Abstract
Obesity is a well-recognized risk factor for adolescent depressive symptoms, but mediating mechanisms of this association have scarcely been studied. This study is unique in examining an indirect pathway of this link via body esteem (BE) prospectively from childhood (8–12 years) to adolescence (13–18 years). In addition, potential gender moderation was examined. This study utilized data from a case–control study comparing 100 children with and without obesity matched on important confounders (age, gender, and socioeconomic status). Our findings provide support for the mediating role of BE in the link between childhood weight status and adolescent depressive symptoms at a 5-year follow-up. This mediation effect did not differ between boys and girls. The findings suggest the relevance of specifically targeting children’s BE in preventive intervention programs among children with obesity to prevent future mental health problems.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00787-023-02348-9.
Keywords: Childhood obesity, Adolescent depression, Body esteem, Mediation, Moderated mediation
Introduction
Depressive disorders are highly prevalent mental problems that rise sharply during puberty, especially for girls, and can seriously impact physical and psychological health [1, 2]. As depressive symptoms importantly underlie depressive disorders, there is a pressing need to identify and understand factors that contribute to the enhanced risk for adolescents’ depressive symptoms [3].
Recently, accumulating evidences have suggested a bi-directional association between depression and obesity [4, 5]. As such, obesity in childhood might be an eminent risk factor for the development of adolescent depressive symptoms [6–8]. This link is supported in adult populations by Mendelian randomization (MR) studies [9–11]. While results appear to be more inconsistent for children [7, 12], a recent MR study also suggests that childhood obesity is linked to the development of major depressive disorder during adulthood [13]. As such, identifying risk factors that mediate between obesity and depressive symptoms may provide a roadmap to prevent the escalating mental health consequences of childhood obesity.
Body esteem-mediating effects
Body esteem (BE), defined as self-evaluation of one’s body or physical appearance [14], could be a prominent underlying mechanism explaining the development of obesity-linked depressive symptoms during adolescence [15, 16]. The subjective perception of the own body depends on the interplay of the person with his or her social context. Specifically, children who deviate from the thin ideal (e.g., children with obesity) are more likely to experience weight stigma, primarily through weight-related teasing [17]. It is thus not surprising that the literature has consistently found that children and adolescents with obesity tend to have lower BE than their normal-weight peers [18–20]. Moreover, body dissatisfaction is one of the most consistent predictors of depressive symptoms during adolescence [21–25]. Accordingly, some previous studies among both adolescent and adult populations have provided evidence for the conjecture that BE may mediate the obesity–depression link [26–32]. However, these studies are limited by their cross-sectional design. That is, they give no insight into the temporal order and developmental pathways of the findings. Our prospective study fills this prominent gap.
Moderating effects of gender
There is evidence of a stronger link between obesity and depressive symptoms among females than males [6, 7, 32]. However, whether this might reflect a gender-specific mediation role of BE has been poorly studied. The study by Xie and colleagues [33] is, to our knowledge, the only one that has examined this potential gender-moderated mediation, and they did it among Asian and Hispanic adolescents. They found a significant mediation effect of BE on the association between being overweight and depressive symptoms among adolescent Asian girls. Regarding specific links, Shriver et al. [34] found that overweight was prospectively associated with BE only among girls, but when weight status reached obesity, the association with BE was significant for boys and girls. In addition, Ricciardelli et al. [18] reported no significant differences in the impact of weight status on BE between girls and boys. Concerning the BE to depressive symptoms pathway, some studies suggest that BE is a stronger predictor of depression in girls than in boys [24, 35, 36], while other studies suggest equivalent effects of BE on depressive symptoms in girls and boys [22, 37, 38]. Possible gender differences can be explained by the fact that boys generally place more importance on other domains than appearance, while appearance plays a prominent role in girls’ self-esteem and mental health [38]. However, since previous studies are scarce and mixed, further research is required to understand potential gender differences, particularly regarding BE prospective mediating effects.
Current study
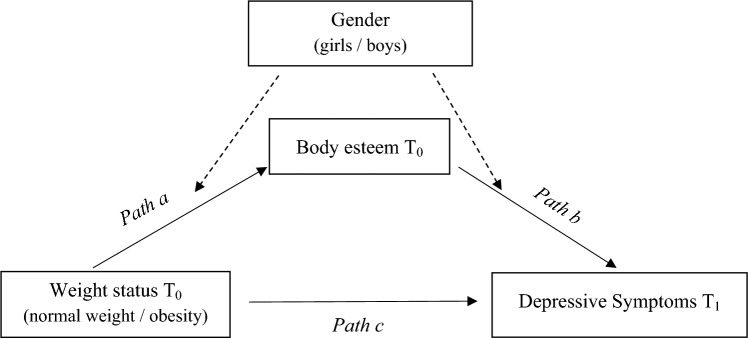
The current study aims to cover the mentioned gaps by investigating whether BE is a mediator of the prospective childhood obesity–adolescent depressive symptoms pathway and whether mediation is different for boys versus girls (see Fig. 1). Based on prior considerations, our first hypothesis was that children with obesity would be concurrently and prospectively at higher risk for depressive symptoms, compared to children with normal weight. Our second hypothesis stated that, longitudinally, the childhood obesity group would develop more depressive symptoms after 5 years, compared to the normal-weight group, controlled for baseline depressive symptoms. The third hypothesis argued that BE would mediate the prospective association between childhood obesity and adolescent depressive symptoms. And in the fourth hypothesis, we hypothesized that the mediating effect of BE would be conditional on gender (i.e., moderated mediation), in the sense that the mediation effect will be stronger for girls than for boys. We made no further a priori hypothesis about the specific moderating role of gender in the obesity-to-body-esteem pathway. However, despite the mixed findings in the literature, we theoretically expected a stronger association for girls for the body esteem-to-depressive symptoms pathway.
Fig. 1.
Diagram of moderated mediation model. Note that solid lines represent the direct and indirect (mediation) pathways; dotted lines represent the moderation effects in the indirect pathway (moderate mediation). Covariates (depressive symptoms T0, Age, and SES) are included in the analyses but are not displayed in the figure
Method
The procedures and data analyses for this paper were pre-registered on the Open Science Framework (https://osf.io/dc67e). A minor deviation from the preregistration is discussed in “Strategy of analysis”.
