Abstract
Introduction
ALZ-801/valiltramiprosate is a small-molecule oral inhibitor of beta amyloid (Aβ) aggregation and oligomer formation being studied in a phase 2 trial in APOE4 carriers with early Alzheimer’s disease (AD) to evaluate treatment effects on fluid and imaging biomarkers and cognitive assessments.
Methods
The single-arm, open-label phase 2 trial was designed to evaluate the effects of the ALZ-801 265 mg tablet taken twice daily (after 2 weeks once daily) on plasma fluid AD biomarkers, hippocampal volume (HV), and cognition over 104 weeks in APOE4 carriers. The study enrolled subjects aged 50–80 years, with early AD [Mini-Mental State Examination (MMSE) ≥ 22, Clinical Dementia Rating-Global (CDR-G) 0.5 or 1], apolipoprotein E4 (APOE4) genotypes including APOE4/4 and APOE3/4 genotypes, and positive cerebrospinal fluid (CSF) AD biomarkers or prior amyloid scans. The primary outcome was plasma p-tau181, HV evaluated by magnetic resonance imaging (MRI) was the key secondary outcome, and plasma Aβ42 and Aβ40 were the secondary biomarker outcomes. The cognitive outcomes were the Rey Auditory Verbal Learning Test and the Digit Symbol Substitution Test. Safety and tolerability evaluations included treatment-emergent adverse events and amyloid-related imaging abnormalities (ARIA). The study was designed and powered to detect 15% reduction from baseline in plasma p-tau181 at the 104-week endpoint. A sample size of 80 subjects provided adequate power to detect this difference at a significance level of 0.05 using a two-sided paired t-test.
Results
The enrolled population of 84 subjects (31 homozygotes and 53 heterozygotes) was 52% females, mean age 69 years, MMSE 25.7 [70% mild cognitive impairment (MCI), 30% mild AD] with 55% on cholinesterase inhibitors. Plasma p-tau181 reduction from baseline was significant (31%, p = 0.045) at 104 weeks and all prior visits; HV atrophy was significantly reduced (p = 0.0014) compared with matched external controls from an observational Early AD study. Memory scores showed minimal decline from baseline over 104 weeks and correlated significantly with decreased HV atrophy (Spearman’s 0.44, p = 0.002). Common adverse events were COVID infection and mild nausea, and no drug-related serious adverse events were reported. Of 14 early terminations, 6 were due to nonserious treatment-emergent adverse events and 1 death due to COVID. There was no vasogenic brain edema observed on MRI over 104 weeks.
Conclusions
The effect of ALZ-801 on reducing plasma p-tau181 over 2 years demonstrates target engagement and supports its anti-Aβ oligomer action that leads to a robust decrease in amyloid-induced brain neurodegeneration. The significant correlation between reduced HV atrophy and cognitive stability over 2 years suggests a disease-modifying effect of ALZ-801 treatment in patients with early AD. Together with the favorable safety profile with no events of vasogenic brain edema, these results support further evaluation of ALZ-801 in a broader population of APOE4 carriers, who represent two-thirds of patients with AD.
Trial Registration
Key Points
| The study enrolled patients with early Alzheimer’s disease (AD), enriched for amyloid pathology by both APOE4 genotype (APOE4 carriers) and positive cerebrospinal fluid biomarkers of AD. |
| Subjects treated with oral ALZ-801 265 mg twice daily showed significant reduction of plasma p-tau181, a marker of brain neurodegeneration, starting at 13 weeks and sustained at every visit through 104 weeks. |
| Compared with matched external control, hippocampal volume (HV) measurements showed decreased atrophy, and memory tests showed stability that correlated significantly with the HV effects. |
| Safety was favorable with no drug-related serious adverse events and no vasogenic edema, supporting the promising benefit–risk profile of ALZ-801 in APOE4 carriers with early AD. |
Introduction
Alzheimer’s disease (AD), the most common form of dementia, currently affects 6.9 million individuals in the USA alone [1]. After aging, carriage of the ε4 allele of apolipoprotein E (APOE4) is the strongest risk factor for AD, with a pronounced gene-dose effect [2–4]. Monoclonal anti-amyloid antibody lecanemab is currently the only anti-amyloid treatment, which has received traditional US Food and Drug Administration (FDA) approval for the treatment of early AD [5]. Lecanemab and other anti-amyloid antibodies are associated with vascular injuries called amyloid-related imaging abnormalities (ARIA) that can be detected on magnetic resonance imaging (MRI) as either brain edema (ARIA-E) or microhemorrhages and/or hemosiderosis (ARIA-H) [6–8]. ARIA is caused by antibody-induced inflammation and clearance of insoluble amyloid plaques and mature fibrils from amyloid-laden vessels affected by cerebral amyloid angiopathy (CAA), mostly found in superficial cortical and penetrating meningeal vessels [9, 10]. APOE4 is also a risk factor for CAA and markedly increases the incidence and severity of ARIA in APOE4 carriers [11–13]. Therefore, the development of AD treatments that can alleviate the risk of ARIA adverse events is a major unmet medical need, especially in APOE4 carriers.
ALZ-801/valiltramiprosate is an oral, highly brain-penetrant agent that is being developed as a disease-modifying agent for patients with early AD [14–16]. Tramiprosate, the active moiety in ALZ-801, inhibits the formation of soluble neurotoxic amyloid oligomers [17–19]. Valiltramiprosate is a prodrug, composed of tramiprosate conjugated to valine, developed to provide improved oral absorption, more consistent pharmacokinetic properties, and reduced gastrointestinal side-effects, as demonstrated in several phase 1 studies [20].
