Abstract
Nearly 14% of American children aged 2–5 have obesity, with higher rates in children from lower-income and Black families. While evidence connects neighborhood socioeconomic environment (SEE) and obesity in adults and adolescents, little is known of this relationship in young children. We compared measures of SEE and family-level socio-demographic factors as predictors of obesity at age two. Methods: Family-level data from the PREVAIL Cohort, a CDC-funded birth cohort in Cincinnati, Ohio, were collected prenatally from the mothers. Residential addresses were geocoded and assigned validated measures of census tract-level SEE, including USDA food desert indicators and the Deprivation Index. Family-level and ecological SEE were compared as predictors of obesity (BMIz ≥1.65) at age two in terms of proportional differences, relative risk, and model fit statistics. Results: Residing outside of Deprivation Index High SEE neighborhoods was significantly associated with higher proportion (20.0% vs 5.9%; χ2 = 4.36, p = 0.037) and increased risk of obesity in univariable (RR = 3.4, 95%CI: 1.26–13.86) and multivariable models (RR = 3.5, 95%CI: 1.06–11.71). There were no differences in proportion or risk of obesity by USDA food desert indicators or family-level factors. Models using categorical Deprivation Index performed better than the family-level and the USDA food desert variables in terms of model fit. Conclusion: In the PREVAIL Cohort, only category of Deprivation Index was a significant predictor of obesity in two-year-old children. Future studies are needed to evaluate the Deprivation Index as a generalizable tool to identify neighborhoods at higher risk for obesity.
Keywords: childhood obesity, food deserts, neighborhood deprivation, social determinants of health
Introduction
Childhood obesity is a growing epidemic in the United States (US) and increases risks for a wide range of metabolic, vascular, and endocrine disorders throughout life (1, 2). Although children aged 12–19 years have the highest obesity rates in childhood (20.7%), nearly 14% of children 2 – 5 years of age meet obesity criteria, a rate that has more than doubled in the last five decades, with significant differences by income category, family education level, race, and ethnicity (3–5). This is especially important, as early childhood obesity is a strong predictor of obesity and obesity-related comorbidities in adolescence and adulthood and can contribute to health disparities in low income and minority populations throughout life (1, 2, 6).
Evidence shows that weight status and obesity in older children and adults is intimately connected to a network of social, structural, racial, and economic differences in family and neighborhood environments (7–12). While this relationship in younger children is understudied, factors that influence parent and sibling weight status are shown to affect the weight status of younger children in the household (13, 14) and socio-demographic measures associated with differences in child obesity risk are correlated with residential neighborhood (15, 16).
However, most studies in the US linking environmental indicators and childhood obesity have focused on the food access environment (i.e., food deserts) rather than socio-economic environment (SEE) and have reported inconsistent results. Two recent systematic reviews found that, while results were generally supportive of a connection between neighborhood food environments and child obesity, results were inconsistent (17, 18). Mei et al. (18) hypothesized that the inconsistency in findings could be due to contextual factors such as individual family characteristics, including race, income, and education; Cobb et al. (17) identified a differential effect between food access and obesity when stratifying children by aggregate neighborhood income, suggesting that food access alone is not a sufficient measure of neighborhood environment.
A validated, national source of ecological socioeconomic and food access data is the US Census Bureau’s annual American Community Survey (ACS) (19). The ACS includes detailed questions regarding social and economic status, such as education level, use of social services, family income, and vehicle ownership. Data are compiled by US census tract, which is generally aligned with neighborhoods in urban environments, and has been used to create two validated sources of census tract-level measures of SEE, the USDA Food Access Research Atlas (formerly the Food Desert Locator) (20) and the Deprivation Index (21).
The Food Access Research Atlas contains multiple measures of food and socio-economic environment, including several binary indicators of census tract fresh food access and availability. Food Access Research Atlas variables are used widely to designate food deserts and have been correlated to higher rates of obesity in adults and school-aged children (22, 23). However, these binary variables have been inconsistently associated with earlier childhood obesity, may not fully reflect community socio-economic environment, and have been shown to more accurately reflect issues of access in rural than in urban neighborhoods (18, 24–28).
The Deprivation Index is a more granular measure of SEE that standardizes census tract aggregate material deprivation (19, 21). Although similar material deprivation indices have been shown to predict child weight status in other Western countries (29), and differences in other child health outcomes have been found by Deprivation Index score (21,30,31), the Deprivation Index has not, to our knowledge, been used in studies of childhood obesity in the US.
Here, we apply these validated measures of fresh food access and neighborhood material deprivation compared with individual family-level factors as potential predictors of risk of early childhood obesity. While both of these indices have been used previously to quantify neighborhood environment, validating USDA and Deprivation Index measures as predictors for obesity in young children could provide a powerful tool to guide public health initiatives by identifying regions of early disparities in weight status, potentially breaking the cycle of obesity and obesity-related health disparities in low-income and minority populations (see Figure 1).
Figure 1.