Participants and procedure
Participants were part of the “ANOBAS project” (PSI2011-23127), a case–control study to assess early risk factors for childhood obesity. The initial sample consisted of 100 children aged 8–12 years: 50 children with obesity (Z-BMI score ≥ 2) matched with 50 children with normal-weight (Z-BMI score ≥ −2 to < 1), according to age, gender and socioeconomic status [38]. The current study has a prospective two-wave design and compares these two groups on the development of depressive symptoms at the 5-year follow-up, when participants were 13–18 years old.
Data at baseline (T0) were collected between 2013 and 2016, while data at follow-up (T1) were collected between 2018 and 2021, in the region of Madrid, Spain. For T0 data collection, the obesity group was recruited from Primary Health Centers and the normal-weight group from 13 primary schools (matched 1:1). Details of the recruitment and sample selection procedure at T0 have been published elsewhere [39, 40]. At T1, participants were contacted by telephone or email to decide whether they wanted to participate in the follow-up, which was completely voluntary. The participation at each time point involved a semi-structured clinical interview with the child and at least one family member, a battery of self-reported questionnaires, and a measurement of weight and height. The assessments were carried out by the trained interviewers at the Niño Jesús Children’s Hospital, and the questionnaires were completed on paper. The study received ethical approval from the Niño Jesus Children Hospital and the Autonomous University of Madrid. Parents’ written consent and adolescents’ assent was obtained.
Out of 100 participants (see Supplementary Table S1), 70 participated in the follow-up (obesity group n = 34, normal-weight group n = 36). When comparing the cohort of children with obesity with the cohort of children with normal-weight that completed the follow-up, no significant differences were found in terms of age (t = 0.24, p > 0.05), gender (χ2 = 0.49, p > 0.05), and socioeconomic status (χ2 = 5.29, p > 0.05) at T0 between these two groups (see Table 1).
Table 1.
Descriptive statistics and weight-status group differences for participants (n = 70)
| Baseline (T0) | 5-year follow-up (T1) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NWG (n = 36) M (SD)/N(%) |
OG (n = 34) M (SD)/N(%) |
t/χ2 | p | d | NWG (n = 36) M (SD)/N (%) |
OG (n = 34) M (SD)/N (%) |
t/χ2 | p | d | |
| Z-BMI | − 0.43 (0.70) | 2.61 (0.83) | − 16.55 | < 0.001 | 3.96 | − 0.08 (1.00) | 2.21 (1.39) | − 7.90 | < 0.001 | 1.89 |
| Age | 10.65 (1.38) | 10.58 (1.15) | 0.24 | 0.811 | 15.80 (1.59) | 16.52 (1.44) | − 1.98 | 0.052 | ||
| Gender | 0.49 | 0.484 | 0.49 | 0.484 | ||||||
| Boys | 15 (41.7) | 17 (50) | 15 (41.7) | 17 (50) | ||||||
| Girls | 21 (58.3) | 17 (50) | 21 (58.3) | 17 (50) | ||||||
| SES | 3.31 (0.71) | 3.12 (1.07) | 0.87 | 0.386 | 3.28 (0.91) | 2.88 (1.23) | 1.54 | 0.129 | ||
| Body esteem (BES/BESAA)* | ||||||||||
| Total | 20.56 (2.44) | 10.53 (6.50) | 8.64 | < 0.001 | 2.05 | 2.62 (0.65) | 1.83 (0.75) | 4.64 | < 0.001 | 1.11 |
| Boys | 20.60 (1.64) | 9.12 (5.59) | 7.66 | < 0.001 | 2.77 | 2.60 (0.64) | 1.99 (0.82) | 2.30 | 0.029 | 0.82 |
| Girls | 20.52 (2.93) | 11.94 (7.18) | 5.00 | < 0.001 | 1.56 | 2.63 (0.67) | 1.69 (0.67) | 4.29 | < 0.001 | 1.40 |
| Depressive symptoms (CDI) | ||||||||||
| Total | 5.89 (3.50) | 9.65 (6.05) | − 3.20 | 0.002 | 0.72 | 8.28 (4.54) | 12.94 (8.66) | − 2.84 | 0.006 | 0.67 |
| Boys | 7.47 (3.16) | 9.53 (6.30) | − 1.15 | 0.261 | 8.27 (4.83) | 11.53 (7.36) | − 1.46 | 0.155 | ||
| Girls | 4.76 (3.35) | 9.76 (6.00) | − 3.26 | 0.002 | 1.03 | 8.29 (4.44) | 14.35 (9.82) | − 2.54 | 0.016 | 0.80 |
| Depressive disorder | 3.32 | 0.068 | 8.30 | 0.004 | ||||||
| Absence | 36 (100) | 31 (91.2) | 34 (94.4) | 23 (67.6) | ||||||
| Risk/presence | 0 (0) | 3 (8.8) | 2 (5.6) | 11 (32.4) | ||||||
Significant p values are in bold. NWG normal-weight group, OB obesity group, Z-BMI body mass index z-scores, SES socioeconomic status, BES Body-Esteem Scale, BESAA Body-Esteem Scale for Adolescents and Adults, M mean, SD standard deviation. Cohen’s d was calculated for statistically significant associations: d < 0.4 = small effect, 0.4 ≤ d ≤ 0.75 = moderate effect, and d > 0.75 = large effect [54]
* The BES (T0) and BESAA (T1) scales differ in the range of values they can take
Measures
Body esteem
At T0, the Body-Esteem Scale (BES) [41, 42] was used. It is a 24-item self-reported scale (yes/no response) that collects information about feelings or perceptions about one’s appearance, weight, and the way participants believe they are valued by others. The total scores ranged from 0 to 24. In the current study, the BES scale demonstrated excellent reliability (α = 0.94).
At T1, the Body-Esteem Scale for Adolescents and Adults (BESAA) [14, 43] was used. The Spanish version consists of a self-administered questionnaire with 14 items on a 5-point Likert scale ranging from 0 (never) to 4 (always). It includes three subscales: BE-appearance, BE-weight, and BE-attribution. A total score is reported as the mean of the three subscale means (total score from 0 to 4), with high scores implying greater BE. Cronbach’s alpha for BESAA’s total score was 0.89.
Depressive symptoms and diagnosis
The Child Depression Inventory (CDI) [44, 45] was used at T0 and T1. This self-reported questionnaire consists of 27 items with three response options (0–2), aimed to measure cognitive, affective, and behavioral signs of depression. The total score of the scale ranged from 0 to 54. In the current study, Cronbach’s alpha for the CDI was 0.84 at T0 and 0.90 at T1.
The Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL) [46, 47] was also used at T0 and T1. It is a semi-structured diagnostic interview to assess current and lifetime psychopathology. For the current study, we used a dichotomous variable to measure depressive disorder: (1) absence of a diagnosis and (2) presence of diagnosis (probable or confirmed clinical diagnosis).
Weight status
Trained interviewers measured height and weight using a Seca-digital weighing scale. Body Mass Index (BMI) was calculated (kg/m2), and BMI standard deviation scores (BMI Z-scores) were computed by comparing the child BMI with the BMI of the Spanish population of the same gender and age [48]. Z-BMI was categorized following the World Health Organization recommendations [49].
Age range
Age was calculated using the test date and the birth date reported by parents.
Socioeconomic-status (SES)
SES was determined by the Hollingshead Index [39], which considers education, occupation, gender, and marital status. It allows to obtain the place that a person occupies within the hierarchical structure of society ranging in level from 1 (lowest) to 5 (highest). To determine a child’s social status, scores for each primary caregiver are summed, and the total is divided by two.
Strategy of analysis
Deviation from preregistration
The analysis reported here deviates on one issue from our preregistration plan. To reduce potential bias, multiple imputation (MI) of the missing values has been performed and MI complete case analyses have additionally been conducted. Strategies to handle missing data were not covered in the preregistration.
Preliminary analyses and data preparation
All analyses were performed in SPSS version 26.0. The Shapiro–Wilk test and plots showed some non-normal distributions for depressive symptoms and BE scores. Outliers were winsorized, after which plots showed no extreme outliers and values of skewness and kurtosis were within the normal range (CDI at T0: 1.19 and 1.11; CDI at T1: 1.06 and 0.53; BES at T0: − 0.14 and − 1.21; BESAA at T1: − 0.14 and − 1.21). Participants’ descriptive statistics and weight-status group differences for all variables were examined. Because very few children were assessed as being depressed, we focused on depressive symptoms measured by CDI instead of depression diagnosis in the regression model. Of note, CDI scores at T1 showed to be highly correlated with the presence of depression based on the diagnosis interview at T1 (χ2 = 0.81, p < 0.001). Pearson correlations between variables included in the tested model were analyzed.
The data were tested for missingness using mean comparisons, logistic regression, and Little’s MCAR test [50]. The results of the attrition analyses, reported in the Supplementary Tables S2 and S3, showed that there is no discernable pattern to the attrition in the data. We subsequently performed MI of the missing values on depressive symptoms at follow-up, using the FSC method in SPSS. Following the recommendation that the number of imputations should be at least equal to the percentage of cases with missing data [51], m = 30 imputed data sets were created, with n = 100 observations each.
Hypothesis testing
The first and second hypothesis were tested using Student’s t tests and multiple regression analysis, respectively. To test the hypotheses three and four on mediation and moderated mediation, models 4 and 58 of the Hayes PROCESS macro in SPSS were employed [52]. We performed the analyses with weight-status category at T0 as the primary independent variable (IV), and depressive symptoms at T1 as the dependent variable (DV). We entered BE at T0 as mediator in the model, and gender as a moderator of the effect of (a path) the IV on the mediator and (b path) the mediator on the DV (see Fig. 1). Mediation is determined by testing the significance of the indirect effect (a × b) of the IV on the DV through the mediator. Moderated mediation occurs when the indirect effect varies across values of the moderator (conditional effect). The c′ path is the direct effect of the IV on the DV, controlled for the proposed moderated mediator effects. The 95% confidence intervals for the indirect effects were obtained using a 5000 bootstrap sample approach. Depressive symptoms at T0 were entered as a covariate to account for baseline symptoms. The effects were also controlled for age and SES.
The regression analyses and (moderated) mediation models were applied to both the subsample of participants with complete information and the imputed data sets with completed information. The MI estimates of the direct effects, their standard errors and associated p values, were obtained by pooling the parameters using Rubin’s rules [53]. To obtain bootstrap standard errors and 95% confidence intervals for the indirect effects, nonparametric bootstrapping was performed, with 5000 bootstrap samples drawn for each imputed data set, and the bootstrap inference results were thereupon pooled.
Results
Preliminary analyses
Descriptive statistics and weight groups’ differences for pre-imputed data are presented in Table 1. As can been seen, at both time points, the group with obesity showed higher scores on depressive symptoms (T0: t = − 3.20, p = 0.002, T1: t = − 2.84, p = 0.006) and lower scores on BE (T0: t = 8.64, p < 0.001, T1: t = 4.64, p < 0.001) compared to the normal-weight group. These results provide support for the first hypothesis of the current study. Note, however, that differences in depressive symptoms were statistically significant only for girls. Effect sizes (d) for all significant correlations ranged from 0.67 to 2.77, indicating moderate-to-large significant differences [54]. No significant differences were found for depression diagnosis at baseline, but the group with obesity had a significantly higher proportion of depression diagnoses at follow-up (χ2 = 8.30, p = 0.004). The correlations between all the variables included in the model are shown in Supplementary Table S4.
Subsequently, multiple regression analyses and analysis of (moderated) mediation were applied to both the complete and the completed (i.e., observed and imputed) data. As the results of the complete and the MI completed case analyses are rather similar, the latter are presented in the text (Tables 2, 3), and the former are displayed in the Supplementary material (Tables 5, 6).
Table 2.
Pooled parameter estimates for the regression of depressive symptoms at T1 on weight status at T0 from completed (observed plus imputed) case analysis (n = 100, m = 30)
| B | SE | p | |
|---|---|---|---|
| Constant | 4.378 | 1.234 | < 0.001 |
| Weight status T0 (1 = obesity) | 2.243 | 1.403 | 0.110 |
| Depressive symptoms T0 | 0.695 | 0.140 | < 0.001 |
| R2 | 0.334 |
Table 3.