ALZ-801 is being evaluated in a pivotal phase 3 trial in APOE4/4 homozygotes with early AD (APOLLOE4, NCT04770220). This 78-week study enrolled 325 subjects and will report topline results in the second half of 2024. The APOE4/4 population was selected for the first target indication as APOE4/4 homozygotes showed promising clinical benefits and no events of ARIA side effects in APOE4 carriers in a 78-week phase 3 trial of tramiprosate, the active agent in ALZ-801 [21, 22]. The consistent clinical benefits of tramiprosate with a clear dose response in APOE4/4 patients with AD provided confidence in initiating a phase 3 trial with a bioequivalent oral dose of ALZ-801. In addition, very high penetrance of AD pathology in semidominant fashion has been described in APOE4/4 homozygotes in recent studies, including high levels of amyloid pathology and soluble oligomers, the mechanistic target of ALZ-801 [11, 23–26].
In the APOE4 heterozygous subgroup, the tramiprosate clinical effects were less consistent and did not exhibit a clear dose response, requiring further investigation before proceeding into phase 3 trials [22]. The phase 2 biomarker study of ALZ-801 was therefore designed to provide evidence of target engagement with the same dose of ALZ-801 (265 mg BID) in APOE4 carriers, including both APOE4/4 (HM) and APOE3/4 heterozygotes (HT). At the time of study design, the AD clinical research criteria required evidence of amyloid pathology on either positron emission tomography (PET) scans or cerebrospinal fluid (CSF) biomarkers [27–29]. Therefore, enrollment in the study required positive CSF amyloid and tau biomarkers. More recently, the AD research criteria were expanded to include the use of plasma biomarkers to confirm an AD diagnosis [30]. CSF and, more recently, plasma p-tau181 levels were shown to be good biomarkers of amyloid-induced neurotoxicity, for tracking AD pathology and for evaluating target engagement of potential treatments, and correlate with tau pathology and disease progression [31–34]. At the time of study initiation, CSF assays for p-tau181 and Aβ42 and 40 were available, and the study’s initial primary outcome was CSF p-tau181. More recently, plasma assays of these biomarkers became available and are now commonly used in AD studies since they are easier to collect and monitor in both longitudinal drug intervention trials and in clinical practice. Over the last 2 years, amyloid antibodies that showed significant efficacy also reported significant p-tau181 reduction between 15% and 22% over 78 weeks [5, 35]. Although the clinical correlations of p-tau effects are not fully understood at present, future cumulative data from this and various other trials may provide further insights into these clinical correlations.
Methods
Protocol Approval and Informed Consent
The study protocol was submitted to the US FDA as part of the Investigational New Drug application for ALZ-801 and complies with the World Medical Association Declaration of Helsinki. The study was conducted at seven sites in the Czech Republic and the Netherlands, after approval of the clinical trial applications by each health authority. The study protocol and informed consents were also approved by the Independent Ethics Committee at each study center, and all patients and/or their legal representatives and study partners provided written informed consent. The trial was conducted in accordance with the International Council for Harmonization (ICH) Guideline for Good Clinical Practice (GCP) and all applicable local regulatory requirements.
Inclusion Criteria
The study enrolled female and male subjects, aged 50–80 years with clinical diagnosis of either mild cognitive impairment (MCI) or mild AD [36, 37] with Mini-Mental State Examination (MMSE) ≥ 22, Clinical Dementia Rating Global (CDR-G) of 0.5 (MCI) or CDR-G of 1 (mild AD), with either APOE4/4 HM or APOE3/4 HT genotypes. Stable cholinesterase inhibitors were allowed, but memantine was exclusionary, since its use in the European Union (EU) is restricted to more advanced stages of AD with MMSE scores < 18. Subjects fulfilling the initial clinical criteria, and with stable medical conditions and a glomerular filtration rate (GFR) ≥ 40 ml/min, underwent brain MRI to exclude significant abnormalities other than those consistent with AD. Severe white matter disease (Fazekas grade 3), ARIA-E, and hemosiderosis > 1 cm were exclusionary. Subjects with > 10 microhemorrhages were allowed after sponsor approval. Subjects were required to have positive amyloid PET or CSF biomarkers fulfilling A/T criteria in the prior 12 months [27] or screening CSF tests that showed A+/T+ profile, namely ratio of Aβ42/40 × 10 < 0.61 and p-tau181 > 61 pg/ml; or if p-tau181 was between 50 and 61 pg/ml, then a ratio of p-tau181/Aβ42 > 0.11 was required.
Study Design, Dosing Regimen, and Study Visits
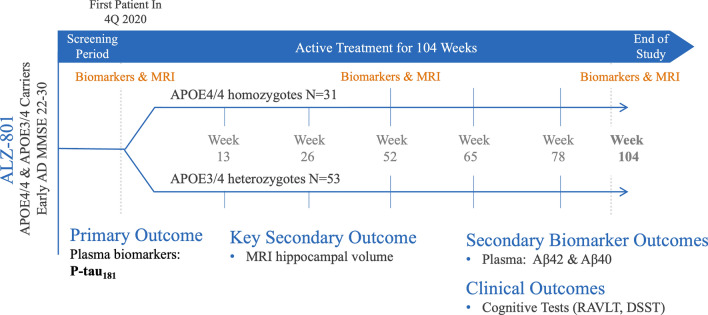
Study design is shown in Fig. 1. The study was designed to show ≥ 15% reduction from baseline of plasma p-tau181 at 104 weeks as the primary efficacy outcome. The plasma biomarkers were measured (in pg/ml) at baseline, visits at 13, 26, 52, 78, and 104 weeks. It was estimated that ~ 80 subjects would provide at least 80% power to show significant plasma p-tau181 effects at two-sided significance level of 0.05 based on the one-sample t-test of change from baseline. This sample size also provides adequate power to detect adverse events with incidence of 2–5%. After completion of the core study, a long-term extension for an additional 104 weeks was added to allow long-term assessment of biomarker, efficacy, and safety outcomes. The study’s secondary fluid biomarkers were plasma amyloid beta (Aβ), namely Aβ42 and Aβ40. CSF biomarkers were exploratory outcomes. Hippocampal volume (HV) was the key secondary outcome; cortical thickness and other brain volumes were secondary imaging outcomes. Two cognitive scales were additional clinical outcomes. Subjects received ALZ-801 265 mg oral tablet once daily for 2 weeks followed by twice-daily dosing with ALZ-801 immediate-release tablets to be taken with meals, for the rest of the study. Subjects underwent CSF and MRI testing at screening/baseline, 52 and 104 weeks. Cognitive testing occurred at 13, 26, 52, 78, and 104 weeks. Plasma biomarkers, safety assessments, and MMSE occurred every 13 weeks. The number of subjects who were screened, randomized, and completed 104 weeks is shown in Fig. 2.
