Abstract
Objective
Obsessive and compulsive symptoms (OCS) are cross-cutting psychopathological manifestations frequently detected in a variety of clinical and non-clinical samples. It has been suggested that impaired mentalization abilities and traumatic experiences during childhood may be relevant etiopathogenetic factors in the development of OCS. The purpose of the current study was to cross-sectionally assess these variables in a non-clinical sample, testing the mediational role of mentalization abilities in the association between childhood trauma (CT) and OCS.
Method
667 participants (488 females; mean age= 29.76 ± 11.87 years; age range: 18-80) answered a survey including the Childhood Trauma Questionnaire, the Mentalization Questionnaire and the Obsession-Compulsion subscale of the Brief Symptom Inventory.
Results
The mediation model was significant for the total effect (p< .001), showing that CT was positively associated with OCS (95% CI: .006; .019) and that this association was mediated by reduced levels of mentalization capacity (95% CI: .003; .009). Such results were significant controlling for potential sociodemographic and clinical confounding variables.
Conclusions
The findings contribute to elucidate the complex relationships between CT, mentalization capacity, and OCS, supporting the possibility that mentalization impairments, arising from CT, may affect top-down control mechanisms thus contributing to the development of OCS.
Keywords: obsessive-compulsive symptoms, childhood trauma, mentalization, anxiety, depression, psychopathology
1. Introduction
Obsessive-compulsive symptoms (OCS) are core features of the obsessive-compulsive disorder (OCD; American Psychiatric Association [APA], 2022) but are also frequently detected in neuropsychiatric conditions (e.g. tic disorders and PANDAS syndrome; Isaacs et al., 2020; Moretti et al., 2008; Rothenberger et al., 2019), in mental diseases different from OCD [including psychotic, eating, anxiety and mood disorders (American Psychiatric Association [APA], 2022; Baer et al., 2015; Citkowska-Kisielewska et al., 2020; Froreich et al., 2016; Tezenas du Montcel et al., 2019)], and in non-clinical samples [where the estimated prevalence ranges between 3-43% (Fineberg et al., 2013; Fullana et al., 2010; Okasha et al., 2001; Skapinakis et al., 2019; Sun et al., 2014)].
Obsessions are considered recurrent and persistent intrusive thoughts, images, impulses or urges, while compulsions are defined as repetitive behaviors or mental acts that the individual feels compelled to perform (Stein et al., 2019). Individuals can experience disturbances related to both obsessions and compulsions; such phenomena can be causally bidirectionally related to each other (De Putter et al., 2017; Maraone et al., 2024).
The underlying psychopathological mechanisms of OCS are still not clear. However, it has been suggested that, as for several psychiatric disorders, impaired mentalization abilities may be a relevant etiopathogenetic factor (e.g. Sloover et al., 2022). The concept of mentalization refers to the process of representing and understanding one’s own and others’ behavior in terms of underlying psychological states [e.g., thoughts, emotions, needs, desires (Fonagy et al., 2002; Luyten et al., 2020)]. The concept of mentalization is considered to partially overlap with certain related constructs, such as theory of mind and metacognition; however, while these latter concepts share with mentalization a focus on the ability to recognize and differentiate (and reflect about) mental states, they tend to marginalize the emotional and relational facets of this process (Allen, 2006; Liljenfors et al., 2015). Mentalization, in fact, is constituted by both cognitive and affective components, encompassing emotional awareness, affect regulation, and empathy (Fonagy et al., 2002).
Mentalization skills are thought to develop since the first year of life (Fonagy et al., 2002; Harris et al., 2018; Kovács et al., 2010; Moll et al., 2008; Scott et al., 2017; Song et al., 2008), and they are suggested to be fostered by parental mirroring and synchrony with the child (Fonagy et al., 2002). Indeed, a large corpus of research links secure infant attachment to effective mentalizing in youth (Becker Razuri et al., 2017; Claussen et al., 2002; Kobak et al., 2017; Kokkinos et al., 2016; Levy et al., 2019; Mcquaid et al., 2008; Meins et al., 2008; Panfile et al., 2012; Troyer et al., 2018; Zaccagnino et al., 2015). Conversely, mentalization development is seen to be negatively influenced by early relational adversities (Dykas et al., 2011), and more specifically by childhood trauma (CT; Barlow et al., 2014; Catalana et al., 2020; Cicchetti et al., 2003; Ensink et al., 2015; Gruhn et al., 2020; Pears et al., 2005; Zhang et al., 2023).
CT is generally defined as the experience of overwhelming inescapable threats which encompass different forms of maltreatment (e.g., emotional abuse, physical abuse, sexual abuse, neglect) occurring during infancy and/or adolescence (Farina et al., 2013; Massullo et al., 2023). CT can profoundly impact psychological and emotional functioning (Massullo et al., 2023; Toof et al., 2020). In particular, studies on emotion recognition, affect regulation, and empathy, showed that these abilities are reduced with increasing severity of abuse and neglect (e.g. Gruhn et al., 2020; Zhang et al., 2023), while inconsistent results seem to emerge from research on theory of mind paradigms (Benarous et al., 2015). Also, it is well known that CT is strongly associated with adult psychopathology (Copeland et al., 2018; Massullo et al., 2023; McKay et al., 2021). More specifically, recent systematic reviews showed that exposure to CT is significantly related to OCS severity in clinical and non-clinical samples (Boger et al., 2020a; Destree et al., 2021; Mathews et al., 2008).
Previous research detected certain cognitive and psychopathological factors that may contribute to mediate this relationship, including experiential avoidance, mindfulness abilities (Kroska et al., 2018), maladaptive coping (Kadivari et al., 2023), rumination, emotion regulation difficulties, posttraumatic stress symptoms (Boger et al., 2020b), and dissociation (Boger et al., 2020b; Santoro et al., 2023).
Despite the fact that some of these mediators (e.g. emotion regulation, mindfulness) fall under the wide umbrella construct of mentalization-related phenomena (Luyten et al., 2015), to the best of our knowledge no study has investigated the relationship among CT, mentalization abilities and OCS. Understanding the relationship between these variables may have important clinical implications. As already mentioned, in fact, according to attachment-oriented developmental theories (Fonagy et al., 2002) impaired mentalizing may arise from repeated maltreatment in the context of caregiving relationships and may represent a major risk factor for psychopathology in adulthood, including OCS.
In order to test this hypothesis, we cross‐sectionally explored in a non-clinical sample the relationship between CT and OCS while considering mentalization abilities as a mediator.
2. Methods
2.1 Participants
In accordance with published guidelines (Fritz et al., 2007), the analyses for a mediational model performed with the bootstrapping procedure required a minimum sample size of 558 to provide a statistical power of 0.80, assuming small effect sizes for both paths “a” and “b”.
This study included 667 individuals (488 females; mean age ± standard deviation = 29.76 ± 11.87 years; age range: 18-80) that answered an online survey shared by social media, mailing lists, and instant messaging applications between February 2021 and April 2022. Participants responded by opening the questionnaire web link from their preferred device (smartphone, tablet or computer). They did not receive any payment or compensation, they responded the survey spontaneously and anonymously. Inclusion criteria for the enrollment in the present study were: (i) age over 18, (ii) good written Italian comprehension, (iii) the provision of written consent to join the study, (iv) correct response to two attentional check items. The study is part of a larger research project on psychopathology in the general population, so the sample partially overlaps with the sample of another manuscript published by our research group (Bersani et al., 2024). The Institutional Board of the Department of Human Neurosciences of Sapienza University of Rome, in accordance with the principles of the Helsinki Declaration, endorsed the study procedure.
