Abstract
Objective
Study on the role of electrocardiographic (ECG) exercise testing for the possibility of permanent pacemaker implantation (PPI) in patients with sinus bradycardia (SB).
Methods
Cross-sectional descriptive, prospective study. The study on 60 patients with SB below 50 beats/minute on 12-lead electrocardiogram at rest, with or without symptoms of SB, conducted at the Vietnam National Heart Institute and Hanoi Heart Hospital from January 2020 to September 2021.
Results
Sixty patients with SB were studied, 36 male (60%) and 24 female patients (40%), p > 0.05. The average age was 55.12 ± 13.89 years old. Maximum exercise capacity (MEC) is low and only reaches 7.78 ± 3.59 metabolic equivalents (METs); Not reaching 85% of predicted MEC accounts for 53.5%; Maximum exercise time is 10.53 ± 0.46 minutes; Impaired heart rate (HR) variability in patients with SB is high: Chronotropic Index <0.8 accounts for 53.5%, not reaching 85% of predicted HR max accounts for 45%. The average HR max was 129.90 ± 29.22 beats per minute (BPM). The average maximum workload systolic blood pressure was 155.23 ± 20.59 mmHg. The average value of maximum exercise diastolic blood pressure was 88.10 ± 9.11 mmHg. The HR decreased by 27.87 ± 16.82 BPM in the first minute. Not achieving 85% of predicted MEC (p = 0.062), so it is not an independent factor predicting the ability for PPI. Only the HR variability index <0.8 is an independent predictor for PPI in bradycardic patients, which has OR = 21.521 (95% CI: 2.27–04.34, p < 0.05).
Conclusion
Results can be seen that Chronotropic Index <0.8 is an important marker for physicians to decide on PPI in ECG during exercise testing in SB patients and is a potential prognostic factor for the need for PPI.
Keywords: role, exercise ECG testing, PPI, possibility of PPI
Introduction
Sinus bradycardia (SB) is defined as a sinus rhythm with a heart rate of <50 beats/minute at rest.1 The worldwide prevalence of bradycardia is about 2.6%.2 Sinus bradycardia can occur in completely healthy people, but it can also be a pathological disorder of the rhythm generation system or the automatic conduction system in the heart.3–6 Exercise capacity assessment using electrocardiographic (ECG) exercise testing has been shown to be effective in providing individual prognosis in patients with sinus bradycardia.7,8 In addition, some other parameters of ECG exercise testing can also assess the status of heart rate modulation in sinus node dysfunction, thereby helping physicians to decide on permanent pacemaker implantation (PPI) in a way that is appropriate for each specific patient.1,9
There have also been a number of studies around the world on the effectiveness of this technique in different populations,7,10–12 which has been endorsed by the ACC/AHA/HRS (2018)1 and ESC (2021).9 However, in clinical practice, the role of ECG exercise testing is not yet given due attention.1,9 Furthermore, currently in Vietnam, there have been no surveys of ECG exercise testing in patients with sinus bradycardia to further study the physiology, pathophysiology, and role of ECG exercise testing in clinical practice. Therefore, we conducted this study with the main goal: “Evaluate exercise capacity the role of ECG exercise testing in patients with sinus bradycardia, thereby evaluating the role of ECG exercise testing in patients with the possibility of PPI”.
Materials and Method
Participant
The study will be conducted on 60 patients with sinus bradycardia below 50 beats/minute on 12-lead electrocardiogram (ECG) at rest, with or without symptoms of bradycardia. The study has been already conducted at the Vietnam Heart Institute – Bach Mai Hospital and Hanoi Heart Hospital between January 2020 and September 2021.
Research Design and Population
Research design: Cross-sectional descriptive, prospective study.
Research Population: The sample size was calculated using a formula to estimate a proportion:
 |
where n: sample size; Z: with a 95% confidence level, the Z value (1 - a/2) = 1.96; p: proportion of sinus node bradycardia. According to Paul N. Jensen et al (2014),2 the proportion of sinus node bradycardia is approximately 2.6% [(339 + 217)/(15,792 + 5888)]; d: allowable error (d = 0.05). Using the formula, the calculated sample size is n = 45.
Measurement Method
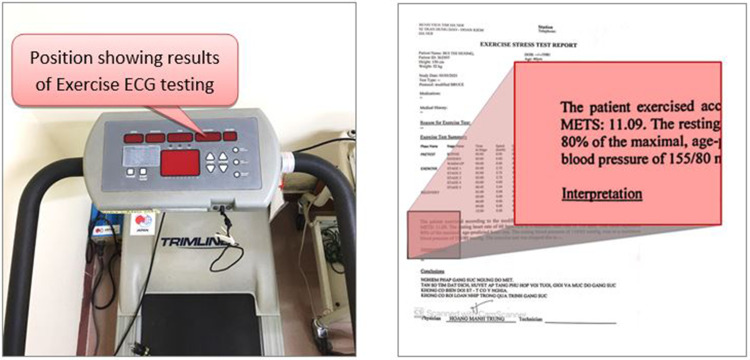
Measurement exercise capacity is based on metabolic equivalent of task (MET) as energy required. One MET represents the energy required that human burn at rest in one minute, which is 3.5 mL of oxygen, per kilogram of body weight, per minute (Figure 1).1,7–9,13
Figure 1.