Fig. 1.
Phase 2 study design, visit schedule, and outcomes. The study was designed to enroll 80 subjects with early AD with APOE4/4 and APOE3/4 genotypes and positive CSF AD biomarkers (A+/T+). Early AD included subjects with MCI (MMSE > 26) and those with mild AD (MMSE 22-26); 84 subjects were enrolled (31 APOE4/4; 53 APOE3/4), and all received ALZ-801 at 265 mg BID dose for 104 weeks. The schedule of assessments is described in Sect. 2.3. Aβ amyloid beta, AD Alzheimer’s disease, APOE apolipoprotein E, CSF cerebrospinal fluid, DSST digit symbol substitution test, MMSE Mini-Mental State Examination, MRI magnetic resonance imaging, RAVLT Rey Auditory Verbal Learning Test
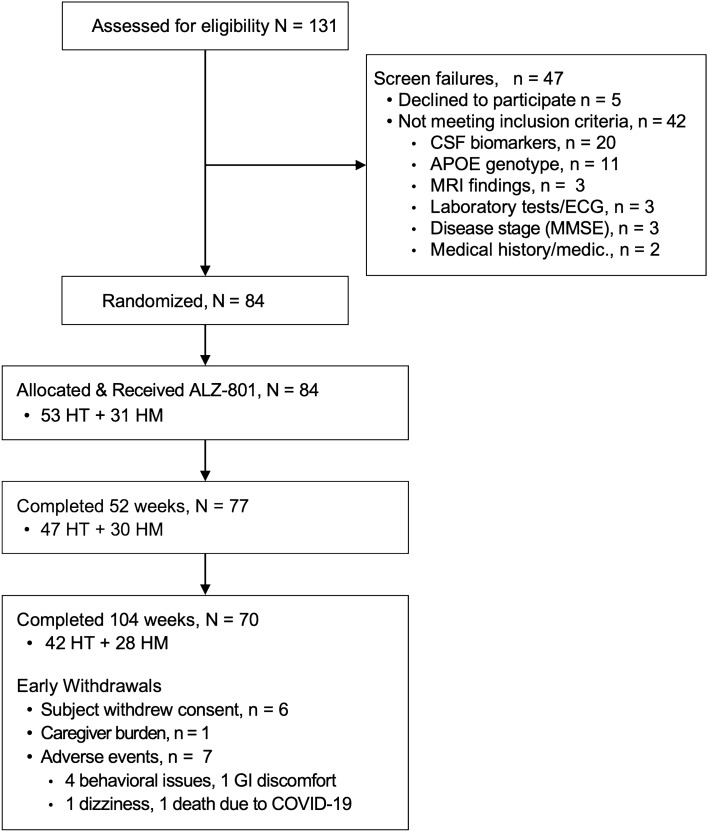
Fig. 2.
Screening, randomization, and follow-up (CONSORT diagram for ALZ-801-201): number of subjects screened, randomized, and those completing 52 and 104 weeks of the study. Medic medications, HT APOE3/4 heterozygotes, HM APOE4/4 homozygotes
Fluid Biomarker Analyses
All fluid biomarker analyses were performed in batched samples at the laboratory of Dr. Blennow (Molndal, Sweden) blinded to subjects’ clinical information. Screening CSF tests for Aβ42, Aβ40, and p-tau181 were analyzed using Lumipulse (Fujirebio assay). Plasma Aβ42 and Aβ40 used the Euroimmun ELISA assay, and p-tau181 was analyzed using a Simoa assay [38]. The screening CSF assays were required for enrollment and were therefore conducted in batches over several months during the screening period. The serial CSF biomarker assessments (screening/baseline, 52 and 104 weeks) were conducted in batches across the various timepoints, at the end of study. The serial plasma biomarkers were similarly analyzed in batches at the end of study, to minimize the effects of assay variability.
Volumetric MRI Analyses (vMRI)
Brain MRIs were performed using either 1.5 or 3 Tesla scanners. The MRI acquisition protocols used standardized Alzheimer’s Disease Neuroimaging Initiative (ADNI) methods. Analyses of volumetric MRI (vMRI) data for HV, cortical thickness, ventricular volume, and whole brain volume were conducted by the central imaging vendor, Clario Inc., using the same analytical protocols as previously reported [39, 40]. Hippocampal volume changes were calculated using both tensor-based-morphometry (TBM) and boundary shift integral (BSI). Cortical thickness was measured using FreeSurfer, and the Mayo AD signature region of interest (ROI) was calculated [39].
Cognitive Outcomes
Two main clinical outcomes were utilized to evaluate cognitive status including episodic and working memory. The first, the Rey Auditory Verbal Learning Test (RAVLT), is a test of hippocampal function that requires subjects to learn a list of 15 words over 5 trials. The immediate recall score is the sum of total words recalled over five trials (maximum score 75), and delayed recall is performed 20 min later (maximum score 15). The RAVLT—total score is the sum of immediate and delayed scores, and the maximum score is 90 [41, 42].
The second cognitive test, the digit symbol substitution test (DSST), is a timed test that measures processing speed and working memory and requires matching nine symbols with nine corresponding numbers for a total of 125 correct items over 2 min (maximum score 125 correct); normal scores of 48 for ages 70–80 years and 57 for ages 60–70 years. The DSST requires engaging wider cortical networks beyond the temporal lobe [43].
The Mini-Mental State Examination (MMSE) was used as a staging instrument for enrollment. The MMSE is a brief cognitive test that assesses orientation, immediate and delayed recall, attention and calculation, language and comprehension, and visual–spatial skills. It is an 11-item test that is used in AD studies, with higher scores indicating better performance, with a maximum score of 30 [44].