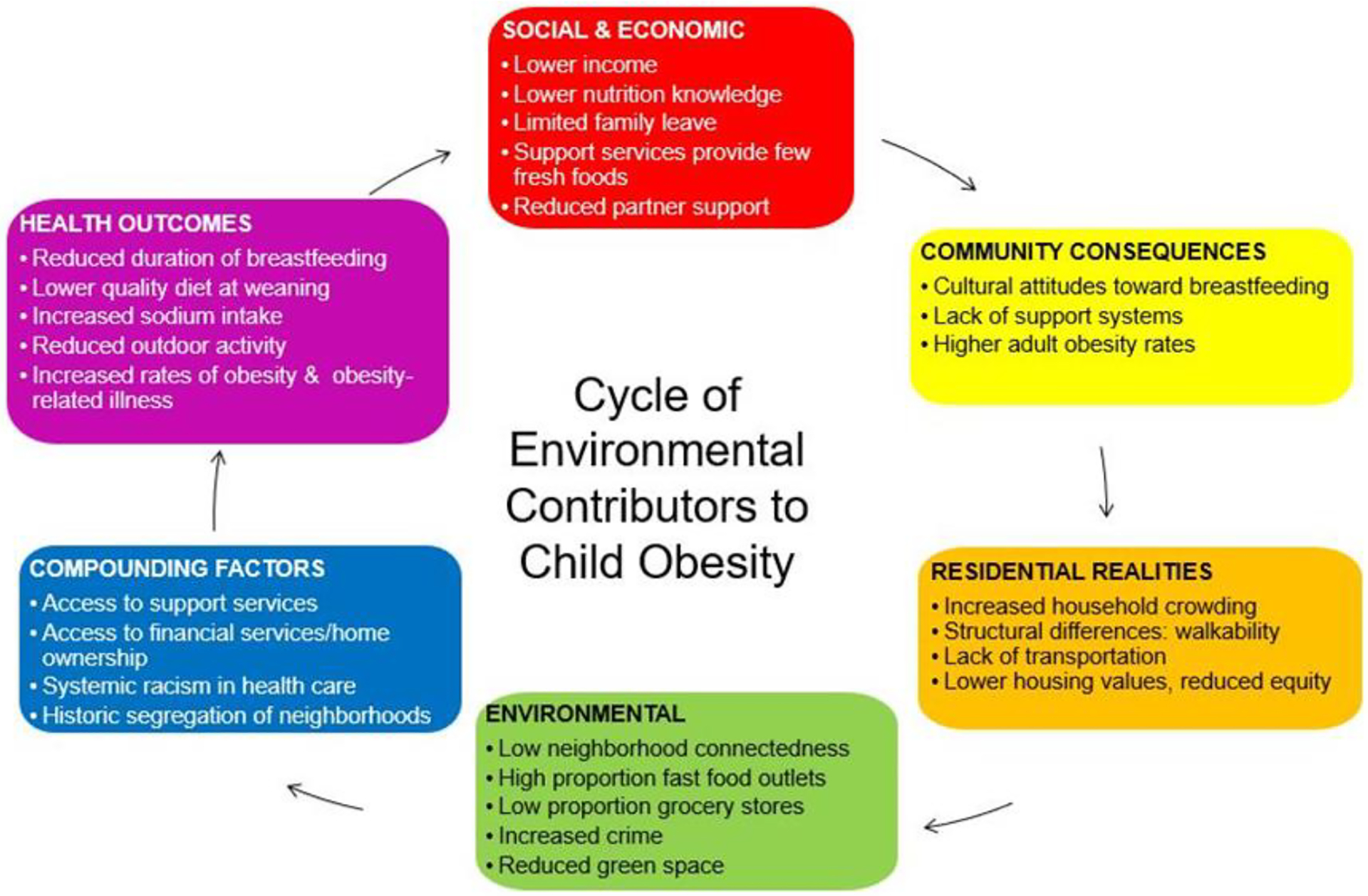
The environmental influences on childhood obesity. Childhood obesity is intimately linked to social, racial and economic differences in neighborhood environments (12). These differences contribute in myriad ways to a cycle of obesity and obesity-related comorbidities in low income and minority populations. While evidence of food access as a contributor to early childhood obesity has been mixed (17, 18) environmental factors, such as green space, neighborhood safety, and access to health care, are shown to predict obesity status in older children and adults (7, 8), while individual factors, such as race and income, are associated with both one’s residential neighborhood and obesity risk (11, 15).
Methods
The Pediatric Respiratory and Enteric Virus Acquisition and Immunogenesis Longitudinal Cohort (PREVAIL), a prospective two-year birth cohort study in Cincinnati, Ohio, was approved by the Institutional Review Boards at the US Centers for Disease Control and Prevention (CDC) and Cincinnati Children’s Hospital Medical Center. Participant enrollment began in April of 2017, and data collection was completed in October 2020. Study methods, including recruitment, enrollment, and data collection have previously been described (32); methods relevant to this work are described here. Inclusion criteria for the study were maternal age ≥18 years and delivery of a healthy, live-born, singleton infant at one of two urban study hospitals. Exclusion criteria included living more than 20 miles from the birth hospital, illicit drug use, major congenital anomaly in the infant, gestational age under 35 weeks, or HIV infection. Provisional enrollment occurred in the third trimester of pregnancy, and final eligibility and study enrollment was determined at a two-week postpartum home visit. Mother-infant dyads were followed from birth until age two through weekly text surveillance and periodic in-clinic study visits. This analysis is a subset of the PREVAIL Cohort, including only those subjects who completed the end-of-study (month 24) visit.
Family-level data
Family-level socio-demographic data were collected in-person at baseline (third trimester of pregnancy). Maternal race was categorized as White, Black, or other (biracial, Asian, Native American, Pacific Islander, or unknown). Due to the small number of participants who identified as Hispanic, ethnicity was not included as a covariate in this analysis; subjects who identified as ethnically Hispanic were included in their self-identified racial group. Maternal education level was defined as completion of any post-secondary education or training (>HS) or less (≤HS). Maternal marital status was defined as married or not, independent of cohabitation status, while living with a partner was defined as cohabitation with a significant other, independent of marital status. Insurance status was categorized as public or private, with the few families reporting either no insurance or use of both public and private insurance classified as publicly insured. Family income level was grouped in line with the Federal Poverty Level for a family of four (< $25,000/year), between 100% and 200% of Federal Poverty Level ($25,000-$50,000/year) and above (>$50,000/year). Maternal age was calculated based on the mother’s age at the time of the child’s birth.
Maternal weight and height from the first trimester of pregnancy were abstracted from the obstetrics medical record for nearly all (94.7%) mothers. When this time point was not available, the maternal-recalled height and pre-pregnancy weight was used. Maternal BMI was calculated as kg/m2 and presence of obesity was defined as a BMI of ≥30 (33). Sensitivity analysis found no significant differences when excluding mothers with recalled weight and height from analysis.
Neighborhood data
Family residential address was reported at the baseline visit and updated, if changed, in REDCap data management software (34). All PREVAIL subject addresses were geocoded to the census tract-level using DeGAUSS software (35). To quantify neighborhood fresh food access, we assigned corresponding 2015 USDA Food Access Research Atlas variables: Low Income (a high percentage of the population at or below the federal poverty level or median income of the region), Low Access (≥100 residents of the tract live more than one-half mile (urban) or 10 miles (rural) from a grocery store and do not own a vehicle) and Low Income/Low Access (LILA, census tracts that meet both Low Income and Low Access criteria) (20). The USDA variables that corresponded to the month 24 visit were used for all analyses.
To quantify neighborhood material deprivation, we assigned Deprivation Index scores (21). The Deprivation Index combines six ACS census tract-level variables: 1) percentage of vacant homes, 2) median home value; and the percentage of the population who 3) are without a high school diploma, 4) have used any government social-services or income support within 12 months, 5) lack health insurance, and 6) meet the federal definition of poverty, using a principal components analysis (19, 21). The score was then standardized into a continuous variable between 0 and 1, with increasing score representing increasing neighborhood deprivation (21).