Position showing results of electrocardiographic exercise testing.
Heart Rate Variability Index (Chronotropic Index - CI)
Since the maximum heart rate during exercise is related to the heart rate at rest, most studies have used the Heart Rate Variability Index (CI) to assess heart rate variability instead of HR max. CI is calculated according to the following formula: CI = (Actual HR max – Resting HR)/(Predicted HR max – Resting HR).1,7–9,13
Inability to Regulate Heart Rate is Diagnosed When CI < 80%
This criterion was included as one of the diagnostic criteria for sinus node dysfunction (SND) in the 2018 ACC/AHA/HRS recommendations.1,7,13
Heart Rate During Recovery Phase
Abnormally slow heart rate during recovery is defined as a decrease of less than 12 beats per minute (BPM) within the first minute upon standing after exercise. This is a predictor of increased mortality from all causes and cardiovascular events.1,7–9,13
Blood Pressure During Exercise
Decrease hypertension during exercise is a decrease in systolic blood pressure (SBP) below resting blood pressure or an increase in diastolic blood pressure (DBP) during early stages of exercise, followed by a decrease of more than 10 mmHg; Increase hypertension during exercise is an increase in SBP above 210 mmHg for male and 190 mmHg for female or an increase in DBP of more than 10 mmHg compared to resting values or above 90 mmHg.1,7–9,13
The study has excluded cases with contraindications for ECG exercise testing according to recommended standards.1,9
Diagnostic criteria on ECG: Diagnostic criteria on Holter 24-hour ECG Apply according to the definition of sinus node dysfunction and conduction disorders of the 2018 ACC/AHA/HRS recommendations.1
Standards for evaluating the results of ECG exercise testing: Apply according to ACC/AHA 2013 guidelines on ECG.8
Research Data Processing
Using SPSS 25.0 statistical analysis software. Descriptive statistics and analysis: Qualitative data will be presented as percentages, and quantitative data will be presented as mean ± standard deviation or median and interquartile range depending on the distribution characteristics. Linear regression: Used to investigate factors associated with exercise capacity in patients with sinus node bradycardia.
Logistic regression: The chi-square test will be used to assess the hypothesis of the model fit compared to the empty model. The Hosmer-Leme show test will assess the goodness of fit. The regression coefficient (β) and OR index evaluate the relationship between the dependent variable and the independent variable (using the Wald test to evaluate).
Result
Characteristics of Electrocardiographic Exercise Testing
Baseline Characteristics
A total of 60 patients with sinus bradycardia were studied, including 36 male patients (accounting for 60%) and 24 female patients (accounting for 40%). There was no statistically significant difference in gender distribution (p < 0.05). The average age of the patients with sinus node bradycardia was 55.12 ± 13.89 years old.
Evaluation of Exercise Capacity by Exercise Electrocardiographic Testing in Patients with Sinus Bradycardia
Distribution of the number and proportion of patients who achieved maximum effort at each stage during ECG exercise testing: In practice, there are eight stages in total when performing an ECG exercise testing. All patients underwent an ECG exercise testing and achieved maximum effort. In particular, the maximum exercise capacity of patients: stopping at stage 5 and stage 3 accounts for the highest rate of 26.7%, stopping at stage 4 is 18.3%, stopping at stage 6 is 13.3%, stopping at stage 2 is 11.7%, and only 3.3% stopped at stage 7. The result shows that all 60 patients completed the ECG exercise testing, meaning they all reached their maximum effort. Stages 2 and 3 had the highest number of patients stopping (26.7% each). Average time to achieve maximum effort was 10.53 ± 0.46 minutes.
In the study patient group, the proportion of patients who did not achieve the target indicators was quite high. The proportion of patients who achieved 85% of predicted maximum heart rate was 45% (predicted HR max = 220 − age). The proportion of patients with a heart rate variability index <0.8 was 53.3%. The proportion of patients who did not achieve 85% of predicted maximum exercise capacity was 53.3%. However, the proportion of patients with heart rate recovery in the first minute below 12 beats/minute was low (11.6%).
Evaluating the resulting indicators when performing physical exertion, the research team observed that the MEC achieved was 7.78 ± 3.59 METs. The average heart rate during peak exercise was 129.90 ± 29.22 (beats/minute), and the heart rate variability index (HRVI) was 0.64 ± 0.25.
At the time before exercise, in the standing position, the average SBP was 122.10 ± 2.23 (mmHg) and the average SBP was 72.50 ± 1.02 (mmHg). During peak exercise, the average SBP was 155.23 ± 20.59 (mmHg) and the average DBP was 88.10 ± 9.11 (mmHg). The change in SBP per METs was 4.84 ± 2.72, and the change in DBP per METs was 2.4 ± 1.75. The heart rate decrease in the first minute of the recovery period was 27.87 ± 16.82 (beats/minute).