Use of External Control from the ADNI-1 Study
To compare the HV and cognitive effects of ALZ-801 with an untreated control, we utilized publicly available data from the ADNI-1 observational study [45]. We selected a matching group from ADNI using the inclusion criteria of the phase 2 study, including age 50–80 years, APOE4/4 or APOE3/4 genotypes, MMSE ≥ 22, and CDR-G > 0. Data were available for HV and other vMRI measures, and for RAVLT—total memory scores and DSST scores at 52 and 104 weeks.
A total of 151 ADNI subjects who fulfilled these criteria were included in the matching and comparative analyses with the phase 2 study.
The ADNI-1 study (N = 819) included three groups: cognitively normal (CN) (n = 229), subjects with MCI (n = 398), and subjects with mild AD dementia (n = 192), and most underwent APOE4 genotyping. ADNI studies allow use of symptomatic AD drugs, including cholinesterase inhibitors (ChEi) and memantine [45]. No disease-modifying agents were allowed. The ADNI-1 clinical measures include the cognitive and functional tests used in the phase 2 study. The vMRI protocol of ADNI and the phase 2 study are identical, and both were analyzed by our central neuroimaging vendor (Clario, formerly Bioclinica). Although the phase 2 study sites are EU-based, the investigators in the Netherlands and the Czech Republic are established AD experts who have participated in global AD drug trials. They are also versed with AD clinical scales and underwent specific scale training at the beginning of the study. Although ADNI-1 had a CSF substudy, CSF biomarkers were not required for enrollment [45], and the CSF biomarker tests were first-generation assays. The current CSF assays have advanced considerably in performance
Statistical Analysis
A statistical analysis plan (SAP) was completed prior to database lock of the 104-week dataset in June 2023. The final SAP defined the primary outcome as plasma p-tau181 and the key secondary outcome as hippocampal volume, and other plasma and imaging biomarkers and the clinical outcomes were secondary or additional outcomes. As per the protocol, an interim analysis was conducted for the 52-week dataset and presented at the 2022 CTAD conference [46]. No corrections for multiplicity testing were conducted for the main 104-week analysis. Primary and secondary analyses were conducted on the full analysis set (FAS), which included data from all subjects who had a baseline assessment, received at least one dose of ALZ-801, and provided any post-dose valid outcome measure. The primary plasma biomarker change from baseline analysis was conducted on observed data using a Student’s t-test. Comparisons of HV and cognitive effects to the ADNI control cohort utilized a mixed-effects model for repeated measures (MMRM) method with baseline age, MMSE, APOE4 genotype, use of ChEi, study (untreated or treated) group, visit, study-by-visit interactions, and the baseline measure as covariates; subjects were treated as random effects. Baseline head size was included as a covariate for vMRI endpoints. Correlations of HV and cognitive effects utilized a Spearman’s correlation coefficient. HV linear regression slope analysis was determined as the best-fit line based on HV data over 2 years. As such, the linear regression slope analysis is a measure of steepness and is calculated as “rise over run,” or change in y over the change in x.
Safety Analyses
Safety was evaluated by the incidence of treatment emergent adverse events (TEAE) and by safety laboratory tests, electrocardiogram (ECG), and brain MRIs with sequences that allow ARIA detection. TEAE are shown by Preferred Term according to MedDRA Version 23.1. Samples for drug levels in CSF and plasma (sparse sampling) will be used for future pharmacokinetic (PK) or safety analyses. COVID virus confirmation testing was completed for symptomatic subjects by primary care physicians.
Results
A total of 131 subjects were screened for this phase 2 study, of whom 110 proceeded to have screening/baseline MRI and 108 had baseline CSF testing. A total of 84 subjects (31 HM and 53 HT) fulfilled all entry criteria and were enrolled (Fig. 2). The demographics and baseline values of the Safety Set are presented in Table 1. The mean age was 69 years with 52% female, 37% were homozygotes, mean MMSE was 25.7, with 57% in mild impairment category (MMSE 22–26) and 43% considered to have MCI, and 55% were on stable cholinesterase inhibitor treatments. The ADNI-matched cohort (151 subjects) had the following baseline characteristics: mean age 72 years with 38% female, 30% homozygotes, and mean MMSE 26.2, with 48% considered to have MCI by investigators, and 18% were on cholinesterase inhibitor treatments. All data shown for the outcome measures are mean ± standard error of the mean (SEM).
Table 1.
Demographics and baseline characteristics of enrolled population
| Characteristics | Baseline values (N = 84) |
|---|---|
| Age (years) | 69.0 (5.4) |
| % Female | 52% |
| MMSE | 25.7 (2.6) |
| MCI | 70% |
| Mild AD | 30% |
| MMSE > 26 | 43% |
| MMSE 22–26 | 57% |
| CDR-Global | 0.58 (0.18) |
| Cholinesterase inhibitor use | 55% |
| Plasma biomarkers (pg/ml) | |
| Plasma p-tau181 | 13.4 ± 2.0 |
| Plasma Aβ42 | 28.4 ± 0.8 |
| Plasma Aβ40 | 144.1 ± 4.3 |
| Clinical and imaging measures | |
| RAVLT-Total | 30.1 (13.0) |
| RAVLT-Immediate | 27.1 (10.6) |
| RAVLT-Delayed | 3.0 (3.2) |
| DSST | 38.3 (18.3) |
| Hippocampal volume (ml) | 6.80 (1.04) |
AD Alzheimer’s disease, CDR-G Clinical Dementia Rating Scale-Global Score, DSST digit symbol substitution test, MCI mild cognitive impairment, MMSE Mini-Mental State Examination, RAVLT Rey Auditory Verbal Learning Test, RAVLT—total score RAVLT—immediate memory score + RAVLT—delayed memory score
Data shown for the outcome measures are mean ± standard error of the mean (SEM) or percentages
Primary Outcome: Plasma p-tau181
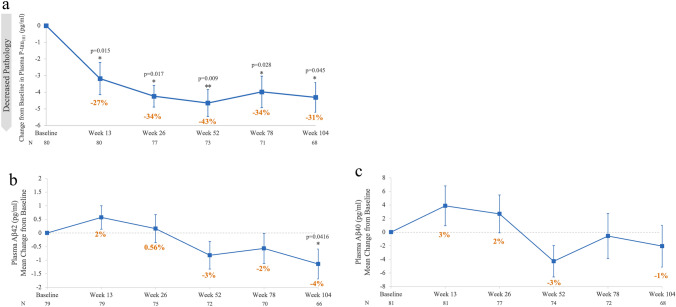
The mean baseline p-tau181 was 13.4 ± 2.0 pg/ml. Plasma p-tau181 showed a significant 31% reduction from baseline (p = 0.045) at 104 weeks. At 13, 26, 52, and 78 weeks, the reductions were 27%, 34%, 43%, and 34% respectively, all p < 0.03 (Fig. 3a).