2.2 Instruments
For the present study, participants answered the following questionnaires: the Childhood Trauma Questionnaire - Short Form (CTQ-SF; Bernstein et al., 2003), the Mentalization Questionnaire (MZQ; Hausberg et al., 2012); and the Obsession-Compulsion subscale of the Brief Symptom Inventory (OC-BSI; Derogatis et al., 1983). Subjects were asked to fill in a form with socio-demographic and clinical data, including: age, sex, educational level, occupation, alcohol, tobacco, and other substances use (i.e. cannabis, heroin, and/or cocaine use) in the last 12 months, current use of psychiatric medications. Clinically relevant self-report anxiety or depression symptomatology was also assessed using the Depression (DEP-BSI) and Anxiety (AXN-BSI) subscales of the BSI (Derogatis et al., 1983). Lastly, alcohol use was assessed using the first item of the Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 2001): “How often do you have a drink containing alcohol?”. Participants that answered “never” were coded as “non-alcohol users”. Conversely, participants that answered “monthly or less”, “2 to 4 times a month”, “2 to 3 times a week” or “4 or more times a week” were coded as “alcohol users”.
The CTQ-SF (Bernstein et al., 2003) is a 28 item self-report commonly used in both clinical and non-clinical samples to assess exposure to five different types of CT (Georgieva et al., 2021; Massullo et al., 2023): emotional abuse (EA), physical abuse (PA), sexual abuse (SA), emotional neglect (EN), and physical neglect (PN). We used the Italian adaptation of the scale (Sacchi et al., 2018). The questionnaire consists of 5 subscales, one for each CT dimension, of 5 items rated on a 5-point Likert scale (ranging from 1=“never” to 5=“very often”). It also includes an additional 3-item scale about Minimization/ Denial (MD), indicative of potential underreporting of maltreatment on a scale of “low”, “intermediate” and “high”. The questionnaire has demonstrated good psychometric properties (Bernstein et al., 2003; Sacchi et al., 2018). Although certain studies did not support the unidimensional factor structure of the CTQ-SF, several psychometric investigations have highlighted the research and clinical utility of the CTQ-SF total score. For example, Kongerslev et al. (2019) observed high inter-correlations amongst the five subscales as well as an excellent internal consistency of the CTQ-SF total score, suggesting that it is feasible to extract a factor representing non-specific or global CT. In our sample the Cronbach’s alpha for the total score was .88 and the correlations among the five subscales ranged from .14 to .53 (p < .001).
The MZQ (Hausberg et al., 2012) is a self-report scale measuring the ability of people to understand and conceptualize their own and others’ psychological states. It assesses different dimensions of mentalization: refusing self-reflection, emotional awareness, psychic equivalence mode, and regulation of affect. It consists of 15 items rated on a 5-point Likert scale (from 1=“I totally disagree” to 5=“I totally agree”), providing a total score where higher values indicate higher mentalizing abilities. We used the Italian adaptation of the scale (Raimondi et al., 2021) and the Cronbach’s α in the present sample was .85 for the total score.
The OC subscale of the BSI (Derogatis et al., 1983) is composed of 6 items and it is considered to be a reliable measure of OCS (Maraz et al., 2015; Miller, 2006; Rice et al., 2006; Woody et al., 1995). According to the authors of the scale: “the focus of this dimension is on thoughts and actions that are experienced as unremitting and irresistible by the patient but are of an ego-alien or unwanted nature” (Derogatis et al., 1983). We used a validated Italian version of the scale (De Leo et al., 1993). Subjects with clinically-relevant levels of OCS were detected using a cut-off score of 63T, as suggested by the test authors (Derogatis et al., 1983) and in accordance with previous studies (Grassi et al., 2018; Grassi et al., 2001; Grassi et al., 2000). Since anxiety and depression appear as potential confounding variables in OCS literature (e.g. See et al., 2022), we used the clinical cut-off (i.e., ≥ 63T) of the depression and anxiety subscales of the BSI to measure the presence of significant corresponding symptomatology. To be classified as reporting clinical levels of anxiety and/ or depression, subjects had to make scores above cutoff on at least one of the subscales. In our sample, the Cronbach’s alpha for the OC, DEP and AXN subscales were .84, .88, and .86, respectively.
2.3 Statistical Analysis
Statistical analyses were performed with the Statistical Package for the Social Sciences 25 (IBM, Armonk, NY, USA). In accordance with the recommendations of Kim et al. (2013) for large samples (i.e., > 300), absolute skew or kurtosis values smaller than 2 and smaller than 7, respectively, were used to determine the normality of the distribution of each variable. Since variables were normally distributed, parametric statistics were used. In particular, descriptive statistics were performed for the entire sample. Furthermore, group differences between males and females were examined using chi-square (χ2) tests for categorical variables and independent t-tests for continuous variables. The association among variables were investigated using Pearson's r correlation coefficients. Lastly, the mediating role of mentalization in the relationship between CT exposure and OCS was tested using the PROCESS v4.1 macro for SPSS (Hayes, 2022). In particular, we set the CTQ total score as the independent variable, the MZQ total score as the mediator and the OC-BSI score as the dependent variable in the Hayes serial model no.4 with 5000 bootstrap samples and a 95% CI. The analyses were performed controlling for potential confounding factors, including sociodemographic variables (i.e. age, sex, educational level and occupation) and clinical variables (i.e. alcohol use, tobacco use, other substances use, clinically-relevant levels of anxiety and/or depression, use of any psychiatric medication, and degree of CT minimization or denial) that are known to be associated with CT, mentalization and/or OCS (e.g. Blom et al., 2011; Imperatori et al., 2020; Laisney et al., 2013; Mathis et al., 2011; Pardini et al., 2009; Piacentino et al., 2020; Valérie et al., 2023). Confounding variables were entered in the model as covariates. We reported the mediation analysis in three separate main pathways (Baron et al., 1986). The pathway “a” is the direct effect of CTQ on MZQ; the pathway “c’” is the direct effect of CTQ on OC-BSI; the pathway “c” is the total effect, as the sum of direct and indirect effects of CTQ on OC-BSI. The direct effect of MZQ on OC-BSI (pathway “b”) and the indirect effect of CTQ on OC-BSI through MZQ (pathway “ab”) are also reported.
3. Results
In our sample 91 subjects met the criteria for possible clinically relevant OCS (13.64%), 121 for possible clinically-relevant anxiety and/or depression (18.14%), 237 subjects stated to use tobacco (35.53%), 177 subjects stated to use substances (cannabis, heroin, and/or cocaine) (26.54%), and 74 subjects stated to use psychiatric medications (11.09%). Compared to females, males participants had less frequently a bachelor’s degree (46.93% vs 55.74%; p= .043), reported more frequent substances use (34.08% vs 23.77%; p= .008), but had less frequently clinically relevant anxiety and/or depression symptoms (11.73% vs 20.49%; p=.009) and OCS (8.94% vs 15.37%; p= .032), as well as lower levels of OCS (.99 ± .82 vs 1.17 ± .96; p=.015). Detailed descriptive statistics are reported in table 1. Correlational analyses revealed that CTQ total score was negatively related to MZQ scores (r = -.306, p< .001), while it was positively related to OC-BSI scores (r = .298 p< .001). In turn, MZQ was negatively related to OC-BSI (r = -.526, p< .001). The full correlation matrix is reported in supplementary table 1.
Table 1.
