Abstract
Background/Objectives: The purpose of this systematic review was to assess the global prevalence of sleep bruxism and awake bruxism in pediatric and adult populations. Methods: This systematic review was conducted by analyzing studies published from 2003 to 2023. The following keyword combination was utilized: prevalence, epidemiology, population, and bruxism. The PubMed database was analyzed, supplemented by manual searches using the Google search. Additionally, the snowballing procedure method was applied. A double assessment of the quality of publications was carried out to preserve the highest possible quality of evidence (e.g., Joanna Briggs Institute critical appraisal checklist). Analyses were conducted using the R statistical language. Results: The global bruxism (sleep and awake) prevalence is 22.22%. The global sleep bruxism prevalence is 21% and awake prevalence is 23%. The occurrence of sleep bruxism, based on polysomnography, was estimated at 43%. The highest prevalence of sleep bruxism was observed in North America at 31%, followed by South America at 23%, Europe at 21%, and Asia at 19%. The prevalence of awake bruxism was highest in South America at 30%, followed by Asia at 25% and Europe at 18%. Conclusions: One in four individuals may experience awake bruxism. Bruxism is a significant factor among women. It was observed that age is a significant factor for the occurrence of sleep bruxism in women. Among the limitations of the study is the lack of analysis of the prevalence of bruxism in Africa and Australia due to not collecting an adequate sample for analysis. The study was registered in the Open Science Framework (10.17605/OSF.IO/ZE786).
Keywords: prevalence, epidemiology, population, nocturnal bruxism, wakefulness bruxism, Europe, Asia, America, Africa, Australia
1. Introduction
The term “bruxism” was introduced by Frohman in 1931 [1]. However, earlier attempts to name the reflex of teeth grinding were made by Pietkiewicz (1907), who described it as “la bruxomanie” [2]. Yet, these dates are not the beginnings of research into the reflex of teeth grinding. The first mentions of this habit appeared in scientific literature in 1860 [3], and descriptions of teeth grinding are present in the Psalms of David, dated before our era [4].
Early observations of patients with bruxism emphasized that it is an unconscious habit (1940, Boyens) and that it affects a significant percentage of the population across various age groups (1957, Nadler) [5,6]. Throughout the 20th and 21st centuries, with rapid developments in dental research, bruxism began to be differentiated [7,8]. Miller, in 1950, proposed distinguishing between daytime and nighttime bruxism [9], and in 1983, a distinction was made between eccentric and centric bruxism [4,10]. In the context of limiting tooth wear, Okeson in 1987 proposed the use of occlusal splints [11]. In 2013, Lobbezoo et al. in a consensus on the definition and classification of bruxism emphasized its two manifestations: during sleep and during wakefulness [12].
Over the years, bruxism was described as a parafunction associated with multifactorial etiology, but primarily with a psychological factor. Therefore, a groundbreaking study was Every’s work in 1960, in which he proposed an evolutionary explanation for bruxism, suggesting that teeth grinding is associated with sharpening teeth to use them as tools or weapons [13]. In 1996, a study by Lavigne et al. opened the era of polysomnographic diagnosis research for bruxism. In the diagnostic context of the 21st century, two tools were published that will undoubtedly influence further research in terms of the described phenomenon [14]. This includes the “BruxApp” smartphone app presented in 2015, allowing for self-reporting of bruxism during the day, created by Bracci et al. [15,16], and the “BruxScreen” tool, created in 2023 [17]. It consists of a questionnaire part filled out by the examinee and a clinical assessment form filled out by the specialist [17].
In terms of key works concerning the etiology of bruxism, a study published in 2001 by Lobbezoo and Naeije is significant [18]. The researchers stated that certain neurotransmitters in the central nervous system might influence the modulation of bruxism [18]. In 2018, a team led by Lobbezoo et al. revised the 2013 consensus [19]. In their work, they revised the definitions of bruxism: “(i) sleep and awake bruxism are masticatory muscle activities that occur during sleep (characterised as rhythmic or non-rhythmic) and wakefulness (characterised by repetitive or sustained tooth contact and/or by bracing or thrusting of the mandible), respectively”; and, among other things, noted that in healthy individuals, bruxism should not be considered a disorder: “(ii) in otherwise healthy individuals, bruxism should not be considered as a disorder, but rather as a behaviour that can be a risk (and/or protective) factor for certain clinical consequences” [19].
The etiology of bruxism is multifactorial and is not fully understood [18,20,21], which is why it garners significant interest from researchers. As described in the historical overview above, the etiology of bruxism was linked to various factors. Every suggested it is related to teeth sharpening [13]. Other suggestions include that the alternating movement is related to maintaining airway patency during sleep [12,22,23]. Bracha indicates that clenching teeth during moments of stress increases blood flow to the frontal lobe, which potentially helps in the fight or flight response [24,25]. Manfredini et al. (2020) suggest that the etiology of bruxism is mainly related to central factors, not peripheral [26]. Giovanni and Giorgia in their work note that bruxism stimulates the nuclei of the ascending reticular activating system. The authors suggest that bruxism activates the production of neurotransmitters that stimulate the brain cortex and protect against neurodegenerative diseases such as dementia [27]. The current division of factors causing bruxism includes primary—idiopathic and secondary—radiogenic (occurrence of diseases and use of specific pharmacology) [20].
Due to the multifactorial etiology of the described condition, there are multiple diagnostic possibilities for bruxism. According to Lobbezoo et al., bruxism assessments can employ both non-instrumental approaches (notably self-report) and instrumental approaches (notably electromyography) [19]. During a non-instrumental examination, the patient or their family may report teeth grinding or strange tooth grinding sounds. Clinical examination may reveal increased tooth wear, jaw muscle pain or fatigue, and muscle hypertrophy [12,28]. In addition to the tools described in earlier paragraphs, “BruxApp” and “BruxScreen”, the “BruxChecker” was introduced in 2006 [29]. This is a simple device that patients use at night to visualize patterns of teeth grinding by marking areas where teeth contact occurs [29]. Questions regarding the occurrence of bruxism can also be found in other questionnaires, such as the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) [30], Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) [31], The Oral Behavior Checklist [32], and the Pittsburgh Sleep Quality Index [33].
In diagnostics, tooth wear was identified as one of the signs of bruxism. It is also one of the main negative consequences of the condition [34].The association of bruxism with temporomandibular disorders (TMDs) and headaches, as well as cervical spine dysfunctions, remains debatable [35,36]. Castrillon and Exposto note that, in light of available scientific evidence, it is doubtful that bruxism is a direct cause of pain [35]. Piekartz et al. emphasize that clinicians should focus on improving orofacial function and the mechanical sensitivity of tissues [36]. Certainly, for individuals without a distinct pathology, bruxism should be reframed not as inherently pathological, but rather as a muscular activity with various potential causes. This behavior can range from detrimental to benign, or even serve a protective function in relation to specific health factors [19,26,37]. In children, the occurrence of sleep bruxism diminishes gradually as they age. Following the natural course, the preferred approach involves observational and non-interventional strategies unless it indicates underlying primary conditions requiring treatment [26].
When treatment for bruxism is needed, the following therapies are applied. Based on the relationship between bruxism and emotional stress, psychological therapies such as cognitive behavioral therapy are used in treatment [38]. Physiotherapy and acupuncture, which have a relaxing effect on overly active muscles, are also employed [39,40]. To protect teeth from damage, occlusal splint therapy is recommended [41]. Biofeedback therapy, based on the premise that individuals with bruxism can unlearn their behavior and attempt to control it, is also utilized [42]. Visual, auditory, vibratory, or gustatory stimuli are used in biofeedback therapy [39]. Pharmacotherapy is also employed, including substances such as botulinum toxin, clonazepam, and clonidine [41,43]. Sleep hygiene is recommended as well, including avoiding stimulants at night (such as coffee, tobacco, and alcohol), limiting physical activity and mental stimulation before sleep [41].
Over the past five years, three meta-analyses regarding the occurrence of bruxism were conducted. Archer et al. conducted a meta-analysis on the prevalence of awake bruxism in the adult population, observing a prevalence rate of 15.44% [44]. Soares et al. conducted a meta-analysis on children with sleep bruxism in the global population, showing a prevalence rate of 31.16% [45]. The meta-analysis by Ferrari-Piloni et al. investigated the occurrence of bruxism in children residing in Brazil, revealing a prevalence of 25.8% in both sleep and awake states. Additionally, Ferrari-Piloni et al. observed regional differences in Brazil: Northeast—35.2%, Southeast—45.0%, and South—19.8% [46].
The meta-analysis by Ferrari-Piloni et al. [46] provided grounds to suggest that bruxism is associated with geographic factors. Additionally, contributing to the debate on the association between TMDs and bruxism, Mortazavi et al. conducted a meta-analysis aiming to examine and quantitatively determine the relationship between bruxism and temporomandibular joint disorders (TMDs). They demonstrated a positive association between bruxism and TMDs, highlighting that the presence of bruxism increases the likelihood of developing TMDs in the future [47]. Furthermore, a recent meta-analysis (2024) published by Zieliński et al. revealed that the occurrence of TMDs varies by continent (South America—47% compared to Asia—33% and Europe—29%, and North America—26%) [48]. Based on the aforementioned information, the authors decided to conduct a meta-analysis with the purpose of assessing the global prevalence of sleep bruxism and awake bruxism in pediatric and adult populations. According to the authors’ best knowledge, such a study was not conducted previously.
Four primary research questions were posed:
What is the global prevalence of sleep and awake bruxism in the population?
What is the global prevalence of sleep and awake bruxism in the population depending on the continent?
What is the global prevalence of sleep bruxism in the population depending on the continent, divided by age and gender?
What is the global prevalence of awake bruxism in the population depending on the continent, divided by age and gender?
The secondary research question was described during the registration of the protocol [49].
2. Materials and Methods
This systematic review is following the Preferred Reporting Items for Systematic reviews and Meta-Analyses [50] (PRISMA 2020 guidelines [51]) (Supplementary Material S1 and S2). The systematic review protocol was registered in the Open Science Framework (OSF) under the number identifier: DOI 10.17605/OSF.IO/ZE786 [49]. This systematic review and meta-analysis was conducted by analyzing studies published from 1 January 2003, to 31 December 2023. This was a 20-year timeframe, chosen based on earlier works [52,53,54].
2.1. The Data Collection Process
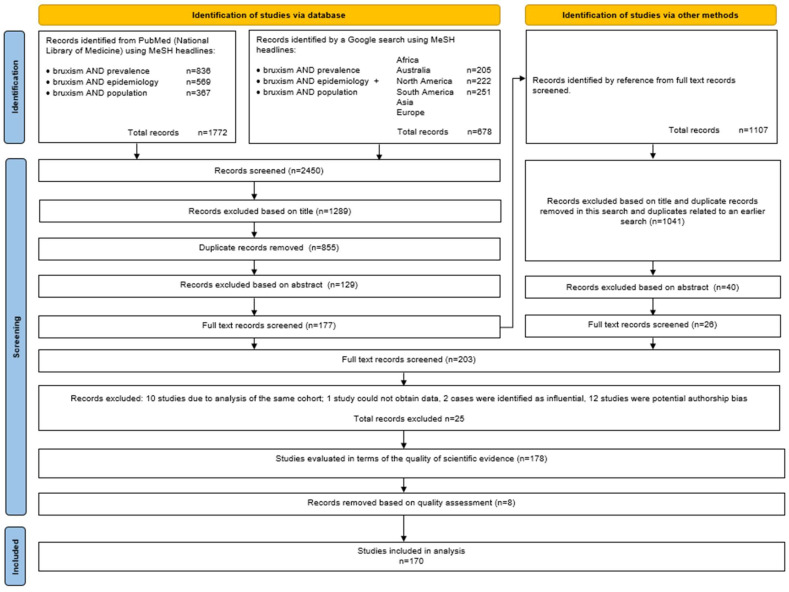
An analysis of the PubMed database (National Library of Medicine) was conducted from 22 March 2024 [49] to 22 June 2024, using keywords consistent with the MeSH (Medical Subject Headings) database. Building upon the previous reviews [48,55], the following keyword combination was utilized: bruxism AND prevalence, bruxism AND epidemiology, and bruxism AND population. Based on earlier work, it was decided to analyze only the PubMed database [48,55,56,57,58], supplemented by manual searches using the Google search engine with keyword combinations including the names of continents. Additionally, the snowballing procedure method was applied according to Wohlin’s recommendations [59] (Figure 1). From each study qualified for full-text assessment, bibliographies were recorded and searched for literature supplementation. This systematic review was carried out by two independent reviewers (G.Z. and A.P.) who first evaluated the titles of the papers, then the abstracts, and finally the full papers. All disputes were assessed by M.W.
Figure 1.
PRISMA flow diagram.
From each study, the following structured information was collected (information gathering methods were adapted from the work [45]): DOI number, PMID or other numerical identifier of the study, last author’s surname, publication year, country, sample size, number of women and number of men, age of participants, percentage and number of individuals with bruxism (sleep and awake bruxism or both), diagnostic methods used, information about the approval of the research ethics committee for the study, and the presence or absence of conflicts of interest.
The summary of the PICO standards (P—population, I—intervention, C—comparison, and O—outcome) [60], is found in Table 1.
Table 1.
PICO Summary of Inclusion and Exclusion Criteria.
| Inclusion | Exclusion | |
|---|---|---|
| Population | ||
|
|
|
| Intervention | ||
|
||
| Comparison | ||
|
||
| Outcome | ||
|
|
|
| Study Design | ||
|
|
2.2. Evaluation of the Quality of Scientific Evidence
After qualifying 180 papers, it was decided to analyze the quality of the publications. A double assessment of the quality of publications was carried out to preserve the highest possible quality of evidence. In the first step, publications identified as doubtful were screened based on an adapted questionnaire created by Berger et al. [61]. Based on this questionnaire, the first selection was carried out. Publications after this stage were evaluated with a standard tool. The second step involved a standard assessment using the Joanna Briggs Institute (JBI) critical appraisal checklist [62]. The assessment was conducted similarly to the process of searching by two independent researchers (G.Z. and A.P.) in agreement with a third (M.W.).
This was accomplished using an adapted questionnaire utilized by Berger et al. [61]. The questionnaire was expanded with questions related to the tools proposed by Giannakopoulos et al. [63] and Stang et al. [64]. The complete questionnaire is available (Supplementary Material S3). It contains 7 questions, with the first Q1–Q4 pertaining to the research methodology (obtaining ethical approval, description of the study group, inclusion and exclusion criteria). Questions Q5 and Q6 relate to the study of bruxism (analysis of group size and tools used for bruxism assessment). The final question, Q7, addresses potential conflicts of interest. The acceptance threshold for the study was set at 9 points. This is because even the maximum score for questions Q1–Q4 and Q7 yields a value of 8 points. The study must gain additional points for significant sample size in question Q5 (over 100 individuals [61]) or for a more reliable diagnostic value of bruxism in Q6 [20,61,65]; the assessment results of the papers are provided (Supplementary Material S4).
The works [66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226,227,228,229,230] were included in the meta-analysis, and the details can be found in Supplementary Material S5.
At this stage, it was noted that only one study concerning Australia [231] and three studies concerning Africa [232,233,234] were qualified. However, the collected sample did not allow for the analysis of the prevalence of bruxism across continents. Nevertheless, the samples were included in the analysis of the global occurrence of bruxism. Works rejected during the analysis of full texts [15,187,235,236,237,238,239,240,241,242,243,244,245,246,247,248,249,250,251,252,253,254,255,256,257,258,259,260,261,262,263,264,265] and based on the above analysis, along with the justification, are included in Supplementary Material S6, (Figure 1).
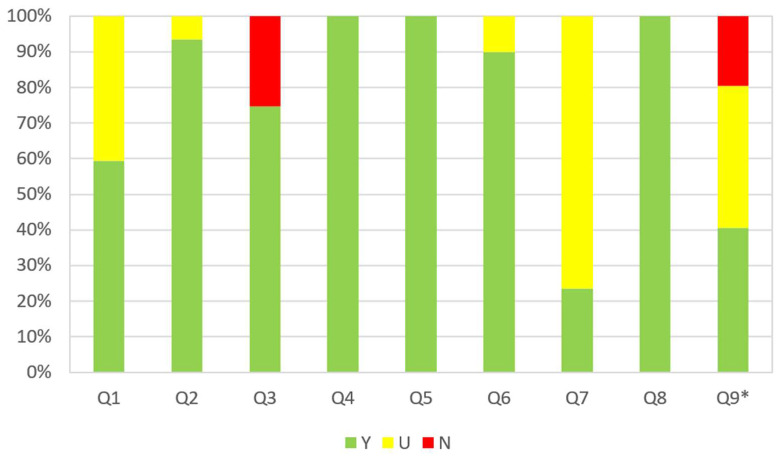
Qualified works were evaluated according to JBI. The assessment tool was provided by the JBI for analyzing analytical cross-sectional, case-control, and longitudinal studies. This tool was previously used in conducted meta-analyses regarding bruxism [44,45]. The JBI critical appraisal checklist consists of 9 questions, to which responses can be Yes (Y), No (N), Unclear (U), or marked as Not Applicable (N/A). The assessment guidelines were adopted according to the work of Munn et al. [266], and adaptations of the questions were made on the basis of previously published works [44,45] (Supplementary Material S7). The full list of questions and the assessment of the studies can be found in Supplementary Material S8. The results are presented graphically in Figure 2.
Figure 2.
The summary results of the evaluation of studies using a Joanna Briggs classification. Q1—Was the sample frame appropriate to address the target population?; Q2—Were study participants recruited in an appropriate way?; Q3—Was the sample size adequate?; Q4—Were the study subjects and setting described in detail?; Q5—Was data analysis conducted with sufficient coverage of the identified sample?; Q6—Were valid methods used for the identification of the condition?; Q7—Was the condition measured in a standard, reliable way for all participants?; Q8—Was there appropriate statistical analysis?; Q9—Was the response rate adequate, and if not, was the low response rate managed appropriately?; Y—yes; N—no; U—unclear; and *—the question did not apply to 37 studies.
Based on the analysis using the JBI questionnaire, the greatest risk associated with the studies analyzed is related to the adequate sample size (Q3) and the response rate (Q9). The most significant uncertainties were observed in question Q7. This was due to the fact that most studies were based on proprietary assessment questionnaires or self-reported surveys.
2.3. Synthesis Methods
The objective of this analysis was to estimate the prevalence of bruxism across the entire sample, with additional stratifications by age and continent, as well as by gender. This approach allows for a comprehensive assessment of demographic variations in bruxism occurrence.
In this meta-analysis, the threshold for statistical significance was established at α = 0.05. The distribution of categorical variables pertaining to the characteristics of the study samples was detailed by reporting frequencies and percentages for each category. The distribution of numerical variables was described using the median (Mdn) and interquartile range, specifically the first (Q1) and third (Q3) quartiles, as metrics of dispersion.