Relationship Between Achieving Target Indicators in Patients Undergoing Electrocardiographic Exercise Testing and the Possibility of Permanent Pacemaker Implantation
Single-variable logistic regression to assess the relationship between achieving target indicators and pacemaker implantation shows the results that did not achieve 85% of maximum predicted exercise capacity have odd ratio (OR) = 21.67 (95% Confidence Interval: 4.35–105.01). Heart rate variability index <0.8 has OR = 51.55 (6.16–431.61), and Abnormal heart rate decrease during recovery period has OR = 3.43 (95% Confidence Interval: 0.73–16.07).
The results of single-variable logistic regression showed that the independent variable of abnormal heart rate decrease during the recovery period with p > 0.05 will not be included in multivariable logistic regression. There are 2 independent variables: heart rate variability index <0.8 with OR = 54.38 (95% Confidence Interval: 6.46–451.28) and did not achieve 85% of maximum predicted exercise capacity with OR = 22.67 (95% Confidence Interval: 4.58–113.01) both have p < 0.05 and are included in multivariable logistic regression to assess the relationship with pacemaker implantation in bradycardic patients.
Multivariable logistic regression results show that not achieving 85% of predicted maximum exercise capacity (p = 0.062), so it is not an independent factor predicting the ability for PPI. Only the heart rate variability index <0.8 is an independent predictor for PPI in bradycardic patients has OR = 21.521 (95% Confidence Interval: 2.27–04.34, p < 0.05).
Discussion
Characteristics of Electrocardiographic Exercise Testing
Baseline Characteristics
In our study, 60.0% of the participants were male and 40.0% were female. There was no significant difference between genders (p > 0.05). This result is consistent with the studies by Chu Dung S (2016)13 and Michael S (2013),14 which showed that the proportion of male and female patients with sinus bradycardia is similar.
The average age of the study participants was 55.12 ± 13.89 years old. The majority of the participants were aged 50 years or older (66.7%), with the most common age group being 50–59 years old. This is also consistent with the study by Chu Dung S et al (58.54 ± 17.74 years old).13 However, the results of our study are still lower than those of some other studies, such as Michael S (2013)14 reported that sinus bradycardia can occur at any age but is more common in patients over 65 years old. Hiss RG and Lamb LE (2015)15 found that sinus bradycardia is most common in people aged 20–24 years old. The epidemiological characteristics of sinus bradycardia occurring mainly in these two age groups can be explained by the fact that in healthy young people, especially athletes, sinus bradycardia can occur due to a strong parasympathetic nervous system response. In older patients, sinus bradycardia is associated with underlying diseases such as degenerative sinus node dysfunction and coronary artery disease.16
Maximum Exercise Capacity
In our study, the average exercise time was 10.53% ± 0.46 minutes. Most patients stopped exercising at stages 3 and 5 (16 patients each, accounting for 26.7% per stage), while 11 patients stopped at stage 4 (18.3%), 8 patients stopped at stage 6 (13.3%), 7 patients stopped at stage 2 (11.7%), and only 2 patients stopped at stage 7 (3.3%). No patients reached maximal exercise capacity at stage 8 (which corresponds to the exercise capacity of athletes).16 This could be due to the fact that our study included patients with sinus node dysfunction, who may have limitations in achieving maximal exercise capacity. Additionally, no patients exercised at stage 1 (which corresponds to the poorest exercise capacity).
The maximum exercise capacity achieved in our study was an average of 7.78 ± 3.56 METs (Table 1). This result is lower than the results of other studies. The study by Ahmed HM11 on 31,090 patients (mean age 55 ± 10 years, 49% female) found a mean maximum exercise capacity of 9 ± 3 METs. The study by Al-Mallah MH et al17 was conducted on 69,885 patients with a mean age of 54 ± 10 years and 54% male, found a mean maximum exercise capacity of 10 ± 3 METs. The study by Nguyen TVK et al (2020)18 on healthy Korean and Vietnamese people showed that the maximum exercise capacity of healthy Vietnamese people aged 19–35 years was 10.9 ± 1.70 METs. The best maximum exercise capacity is at 20–39 years old (around 12 METs) and at 65–79 years old, the maximum exercise capacity is only about two-thirds of the exercise capacity at 20–39 years old (8 METs).19 The results of maximum exercise capacity in these studies were higher than those in our study because this study was conducted on healthy people, while our study was conducted on a group of patients with sick sinus syndrome.
Table 1.