Socio-demographic and clinical data of the sample
| Variables | Total N=667 | Males N=179 (26.84%) | Females N=488 (73.16%) | Test | p |
|---|---|---|---|---|---|
| Age -M ± SD | 29.76 ± 11.87 | 30.05 ± 12.09 | 29.65 ± 11.79 | t(665)=.388 | .698 |
| Bachelor’s degree -N (%) | 356 (53.37) | 84 (46.93) | 272 (55.74) | χ2=4.085 | .043 |
| University students -N (%) | 344 (51.57) | 94 (52.51) | 250 (51.23) | χ2=.087 | .769 |
| Employed -N (%) | 294 (44.08) | 75 (41.90) | 219 (44.88) | χ2=.471 | .492 |
| Alcohol use -N (%) | 563 (84.41) | 159 (88.83) | 404 (82.79) | χ2=3.630 | .057 |
| Tobacco use -N (%) | 237 (35.53) | 60 (33.52) | 177 (36.27) | χ2=.433 | .511 |
| cocaine) Substances -N use (%) (cannabis, heroin, | 177 (26.54) | 61 (34.08) | 116 (23.77) | χ2=7.138 | .008 |
| use Current -N (%) psychiatric medication | 74 (11.09) | 20 (11.17) | 54 (11.07) | χ2=.002 | .969 |
| CTQ -M ± SD | 34.90 ± 9.88 | 34.63 ± 9.22 | 35.00 ± 10.12 | t(665)=-.433 | .665 |
| CTQ-MD - M ± SD | .63 ± 1.00 | .60 ± .97 | .64 ± 1.01 | t(665)=-.452 | .651 |
| MZQ -M ± SD | 49.95 ± 11.65 | 49.53 ± 11.18 | 50.11 ± 11.82 | t(665)=-.571 | .568 |
| OC-BSI -M ± SD | 1.12 ± .93 | .99 ± .82 | 1.17 ± .96 | t(370.052)=-2.432 | .015 |
| OC-BSI ≥ 63T -N (%) | 91 (13.64) | 16 (8.94) | 75 (15.37) | χ2=4.596 | .032 |
| (%) DEP-BSI and/or ANX-BSI ≥63T - N | 121 (18.14) | 21 (11.73) | 100 (20.49) | χ2=6.767 | .009 |
Abbreviations: ANX: Anxiety subscale; BSI: Brief Symptom Inventory; CTQ: Childhood Trauma Questionnaire; MD: Minimization/Denial subscale; DEP: Depression subscale; MZQ: Mentalization questionnaire; OC: Obsessive-compulsive subscale.
Note: Bold values indicate statistically significant p values.
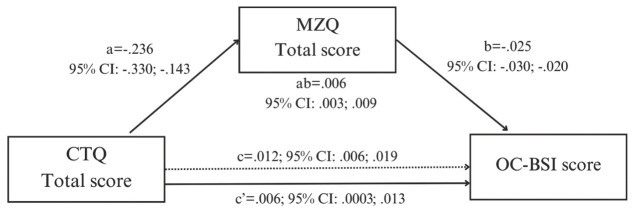
The mediation model was significant for the total effect (R2=.421; F12;654= 39.693; p< .001), indicating that higher scores on CTQ were associated with higher OC-BSI scores (B=.012; SE=.003; 95% CI: .006; .019). The effect of CTQ on MZQ was significant and negative (B=-.236; SE=.048; 95% CI: -.330; -.143); similarly, the effect of MZQ on OC-BSI was significant and negative (B=-.025; SE=.003; 95% CI: -.030; -.020). The indirect effect of CTQ on OC-BSI through MZQ was significant (B=.006; SE=.001; 95% CI: .003; .009), as well as the direct effect (B=.006; SE=.003; 95% CI: .0003; .013). These results are fully reported in supplementary table 2 and showed in figure 1.
Figure 1.
Graphical representation of the results of the mediation model. These results were obtained controlling for potentially-confounding variables (age, sex, educational level, occupation, alcohol use, tobacco use, substance use, self-report clinical anxiety and/or depressive symptomatology, use of psychiatric medications, potential minimization/denial of childhood trauma). Abbreviations: CTQ= Childhood Trauma Questionnaire; MZQ=Mentalization Questionnaire; OC-BSI=Obsessive Compulsive subscale of the Brief Symptom Inventory
4. Discussion
The main aim of the current study was to assess the association among CT, mentalization abilities and OCS in a non-clinical sample, which were significantly correlated to each other in the expected directions (supplementary table 1).
The results support a pathway (figure 1) in which CT affect mentalization abilities which, in turn, affects OCS severity, highlighting a mediating role of mentalization deficits in the association between CT and OCS even controlling for relevant confounding variables, such as clinical levels of anxiety and/or depression, which are known to be strong confounding variables in OCS research (e.g. See et al., 2022).
Although the association between CT and OCS is well known (Boger et al., 2020a; Destree et al., 2021; Mathews et al., 2008), to the best of our knowledge no study had investigated the mediating role of mentalization in such relationship.
Our results are in line with previous research suggesting that mentalization impairment may partially explain the pervasive detrimental effects of CT on mental health, as part of a trans-diagnostic etiopathogenic mechanism for emotional and behavioral disorders (Adler et al., 2021; Belvederi Murri et al., 2017; Borghesi et al., 2022; Hopfinger et al., 2016; Huang et al., 2020; Li et al., 2020; MacIntosh, 2013; Taubner et al., 2013).
More specifically, the negative association between CT severity and mentalization abilities is widely reported in clinical samples (e.g. in patients with personality or other psychiatric disorders; Adler et al., 2021; Belvederi Murri et al., 2017; Brüne et al., 2016; Duval et al., 2018), with less evidence in the general population (Schwarzer et al., 2021). It has been suggested (Fonagy et al., 2002) that positive caregiving behavior promotes children mentalization abilities through the mirroring function of recognizing, elaborating, and adequately returning children internal states. Conversely, CT by definition is an overwhelming experience implying the failure of this caregiving function (Bateman et al., 2019; World Health Organization, 2022). Thus, when facing recurrent maltreatment, children mentalization development can be hampered with growing under-representation of internal states. Consequently, individuals may begin to rely on non-mentalizing modes of self-experience, such as the psychic equivalence mode (i.e., a state of concrete thinking where there is no difference between internal and external world; Bateman et al., 2019), and/ or maladaptive cognitive emotion regulation strategies (e.g. self-blame, rumination, and catastrophizing; Doba et al., 2022).
It has been suggested that such under-representation of internal states affects top-down goal-directed control systems through the attitude to automatic behaviors (Luyten et al., 2015). Coherently, abnormal activity of brain structures and circuits involved in habit learning, inhibition of automatisms and goal-driven behavior has been observed in OCD (Maraone et al., 2024). In particular, it has been suggested that a disruption in the balance between habits learning and goal-direct systems could represent an adequate model of compulsive behaviors and that these may have a primary role in this clinical picture (Gillan et al., 2011). Accordingly, psychopathological core features of OCS, such as repetitive behaviors, pathological doubting and distrust in one own sensory and memory (Cervin et al., 2020; Dar et al., 2022; Fradkin et al., 2020; Nikodijevic et al., 2015; Samuels et al., 2017), may arise from difficulties in inhibiting habitual behaviors and enhanced errors-related signals (Maraone et al., 2024).
Of notice, consistent with previous studies, our regression models (i.e., supplementary table 2 path a and path c’) also indicated that some clinical factors (i.e., clinical levels of anxiety and/or depression) and sociodemographic factors (i.e., sex, age, occupation and educational level) were associated with our main study variables.
For example, the presence of clinically relevant anxiety and/or depression was positively associated with OCS (e.g., See et al., 2022). Consistent with previous studies (Stavropoulos et al., 2017; Vivan Ade et al., 2014) we also detected that OCS were higher in females participants, indicating a possible role of sex or gender hormones in their phenomenology (Labad et al., 2008; Vivan Ade et al., 2014).
Regarding mentalization, in the present report we found a positive association between age and MZQ total score. Although previous literature reported mixed results on the issue, which may depend on sample size and characteristics (e.g., age range) or on the instruments used (e.g., Pardini et al., 2009), this observation is in agreement with findings from reports in which the MZQ was used for the assessment of mentalization abilities (e.g., Bersani et al., 2022; Imperatori et al., 2020), raising the possibility that at least some mentalization skills (e.g., self-reflection) may continue to develop even in adulthood.
Consistent with previous studies (e.g., Bly et al., 2012; Laisney et al., 2013; Siswati et al., 2017), we also detected that being employed, having a bachelor’s degree, and being a student, were positively associated with mentalization scores. Since the ability to mentalize emerges during childhood and gradually improves from early adolescence through late adolescence and young adulthood (Desatnik et al., 2023), these findings suggest that adequate mentalization skills may be considered as psychological features associated with higher global psychosocial functioning (Bly et al., 2012). Accordingly, and in line with previous reports (Valérie et al., 2023), in the present study lower levels of mentalization were associated with the presence of clinically relevant anxiety and/or depression.