Fig. 3.
Plasma biomarker changes from baseline over 104 weeks of ALZ-801 treatment. a Plasma p-tau181 change from baseline at each study visit (observed case analysis). The p values are for LS mean difference in the change from baseline at each visit with SEM. b Plasma Aβ42 change from baseline at each study visit (observed case analysis). The p-values are for LS mean difference in the change from baseline at each visit with SEM. c Plasma Aβ40 changes from baseline (144.1 pg/ml) at each study visit (observed case analysis). The LS means for changes from baseline were not significant at any visit with SEM. % CBL, VisitX value − baseline value/baseline value × 100; N number of subjects at each visit, LS mean least squares means, SEM standard error of the mean; * p < 0.05, ** p < 0.01, *** p < 0.001
Secondary Fluid Biomarker Outcomes: Plasma Aβ42 and Aβ40
The mean plasma Aβ42 level at baseline was 28.4 ± 0.8 pg/ml and showed an initial numerical increase from baseline to 13 weeks followed by a progressive decrease below baseline to a significant 4% decrease at 104 weeks (p = 0.042), as shown in Fig. 3b. Mean plasma Aβ40 at baseline was 144.1 ± 4.3 pg/ml, and showed a biphasic response to ALZ-801 treatment with an early increase over 13–26 weeks followed by a decrease and a return to a new level below baseline; however, these effects were not statistically significant (Fig. 3c).
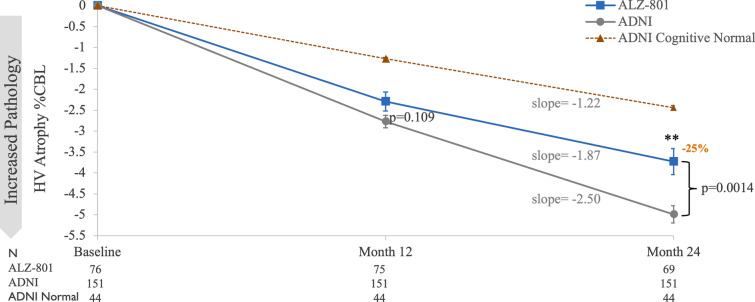
Imaging Outcome (Key Secondary Outcomes): Hippocampal Volume
At baseline, the mean bilateral hippocampal volume (HV) was 6.80 ± 1.06 ml. HV declined significantly from baseline by 3.6% over 104 weeks (Fig. 4). The ADNI-1-matched cohort had a lower baseline HV (N = 151, HV 6.04 ± 0.99 ml), and also declined significantly over 104 weeks by 5.06%. Compared with the ADNI-1-matched cohort, subjects on ALZ-801 showed a trend to decreased atrophy at 52 weeks (p = 0.109) that became statistically significant at 104 weeks (p = 0.0014), as shown in Fig. 4. These differences represent ~ 25% reduction in HV atrophy in the ALZ-801-treated arm. The slope analysis of HV atrophy using linear regression showed a slope of − 1.87 in the ALZ-801 arm compared with − 2.50 for the matched ADNI group, displaying a slowing of HV atrophy in subjects treated with ALZ-801. To provide further context for the HV changes, Fig. 4 also shows the ADNI group of APOE4 HM and HT subjects with normal cognition, who also show progressive but less steep HV atrophy reaching 2% at 2 years even at the presymptomatic phase. In ADNI APOE4 carriers, the early AD group displayed a faster rate of HV atrophy compared with the cognitively normal group (slope of − 1.22), reflecting acceleration of hippocampal atrophy at the symptomatic phase of AD. Other secondary volumetric measures, including cortical thickness and whole brain volumes, will be presented in a second dedicated manuscript that will also include their correlations with cognitive outcomes.
Fig. 4.