Proportion of Patients Who Did Not Achieve Target Indicators During Electrocardiographic Exercise Testing
| Indicator | Number (n = 60) | Percentage (%) |
|---|---|---|
| Maximum heart rate < 85% of predicted maximum heart rate | 27 | 45 |
| Heart rate variability index < 0.8 | 32 | 53.3 |
| Did not achieve 85% of predicted maximum exercise capacity | 32 | 53.3 |
| Heart rate decrease in the first 1 minute < 12 beats/minute | 7 | 11.6 |
The average peak exercise capacity in our study was low and corresponded to a high number of patients who did not achieve 85% of their predicted peak exercise capacity (32 cases, accounting for 53.5%) (Table 1). This could be explained by the fact that our study had a high number of patients who did not reach their target heart rate (85% of predicted maximum heart rate) (27 cases, accounting for 45%) and a high number of patients with a heart rate recovery index (HRRI) <0.8 (32 cases, accounting for 53.5%) (Table 1). The mechanism causing that a positive correlation exists between HR max and maximum oxygen uptake (VO2max) – patients with a lower HR max will also have a lower VO2max.
Maximum Exercise Heart Rate (HR Max)
The average HR max (Table 2) in this study was 129.90 ± 29.22 beats per minute (BPM). The authors compared this to findings from other studies such as Gulati M et al20 show that group CI 0.8 has HR max of 162 ± 13 beats/minute and group CI < 0.8 has HR max of 135 ± 12 beats/minute.
Table 2.
Characteristics of Outcome Indicators During Electrocardiographic Exercise Testing
| Indices of Heart Rate Variability and Blood Pressure During ECG Exercise Testing | Mean (X+SD) | Minimum Value | Maximum Value | |
|---|---|---|---|---|
| Maximum exercise heart rate (beats/minute) | 129,90 ± 29.22 | 80 | 168 | |
| Heart rate variability index (HRVI) | 0.64 ± 0.25 | 0,16 | 1,03 | |
| Maximum exercise capacity (MEC) | 7.78 ± 3.59 | 3,2 | 16 | |
| Heart rate decrease in the first minute of recovery (beats/minute) | 27.87 ± 16.82 | 8 | 45 | |
| Systolic blood pressure (mmHg) | Pre-exercise standing posture | 122.10 ± 2.23 | 100 | 140 |
| During peak exercise | 155,23 ± 20.59 | 110 | 180 | |
| Change in systolic blood pressure per MEC | 4,84 ± 2.72 | |||
| Diastolic blood pressure (mmHg) | Pre-exercise standing posture | 72.50 ± 1.02 | 60 | 90 |
| During peak exercise | 88,10 ± 9.11 | 70 | 110 | |
| Change in diastolic blood pressure per MEC | 2,4 ± 1.75 | |||
Al-Mallah MH et al17 reported an average HR max of 151 ± 28 beats/minute. Ahmed MH et al11 found an average HR max of 154 ± 15 BPM. Sydo N (2014)21 reported HR max of 166 ± 17 BPM in males and 163 ± 14 BPM in females.
The study suggests that the HR max obtained in their research is similar to findings in patients with CI < 0.8 from other studies and lower than results from studies on healthy patients or those with CI ≥ 0.8. The authors attribute this to the high number of patients in their study who did not reach their target heart rate (45%) and a lower average CI (0.64 ± 0.25) (Table 2).
Maximum Workload Blood Pressure (MWBP)
The average maximum workload systolic blood pressure (MWBP) in the study was 155.23 ± 20.59 mmHg (Table 2), which is significantly lower than values reported in studies by Sydo N et al21 reported (males: 184 ± 24 mmHg for men and 168 ± 24 mmHg for females), and Ahmed HM et al11 reported 180 ± 25 mmHg for a group with CI ≥ 0.8 and 174 ± 33 mmHg for a group with CI < 0.8. The average increase in systolic blood pressure (SBP) during exercise (4.84 ± 2.72 mmHg/MET) was also lower than reference values reported in literature (10 mmHg/MET).19 The passage concludes that the lower MWBP and lower blood pressure increase in their study may be due to the high proportion (53.3%) of patients who did not reach their target heart rate and had a lower CI.
The average value of maximum exercise diastolic blood pressure (DBP) was 88.10 ± 9.11 mmHg, which is quite consistent with findings from Ahmed HM et al (CI ≥ 0.8: 85 ± 11 mmHg, CI < 0.8: 86 ± 16 mmHg).11 The study of Sydo N et al21 found an average maximum exercise diastolic blood pressure of 78.0 ± 16.0 mmHg in males and 75.0 ± 16 mmHg in females. The average increase in DBP during exercise (2.40 ± 1.75 mmHg/MET) is consistent with the literature (reference values): during exercise, diastolic blood pressure often increases slightly or remains the same, or decreases due to peripheral vasodilation.19
Heart Rate During Recovery
The results of Table 2 show that the heart rate decreased by 27.87 ± 16.82 beats/minute in the first minute in our study, and only 7 patients (11.6%) had a heart rate decrease of less than 12 beats/minute in the first minute during recovery. The results of many other studies around the world agree that a heart rate decrease of less than 12 beats/minute in the first minute of recovery is abnormal.19,22,23 The increase in heart rate during exercise is mainly due to increased sympathetic nervous system tone. Recovery of heart rate after exercise is related to reactivation of the parasympathetic nervous system. Reduced parasympathetic nervous system activity is closely related to increased overall mortality.16 In this study, we found that the majority of most patients had abnormalities in increased heart rate during exercise period. However, there was no abnormal heart rate decrease during the recovery period (abnormal parasympathetic nervous system activity). This discrepancy may be explained by the fact that the study had a high proportion of patients with sinus node dysfunction (19 cases, 31.7%) who had abnormal heart rate changes during exercise, mainly related to the mechanism of sinus node dysfunction due to other causes without abnormalities of the parasympathetic nervous system.