Our study has some potential clinical implications. For example, the current data seem to suggest that, together with the recommended psychological and pharmacological treatments for OCD (such as cognitive-behavioural therapy and certain selective serotonin reuptake inhibitors; Nezgovorova et al., 2022), individuals with OCS may benefit from mentalization-focused interventions. Consistently, interventions focusing on mentalization have shown positive results in patients with impaired top-down control associated with CT, such as individuals with borderline personality disorder and eating disorders, and can be integrated with other forms of psychotherapeutic interventions (Malda-Castillo et al., 2019; Robinson et al., 2016; Volkert et al., 2019). Furthermore, mentalization-based treatments seem to be also effective in children exposed to trauma, resulting in a promising preventive therapy for high-risk psychopathology children (Oehlman Forbes et al., 2021).
Our results also remark the need to carefully assess the presence of CT in individuals with OCS. Indeed, it is known that CT may lead to enduring interpersonal difficulties that hamper the therapeutic alliance and is associated with negative treatment outcomes, requiring tailored strategies besides conventional therapies (Farina et al., 2019).
5. Conclusion
The present research has several limitations that should be considered. Although we used validated and reliable questionnaires, self-report measures intrinsically expose to attentional, recall and social desirability bias (Althubaiti, 2016). Future studies may consider the use of structured interviews and/or cognitive tests. Secondly, the cross-sectional design of our mediation study implies that causality cannot be considered unequivocal, thus, results should be replicated by experimental or longitudinal research. Furthermore, participants were non-clinical subjects (i.e. recruited from the general population), thus further research is needed to investigate the association among CT, mentalization and OCS in patients with OCD diagnosis. Thirdly, data were collected using an on-line survey with certain groups of individuals that are more represented in the current sample (e.g. students compared to non-students, and females compared to males), affecting the generalizability of the results. Lastly, the observed rates of psychopathology may have been influenced by the fact that recruitment occurred in the period of COVID-19 pandemic, which has been a risk factor for increased mental health disturbances. Therefore, future research may ensure generalizability including a clinical sample.
Despite these limitations, our findings overall contribute to elucidate the complex relationships between CT, mentalization capacity, and OCS. More specifically, the results support the possibility that mentalization impairment arising from CT may affect top-down control mechanisms, possibly contributing to the development of OCS (e.g., to the development of distrust towards inner processes, obsessive doubts and compulsive-like behaviors).
References
- Adler, A., Gervinskaitė-Paulaitienė, L., Čekuolienė, D., & Barkauskienė, R. (2021). Childhood maltreatment and adolescents’ externalizing problems: Mentalization and aggression justification as mediators. Journal of Aggression, Maltreatment & Trauma, 30(1), 54-69. doi: 10.1080/10926771.2020.1783733 [DOI] [Google Scholar]
- Allen, J. G. (2006). Mentalizing in practice. In Allen J. G. & Fonagy P. (Eds.), Handbook of mentalization-based treatment (pp. 3-30). Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- Althubaiti, A. (2016). Information bias in health research: definition, pitfalls, and adjustment methods. Journal of Multidisciplinary Healthcare, 4(9), 211-217. doi: 10.2147/JMDH.S104807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association [APA]. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.) (5th ed., text rev. ed.). Washington, DC: American Psychiatric Association Publishing. [Google Scholar]
- Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B., & Monteiro, M. G. (2001). AUDIT: The Alcohol Use Disorders Identification Test (AUDIT): guidelines for use in primary care. Geneva: World Health Organizaton Department of Mental Health and Substance Abuse. [Google Scholar]
- Baer, L., Trivedi, M. H., Huz, I., Rush, A. J., Wisniewski, S. R., & Fava, M. (2015). Prevalence and impact of obsessive-compulsive symptoms in depression: a STAR* D report. The Journal of Clinical Psychiatry, 76(12), 15432. doi: 10.4088/JCP.14m09670 [DOI] [PubMed] [Google Scholar]
- Barlow, M. R., & Goldsmith, R. E. (2014). Childhood trauma and active mental processes: Dissociation and metacognition influence control of negative thoughts. Journal of Child & Adolescent Trauma, 7, 131-140. doi: 10.1007/s40653-014-0010-3 [DOI] [Google Scholar]
- Baron, R. M., & Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173-1182. doi: 10.1037//0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Bateman, A. W., & Fonagy, P. (2019). Handbook of Mentalizing in Mental Health Practice (Second Edition ed.). American Psychiatric Publishing: American Psychiatric Pub. [DOI] [PubMed] [Google Scholar]
- Becker Razuri, E., Hiles Howard, A. R., Purvis, K. B., & Cross, D. R. (2017). Mental state language development: The longitudinal roles of attachment and maternal language. Infant Mental Health Journal, 38(3), 329-342. doi: 10.1002/imhj.21638 [DOI] [PubMed] [Google Scholar]
- Belvederi Murri, M., Ferrigno, G., Penati, S., Muzio, C., Piccinini, G., Innamorati, M., Ricci, F., Pompili, M., & Amore, M. (2017). Mentalization and depressive symptoms in a clinical sample of adolescents and young adults. Child and Adolescent Mental Health, 22(2), 69-76. doi: 10.1111/camh.12195 [DOI] [PubMed] [Google Scholar]
- Benarous, X., Guile, J.-M., Consoli, A., & Cohen, D. (2015). A systematic review of the evidence for impaired cognitive theory of mind in maltreated children. Frontiers in Psychiatry, 6, 108. doi: 10.3389/fpsyt.2015.00108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein, D., Stein, J. A., Newcomb, M., Walker, E., Pogge, D., Ahluvalia, T., Stokes, J., Handelsman, L., Medrano, M., & Desmond, D. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169-190. [DOI] [PubMed] [Google Scholar]
- Bersani, F. S., Accinni, T., Carbone, G. A., Corazza, O., Panno, A., Prevete, E., Bernabei, L., Massullo, C., Burkauskas, J., Tarsitani, L., Pasquini, M., Biondi, M., Farina, B., & Imperatori, C. (2022). Problematic Use of the Internet Mediates the Association between Reduced Mentalization and Suicidal Ideation: A Cross-Sectional Study in Young Adults. Healthcare (Basel), 10(5). doi: 10.3390/healthcare10050948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bersani, F. S., Canevelli, M., Imperatori, C., Barchielli, B., Prevete, E., Sciancalepore, F., Vicinanza, R., Maraone, A., Salzillo, M., Tarsitani, L., Ferracuti, S., Pasquini, M., & Bruno, G. (2024). The Relationship of Frailty with Psychopathology, Childhood Traumas and Insecure Attachment in Young Adults: A Cross-Sectional Investigation. The Journal of Frailty & Aging, 1-8. doi: 10.14283/jfa.2024.4938305437 [DOI]
- Blom, R. M., Koeter, M., van den Brink, W., de Graaf, R., ten Have, M., & Denys, D. (2011). Co-occurrence of obsessive-compulsive disorder and substance use disorder in the general population. Addiction, 106(12), 2178-2185. doi: 10.1111/j.1360-0443.2011.03559.x [DOI] [PubMed] [Google Scholar]