Hippocampal volume (HV) change from baseline in ALZ-801-treated group compared with matched ADNI control at 52 and 104 weeks (MMRM analysis). The ALZ-801 arm is for the phase 2 group with valid HV measures. The ADNI arm is for the matched APOE4/4 and APOE3/4 subjects with early AD. The dashed line is for the ADNI arm of APOE4/4 and APOE3/4 subjects with normal cognition (not part of formal MMRM analysis, shown for clinical context). The p values are for the LS mean difference in the % change from baseline. The % reductions in HV atrophy are calculated as: VisitX value − baseline value/baseline value × 100; N number of subjects with HV measure from each group, AD Alzheimer’s disease, ADNI Alzheimer’s Disease Neuroimaging Initiative, LS mean least squares means, MMRM mixed-effects model for repeated measures. * p < 0.05, ** p < 0.01, *** p < 0.001
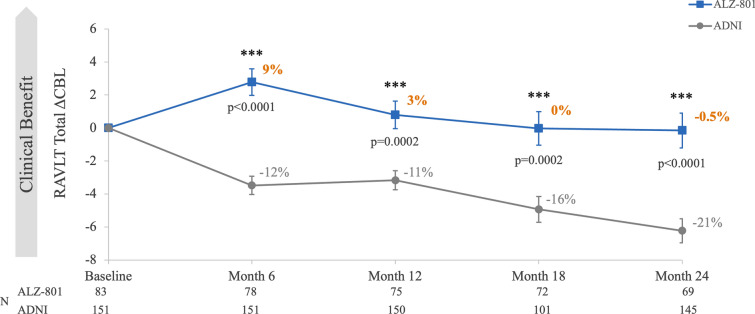
Cognitive Outcomes: RAVLT and DSST
At baseline, the RAVLT—total memory score (sum of immediate and delayed memory scores) was 30.1 ± 1.4. The RAVLT—total score showed significant improvement from baseline to 26 weeks (% change), then decreased but stayed close to baseline level at 104 weeks (Fig. 5). The ADNI-1-matched cohort, which started at the same RAVLT—total score (N = 151, score 30.1 ± 0.9) showed progressive decrease over 104 weeks, reaching ~ 21% decrease from baseline. Compared with the control arm, in subjects treated with ALZ-801, RAVLT—total scores were significantly higher (better) at each visit as shown in Fig. 5. In the ALZ-801 arm, the DSST showed minimal decline from baseline at 52 weeks and 104 weeks (observed case analysis < 2% and < 7%, respectively, p values not significant). Of note, in subjects treated with ALZ-801, HV effects correlated significantly with the cognitive benefits at 104 weeks, with Spearman’s correlation coefficients of 0.44 (p = 0.0002) for RAVLT—total, and 0.38 (p = 0.002) for DSST tests.
Fig. 5.
Changes from baseline in RAVLT—total scores in ALZ-801-treated group compared with matched ADNI control at each visit (MMRM analysis). The ALZ-801 arm is the phase 2 group with an RAVLT—total score at any post-baseline visit. The ADNI arm is from the matched APOE4/4 and APOE3/4 subjects with early AD with RAVLT—total score at any post-baseline visit. The p values are for the LS mean difference in the % change from baseline. The % change from baseline for each group is calculated as VisitX value − baseline value/baseline value × 100; N number of subjects with RAVLT—total score from each group, ADNI Alzheimer’s Disease Neuroimaging Initiative, MMRM mixed-effects model for repeated measures, RAVLT Rey Auditory Verbal Learning Test. * p < 0.05, ** p < 0.01, *** p < 0.001
Safety
Of 84 enrolled subjects, 84 completed 6 weeks, 83 completed 13 weeks, and 80, 77, and 70 completed 26, 52, and 104 weeks, respectively (Fig. 2). The incidence of treatment-emergent adverse events (TEAE) with incidence > 5% is presented in Table 2. The most common TEAE with incidence > 10% were COVID infection, nausea, and urinary tract infections. This study was initiated and conducted during the COVID pandemic, and all COVID infections were reported as not related to the study drug. Most nausea events were mild and showed tolerance with continued treatment. Of 14 withdrawals, 7 were due to TEAE that included one death due to COVID infection (not related to study drug), 4 subjects with psychiatric symptoms, 1 with dizziness, and 1 with gastrointestinal symptoms. There were no drug-related serious adverse events. The safety laboratory tests and ECG showed no abnormal patterns, and there was no evidence of organ toxicity with long-term treatment. A total of 78 subjects had at least one post-baseline MRI scan. There were no events of ARIA-E (vasogenic edema) in subjects treated with ALZ-801 over 2 years.
Table 2.
Summary of treatment-emergent adverse events (TEAE) with incidence > 5%, shown by decreasing incidence
| Preferred Term | Safety population N = 84 | Incidence (%) |
|---|---|---|
| Unique subjects with at least one TEAE | 72 | 86 |
| COVID-19 infection | 26 | 31 |
| Nausea | 19 | 23 |
| UTI | 9 | 11 |
| Vomiting | 8 | 9.5 |
| Decreased appetite | 8 | 9.5 |
| Anxiety | 7 | 8 |
| Weight decreased | 6 | 7 |
| Fall | 5 | 6 |
| Insomnia | 5 | 6 |
| Back pain | 5 | 6 |
| Hypertension | 5 | 6 |
Incidence of TEAE included any subject that received at least one dose of study drug. Coding of TEAE Preferred Terms per MedDRA version 23.1.
MedDRA Medical Dictionary for Regulatory Activities, UTI urinary tract infection
Discussion
This phase 2 biomarker study was designed to inform the development of ALZ-801 in the broader population of APOE4 carriers, which represents ~ 65% of all patients with AD [1, 4]. Previous data with the active tramiprosate moiety had shown consistent positive effects on three clinical outcomes in APOE4/4 homozygotes with mild AD that provided the rationale for conducting the phase 3 APOLLOE4 trial in APOE4/4 homozygotes [21, 22]. In the same tramiprosate study, the effects on the APOE3/4 heterozygote subjects showed nominally significant effects on the composite cognitive/functional Clinical Dementia Rating-Sum of Boxes (CDR-SB) [47], but the cognitive effects were less pronounced. Importantly, the previous tramiprosate studies enrolled subjects solely on the basis of clinical criteria and did not include biomarker confirmation of AD, which were not yet available at the time of the trial. In contrast, this phase 2 study enrolled subjects with CSF biomarker confirmation, which is the current standard for AD clinical trials [27].
The lack of a placebo arm is a limitation of this study. The open-label design was determined to be reasonable since the main outcomes were the changes from baseline status in objective fluid and imaging biomarkers, and the effects on plasma p-tau181 were expected to be a decrease from baseline versus the natural increase with disease progression. In contrast, the hippocampal volume and clinical effects were expected to show slowing of the natural decline in these measures; therefore, the drug effects on clinical and imaging outcomes required a comparator arm. In the absence of an internal comparator arm with similar baseline characteristics, we utilized the observational ADNI-1 study [45]. The ADNI-1 cohort served as an external control arm for the purpose of comparisons, with adjustment for baseline differences using an MMRM analysis that incorporates the appropriate baseline variables as covariates. This provided clinical context for the interpretation of the volumetric and clinical effects of ALZ-801. However, the use of matching analyses in selecting the external control and the statistical adjustments may not fully correct for inherent differences between the two cohorts. Another limitation of the study was the unequal distribution of subjects between the two genotypes and the lack of stratification within these two genotypes. Although the study was intended to enroll approximately 40 subjects of each APOE4 genotype, the majority of study subjects were APOE3/4 heterozygotes (53) and only 31 were APOE4/4 homozygotes, thus potentially limiting the ability to adequately compare the biomarker effects between the two genotypes.