Pooled parameter estimates of mediation and moderated mediation models from completed (observed plus imputed) case analysis (n = 100, m = 30)
| Mediation | Moderated mediation | |||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
| Body esteem T0 | ||||||
| Constant | 30.916 | 3.605 | < 0.001 | 30.506 | 3.556 | < 0.001 |
| Gender (1 = boys) | − 0.798 | 0.835 | 0.342 | 0.866 | 1.172 | 0.462 |
| Weight status T0 (1 = obesity) | − 8.061 | 0.851 | < 0.001 | − 6.721 | 1.074 | < 0.001 |
| Weight status T0 × gender | − 3.300 | 1.656 | 0.049 | |||
| Depressive symptoms T0 | − 0.504 | 0.081 | < 0.001 | − 0.522 | 0.080 | < 0.001 |
| Age T0 | − 0.586 | 0.310 | 0.061 | − 0.590 | 0.305 | 0.056 |
| SES T0 | − 0.116 | 0.484 | 0.812 | 0.133 | 0.477 | 0.780 |
| R2 | 0.657 | 0.671 | ||||
| Depressive symptoms T1 | ||||||
| Constant | 13.439 | 7. 289 | 0.065 | 16.720 | 7.605 | 0.028 |
| Gender | − 2.535 | 1.359 | 0.063 | − 6.960 | 3.276 | 0.034 |
| Weight status T0 | − 0.359 | 1.943 | 0.853 | − 0.358 | 1.928 | 0.853 |
| Body esteem T0 | − 0.337 | 0.170 | 0.048 | − 0.465 | 0.198 | 0.020 |
| Body esteem T0 × gender | 0.281 | 0.192 | 0.144 | |||
| Depressive symptoms T0 | 0.506 | 0.162 | 0.002 | 0.485 | 0.161 | 0.003 |
| Age T0 | 0.237 | 0.532 | 0.656 | 0.167 | 0.526 | 0.751 |
| SES T0 | − 0.757 | 0.746 | 0.311 | − 0.848 | 0.747 | 0.256 |
| R2 | 0.415 | 0.433 | ||||
| Effect | SE | p | Effect | SE | p | |
|---|---|---|---|---|---|---|
| Direct effects | ||||||
| Weight status T0 on body esteem T0 | − 8.061 | 0.851 | < 0.001 | |||
| Girls | − 6.721 | 1.074 | < 0.001 | |||
| Boys | − 10.021 | 1.293 | < 0.001 | |||
| Body esteem T0 on depressive symptoms T1 | − 0.337 | 0.170 | 0.048 | |||
| Girls | − 0.465 | 0.198 | 0.020 | |||
| Boys | − 0.184 | 0.188 | 0.330 | |||
| Weight status T0 on depressive symptoms T1 | − 0.359 | 1.943 | 0.853 | − 0.358 | 1.928 | 0.853 |
| Effect | Boot SE | Boot [LLCI, ULCI]* | Effect | Boot SE | Boot [LLCI, ULCI]* | |
|---|---|---|---|---|---|---|
| Indirect effect | ||||||
| Weight status T0 on depressive symptoms T1 via body esteem T0 | 2.717 | 1.434 | [0.016, 5.627] | |||
| Girls | 3.124 | 1.390 | [0.490, 5.923] | |||
| Boys | 1.842 | 2.006 | [− 1.923, 5.972] | |||
| Index of moderated mediation | ||||||
| Gender | − 1.282 | 1.799 | [− 4.654, 2.416] |
Significant p values and bootstrap 95% CI are in bold. Reference category for weight status T0 is normal weight, and for Gender girls
* Lower and upper level of 95% bootstrap confidence interval
Table 2 shows the results of the regression of depressive symptoms at follow-up on weight-status at baseline, with depressive symptoms at T0 entered as a covariate to account for baseline symptoms.
The table provides evidence that the second hypothesis should be rejected. Controlled for baseline depressive symptoms, there appeared to be no significant difference in depressive symptoms at T1 between children with obesity at baseline and those with normal weight (t = 1.60, p = 0.110).
Mediation and moderated mediation results
The mediation hypothesis 3 was tested using PROCESS model 4 by Hayes [52]. The results are displayed in Table 3.
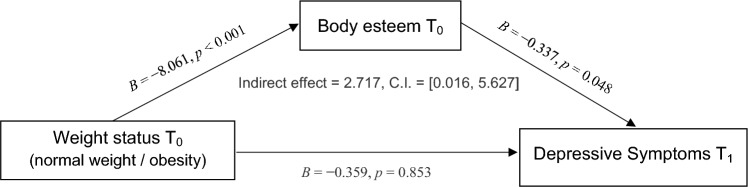
As can be seen, weight status had a significant negative effect on BE (B = − 8.601, p < 0.001), and BE had a significant negative effect on depressive symptoms (B = − 0.337, p = 0.048). The unconditional indirect effect of weight status on depressive symptoms through BE is positive (i.e., 2.717) and significantly different from zero (95% bootstrap C.I. [0.016, 5.627]). Hence, the third hypothesis, which argues that BE mediates the prospective association between childhood obesity and adolescent depressive symptoms, is supported. A graphical display of the mediation model results is provided in Fig. 2.
Fig. 2.
Diagram of mediation model results. Note that covariates (depressive symptoms, Age and SES at T0, and Gender) are included in the analyses but are not displayed in the figure
We subsequently tested the moderated mediation hypothesis 4 using PROCESS model 58 [52]. To facilitate interpretation, a bottom–up approach is used.
Analysis of path a showed no significant difference in BE between normal-weight boys and normal-weight girls (B = 0.866, p = 0.462). The interaction between weight status and gender, however, revealed a significant difference in BE between boys and girls with weight-status obesity, with boys with obesity having lower esteem than girls with obesity (B = − 3.300, p < 0.049). Among girls, a significant negative association was found between weight status and BE (B = − 6.721, p < 0.001). Among boys, the association between weight status and BE was B = − 10.021 (p < 0.001). Hence, controlled for the other predictor variables, girls with obesity are predicted to score 6.721 lower on BE at baseline than normal-weight girls, whereas boys with obesity 10.021 lower than normal-weight boys. Examination of path b revealed a significant negative effect of BE on depressive symptoms at T1 among girls (B = − 0.465, p < 0.020). This conditional effect for girls was not statistical different from the effect for boys (B = 0.281, p < 0.144). The direct effect of weight status on depressive symptoms at T1, corresponding to path c′, was also not significant.
With respect to mediation via BE and moderation by gender, the analysis revealed a significant positive indirect effect of weight status on depressive symptoms via BE of 3.124 for girls (95% bootstrap C.I. [0.490, 5.923]), and an insignificant effect of 1.842 for boys (95% bootstrap C.I. [− 1.923, 5.972]). The index of moderated mediation revealed that the difference between these conditional effects (i.e., − 1.282) was not significant (95% bootstrap C.I. [− 4.654, 2.416]). This implies that the mediation is not moderated by gender, so the fourth hypothesis should be rejected.