Deprivation Index category was calculated by first averaging each family’s Deprivation Index scores from all visits, then calculating quartiles of scores from the averages. Census tracts were grouped by quartile of score into High SEE (least deprived quartile), High-Mid and Low-Mid (intermediate quartiles) and Low SEE (most deprived quartile). As children in middle- and low-income families have been shown to have significantly different obesity rates than those in the highest income bracket (5), a binary variable indicating residence in the High SEE quartile or the remaining cohort (Not High SEE) was also assessed. The Deprivation Index score and category that corresponded to the month 24 study visit were used for all analyses. A map of Deprivation Index and LILA census tracts included in this analysis can be found in Figure 2.
Figure 2.
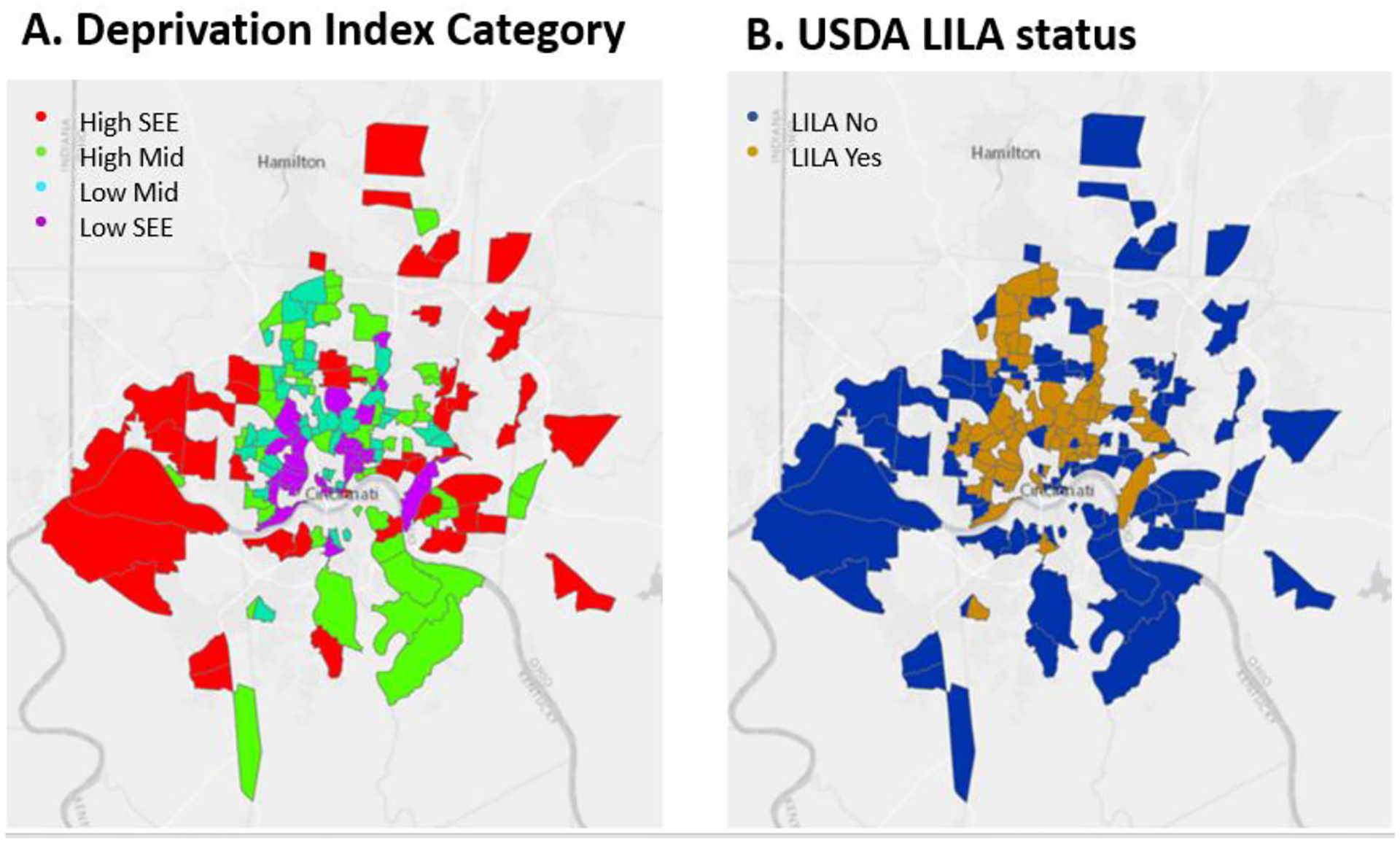
Maps of the PREVAIL Cohort catchment area categorized by measures of census tract socio-economic environment. Maps of census tracts included in the PREVAIL Cohort, a CDC-funded birth cohort in Cincinnati, OH, color-coded by Deprivation Index Category (A) and USDA Low Income/Low Access (LILA, B) status. Residential addresses were geocoded to the census tract level and assigned Deprivation Index (21) and USDA Food Access Research Atlas (20) indicators of socio-economic environment (SEE). Deprivation Index category was assigned based on quartile of score, with the lowest quartile of scores indicating the least deprived census tracts (High SEE) and highest quartile of scores designated as the most deprived census tracts (Low SEE). LILA designation was used to identify census tracts that met both USDA Low Income and Low Access criteria, a frequently used food desert indicator.
Child obesity status
Age and sex normative body mass index z scores (BMIz) from the 24-month study visit were calculated using the parameters provided by the CDC National Center for Health Statistics (36). Presence of obesity was defined as a BMIz score ≥1.65 at age two (37). Imputation for erroneous entries (< 0.5% of all entries) was performed by averaging the BMIz score from the two proximal visits. Sensitivity analysis found no significant differences in obesity rates due to these imputations.
Statistical analysis
Power was calculated post-hoc, based on the number that completed the month 24 study visit. All analytic methods had at least 80% power to detect a minimum of 1.75-fold increase in obesity risk at a significance level of 0.05.
Fisher’s exact test was used to identify differences in proportions for categorical and Kruskal-Wallis identified differences in medians of continuous family-level factors by SEE categories. Spearman correlations were calculated between each family socio-demographic factor and neighborhood SEE indicator. Differences in obesity proportions were tested using a Pearson χ2 test with Yates continuity corrections. Log binomial regression assessed risk of obesity at 24 months of age, first in univariable models with each measure, then as multivariable models with Deprivation Index score, category, or LILA designation and family measures that met non-multi-collinearity criteria and produced converged models. Model fit was assessed by comparing each model’s Akaike Information Criteria (AIC), the percent of variance explained by the model (R2), and the Area Under the Receiver Operator Characteristic Curve (AUROC), with higher AUROC and R2 and lower AIC associated with better model fit and an AUROC ≥ 0.70 considered adequate predictive value. Models were compared to each other using DeLong’s test for correlated AUROC, with a significant test indicating a significant difference in predictive accuracy between models.