2.3.1. Pooling Effect Size Estimation
To estimate the pooled effect size, we employed the Generalized Linear Mixed-Effects Model (GLMM) with a binomial logit link. The GLMM integrates both fixed and random effects, and is particularly well-suited for meta-analyses, as it adeptly handles variations within and across a range of studies. Unlike the traditional inverse-variance method, the GLMM excels in managing heterogeneous datasets, ensuring a robust analysis of data involving diverse measurement scales such as counts and proportions [267,268].
The overall proportions were calculated employing the logit transformation, followed by back-transformation to the original scale. The selection of this transformation method was guided by specific characteristics of the dataset and the distribution of proportion values, with the assumption that there were no extreme values (i.e., very small or very large proportions). Confidence intervals for individual study results were estimated using the Agresti-Coull interval [269].
Heterogeneity among study results was quantified using the τ2, the square root of tau-squared (τ), and the I2 statistic [270]. The Higgins and Thompson’s H statistic was also calculated to measure the consistency of effect sizes across studies.
Variance components for τ2 were estimated using the maximum likelihood (ML) estimator, which facilitates an accurate estimation of between-study variance, which is critical given the substantial heterogeneity indicated by our data. The confidence intervals for the I2 and H statistics were estimated using methods based on the chi-squared distribution. The presence of heterogeneity was tested using both the Wald and the likelihood ratio test.
The evaluation of subgroup differences within the meta-analysis was performed using the Q-test for heterogeneity. The prediction interval for the prevalence of bruxism was estimated using the t-distribution.
The pooled effect of the studies was graphically depicted using a forest plot. This visualization method systematically represents the individual study results alongside their aggregated effect, facilitating a comprehensive overview of the data.
2.3.2. Leave-One-Out Diagnostics
We utilized several leave-one-out diagnostics, such as externally standardized residual, DFFITS value, Cook’s distance, covariance ratio, the leave-one-out amount of (residual) heterogeneity, the leave-one-out test statistic of the test for (residual) heterogeneity, and DFBETAS values [271,272,273,274,275,276].
A case may be considered to be ‘influential’ if at least one of the following is true:
If the absolute value of DFFITS exceeds , where p denotes the number of model coefficients and k the total number of cases. This threshold identifies cases that significantly affect the model’s predictions.
A case is considered influential if the lower tail probability of a chi-square distribution, calculated using the degrees of freedom defined by the Cook’s distance, exceeds 50%. This metric highlights cases that have a substantial impact on the parameter estimates across the model.
Influence is attributed to a case if its hat value surpasses . This measure quantifies the leverage of a case, indicating its relative ability to influence the fit of the model disproportionately.
A case is marked as influential if any of its DFBETAS values exceed 1.0. This condition reveals cases that, when excluded, lead to a significant change in the estimated regression coefficients, shifting them by more than one standard deviation.
2.3.3. Publication Bayes
To evaluate publication bias in the study, a funnel plot was utilized for graphical representation. The asymmetry in the funnel plot was quantitatively assessed using Egger’s test as the primary statistical approach. This method involves regressing the standardized effect estimates against their precision, in accordance with the established guidelines by Egger et al. [277]. The regression analysis uses the standard error of the estimates as a predictor, with each study’s impact on the analysis adjusted by weighting inversely to their variance.
2.3.4. Characteristics of the Statistical Tool
Analyses were conducted using the R Statistical language (version 4.3.1; R Core Team, 2023) on Windows 10 Pro 64 bit (build 19045), using the packages meta (version 6.5.0; [278]), dmetar (version 0.1.0; [279]), report (version 0.5.7; [280]), gtsummary (version 1.7.2; [281]), dplyr (version 1.1.3; [282]), and psych (version 2.3.9; [283]).
2.3.5. Characteristics of the Meta-Analysis Sample
The prevalence of bruxism was analyzed across 176 scientific studies (170 publications analyzed 176 populations). Six studies [110,128,156,189,191,198] analyzed more than one population/age group) with sample sizes varied from 30 to 99,416 (Mdn = 533.5, Q1 = 224.3, Q3 = 1097.3). Of these, 97 studies (55.11%) focused on adult populations (aged over 18 years), while the remaining 79 studies targeted minors (up to 18 years of age). Geographically, the studies were distributed as follows: 63 studies (36.63%) involved individuals in South America, 58 studies (33.72%) in Asia, 43 studies (25.00%) in Europe, and 12 studies (6.82%) in North America.
Additionally, the studies explored the incidence of bruxism with regard to two specific variables: gender and the time of occurrence, distinguishing between events during sleep and those occurring after waking.
3. Results
Due to the number of analyses, the full description of the results can be found in Supplementary Material S9. Forest plots and funnel plots are included in Supplementary Materials S10 and S11.
3.1. Meta-Analysis of Global Bruxism (Sleep and Awake) Prevalence
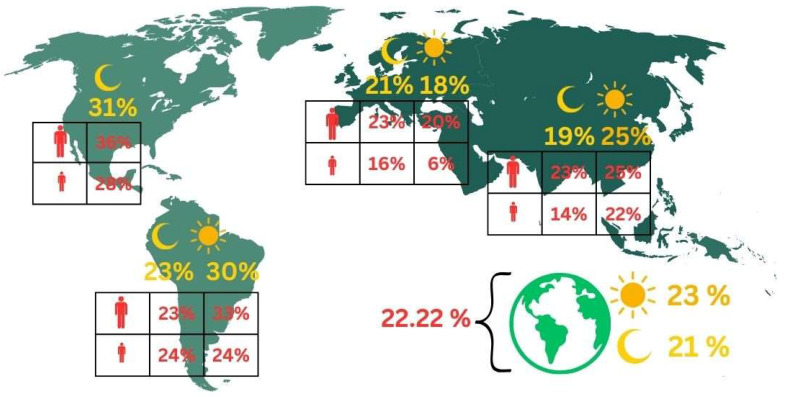
Using a random effects model, the pooled prevalence of bruxism was estimated at 22.22%, with a 95% confidence interval ranging from 19.59% to 25.11%. Additionally, a prediction interval was calculated, extending from 4.23% to 64.87%, indicating substantial variability in bruxism prevalence across different settings and populations (Figure 3).
Figure 3.
Graphical representation of the obtained results on the occurrence of bruxism in the population.
3.2. Meta-Analysis of Global Bruxism (Sleep and Awake) Prevalence across Continents
The subgroup analysis by continent in Table 2 revealed significant variability in the prevalence of bruxism, reflecting the diverse geographical patterns of this condition. North America exhibits the highest prevalence rate at 29.07%, with a notably broad 95% confidence interval ranging from 15.85% to 47.14%. This wide interval suggests a high degree of uncertainty or variability in the data, possibly due to fewer studies (only eight in total) contributing to this regional estimate, as indicated by the highest τ2 = 1.22, suggesting substantial heterogeneity among the studies.
Table 2.
Variability in bruxism (sleep and awake) prevalence: a subgroup analysis by continent.
| Continent | k | Proportion | CI 95% | τ2 | Q | I2 |
|---|---|---|---|---|---|---|
| Europe | 29 | 0.22 | 0.18–0.27 | 0.52 | 2023.04 | 98.6% |
| North America | 8 | 0.29 | 0.16–0.47 | 1.22 | 3041.78 | 99.8% |
| South America | 56 | 0.25 | 0.21–0.29 | 0.74 | 2580.68 | 97.9% |
| Asia | 43 | 0.19 | 0.15–0.24 | 1.03 | 12,177.51 | 99.7% |
k—number of studies; CI 95%—confidence interval 95%.
Europe and South America presented more moderate prevalence rates of 22.17% and 24.89%, respectively, with narrower confidence intervals, indicating more precise estimates. Europe’s studies, although more numerous (29 studies), still showed a high level of heterogeneity (I2 = 98.6%), which was slightly lower than that of South America, which had an I2 = 97.9%.
Asia, with 43 studies, reported the lowest prevalence of bruxism at 19.10%. However, it also presented a high level of heterogeneity (I2 = 99.7%), similar to North America, and a high τ2 = 1.03. This suggests that, despite having a larger number of studies, there is significant variation in the study results, which could be attributed to differences in study methodologies, populations, and diagnostic criteria across the continent.
The Q-statistics further support the presence of significant heterogeneity within each continent’s subgroup, with extremely high values observed, particularly in Asia (Q = 12,177.51). This reinforces the complexity and variability of bruxism prevalence across different geographical and cultural contexts.
3.3. Meta-Analysis of Global Sleep and Awake Bruxism Prevalence
3.3.1. Sleep Bruxism
The analysis, employing a random effects model, estimated the prevalence to show sleep bruxism of 20.99%, with a 95% confidence interval that stretches from 18.69% to 23.50%. This prevalence estimate highlights the notable incidence of sleep bruxism among the global population studied (Figure 3).
3.3.2. Sleep Bruxism as Assessed through Polysomnography
The present meta-analysis examines the global prevalence of sleep bruxism as assessed through polysomnography. It includes data from four studies, notably featuring two influential cases: Raphael et al. [182] and Maluly et al. [255]. This comprehensive dataset encompasses a total of 830 observations and 186 documented instances of sleep bruxism.
The random effects model, optimal for heterogeneous data, suggests a central prevalence estimate of 43.42%, with a 95% confidence interval ranging from 16.65% to 74.68%. This extensive range indicates considerable variation across the studies, likely attributable to differences in population demographics, diagnostic criteria, or methodological approaches.
The prediction interval, spanning from 0.11% to 99.81%, underscores the substantial diversity in sleep bruxism prevalence among different populations as assessed by future studies. This wide interval suggests that while some populations may exhibit almost no occurrence of sleep bruxism, in others, nearly all individuals could be affected, depending on genetic, environmental, and behavioral factors.
Heterogeneity quantification reveals extremely high variability among the included studies (I2 = 98.5%). The τ2 = 1.81 and τ = 1.35 further confirm significant dispersion in effect sizes beyond what would be expected by sampling error alone. This is also reflected in the high H = 8.16, indicating that the true effect size varies substantially across the studies, much more than would be expected if the studies were homogeneous.
Both the Wald and LRT for heterogeneity confirm this observation, with p < 0.001, indicating that the differences in prevalence estimates across studies are indeed statistically significant and not due to random chance. These tests, therefore, reinforce the presence of high heterogeneity, suggesting that factors unique to each study or population significantly influence the prevalence of sleep bruxism.
3.3.3. Awake Bruxism
The results from a random effects model reveal a mean prevalence rate and show awake bruxism of 23.29%, with a 95% confidence interval ranging from 18.78% to 28.52%. This indicates that nearly one in four individuals may experience awake bruxism, a condition characterized by involuntary teeth grinding or jaw clenching while awake (Figure 3).
3.4. Meta-Analysis of Global Sleep and Awake Bruxism Prevalence across Continents
3.4.1. Sleep Bruxism
The subgroup analysis of sleep bruxism prevalence by continent in Table 3 reveals a complex picture of how this condition manifests across different geographical regions, influenced by varying study characteristics, methodologies, and potentially underlying regional factors affecting bruxism rates.
Table 3.
Variability in sleep bruxism prevalence: a subgroup analysis by continent.
| Continent | k | Proportion | CI 95% | τ2 | Q | I2 |
|---|---|---|---|---|---|---|
| Europe | 35 | 0.21 | 0.18–0.26 | 0.49 | 3855.24 | 99.1% |
| North America | 5 | 0.31 | 0.12–0.57 | 1.52 | 1575.75 | 99.7% |
| South America | 54 | 0.23 | 0.19–0.28 | 0.75 | 2800.83 | 98.1% |
| Asia | 46 | 0.19 | 0.15–0.23 | 0.71 | 10,727.90 | 99.6% |
k—number of studies; CI 95%—confidence interval 95%.
In Europe, where 35 studies were analyzed, the prevalence of sleep bruxism is estimated at 21%. The narrower confidence interval of 18% to 26% suggests a somewhat consistent measurement across studies, albeit the high I2 = 99.1% indicates that the variability among study findings is predominantly due to heterogeneity rather than chance. This could be reflective of different population demographics studied or varying diagnostic criteria used across European countries.
North America presents the highest prevalence at 31%, but this figure comes with a wide confidence interval from 12% to 57%, largely attributable to the small number (only 5) of studies conducted there. Such a wide interval indicates a significant uncertainty in the estimate, compounded by the highest τ2 = 1.52 among the groups, suggesting that the few studies included may be highly diverse in terms of methodology or population characteristics. The extremely high I2 = 99.7% further supports this view, pointing to substantial inconsistencies among the findings of these studies.
In contrast, South America, with the highest number of studies (54), shows a prevalence of 23%. The relatively tighter confidence interval of 19% to 28% alongside a τ2 = 0.75 suggests that while there is considerable variation among the studies, it is somewhat less than that observed in North America. The high I2 = 98.1% still underscores significant heterogeneity, indicating that despite a larger data pool, the consistency across study results is limited.
Asia, with 46 studies, reports the lowest prevalence at 19%, and its confidence interval ranges from 15% to 23%. The τ2 = 0.71, closely aligned with that of South America, and the extremely high Q = 10,727.90 combined with an I2 = 99.6% highlights that heterogeneity is also a major factor in Asian studies. This suggests that, similar to other continents, varying study designs, populations, and diagnostic criteria across Asian countries contribute to the diverse findings.
The test for subgroup differences across the continents yielded a Q(3) = of 3.07, p = 0.380, suggesting that the variations in bruxism prevalence between the continents are not statistically significant, despite the apparent differences in point estimates. This indicates that while there are numerical differences in the reported prevalence rates, these differences could be attributed to the high heterogeneity within each subgroup rather than true differences in prevalence across continents (Figure 3).
3.4.2. Awake Bruxism
The prevalence rates broken down by continent are shown in Table 4. Europe shows the lowest bruxism prevalence at 17.90%, with a very narrow confidence interval but still substantial heterogeneity (I2 = 99.0%). South America exhibits the highest prevalence at 29.86%, albeit with a wider confidence interval, reflecting more variability in the estimates and slightly less, yet still very high, heterogeneity (I2 = 97.8%). Asia has a prevalence rate of 24.91%, with associated confidence intervals and heterogeneity metrics similar to those of Europe (Table 4).
Table 4.
Variability in awake bruxism prevalence: a subgroup analysis by continent.
| Continent | k | Proportion | CI 95% | τ2 | Q | I2 |
|---|---|---|---|---|---|---|
| Europe | 22 | 0.18 | 0.13–0.25 | 0.88 | 2034.28 | 99.0% |
| South America | 15 | 0.30 | 0.19–0.44 | 1.44 | 648.92 | 97.8% |
| Asia | 19 | 0.25 | 0.18–0.34 | 0.91 | 1161.37 | 98.5% |
k—number of studies; CI 95%—confidence interval 95%.
Despite these differences, the test for subgroup differences across continents (Q = 3.84, df = 2, and p = 0.147) indicates that these variations are not statistically significant. This suggests that while numerically different, the variability within each continent’s estimates might be influencing the perception of between-continent differences (Figure 3).
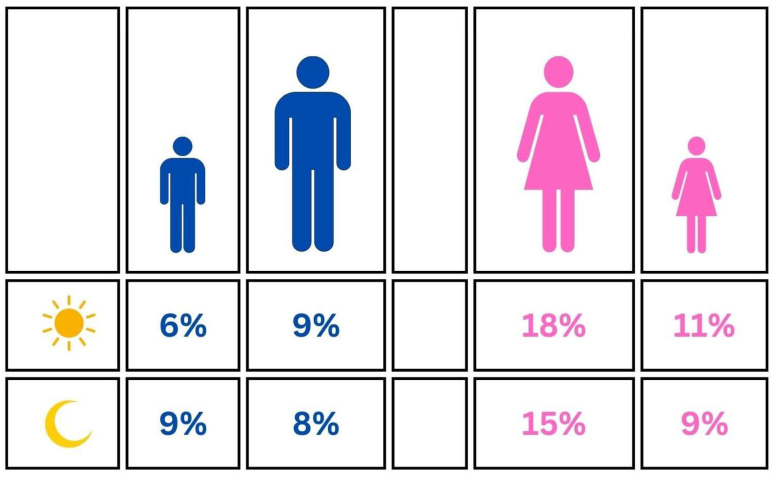
3.5. Meta-Analysis of Global Sleep and Awake Bruxism Prevalence among Females
3.5.1. Sleep Bruxism
The results derived from this comprehensive analysis, which employed a random effects model, suggest a central estimate of sleep bruxism prevalence at 11.68%, with a 95% confidence interval ranging from 9.07% to 14.07%. This prevalence rate indicates that sleep bruxism is a relatively common condition among females globally, albeit with significant variability.
When breaking down the data into subgroups of minors and adults, notable differences emerge. The prevalence among minors is 8.90%, with a narrower confidence interval of 6.96% to 11.30%, and among adults, it is higher at 14.49%, with a confidence interval of 11.14% to 18.64%. The heterogeneity within these subgroups remains high, with τ2 = 0.62 and 1.00, respectively, and both groups showing I2 = 98%.
Furthermore, the test for subgroup differences reveals a Q(1) = 7.23 with p = 0.007, indicating statistically significant differences between the prevalence rates of minors and adults. This suggests that age is a significant factor influencing the prevalence of sleep bruxism among females (Figure 4).
Figure 4.
Graphical representation of the prevalence among males and females.
3.5.2. Awake Bruxism
The findings from this specific subset reveal a pooled prevalence estimate of 17.07%, as indicated by the random effects model with a 95% confidence interval ranging from 12.39% to 23.05%. This prevalence suggests that awake bruxism is a significant concern among females, though the variation is notable.
When examining the results by age subgroups, the prevalence in minors is estimated at 11.28%, with a CI 95% stretching from 5.19% to 22.79%. Adults, however, exhibit a higher prevalence rate of 18.35%, with a CI 95% from 13.02% to 25.21%. Despite the apparent difference in prevalence rates, the test for subgroup differences, which yields a Q = 1.43 with p = 0.233, indicates that these differences are not statistically significant. This suggests that while numerically different, the prevalence rates between minors and adults do not diverge sufficiently when accounting for the high levels of variability within each subgroup (Figure 4).
3.6. Meta-Analysis of Global Sleep and Awake Bruxism Prevalence among Males
3.6.1. Sleep Bruxism
The results from this analysis, utilizing a random effects model, indicate a pooled prevalence rate of 8.48%, with a CI 95% from 7.25% to 9.89%. This suggests that while sleep bruxism is a notable health concern among males globally, the prevalence is somewhat moderate.
When dissecting the data into age subgroups, the prevalence in minors is slightly higher at 8.96%, with a 95% confidence interval of 7.00% to 11.40%, compared to 8.11% among adults, whose confidence interval ranges from 6.64% to 9.88%. The heterogeneity within these subgroups is notably high, with τ2 = 0.59 for minors and 0.47 for adults, and I2 = 99.4% and 98.7%, respectively.
The test for subgroup differences presents a Q = 0.38 with one degree of freedom and a p = 0.536, indicating that the differences in prevalence between minors and adults are not statistically significant. This suggests that age, within this data set, does not play a major role in differentiating the prevalence of sleep bruxism among males (Figure 4).