Discussion
The current prospective study filled an eminent gap in the literature by investigating the mediating role of BE in explaining the childhood obesity–adolescent depressive symptoms link. In addition, potential gender moderation was examined. We found that the link between childhood obesity and follow-up depressive symptoms was mediated through BE. We did not find significant evidence of gender moderation for the full mediation model.
In line with prior evidence [6–8] and the concurrent part of our hypothesis, children with obesity reported higher rates of depressive symptoms at baseline and follow-up compared to children without obesity. However, in contrast to the hypothesis, no evidence of a direct prospective association between childhood obesity and later depressive symptoms was found. Previous studies have also reported inconsistent results [7, 12], and comparison between studies is hampered by differences in age of the target group and time of follow-up. Of note, the meta-analysis by Mannan et al. [5] noted a stronger prospective association between obesity and depressive symptoms for females in young adulthood than in adolescence, and among studies with longer follow-up periods (more than 10 years). A recent MR study found a causal relationship from childhood obesity to depression in adulthood [13]. Future research with longer term follow-up is needed to further increase insight into the link between childhood obesity and late adolescent depressive symptoms.
Whereas we did not find any evidence for the direct link between weight status and the development of depressive symptoms, we found that BE mediated this association, which is in line with our hypothesis. Thus, our results suggest that it is not obesity in childhood (i.e., weight status) per se, but the effect of weight status on BE, that plays a prominent role in whether children with obesity develop more depressive symptoms during adolescence. Although some previous cross-sectional studies have also found some support for the mediating role of BE [26–32], our study is unique by examining this link prospectively from childhood to adolescence. As such, our findings provide important implications for future preventive interventions in this stage. Specifically, targeting low BE among children with obesity may reduce later depressive symptoms during adolescence. In turn, derived behavioral changes (i.e., decreased sedentary lifestyle, less emotional eating) may reduce obesity [55], helping to prevent the vicious cycle of obesity and depressive symptomatology. Our results revealed a significant indirect effect of weight status on depressive symptoms via BE for girls but not for boys. However, the index of moderated mediation was not significant, which means that the difference in indirect effects between boys and girls is not significantly different [52]. And this implies that BE-mediating effects do not differ by gender. Of note, one previous cross-sectional study found a mediation effect of BE among adolescent girls, but not boys [33]. It is possible that gender differences regarding the mediating effect of BE become more important when children become older. Further research is needed to examine this potential relationship.
Although BE mediation did not differ between boys and girls, the specific link between obesity and BE was stronger in boys compared to girls. Boys with obesity had lower BE compared to girls. This is a remarkable finding, as previous studies mostly reported similar associations between obesity and BE for boys and girls [18, 34]. An explanation for this finding might be that children with obesity are generally limited in doing sports, while these sport activities prove to be particularly important for body image among boys [56]. Moreover, McCabe et al. [57] pointed out that boys received more messages aimed at muscle gain. In this sense, BE refers to a nuanced concept that goes beyond weight status [14] and might also reflect the muscular ideal, which is particularly internalized by boys [58]. Future studies should further explore whether there are specific components of BE (i.e., weight, appearance) that are influenced by weight status. Finally, in contrast to our hypothesis, we found no evidence that gender moderated the association between BE and the development of depressive symptoms at follow-up. This finding is in line with some other studies [22, 37, 38], but there are also studies suggesting stronger links among females compared to males. One possible explanation relates to the increasing pressures regarding body ideals at younger ages also among boys [59].
Strengths, limitations, and future directions
Our study is based on a case–control design of children with and without obesity who were matched on important sociodemographic characteristics (i.e., SES, age) and who were followed over time. Our prospective design and the matching are notable strengths. However, there are also some limitations that should be acknowledged. First, although we prospectively examined the development of depressive symptoms over time, the IV and the mediator were assessed at the same time point. For further studies, it would be relevant to test for competing explanations, such as the role of weight bias and weight teasing on BE and depressive symptoms [60]. Moreover, our sample comes from a specific region of Spain. This may limit the generalizability of the results. Finally, while our sample size is relatively small, the case–control design lowered the need to control for various covariates. Moreover, we have imputed missing data and findings were rather similar for complete and completed (i.e., observed and imputed) case analyses. Nevertheless, future studies are encouraged to recruit larger, representative samples. To help guide sample size decisions for such a study, post hoc Monte Carlo power analysis for the unconditional indirect effect in this study, with sample size set to n = 100 and α set to 0.05, revealed an acceptable power of 0.76 [61]. Following Aberson et al. [62], to achieve similar statistical power for the conditional indirect effects in the moderated mediation model, a sample size of 2n is recommended.
Conclusions
The current study provides evidence that BE mediates the prospective association between childhood obesity and adolescent depressive symptoms. We did not find significant evidence that gender moderates this mediation. Future studies with larger sample sizes and longer term follow-ups are urged to re-examine this moderated mediation. The findings may have important implications for clinical practice. Future clinical preventive intervention trials should examine whether improving BE in high-risk children (i.e., children with obesity) reduces the development of adolescent depressive symptoms.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Dr. Sepulveda had a postdoctoral Ramon and Cajal scholarship from the Spanish Ministry of Science and Innovation (RYC‐2009‐ 05092) to carry out this project. Ms. L. Beltrán and Ms. Blanco were awarded a Research Fellowship from (FPU) for students of Ph.D. programs. The authors thank pediatricians, nurses, the headmaster, and teachers at the schools for their involvement in the recruitment process. The authors would also like to recognize all the research group’s colleagues (www.anobas.es) (C. Bustos, L. Cabrera, S. Solano, T. Lacruz, T. Moreno, A. Román, M. Rojo, B. Quirós, and S. Rodríguez) for their involvement in the assessment process. The authors also express our gratitude to all the children and their families who participated in this study.