Comparisons were made with the highest SEE category as the reference group unless otherwise specified. The continuous Deprivation Index score was base 10 log-transformed for all analyses. Results are reported as estimate and 95% confidence interval, except where indicated. All analysis was performed using the R Environment for Statistical Computing (38).
Results
PREVAIL enrolled a total of 245 participants, of which 171 (69.8%) completed the month 24 visit and were included in this analysis (see Table 1).
Table 1.
Family-level socio-demographics of the PREVAIL Cohort by measures of neighborhood socio-economic environment
| Deprivation Index Categories | USDA Food Access Research Atlas categories | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | High SEE | High Mid SEE | Low Mid SEE | Low SEE | P | Low Income | p | Low Access | p | LILA | p | ||
| 171 | 51 (29.8%) | 44 (25.7%) | 40 (23.4%) | 36 (21.1%) | 86 (50.3%) | 153 (89.5%) | 71 (41.5%) | ||||||
| Other | 7 (4.1%) | 1 (2.0%) | 2 (4.6%) | 3 (7.5%) | 1 (2.8%) | 4 (4.7%) | 6 (3.9%) | 4 (5.6%) | |||||
| >$50,000/year | 94 (55.0%) | 44 (86.3%) | 32 (72.8%) | 13 (32.5%) | 5 (13.9%) | 24 (27.9%) | 86 (56.2%) | 19 (26.8%) | |||||
| Private | 86 (50.3%) | 41 (80.4%) | 29 (65.9%) | 13 (32.5%) | 3 (8.3%) | 20 (23.3%) | 81 (52.9%) | 17 (23.9%) | |||||
| >High School | 105 (61.4%) | 46 (90.2%) | 32 (72.7%) | 22 (55.0%) | 5 (13.9%) | 34 (37.5%) | 98 (64.1%) | 30 (42.3%) | |||||
| Married | 98 (57.3%) | 43 (84.3%) | 32 (72.7%) | 16 (40.0% | 7 (19.4%) | 30 (34.9%) | 93 (60.7%) | 27 (38.0%) | |||||
| Yes | 117 (70.1%) | 44 (88.0%) | 35 (81.4%) | 26 (65.0%) | 12 (35.3%) | 45 (54.2%) | 108 (72.5%) | 39 (57.4%) | |||||
| Yes | 71 (41.5%) | 18 (35.3%) | 17 (38.6%) | 13 (42.5%) | 19 (52.8%) | 43 (50.0%) | 61 (39.9%) | 34 (47.9%) | |||||
Demographic distribution by measures of neighborhood socio-economic environment (SEE) in the PREVAIL Cohort (n = 171). Residential addresses were geocoded and assigned validated measures of census tract-level SEE, including the Deprivation Index and USDA low income and low access variables. Categorical Deprivation Index was based on quartile of score (High, High Mid, Low Mid, and Low SEE) and a low income/low access (LILA) designation was defined as census tracts that met both USDA low income and low access criteria. Comparisons were made using Fisher’s Exact test, with a significant p-value indicating that the proportionate distribution of each factor differed by SEE category.
Cohabitation data was missing for n = 4 subjects.
Maternal obesity was calculated based on the height and weight reported in the obstetrics record from the first trimester of pregnancy and defined as kg/m2 ≥30.
The cohort was racially and economically diverse, with 40.9% of mothers self-reporting as Black, 45.0% reporting incomes at or below $50,000 per year, and public and private insurance status equally distributed. Only six subjects (2.4%) identified as Hispanic ethnicity; three identified their race as Black, two as other, and one as White. Over one-third of the mothers (38.6%) completed no post-secondary training or education. Over half (57.3%) were married, while 70.1% reported living with a partner. The overall rate of maternal obesity (41.5%) was modestly higher than the NHANES-reported obesity rates for female adult (20–39 years) in the US (39.7%) (33).
Significant differences were found by SEE in the proportion of all family-level demographic factors, with increasing material deprivation and low income and LILA designation corresponding with increasing proportion of Black race, public insurance, unmarried status, lower maternal education, and lower income level (Table 1, all p < 0.01). The proportion of mothers with obesity differed only by Low Income status (p = 0.030).
Correlations were moderate to high between all family-level factors and Deprivation Index score, category, Low Income, and LILA (see Table 2). Low Access designation, however, was only modestly associated with family socio-demographic factors, and negatively associated with the lower socio-demographic category. For example, residence in Low Access census tracts was negatively correlated to unmarried status, lower education level, Deprivation Index score and category, and income < $25,000/year (all p < 0.05).
Table 2.
Correlations between neighborhood socio-economic environment and family-level measures in the PREVAIL Cohort
| Black Race | Maternal Age | Lower Income Level | Public Insurance | Lower Maternal Educ | Married | Lives with Partner | Dep. Index Score | Dep. Index Category | LILA | Low Income | Low Access | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black Race | −0.30 | 0.66 | 0.77 | 0.63 | −0.58 | −0.63 | 0.56 | 0.53 | 0.43 | 0.52 | −0.10 | |
| Maternal Age | < 0.001 | −0.31 | −0.35 | −0.43 | 0.31 | 0.24 | −0.28 | −0.31 | −0.20 | −0.20 | −0.04 | |
| Lower Income Level | < 0.001 | < 0.001 | 0.81 | 0.71 | −0.72 | −0.63 | 0.60 | 0.57 | 0.43 | 0.53 | −0.12 | |
| Public Insurance | < 0.001 | < 0.001 | < 0.001 | 0.70 | −0.75 | −0.63 | 0.58 | 0.55 | 0.44 | 0.54 | −0.15 | |
| Lower Maternal Educ | < 0.001 | < 0.001 | < 0.001 | < 0.001 | −0.60 | −0.61 | 0.58 | 0.55 | 0.33 | 0.45 | −0.16 | |
| Married | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.65 | −0.54 | −0.50 | −0.33 | −0.46 | 0.20 | |
| Lives with Partner | < 0.001 | 0.002 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | −0.43 | −0.40 | −0.23 | −0.34 | 0.15 | |
| Deprivation Index Score | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.97 | 0.62 | 0.82 | −0.30 | |
| Deprivation Index Category | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.64 | 0.82 | −0.26 | |
| LILA | < 0.001 | 0.008 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.84 | 0.29 | |
| Low Income | < 0.001 | 0.007 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | −0.23 | |
| Low Access | 0.184 | 0.645 | 0.113 | 0.044 | 0.038 | 0.007 | 0.050 | < 0.001 | 0.001 | < 0.001 | 0.003 |
Spearman correlation coefficients (unshaded) and p values (shaded) for measures of neighborhood socio-economic environment (SEE) and family-level factors in the PREVAIL Cohort (n = 171). Residential addresses were geocoded and assigned validated measures of census tract-level SEE, including the Deprivation Index and USDA low income and low access variables. Categorical Deprivation Index was based on quartile of score and a low income/low access (LILA) designation was defined as census tracts that met both USDA low income and low access criteria.
