheric fissure presenting with frontal lobe syndrome. Turk Neurosurg 17(2):147–151 [PubMed] [Google Scholar]
- 2.Giannetti AV, Ferreira Fraga SM, Silva MC, Gurgel-Giannetti J (2012) Endoscopic treatment of interhemispheric arachnoid cysts. Pediatr Neurosurg 48(3):157–162. 10.1159/000346263 10.1159/000346263 [DOI] [PubMed] [Google Scholar]
- 3.Albakr A, Sader N, Lama S, Sutherland GR (2021) Interhemispheric arachnoid cyst Surg Neurol Int 12:125. 10.25259/SNI_660_2020 10.25259/SNI_660_2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spennato P, Ruggiero C, Aliberti F, Buonocore MC, Trischitta V, Cinalli G (2013) Interhemispheric and quadrigeminal cysts. World Neurosurg. 79(2):s20.e1–s20.e7. 10.1016/j.wneu.2012.02.010 10.1016/j.wneu.2012.02.010 [DOI] [PubMed] [Google Scholar]
- 5.Yamasaki F, Kodama Y, Hotta T et al (2003) Interhemispheric arachnoid cyst in the elderly: case report and review of the literature. Surg Neurol 59(1):68–74. 10.1016/s0090-3019(02)00876-5 10.1016/s0090-3019(02)00876-5 [DOI] [PubMed] [Google Scholar]
- 6.Cinalli G, Peretta P, Spennato P et al (2006) Neuroendoscopic management of interhemispheric cysts in children. J Neurosurg Pediatr 105(3):194–202. 10.3171/ped.2006.105.3.194 10.3171/ped.2006.105.3.194 [DOI] [PubMed] [Google Scholar]
- 7.Kim TK, Kim JW, Kim SK, Lee JY, Kim KH, Phi JH (2023) Surgical treatment of interhemispheric arachnoid cysts. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg. 10.1007/s00381-023-06243-1 10.1007/s00381-023-06243-1 [DOI] [PubMed] [Google Scholar]
- 8.Lena G, van Calenberg F, Genitori L, Choux M (1995) Supratentorial interhemispheric cysts associated with callosal agenesis: surgical treatment and outcome in 16 children. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 11(10):568–573. 10.1007/BF00300994 10.1007/BF00300994 [DOI] [PubMed] [Google Scholar]
- 9.Ferrera G, Vetrano IG, Chiapparini L et al (2021) Surgical treatment and clinical outcome of large pediatric interhemispheric cysts with callosal agenesis: a systematic literature review with four additional patients. Clin Neurol Neurosurg 204:106600. 10.1016/j.clineuro.2021.106600 10.1016/j.clineuro.2021.106600 [DOI] [PubMed] [Google Scholar]
- 10.Mankotia DS, Sardana H, Sinha S et al (2016) Pediatric interhemispheric arachnoid cyst: an institutional experience. J Pediatr Neurosci 11(1):29–34. 10.4103/1817-1745.181258 10.4103/1817-1745.181258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Holou WN, Yew AY, Boomsaad ZE, Garton HJL, Muraszko KM, Maher CO (2010) Prevalence and natural history of arachnoid cysts in children. J Neurosurg Pediatr 5(6):578–585. 10.3171/2010.2.PEDS09464 10.3171/2010.2.PEDS09464 [DOI] [PubMed] [Google Scholar]
- 12.Caldarelli M, Di Rocco C (1996) Surgical options in the treatment of interhemispheric arachnoid cysts. Surg Neurol 46(3):212–221. 10.1016/0090-3019(96)00155-3 10.1016/0090-3019(96)00155-3 [DOI] [PubMed] [Google Scholar]
- 13.Korsic M, Jugović D, Porcnik A (2013) Endoscopic treatment of in utero diagnosed multiloculated interhemispheric cyst in a newborn: case report. Acta Clin Croat 52(1):119–124 [PubMed] [Google Scholar]