Author contributions
LBG drafted the article. JKL revised it critically for important intellectual content. RE contributed to analysis and interpretation of data for the article, and prepared tables and figures. ARS have made a substantial contribution to the design of the article. All authors reviewed the manuscript, provided guidance, and edits.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. The authors did not receive financial support from any organization for the submitted work.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Compliance with ethical standards
The study received ethical approval from the Ethics Committee of The Niño Jesus Children Hospital (T0: Ref. 0009/10, T1: Ref.0076/18) and the Research Ethics Committee of University Autonomous of Madrid (T0: CEI 27–673, T1: CEI-98-103). All procedures performed in this study involving human participants were under the ethical standards and with de Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all the surveyed participants and their parents.
Footnotes
Junilla K. Larsen and Rob Eisinga have contributed equally to this work.
Contributor Information
Lucia Beltrán-Garrayo, Email: lucia.beltran@uam.es.
Ana Rosa Sepúlveda, Email: anarosa.sepulveda@uam.es.
References
- 1.Salk RH, Hyde JS, Abramson LY (2017) Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull 143(8):783–822. 10.1037/bul0000102 10.1037/bul0000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naicker K, Galambos NL, Zeng Y, Senthilselvan A, Colman I (2013) Social, demographic, and health outcomes in the 10 years following adolescent depression. J Adolesc Health 52(5):533–538. 10.1016/j.jadohealth.2012.12.016 10.1016/j.jadohealth.2012.12.016 [DOI] [PubMed] [Google Scholar]
- 3.Davis M, Jones JD, So A, Benton TD, Boyd RC, Melhem N et al (2022) Adolescent depression screening in primary care: who is screened and who is at risk? J Affect Disord 299:318–325. 10.1016/j.jad.2021.12.022 10.1016/j.jad.2021.12.022 [DOI] [PubMed] [Google Scholar]
- 4.Chen W, Feng J, Jiang S, Guo J, Zhang X, Zhang X et al (2023) Mendelian randomization analyses identify bidirectional causal relationships of obesity with psychiatric disorders. J Affect Disord 339:807–814. 10.1016/j.jad.2023.07.044 10.1016/j.jad.2023.07.044 [DOI] [PubMed] [Google Scholar]
- 5.Mannan M, Mamun A, Doi S, Clavarino A (2016) Prospective associations between depression and obesity for adolescent males and females—a systematic review and meta-analysis of longitudinal studies. PLoS ONE 11(6):e0157240. 10.1371/journal.pone.0157240 10.1371/journal.pone.0157240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quek YH, Tam WW, Zhang MW, Ho RC (2017) Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes Rev 18(7):742–754. 10.1111/obr.12535 10.1111/obr.12535 [DOI] [PubMed] [Google Scholar]
- 7.Mühlig Y, Antel J, Föcker M, Hebebrand J (2016) Are bidirectional associations of obesity and depression already apparent in childhood and adolescence as based on high-quality studies? A systematic review. Obes Rev 17(3):235–249. 10.1111/obr.12357 10.1111/obr.12357 [DOI] [PubMed] [Google Scholar]
- 8.Rao WW, Zong QQ, Zhang JW, An FR, Jackson T, Ungvari GS et al (2020) Obesity increases the risk of depression in children and adolescents: results from a systematic review and meta-analysis. J Affect Disord 267:78–85. 10.1016/j.jad.2020.01.154 10.1016/j.jad.2020.01.154 [DOI] [PubMed] [Google Scholar]
- 9.van den Broek N, Treur JL, Larsen JK, Verhagen M, Verweij KJH, Vink JM (2018) Causal associations between body mass index and mental health: a Mendelian randomisation study. J Epidemiol Community Health 72(8):708–710. 10.1136/jech-2017-210000 10.1136/jech-2017-210000 [DOI] [PubMed] [Google Scholar]
- 10.Speed MS, Jefsen OH, Børglum AD, Speed D, Østergaard SD (2019) Investigating the association between body fat and depression via Mendelian randomization. Transl Psychiatry 9(1):184. 10.1038/s41398-019-0516-4 10.1038/s41398-019-0516-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pistis G, Milaneschi Y, Vandeleur CL, Lasserre AM, Penninx BW, Lamers F et al (2021) Obesity and atypical depression symptoms: findings from Mendelian randomization in two European cohorts. Transl Psychiatry 11(1):96. 10.1038/s41398-021-01236-7 10.1038/s41398-021-01236-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kanellopoulou A, Antonogeorgos G, Douros K, Panagiotakos DB (2022) The association between obesity and depression among children and the role of family: a systematic review. Children 9(8):1244. 10.3390/children9081244 10.3390/children9081244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yan S-S, Xu Q, Han B-X, Ni J-J, Wei X-T, Feng G-J, Zhang H, Zhang Y-J, Zhang L, Yu W-Y, Pei Y-F (2022) Mendelian randomization analysis identified causal Association of Childhood Obesity with adult major depressive disorder. Pediatr Obes 17(12):e12960. 10.1111/ijpo.12960 10.1111/ijpo.12960 [DOI] [PubMed] [Google Scholar]
- 14.Mendelson BK, Mendelson MJ, White DR (2001) Body-esteem scale for adolescents and adults. J Pers Assess 76(1):90–106. 10.1207/S15327752JPA7601_6 10.1207/S15327752JPA7601_6 [DOI] [PubMed] [Google Scholar]
- 15.Markowitz S, Friedman MA, Arent SM (2008) Understanding the relation between obesity and depression: causal mechanisms and implications for treatment. Clin Psychol Sci Pract 15(1):1–20. 10.1111/j.1468-2850.2008.00106.x 10.1111/j.1468-2850.2008.00106.x [DOI] [Google Scholar]
- 16.Preiss K, Brennan L, Clarke D (2013) A systematic review of variables associated with the relationship between obesity and depression. Obes Rev 14(11):906–918. 10.1111/obr.12052 10.1111/obr.12052 [DOI] [PubMed] [Google Scholar]
- 17.Pont SJ, Puhl R, Cook SR, Slusser W (2017) Stigma experienced by children and adolescents with obesity. Pediatrics 140(6):e20173034. 10.1542/peds.2017-3034 10.1542/peds.2017-3034 [DOI] [PubMed] [Google Scholar]