3.6.2. Awake Bruxism
Awake bruxism presents a pooled prevalence of 8.33%, as per the random effects model. The 95% confidence interval for this estimate ranges from 6.33% to 10.89%, indicating a moderate level of prevalence, but with considerable uncertainty about the precise rate.
By brokering down into age-specific subgroups, the results reveal that minors have a lower estimated prevalence of awake bruxism at 5.62%, with a confidence interval from 2.31% to 13.05%. Adults, on the other hand, show a higher prevalence of 8.91%, with a confidence interval ranging from 6.75% to 11.69%. Despite these numerical differences, the test for subgroup differences yields a Q = 1.00 with p = 0.317, indicating that these differences are not statistically significant.
This suggests that while there appears to be a trend towards higher prevalence in adults, the data do not strongly differentiate between the two age groups in terms of statistical significance, likely due to the high levels of variability and heterogeneity within each subgroup (Figure 4).
3.7. Meta-Analysis of Global Sleep and Awake Bruxism Prevalence by Age and Continent
3.7.1. Sleep Bruxism
Subgroup by continent and age group analysis reported a in Table 5 reveals nuanced insights. For instance, the prevalence in European adults is notably higher at 22.55% compared to European minors at 16.17%, with a relatively lower but still substantial heterogeneity in European adults (τ2 = 0.47, I2 = 99.0%). North American data show higher prevalence rates, particularly among adults at 36.39%, though this subgroup has a notably wide confidence interval, reflecting high uncertainty possibly due to the small number of studies (k = 2). This is supported by a very high τ2 = 3.32, indicating extreme variability.
Table 5.
Variability in sleep bruxism prevalence: a subgroup analysis by age.
| Continent | Age | k | Proportion | CI 95% | τ2 | Q | I2 |
|---|---|---|---|---|---|---|---|
| Europe | Minors | 6 | 0.16 | 0.10–0.25 | 0.44 | 260.30 | 98.1% |
| Europe | Adults | 29 | 0.23 | 0.18–0.27 | 0.47 | 2803.02 | 99.0% |
| North America | Minors | 3 | 0.28 | 0.16–0.45 | 0.38 | 147.98 | 98.6% |
| North America | Adults | 2 | 0.36 | 0.04–0.88 | 3.31 | 102.31 | 99.0% |
| South America | Minors | 34 | 0.24 | 0.20–0.28 | 0.48 | 1202.59 | 97.3% |
| South America | Adults | 20 | 0.23 | 0.16–0.32 | 1.18 | 1579.70 | 98.8% |
| Asia | Minors | 19 | 0.14 | 0.10–0.20 | 0.78 | 2527.53 | 99.3% |
| Asia | Adults | 27 | 0.23 | 0.18–0.28 | 0.54 | 2612.05 | 99.0% |
k—number of studies; CI 95%—confidence interval 95%.
In South America and Asia, the prevalence rates tend to be lower among minors compared to adults, with Asian minors showing the lowest prevalence at 14.40%. The heterogeneity remains very high across all subgroups, suggesting that even within continents and age groups, there are significant differences in study outcomes (Table 5).
The test for subgroup differences across continent-age categories shows a Q (7) = 10.04, p = 0.187, suggesting that while there are differences in prevalence rates across different subgroups, these differences are not statistically significant. This could imply that factors other than just continent and age might be influencing the prevalence rates, such as cultural differences, healthcare access, and diagnostic criteria.
3.7.2. Awake Bruxism
The meta-analysis detailed in Table 6 offers a nuanced look at the prevalence of awake bruxism across different continents and age groups, revealing a complex pattern influenced by geographic and demographic factors. The results underscore the variation not only in prevalence rates but also in the degree of heterogeneity among the subgroups analyzed.
Table 6.
Variability in awake bruxism prevalence: a subgroup analysis by continent and age.
| Continent | Age | k | Proportion | CI 95% | τ2 | Q | I2 |
|---|---|---|---|---|---|---|---|
| Europe | minors | 2 | 0.06 | 0.04–0.10 | 0.14 | 13.37 | 92.5% |
| Europe | adults | 20 | 0.20 | 0.14–0.27 | 0.79 | 1499.74 | 98.7% |
| South America | minors | 5 | 0.24 | 0.08–0.54 | 2.23 | 412.04 | 99.0% |
| South America | adults | 10 | 0.33 | 0.21–0.48 | 0.95 | 220.62 | 95.9% |
| Asia | minors | 3 | 0.22 | 0.18–0.28 | 0.06 | 49.06 | 95.9% |
| Asia | adults | 16 | 0.25 | 0.17–0.36 | 1.09 | 987.94 | 98.5% |
k—number of studies; CI 95%—confidence interval 95%.
Starting with Europe, the contrast between minors and adults in terms of bruxism prevalence is striking. Minors show a notably lower prevalence at 6%, which, despite being based on just two studies, suggests a lesser degree of awake bruxism in younger populations within Europe. However, the high level of heterogeneity (I2 = 92.5%) in this subgroup indicates that even within this narrow age range, factors contributing to bruxism are varied and possibly influenced by diverse cultural or environmental conditions. On the other hand, the adult population in Europe shows a higher prevalence at 20%, supported by a more substantial number of studies (20 in total). The even higher heterogeneity seen here (I2 = 98.7%) could reflect a wider range of contributing factors, such as stress, lifestyle, and possibly even differences in how bruxism is diagnosed and reported across European countries.
Moving to South America, the findings are intriguing due to the higher prevalence rates observed, especially in adults (33%). This region also exhibits significant variability, particularly among minors where the prevalence rate of 24% comes with a very broad confidence interval (0.08 to 0.54) and an extremely high heterogeneity (I2 = 99.0%). This suggests that there are specific local factors, possibly including socio-economic and cultural influences, that might exacerbate or mitigate the incidence of bruxism. The adult group, while also showing substantial heterogeneity (I2 = 95.9%), indicates a consistently higher prevalence across studies compared to minors, hinting at age-related factors that might influence the condition’s manifestation.
Asia presents a more consistent picture between minors and adults, with prevalence rates of 22% and 25%, respectively. The lower heterogeneity in minors (I2 = 95.9% with a lower τ2 value) compared to adults (I2 = 98.5%) could indicate more uniform diagnostic criteria or reporting practices within this demographic across the Asian studies. However, the high heterogeneity in adults suggests diverse underlying factors and possibly a range of responses to cultural, environmental, and biological influences.
The test for subgroup differences yielded a Q = 28.13 with a p < 0.001, indicating statistically significant differences in awake bruxism prevalence across different continental and age subgroups. This variation could be influenced by a range of factors, including genetic predispositions, cultural differences in stress management, diagnostic criteria, and awareness of the condition.
3.8. Meta-Analysis of Sleep and Awake Bruxism Prevalence by Continent and Age
In the meta-analysis of sleep bruxism prevalence among females by age and continent, the test for subgroup differences across continent and age categories reveals a Q(7) = 121.17, p < 0.001, indicating significant differences in the prevalence of sleep bruxism among different demographic and geographic groups, probably through small group sizes (Table 7).
Table 7.
Variability in sleep bruxism prevalence by continent and age among sex.
| Continent | Age | Proportion Females |
Proportion Males |
||
|---|---|---|---|---|---|
| Sleep Bruxism |
Awake Bruxism |
Sleep Bruxism |
Awake Bruxism |
||
| Europe | Minors | 0.05 | 0.03 | 0.06 | 0.01 |
| Europe | Adults | 0.15 | 0.14 | 0.08 | 0.06 |
| North America | Minors | 0.15 | - | 0.27 | - |
| North America | Adults | 0.78 | - | - | - |
| South America | Minors | 0.11 | - | 0.11 | - |
| South America | Adults | 0.15 | 0.26 | 0.08 | 0.10 |
| Asia | Minors | 0.07 | 0.15 | 0.07 | 0.09 |
| Asia | Adults | 0.13 | 0.27 | 0.07 | 0.17 |
In the meta-analysis of awake bruxism prevalence by continent and age among females, the test for subgroup differences confirms significant variability between these groups (Q = 72.17, p < 0.001), highlighting the influence of both geographic and age-related factors on awake bruxism prevalence among females. The notable differences in heterogeneity and prevalence rates between continents and age groups suggest that local environmental, cultural, and healthcare factors play critical roles in the manifestation and reporting of awake bruxism among females (Table 7).
In the meta-analysis of sleep bruxism prevalence among males by age and continent, the test for subgroup differences yields a Q = 339.82 with 6 degrees of freedom, accompanied by a p < 0.001. This result indicates that the variations in prevalence rates across different demographic and geographic subgroups are statistically significant. The notably high prevalence rate within the North American minors subgroup, which is considerably greater than those observed in other groups, likely contributes to these differences. However, the impact of this subgroup on the overall analysis should be interpreted with caution due to its small size (Table 6).
In the meta-analysis of awake bruxism prevalence by continent and age among males, the significant test for subgroup differences (Q = 53.34, p < 0.001) confirms that geographical and age-related factors play a crucial role in the prevalence of awake bruxism among males. These findings underscore the complexity of awake bruxism as a global health concern, influenced by a myriad of factors ranging from genetics and lifestyle to healthcare practices and cultural norms. The marked differences between continents and age groups highlight the need for targeted research and tailored interventions to effectively manage and mitigate awake bruxism in diverse male populations (Table 7).
4. Discussion
This meta-analysis had the purpose of assessing the global prevalence of sleep bruxism and awake bruxism in pediatric and adult populations. In response to the research questions posed in the introduction:
Question 1. What is the global prevalence of sleep and awake bruxism in the population? The global prevalence of sleep bruxism is 21%, and awake bruxism prevalence is 23%.
Question 2. What is the global prevalence of sleep and awake bruxism in the population depending on the continent? The prevalence of sleep bruxism was highest in North America at 31%, followed by South America at 23%, Europe at 21%, and Asia at 19%. The prevalence of awake bruxism was highest in South America at 30%, followed by Asia at 25%, and Europe at 18%.
Question 3. What is the global prevalence of sleep bruxism in the population depending on the continent, divided by age and gender? Sleep bruxism prevalence in North America was 36% in adults and 28% in minors, in South America 23% in adults and 24% in minors, in Europe 23% in adults and 16% in minors, and in Asia 23% in adults and 14% in minors.
Question 4. What is the global prevalence of awake bruxism in the population depending on the continent, divided by age and gender? Awake bruxism prevalence in South America was 33% in adults and 24% in minors, in Europe 20% in adults and 6% in minors, and in Asia 25% in adults and 22% in minors.
In the context of the main research questions, we want to highlight the potential impact of study heterogeneity. Regarding the first question and the occurrence of sleep bruxism, the result of the Egger’s test yielded a t (142) = 1.13, p = 0.258, indicating no statistically significant evidence of publication bias in the dataset. This suggests that the funnel plot is symmetrical, implying a balanced representation of studies with varying levels of variance. Smaller studies with less favorable outcomes are not disproportionately missing from the analysis. It is important to note that the analysis also considered substantial residual heterogeneity variance (τ2 = 151.99), indicating significant variability among the study estimates even after accounting for sampling variance. In the analysis of awake bruxism, the Egger linear regression test of funnel plot asymmetry yielded a t (57) = −1.27, p = 0.208. This p-value, above the significance threshold of 0.05, suggests no statistically significant evidence of publication bias in the dataset being analyzed. This indicates that the funnel plot is relatively symmetric, and the results of the meta-analysis are unlikely to be significantly influenced by selective publication of studies with more favorable outcomes (Supplementary Material S9).
Analyzing heterogeneity in response to the second question regarding sleep bruxism, the test for subgroup differences across continents yielded a Q(3) = 3.07, p = 0.380. This result suggests that the variations in bruxism prevalence between continents are not statistically significant, despite apparent differences in point estimates. This indicates that the numerical differences in reported prevalence rates may be due to high heterogeneity within each subgroup rather than genuine differences in prevalence across continents. In the analysis of awake bruxism, both the Wald and likelihood ratio tests for heterogeneity yielded p < 0.001, indicating significant heterogeneity among studies. This confirms that the studies included in the meta-analysis are estimating a range of effect sizes influenced by various factors, rather than a single underlying effect size. Despite this heterogeneity, the test for subgroup differences across continents (Q = 3.84, df = 2, and p = 0.147) suggests that these variations are not statistically significant. This implies that although there are numerical differences, the variability within estimates for each continent may be affecting the perception of differences between continents (Supplementary Material S9).
Analyzing question 3 in the context of sleep bruxism, the meta-analysis shows exceptionally high heterogeneity, with I2 = 99.4%, τ2 = 0.72, and τ = 0.85. These values indicate significant differences in study outcomes, likely stemming from methodological disparities, demographic variations, or differing diagnostic criteria across studies. The heterogeneity is further supported by the Q test (Wald = 21506.21, LRT = 23658.28), both yielding p < 0.001, indicating that the variability among studies is statistically significant and not due to chance (Supplementary Material S9).
Analyzing question 4 regarding awake bruxism, the heterogeneity observed in this meta-analysis is exceptionally high, with I2 = 98.8%. This suggests that nearly all of the variability in reported prevalence rates arises from genuine differences in study characteristics rather than random variance. Supporting this, τ2 = 1.12 and τ = 1.06 highlight substantial differences in true effect sizes across studies. The H statistic (H = 8.97) confirms significant dispersion in effect sizes among the included studies. Both the Wald and likelihood ratio tests for heterogeneity yielded p-values of zero, indicating significant variability that is not attributable to chance. These findings underscore the intricate nature of awake bruxism, influenced by a complex interplay of geographic, demographic, and methodological factors (Supplementary Material S9).
In our study, we determined that the global prevalence of bruxism (sleep and awake) is 22.22%, a result similar to the study by Ferrari-Piloni et al. [46]. It is worth noting further observations that sleep bruxism had the second highest occurrence in South America at 23%, and awake bruxism was highest in South America at 30%. These findings are consistent with those of Ferrari-Piloni et al. [46]. They also align with a meta-analysis on the prevalence of TMDs [48], where the highest occurrence of TMDs was similarly reported in South America at 47%. These results hypothetically suggest a connection between the occurrence of bruxism and TMDs. Such a connection was noted in the study by Mortazavi et al. [47], where the authors highlighted a positive association between bruxism and TMDs, with the presence of bruxism increasing the likelihood of future TMDs development.
It is also worth noting that despite the differences in percentage values in both cases, there were no statistically significant differences in the occurrence depending on the continent for sleep bruxism and awake bruxism. For sleep bruxism, the test for subgroup differences across the continents yielded a Q(3) = of 3.07, p = 0.380, suggesting that the variations in bruxism prevalence between the continents are not statistically significant, despite the apparent differences in point estimates. This indicates that while there are numerical differences in the reported prevalence rates, these differences could be attributed to the high heterogeneity within each subgroup rather than true differences in prevalence across continents. Similarly, for awake bruxism, the test for subgroup differences between continents (Q = 3.84, df = 2, and p = 0.147) indicates that these variations are not statistically significant. This suggests that, although numerically different, the variability within each continent’s estimates may influence the perception of differences between continents.
Soares et al. conducted a meta-analysis on children with sleep bruxism in the global population, showing a prevalence rate of 31.16% [45]. In our study, it turned out that sleep bruxism affects 21%, including both adults and minors. When divided among minors, bruxism was reported in 9% of minor females and males. Observable differences are likely associated with the period included in the analysis. In the study by Soares et al., this period was 10 years [45], whereas in our study, it was 20 years. However, analysis restricted to polysomnographic studies revealed a prevalence of sleep bruxism at 43%. Due to the small sample size, these results should be interpreted cautiously, and further analyses should be conducted in the future. This underscores the ongoing need to monitor the occurrence of bruxism in the population.
Archer et al. conducted a meta-analysis on the prevalence of awake bruxism in adults, finding a prevalence rate of 15.44% [44]. These results are similar to what we obtained. The global prevalence of awake bruxism was estimated at 23%. Among adult females, it was 18%, and among males, 9%.
The meta-analysis by Ferrari-Piloni et al. investigated the occurrence of bruxism in children residing in Brazil, revealing a prevalence of 25.8% in both sleep and awake states. Additionally, Ferrari-Piloni et al. observed regional differences in Brazil: Northeast—35.2%, Southeast—45.0%, and South—19.8% [46]. The meta-analysis by Ferrari-Piloni et al. [46] provided grounds to suggest that bruxism is associated with geographic factors.
Limitations of the Study
Among the limitations of the study is the lack of analysis of the prevalence of bruxism (sleep and awake bruxism) on the continents of Africa and Australia. As mentioned in the methodology, this was due to not collecting an adequate sample for analysis (one study concerning Australia [231] and three studies concerning Africa [232,233,234]). This illustrates a dependency that was already observed in an earlier meta-analysis concerning the occurrence of TMDs [48]. An additional limitation is the lack of analyses regarding awake bruxism in North America. At that time, an adequate number of studies needed to conduct the meta-analysis was also not collected. This indicates a research gap and underscores the need to conduct high-quality dental research on the epidemiology of diseases and parafunctions of the stomatognathic system on these continents [8,48,58]. Another limitation is the failure to consider the division in the pediatric population into permanent and mixed dentition. We suggest including these variables in subsequent analyses.
Another limitation of the study is what was observed in the analysis of the JBI questionnaire, specifically Q3, regarding the selection of an appropriate sample size, Q9, addressing the adequacy of the response rate, and Q7, concerning the diagnostic method for bruxism. Most studies relied on custom-made research questionnaires and self-reports from participants or their caregivers (in the case of children). Probably contributing to the high heterogeneity of results in this meta-analysis. Of course, both non-instrumental approaches (e.g., self-reports) and instrumental methods (e.g., electromyography) can be used to assess bruxism [19]. However, different research questionnaires create the potential for errors (for example, studies by Raphael et al. [182] and Restrepo et al. [185] highlight the risk of potential error associated with self-reported and parent-reported bruxism). Therefore, we highlight this potential risk. With the emergence of the standardized diagnostic tool BruxScreen [17], we hope that future epidemiological studies will be conducted using this tool among others.
The final limitation of this meta-analysis is the use of a single database. Despite conducting additional searches using an internet search engine and employing snowball sampling, there is a risk of selection bias.
5. Conclusions
The global bruxism (sleep and awake) prevalence is 22.22%.
The bruxism (sleep and awake) prevalence in North America is 29%, in South America is 25%, in Europe is 22%, and in Asia is 19%.
The global sleep bruxism prevalence is 21% and awake prevalence is 23%.
The occurrence of sleep bruxism, based on polysomnography, was estimated at 43%; however, due to the small sample size, these results should be approached with caution and the analyses should be repeated in the future.
One in four individuals may experience awake bruxism.
In the women population, it was determined that 12% of women experience sleep bruxism and 17% experience awake bruxism. Bruxism is a significant factor among women.
In adult women, the frequency of sleep bruxism was 15%, while in minors it was 9%. This suggests that age is a significant factor influencing the prevalence of sleep bruxism among females.
Age did not play a key role in the occurrence of awake bruxism in women. In adult women, it occurred at a rate of 18%, while in minors, it was 11%.