- Bly, E. M., Wright, A. J., & Tuber, S. B. (2012). Unemployed and poor in New York: the impact of mentalization and Axis II psychopathology on job outcome. Bulletin of the Menninger Clinic, 76(2), 101-129. doi: 10.1521/bumc.2012.76.2.101 [DOI] [PubMed] [Google Scholar]
- Boger, S., Ehring, T., Berberich, G., & Werner, G. G. (2020a). Impact of childhood maltreatment on obsessive-compulsive disorder symptom severity and treatment outcome. European Journal of Psychotraumatology, 11(1), 1753942. doi: 10.1080/20008198.2020.1753942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boger, S., Ehring, T., Schwarzkopf, W., & Werner, G. G. (2020b). Potential mediators of the association between childhood maltreatment and obsessive-compulsive disorder in adulthood. Journal of Obsessive-Compulsive and Related Disorders, 27, 100587. doi: 10.1016/j.jocrd.2020.100587 [DOI] [Google Scholar]
- Borghesi, F., Cipresso, P., Franceschini, C., Guglielmucci, F., & Musetti, A. (2022). Understanding the relationship between Traumatic experiences and Compulsive Internet use through the lens of mentalization: A mediation analysis. Annual Review of Cybertherapy and Telemedicine, 20, 121-126. [Google Scholar]
- Brüne, M., Walden, S., Edel, M.-A., & Dimaggio, G. (2016). Mentalization of complex emotions in borderline personality disorder: The impact of parenting and exposure to trauma on the performance in a novel cartoon-based task. Comprehensive Psychiatry, 64, 29-37. doi: 10.1016/j.comppsych.2015.08.003 [DOI] [PubMed] [Google Scholar]
- Catalana, A., Díaz, A., Angosto, V., Zamalloa, I., Martínez, N., Guede, D., Aguirregomoscorta, F., Bustamante, S., Larrañaga, L., & Osa, L. (2020). Can childhood trauma influence facial emotion recognition independently from a diagnosis of severe mental disorder? Revista de Psiquiatría y Salud Mental (English Edition), 13(3), 140-149. doi: 10.1016/j.rpsm.2018.10.003 [DOI] [PubMed] [Google Scholar]
- Cervin, M., Perrin, S., Olsson, E., Aspvall, K., Geller, D. A., Wilhelm, S., McGuire, J., Lázaro, L., Martínez-González, A. E., & Barcaccia, B. (2020). The centrality of doubting and checking in the network structure of obsessive-compulsive symptom dimensions in youth. Journal of the American Academy of Child & Adolescent Psychiatry, 59(7), 880-889. doi: 10.1016/j.jaac.2019.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti, D., Rogosch, F. A., Maughan, A., Toth, S. L., & Bruce, J. (2003). False belief understanding in maltreated children. Development and Psychopathology, 15(4), 1067-1091. doi: 10.1017/s0954579403000440 [DOI] [PubMed] [Google Scholar]
- Citkowska-Kisielewska, A., Rutkowski, K., Mielimaka, M., Sobanski, J. A., & Dembinska, E. (2020). Obsessive-compulsive symptoms in obsessive-compulsive disorder and in generalized anxiety disorder: occurrence and correlations. Journal of Psychiatric Practice, 26(2), 101-119. doi: 10.1097/PRA.0000000000000451 [DOI] [PubMed] [Google Scholar]
- Claussen, A. H., Mundy, P. C., Mallik, S. A., & Willoughby, J. C. (2002). Joint attention and disorganized attachment status in infants at risk. Development and Psychopathology, 14(2), 279-291. doi: 10.1017/s0954579402002055 [DOI] [PubMed] [Google Scholar]
- Copeland, W. E., Shanahan, L., Hinesley, J., Chan, R. F., Aberg, K. A., Fairbank, J. A., van den Oord, E. J., & Costello, E. J. (2018). Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Network Open, 1(7), e184493-e184493. doi: 10.1001/jamanetworkopen.2018.4493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dar, R., Sarna, N., Yardeni, G., & Lazarov, A. (2022). Are people with obsessive-compulsive disorder under-confident in their memory and perception? A review and meta-analysis. Psychological Medicine, 52(13), 2404-2412. doi: 10.1017/S0033291722001908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Leo, D. , Frisoni, G. B., Rozzini, R., & Trabucchi, M. (1993). Italian community norms for the Brief Symptom Inventory in the elderly. The British Journal of Clinical Psychology, 32(2), 209-213. doi: 10.1111/j.2044-8260.1993.tb01045.x [DOI] [PubMed] [Google Scholar]
- De Putter, L. M. S., Van Yper, L., & Koster, E. H. W. (2017). Obsessions and compulsions in the lab: A meta-analysis of procedures to induce symptoms of obsessive-compulsive disorder. Clinical Psychology Review, 52, 137-147. doi: 10.1016/j.cpr.2017.01.001 [DOI] [PubMed] [Google Scholar]
- Derogatis, L. R., & Melisaratos, N. (1983). The Brief Symptom Inventory: an introductory report. Psychological Medicine, 13(3), 595-605. [PubMed] [Google Scholar]
- Desatnik, A., Bird, A., Shmueli, A., Venger, I., & Fonagy, P. (2023). The mindful trajectory: Developmental changes in mentalizing throughout adolescence and young adulthood. PLoS One, 18(6), e0286500. doi: 10.1371/journal.pone.0286500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Destree, L., Brierley, M.-E. E., Albertella, L., Jobson, L., & Fontenelle, L. F. (2021). The effect of childhood trauma on the severity of obsessive-compulsive symptoms: A systematic review. Journal of Psychiatric Research, 142, 345-360. doi: 10.1016/j.jpsychires.2021.08.017 [DOI] [PubMed] [Google Scholar]
- Doba, K., Saloppé, X., Choukri, F., & Nandrino, J.-L. (2022). Childhood trauma and posttraumatic stress symptoms in adolescents and young adults: The mediating role of mentalizing and emotion regulation strategies. Child Abuse & Neglect, 132, 105815. doi: 10.1016/j.chiabu.2022.105815 [DOI] [PubMed] [Google Scholar]
- Duval, J., Ensink, K., Normandin, L., & Fonagy, P. (2018). Mentalizing mediates the association between childhood maltreatment and adolescent borderline and narcissistic personality traits. Adolescent Psychiatry, 8(3), 156-173. doi: 10.3390/jcm10225293 [DOI] [Google Scholar]
- Dykas, M. J., & Cassidy, J. (2011). Attachment and the processing of social information across the life span: theory and evidence. Psychological Bulletin, 137(1), 19. doi: 10.1037/a0021367 [DOI] [PubMed] [Google Scholar]
- Ensink, K., Normandin, L., Target, M., Fonagy, P., Sabourin, S., & Berthelot, N. (2015). Mentalization in children and mothers in the context of trauma: An initial study of the validity of the Child Reflective Functioning Scale. British Journal of Developmental Psychology, 33(2), 203-217. doi: 10.1111/bjdp.12074 [DOI] [PubMed] [Google Scholar]
- Farina, B., & Liotti, G. (2013). Does a dissociative psychopathological dimension exist? A review on dissociative processes and symptoms in developmental trauma spectrum disorders. Clinical Neuropsychiatry, 10(1), 11-18. doi: 10.3389/fpsyg.2019.00933 [DOI] [Google Scholar]
- Farina, B., Liotti, M., & Imperatori, C. (2019). The Role of Attachment Trauma and Disintegrative Pathogenic Processes in the Traumatic-Dissociative Dimension. Front Psychol, 10, 933. doi: 10.3389/fpsyg.2019.00933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fineberg, N. A., Hengartner, M. P., Bergbaum, C. E., Gale, T. M., Gamma, A., Ajdacic-Gross, V., Rössler, W., & Angst, J. (2013). A prospective population-based cohort study of the prevalence, incidence and impact of obsessive-compulsive symptomatology. International Journal of Psychiatry in Clinical Practice, 17(3), 170-178. doi: 10.3109/13651501.2012.755206 [DOI] [PubMed] [Google Scholar]
- Fonagy, P., Gergely, G., Jurist, E., & Target, M. (2002). Affect regulation, mentalization and the development of the self. London: Routledge. [Google Scholar]