Overall, 15.8% of the children in the cohort had obesity (27/171). Proportion of obesity differed by SEE only in comparing the binary Deprivation Index High SEE (3/51, 5.9%) to the remaining cohort (24/120, 20.0%; χ2 = 4.36, p = 0.037). In univariable log binomial models (see Table 3), only High Mid (RR 3.48 (95%CI: 1.12, 14.97)) and Low Mid (RR 3.40 (95%CI: 1.06, 14.79)) in the Deprivation Index categorical model and Not High SEE (RR 3.40 (95%CI: 1.26–13.86)) in the binary model were associated with significant increases in obesity risk. In terms of model fit, both categorical and binary Deprivation Index explained the highest percentage of variance (Table 3, R2 = 0.062), and the binary Not High SEE model had the second-lowest AIC (Table 3, 146.92). However, none of the models met adequate prediction criteria (all AUROC < 0.70), and none of the AUROC significantly differed per DeLong’s test.
Table 3.
Log binomial models for obesity risk at age two in the PREVAIL Cohort
| Variable | Level | RR | 95%CI | R2 | AIC | AUROC | |
|---|---|---|---|---|---|---|---|
| Univariable Models | Deprivation Index score | Log10(score) | 4.75 | 0.69 – 33.34 | 0.025 | 150.68 | 0.597 |
| High Mid1 | 3.48 | 1.12 – 14.97 | |||||
| Not High SEE | Yes1 | 3.40 | 1.26 – 13.86 | 0.062 | 146.92 | 0.611 | |
| Low income | Yes2 | 1.68 | 0.83 – 3.61 | 0.021 | 151.09 | 0.575 | |
| Low access a b | Yes3 | 0.68 | 0.30 – 2.11 | 0.006 | 152.59 | 0.526 | |
| LILA | Yes4 | 1.52 | 0.75 – 3.08 | 0.014 | 151.78 | 0.561 | |
| Other5 | 3.36 | 0.93 – 8.07 | |||||
| Maternal Educ | ≤High School6 | 1.09 | 0.52 – 2.19 | 0.001 | 153.11 | 0.513 | |
| Maternal Age | Years | 1.03 | 0.96 – 1.11 | 0.009 | 152.32 | 0.563 | |
| $25–50k/year7 | 1.41 | 0.53 – 3.74 | |||||
| Insurance | Public8 | 1.26 | 0.63 – 2.60 | 0.004 | 152.73 | 0.535 | |
| Marital status | Unmarried9 | 1.45 | 0.72 – 2.93 | 0.011 | 152.08 | 0.554 | |
| Lives with Partner | No10 | 0.91 | 0.37 – 1.95 | 0.001 | 144.96 | 0.511 | |
| Maternal obesity | Yes11 | 1.31 | 0.65 – 2.6 | 0.006 | 152.59 | 0.539 | |
| Mat. obesity11 | 1.24 | 0.59 – 2.60 | |||||
| Mat. obesity11 | 1.19 | 0.58 – 2.45 | |||||
| Mat. obesity11 | 1.18 | 0.58 – 2.41 | |||||
| Mat. obesity11 | 1.20 | 0.57 – 2.52 |
Log binomial models of risk of obesity at age two for children enrolled in the PREVAIL cohort (n = 171) by family-level socio-demographic and neighborhood socio-economic environment (SEE). Residential addresses were geocoded and assigned validated measures of census tract-level SEE, including the Deprivation Index and USDA low income and low access variables. Categorical Deprivation Index was based on quartile of score and a low income/low access (LILA) designation was defined as census tracts that met both USDA low income and low access criteria. An area under the receiver operator characteristic curve (AUROC) ≥0.70 was considered adequate predictive accuracy, with higher variance explained (R2) and lower Akaike information criterion (AIC) indicating better model fit. Superscript letters indicate significant differences in AUROC per DeLong’s test for correlated AUROC for the model comparisons.
Reference values are
High SEE,
not Low Income,
not Low Access,
not LILA,
white race,
> high school education level,
income > $50,000/year,
private insurance,
married,
cohabitating,
no maternal obesity.
Due to issues of model convergence, multivariable log binomial models were limited to the SEE variables of Deprivation Index score, Deprivation Index category, Not SEE, and LILA, and the family-level variables of race, maternal education level, and maternal obesity. Increased risk of child obesity was associated with residence in High Mid (RR 3.63 (95%CI 1.04–12.68)) in the categorical Deprivation Index model and residing outside of the High SEE census tracts (RR 3.52 (95%CI 1.06–11.71) in the binary Deprivation Index model. In terms of model fit, multivariable models using the Deprivation Index, including the log(10) of Deprivation index score, category, and Not High SEE, had higher R2 than any of the univariable models. In comparing all model AUROC (Figure 3, A & B), the Deprivation Index category and Not High SEE multivariable models had significantly greater AUROC than the univariable model for Low Access. No other model, whether univariable or multivariable, significantly differed in AUROC; no model explained over 10% of the variance, and none of the models met adequate prediction criteria (Figure 3, all AUROC < 0.70).
Figure 3.