In the male population, it was determined that 9% of men experience sleep bruxism and 8% experience awake bruxism.
In adult men, the frequency of sleep bruxism was 8%, while in minors it was 9%. This suggests that age, within this data set, does not play a major role in differentiating the prevalence of sleep bruxism among males.
Age did not play a key role in the occurrence of awake bruxism in men. In adult men, it occurred at a rate of 9%, while in minors, it was 6%.
The highest prevalence of sleep bruxism was observed in North America at 31%, followed by South America at 23%, Europe at 21%, and Asia at 19%.
The prevalence of awake bruxism was highest in South America at 30%, followed by Asia at 25%, and Europe at 18%.
When divided by age, it was observed that sleep bruxism occurred in North America in 36% of adults and 28% of minors, in South America in 23% of adults and 24% of minors, in Europe in 23% of adults and 16% of minors, and in Asia in 23% of adults and 14% of minors.
When divided by age, it was observed that awake bruxism occurred in South America in 33% of adults and 24% of minors, in Europe in 20% of adults and 6% of minors, and in Asia in 25% of adults and 22% of minors.
It was observed that age is a significant factor for the occurrence of sleep bruxism in women, but this was not observed in men.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13144259/s1, Supplementary Material S1: PRISMA 2020 Abstract Checklist. Supplementary Material S2: PRISMA 2020 Checklist. Supplementary Material S3: Adapted questionnaire for initial selection. Supplementary Material S4: The results of the evaluation of studies using an adapted questionnaire. Supplementary Material S5: Presentation of the studies included the meta-analysis. Supplementary Material S6: Rejected studies from the meta-analysis. Supplementary Material S7: Adapted Joanna Briggs classification. Supplementary Material S8: The results of the evaluation of studies using an Joanna Briggs classification. Supplementary Material S9: Detailed description of the conducted meta-analysis. Supplementary Material S10: Presentation of forest plots. Supplementary Material S11: Presentation of funnel plots.
Author Contributions
Conceptualization, G.Z.; methodology, G.Z.; formal analysis, G.Z.; investigation, G.Z. and A.P.; data curation, G.Z.; writing—original draft preparation, G.Z.; writing—review and editing, G.Z., A.P. and M.W.; visualization, G.Z.; supervision, M.W.; project administration, G.Z.; funding acquisition, G.Z. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Frohman B. The Application of Psychotherapy to Dental Problems. Dent. Cosm. 1931;73:1117–1122. [Google Scholar]
- 2.Pietkiewicz M. La Bruxomanie: Memoires Originaux. Rev. Stomatol. 1907;14:107–116. [Google Scholar]
- 3.Editorial Attrition of the Grinding and Cutting Surfaces of Teeth. South Dent. Exam. 1860;1:24–25. [Google Scholar]
- 4.Faulkner K.D. Bruxism: A Review of the Literature. Part I. Aust. Dent. J. 1990;35:266–276. doi: 10.1111/j.1834-7819.1990.tb05406.x. [DOI] [PubMed] [Google Scholar]
- 5.Boyens P.J. Value of Autosuggestion in the Therapy of “Bruxism” and Other Biting Habits. J. Am. Dent. Assoc. 1940;27:1773–1777. doi: 10.14219/jada.archive.1940.0331. [DOI] [Google Scholar]
- 6.Nadler S.C. Bruxism, a Classification: Critical Review. J. Am. Dent. Assoc. 1957;54:615–622. doi: 10.14219/jada.archive.1957.0097. [DOI] [PubMed] [Google Scholar]
- 7.Wieckiewicz M., Paradowska-Stolarz A., Wieckiewicz W. Psychosocial Aspects of Bruxism: The Most Paramount Factor Influencing Teeth Grinding. BioMed Res. Int. 2014;2014:469187. doi: 10.1155/2014/469187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zieliński G., Gawda P. Surface Electromyography in Dentistry—Past, Present and Future. J. Clin. Med. 2024;13:1328. doi: 10.3390/jcm13051328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller S.C. Textbook of Periodontia. Blakiston Co.; Philadelphia, PA, USA: 1950. [Google Scholar]
- 10.Reddy S.V., Kumar M.P., Sravanthi D., Mohsin A.H.B., Anuhya V. Bruxism: A Literature Review. J. Int. Oral. Health. 2014;6:105–109. [PMC free article] [PubMed] [Google Scholar]
- 11.Okeson J.P. The Effects of Hard and Soft Occlusal Splints on Nocturnal Bruxism. J. Am. Dent. Assoc. 1987;114:788–791. doi: 10.14219/jada.archive.1987.0165. [DOI] [PubMed] [Google Scholar]
- 12.Lobbezoo F., Ahlberg J., Glaros A.G., Kato T., Koyano K., Lavigne G.J., de Leeuw R., Manfredini D., Svensson P., Winocur E. Bruxism Defined and Graded: An International Consensus. J. Oral Rehabil. 2013;40:2–4. doi: 10.1111/joor.12011. [DOI] [PubMed] [Google Scholar]
- 13.Every R.G. The Significance of Extreme Mandibular Movements. Lancet. 1960;276:37–39. doi: 10.1016/S0140-6736(60)92678-7. [DOI] [PubMed] [Google Scholar]
- 14.Lavigne G.J., Rompré P.H., Montplaisir J.Y. Sleep Bruxism: Validity of Clinical Research Diagnostic Criteria in a Controlled Polysomnographic Study. J. Dent. Res. 1996;75:546–552. doi: 10.1177/00220345960750010601. [DOI] [PubMed] [Google Scholar]
- 15.Bracci A., Djukic G., Favero L., Salmaso L., Guarda-Nardini L., Manfredini D. Frequency of Awake Bruxism Behaviours in the Natural Environment. A 7-Day, Multiple-Point Observation of Real-Time Report in Healthy Young Adults. J. Oral Rehabil. 2018;45:423–429. doi: 10.1111/joor.12627. [DOI] [PubMed] [Google Scholar]
- 16.Bracci A. First BruxApp Presentation. [(accessed on 27 April 2024)]. Available online: https://www.bruxapp.info/bruxism/en/first-bruxapp-presentation/
- 17.Lobbezoo F., Ahlberg J., Verhoeff M.C., Aarab G., Bracci A., Koutris M., Nykänen L., Thymi M., Wetselaar P., Manfredini D. The Bruxism Screener (BruxScreen): Development, Pilot Testing and Face Validity. J. Oral Rehabil. 2024;51:59–66. doi: 10.1111/joor.13442. [DOI] [PubMed] [Google Scholar]
- 18.Lobbezoo F., Naeije M. Bruxism Is Mainly Regulated Centrally, Not Peripherally. J. Oral Rehabil. 2001;28:1085–1091. doi: 10.1046/j.1365-2842.2001.00839.x. [DOI] [PubMed] [Google Scholar]
- 19.Lobbezoo F., Ahlberg J., Raphael K.G., Wetselaar P., Glaros A.G., Kato T., Santiago V., Winocur E., De Laat A., De Leeuw R., et al. International Consensus on the Assessment of Bruxism: Report of a Work in Progress. J. Oral Rehabil. 2018;45:837–844. doi: 10.1111/joor.12663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bulanda S., Ilczuk-Rypuła D., Nitecka-Buchta A., Nowak Z., Baron S., Postek-Stefańska L. Sleep Bruxism in Children: Etiology, Diagnosis, and Treatment-A Literature Review. Int. J. Environ. Res. Public Health. 2021;18:9544. doi: 10.3390/ijerph18189544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Oliveira M.T., Bittencourt S.T., Marcon K., Destro S., Pereira J.R. Sleep Bruxism and Anxiety Level in Children. Braz. Oral Res. 2015;29:S1806-83242015000100221. doi: 10.1590/1807-3107BOR-2015.vol29.0024. [DOI] [PubMed] [Google Scholar]
- 22.Khoury S., Rouleau G.A., Rompré P.H., Mayer P., Montplaisir J.Y., Lavigne G.J. A Significant Increase in Breathing Amplitude Precedes Sleep Bruxism. Chest. 2008;134:332–337. doi: 10.1378/chest.08-0115. [DOI] [PubMed] [Google Scholar]
- 23.Landry M.-L., Rompré P.H., Manzini C., Guitard F., de Grandmont P., Lavigne G.J. Reduction of Sleep Bruxism Using a Mandibular Advancement Device: An Experimental Controlled Study. Int. J. Prosthodont. 2006;19:549–556. [PubMed] [Google Scholar]
- 24.Bracha H.S., Ralston T.C., Matsukawa J.M., Williams A.E., Bracha A.S. Does “Fight or Flight” Need Updating? Psychosomatics. 2004;45:448–449. doi: 10.1176/appi.psy.45.5.448. [DOI] [PubMed] [Google Scholar]
- 25.Bracha H.S. Freeze, Flight, Fight, Fright, Faint: Adaptationist Perspectives on the Acute Stress Response Spectrum. CNS Spectr. 2004;9:679–685. doi: 10.1017/S1092852900001954. [DOI] [PubMed] [Google Scholar]
- 26.Manfredini D., Colonna A., Bracci A., Lobbezoo F. Bruxism: A Summary of Current Knowledge on Aetiology, Assessment and Management. Oral Surg. 2020;13:358–370. doi: 10.1111/ors.12454. [DOI] [Google Scholar]
- 27.Giovanni A., Giorgia A. The Neurophysiological Basis of Bruxism. Heliyon. 2021;7:e07477. doi: 10.1016/j.heliyon.2021.e07477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The International Classification Of Sleep Disorders, American Academy of Sleep Medicine. [(accessed on 20 March 2024)]. Available online: http://www.drawbridgedds.com/PM_PDF/The_International_Classification_of_Sleep_Disorders.pdf.
- 29.Onodera K., Kawagoe T., Sasaguri K., Protacio-Quismundo C., Sato S. The Use of a Bruxchecker in the Evaluation of Different Grinding Patterns during Sleep Bruxism. Cranio J. Craniomandib. Pract. 2006;24:292–299. doi: 10.1179/crn.2006.045. [DOI] [PubMed] [Google Scholar]
- 30.Dworkin S.F., LeResche L. Research Diagnostic Criteria for Temporomandibular Disorders: Review, Criteria, Examinations and Specifications, Critique. J. Craniomandib. Disord. Facial Oral Pain. 1992;6:301–355. [PubMed] [Google Scholar]
- 31.Schiffman E., Ohrbach R., Truelove E., Look J., Anderson G., Goulet J.-P., List T., Svensson P., Gonzalez Y., Lobbezoo F., et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache. 2014;28:6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ohrbach R., Beneduce C., Markiewicz M., McCall W., Jr. Psychometric Properties of the Oral Behaviors Checklist: Preliminary Findings. J. Dent. Res. 2004;83:1194. [Google Scholar]
- 33.Buysse D.J., Reynolds C.F., Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 34.Alkhatatbeh M.J., Hmoud Z.L., Abdul-Razzak K.K., Alem E.M. Self-Reported Sleep Bruxism Is Associated with Vitamin D Deficiency and Low Dietary Calcium Intake: A Case-Control Study. BMC Oral Health. 2021;21:21. doi: 10.1186/s12903-020-01349-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castrillon E.E., Exposto F.G. Sleep Bruxism and Pain. Dent. Clin. North Am. 2018;62:657–663. doi: 10.1016/j.cden.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 36.von Piekartz H., Rösner C., Batz A., Hall T., Ballenberger N. Bruxism, Temporomandibular Dysfunction and Cervical Impairments in Females—Results from an Observational Study. Musculoskelet. Sci. Pract. 2020;45:102073. doi: 10.1016/j.msksp.2019.102073. [DOI] [PubMed] [Google Scholar]
- 37.Casazza E., Ballester B., Philip-Alliez C., Raskin A. Evaluation of Mandibular Bone Density in Bruxers: The Value of Panoramic Radiographs. Oral Radiol. 2023;39:117–124. doi: 10.1007/s11282-022-00612-3. [DOI] [PubMed] [Google Scholar]
- 38.Amorim C.S.M., Espirito Santo A.S., Sommer M., Marques A.P. Effect of Physical Therapy in Bruxism Treatment: A Systematic Review. J. Manip. Physiol. Ther. 2018;41:389–404. doi: 10.1016/j.jmpt.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 39.Lal S.J., Sankari A., Weber D.D.S. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2024. Bruxism Management. [PubMed] [Google Scholar]
- 40.Dallanora L.J., Faltin P., Inoue R., Santos V. Acunpucture Use in the Treatment of Patients with Bruxism. RGO. 2004;52:333–339. [Google Scholar]
- 41.Guaita M., Högl B. Current Treatments of Bruxism. Curr. Treat. Options Neurol. 2016;18:10. doi: 10.1007/s11940-016-0396-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lobbezoo F., van der Zaag J., van Selms M.K.A., Hamburger H.L., Naeije M. Principles for the Management of Bruxism. J. Oral Rehabil. 2008;35:509–523. doi: 10.1111/j.1365-2842.2008.01853.x. [DOI] [PubMed] [Google Scholar]
- 43.Bussadori S.K., Motta L.J., Horliana A.C.R.T., Santos E.M., Martimbianco A.L.C. The Current Trend in Management of Bruxism and Chronic Pain: An Overview of Systematic Reviews. J. Pain Res. 2020;13:2413–2421. doi: 10.2147/JPR.S268114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Archer A.B., Da-Cas C.D., Valesan L.F., Cunha T.C.A., Januzzi E., Garanhani R.R., de La Torre Canales G., de Souza B.D.M. Prevalence of Awake Bruxism in the Adult Population: A Systematic Review and Meta-Analysis. Clin. Oral Investig. 2023;27:7007–7018. doi: 10.1007/s00784-023-05302-w. [DOI] [PubMed] [Google Scholar]
- 45.Soares J.P., Moro J., Massignan C., Cardoso M., Serra-Negra J.M., Maia L.C., Bolan M. Prevalence of Clinical Signs and Symptoms of the Masticatory System and Their Associations in Children with Sleep Bruxism: A Systematic Review and Meta-Analysis. Sleep Med. Rev. 2021;57:101468. doi: 10.1016/j.smrv.2021.101468. [DOI] [PubMed] [Google Scholar]
- 46.Ferrari-Piloni C., Barros L.A.N., Evangelista K., Serra-Negra J.M., Silva M.A.G., Valladares-Neto J. Prevalence of Bruxism in Brazilian Children: A Systematic Review and Meta-Analysis. Pediatr. Dent. 2022;44:8–20. [PubMed] [Google Scholar]
- 47.Mortazavi N., Tabatabaei A.H., Mohammadi M., Rajabi A. Is Bruxism Associated with Temporomandibular Joint Disorders? A Systematic Review and Meta-Analysis. Evid. Based Dent. 2023;24:144. doi: 10.1038/s41432-023-00911-6. [DOI] [PubMed] [Google Scholar]
- 48.Zieliński G., Pająk-Zielińska B., Ginszt M. A Meta-Analysis of the Global Prevalence of Temporomandibular Disorders. J. Clin. Med. 2024;13:1365. doi: 10.3390/jcm13051365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zieliński G., Pająk A., Wójcicki M. A Meta-Analysis of the Global Prevalence of Sleep Bruxism and Awake Bruxism in Pediatric and Adult Populations. OSF; Toronto, ON, USA: 2024. [DOI] [Google Scholar]
- 50.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Han S., Harold C.M., Oh I.-S., Kim J.K., Agolli A. A Meta-Analysis Integrating 20 Years of Workplace Incivility Research: Antecedents, Consequences, and Boundary Conditions. J. Organ. Behav. 2022;43:497–523. doi: 10.1002/job.2568. [DOI] [Google Scholar]
- 53.Zhou S., Page-Gould E., Aron A., Moyer A., Hewstone M. The Extended Contact Hypothesis: A Meta-Analysis on 20 Years of Research. Personal. Soc. Psychol. Rev. 2019;23:132–160. doi: 10.1177/1088868318762647. [DOI] [PubMed] [Google Scholar]
- 54.Kothgassner O.D., Robinson K., Goreis A., Ougrin D., Plener P.L. Does Treatment Method Matter? A Meta-Analysis of the Past 20 Years of Research on Therapeutic Interventions for Self-Harm and Suicidal Ideation in Adolescents. Borderline Personal. Disord. Emot. Dysregulation. 2020;7:9. doi: 10.1186/s40479-020-00123-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Holden B.A., Fricke T.R., Wilson D.A., Jong M., Naidoo K.S., Sankaridurg P., Wong T.Y., Naduvilath T.J., Resnikoff S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123:1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 56.Halladay C.W., Trikalinos T.A., Schmid I.T., Schmid C.H., Dahabreh I.J. Using Data Sources beyond PubMed Has a Modest Impact on the Results of Systematic Reviews of Therapeutic Interventions. J. Clin. Epidemiol. 2015;68:1076–1084. doi: 10.1016/j.jclinepi.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 57.Manfredini D., Restrepo C., Diaz-Serrano K., Winocur E., Lobbezoo F. Prevalence of Sleep Bruxism in Children: A Systematic Review of the Literature. J. Oral Rehabil. 2013;40:631–642. doi: 10.1111/joor.12069. [DOI] [PubMed] [Google Scholar]
- 58.Zieliński G., Gawda P. Analysis of the Use of Sample Size and Effect Size Calculations in a Temporomandibular Disorders Randomised Controlled Trial—Short Narrative Review. J. Pers. Med. 2024;14:655. doi: 10.3390/jpm14060655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wohlin C. Guidelines for Snowballing in Systematic Literature Studies and a Replication in Software Engineering; Proceedings of the 18th International Conference on Evaluation and Assessment in Software Engineering; London, UK. 13–14 May 2014; London, UK: ACM; 2014. pp. 1–10. [Google Scholar]
- 60.Brown D. A Review of the PubMed PICO Tool: Using Evidence-Based Practice in Health Education. Health Promot. Pract. 2020;21:496–498. doi: 10.1177/1524839919893361. [DOI] [PubMed] [Google Scholar]