In AD pathology-enriched APOE4 carriers, oral ALZ-801 showed significant effects on the primary and key secondary outcomes over 2 years of treatment. ALZ-801 showed early and sustained significant reduction of plasma p-tau181 and plasma Aβ42 levels over 2 years, suggesting alleviation of neurodegeneration due to toxic effects of soluble amyloid oligomers. The fluid biomarker effects were accompanied by reduced hippocampal atrophy compared with the matched group of APOE4 carriers with early AD from the ADNI-1 study. Hippocampal volume is an established marker of disease progression in AD [39, 48] and reflects the neurodegenerative index “N” of the A/T/N biomarker diagnostic framework for AD [27, 49]. The effects of ALZ-801 on CSF biomarkers are presented and discussed in a dedicated paper using a quantitative systems pharmacology (QSP) model [57]. The learning and memory tests showed an initial benefit at 26 weeks and then subsequent clinical stabilization that was significantly correlated with the decreased hippocampal atrophy in individual subjects. Despite enrolling APOE4 carrier subjects with a high burden of CAA, two major risk factors for ARIA, no brain edema (ARIA-E) was detected over 2 years of ALZ-801 treatment.
These results are further strengthened by their biological plausibility as they can be explained by the molecular mechanism of action of ALZ-801 that has been confirmed in multiple studies [17–19]. The inhibition of Aβ42 oligomer formation maintains amyloid in soluble monomeric form that can be cleared by the brain’s multiple homeostatic clearance mechanisms, including the glymphatic system [16, 50]. The biphasic time course of the plasma Aβ effects can be explained by this potential mechanism. More than 80% of the Aβ42 pool in the plasma originates from peripheral organs [51]. Therefore, the 4% reduction of plasma Aβ42 over 2 years corresponds to an appreciable amount (~ 20%) of brain Aβ42 clearance to the systemic circulation.
The lack of ARIA brain edema or vascular complications in patients treated with ALZ-801 is consistent with the lack of interaction with insoluble amyloid plaques in the vessel wall. Acute plaque clearance by anti-amyloid antibodies and associated vascular inflammation led to brain edema and microhemorrhage in clinical trials, in particular in the setting of CAA, which overlaps with AD and is more pronounced in APOE4 carriers. In a transgenic mouse model, chronic treatment with tramiprosate, the active agent in ALZ-801, showed clearance of Aβ from both brain parenchyma and vasculature without evidence of peri-plaque or perivascular inflammation. [52]. Such clearance of vascular amyloid without inducing inflammation may allow vascular repair and be an attractive attribute of ALZ-801, warranting its evaluation in patients with CAA who suffer from an increased risk of hemorrhagic strokes and/or cognitive decline.
A major strength of the phase 2 biomarker study that evaluated long-term treatment with oral ALZ-801 is that it has enrolled an APOE4 carrier population that is genetically enriched with amyloid pathology, with biomarker-confirmed AD and high levels of CSF p-tau181. p-tau181 is a marker of amyloid-induced neuronal injury, and this study population carries a high burden of both amyloid and tau pathologies [31, 33, 53] and would be expected to show substantial cognitive and biomarker decline over 2 years at the early AD stage [32, 54].
In addition, this study allowed enrollment of subjects with a high burden of microhemorrhages (> 10) that indicates underlying cerebral amyloid angiopathy [11]. These subjects are typically excluded from amyloid-antibody trials owing to their increased risk of ARIA [5, 35, 55]. The boxed warning of lecanemab’s prescribing information highlights the risk of ARIA in APOE4/4 patients with AD. Similarly, the appropriate use recommendations for lecanemab also warn about risk of ARIA in APOE4 AD carriers [56].
Conclusions
This positive trial evaluating oral ALZ-801 in APOE4 patients with early AD achieved its primary efficacy endpoint of reduction in plasma p-tau181 over 2 years, suggesting a robust decrease in amyloid-induced brain neurodegeneration and target engagement.
Despite enrolling subjects with a high burden of CAA, no ARIA-E brain edema was detected over 2 years of treatment and the long-term safety and tolerability of ALZ-801 was favorable. The significant biomarker and imaging effects and the cognitive stabilization over 2 years, especially in the absence of symptomatic ARIA events, are encouraging in a population that otherwise shows relentless progression of the disease and limited treatment options.
Compelling clinical effects and safety profile of oral ALZ-801/valiltramiprosate also support the initiation of a phase 3 trial in APOE4 carriers with early AD. The plasma biomarker and HV effects may help in the selection of surrogate measures for future prevention studies in presymptomatic AD. A well-tolerated oral agent with a simple dosing regimen would be optimal for presymptomatic individuals who may require life-long treatment. These positive phase 2 results increase confidence in the outcome of the ongoing pivotal APOLLOE4 phase 3 trial in APOE4/4 patients that may allow regulatory approval in this high-risk AD population. APOLLOE4 phase 3 topline data in APOE4/4 patients are expected in 2024.
Declarations
Funding
This research was funded by Alzheon, Inc.
Conflict of Interest
J.A.H., S.A.S., P.K., A.A., J.P., J.F.S., A.P., and M.T. are employees of Alzheon Inc. and hold stocks or stock options in Alzheon Inc. L.S. and X.Z. are employees of Wuxi Apptec that provides statistical contracting services to Alzheon Inc. K.B., E.M.R., J.H., and K.S. are scientific advisors to Alzheon Inc. and hold stocks or stock options in Alzheon Inc. N.D.P. is an investigator in the phase 2 and phase 3 studies of ALZ-801.