- Fradkin, I., Ludwig, C., Eldar, E., & Huppert, J. D. (2020). Doubting what you already know: Uncertainty regarding state transitions is associated with obsessive compulsive symptoms. PLoS Computational Biology, 16(2), e1007634. doi: 10.1371/journal.pcbi.1007634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz, M. S., & Mackinnon, D. P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18(3), 233-239. doi: 10.1111/j.1467-9280.2007.01882.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Froreich, F. V., Vartanian, L. R., Grisham, J. R., & Touyz, S. W. (2016). Dimensions of control and their relation to disordered eating behaviours and obsessive-compulsive symptoms. Journal of Eating Disorders, 4(1), 1-9. doi: 10.1186/s40337-016-0104-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullana, M. A., Vilagut, G., Rojas-Farreras, S., Mataix-Cols, D., de Graaf, R., Demyttenaere, K., Haro, J. M., de Girolamo, G., Lépine, J. P., & Matschinger, H. (2010). Obsessive–compulsive symptom dimensions in the general population: Results from an epidemiological study in six European countries. Journal of Affective Disorders, 124(3), 291-299. doi: 10.1016/j.jad.2009.11.020 [DOI] [PubMed] [Google Scholar]
- Georgieva, S., Tomas, J. M., & Navarro-Perez, J. J. (2021). Systematic review and critical appraisal of Childhood Trauma Questionnaire - Short Form (CTQ-SF). Child Abuse & Neglect, 120, 105223. doi: 10.1016/j.chiabu.2021.105223 [DOI] [PubMed] [Google Scholar]
- Gillan, C. M., Papmeyer, M., Morein-Zamir, S., Sahakian, B. J., Fineberg, N. A., Robbins, T. W., & de Wit, S. (2011). Disruption in the balance between goal-directed behavior and habit learning in obsessive-compulsive disorder. The American Journal of Psychiatry, 168(7), 718-726. doi: 10.1176/appi.ajp.2011.10071062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grassi, L., Caruso, R., Mitchell, A. J., Sabato, S., & Nanni, M. G. (2018). Screening for emotional disorders in patients with cancer using the Brief Symptom Inventory (BSI) and the BSI-18 versus a standardized psychiatric interview (the World Health Organization Composite International Diagnostic Interview). Cancer, 124(11), 2415-2426. doi: 10.1002/cncr.31340 [DOI] [PubMed] [Google Scholar]
- Grassi, L., Mondardini, D., Pavanati, M., Sighinolfi, L., Serra, A., & Ghinelli, F. (2001). Suicide probability and psychological morbidity secondary to HIV infection: a control study of HIV-seropositive, hepatitis C virus (HCV)-seropositive and HIV/HCV-seronegative injecting drug users. Journal of Afective Disorders, 64(2-3), 195-202. doi: 10.1016/s0165-0327(00)00244-5 [DOI] [PubMed] [Google Scholar]
- Grassi, L., Rasconi, G., Pedriali, A., Corridoni, A., & Bevilacqua, M. (2000). Social support and psychological distress in primary care attenders. Ferrara SIMG Group. Psychotherapy and Psychosomatics, 69(2), 95-100. doi: 10.1159/000012372 [DOI] [PubMed] [Google Scholar]
- Gruhn, M. A., & Compas, B. E. (2020). Effects of maltreatment on coping and emotion regulation in childhood and adolescence: A meta-analytic review. Child Abuse & Neglect, 103, 104446. doi: 10.1016/j.chiabu.2020.104446 [DOI] [PubMed] [Google Scholar]
- Harris, P. L., Koenig, M. A., Corriveau, K. H., & Jaswal, V. K. (2018). Cognitive foundations of learning from testimony. Annual Review of Psychology, 69, 251-273. doi: 10.1146/annurev-psych-122216-011710 [DOI] [PubMed] [Google Scholar]
- Hausberg, M. C., Schulz, H., Piegler, T., Happach, C. G., Klöpper, M., Brütt, A. L., Sammet, I., & Andreas, S. (2012). Is a self-rated instrument appropriate to assess mentalization in patients with mental disorders? Development and first validation of the Mentalization Questionnaire (MZQ). Psychotherapy Research, 22(6), 699-709. doi: 10.1080/10503307.2012.709325 [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2022). Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Publications. [Google Scholar]
- Hopfinger, L., Berking, M., Bockting, C. L., & Ebert, D. D. (2016). Emotion regulation mediates the effect of childhood trauma on depression. Journal of Afective Disorders, 198, 189-197. doi: 10.1016/j.jad.2016.03.050 [DOI] [PubMed] [Google Scholar]
- Huang, Y. L., Fonagy, P., Feigenbaum, J., Montague, P. R., Nolte, T., & Consortium, M. D. R. (2020). Multidirectional pathways between attachment, mentalizing, and posttraumatic stress symptomatology in the context of childhood trauma. Psychopathology, 53(1), 48-58. doi: 10.1159/000506406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imperatori, C., Corazza, O., Panno, A., Rinaldi, R., Pasquini, M., Farina, B., Biondi, M., & Bersani, F. S. (2020). Mentalization Impairment Is Associated with Problematic Alcohol Use in a Sample of Young Adults: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 17(22), 8664. doi: 10.3390/ijerph17228664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs, D., Key, A. P., Cascio, C. J., Conley, A. C., Walker, H. C., Wallace, M. T., & Claassen, D. O. (2020). Sensory hypersensitivity severity and association with obsessive-compulsive symptoms in adults with tic disorder. Neuropsychiatric Disease and Treatment, 2591-2601. doi: 10.2147/NDT.S274165 [DOI] [PMC free article] [PubMed]
- Kadivari, F., Najafi, M., & Khosravani, V. (2023). Childhood emotional maltreatment, maladaptive coping and obsessive–compulsive symptoms in patients with obsessive–compulsive disorder. Clinical Psychology & Psychotherapy, 30(3), 620-630. 10.1002/cpp.2829 [DOI] [PubMed] [Google Scholar]
- Kim, H. Y. (2013). Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restorative Dentistry & Endodontics, 38(1), 52-54. doi: 10.5395/rde.2013.38.1.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobak, R., Zajac, K., Abbott, C., Zisk, A., & Bounoua, N. (2017). Atypical dimensions of caregiver–adolescent interaction in an economically disadvantaged sample. Development and Psychopathology, 29(2), 405-416. doi: 10.1017/S0954579417000074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokkinos, C. M., Kakarani, S., & Kolovou, D. (2016). Relationships among shyness, social competence, peer relations, and theory of mind among pre-adolescents. Social Psychology of Education, 19, 117-133. doi: 10.1007/s11218-015-9317-7 [DOI] [Google Scholar]
- Kongerslev, M. T., Bach, B., Rossi, G., Trauelsen, A. M., Ladegaard, N., Lokkegaard, S. S., & Bo, S. (2019). Psychometric validation of the Childhood Trauma Questionnaire-Short Form (CTQ-SF) in a Danish clinical sample. Child Abuse Negl, 94, 104026. doi: 10.1016/j.chiabu.2019.104026 [DOI] [PubMed] [Google Scholar]
- Kovács, Á. M., Téglás, E., & Endress, A. D. (2010). The social sense: Susceptibility to others’ beliefs in human infants and adults. Science, 330(6012), 1830-1834. doi: 10.1126/science.1190792 [DOI] [PubMed] [Google Scholar]
- Kroska, E. B., Miller, M. L., Roche, A. I., Kroska, S. K., & O’Hara, M. W. (2018). Effects of traumatic experiences on obsessive-compulsive and internalizing symptoms: The role of avoidance and mindfulness. Journal of Affective Disorders, 225, 326-336. doi: 10.1016/j.jad.2017.08.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labad, J., Menchon, J. M., Alonso, P., Segalas, C., Jimenez, S., Jaurrieta, N., Leckman, J. F., & Vallejo, J. (2008). Gender differences in obsessive-compulsive symptom dimensions. Depression and Anxiety, 25(10), 832-838. doi: 10.1002/da.20332 [DOI] [PubMed] [Google Scholar]