Relationship Between Achieving These Indices on Electrocardiography Exercise Testing and the Possibility of Permanent Pacemaker Implantation in Patients with Sinus Node Bradycardia
A frequently asked clinical question of great importance that we are interested in here is what factors are related to the need for pacemaker implantation in patients with sinus node bradycardia, and whether it is possible to predict the need for pacemaker implantation based on the results of maximal exercise testing? The results of the single-variable and multivariable (Table 3) regression analysis above answered this question.
Table 3.
Multivariable Logistic Regression to Assess the Relationship Between Achieving Target Indicators and Permanent Pacemaker Implantation
| Predictive Variables | B Coefficient | OR | 95% CI | P |
|---|---|---|---|---|
| Heart rate variability index < 0.8 | 3.069 | 21.521 | 2.27–04.34 | 0.008 |
| Not achieving 85% of predicted maximum exercise capacity | 1.762 | 5.826 | 0.92–37.04 | 0.062 |
| Constant | −3.882 | 0.021 | 0.001 |
Note: Bold value indicates significance, P<0.01.
In our study, the indication for pacemaker implantation was mainly based on the results of Holter electrocardiography (14 patients had sinus node dysfunction, 5 patients had 2:1 atrioventricular block, and 1 patient with Mobitz type II second-degree atrioventricular block). Electrophysiological examination helped to identify 5 patients with 2:1 atrioventricular block with inducible retrograde conduction the atrioventricular node ablation for additional pacing indications in patients, especially those who do not show signs of sinus node dysfunction and conduction disorders on 24-hour Holter electrocardiography pacing (our study has 1 patient with severe sinus node dysfunction which was found on electrophysiological examination, 2 patients had CI < 0.8 during exercise testing).24,25
Through single-variable logistic regression analysis, it was shown that there were two factors related to the possibility of pacemaker implantation in the bradycardic sinus node group: inability to achieve chronotropic competence (CI < 0.8) and failure to achieve 85% of predicted maximum exercise capacity.
Through multivariable regression analysis (Table 3), only the chronotropic competence index below 0.8 had an OR = 21.521 (95% CI: 2.27–204.34) with p < 0.01, which was an independent predictor for the possibility of permanent pacemaker implantation in patients with sinus bradycardia.
Thus, it can be seen that CI < 0.8 is an important marker for physicians to decide on pacemaker implantation for patients, and it has been recommended by the ACC/AHA/HRS in 2018 for sinus node dysfunction and conduction disorders with a Class IIa recommendation. (The text reference recommendations from the 2018 ACC/AHA/HRS guidelines on bradycardia and conduction disorders which state that CI less than 0.8 is a Class IIa recommendation for pacemaker implantation). This means there is strong evidence to support pacemaker implantation in this case.
The decision to implant a pacemaker in patients with sinus node dysfunction depends on many factors, including the patient’s symptoms.26,27 Syncope is the most specific symptom, but not all patients with syncope can immediately be diagnosed with electrocardiography. Holter electrocardiography may not detect anything in many cases because symptoms can occur at unpredictable times. In such cases, exercise testing with inability to achieve chronotropic competence, along with symptoms during exercise, is an indication for PPI (in our study); There were 2 patients (3.3%) with SND combined with intermittent claudication conduction disorders, two cases with a male-49 year old and a female-54 year old of claudication Mobitz type I Second-degree atrioventricular block with symptoms of syncope, and these two cases were received DDDR 2-chamber permanent pacemakers according to this indication and both showed good improvement in symptoms after the procedure.
Many studies have shown that pacemakers with frequency responsive function are indicated to increase heart rate, improve exercise capacity, and reduce recurrent rhythm disturbances during exercise in patients with chronotropic incompetence.28 The ability to exercise is an important factor in a patient’s quality of life. In patients with bradycardia and atrioventricular block, ventricular pacing can improve exercise capacity. However, atrioventricular pacing is more physiological than ventricular pacing and may be more effective in improving exercise capacity.
In the study by Maity AK et al (1992),29 there was a significant improvement in exercise time (p < 0.001) and the maximum rate pressure product (p < 0.001) after pacemaker implantation in patients with sick sinus syndrome (SSS) and chronotropic incompetence. This study found that patients with VVIR pacing mode had a significantly lower maximum heart rate during exercise compared to patients with DDD and VVI pacing modes (p < 0.001). Exercise time was also shorter in patients with VVIR pacing mode compared to patients with DDI and DDD pacing modes (p < 0.05). However, there was still a statistically significant improvement in exercise capacity in patients with VVIR pacing mode compared to baseline (VVI or DDD mode).