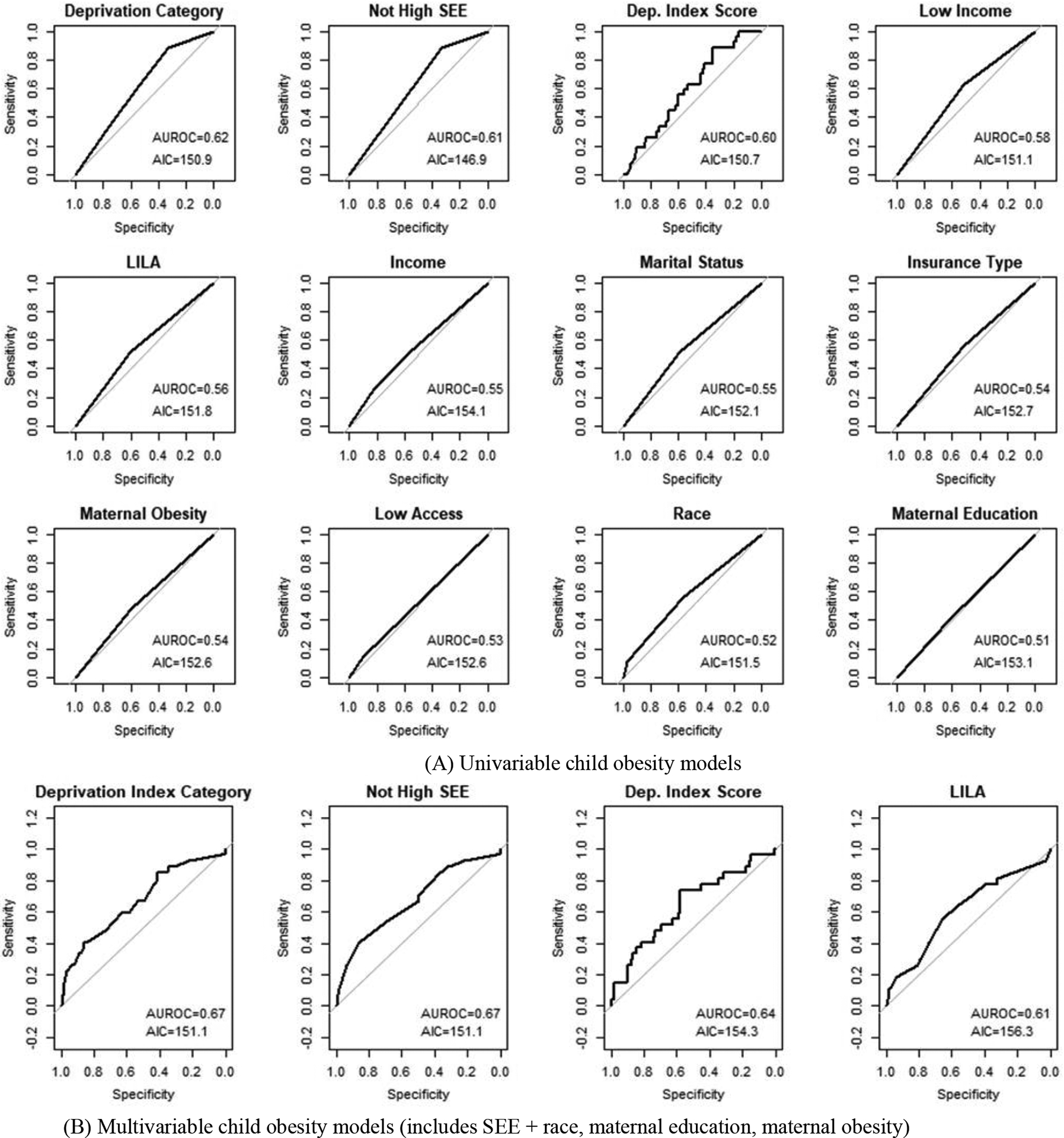
Area under the receiver operator characteristic curves for log binomial obesity models in the PREVAIL Cohort. Visualizations of areas under the receiver characteristic curves (AUROC) for log binomial models of obesity risk in two-year-old children enrolled in the PREVAIL Cohort. Residential addresses were geocoded and assigned two validated measures of census tract socio-economic environment (SEE), the Deprivation Index (21) and the USDA Food Access Research Atlas variables Low Income, Low Access, and Low Income/Low Access (LILA) (20). Deprivation Index categories were assigned based on quartile of Deprivation Index score. A binary comparison of the Least Deprived quartile compared to the remaining cohort was also included. Family-level factors were collected at the baseline study visit from the mother. Univariable models assessed risk of obesity at age two by each variable. Multivariable models included measures of SEE and the family-level variables of maternal race, education level, and presence of obesity. Model fit was compared for univariable (A) and multivariable (B) models using Akaike Information criteria (AIC) and area under the receiver operator characteristic curve (AUROC), with lower AIC and higher AUROC indicating better model fit, and an AUROC ≥0.70 considered adequate predictive accuracy.
Discussion
In the PREVAIL Cohort, 15.8% of children had obesity at age two. Significant differences in the proportion of obesity at age two were identified only when comparing the Deprivation Index High SEE census tracts to the remaining cohort; we found no differences in obesity rates among individual Deprivation Index categories, any of the USDA Food Access Research Atlas variables, or any of the family-level socio-demographic factors. In regression models, residing in either of the Deprivation Index intermediate SEE categories or in any neighborhood outside of the High SEE neighborhoods was associated with ≥ 3.4 times the risk of obesity, a relationship that did not significantly change when controlling for subject race, maternal education level, and presence of maternal obesity. When analyzing obesity risk in relation to the binary USDA Low Income, Low Access, or LILA designations, no differences were identified. When comparing model performance, all univariable and multivariable models were similar in model fit, and there were few differences in terms of predictive accuracy. Despite significant associations with obesity risk, none of the models met criteria for adequate model prediction and none explained more than 10% of the variance.
Previous studies using NHANES data have identified family-level socio-demographic indicators as risk factors for increased obesity in children as young as two years (3, 4). None of our family-level variables were significant in univariable or multivariable analysis of obesity risk, and no differences in obesity proportions were identified by any of these factors. However, we did find moderate to high correlations between all of these factors and our ecological measures of SEE and significant differences in the proportional distribution of family demographic factors by most SEE measures. Further examination of the distribution by Deprivation Index category found that these differences were mostly between the High SEE group and the remaining cohort. The High SEE group was 11.8% Black, 7.8% reported a family income below $25,000/year, and 91.2% had completed at least 2 years of post-secondary education or training. The remaining cohort, in contrast, was 53.3% Black, 34.2% were at the lowest income level, and 49.2% were in the higher education category (all p < 0.001). Importantly, these differences align with family-level factors previously associated with child obesity risk (3, 4, 37).
That obesity differences were found using the Deprivation Index to categorize neighborhood SEE and not by the more commonly used USDA food desert variables in our study is unsurprising, given the inconsistency of findings surrounding child obesity and food deserts (17, 18). The Deprivation Index’s inclusion of aggregated socio-demographic variables, such as education level and use of public assistance, provides more granularity compared to the binary USDA measures, and includes variables shown on an individual level to be associated with increased obesity. This was especially true with the frequently used Low Access variable, which had the lowest R2 and AUROC and the highest AIC of all of the ecological univariable models and was the only model to have a significantly lower AUROC compared to any other model. While not significantly different in terms of predictive value from the Deprivation Index models, the models including Low Income and LILA also failed to find significant risk of obesity in our population and had inferior model fit statistics compared to all permutations of the Deprivation Index. The lack of significance in the USDA measures as predictors of child obesity suggests that the associations between neighborhood SEE and child weight are more complex than simply neighborhood average income level or access to a grocery store.