- 61.Berger M., Szalewski L., Bakalczuk M., Bakalczuk G., Bakalczuk S., Szkutnik J. Association between Estrogen Levels and Temporomandibular Disorders: A Systematic Literature Review. Menopause Rev. Menopauzalny. 2015;14:260–270. doi: 10.5114/pm.2015.56538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Aromataris E., Lockwood C., Porritt K., Pilla B., Jordan Z. Manual for Evidence Synthesis. JBI; Miami, FL, USA: 2018. [DOI] [Google Scholar]
- 63.Giannakopoulos N.N., Rammelsberg P., Eberhard L., Schmitter M. A New Instrument for Assessing the Quality of Studies on Prevalence. Clin. Oral Investig. 2012;16:781–788. doi: 10.1007/s00784-011-0557-4. [DOI] [PubMed] [Google Scholar]
- 64.Stang A. Critical Evaluation of the Newcastle-Ottawa Scale for the Assessment of the Quality of Nonrandomized Studies in Meta-Analyses. Eur. J. Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 65.Palinkas M., De Luca Canto G., Rodrigues L.A.M., Bataglion C., Siéssere S., Semprini M., Regalo S.C.H. Comparative Capabilities of Clinical Assessment, Diagnostic Criteria, and Polysomnography in Detecting Sleep Bruxism. J. Clin. Sleep Med. 2015;11:1319–1325. doi: 10.5664/jcsm.5196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Aguiar S.O., Prado I.M., Silveira K.S.R., Abreu L.G., Auad S.M., Paiva S.M., Serra-Negra J.M.C. Possible Sleep Bruxism, Circadian Preference, and Sleep-Related Characteristics and Behaviors among Dental Students. Cranio J. Craniomandib. Pract. 2019;37:389–394. doi: 10.1080/08869634.2018.1471113. [DOI] [PubMed] [Google Scholar]
- 67.Ahlberg J., Lobbezoo F., Manfredini D., Piirtola M., Hublin C., Kaprio J. Self-Reported Sleep Bruxism and Mortality in 1990–2020 in a Nationwide Twin Cohort. J. Oral Rehabil. 2024;51:125–130. doi: 10.1111/joor.13441. [DOI] [PubMed] [Google Scholar]
- 68.Ahlberg K., Jahkola A., Savolainen A., Könönen M., Partinen M., Hublin C., Sinisalo J., Lindholm H., Sarna S., Ahlberg J. Associations of Reported Bruxism with Insomnia and Insufficient Sleep Symptoms among Media Personnel with or without Irregular Shift Work. Head Face Med. 2008;4:4. doi: 10.1186/1746-160X-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Alfano C.A., Bower J.L., Meers J.M. Polysomnography-Detected Bruxism in Children Is Associated with Somatic Complaints but Not Anxiety. J. Clin. Sleep Med. 2018;14:23–29. doi: 10.5664/jcsm.6872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brandão de Almeida A., Rodrigues R.S., Simão C., de Araújo R.P., Figueiredo J. Prevalence of Sleep Bruxism Reported by Parents/Caregivers in a Portuguese Pediatric Dentistry Service: A Retrospective Study. Int. J. Environ. Res. Public Health. 2022;19:7823. doi: 10.3390/ijerph19137823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Almutairi A.F., Albesher N., Aljohani M., Alsinanni M., Turkistani O., Salam M. Association of Oral Parafunctional Habits with Anxiety and the Big-Five Personality Traits in the Saudi Adult Population. Saudi Dent. J. 2021;33:90–98. doi: 10.1016/j.sdentj.2020.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Alonso L.S., Serra-Negra J.M., Abreu L.G., Martins I.M., Tourino L.F.P.G., Vale M.P. Association between Possible Awake Bruxism and Bullying among 8- to 11-Year-Old Children/Adolescents. Int. J. Paediatr. Dent. 2022;32:41–48. doi: 10.1111/ipd.12789. [DOI] [PubMed] [Google Scholar]
- 73.Al-Swaje N., Shammary A.-A., Al-Khalifah S.S., Shafshaks S. The Prevalence of Bruxism and Dental Wear in Children in Relation to Smart Devices and Video Games. Indo Am. J. Pharm. Sci. 2019;6:4560–4565. doi: 10.5281/zenodo.2579294. [DOI] [Google Scholar]
- 74.Amaral C.C., dos Santos Fernandez M., Jansen K., da Silva R.A., Boscato N., Goettems M.L. Daily Screen Time, Sleep Pattern, and Probable Sleep Bruxism in Children: A Cross-Sectional Study. Oral Dis. 2023;29:2888–2894. doi: 10.1111/odi.14395. [DOI] [PubMed] [Google Scholar]
- 75.Antunes L.A.A., Castilho T., Marinho M., Fraga R.S., Antunes L.S. Childhood Bruxism: Related Factors and Impact on Oral Health-Related Quality of Life. Spec. Care Dentist. 2016;36:7–12. doi: 10.1111/scd.12140. [DOI] [PubMed] [Google Scholar]
- 76.Arısan V., Bedeloğlu E., Pişkin B. Prevalence and Predictors of Bruxism in Two University Clinic Patient Populations with Dental Implants: A Cross-Sectional Analysis. Cranio J. Craniomandib. Pract. 2022:1–12. doi: 10.1080/08869634.2022.2071794. [DOI] [PubMed] [Google Scholar]
- 77.de Lima Bach S., Moreira F.P., Goettems M.L., Brancher L.C., Oses J.P., da Silva R.A., Jansen K. Salivary Cortisol Levels and Biological Rhythm in Schoolchildren with Sleep Bruxism. Sleep Med. 2019;54:48–52. doi: 10.1016/j.sleep.2018.09.031. [DOI] [PubMed] [Google Scholar]
- 78.Mercan Başpınar M., Mercan Ç., Mercan M., Arslan Aras M. Comparison of the Oral Health-Related Quality of Life, Sleep Quality, and Oral Health Literacy in Sleep and Awake Bruxism: Results from Family Medicine Practice. Int. J. Clin. Pract. 2023;2023:1186278. doi: 10.1155/2023/1186278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Berger M., Szalewski L., Szkutnik J., Ginszt M., Ginszt A. Different Association between Specific Manifestations of Bruxism and Temporomandibular Disorder Pain. Neurol. Neurochir. Pol. 2017;51:7–11. doi: 10.1016/j.pjnns.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 80.Bharti B., Malhi P., Kashyap S. Patterns and Problems of Sleep in School Going Children. Indian Pediatr. 2006;43:35–38. [PubMed] [Google Scholar]
- 81.Bolsson G.B., Knorst J.K., Menegazzo G.R., Ardenghi T.M. Impact of Dental Bullying on Bruxism Associated with Poor Sleep Quality among Adolescents. Braz. Oral Res. 2023;37:e36. doi: 10.1590/1807-3107bor-2023.vol37.0036. [DOI] [PubMed] [Google Scholar]
- 82.Borie L., Langbour N., Guehl D., Burbaud P., Ella B. Bruxism in Craniocervical Dystonia: A Prospective Study. Cranio J. Craniomandib. Pract. 2016;34:291–295. doi: 10.1080/08869634.2015.1120473. [DOI] [PubMed] [Google Scholar]
- 83.Bortoletto C.C., da Consolação Canuto Salgueiro M., Valio R., Fragoso Y.D., Motta P.d.B., Motta L.J., Kobayashi F.Y., Fernandes K.P.S., Mesquita-Ferrari R.A., Deana A., et al. The Relationship between Bruxism, Sleep Quality, and Headaches in Schoolchildren. J. Phys. Ther. Sci. 2017;29:1889–1892. doi: 10.1589/jpts.29.1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Botelho J., Machado V., Proença L., Rua J., Martins L., Alves R., Cavacas M.A., Manfredini D., Mendes J.J. Relationship between Self-Reported Bruxism and Periodontal Status: Findings from a Cross-Sectional Study. J. Periodontol. 2020;91:1049–1056. doi: 10.1002/JPER.19-0364. [DOI] [PubMed] [Google Scholar]
- 85.Brancher L.C., Cademartori M.G., Jansen K., da Silva R.A., Bach S., Reyes A., Boscato N., Goettems M.L. Social, Emotional, and Behavioral Problems and Parent-Reported Sleep Bruxism in Schoolchildren. J. Am. Dent. Assoc. 2020;151:327–333. doi: 10.1016/j.adaj.2020.01.025. [DOI] [PubMed] [Google Scholar]
- 86.Breda M., Belli A., Esposito D., Di Pilla A., Melegari M.G., DelRosso L., Malorgio E., Doria M., Ferri R., Bruni O. Sleep Habits and Sleep Disorders in Italian Children and Adolescents: A Cross-Sectional Survey. J. Clin. Sleep Med. 2023;19:659–672. doi: 10.5664/jcsm.10400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bucci C., Amato M., Zingone F., Caggiano M., Iovino P., Ciacci C. Prevalence of Sleep Bruxism in IBD Patients and Its Correlation to Other Dental Disorders and Quality of Life. Gastroenterol. Res. Pract. 2018;2018:7274318. doi: 10.1155/2018/7274318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cai X.-H., Xie Y.-P., Li X.-C., Qu W.-L., Li T., Wang H.-X., Lv J.-Q., Wang L.-X. The Prevalence and Associated Risk Factors of Sleep Disorder-Related Symptoms in Pregnant Women in China. Sleep Breath. Schlaf Atm. 2013;17:951–956. doi: 10.1007/s11325-012-0783-2. [DOI] [PubMed] [Google Scholar]
- 89.Câmara-Souza M.B., Carvalho A.G., Figueredo O.M.C., Bracci A., Manfredini D., Rodrigues Garcia R.C.M. Awake Bruxism Frequency and Psychosocial Factors in College Preparatory Students. Cranio J. Craniomandib. Pract. 2023;41:178–184. doi: 10.1080/08869634.2020.1829289. [DOI] [PubMed] [Google Scholar]
- 90.Carra M.C., Huynh N., Morton P., Rompré P.H., Papadakis A., Remise C., Lavigne G.J. Prevalence and Risk Factors of Sleep Bruxism and Wake-Time Tooth Clenching in a 7- to 17-Yr-Old Population. Eur. J. Oral Sci. 2011;119:386–394. doi: 10.1111/j.1600-0722.2011.00846.x. [DOI] [PubMed] [Google Scholar]
- 91.Cavalcante-Leão B.L., Todero S.R.B., Ferreira F.M., Gavião M.B.D., Fraiz F.C. Profile of Orofacial Dysfunction in Brazilian Children Using the Nordic Orofacial Test-Screening. Acta Odontol. Scand. 2017;75:262–267. doi: 10.1080/00016357.2017.1290823. [DOI] [PubMed] [Google Scholar]
- 92.Cavallo P., Carpinelli L., Savarese G. Perceived Stress and Bruxism in University Students. BMC Res. Notes. 2016;9:514. doi: 10.1186/s13104-016-2311-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chattrattrai T., Blanken T.F., Lobbezoo F., Su N., Aarab G., Van Someren E.J.W. A Network Analysis of Self-Reported Sleep Bruxism in the Netherlands Sleep Registry: Its Associations with Insomnia and Several Demographic, Psychological, and Life-Style Factors. Sleep Med. 2022;93:63–70. doi: 10.1016/j.sleep.2022.03.018. [DOI] [PubMed] [Google Scholar]
- 94.Cheifetz A.T., Osganian S.K., Allred E.N., Needleman H.L. Prevalence of Bruxism and Associated Correlates in Children as Reported by Parents. J. Dent. Child. 2005;72:67–73. [PubMed] [Google Scholar]
- 95.Ciancaglini R., Gherlone E.F., Radaelli G. The Relationship of Bruxism with Craniofacial Pain and Symptoms from the Masticatory System in the Adult Population. J. Oral Rehabil. 2001;28:842–848. doi: 10.1111/j.1365-2842.2001.00753.x. [DOI] [PubMed] [Google Scholar]
- 96.Clementino M.A., Siqueira M.B., Serra-Negra J.M., Paiva S.M., Granville-Garcia A.F. The Prevalence of Sleep Bruxism and Associated Factors in Children: A Report by Parents. Eur. Arch. Paediatr. Dent. Off. J. Eur. Acad. Paediatr. Dent. 2017;18:399–404. doi: 10.1007/s40368-017-0312-x. [DOI] [PubMed] [Google Scholar]
- 97.Colonna A., Guarda-Nardini L., Ferrari M., Manfredini D. COVID-19 Pandemic and the Psyche, Bruxism, Temporomandibular Disorders Triangle. Cranio J. Craniomandib. Pract. 2021;42:429–434. doi: 10.1080/08869634.2021.1989768. [DOI] [PubMed] [Google Scholar]
- 98.da Costa S.V., de Souza B.K., Cruvinel T., Oliveira T.M., Lourenço Neto N., Machado M.A.A.M. Factors Associated with Preschool Children’s Sleep Bruxism. Cranio J. Craniomandib. Pract. 2024;42:48–54. doi: 10.1080/08869634.2021.1903663. [DOI] [PubMed] [Google Scholar]
- 99.Costa F.D.S., Fernandez M.D.S., da Silva-Junior I.F., Karam S.A., Chisini L.A., Goettems M.L. Association Involving Possible Sleep Bruxism, Stress, and Depressive Symptoms in Brazilian University Students: A Cross-Sectional Study. Sleep Sci. 2023;16:e317–e322. doi: 10.1055/s-0043-1772808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Coutinho E.N., dos Santos K.P.R., Ferreira E.H.B., Pinto R.G.S., de Oliveira Sanchez M. Association between Self-Reported Sleep Bruxism and Temporomandibular Disorder in Undergraduate Students from Brazil. Cranio J. Craniomandib. Pract. 2020;38:91–98. doi: 10.1080/08869634.2018.1495874. [DOI] [PubMed] [Google Scholar]
- 101.Dantas-Neta N.B., Laurentino J.B., Souza C.H.d.C.e., Nunes-Dos-Santos D.L., Mendes R.F., Prado-Júnior R.R. Prevalence and Potential Factors Associated with Probable Sleep or Awake Bruxism and Dentin Hypersensitivity in Undergraduate Students. Rev. Odontol. UNESP. 2014;43:245–251. doi: 10.1590/rou.2014.040. [DOI] [Google Scholar]
- 102.Delgado-Delgado R., Iriarte-Álvarez N., Valera-Calero J.A., Centenera-Centenera M.B., Garnacho-Garnacho V.E., Gallego-Sendarrubias G.M. Association between Temporomandibular Disorders with Clinical and Sociodemographic Features: An Observational Study. Int. J. Clin. Pract. 2021;75:e13961. doi: 10.1111/ijcp.13961. [DOI] [PubMed] [Google Scholar]
- 103.Demir A., Uysal T., Guray E., Basciftci F.A. The Relationship between Bruxism and Occlusal Factors among Seven- to 19-Year-Old Turkish Children. Angle Orthod. 2004;74:672–676. doi: 10.1043/0003-3219(2004)074<0672:TRBBAO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 104.Diéguez-Pérez M., Ticona-Flores J.M., Prieto-Regueiro B. Prevalence of Possible Sleep Bruxism and Its Association with Social and Orofacial Factors in Preschool Population. Healthcare. 2023;11:1450. doi: 10.3390/healthcare11101450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Drumond C.L., Ramos-Jorge J., Vieira-Andrade R.G., Paiva S.M., Serra-Negra J.M.C., Ramos-Jorge M.L. Prevalence of Probable Sleep Bruxism and Associated Factors in Brazilian Schoolchildren. Int. J. Paediatr. Dent. 2018;29:221–227. doi: 10.1111/ipd.12443. [DOI] [PubMed] [Google Scholar]
- 106.Duarte J., de Souza J.F., Cavalcante-Leão B., Todero S.R.B., Ferreira F.M., Fraiz F.C. Association of Possible Sleep Bruxism with Daytime Oral Habits and Sleep Behavior in Schoolchildren. Cranio J. Craniomandib. Pract. 2021;39:372–378. doi: 10.1080/08869634.2019.1661113. [DOI] [PubMed] [Google Scholar]
- 107.Ekman A., Rousu J., Näpänkangas R., Kuoppala R., Raustia A., Sipilä K. Association of Self-Reported Bruxism with Temporomandibular Disorders—Northern Finland Birth Cohort (NFBC) 1966 Study. Cranio J. Craniomandib. Pract. 2023;41:212–217. doi: 10.1080/08869634.2020.1853306. [DOI] [PubMed] [Google Scholar]
- 108.Eli I., Zigler-Garburg A., Winocur E., Friedman-Rubin P., Shalev-Antsel T., Levartovsky S., Emodi-Perlman A. Temporomandibular Disorders and Bruxism among Sex Workers—A Cross Sectional Study. J. Clin. Med. 2022;11:6622. doi: 10.3390/jcm11226622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Emmanuelli B., de Araujo G., Knorst J.K., Tagliari C.V.d.C., Baldissera B.S., Tuchtenhagen S. Social Capital and Possible Bruxism during the COVID-19 Pandemic among Brazilian Undergraduates. Braz. Oral Res. 2023;37:e108. doi: 10.1590/1807-3107bor-2023.vol37.0108. [DOI] [PubMed] [Google Scholar]
- 110.Emodi-Perlman A., Eli I., Smardz J., Uziel N., Wieckiewicz G., Gilon E., Grychowska N., Wieckiewicz M. Temporomandibular Disorders and Bruxism Outbreak as a Possible Factor of Orofacial Pain Worsening during the COVID-19 Pandemic-Concomitant Research in Two Countries. J. Clin. Med. 2020;9:3250. doi: 10.3390/jcm9103250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Emodi Perlman A., Lobbezoo F., Zar A., Friedman Rubin P., van Selms M.K.A., Winocur E. Self-Reported Bruxism and Associated Factors in Israeli Adolescents. J. Oral Rehabil. 2016;43:443–450. doi: 10.1111/joor.12391. [DOI] [PubMed] [Google Scholar]
- 112.Farsi N.M.A. Symptoms and Signs of Temporomandibular Disorders and Oral Parafunctions among Saudi Children. J. Oral Rehabil. 2003;30:1200–1208. doi: 10.1111/j.1365-2842.2003.01187.x. [DOI] [PubMed] [Google Scholar]
- 113.Ferreira N.M.R., dos Santos J.F.F., dos Santos M.B.F., Marchini L. Sleep Bruxism Associated with Obstructive Sleep Apnea Syndrome in Children. Cranio J. Craniomandib. Pract. 2015;33:251–255. doi: 10.1179/2151090314Y.0000000025. [DOI] [PubMed] [Google Scholar]
- 114.Feteih R.M. Signs and Symptoms of Temporomandibular Disorders and Oral Parafunctions in Urban Saudi Arabian Adolescents: A Research Report. Head Face Med. 2006;2:25. doi: 10.1186/1746-160X-2-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Medina Flores D., Barragán Nuñez M.I., Müller de Quevedo H., Bonjardim L.R., Rodrigues Conti P.C. Real Time Evaluation of Awake Bruxism Behaviors in Young Asymptomatic Students and Its Impact on the Masticatory Muscles. J. Prosthet. Dent. 2023 doi: 10.1016/j.prosdent.2023.03.009. ahead-of-print . [DOI] [PubMed] [Google Scholar]