Another study by Santini M et al (1997)30 evaluated the long-term benefits of DDIR pacing mode compared to DDI pacing mode in improving hemodynamics and preventing arrhythmias in patients with bradycardia and loss of chronotropic competence. The results showed that DDIR pacing mode improved exercise capacity, with maximum heart rate increasing from 96 ± 17 beats/minute to 115 ± 17 beats/minute (+20%, p < 0.0001), exercise time increasing from 7.0 ± 3.5 minutes to 8.8±4.3 minutes (+26%, p < 0.0001), VO2max increasing from 1238 ± 406 mL/minute to 1453 ± 423 mL/minute (+17%, p < 0.001), and VO2 at anaerobic threshold increasing from 977 ± 343 mL/minute to 1222 ± 415 mL/minute (+25%, p < 0.001). These benefits remained unchanged throughout a one-year follow-up period. In terms of antiarrhythmic effects, there was a statistically significant reduction in the recurrence of paroxysmal atrial fibrillation after 6 months in all patients in the study. However, after one year, there was no significant difference between the DDI and DDIR pacing modes.
Another study by Occhetta E et al (1997)31 compared the exercise response during aerobic and anaerobic phases in three pacing modes: DDD, VVIR, and DDDR in patients with loss of chronotropic competence. The results showed that DDDR pacing mode was better than VVIR and DDD pacing modes. Maximum heart rate during exercise was significantly higher in VVIR pacing mode (131 ± 21 beats/minute) and DDDR pacing mode (136 ± 14 beats/minute) compared to DDD pacing mode (105 ± 21 beats/minute) (p < 0.05). In DDDR pacing mode, exercise time (652 ± 161 seconds) and maximum oxygen consumption (22.7 ± 7.1 mL.kg-1 minute-1) were higher than in DDD pacing mode (565 ± 106 seconds and 20.1 ± 6.5 mL.kg-1 minute-1) and VVIR pacing mode (599 ± 155 seconds; 18.8 ± 6.5 mL.kg-1 minute-1) (p < 0.05). In addition, exercise time and oxygen consumption at anaerobic threshold were better in DDDR pacing mode (350 ± 119 seconds; 14.2 ± 4.9 mL.kg-1 minute-1) compared to DDD pacing mode (280 ± 101 seconds; 12.2 ± 4.6 mL.kg-1 minute-1) and VVIR pacing mode (306 ± 122 seconds; 11.6 ± 4.60 mL.kg minute-1) (p < 0.05). In conclusion, the article suggests that DDDR pacing mode is more effective (improving exercise capacity) than VVIR and DDD pacing modes in patients with sinus node dysfunction and loss of chronotropic competence. However, more research is needed to confirm these findings.
Overall, the content as above discusses three studies that compared the effectiveness of different pacemaker modes in improving exercise capacity and reducing symptoms in patients with heart failure.29–31 The first study found that VVIR pacing was more effective than DDD or VVI pacing in improving exercise capacity in patients with complete heart block and no sinus node function. The second study found that DDIR pacing was more effective than DDI pacing in improving exercise capacity and reducing symptoms in patients with heart failure and chronotropic incompetence. The third study found that DDDR pacing was more effective than VVIR or DDD pacing in improving exercise capacity in patients with heart failure and chronotropic incompetence.
Conclusion
Maximum exercise capacity in patients with sinus node bradycardia is low and only reaches 7.78 ± 3.59 METs; Not reaching 85% of predicted maximum exercise capacity accounts for 53.5%; Maximum exercise time is 10.53 ± 0.46 minutes; Impaired heart rate variability in patients with sinus node bradycardia is high: CI < 0.8 accounts for 53.5%, not reaching 85% of predicted HR max accounts for 45%.
Therefore, exercise electrocardiography in patients with sinus node bradycardia is a potential prognostic factor for the need for permanent pacemaker implantation. It is recommended that further prospective studies be conducted to evaluate the use of heart rate variability index in predicting the need for permanent pacemaker implantation for patients suspected of having sinus node dysfunction and conduction disorders.
Limitation and Recommendations
It is a medical research in Vietnam about the use of the heart rate variability to predict the need for permanent pacemaker implantation in patients with suspected sinus node dysfunction and conduction disorders. This study also recommends that further prospective studies be conducted to evaluate the use of heart rate variability index in predicting the need for permanent pacemaker implantation for patients suspected of having sinus node dysfunction and conduction disorders.
Acknowledgment
The authors are grateful to the Hanoi Medical University and were implemented with the permission of the Vietnam Heart Institute – Bach Mai Hospital and Hanoi Heart Hospital for their approval and their assistance in date collect.
Funding Statement
There is no funding to report.