That neighborhoods can be best categorized by multiple indicators of material deprivation is illustrative of the socio-demographic segregation found at either end of the affluence spectrum in the U.S. While lending policies of the early to mid-20th century resulted in the segregation of Black Americans into increasingly impoverished urban centers, higher-income, White residents moved from the urban core into newer, wealthier exurbs and suburbs (16). We detected this pattern in Deprivation Index and LILA maps of PREVAIL census tracts (see Figure 2). Clear clustering of increasing neighborhood deprivation is seen in the urban center, with lower deprivation radiating to the exurban and suburban areas.
In 1993, Massey and Denton found that race and neighborhood were so collinear as to make it “impossible to precisely estimate their separate effects” (16). More recent studies, however, have found that multiplicative levels of segregation, including inter- and intra-racial income segregation, can be used to examine health disparities including obesity (11, 15, 39). This segregation, along lines associated with obesity risk, explains why differences in these factors are significantly different by neighborhood SEE and why the more granular Deprivation Index outperforms the binary USDA variables.
Consistent with the above, we found a high level of racial and income segregation, with low-income Black mothers over five times as likely to live in the Low SEE neighborhoods than low-income White mothers. We also found that adding additional socio-demographic variables, outside of race and maternal education, to our neighborhood models of obesity risk resulted in a failure in our models to converge, suggesting an overfitting of the models, possibly due to insufficient sample size and high multicollinearity between our subjects’ family demographics and neighborhood of residence.
Limitations
Our analysis has some limitations. Domestic stressors, such as neighborhood crime, financial hardship and food security, as well as structural elements, such as green space and walkability, have been significantly associated with increased risk of obesity in older children (7, 8, 40, 41). We did not account for these factors, and the only structural variable that we included, Low Access, was shown to have limited validity in this context. However, given the strong association with individual family-level factors and neighborhood SEE, the possibility that these other measures of neighborhood environment contributed to our outcomes cannot be discounted. As we were primarily interested in comparing the predictive power of our measures, testing the multiplicative effects of segregation was outside of the scope of this project. Future work should include measures of segregation, and interaction by race or education level, which may better clarify causality and improve the models’ predictive value. While ethnicity has been shown to be a risk factor for childhood obesity (3), due to limited numbers of subjects who identified as Hispanic (n = 6, 2.4%), we were unable to include ethnicity in our analysis. However, our population was representative of Cincinnati and the birth hospitals from which we recruited (32). Future studies are needed with larger, more geographically and ethnically diverse, populations.
Finally, these data were drawn only from the last visit (month 24) of a birth cohort, while allocation of Deprivation Index categories was based on quartiles of score at each study point from birth to age two. We did find significant differences in those lost-to-follow up (n = 74) compared to those who completed the study at two years (n = 171). Those lost-to-follow up were more likely to be publicly insured, in the lowest income group, younger, unmarried, and in the lower education group (all p < 0.01). Of the ecological predictors, those lost to follow up lived in more deprived neighborhoods when comparing median Deprivation Index scores (p = 0.015).
This differential drop-out may, in part, explain our finding that High SEE census tracts had decreased risk of obesity compared to the remaining cohort rather than when comparing across categories. Sensitivity analysis did not find any significant differences when allocating categories based on the 24 month visit alone and there was no significant difference in terms of obesity prevalence in those lost to follow up compared to those included in this analysis. However, the differential change in sample size, rather than a lack of effect, may have limited detection of differences in the Low SEE group in the categorical model, as evidenced by the similarity in effect sizes for the three categories outside of High SEE, and no significant difference in risk was found among the High Mid, Low Mid, and Low SEE categories.
Thus, given the correlations between Deprivation Index category and socio-demographic factors and the lack of significant differences in predictive value from both family-level demographics and USDA food desert indicators, we conclude that level of neighborhood deprivation, measured by the Deprivation Index, functions as a summary of multiple measures of family socio-demographic and economic factors and may be useful to identify neighborhoods at higher risk for early childhood obesity - a critical first step to breaking the cycle of obesity and obesity-related health disparities attributable to neighborhood environment. However, due to the small sample size, geographic restriction, and low ethnic diversity of this study population, further research is needed to consider neighborhood material deprivation, as measured by the Deprivation Index, a generalizable risk factor for child obesity in the US.
Conclusion
While it has been inconsistently shown that factors associated with the built environment such as food desert status, walkability, and recreational space, are associated with increased rates of childhood obesity, our approach showed that areas of increased obesity risk can be identified by examining a more granular measure of SEE of the neighborhood, which is best summarized by the neighborhood’s level of deprivation. We found that the Deprivation Index efficiently identified areas of increased risk of obesity in very young children in our population and appeared to perform better or on par with more commonly used measures, such as USDA food desert status and family-level socio-demographic factors. Future studies including more geographic and ethnic diversity and larger sample size are needed to to validate this measure as a generalizable predictor of child obesity.