- 116.Flueraşu M.I., Bocşan I.C., Țig I.-A., Iacob S.M., Popa D., Buduru S. The Epidemiology of Bruxism in Relation to Psychological Factors. Int. J. Environ. Res. Public Health. 2022;19:691. doi: 10.3390/ijerph19020691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Fonseca C.M.E., dos Santos M.B.F., Consani R.L.X., dos Santos J.F.F., Marchini L. Incidence of Sleep Bruxism among Children in Itanhandu, Brazil. Sleep Breath. 2011;15:215–220. doi: 10.1007/s11325-010-0427-3. [DOI] [PubMed] [Google Scholar]
- 118.Fulgencio L.B., Corrêa-Faria P., Lage C.F., Paiva S.M., Pordeus I.A., Serra-Negra J.M. Diagnosis of Sleep Bruxism Can Assist in the Detection of Cases of Verbal School Bullying and Measure the Life Satisfaction of Adolescents. Int. J. Paediatr. Dent. 2017;27:293–301. doi: 10.1111/ipd.12264. [DOI] [PubMed] [Google Scholar]
- 119.Gao Y., Xu P., Aizetiguli M., Surong S., Zhu Z., Zhang J. Prevalence and Influencing Factors of Sleep Disorders among Preschool Children in Urumqi City: A Cross-Sectional Survey. Ital. J. Pediatr. 2023;49:68. doi: 10.1186/s13052-023-01477-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Garde J.B., Suryavanshi R.K., Jawale B.A., Deshmukh V., Dadhe D.P., Suryavanshi M.K. An Epidemiological Study to Know the Prevalence of Deleterious Oral Habits among 6 to 12 Year Old Children. J. Int. Oral Health. 2014;6:39–43. [PMC free article] [PubMed] [Google Scholar]
- 121.Ghafournia M., Hajenourozali Tehrani M. Relationship between Bruxism and Malocclusion among Preschool Children in Isfahan. J. Dent. Res. Dent. Clin. Dent. Prospects. 2012;6:138–142. doi: 10.5681/joddd.2012.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ghalebandi M., Salehi M., Rasoulain M., Shooshtari M.H., Naserbakht M., Salarifar M.H. Prevalence of Parasomnia in School Aged Children in Tehran. Iran. J. Psychiatry. 2011;6:75–79. [PMC free article] [PubMed] [Google Scholar]
- 123.Goettems M.L., Poletto-Neto V., Shqair A.Q., Pinheiro R.T., Demarco F.F. Influence of Maternal Psychological Traits on Sleep Bruxism in Children. Int. J. Paediatr. Dent. 2017;27:469–475. doi: 10.1111/ipd.12285. [DOI] [PubMed] [Google Scholar]
- 124.Gomes M.C., Neves É.T., Perazzo M.F., de Souza E.G.C., Serra-Negra J.M., Paiva S.M., Granville-Garcia A.F. Evaluation of the Association of Bruxism, Psychosocial and Sociodemographic Factors in Preschoolers. Braz. Oral Res. 2018;32:e009. doi: 10.1590/1807-3107bor-2018.vol32.0009. [DOI] [PubMed] [Google Scholar]
- 125.Goulart A.C., Arap A.M., Bufarah H.B., Bismarchi D., Rienzo M., Syllos D.H., Wang Y.-P. Anxiety, Depression, and Anger in Bruxism: A Cross-Sectional Study among Adult Attendees of a Preventive Center. Psychiatry Res. 2021;299:113844. doi: 10.1016/j.psychres.2021.113844. [DOI] [PubMed] [Google Scholar]
- 126.Hermesh H., Schapir L., Marom S., Skopski R., Barnea E., Weizman A., Winocur E. Bruxism and Oral Parafunctional Hyperactivity in Social Phobia Outpatients. J. Oral Rehabil. 2015;42:90–97. doi: 10.1111/joor.12235. [DOI] [PubMed] [Google Scholar]
- 127.Hilgenberg-Sydney P.B., Lorenzon A.L., Pimentel G., Petterle R.R., Bonotto D. Probable Awake Bruxism—Prevalence and Associated Factors: A Cross-Sectional Study. Dent. Press. J. Orthod. 2022;27:e2220298. doi: 10.1590/2177-6709.27.4.e2220298.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.de Holanda T.A., Marmitt L.P., Cesar J.A., Svensson P., Boscato N. Sleep Bruxism in Puerperal Women: Data from a Population-Based Survey. Matern. Child. Health J. 2023;27:262–271. doi: 10.1007/s10995-022-03576-2. [DOI] [PubMed] [Google Scholar]
- 129.Azario de Holanda T., Castagno C.D., Barbon F.J., Mota Freitas M.P., Goettems M.L., Boscato N. Influence of Respiratory Allergy and Restless Sleep on Definite Sleep Bruxism: A Cross-Sectional Clinical Study. Sleep Med. 2020;70:43–49. doi: 10.1016/j.sleep.2020.02.010. [DOI] [PubMed] [Google Scholar]
- 130.Huhtela O.S., Näpänkangas R., Suominen A.L., Karppinen J., Kunttu K., Sipilä K. Association of Psychological Distress and Widespread Pain with Sympatoms of Temporomandibular Disorders and Self-Reported Bruxism in Students. Clin. Exp. Dent. Res. 2021;7:1154–1166. doi: 10.1002/cre2.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Insana S.P., Gozal D., McNeil D.W., Montgomery-Downs H.E. Community Based Study of Sleep Bruxism during Early Childhood. Sleep Med. 2013;14:183–188. doi: 10.1016/j.sleep.2012.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Itani O., Kaneita Y., Ikeda M., Kondo S., Yamamoto R., Osaki Y., Kanda H., Suzuki K., Higuchi S., Ohida T. Disorders of Arousal and Sleep-Related Bruxism among Japanese Adolescents: A Nationwide Representative Survey. Sleep Med. 2013;14:532–541. doi: 10.1016/j.sleep.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 133.Johansson A., Unell L., Carlsson G.E., Söderfeldt B., Halling A., Widar F. Associations between Social and General Health Factors and Symptoms Related to Temporomandibular Disorders and Bruxism in a Population of 50-year-old Subjects. Acta Odontol. Scand. 2004;62:231–237. doi: 10.1080/00016350410001649. [DOI] [PubMed] [Google Scholar]
- 134.Jokubauskas L., Baltrušaitytė A., Pileičikienė G., Žekonis G. Interrelationships between Distinct Circadian Manifestations of Possible Bruxism, Perceived Stress, Chronotype and Social Jetlag in a Population of Undergraduate Students. Chronobiol. Int. 2019;36:1558–1569. doi: 10.1080/07420528.2019.1660356. [DOI] [PubMed] [Google Scholar]
- 135.de Paula Rodrigues Juliatte T., Costa P.D., Canaan J.D.R., Fonseca D.C., Serra-Negra J.M., Andrade E.F., Castelo P.M., Pereira L.J. Circadian Preference and Its Relationship with Possible Sleep and Awake Bruxism in Adults Assisted by the Public Health System. Chronobiol. Int. 2022;39:68–76. doi: 10.1080/07420528.2021.1973487. [DOI] [PubMed] [Google Scholar]
- 136.Junqueira T.H., Nahás-Scocate A.C.R., do Valle-Corotti K.M., Conti A.C.d.C.F., Trevisan S. Association of Infantile Bruxism and the Terminal Relationships of the Primary Second Molars. Braz. Oral Res. 2013;27:42–47. doi: 10.1590/S1806-83242013000100008. [DOI] [PubMed] [Google Scholar]
- 137.Kirarslan Karagoz O., Yildirim B., Tekeli Simsek A., Koca C.G., Igneci M. Possible Sleep and Awake Bruxism, Chronotype Profile and TMD Symptoms among Turkish Dental Students. Chronobiol. Int. 2021;38:1367–1374. doi: 10.1080/07420528.2021.1931279. [DOI] [PubMed] [Google Scholar]
- 138.Kataoka K., Ekuni D., Mizutani S., Tomofuji T., Azuma T., Yamane M., Kawabata Y., Iwasaki Y., Morita M. Association Between Self-Reported Bruxism and Malocclusion in University Students: A Cross-Sectional Study. J. Epidemiol. 2015;25:423–430. doi: 10.2188/jea.JE20140180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kato T., Velly A.M., Nakane T., Masuda Y., Maki S. Age Is Associated with Self-Reported Sleep Bruxism, Independently of Tooth Loss. Sleep Breath. 2012;16:1159–1165. doi: 10.1007/s11325-011-0625-7. [DOI] [PubMed] [Google Scholar]
- 140.Kaya M., Koroglu A., Sahin O. The Relationship of Psychological Status and Sociodemographic Factors with Bruxism among Undergraduate Dental Students: A National Survey. Niger. J. Clin. Pract. 2022;25:944–950. doi: 10.4103/njcp.njcp_1980_21. [DOI] [PubMed] [Google Scholar]
- 141.Khatami R., Zutter D., Siegel A., Mathis J., Donati F., Bassetti C.L. Sleep-Wake Habits and Disorders in a Series of 100 Adult Epilepsy Patients—A Prospective Study. Seizure. 2006;15:299–306. doi: 10.1016/j.seizure.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 142.Khayat N., Winocur E., Emodi Perelman A., Friedman-Rubin P., Gafni Y., Shpack N. The Prevalence of Posterior Crossbite, Deep Bite, and Sleep or Awake Bruxism in Temporomandibular Disorder (TMD) Patients Compared to a Non-TMD Population: A Retrospective Study. Cranio J. Craniomandib. Pract. 2021;39:398–404. doi: 10.1080/08869634.2019.1650217. [DOI] [PubMed] [Google Scholar]
- 143.Khoury S., Carra M.C., Huynh N., Montplaisir J., Lavigne G.J. Sleep Bruxism-Tooth Grinding Prevalence, Characteristics and Familial Aggregation: A Large Cross-Sectional Survey and Polysomnographic Validation. Sleep. 2016;39:2049–2056. doi: 10.5665/sleep.6242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kilincaslan A., Yilmaz K., Oflaz S.B., Aydin N. Epidemiological Study of Self-Reported Sleep Problems in Turkish High School Adolescents. Pediatr. Int. Off. J. Jpn. Pediatr. Soc. 2014;56:594–600. doi: 10.1111/ped.12287. [DOI] [PubMed] [Google Scholar]
- 145.Kim D.S., Lee C.L., Ahn Y.M. Sleep Problems in Children and Adolescents at Pediatric Clinics. Korean J. Pediatr. 2017;60:158–165. doi: 10.3345/kjp.2017.60.5.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kolak V., Pavlovic M., Aleksic E., Biocanin V., Gajic M., Nikitovic A., Lalovic M., Melih I., Pesic D. Probable Bruxism and Psychological Issues among Dental Students in Serbia during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2022;19:7729. doi: 10.3390/ijerph19137729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lam M.H.B., Zhang J., Li A.M., Wing Y.K. A Community Study of Sleep Bruxism in Hong Kong Children: Association with Comorbid Sleep Disorders and Neurobehavioral Consequences. Sleep Med. 2011;12:641–645. doi: 10.1016/j.sleep.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 148.Leal T.R., de Lima L.C.M., Perazzo M.F., Neves É.T.B., Paiva S.M., Serra-Negra J.M.C., Ferreira F.M., Granville-Garcia A.F. Influence of the Practice of Sports, Sleep Disorders, and Habits on Probable Sleep Bruxism in Children with Mixed Dentition. Oral Dis. 2023;29:211–219. doi: 10.1111/odi.13917. [DOI] [PubMed] [Google Scholar]
- 149.Le A., Khoo E., Palamar J.J. Associations between Oral Health and Cannabis Use among Adolescents and Young Adults: Implications for Orthodontists. Int. J. Environ. Res. Public Health. 2022;19:15261. doi: 10.3390/ijerph192215261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Levartovsky S., Msarwa S., Reiter S., Eli I., Winocur E., Sarig R. The Association between Emotional Stress, Sleep, and Awake Bruxism among Dental Students: A Sex Comparison. J. Clin. Med. 2021;11:10. doi: 10.3390/jcm11010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.de Lima L.C.M., Leal T.R., de AraúJo L.J.S., Sousa M.L.C., da Silva S.E., Serra-Negra J.M.C., Ferreira F.d.M., Paiva S.M., Granville-Garcia A.F. Impact of the COVID-19 Pandemic on Sleep Quality and Sleep Bruxism in Children Eight to Ten Years of Age. Braz. Oral Res. 2022;36:e046. doi: 10.1590/1807-3107bor-2022.vol36.0046. [DOI] [PubMed] [Google Scholar]
- 152.Liu X., Ma Y., Wang Y., Jiang Q., Rao X., Lu X., Teng H. Brief Report: An Epidemiologic Survey of the Prevalence of Sleep Disorders among Children 2 to 12 Years Old in Beijing, China. Pediatrics. 2005;115:266–268. doi: 10.1542/peds.2004-0815I. [DOI] [PubMed] [Google Scholar]
- 153.Macfarlane T.V., Blinkhorn A.S., Davies R.M., Worthington H.V. Association between Local Mechanical Factors and Orofacial Pain: Survey in the Community. J. Dent. 2003;31:535–542. doi: 10.1016/S0300-5712(03)00108-8. [DOI] [PubMed] [Google Scholar]
- 154.Maluly M., Dal Fabbro C., Andersen M.L., Herrero Babiloni A., Lavigne G.J., Tufik S. Sleep Bruxism and Its Associations with Insomnia and OSA in the General Population of Sao Paulo. Sleep Med. 2020;75:141–148. doi: 10.1016/j.sleep.2020.06.016. [DOI] [PubMed] [Google Scholar]
- 155.Manfredini D., Lobbezoo F., Giancristofaro R.A., Restrepo C. Association between Proxy-Reported Sleep Bruxism and Quality of Life Aspects in Colombian Children of Different Social Layers. Clin. Oral Investig. 2017;21:1351–1358. doi: 10.1007/s00784-016-1901-5. [DOI] [PubMed] [Google Scholar]
- 156.Manfredini D., Winocur E., Guarda-Nardini L., Lobbezoo F. Self-Reported Bruxism and Temporomandibular Disorders: Findings from Two Specialised Centres. J. Oral Rehabil. 2012;39:319–325. doi: 10.1111/j.1365-2842.2011.02281.x. [DOI] [PubMed] [Google Scholar]
- 157.Martynowicz H., Wieckiewicz M., Poreba R., Wojakowska A., Smardz J., Januszewska L., Markiewicz-Gorka I., Mazur G., Pawlas K., Gac P. The Relationship between Sleep Bruxism Intensity and Renalase Concentration—An Enzyme Involved in Hypertension Development. J. Clin. Med. 2020;9:16. doi: 10.3390/jcm9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Massignan C., de Alencar N.A., Soares J.P., Santana C.M., Serra-Negra J., Bolan M., Cardoso M. Poor Sleep Quality and Prevalence of Probable Sleep Bruxism in Primary and Mixed Dentitions: A Cross-Sectional Study. Sleep Breath. 2019;23:935–941. doi: 10.1007/s11325-018-1771-y. [DOI] [PubMed] [Google Scholar]
- 159.Melis M., Abou-Atme Y.S. Prevalence of Bruxism Awareness in a Sardinian Population. Cranio J. Craniomandib. Pract. 2003;21:144–151. doi: 10.1080/08869634.2003.11746243. [DOI] [PubMed] [Google Scholar]
- 160.Melo P.E.D., Pontes J.R.D.S. Deleterious Oral Habits in a Group of Children from a Public School in Sao Paulo City. Rev. CEFAC. 2014;16:1945–1952. doi: 10.1590/1982-0216201418213. [DOI] [Google Scholar]
- 161.Miamoto C.B., Pereira L.J., Ramos-Jorge M.L., Marques L.S. Prevalence and Predictive Factors of Sleep Bruxism in Children with and without Cognitive Impairment. Braz. Oral Res. 2011;25:439–445. doi: 10.1590/S1806-83242011000500011. [DOI] [PubMed] [Google Scholar]
- 162.Montero J., Gómez-Polo C. Personality Traits and Dental Anxiety in Self-Reported Bruxism. A Cross-Sectional Study. J. Dent. 2017;65:45–50. doi: 10.1016/j.jdent.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 163.Nagamatsu-Sakaguchi C., Minakuchi H., Clark G.T., Kuboki T. Relationship between the Frequency of Sleep Bruxism and the Prevalence of Signs and Symptoms of Temporomandibular Disorders in an Adolescent Population. Int. J. Prosthodont. 2008;21:292–298. [PubMed] [Google Scholar]
- 164.Nahás-Scocate A.C.R., Coelho F.V., Almeida V.C. de Bruxism in Children and Transverse Plane of Occlusion: Is There a Relationship or Not? Dent. Press J. Orthod. 2014;19:67–73. doi: 10.1590/2176-9451.19.5.067-073.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Nakata A., Takahashi M., Ikeda T., Hojou M., Araki S. Perceived Psychosocial Job Stress and Sleep Bruxism among Male and Female Workers. Community Dent. Oral. Epidemiol. 2008;36:201–209. doi: 10.1111/j.1600-0528.2007.00388.x. [DOI] [PubMed] [Google Scholar]
- 166.Nazzal H., Baccar M., Ziad T., Al-Musfir T., Al Emadi B., Matoug-Elwerfelli M., Narasimhan S., Khan Y., Reagu S. Prevalence of Anxiety, Sleep Bruxism and Temporomandibular Disorders during COVID-19 in Qatari Children and Adolescents: A Cross-Sectional Study. Eur. Arch. Paediatr. Dent. Off. J. Eur. Acad. Paediatr. Dent. 2023;24:787–795. doi: 10.1007/s40368-023-00847-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Nekora-Azak A., Yengin E., Evlioglu G., Ceyhan A., Ocak O., Issever H. Prevalence of Bruxism Awareness in Istanbul, Turkey. Cranio J. Craniomandib. Pract. 2010;28:122–127. doi: 10.1179/crn.2010.017. [DOI] [PubMed] [Google Scholar]
- 168.Nykänen L., Manfredini D., Lobbezoo F., Kämppi A., Bracci A., Ahlberg J. Assessment of Awake Bruxism by a Novel Bruxism Screener and Ecological Momentary Assessment among Patients with Masticatory Muscle Myalgia and Healthy Controls. J. Oral Rehabil. 2024;51:162–169. doi: 10.1111/joor.13462. [DOI] [PubMed] [Google Scholar]
- 169.Okawara A., Matsuyama Y., Yoshizawa Araki M., Unnai Yasuda Y., Ogawa T., Tumurkhuu T., Ganburged G., Bazar A., Fujiwara T., Moriyama K. Association between Child Abuse and Poor Oral Habits in Mongolian Adolescents. Int. J. Environ. Res. Public Health. 2022;19:10667. doi: 10.3390/ijerph191710667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Osses-Anguita Á.E., Sánchez-Sánchez T., Soto-Goñi X.A., García-González M., Alén Fariñas F., Cid-Verdejo R., Sánchez Romero E.A., Jiménez-Ortega L. Awake and Sleep Bruxism Prevalence and Their Associated Psychological Factors in First-Year University Students: A Pre-Mid-Post COVID-19 Pandemic Comparison. Int. J. Environ. Res. Public Health. 2023;20:2452. doi: 10.3390/ijerph20032452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Panek H., Nawrot P., Mazan M., Bielicka B., Sumisławska M., Pomianowski R. Coincidence and Awareness of Oral Parafunctions in College Students. Community Dent. Health. 2012;29:74–77. doi: 10.1922/CDH_2684Panek04. [DOI] [PubMed] [Google Scholar]