Abbreviations
ECG, Electrocardiographic; SB, sinus bradycardia; SND, sinus node dysfunction; PPI, permanent pacemaker implantation; MEC, Maximum exercise capacity; MET, Metabolic equivalent of task; HRVI, Heart rate variability index (Chronotropic index); CI: Chronotropic index; HRV, Heart rate variability; HR, Heart rate; HRRI, Heart rate recovery index; CI, Confidence Interval; OR: Odds ratio; ACC/AHA/HRS, the American College of Cardiology/American Heart Association/Heart Rhythm Society; ESC, The European Society of Cardiology; SPSS, Statistical Product and Services Solution; BPM, Beats per minute; MWBP, Maximum workload blood pressure; DBP, Diastolic blood pressure; SBP, Systolic blood pressure; VVI, Single chamber ventricular inhibited; VVIR, Single chamber; DDD, Dual-chamber demand pacing; DDDR, Dual-chamber rate-modulated; DDI, Dual-chamber; DDIR, Dual chamber rate responsive; VO2, the O2 uptake value; P: Prevalence.
Date Sharing Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Ethical Statement
The authors confirmed that the guidelines in the Declaration of Helsinki were followed. Informed consent was obtained from each participant. This study was conducted after the research outline and protocol is approved by the Scientific Council of Hanoi Medical University and was implemented with the permission of the Vietnam Heart Institute – Bach Mai Hospital and Hanoi Heart Hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kusumoto FM, Schoenfeld MH, Barrett C. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay. Circulation. 2019;140(8):e382–e482. doi: 10.1161/CIR.0000000000000628 [DOI] [PubMed] [Google Scholar]
- 2.Jensen PN, Gronroos NN, Chen LY, et al. Incidence of and risk factors for sick sinus syndrome in the general population. J Am Coll Cardiol. 2014;64(6):531–538. doi: 10.1016/j.jacc.2014.03.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaw DB, Holman RR, Gowers JI. Survival in sinoatrial disorder (sick-sinus syndrome). Br Med J. 1980;280(6208):139–141. doi: 10.1136/bmj.280.6208.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lien W-P, Lee Y-S, Chang F-Z, Lee S-Y, Chen C-M, Tsai H-C. The natural history of sick sinus syndrome. Chest. 1977;72(5):628–634. doi: 10.1378/chest.72.5.628 [DOI] [PubMed] [Google Scholar]
- 5.Friedberg CK, Donoso E, Stein WG. Nonsurgical acquired heart block. Ann. N.Y. Acad. Sci. 1963;111(3):835–847. doi: 10.1111/j.1749-6632.1964.tb53151.x [DOI] [PubMed] [Google Scholar]
- 6.Edhag O, Swahn A. Prognosis of patients with complete heart block or arrhythmic syncope who were not treated with artificial pacemakers. A long-term follow-up study of 101 patients. Acta Med Scand. 1976;200(6):457–463. doi: 10.1111/j.0954-6820.1976.tb08264.x [DOI] [PubMed] [Google Scholar]
- 7.Kim ESH, Ishwaran H, Blackstone E, Lauer MS. External prognostic validations and comparisons of age- and gender-adjusted exercise capacity predictions. J Am Coll Cardiol. 2007;50(19):1867–1875. doi: 10.1016/j.jacc.2007.08.003 [DOI] [PubMed] [Google Scholar]
- 8.Fletcher GF, Ades PA, Kligfield P, et al. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128(8):873–934. doi: 10.1161/CIR.0b013e31829b5b44 [DOI] [PubMed] [Google Scholar]
- 9.Glikson M, Nielsen JC, Kronborg MB. 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: developed by the task force on cardiac pacing and cardiac resynchronization therapy of the European Society of Cardiology (ESC) With the special contribution of the European Heart Rhythm Association (EHRA). Eur Heart J. 2021;42(35):3427–3520. doi: 10.1093/eurheartj/ehab364 [DOI] [PubMed] [Google Scholar]
- 10.Lauer MS, Francis GS, Okin PM, et al. Impaired chronotropic response to exercise stress testing as a predictor of mortality. JAMA. 1999;281(6):524–529. doi: 10.1001/jama.281.6.524 [DOI] [PubMed] [Google Scholar]
- 11.Ahmed HM, Al-Mallah MH, Keteyian Steven J, et al. Sex-specific maximum predicted heart rate and its prognosis for mortality and myocardial infarction. Med Sci Sports Exercise. 2017;49(8):1704–1710. doi: 10.1249/MSS.0000000000001285 [DOI] [PubMed] [Google Scholar]