- Laisney, M., Bon, L., Guiziou, C., Daluzeau, N., Eustache, F., & Desgranges, B. (2013). Cognitive and afective Theory of Mind in mild to moderate Alzheimer's disease. Journal of Neuropsycholgy, 7(1), 107-120. doi: 10.1111/j.1748-6653.2012.02038.x [DOI] [PubMed] [Google Scholar]
- Levy, J., Goldstein, A., & Feldman, R. (2019). The neural development of empathy is sensitive to caregiving and early trauma. Nature Communications, 10(1), 1905. doi: 10.1038/s41467-019-09927-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, E. T., Carracher, E., & Bird, T. (2020). Linking childhood emotional abuse and adult depressive symptoms: The role of mentalizing incapacity. Child Abuse & Neglect, 99, 104253. doi: 10.1016/j.chiabu.2019.104253 [DOI] [PubMed] [Google Scholar]
- Liljenfors, R., & Lundh, L.-G. (2015). Mentalization and intersubjectivity towards a theoretical integration. Psychoanalytic Psychology, 32(1), 36. doi: 10.1037/a0037129 [DOI] [Google Scholar]
- Luyten, P., Campbell, C., Allison, E., & Fonagy, P. (2020). The mentalizing approach to psychopathology: State of the art and future directions. Annual Review of Clinical Psychology, 16, 297-325. doi: 10.1146/annurev-clinpsy-071919-015355 [DOI] [PubMed] [Google Scholar]
- Luyten, P., & Fonagy, P. (2015). The neurobiology of mentalizing. Personality Disorders, 6(4), 366. [DOI] [PubMed] [Google Scholar]
- MacIntosh, H. B. (2013). Mentalizing and its role as a mediator in the relationship between childhood experiences and adult functioning: Exploring the empirical evidence. Psihologija, 46(2), 193-212. doi: 10.2298/PSI1302193M [DOI] [Google Scholar]
- Malda-Castillo, J., Browne, C., & Perez-Algorta, G. (2019). Mentalization-based treatment and its evidence-base status: A systematic literature review. Psychology and Psychotherapy: Theory, Research and Practice, 92(4), 465-498. doi: 10.1111/papt.12195 [DOI] [PubMed] [Google Scholar]
- Maraone, A., Panfili, M., Jones, G. W., Pinucci, I., Biondi, M., & Pasquini, M. (2024). The Compulsive Obsessive Disorder: many clues, still little evidence. Journal of Psychopathology, 30(1), 8-19. doi: 10.36148/2284-0249-N452 [DOI] [Google Scholar]
- Maraz, A., Van den Brink, W., & Demetrovics, Z. (2015). Prevalence and construct validity of compulsive buying disorder in shopping mall visitors. Psychiatry Research, 228(3), 918-924. doi: 10.1016/j.psychres.2015.04.012 [DOI] [PubMed] [Google Scholar]
- Massullo, C., De Rossi, E., Carbone, G. A., Imperatori, C., Ardito, R. B., Adenzato, M., & Farina, B. (2023). Child Maltreatment, Abuse, and Neglect: An Umbrella Review of Their Prevalence and Definitions. Clinical Neuropsychiatry, 20(2), 72-99. doi: 10.36131/cnfioritieditore20230201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews, C. A., Kaur, N., & Stein, M. B. (2008). Childhood trauma and obsessive-compulsive symptoms. Depression and Anxiety, 25(9), 742-751. doi: 10.1002/da.20316 [DOI] [PubMed] [Google Scholar]
- Mathis, M. A. d., Alvarenga, P. d., Funaro, G., Torresan, R. C., Moraes, I., Torres, A. R., Zilberman, M. L., & Hounie, A. G. (2011). Gender differences in obsessive-compulsive disorder: a literature review. Brazilian Journal of Psychiatry, 33(4), 390-399. doi: 10.1590/S1516-44462011000400014 [DOI] [PubMed] [Google Scholar]
- McKay, M. T., Cannon, M., Chambers, D., Conroy, R. M., Coughlan, H., Dodd, P., Healy, C., O’Donnell, L., & Clarke, M. C. (2021). Childhood trauma and adult mental disorder: A systematic review and meta‐analysis of longitudinal cohort studies. Acta Psychiatrica Scandinavica, 143(3), 189-205. doi: 10.1111/acps.13268 [DOI] [PubMed] [Google Scholar]
- Mcquaid, N., Bigelow, A. E., McLaughlin, J., & MacLean, K. (2008). Maternal mental state language and preschool children's attachment security: Relation to children's mental state language and expressions of emotional understanding. Social Development, 17(1), 61-83. doi: 10.1111/j.1467-9507.2007.00415.x [DOI] [Google Scholar]
- Meins, E., Harris-Waller, J., & Lloyd, A. (2008). Understanding alexithymia: Associations with peer attachment style and mind-mindedness. Personality and Individual Differences, 45(2), 146-152. doi: 10.1016/j.paid.2008.03.013 [DOI] [Google Scholar]
- Miller, D. K. (2006). The effects of childhood physical abuse or childhood sexual abuse in battered women's coping mechanisms: Obsessive-compulsive tendencies and severe depression. Journal of Family Violence, 21(3), 185-195. [Google Scholar]
- Moll, H., Richter, N., Carpenter, M., & Tomasello, M. (2008). Fourteen-month-olds know what “we” have shared in a special way. Infancy, 13(1), 90-101. doi: 10.1080/15250000701779402 [DOI] [Google Scholar]
- Moretti, G., Pasquini, M., Mandarelli, G., Tarsitani, L., & Biondi, M. (2008). What every psychiatrist should know about PANDAS: a review. Clinical Practice and Epidemiology in Mental Health, 4, 13. doi: 10.1186/1745-0179-4-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nezgovorova, V., Reid, J., Fineberg, N. A., & Hollander, E. (2022). Optimizing first line treatments for adults with OCD. Comprehensive Psychiatry, 115, 152305. doi: 10.1016/j.comppsych.2022.152305 [DOI] [PubMed] [Google Scholar]
- Nikodijevic, A., Moulding, R., Anglim, J., Aardema, F., & Nedeljkovic, M. (2015). Fear of self, doubt and obsessive compulsive symptoms. Journal of Behavior Therapy and Experimental Psychiatry, 49, 164-172. doi: 10.1016/j.jbtep.2015.02.005 [DOI] [PubMed] [Google Scholar]
- Oehlman Forbes, D., Lee, M., & Lakeman, R. (2021). The role of mentalization in child psychotherapy, interpersonal trauma, and recovery: A scoping review. Psychotherapy, 58(1), 50. doi: 10.1037/pst0000341 [DOI] [PubMed] [Google Scholar]
- Okasha, A., Ragheb, K., Attia, A., Seif el Dawla, A., Okasha, T., & Ismail, R. (2001). Prevalence of obsessive compulsive symptoms (OCS) in a sample of Egyptian adolescents. L'encephale, 27(1), 8-14. [PubMed] [Google Scholar]
- Panfile, T. M., & Laible, D. J. (2012). Attachment security and child's empathy: The mediating role of emotion regulation. Merrill-Palmer Quarterly, 58(1), 1-21. [Google Scholar]
- Pardini, M., & Nichelli, P. F. (2009). Age-Related Decline in Mentalizing Skills Across Adult Life Span. Experimental Aging Research, 35(1), 98-106. doi: 10.1080/03610730802545259 [DOI] [PubMed] [Google Scholar]
- Pears, K. C., & Fisher, P. A. (2005). Emotion understanding and theory of mind among maltreated children in foster care: Evidence of deficits. Development and Psychopathology, 17(1), 47-65. doi: 10.1017/s0954579405050030 [DOI] [PubMed] [Google Scholar]
- Piacentino, D., Maraone, A., Roselli, V., Berardelli, I., Biondi, M., Kotzalidis, G. D., & Pasquini, M. (2020). Eficacy of nicotine administration on obsessions and compulsions in OCD: a systematic review. Annals of General Psychiatry, 19(1), 57. doi: 10.1186/s12991-020-00309-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raimondi, G., Samela, T., Lester, D., Imperatori, C., Carlucci, L., Contardi, A., Balsamo, M., & Innamorati, M. (2021). Psychometric Properties of the Italian Mentalization Questionnaire: Assessing Structural Invariance and Construct Validity. Journal of Personality Assessment, 1-9. doi: 10.1080/00223891.2021.1991362 [DOI] [PubMed]
- Rice, K. G., & Pence, S. L. (2006). Perfectionism and obsessive-compulsive symptoms. Journal of Psychopathology and Behavioral Assessment, 28(2), 103-111. doi: 10.1007/s10862-006-7488-4 [DOI] [Google Scholar]