- 172.Peixoto K.O., de Resende C.M.B.M., de Almeida E.O., Almeida-Leite C.M., Conti P.C.R., Barbosa G.A.S., Barbosa J.S. Association of Sleep Quality and Psychological Aspects with Reports of Bruxism and TMD in Brazilian Dentists during the COVID-19 Pandemic. J. Appl. Oral. Sci. Rev. 2021;29:e20201089. doi: 10.1590/1678-7757-2020-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Pereira N.C., Oltramari P.V.P., Conti P.C.R., Bonjardim L.R., de Almeida-Pedrin R.R., Fernandes T.M.F., de Almeida M.R., Conti A.C.C.F. Frequency of Awake Bruxism Behaviour in Orthodontic Patients: Randomised Clinical Trial: Awake Bruxism Behaviour in Orthodontic Patients. J. Oral Rehabil. 2021;48:422–429. doi: 10.1111/joor.13130. [DOI] [PubMed] [Google Scholar]
- 174.González-Aragón Pineda Á.E., García Pérez A., Rosales-Ibáñez R., Stein-Gemora E. Relationship between the Normative Need for Orthodontic Treatment and Oral Health in Mexican Adolescents Aged 13–15 Years Old. Int. J. Environ. Res. Public Health. 2020;17:8107. doi: 10.3390/ijerph17218107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Pontes L.d.S., Prietsch S.O.M. Sleep bruxism: Population based study in people with 18 years or more in the city of Rio Grande, Brazil. Rev. Bras. Epidemiol. Braz. J. Epidemiol. 2019;22:e190038. doi: 10.1590/1980-549720190038. [DOI] [PubMed] [Google Scholar]
- 176.Prado I.M., Abreu L.G., Silveira K.S., Auad S.M., Paiva S.M., Manfredini D., Serra-Negra J.M. Study of Associated Factors with Probable Sleep Bruxism Among Adolescents. J. Clin. Sleep Med. 2018;14:1369–1376. doi: 10.5664/jcsm.7276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Prado I.M., Abreu L.G., Pordeus I.A., Amin M., Paiva S.M., Serra-Negra J.M. Diagnosis and Prevalence of Probable Awake and Sleep Bruxism in Adolescents: An Exploratory Analysis. Braz. Dent. J. 2023;34:9–24. doi: 10.1590/0103-6440202305202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Prado I.M., Paiva S.M., Fonseca-Gonçalves A., Maia L.C., Tavares-Silva C., Fraiz F.C., Ferreira F.M., Duarte J., Granville-Garcia A.F., Costa E.M.M.B., et al. Knowledge of Parents/Caregivers about the Sleep Bruxism of Their Children from All Five Brazilian Regions: A Multicenter Study. Int. J. Paediatr. Dent. 2019;29:507–523. doi: 10.1111/ipd.12486. [DOI] [PubMed] [Google Scholar]
- 179.Ramos P.F.C., de Lima M.d.D.M., de Moura M.S., Bendo C.B., Moura L. de F.A. de D.; Lima, C.C.B. Breathing Problems, Being an Only Child and Having Parents with Possible Sleep Bruxism Are Associated with Probable Sleep Bruxism in Preschoolers: A Population-Based Study. Sleep Breath. 2021;25:1677–1684. doi: 10.1007/s11325-020-02281-0. [DOI] [PubMed] [Google Scholar]
- 180.Alouda R., Alshehri M., Alnaghmoosh S., Shafique M., Al-Khudhairy M.W. Mother’s Work Status on Children’s Bruxism in a Subset of Saudi Population. J. Int. Soc. Prev. Community Dent. 2017;7:S170–S178. doi: 10.4103/jispcd.JISPCD_384_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Rao S.K., Bhat M., David J. Work, Stress, and Diurnal Bruxism: A Pilot Study among Information Technology Professionals in Bangalore City, India. Int. J. Dent. 2011;2011:650489. doi: 10.1155/2011/650489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Raphael K.G., Janal M.N., Sirois D.A., Dubrovsky B., Klausner J.J., Krieger A.C., Lavigne G.J. Validity of Self-Reported Sleep Bruxism among Myofascial Temporomandibular Disorder Patients and Controls. J. Oral Rehabil. 2015;42:751–758. doi: 10.1111/joor.12310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Rauch A., Nitschke I., Hahnel S., Weber S., Zenthöfer A., Schierz O. Prevalence of Temporomandibular Disorders and Bruxism in Seniors. J. Oral Rehabil. 2023;50:531–536. doi: 10.1111/joor.13450. [DOI] [PubMed] [Google Scholar]
- 184.Renner A.C., da Silva A.A.M., Rodriguez J.D.M., Simões V.M.F., Barbieri M.A., Bettiol H., Thomaz E.B.A.F., da Conceição Saraiva M. Are Mental Health Problems and Depression Associated with Bruxism in Children? Community Dent. Oral. Epidemiol. 2012;40:277–287. doi: 10.1111/j.1600-0528.2011.00644.x. [DOI] [PubMed] [Google Scholar]
- 185.Restrepo C., Manfredini D., Castrillon E., Svensson P., Santamaria A., Alvarez C., Manrique R., Lobbezoo F. Diagnostic Accuracy of the Use of Parental-Reported Sleep Bruxism in a Polysomnographic Study in Children. Int. J. Paediatr. Dent. 2017;27:318–325. doi: 10.1111/ipd.12262. [DOI] [PubMed] [Google Scholar]
- 186.Ribeiro M.B., Manfredini D., Tavares-Silva C., Costa L., Luiz R.R., Paiva S., Serra-Negra J.M., Fonseca-Gonçalves A., Maia L.C. Association of Possible Sleep Bruxism in Children with Different Chronotype Profiles and Sleep Characteristics. Chronobiol. Int. 2018;35:633–642. doi: 10.1080/07420528.2018.1424176. [DOI] [PubMed] [Google Scholar]
- 187.Rintakoski K., Hublin C., Lobbezoo F., Rose R.J., Kaprio J. Genetic Factors Account for Half of the Phenotypic Variance in Liability to Sleep-Related Bruxism in Young Adults: A Nationwide Finnish Twin Cohort Study. Twin Res. Hum. Genet. 2012;15:714–719. doi: 10.1017/thg.2012.54. [DOI] [PubMed] [Google Scholar]
- 188.Saczuk K., Lapinska B., Wawrzynkiewicz A., Witkowska A., Arbildo-Vega H.I., Domarecka M., Lukomska-Szymanska M. Temporomandibular Disorders, Bruxism, Perceived Stress, and Coping Strategies among Medical University Students in Times of Social Isolation during Outbreak of COVID-19 Pandemic. Healthcare. 2022;10:740. doi: 10.3390/healthcare10040740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.van Selms M.K.A., Marpaung C., Pogosian A., Lobbezoo F. Geographical Variation of Parental-Reported Sleep Bruxism among Children: Comparison between the Netherlands, Armenia and Indonesia. Int. Dent. J. 2019;69:237–243. doi: 10.1111/idj.12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Seraj B., Shahrabi M., Ghadimi S., Ahmadi R., Nikfarjam J., Zayeri F., Taghi F.P., Zare H. The Prevalence of Bruxism and Correlated Factors in Children Referred to Dental Schools of Tehran, Based on Parent’s Report. Iran. J. Pediatr. 2010;20:174–180. [PMC free article] [PubMed] [Google Scholar]
- 191.Serra-Negra J.M., Dias R.B., Rodrigues M.J., Aguiar S.O., Auad S.M., Pordeus I.A., Lombardo L., Manfredini D. Self-Reported Awake Bruxism and Chronotype Profile: A Multicenter Study on Brazilian, Portuguese and Italian Dental Students. Cranio J. Craniomandib. Pract. 2021;39:113–118. doi: 10.1080/08869634.2019.1587854. [DOI] [PubMed] [Google Scholar]
- 192.Serra-Negra J.M., Ramos-Jorge M.L., Flores-Mendoza C.E., Paiva S.M., Pordeus I.A. Influence of Psychosocial Factors on the Development of Sleep Bruxism among Children. Int. J. Paediatr. Dent. 2009;19:309–317. doi: 10.1111/j.1365-263X.2009.00973.x. [DOI] [PubMed] [Google Scholar]
- 193.Shalev-Antsel T., Winocur-Arias O., Friedman-Rubin P., Naim G., Keren L., Eli I., Emodi-Perlman A. The Continuous Adverse Impact of COVID-19 on Temporomandibular Disorders and Bruxism: Comparison of Pre- during- and Post-Pandemic Time Periods. BMC Oral Health. 2023;23:716. doi: 10.1186/s12903-023-03447-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Prakash J., Ranvijay K., Devi L.S., Shenoy M., Abdul N.S., Shivakumar G.C., Gupta P. Assessment of Symptoms Associated with Temporomandibular Dysfunction and Bruxism among Elderly Population: An Epidemiological Survey. J. Contemp. Dent. Pract. 2022;23:393–398. [PubMed] [Google Scholar]
- 195.Shokry S.M., El Wakeel E.E., Al-Maflehi N., RasRas Z., Fataftah N., Abdul Kareem E. Association between Self-Reported Bruxism and Sleeping Patterns among Dental Students in Saudi Arabia: A Cross-Sectional Study. Int. J. Dent. 2016;2016:e4327081. doi: 10.1155/2016/4327081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Sierwald I., John M.T., Schierz O., Jost-Brinkmann P.-G., Reissmann D.R. Association of Overjet and Overbite with Esthetic Impairments of Oral Health-Related Quality of Life. J. Orofac. Orthop. Fortschr. Kieferorthop. 2015;76:405–420. doi: 10.1007/s00056-015-0300-x. [DOI] [PubMed] [Google Scholar]
- 197.da Silva S.E., de Lima L.C.M., Leal T.R., Firmino R.T., Granville-Garcia A.F. Use of Electronic Devices, Practice of Sports, and Awake Bruxism in Schoolchildren Aged Eight to Ten Years. Braz. Oral Res. 2022;36:e137. doi: 10.1590/1807-3107bor-2022.vol36.0137. [DOI] [PubMed] [Google Scholar]
- 198.Tavares Silva C., Calabrio I.R., Serra-Negra J.M., Fonseca-Gonçalves A., Maia L.C. Knowledge of Parents/Guardians about Nocturnal Bruxism in Children and Adolescents. Cranio J. Craniomandib. Pract. 2017;35:223–227. doi: 10.1080/08869634.2016.1201633. [DOI] [PubMed] [Google Scholar]
- 199.de Siqueira S.R.D.T., Vilela T.T., Florindo A.A. Prevalence of Headache and Orofacial Pain in Adults and Elders in a Brazilian Community: An Epidemiological Study. Gerodontology. 2015;32:123–131. doi: 10.1111/ger.12063. [DOI] [PubMed] [Google Scholar]
- 200.Siva L., Krishnamoorthy V., Durai K.S., Shaheed Ahamed S.S., Rajakumari S., Catherine N.C. Comparative Evaluation of Body Mass Index among School Children with and without Bruxism of Age Group of 6-12 Years in Kanchipuram District: A Cross-Sectional Study. J. Indian Soc. Pedod. Prev. Dent. 2021;39:42–46. doi: 10.4103/jisppd.jisppd_523_20. [DOI] [PubMed] [Google Scholar]
- 201.Soares L.G., Costa I.R., Brum Júnior J.D.S., Cerqueira W.S.B., de Oliveira E.S., Douglas de Oliveira D.W., Gonçalves P.F., Glória J.C.R., Tavano K.T.A., Flecha O.D. Prevalence of Bruxism in Undergraduate Students. Cranio J. Craniomandib. Pract. 2017;35:298–303. doi: 10.1080/08869634.2016.1218671. [DOI] [PubMed] [Google Scholar]
- 202.Pezzini Soares J., Klein D., Ximenes M., Pereira C., Antunes E., Dias L., Borgatto A., Cardoso M., Bolan M. Mouth Breathing and Prevalence of Sleep Bruxism among Preschoolers Aged 2 to 5 Years. Pesqui. Bras. Odontopediatria Clín. Integr. 2018;18:3490–3492. doi: 10.4034/PBOCI.2018.181.46. [DOI] [Google Scholar]
- 203.Sousa H.C.S., Lima M.D., Dantas Neta N.B., Tobias R.Q., Moura M.S., Moura L.D. Prevalence and Associated Factors to Sleep Bruxism in Adolescents from Teresina, Piauí. Rev. Bras. Epidemiol. Braz. J. Epidemiol. 2018;21:e180002. doi: 10.1590/1980-549720180002. [DOI] [PubMed] [Google Scholar]
- 204.Somay E., Tekkarismaz N. Evaluation of Sleep Bruxism and Temporomandibular Disorders in Patients Undergoing Hemodialysis. Niger. J. Clin. Pract. 2020;23:1375–1380. doi: 10.4103/njcp.njcp_630_19. [DOI] [PubMed] [Google Scholar]
- 205.Souza G.L.N., Serra-Negra J.M., Prado I.M., Aguiar S.O., Hoffmam G.d.F.E.B., Pordeus I.A., Auad S.M., Abreu L.G. Association of Facial Type with Possible Bruxism and Its Related Clinical Features in Adolescents: A Cross-Sectional Study. Int. Orthod. 2020;18:758–769. doi: 10.1016/j.ortho.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 206.Suwa S., Takahara M., Shirakawa S., Komada Y., Sasaguri K., Onozuka M., Sato S. Sleep Bruxism and Its Relationship to Sleep Habits and Lifestyle of Elementary School Children in Japan. Sleep Biol. Rhythm. 2009;7:93–102. doi: 10.1111/j.1479-8425.2009.00394.x. [DOI] [Google Scholar]
- 207.Tachibana M., Kato T., Kato-Nishimura K., Matsuzawa S., Mohri I., Taniike M. Associations of Sleep Bruxism with Age, Sleep Apnea, and Daytime Problematic Behaviors in Children. Oral Dis. 2016;22:557–565. doi: 10.1111/odi.12492. [DOI] [PubMed] [Google Scholar]
- 208.Tay K.J., Ujin Y.A., Allen P.F. Impact of Sleep Bruxism on Oral Health-Related Quality of Life. Int. J. Prosthodont. 2020;33:285–291. doi: 10.11607/ijp.6782. [DOI] [PubMed] [Google Scholar]
- 209.Phuong N.T.T., Ngoc V.T.N., Linh L.M., Duc N.M., Tra N.T., Anh L.Q. Bruxism, Related Factors and Oral Health-Related Quality of Life Among Vietnamese Medical Students. Int. J. Environ. Res. Public Health. 2020;17:7408. doi: 10.3390/ijerph17207408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Tinastepe N., Iscan I. Relationship between Bruxism and Smartphone Overuse in Young Adults. Cranio J. Craniomandib. Pract. 2024;42:55–62. doi: 10.1080/08869634.2021.1909456. [DOI] [PubMed] [Google Scholar]
- 211.Toyama N., Ekuni D., Taniguchi-Tabata A., Yoneda T., Kataoka K., Yokoi A., Uchida Y., Fukuhara D., Saho H., Monirul I.M., et al. Associations between Sleep Bruxism, Sleep Quality, and Exposure to Secondhand Smoke in Japanese Young Adults: A Cross-Sectional Study. Sleep Med. 2020;68:57–62. doi: 10.1016/j.sleep.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 212.Traebert E., Nazário A., Nunes R., Margreiter S., Pereira K., Costa S., Traebert J. Prevalence of Sleep Bruxism and Association with Oral Health Conditions in Schoolchildren in a Municipality in Southern Brazil. Pesqui. Bras. Odontopediatria Clín. Integr. 2020;20:e0019. doi: 10.1590/pboci.2020.125. [DOI] [Google Scholar]
- 213.Tsuchiya M., Tsuchiya S., Momma H., Mizuno K., Nagatomi R., Yaegashi N., Arima T. Japan Environment and Children’s Study Group Prospective Association of Short Sleep Duration in Newborns with Bruxism Behavior in Children: The Japan Environment and Children’s Study (JECS) Sleep Med. 2022;100:71–78. doi: 10.1016/j.sleep.2022.07.018. [DOI] [PubMed] [Google Scholar]
- 214.Uca A.U., Uğuz F., Kozak H.H., Gümüş H., Aksoy F., Seyithanoğlu A., Kurt H.G. Antidepressant-Induced Sleep Bruxism: Prevalence, Incidence, and Related Factors. Clin. Neuropharmacol. 2015;38:227–230. doi: 10.1097/WNF.0000000000000108. [DOI] [PubMed] [Google Scholar]
- 215.Uma U., Fongpisuttikul P., Padungpipatbawon P., Luyapan P. Prevalence, Awareness, and Management of Bruxism in Thai Dental Students: A Cross-Sectional Study. Cranio J. Craniomandib. Pract. 2021 doi: 10.1080/08869634.2021.2015557. ahead-of-print . [DOI] [PubMed] [Google Scholar]
- 216.Unell L., Johansson A., Ekbäck G., Ordell S., Carlsson G.E. Prevalence of Troublesome Symptoms Related to Temporomandibular Disorders and Awareness of Bruxism in 65- and 75-Year-Old Subjects. Gerodontology. 2012;29:e772–e779. doi: 10.1111/j.1741-2358.2011.00558.x. [DOI] [PubMed] [Google Scholar]
- 217.Us M.C., Us Y.O. Evaluation of the Relationship between Sleep Bruxism and Sleeping Habits in School-Aged Children. Cranio J. Craniomandib. Pract. 2023;41:569–577. doi: 10.1080/08869634.2021.1890454. [DOI] [PubMed] [Google Scholar]
- 218.van Selms M.K.A., Visscher C.M., Naeije M., Lobbezoo F. Bruxism and Associated Factors among Dutch Adolescents. Community Dent. Oral. Epidemiol. 2013;41:353–363. doi: 10.1111/cdoe.12017. [DOI] [PubMed] [Google Scholar]
- 219.Vieira K.R.M., Folchini C.M., Heyde M.D.V.D., Stuginski-Barbosa J., Kowacs P.A., Piovesan E.J. Wake-Up Headache Is Associated with Sleep Bruxism. Headache. 2020;60:974–980. doi: 10.1111/head.13816. [DOI] [PubMed] [Google Scholar]
- 220.Vieira-Andrade R.G., Drumond C.L., Martins-Júnior P.A., Corrêa-Faria P., Gonzaga G.C., Marques L.S., Ramos-Jorge M.L. Prevalence of Sleep Bruxism and Associated Factors in Preschool Children. Pediatr. Dent. 2014;36:46–50. [PubMed] [Google Scholar]