- 12.Kodama S, Saito K, Allison TG, Kopecky SL. Cardiopulmonary fitness and heart rate recovery as predictors of mortality in a referral population. J Am Heart Assoc. 2014;3(2):e000559. doi: 10.1161/JAHA.113.000559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chu Dung S, Tran Van D. Clinical characteristics and arrhythmias in patients with sinus bradycardia recorded on 24-hour Holter electrocardiography in Vietnamese people. Vietnam J Physiol. 2016;20:9–16. [Google Scholar]
- 14.Semelka M, Gera J, Usman S. Sick sinus syndrome: a review. Am Fam Physician. 2013;87(10):691–696. [PubMed] [Google Scholar]
- 15.Hiss RG, Lamb LE. Electrocardiographic findings in 122,043 individuals. Circulation. 1962;25(6):947–961. doi: 10.1161/01.CIR.25.6.947 [DOI] [PubMed] [Google Scholar]
- 16.John E, Michael E. Guyton and hall textbook of medical physiology; Copyright©2021 by Elsevier, Inc; 2020. P40–P74. Available from: http://evolve.elsevier.com/Hall/Physiology. Accessed July 15, 2024. [Google Scholar]
- 17.Mouaz H, Steven J, Clinton A, et al. Rationale and Design of the Henry Ford ExercIse Testing Project (The FIT Project). Clin Cardiol. 2014;37(8):456–461. doi: 10.1002/clc.22302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kieu NTV, Jung S-J, Shin S-W. The Validity of the YMCA 3-minute step test for estimating maximal oxygen uptake in healthy Korean and Vietnamese adults. J Lifestyle Med. 2020;10(1):21–29. doi: 10.15280/jlm.2020.10.1.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA Guidelines for exercise testing. a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on Exercise Testing). J Am Coll Cardiol. 2013;30(1):260–311. [DOI] [PubMed] [Google Scholar]
- 20.Gulati M, Shaw LJ, Thisted RA, et al. Heart rate response to exercise stress testing in asymptomatic women: the St. James women take heart project. Circulation. 2010;122(2):130–137. doi: 10.1161/CIRCULATIONAHA.110.939249 [DOI] [PubMed] [Google Scholar]
- 21.Sydo N, Abdelmoneim SS, Mulvagh SL, et al. Relationship between exercise heart rate and age in men vs women. Mayo Clin Proc. 2014;89(12):1664–1672. doi: 10.1016/j.mayocp.2014.08.018 [DOI] [PubMed] [Google Scholar]
- 22.Nishime EO, Cole CR, Blackstone EH, et al. Heart rate recovery and treadmill exercise score as predictors of mortality in patients referred for exercise ECG. Ital Heart J Suppl. 2001;2(2):200–202. [DOI] [PubMed] [Google Scholar]
- 23.Cole CR, Blackstone EH, Pashkow FJ, et al. Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med. 1999;341(18):1351–1357. doi: 10.1056/NEJM199910283411804 [DOI] [PubMed] [Google Scholar]
- 24.Reiffel JA, Bigger JT, Cramer M, et al. Ability of Holter electrocardiographic recording and atrial stimulation to detect sinus nodal dysfunction in symptomatic and asymptomatic patients with sinus bradycardia. Am J Cardiol. 1977;40(2):189–194. doi: 10.1016/0002-9149(77)90007-8 [DOI] [PubMed] [Google Scholar]
- 25.Lipski J, Cohen L, Espinoza J, et al. Value of Holter monitoring in assessing cardiac arrhythmias in symptomatic patients. Am J Cardiol. 1976;37(1):102–107. doi: 10.1016/0002-9149(76)90507-5 [DOI] [PubMed] [Google Scholar]
- 26.Sridhar S, Benchimol A, Desser KB. Clinical spectrum of the sick sinus syndrome. Ariz Med. 1977;34(2):82–84. [PubMed] [Google Scholar]
- 27.Udo EO, Zuithoff NPA, van Hemel NM. Incidence and predictors of short- and long-term complications in pacemaker therapy: the FOLLOWPACE study. Heart Rhythm. 2012;9(5):728–735. doi: 10.1016/j.hrthm.2011.12.014 [DOI] [PubMed] [Google Scholar]
- 28.Erik OU, Hemel V, Norbert M, et al. Long term quality of life in patients with bradycardia pacemaker implantation. Int J Cardiol. 2013;1968(3):2159–2163. [DOI] [PubMed] [Google Scholar]
- 29.Maity AK, Ghosh SP, Dasbiswas A, et al. Haemodynamic advantage with single chamber rate responsive pacemakers over dual chamber pacemakers during exercise in chronotropic incompetence. Indian Heart J. 1992;44(4):231–234. [PubMed] [Google Scholar]
- 30.Santini M, Ricci R, Puglisi A, et al. Long-term haemodynamic and antiarrhythmic benefits of DDIR versus DDI pacing mode in sick sinus syndrome and chronotropic incompetence. G Ital Cardiol. 1997;27(9):892–900. [PubMed] [Google Scholar]
- 31.Occhetta E, Perucca A, Fazzari M, et al. [An intrapatient comparison of adaptation to aerobic and anaerobic exertion during 3 types of physiological cardiac stimulation in chronotropic failure of the sinus node: DDD, VVIR and DDDR]. Cardiologia. 1997;42(1):51–57. Italian. [PubMed] [Google Scholar]