- 14.Mori T, Fujimoto M, Sakae K et al (1995) Disappearance of arachnoid cysts after head injury. Neurosurgery. 36(5):938–941; discussion 941-942. 10.1227/00006123-199505000-00008 10.1227/00006123-199505000-00008 [DOI] [PubMed] [Google Scholar]
- 15.Castro-Bouzas D, Frieiro-Dantas C, Serramito-García R, Gelabert-González M (2012) Post-traumatic resolution of an intracranial arachnoid cyst. Rev Neurol 54(6):380–381 [PubMed] [Google Scholar]
- 16.Yamanouchi Y, Someda K, Oka N (1986) Spontaneous disappearance of middle fossa arachnoid cyst after head injury. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 2(1):40–43. 10.1007/BF00274033 10.1007/BF00274033 [DOI] [PubMed] [Google Scholar]
- 17.Seizeur R, Forlodou P, Coustans M, Dam-Hieu P (2007) Spontaneous resolution of arachnoid cysts: review and features of an unusual case. Acta Neurochir (Wien) 149(1):75–78; discussion 78. 10.1007/s00701-006-1073-1 10.1007/s00701-006-1073-1 [DOI] [PubMed] [Google Scholar]
- 18.Yoshioka H, Kurisu K, Arita K et al (1998) Spontaneous disappearance of a middle cranial fossa arachnoid cyst after suppurative meningitis. Surg Neurol 50(5):487–491. 10.1016/s0090-3019(97)00192-4 10.1016/s0090-3019(97)00192-4 [DOI] [PubMed] [Google Scholar]
- 19.Ammar A, Alojan AA, Turkistani AN, Alrayes MM (2020) Spontaneous regression of pineal region arachnoid cyst: a case report and review of literature. Asian J Neurosurg 15(1):155–158. 10.4103/ajns.AJNS_289_19 10.4103/ajns.AJNS_289_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kikuchi A, Chernov M, Hagiwara S, Ohbuchi H, Kubota Y, Kasuya H (2021) Resolution of the large middle fossa arachnoid cyst without any identifiable cause: case report. J Clin Neurosci 88:147–149. 10.1016/j.jocn.2021.03.029 10.1016/j.jocn.2021.03.029 [DOI] [PubMed] [Google Scholar]
- 21.Adilay U, Guclu B, Tiryaki M, Hicdonmez T (2017) Spontaneous resolution of a Sylvian arachnoid cyst in a child: a case report. Pediatr Neurosurg 52(5):343–345. 10.1159/000479328 10.1159/000479328 [DOI] [PubMed] [Google Scholar]
- 22.Peterson C, Lawless M, Sood S (2020) Spontaneous resolution of asymptomatic pediatric suprasellar arachnoid cysts: report of 2 cases and review of the literature. Pediatr Neurosurg 55(1):62–66. 10.1159/000504262 10.1159/000504262 [DOI] [PubMed] [Google Scholar]
- 23.Russo N, Domenicucci M, Beccaglia MR, Santoro A (2008) Spontaneous reduction of intracranial arachnoid cysts: a complete review. Br J Neurosurg 22(5):626–629. 10.1080/02688690802295652 10.1080/02688690802295652 [DOI] [PubMed] [Google Scholar]
- 24.Dodd RL, Barnes PD, Huhn SL (2002) Spontaneous resolution of a prepontine arachnoid cyst. Case report and review of the literature. Pediatr Neurosurg 37(3):152–157. 10.1159/000064394 10.1159/000064394 [DOI] [PubMed] [Google Scholar]
- 25.Moon KS, Lee JK, Kim JH, Kim SH (2007) Spontaneous disappearance of a suprasellar arachnoid cyst: case report and review of the literature. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 23(1):99–104. 10.1007/s00381-006-0161-0 10.1007/s00381-006-0161-0 [DOI] [PubMed] [Google Scholar]
- 26.Cokluk C, Senel A, Celik F, Ergür H (2003) Spontaneous disappearance of two asymptomatic arachnoid cysts in two different locations. Minim Invasive Neurosurg MIN 46(2):110–112. 10.1055/s-2003-39337 10.1055/s-2003-39337 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.