- 221.Vlăduțu D., Popescu S.M., Mercuț R., Ionescu M., Scrieciu M., Glodeanu A.D., Stănuși A., Rîcă A.M., Mercuț V. Associations between Bruxism, Stress, and Manifestations of Temporomandibular Disorder in Young Students. Int. J. Environ. Res. Public Health. 2022;19:5415. doi: 10.3390/ijerph19095415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Wetselaar P., Vermaire E.J.H., Lobbezoo F., Schuller A.A. The Prevalence of Awake Bruxism and Sleep Bruxism in the Dutch Adult Population. J. Oral Rehabil. 2019;46:617–623. doi: 10.1111/joor.12787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Wetselaar P., Vermaire E.J.H., Lobbezoo F., Schuller A.A. The Prevalence of Awake Bruxism and Sleep Bruxism in the Dutch Adolescent Population. J. Oral Rehabil. 2021;48:143–149. doi: 10.1111/joor.13117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Winocur E., Messer T., Eli I., Emodi-Perlman A., Kedem R., Reiter S., Friedman-Rubin P. Awake and Sleep Bruxism Among Israeli Adolescents. Front. Neurol. 2019;10:443. doi: 10.3389/fneur.2019.00443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Winocur-Arias O., Winocur E., Shalev-Antsel T., Reiter S., Shifra L., Emodi-Perlman A., Friedman-Rubin P. Painful Temporomandibular Disorders, Bruxism and Oral Parafunctions before and during the COVID-19 Pandemic Era: A Sex Comparison among Dental Patients. J. Clin. Med. 2022;11:589. doi: 10.3390/jcm11030589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Yachida W., Arima T., Castrillon E.E., Baad-Hansen L., Ohata N., Svensson P. Diagnostic Validity of Self-Reported Measures of Sleep Bruxism Using an Ambulatory Single-Channel EMG Device. J. Prosthodont. Res. 2016;60:250–257. doi: 10.1016/j.jpor.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 227.Yalçın Yeler D., Yılmaz N., Koraltan M., Aydın E. A Survey on the Potential Relationships between TMD, Possible Sleep Bruxism, Unilateral Chewing, and Occlusal Factors in Turkish University Students. Cranio J. Craniomandib. Pract. 2017;35:308–314. doi: 10.1080/08869634.2016.1239851. [DOI] [PubMed] [Google Scholar]
- 228.Yıldırım B., Kırarslan Karagoz O., Tekeli Simsek A., Koca C., Cicek M.F. Associations between Self-Reported Bruxism, Sleep Quality, and Psychological Status among Dental Students in Turkey. Cranio J. Craniomandib. Pract. 2024;42:63–68. doi: 10.1080/08869634.2021.1909458. [DOI] [PubMed] [Google Scholar]
- 229.Yoshinaka M., Ikebe K., Furuya-Yoshinaka M., Hazeyama T., Maeda Y. Prevalence of Torus Palatinus among a Group of Japanese Elderly. J. Oral Rehabil. 2010;37:848–853. doi: 10.1111/j.1365-2842.2010.02100.x. [DOI] [PubMed] [Google Scholar]
- 230.Zani A., Lobbezoo F., Bracci A., Ahlberg J., Manfredini D. Ecological Momentary Assessment and Intervention Principles for the Study of Awake Bruxism Behaviors, Part 1: General Principles and Preliminary Data on Healthy Young Italian Adults. Front. Neurol. 2019;10:169. doi: 10.3389/fneur.2019.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Fan W.-Y., Tiang N., Broadbent J.M., Thomson W.M. Occurrence, Associations, and Impacts of Nocturnal Parafunction, Daytime Parafunction, and Temporomandibular Symptoms in 38-Year-Old Individuals. J. Oral Facial Pain Headache. 2019;33:254–259. doi: 10.11607/ofph.2221. [DOI] [PubMed] [Google Scholar]
- 232.Azodo C., Ojehanon P. Bruxism Experience among Undergraduates of a Nigerian University. Indian J. Multidiscip. Dent. 2016;6:14. doi: 10.4103/2229-6360.188219. [DOI] [Google Scholar]
- 233.Friedman Rubin P., Erez A., Peretz B., Birenboim-Wilensky R., Winocur E. Prevalence of Bruxism and Temporomandibular Disorders among Orphans in Southeast Uganda: A Gender and Age Comparison. Cranio J. Craniomandib. Pract. 2018;36:243–249. doi: 10.1080/08869634.2017.1331784. [DOI] [PubMed] [Google Scholar]
- 234.Shahbour S.A., Abohamila N., EL-Bayoumi M.H. Prevalence of Sleep Bruxism and Associated Factors in Tanta Preschool Children. Alex. Dent. J. 2022;47:155–162. doi: 10.21608/adjalexu.2022.72061.1187. [DOI] [Google Scholar]
- 235.Ahlberg J., Piirtola M., Lobbezoo F., Manfredini D., Korhonen T., Aarab G., Hublin C., Kaprio J. Correlates and Genetics of Self-Reported Sleep and Awake Bruxism in a Nationwide Twin Cohort. J. Oral Rehabil. 2020;47:1110–1119. doi: 10.1111/joor.13042. [DOI] [PubMed] [Google Scholar]
- 236.Ahlberg J., Lobbezoo F., Hublin C., Piirtola M., Kaprio J. Self-Reported Sleep Bruxism in 1990 and 2011 in a Nationwide Twin Cohort: Evidence of Trait Persistence and Genetic Liability. J. Oral Rehabil. 2022;51:119–124. doi: 10.1111/joor.13368. [DOI] [PubMed] [Google Scholar]
- 237.Ahlberg J., Lobbezoo F., Ahlberg K., Manfredini D., Hublin C., Sinisalo J., Könönen M., Savolainen A. Self-Reported Bruxism Mirrors Anxiety and Stress in Adults. Med. Oral Patol. Oral Cir. Bucal. 2013;18:e7–e11. doi: 10.4317/medoral.18232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Ahlberg K., Ahlberg J., Könönen M., Alakuijala A., Partinen M., Savolainen A. Perceived Orofacial Pain and Its Associations with Reported Bruxism and Insomnia Symptoms in Media Personnel with or without Irregular Shift Work. Acta Odontol. Scand. 2005;63:213–217. doi: 10.1080/00016350510019937. [DOI] [PubMed] [Google Scholar]
- 239.Ahlberg J., Savolainen A., Rantala M., Lindholm H., Könönen M. Reported Bruxism and Biopsychosocial Symptoms: A Longitudinal Study. Community Dent. Oral. Epidemiol. 2004;32:307–311. doi: 10.1111/j.1600-0528.2004.00163.x. [DOI] [PubMed] [Google Scholar]
- 240.Rintakoski K., Ahlberg J., Hublin C., Lobbezoo F., Rose R.J., Murtomaa H., Kaprio J. Tobacco Use and Reported Bruxism in Young Adults: A Nationwide Finnish Twin Cohort Study. Nicotine Tob. Res. 2010;12:679–683. doi: 10.1093/ntr/ntq066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Serra-Negra J.M., Tirsa-Costa D., Guimarães F.H., Paiva S.M., Pordeus I.A. Evaluation of Parents/Guardian Knowledge about the Bruxism of Their Children: Family Knowledge of Bruxism. J. Indian Soc. Pedod. Prev. Dent. 2013;31:153–158. doi: 10.4103/0970-4388.117965. [DOI] [PubMed] [Google Scholar]
- 242.Yoshinaka M., Ikebe K., Furuya-Yoshinaka M., Maeda Y. Prevalence of Torus Mandibularis among a Group of Elderly Japanese and Its Relationship with Occlusal Force. Gerodontology. 2014;31:117–122. doi: 10.1111/ger.12017. [DOI] [PubMed] [Google Scholar]
- 243.Colonna A., Segù M., Lombardo L., Manfredini D. Frequency of Sleep Bruxism Behaviors in Healthy Young Adults over a Four-Night Recording Span in the Home Environment. Appl. Sci. 2021;11:195. doi: 10.3390/app11010195. [DOI] [Google Scholar]
- 244.Soares J.P., Giacomin A., Cardoso M., Serra-Negra J.M., Bolan M. Association of Gender, Oral Habits, and Poor Sleep Quality with Possible Sleep Bruxism in Schoolchildren. Braz. Oral Res. 2020;34:e019. doi: 10.1590/1807-3107bor-2020.vol34.0019. [DOI] [PubMed] [Google Scholar]
- 245.Quadri M.F.A., Mahnashi A., Al Almutahhir A., Tubayqi H., Hakami A., Arishi M., Alamir A. Association of Awake Bruxism with Khat, Coffee, Tobacco, and Stress among Jazan University Students. Int. J. Dent. 2015;2015:e842096. doi: 10.1155/2015/842096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Serra-Negra J.M., Scarpelli A.C., Tirsa-Costa D., Guimarães F.H., Pordeus I.A., Paiva S.M. Sleep Bruxism, Awake Bruxism and Sleep Quality among Brazilian Dental Students: A Cross-Sectional Study. Braz. Dent. J. 2014;25:241–247. doi: 10.1590/0103-6440201302429. [DOI] [PubMed] [Google Scholar]
- 247.Serra-Negra J.M., Ribeiro M.B., Prado I.M., Paiva S.M., Pordeus I.A. Association between Possible Sleep Bruxism and Sleep Characteristics in Children. Cranio J. Craniomandib. Pract. 2017;35:315–320. doi: 10.1080/08869634.2016.1239894. [DOI] [PubMed] [Google Scholar]
- 248.Serra-Negra J.M., Lobbezoo F., Correa-Faria P., Lombardo L., Siciliani G., Stellini E., Manfredini D. Relationship of Self-Reported Sleep Bruxism and Awake Bruxism with Chronotype Profiles in Italian Dental Students. Cranio J. Craniomandib. Pract. 2019;37:147–152. doi: 10.1080/08869634.2018.1431600. [DOI] [PubMed] [Google Scholar]
- 249.Soares K.A.N., Melo R.M.C.S., Gomes M.C., Perazzo M.F., Granville-Garcia A.F., Menezes V.A. Prevalence and Factors Associated to Bruxism in Preschool Children. J. Public Health. 2016;24:209–214. doi: 10.1007/s10389-016-0713-z. [DOI] [Google Scholar]
- 250.Emodi-Perlman A., Eli I., Friedman-Rubin P., Goldsmith C., Reiter S., Winocur E. Bruxism, Oral Parafunctions, Anamnestic and Clinical Findings of Temporomandibular Disorders in Children. J. Oral Rehabil. 2012;39:126–135. doi: 10.1111/j.1365-2842.2011.02254.x. [DOI] [PubMed] [Google Scholar]
- 251.Emodi-Perlman A., Hochhauser T., Winocur P., Friedman-Rubin P., Eli I. The Effect of Smartphones on Daytime Sleepiness, Temporomandibular Disorders, and Bruxism among Young Adults. Quintessence Int. 2021;52:548–559. doi: 10.3290/j.qi.b1244431. [DOI] [PubMed] [Google Scholar]
- 252.Drumond C.L., Souza D.S., Serra-Negra J.M., Marques L.S., Ramos-Jorge M.L., Ramos-Jorge J. Respiratory Disorders and the Prevalence of Sleep Bruxism among Schoolchildren Aged 8 to 11 Years. Sleep Breath. Schlaf Atm. 2017;21:203–208. doi: 10.1007/s11325-017-1466-9. [DOI] [PubMed] [Google Scholar]
- 253.Duarte J., Serra-Negra J.M., Ferreira F.M., Paiva S.M., Fraiz F.C. Agreement between Two Different Approaches to Assess Parent-Reported Sleep Bruxism in Children. Sleep Sci. Sao Paulo Braz. 2017;10:73–77. doi: 10.5935/1984-0063.20170013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Huhtela O.S., Näpänkangas R., Joensuu T., Raustia A., Kunttu K., Sipilä K. Self-Reported Bruxism and Symptoms of Temporomandibular Disorders in Finnish University Students. J. Oral Facial Pain Headache. 2016;30:311–317. doi: 10.11607/ofph.1674. [DOI] [PubMed] [Google Scholar]
- 255.Maluly M., Andersen M.L., Dal-Fabbro C., Garbuio S., Bittencourt L., De Siqueira J.T.T., Tufik S. Polysomnographic Study of the Prevalence of Sleep Bruxism in a Population Sample. J. Dent. Res. 2013;92:S97–S103. doi: 10.1177/0022034513484328. [DOI] [PubMed] [Google Scholar]
- 256.Winocur E., Uziel N., Lisha T., Goldsmith C., Eli I. Self-Reported Bruxism—Associations with Perceived Stress, Motivation for Control, Dental Anxiety and Gagging. J. Oral Rehabil. 2011;38:3–11. doi: 10.1111/j.1365-2842.2010.02118.x. [DOI] [PubMed] [Google Scholar]
- 257.Bucci R., Manfredini D., Lenci F., Simeon V., Bracci A., Michelotti A. Comparison between Ecological Momentary Assessment and Questionnaire for Assessing the Frequency of Waking-Time Non-Functional Oral Behaviours. J. Clin. Med. 2022;11:5880. doi: 10.3390/jcm11195880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Simões-Zenari M., Bitar M.L. Factors Associated to Bruxism in Children from 4–6 Years. Pró-Fono Rev. Atualização Cient. 2010;22:465–472. doi: 10.1590/S0104-56872010000400018. [DOI] [PubMed] [Google Scholar]
- 259.Zani A., Lobbezoo F., Bracci A., Djukic G., Guarda-Nardini L., Favero R., Ferrari M., Aarab G., Manfredini D. Smartphone-Based Evaluation of Awake Bruxism Behaviours in a Sample of Healthy Young Adults: Findings from Two University Centres. J. Oral Rehabil. 2021;48:989–995. doi: 10.1111/joor.13212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Strausz T., Ahlberg J., Lobbezoo F., Restrepo C.C., Hublin C., Ahlberg K., Könönen M. Awareness of Tooth Grinding and Clenching from Adolescence to Young Adulthood: A Nine-Year Follow-Up. J. Oral Rehabil. 2010;37:497–500. doi: 10.1111/j.1365-2842.2010.02071.x. [DOI] [PubMed] [Google Scholar]
- 261.Ng E.P., Ng D.K., Chan C.H. Sleep Duration, Wake/Sleep Symptoms, and Academic Performance in Hong Kong Secondary School Children. Sleep Breath. 2009;13:357–367. doi: 10.1007/s11325-009-0255-5. [DOI] [PubMed] [Google Scholar]
- 262.Rossi D., Manfredini D. Family and School Environmental Predictors of Sleep Bruxism in Children. J. Orofac. Pain. 2013;27:135–141. doi: 10.11607/jop.1057. [DOI] [PubMed] [Google Scholar]
- 263.Dias R., Vaz R., Rodrigues M.J., Serra-Negra J.M., Bracci A., Manfredini D. Utility of Smartphone-Based Real-Time Report (Ecological Momentary Assessment) in the Assessment and Monitoring of Awake Bruxism: A Multiple-Week Interval Study in a Portuguese Population of University Students. J. Oral Rehabil. 2021;48:1307–1313. doi: 10.1111/joor.13259. [DOI] [PubMed] [Google Scholar]
- 264.Serra-Negra J.M., Paiva S.M., Seabra A.P., Dorella C., Lemos B.F., Pordeus I.A. Prevalence of Sleep Bruxism in a Group of Brazilian Schoolchildren. Eur. Arch. Paediatr. Dent. 2010;11:192–195. doi: 10.1007/BF03262743. [DOI] [PubMed] [Google Scholar]
- 265.Serra-Negra J.M., Paiva S.M., Abreu M.H., Flores-Mendoza C.E., Pordeus I.A. Relationship between Tasks Performed, Personality Traits, and Sleep Bruxism in Brazilian School Children—A Population-Based Cross-Sectional Study. PLoS ONE. 2013;8:e80075. doi: 10.1371/journal.pone.0080075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological Guidance for Systematic Reviews of Observational Epidemiological Studies Reporting Prevalence and Cumulative Incidence Data. JBI Evid. Implement. 2015;13:147. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 267.Stijnen T., Hamza T.H., Özdemir P. Random Effects Meta-Analysis of Event Outcome in the Framework of the Generalized Linear Mixed Model with Applications in Sparse Data. Stat. Med. 2010;29:3046–3067. doi: 10.1002/sim.4040. [DOI] [PubMed] [Google Scholar]
- 268.Schwarzer G., Chemaitelly H., Abu-Raddad L.J., Rücker G. Seriously Misleading Results Using Inverse of Freeman-Tukey Double Arcsine Transformation in Meta-Analysis of Single Proportions. Res. Synth. Methods. 2019;10:476–483. doi: 10.1002/jrsm.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Agresti A., Coull B.A. Approximate Is Better than “Exact” for Interval Estimation of Binomial Proportions. Am. Stat. 1998;52:119–126. doi: 10.2307/2685469. [DOI] [Google Scholar]
- 270.Higgins J.P.T., Thompson S.G. Quantifying Heterogeneity in a Meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 271.Belsley D.A., Kuh E., Welsch R.E. Regression Diagnostics: Identifying Influential Data and Sources of Collinearity. 1st ed. Wiley; Hoboken, NJ, USA: 1980. (Wiley Series in Probability and Statistics). [Google Scholar]
- 272.Cook R.D., Weisberg S. Residuals and Influence in Regression. Chapman and Hall; New York, NY, USA: 1982. [Google Scholar]
- 273.Hedges L.V., Olkin I. Statistical Methods for Meta-Analysis. 1st ed. Academic Press; Orlando, FL, USA: 1985. [Google Scholar]
- 274.Viechtbauer W. Conducting Meta-Analyses in R with the Metafor Package. J. Stat. Softw. 2010;36:1–48. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 275.Viechtbauer W., Cheung M.W.-L. Outlier and Influence Diagnostics for Meta-Analysis. Res. Synth. Methods. 2010;1:112–125. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- 276.Schmid C.H., Stijnen T., White I.R. In: Handbook of Meta-Analysis. 1st ed. Schmid C.H., Stijnen T., White I., editors. Taylor and Francis; Boca Raton, FL, USA: 2020. Chapman and Hall/CRC: First Edition. Chapman & Hall/CRC Handbooks of Modern Statistical Methods. [Google Scholar]
- 277.Egger M., Smith G.D., Schneider M., Minder C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Balduzzi S., Rücker G., Schwarzer G. How to Perform a Meta-Analysis with R: A Practical Tutorial. Evid. Based Ment. Health. 2019;22:153–160. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Harrer M., Cuijpers P., Furukawa T., Ebert D. Dmetar: Companion R Package for the Guide ‘Doing Meta-Analysis in R’ (R Package Version 0.0.9000) [(accessed on 16 November 2023)]. Available online: https://dmetar.protectlab.org/
- 280.Makowski D., Lüdecke D., Patil I., Thériault R., Ben-Shachar M., Wiernik B. Automated Results Reporting as a Practical Tool to Improve Reproducibility and Methodological Best Practices Adoption. [(accessed on 16 November 2023)]. Available online: https://easystats.github.io/report/
- 281.Sjoberg D.D., Whiting K., Curry M., Lavery J.A., Larmarange J. Reproducible Summary Tables with the Gtsummary Package. R J. 2021;13:570. doi: 10.32614/RJ-2021-053. [DOI] [Google Scholar]
- 282.Wickham H., François R., Henry L., Müller K., Vaughan D. PBC Dplyr: A Grammar of Data Manipulation. 2023. [(accessed on 20 March 2024)]. Available online: https://dplyr.tidyverse.org/
- 283.Revelle W. Psych: Procedures for Psychological, Psychometric, and Personality Research. Elsevier; Amsterdam, The Netherlands: 2024. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.