- 18.Ricciardelli LA, McCabe MP, Holt KE, Finemore J (2003) A biopsychosocial model for understanding body image and body change strategies among children. J Appl Dev Psychol 24(4):475–495. 10.1016/S0193-3973(03)00070-4 10.1016/S0193-3973(03)00070-4 [DOI] [Google Scholar]
- 19.Moradi M, Mozaffari H, Askari M, Azadbakht L (2020) Association between overweight/obesity with depression, anxiety, low self-esteem, and body dissatisfaction in children and adolescents: a systematic review and meta-analysis of observational studies. Crit Rev Food Sci Nutr 62(2):555–570. 10.1080/10408398.2020.1823813 10.1080/10408398.2020.1823813 [DOI] [PubMed] [Google Scholar]
- 20.Sanders RH, Han A, Baker JS, Cobley S (2015) Childhood obesity and its physical and psychological co-morbidities: a systematic review of Australian children and adolescents. Eur J Pediatr 174(6):715–746. 10.1007/s00431-015-2551-3 10.1007/s00431-015-2551-3 [DOI] [PubMed] [Google Scholar]
- 21.McLean SA, Rodgers RF, Slater A, Jarman HK, Gordon CS, Paxton SJ (2022) Clinically significant body dissatisfaction: prevalence and association with depressive symptoms in adolescent boys and girls. Eur Child Adolesc Psychiatry 31(12):1921–1932. 10.1007/s00787-021-01824-4 10.1007/s00787-021-01824-4 [DOI] [PubMed] [Google Scholar]
- 22.Bornioli A, Lewis-Smith H, Slater A, Bray I (2021) Body dissatisfaction predicts the onset of depression among adolescent females and males: a prospective study. J Epidemiol Community Health 75(4):343–348. 10.1136/jech-2019-213033 10.1136/jech-2019-213033 [DOI] [PubMed] [Google Scholar]
- 23.Duchesne A-P, Dion J, Lalande D, Bégin C, Émond C, Lalande G, McDuff P (2017) Body dissatisfaction and psychological distress in adolescents: is self-esteem a mediator? J Health Psychol 22(12):1563–1569. 10.1177/1359105316631196 10.1177/1359105316631196 [DOI] [PubMed] [Google Scholar]
- 24.Ramos P, Moreno-Maldonado C, Moreno C, Rivera F (2019) The role of body image in internalizing mental health problems in Spanish adolescents: an analysis according to sex, age, and socioeconomic status. Front Psychol 10:1952. 10.3389/fpsyg.2019.01952 10.3389/fpsyg.2019.01952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharpe H, Patalay P, Choo T-H, Wall M, Mason SM, Goldschmidt AB, Neumark-Sztainer D (2018) Bidirectional associations between body dissatisfaction and depressive symptoms from adolescence through early adulthood. Dev Psychopathol 30(4):1447–1458. 10.1017/S0954579417001663 10.1017/S0954579417001663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaiton M, Sabiston C, O’Loughlin J, McGrath JJ, Maximova K, Lambert M (2009) A structural equation model relating adiposity, psychosocial indicators of body image and depressive symptoms among adolescents. Int J Obes 33(5):588–596. 10.1038/ijo.2009.43 10.1038/ijo.2009.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Friedman KE, Reichmann SK, Costanzo PR, Musante GJ (2002) Body image partially mediates the relationship between obesity and psychological distress. Obes Res 10(1):33–41. 10.1038/oby.2002.5 10.1038/oby.2002.5 [DOI] [PubMed] [Google Scholar]
- 28.Gavin AR, Simon GE, Ludman EJ (2010) The association between obesity, depression, and educational attainment in women: the mediating role of body image dissatisfaction. J Psychosom Res 69(6):573–581. 10.1016/j.jpsychores.2010.05.001 10.1016/j.jpsychores.2010.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mond J, Van den Berg P, Boutelle K, Hannan P, Neumark-Sztainer D (2011) Obesity, body dissatisfaction, and emotional well-being in early and late adolescence: findings from the project EAT study. J Adolesc Health 48(4):373–378. 10.1016/j.jadohealth.2010.07.022 10.1016/j.jadohealth.2010.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ozmen D, Ozmen E, Ergin D, Cetinkaya AC, Sen N, Dundar PE, Taskin EO (2007) The association of self-esteem, depression and body satisfaction with obesity among Turkish adolescents. BMC Public Health 7(1):80. 10.1186/1471-2458-7-80 10.1186/1471-2458-7-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weinberger N-A, Kersting A, Riedel-Heller SG, Luck-Sikorski C (2018) The relationship between weight status and depressive symptoms in a population sample with obesity: the mediating role of appearance evaluation. Obes Facts 11(6):514–523. 10.1159/000492000 10.1159/000492000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sutaria S, Devakumar D, Yasuda SS, Das S, Saxena S (2018) Is obesity associated with depression in children? Systematic review and meta-analysis. Arch Dis Child 104(1):64–74. 10.1136/archdischild-2017-314608 10.1136/archdischild-2017-314608 [DOI] [PubMed] [Google Scholar]
- 33.Xie B, Unger JB, Gallaher P, Johnson CA, Wu Q, Chou C-P (2010) Overweight, body image, and depression in Asian and Hispanic adolescents. Am J Health Behav 34(4):476–488. 10.5993/AJHB.34.4.9 10.5993/AJHB.34.4.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shriver LH, Harrist AW, Page M, Hubbs-Tait L, Moulton M, Topham G (2013) Differences in body esteem by weight status, gender, and physical activity among young elementary school-aged children. Body Image 10(1):78–84. 10.1016/j.bodyim.2012.10.005 10.1016/j.bodyim.2012.10.005 [DOI] [PubMed] [Google Scholar]
- 35.Hankin BL, Abramson LY (2001) Development of gender differences in depression: an elaborated cognitive vulnerability–transactional stress theory. Psychol Bull 127(6):773–796. 10.1037/0033-2909.127.6.773 10.1037/0033-2909.127.6.773 [DOI] [PubMed] [Google Scholar]
- 36.Bearman SK, Stice E (2008) Testing a gender additive model: the role of body image in adolescent depression. J Abnorm Child Psychol 36(8):1251–1263. 10.1007/s10802-008-9248-2 10.1007/s10802-008-9248-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Holsen I, Kraft P, Røysamb E (2001) The relationship between body image and depressed mood in adolescence: a 5-year longitudinal panel study. J Health Psychol 6(6):613–627. 10.1177/135910530100600601 10.1177/135910530100600601 [DOI] [PubMed] [Google Scholar]