Acknowledgments
We gratefully acknowledge the participation of the PREVAIL birth cohort families. The authors also wish to thank our researchers at the University of Cincinnati, Cincinnati Children’s Hospital, and The Christ Hospital – Cincinnati and gratefully acknowledge the hard work of the dedicated PREVAIL staff. This work was funded by a cooperative agreement from the US Centers for Disease Control and Prevention (IP16-004), the Molecular Epidemiology in Children’s Environmental Health Training program (grant 5 T32 ES 10957-18), and the Center for Clinical and Translational Science and Training at the University of Cincinnati and Cincinnati Children’s Hospital Medical Center (grant 2UL2TROO1425-05A1). Guidance, mentorship, and editorial assistance was provided by the Break the Cycle of Children’s Environmental Health Disparities training program, based at Emory University in Atlanta, GA. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
References
- [1].Kelsey MM, Zaepfel A, Bjornstad P, Nadeau KJ. Age-related consequences of childhood obesity. Gerontology 2014;60(3):222–8. [DOI] [PubMed] [Google Scholar]
- [2].Llewellyn A, Simmonds M, Owen CG, Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev 2016;17(1):56–67. [DOI] [PubMed] [Google Scholar]
- [3].Ogden C, Fryar C, Martin C, Freedman D, Carroll M, Gu Q, et al. Trends in obesity prevalence by race and Hispanic origin—1999–2000 to 2017–2018. JAMA 2020;324(12):1208–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hales C, Carroll M, Fryar C, Ogden C. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief. Hyattsville, MD: National Center for Health Statistics, 2020:360. [PubMed] [Google Scholar]
- [5].Ogden C, Carroll M, Fakhouri T, Hales C, Fryar C, Li X, et al. Prevalence of obesity among youths by household income and education level of head of household — United States 2011–2014. MMWR 2018; 67:186–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Vargas CM, Stines EM, Granado HS. Health-equity issues related to childhood obesity: a scoping review. J Public Health Dent 2017;77(S1):S32–42. [DOI] [PubMed] [Google Scholar]
- [7].Duncan DT, Sharifi M, Melly SJ, Marshall R, Sequist TD, Rifas-Shiman SL, et al. Characteristics of walkable built environments and BMI z-scores in children: evidence from a large electronic health record database. Environ Health Perspect 2014;122(12):1359–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, Peters SM, McCaslin C, Joyce R, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med 2013;95:106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Johnson KA, Showell NN, Flessa S, Janssen M, Reid N, Cheskin LJ, et al. Do neighborhoods matter? A systematic review of modifiable risk factors for obesity among low socio-economic status Black and Hispanic children. Child Obes 2019;15(2):71–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Fiechtner L, Sharifi M, Sequist T, Block J, Duncan DT, Melly SJ, et al. Food environments and childhood weight status: effects of neighborhood median income. Child Obes 2015;11(3):260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Do DP, Frank R, Iceland J. Black-white metropolitan segregation and self-rated health: Investigating the role of neighborhood poverty. Soc Sci Med 2017;187:85–92. [DOI] [PubMed] [Google Scholar]
- [12].Davison KK, Birch LL. Childhood overweight: A contextual model and recommendations for future research. Obes Rev 2001;2(3):159–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Saelens BE, Sallis JF, Frank LD, Couch SC, Zhou C, Colburn T, et al. Obesogenic neighborhood environments, child and parent obesity: The Neighborhood Impact on Kids study. Am J Prev Med 2012;42(5):e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kang Sim DE, Strong DR, Manzano MA, Rhee KE, Boutelle KN. Evaluation of dyadic changes of parent-child weight loss patterns during a family-based behavioral treatment for obesity. Pediatr Obes 2020; 15(6):e12622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Quillian L. Segregation and poverty concentration: The role of three segregations. Am Sociol Rev 2012; 77(3):354–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Massey DS, Denton NA. American apartheid: segregation and the making of the underclass. Cambridge, MA: Harvard University Press,1993. [Google Scholar]
- [17].Cobb LK, Appel LJ, Franco M, Jones-Smith JC, Nur A, Anderson CAM. The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results. Obesity 2015;23(7): 1331–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mei K, Huang H, Xia F, Hong A, Chen X, Zhang C, et al. State-of-the-art of measures of the obesogenic environment for children. Obes Rev 2020. Jul 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].American Community Survey. URL: https://www.census.gov/programs-surveys/acs.
- [20].Food Access Research Atlas. URL: https://www.ers.usda.gov/data-products/food-access-research-atlas/.
- [21].Brokamp C, Beck AF, Goyal NK, Ryan P, Greenberg JM, Hall ES. Material community deprivation and hospital utilization during the first year of life: an urban population–based cohort study. Ann Epidemiol 2019; 30:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Woodruff RC, Haardörfer R, Raskind IG, Hermstad A, Kegler MC. Comparing food desert residents with non-food desert residents on grocery shopping behaviours, diet and BMI: results from a propensity score analysis. Public Health Nutr 2020;23(5):806–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Thomsen MR, Nayga RM, Alviola PA, Rouse HL. The effect of food deserts on the body mass index of elementary schoolchildren. Am J Agric Econ 2016;98 (1):1–18. [Google Scholar]
- [24].Briggs AC, Black AW, Lucas FL, Siewers AE, Fairfield KM. Association between the food and physical activity environment, obesity, and cardiovascular health across Maine counties. BMC Public Health 2019;19(1):374–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].MacNell L A geo-ethnographic analysis of low-income rural and urban women’s food shopping behaviors. Appetite 2018;128:311–20. [DOI] [PubMed] [Google Scholar]
- [26].Santorelli ML, Okeke JO. Evaluating community measures of healthy food access. J Commun Health 2017;42(5):991–7. [DOI] [PubMed] [Google Scholar]
- [27].Block JP, Subramanian SV. Moving beyond “food deserts”: Reorienting United States policies to reduce disparities in diet quality. PLoS Med 2015;12(12): e1001914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kimbro RT, Denney JT. Neighborhood context and racial/ethnic differences in young children’s obesity: structural barriers to interventions. Soc Sci Med 2013; 95:97. [DOI] [PubMed] [Google Scholar]
- [29].Phillips RL, Liaw W, Crampton P, Exeter DJ, Bazemore A, Vickery KD, et al. How other countries use deprivation indices-and why the United States desperately needs one. Health Aff (Millwood) 2016; 35(11):1991–8. [DOI] [PubMed] [Google Scholar]
- [30].Brokamp C, Jandarov R, Rao MB, LeMasters G, Ryan P. Exposure assessment models for elemental components of particulate matter in an urban environment: A comparison of regression and random forest approaches. Atmos Environ 2017;151:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Brokamp C, LeMasters GK, Ryan PH. Residential mobility impacts exposure assessment and community socioeconomic characteristics in longitudinal epidemiology studies. J Expo Sci Environ Epidemiol 2016;26(4):428–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Morrow AL, Staat MA, DeFranco EA, McNeal MM, Cline AR, Conrey SC, et al. Pediatric respiratory and enteric virus acquisition and immunogenesis in US mothers and children aged 0–2: PREVAIL Cohort Study. JMIR Res Protoc 2021;12;10(2):e22222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Overweight and obesity. URL: https://www.cdc.gov/obesity/data/adult.html.
- [34].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Brokamp C DeGAUSS: Decentralized Geomarker Assessment for Multi-Site Studies. J Open Source Software 2018;3(30):812. [Google Scholar]
- [36].Growth charts-Z score data files. URL: https://www.cdc.gov/growthcharts/zscore.htm.
- [37].Data, trend and maps. URL: https://www.cdc.gov/nccdphp/dnpao/data-trends-maps/index.html.
- [38].R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2018. URL: https://www.R-project.org/. [Google Scholar]
- [39].Anderson KF. Racial residential segregation and the distribution of health-related organizations in urban neighborhoods. Social Problems 2017;64(2):256–76. [Google Scholar]
- [40].Metallinos-Katsaras Elizabeth,PhD RD, Must A PhD, Gorman K PhD. A longitudinal study of food insecurity on obesity in preschool children. J Acad Nutr Diet 2012;112(12):1949–58. [DOI] [PubMed] [Google Scholar]
- [41].Kim Y, Cubbin C, Oh S. A systematic review of neighbourhood economic context on child obesity and obesity-related behaviours. Obes Rev 2019;20(3):420–31. [DOI] [PMC free article] [PubMed] [Google Scholar]