- Robinson, P., Hellier, J., Barrett, B., Barzdaitiene, D., Bateman, A., Bogaardt, A., Clare, A., Somers, N., O’Callaghan, A., & Goldsmith, K. (2016). The NOURISHED randomised controlled trial comparing mentalisation-based treatment for eating disorders (MBT-ED) with specialist supportive clinical management (SSCM-ED) for patients with eating disorders and symptoms of borderline personality disorder. Trials, 17, 1-15. doi: 10.1186/s13063-016-1606-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothenberger, A., & Roessner, V. (2019). Psychopharmacotherapy of obsessive-compulsive symptoms within the framework of Tourette syndrome. Current Neuropharmacology, 17(8), 703-709. doi: 10.2174/1570159X16666180828095131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacchi, C., Vieno, A., & Simonelli, A. (2018). Italian validation of the Childhood Trauma Questionnaire-Short Form on a college group. Psychological Trauma, 10(5), 563-571. doi: 10.1037/tra0000333 [DOI] [PubMed] [Google Scholar]
- Samuels, J., Bienvenu, O. J., Krasnow, J., Wang, Y., Grados, M. A., Cullen, B., Goes, F. S., Maher, B., Greenberg, B. D., & McLaughlin, N. C. (2017). An investigation of doubt in obsessive–compulsive disorder. Comprehensive Psychiatry, 75, 117-124. doi: 10.1016/j.comppsych.2017.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoro, G., Sideli, L., Gugliemucci, F., Terrone, G., & Schimmenti, A. (2023). Traumatic Experiences and Obsessive-Compulsive Symptoms: The Mediating Role of Dissociation. The Journal of Nervous and Mental Disease, 211(7), 543-549. doi: 10.1097/nmd.0000000000001649 [DOI] [PubMed] [Google Scholar]
- Schwarzer, N.-H., Nolte, T., Fonagy, P., & Gingelmaier, S. (2021). Mentalizing mediates the association between emotional abuse in childhood and potential for aggression in non-clinical adults. Child Abuse & Neglect, 115, 105018. doi: 10.1016/j.chiabu.2021.105018 [DOI] [PubMed] [Google Scholar]
- Scott, R. M., & Baillargeon, R. (2017). Early false-belief understanding. Trends in Cognitive Sciences, 21(4), 237-249. doi: 10.1016/j.tics.2017.01.012 [DOI] [PubMed] [Google Scholar]
- See, C. C., Tan, J. M., Tan, V. S., & Sündermann, O. (2022). A systematic review on the links between emotion regulation difficulties and obsessive-compulsive disorder. Journal of Psychiatric Research. doi: 10.1016/j.jpsychires.2022.07.023 [DOI] [PubMed]
- Siswati, B. H., & Corebima, A. D. (2017). The effect of education level and gender on students’ metacognitive skills in Malang, Indonesia. Advances in Social Sciences Research Journal, 4(4), 163-168. doi: 10.14738/assrj.44.2813. [DOI] [Google Scholar]
- Skapinakis, P., Politis, S., Karampas, A., Petrikis, P., & Mavreas, V. (2019). Prevalence, comorbidity, quality of life and use of services of obsessive-compulsive disorder and subthreshold obsessive-compulsive symptoms in the general adult population of Greece. International Journal of Psychiatry in Clinical Practice, 23(3), 215-224. doi: 10.1080/13651501.2019.1588327 [DOI] [PubMed] [Google Scholar]
- Sloover, M., van Est, L. A., Janssen, P. G., Hilbink, M., & van Ee, E. (2022). A Meta-analysis of Mentalizing in Anxiety Disorders, Obsessive-Compulsive and Related Disorders, and Trauma-and Stressor Related Disorders. Journal of Anxiety Disorders, 92, 102641. doi: 10.1016/j.janxdis.2022.102641 [DOI] [PubMed] [Google Scholar]
- Song, H.-j., Onishi, K. H., Baillargeon, R., & Fisher, C. (2008). Can an agent’s false belief be corrected by an appropriate communication? Psychological reasoning in 18-month-old infants. Cognition, 109(3), 295-315. doi: 10.1016/j.cognition.2008.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stavropoulos, V., Moore, K. A., Lazaratou, H., Dikaios, D., & Gomez, R. (2017). A multilevel longitudinal study of obsessive compulsive symptoms in adolescence: male gender and emotional stability as protective factors. Annals of General Psychiatry, 16, 42. doi: 10.1186/s12991-017-0165-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein, D. J., Costa, D. L. C., Lochner, C., Miguel, E. C., Reddy, Y. C. J., Shavitt, R. G., van den Heuvel, O. A., & Simpson, H. B. (2019). Obsessive-compulsive disorder. Nature Reviews Disease Primers, 5(1), 52. doi: 10.1038/s41572-019-0102-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun, J., Boschen, M. J., Farrell, L. J., Buys, N., & Li, Z.-J. (2014). Obsessive–compulsive symptoms in a normative Chinese sample of youth: Prevalence, symptom dimensions, and factor structure of the Leyton Obsessional Inventory—Child Version. Journal of Affective Disorders, 164, 19-27. doi: 10.1016/j.jad.2014.04.004 [DOI] [PubMed] [Google Scholar]
- Taubner, S., & Curth, C. (2013). Mentalization mediates the relation between early traumatic experiences and aggressive behavior in adolescence. Psihologija, 46(2), 177-192. doi: 10.1159/000448053 [DOI] [Google Scholar]
- Tezenas du Montcel, C., Pelissolo, A., Schürhoff, F., & Pignon, B. (2019). Obsessive-compulsive symptoms in schizophrenia: an up-to-date review of literature. Current Psychiatry Reports, 21(8), 1-8. doi: 10.1007/s11920-019-1051-y [DOI] [PubMed] [Google Scholar]
- Toof, J., Wong, J., & Devlin, J. M. (2020). Childhood trauma and attachment. Fam J, 28(2), 194-198. doi: 10.1177/1066480720902106 [DOI] [Google Scholar]
- Troyer, D., & Greitemeyer, T. (2018). The impact of attachment orientations on empathy in adults: Considering the mediating role of emotion regulation strategies and negative affectivity. Personality and Individual Differences, 122, 198-205. doi: 10.1016/j.paid.2017.10.033 [DOI] [Google Scholar]
- Valérie, C., Valérie, S., & Julie, A. (2023). Meta-analyses of the associations of mentalization and proxy variables with anxiety and internalizing problems. Journal of Anxiety Disorders, 95(8), 1–20. 10.1016/j.janxdis.2023.102694 [DOI] [PubMed] [Google Scholar]
- Vivan Ade, S., Rodrigues, L., Wendt, G., Bicca, M. G., Braga, D. T., & Cordioli, A. V. (2014). Obsessive-compulsive symptoms and obsessive-compulsive disorder in adolescents: a population-based study. Revista Brasileira de Psiquiatria 36(2), 111-118. doi: 10.1590/1516-4446-2013-1113 [DOI] [PubMed] [Google Scholar]
- Volkert, J., Hauschild, S., & Taubner, S. (2019). Mentalization-based treatment for personality disorders: efficacy, effectiveness, and new developments. Current Psychiatry Reports, 21, 1-12. doi: 10.1007/s11920-019-1012-5 [DOI] [PubMed] [Google Scholar]
- Woody, S. R., Steketee, G., & Chambless, D. L. (1995). The usefulness of the obsessive compulsive scale of the Symptom Checklist-90-Revised. Behaviour Research and Therapy, 33(5), 607-611. doi: 10.1016/0005-7967(94)00090-7 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2022). Child Maltreatment. https://www.who.int/news-room/fact-sheets/detail/child-mal-treatment.
- Zaccagnino, M., Cussino, M., Preziosa, A., Veglia, F., & Carassa, A. (2015). Attachment representation in institutionalized children: A preliminary study using the child attachment interview. Clinical Psychology & Psychotherapy, 22(2), 165-175. doi: 10.1002/cpp.1882 [DOI] [PubMed] [Google Scholar]
- Zhang, H., Gao, X., Liang, Y., Yao, Q., & Wei, Q. (2023). Does child maltreatment reduce or increase empathy? A systematic review and meta-analysis. Trauma, Violence, & Abuse, 15248380221145734. doi: 10.1177/15248380221145734 [DOI] [PubMed] [Google Scholar]