- 38.Paxton SJ, Neumark-Sztainer D, Hannan PJ, Eisenberg ME (2006) Body dissatisfaction prospectively predicts depressive mood and low self-esteem in adolescent girls and boys. J Clin Child Adolesc Psychol 35(4):539–549. 10.1207/s15374424jccp3504_5 10.1207/s15374424jccp3504_5 [DOI] [PubMed] [Google Scholar]
- 39.Hollingshead AB (1975) Four factor index of social status. Unpublished manuscript. Yale University, New Haven, CT
- 40.Sepulveda AR, Blanco M, Nova E, Marcos A, Martínez SG, Carrobles JA, Graell M (2019) Identifying the relationship between biological, psychosocial and family markers associated with childhood obesity: case-control “ANOBAS” study. Psychoneuroendocrinology 110:104428. 10.1016/j.psyneuen.2019.104428 10.1016/j.psyneuen.2019.104428 [DOI] [PubMed] [Google Scholar]
- 41.Mendelson BK, White DR (1982) Relation between body-esteem and self-esteem of obese and normal children. Percept Mot Skills 54(3):899–905. 10.2466/pms.1982.54.3.899 10.2466/pms.1982.54.3.899 [DOI] [PubMed] [Google Scholar]
- 42.De Gracia M, Marcó M, Trujano P (2007) Factores asociados a la conducta alimentaria en preadolescentes. Psicothema 19:646–653 [PubMed] [Google Scholar]
- 43.Beltrán-Garrayo L, Mercado-Garrido E, Román FJ, Rojo M, Sepúlveda AR (2022) Assessing body esteem in adolescents: psychometric properties of the Spanish version of the Body Esteem Scale (BESAA-S). Child Youth Care Forum 52:683–701. 10.1007/s10566-022-09705-w 10.1007/s10566-022-09705-w [DOI] [Google Scholar]
- 44.Kovacs M (1992) Child Depression Inventory (CDI). APA PsycTests. 10.1037/t19482-000 10.1037/t19482-000 [DOI] [Google Scholar]
- 45.Del Barrio V, Carrasco MA (2004) CDI. Inventario de depresión infantil. TEA Ediciones, Madrid [Google Scholar]
- 46.Kaufman J, Birmaher B, Brent D, Rao UMA, Flynn C, Moreci P et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36(7):980–988. 10.1097/00004583-199707000-00021 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- 47.Arechavaleta B, Foulliux C, Martínez P, Hernández L, Domínguez E, de la Peña F (2006) Interrater reliability of the Spanish version of schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL). Actas Esp Psiquiatr 35(1):36–40 [PubMed] [Google Scholar]
- 48.Sobradillo B, Aguirre A, Aresti U, Bilbao A, Fernández Ramos C, Lizárraga A, Lorenzo H, Madariaga L, Rica I, Ruiz I, Sánchez E, Santamariá C, Serrano JM, Zabala A, Zurimendi B, Hernández M (2014) Curvas y Tablas de Crecimiento. Estudios longitudinal y transversal. Fundación Faustino Orbegozo
- 49.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85(9):660–667. 10.2471/blt.07.043497 10.2471/blt.07.043497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Little RJA (1988) A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc 83(404):1198–1202. 10.1080/01621459.1988.10478722 10.1080/01621459.1988.10478722 [DOI] [Google Scholar]
- 51.White IR, Royston P, Wood AM (2011) Multiple imputation using chained equations: issues and guidance for practice. Stat Med 30(4):377–399. 10.1002/sim.4067 10.1002/sim.4067 [DOI] [PubMed] [Google Scholar]
- 52.Hayes AF (2017) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Press, New York [Google Scholar]
- 53.Rubin DB (1987) Multiple imputation for nonresponse in surveys. Wiley, New York [Google Scholar]
- 54.Cohen J (1988) Statistical power analysis for the behavioral science. Elrbaum, Hillsdale, NJ [Google Scholar]
- 55.Smith JD, Egan KN, Montaño Z, Dawson-McClure S, Jake-Schoffman DE, Larson M, St. George SM (2018) A developmental cascade perspective of paediatric obesity: a conceptual model and scoping review. Health Psychol Rev 12(3):271–293. 10.1080/17437199.2018.1457450 10.1080/17437199.2018.1457450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Allen CP, Telford RM, Telford RD, Olive LS (2019) Sport, physical activity and physical education experiences: associations with functional body image in children. Psychol Sport Exerc 45:101572. 10.1016/j.psychsport.2019.101572 10.1016/j.psychsport.2019.101572 [DOI] [Google Scholar]
- 57.McCabe MP, Ricciardelli LA, Holt K (2010) Are there different sociocultural influences on body image and body change strategies for overweight adolescent boys and girls? Eat Behav 11(3):156–163. 10.1016/j.eatbeh.2010.01.005 10.1016/j.eatbeh.2010.01.005 [DOI] [PubMed] [Google Scholar]
- 58.Lewis-Smith H, Garbett K, Chaudhry A, Uglik-Marucha N, Vitoratou S, Dhillon M, Shroff H, Diedrichs PC (2021) Adaptation and validation of the Internalisation-General subscale of the Sociocultural Attitudes Towards Appearance Questionnaire (SATAQ-3) in English among urban Indian adolescents. Body Image 36:254–262. 10.1016/j.bodyim.2020.12.004 10.1016/j.bodyim.2020.12.004 [DOI] [PubMed] [Google Scholar]
- 59.Maheux AJ, Roberts SR, Nesi J, Widman L, Choukas-Bradley S (2022) Longitudinal associations between appearance-related social media consciousness and adolescents’ depressive symptoms. J Adolesc 94(2):264–269. 10.1002/jad.12009 10.1002/jad.12009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Warnick JL, Darling KE, West CE, Jones L, Jelalian E (2022) Weight stigma and mental health in youth: a systematic review and meta-analysis. J Pediatr Psychol 47(3):237–255. 10.1093/jpepsy/jsab110 10.1093/jpepsy/jsab110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schoemann A, Boulton A, Short S (2017) Determining power and sample size for simple and complex mediation models. Soc Psychol Pers Sci 8(4):379–386. 10.1177/1948550617715068 10.1177/1948550617715068 [DOI] [Google Scholar]
- 62.Aberson CL, Bostyn DH, Carpenter T, Conrique BG, Giner-Sorolla R, Lewis Jr NA, Montoya AM, Ng BW, Reifman A, Schoemann AM, Soderberg C (2020) Techniques and solutions for sample size determination in psychology: supplementary material for “power to detect what? Considerations for planning and evaluating sample size”. [Unpublished manuscript] [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.