Ethical Approval
The protocol was approved by the assigned ethics committees (EC) in the Netherlands and in Czech Republic and by some institutional EC in the Czech Republic.
Consent to Participate
All subjects and their partners, caregivers, or legal representatives signed informed consent before participation in the study.
Consent for Publication
Not applicable.
Availability of Data and Material
ADNI datasets are publicly available at the website http//ADNI.LONI.USC.edu. The ALZ-801 data are proprietary to Alzheon Inc.
Code Availability
Not applicable.
Author Contributions
J.A.H., S.A.S., and A.P. created the study concept and design; K.B., E.M.R., J.H., and K.S. provided advice on study design or biomarker selection; S.A.S., P.K., J.A.H., A.P., J.P., and L.S. wrote the protocol; S.A.S. and J.A.H. selected the study sites and oversaw the study conduct; N.D.P. provided oversight of study enrollment and conduct; S.A.S. and P.K. oversaw subject safety; J.A.H., J.P., and J.F.S. oversaw the laboratory and biomarker sample workstream and drug supply; S.A.S. and J.A.H. wrote the manuscript; S.A.S., J.A.H., A.P., P.K., A.A., P.K., J.F.S., L.S., X.Z., and M.T. reviewed the manuscript and provided substantial edits. All authors have read and approve the final submitted manuscript and agree to be accountable for the work
References
- 1.Alzheimer’s Association Facts and Figures. 2024. https://www.alz.org/media/Documents/alzheimers-facts-and-figures.pdf.
- 2.Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993;261(5123):921–3. 10.1126/science.8346443. 10.1126/science.8346443 [DOI] [PubMed] [Google Scholar]
- 3.Roses AD. Apolipoprotein E alleles as risk factors in Alzheimer’s disease. Annu Rev Med. 1996;47:387–400. 10.1146/annurev.med.47.1.387. 10.1146/annurev.med.47.1.387 [DOI] [PubMed] [Google Scholar]
- 4.Ward A, Crean S, Mercaldi CJ, Collins JM, Boyd D, Cook MN, et al. Prevalence of Apolipoprotein E4 genotype and homozygotes (APOE e4/4) among patients diagnosed with alzheimer’s disease: a systematic review and meta-analysis. Neuroepidemiology. 2012;38:1–17. 10.1159/000334607. 10.1159/000334607 [DOI] [PubMed] [Google Scholar]
- 5.van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388:9–21. 10.1056/NEJMoa2212948. 10.1056/NEJMoa2212948 [DOI] [PubMed] [Google Scholar]
- 6.Sperling RA, Jack CR Jr, Black SE, Frosch MP, Greenberg SM, Hyman BT, et al. Amyloid-related imaging abnormalities in amyloid-modifying therapeutic trials: Recommendations from the Alzheimer’s Association Research Roundtable Workgroup. Alzheimers Dement. 2011;7:367–85. 10.1016/j.jalz.2011.05.2351. 10.1016/j.jalz.2011.05.2351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hampel H, Elhage A, Cho M, Apostolova LG, Nicoll JAR, Atri A. Amyloid-related imaging abnormalities (ARIA): radiological, biological and clinical characteristics. Brain. 2023;146:4414–24. 10.1093/brain/awad188. 10.1093/brain/awad188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barakos J, Purcell D, Suhy J, Chalkias S, Burkett P, Marsica Grassi C, et al. Detection and management of amyloid- related imaging abnormalities in patients with Alzheimer’s disease treated with anti-amyloid beta therapy. J Prev Alzheimers Dis. 2022;9:211–20. 10.14283/jpad.2022.21. 10.14283/jpad.2022.21 [DOI] [PubMed] [Google Scholar]
- 9.Wilcock DM, Rojiani A, Rosenthal A, Subbarao S, Freeman MJ, Gordon MN, et al. Passive immunotherapy against Aβ in aged APP-transgenic mice reverses cognitive deficits and depletes parenchymal amyloid deposits in spite of increased vascular amyloid and microhemorrhage. J Neuroinflamm. 2004;1:24. 10.1186/1742-2094-1-24. 10.1186/1742-2094-1-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greenberg SM, Bacskai BJ, Hernandez-Guillamon M, Pruzin J, Sperling R, van Veluw SJ. Cerebral amyloid angiopathy and Alzheimer disease—one peptide, two pathways. Nat Rev Neurol. 2020;16:30–42. 10.1038/s41582-019-0281-2. 10.1038/s41582-019-0281-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rannikmäe K, Kalaria RN, Greenberg SM, Chui HC, Schmitt FA, Samarasekera N, et al. APOE associations with severe CAA-associated vasculopathic changes: collaborative meta-analysis. J Neurol Neurosurg Psychiatry. 2014;85:300–5. 10.1136/jnnp-2013-306485. 10.1136/jnnp-2013-306485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jansen WJ, Janssen O, Tijms BM, Vos SJB, Ossenkoppele R, Visser PJ, et al. Prevalence estimates of amyloid abnormality across the Alzheimer disease clinical spectrum. JAMA Neurol. 2022;79:228–43. 10.1001/jamaneurol.2021.5216. 10.1001/jamaneurol.2021.5216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Withington CG, Turner RS. Amyloid-related imaging abnormalities with anti- amyloid antibodies for the treatment of dementia due to Alzheimer’s disease. Front Neurol. 2022;13: 862369. 10.3389/fneur.2022.862369. 10.3389/fneur.2022.862369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tolar M, Abushakra S, Hey JA, Porsteinsson A, Sabbagh M. Aducanumab, gantenerumab, BAN2401, and ALZ-801-the first wave of amyloid-targeting drugs for Alzheimer’s disease with potential for near term approval. Alzheimers Res Ther. 2020;12(1):95. 10.1186/s13195-020-00663-w. 10.1186/s13195-020-00663-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tolar M, Hey J, Power A, Abushakra S. Neurotoxic soluble amyloid oligomers drive Alzheimer’s pathogenesis and represent a clinically validated target for slowing disease progression. Int J Mol Sci. 2021;22(12):6355. 10.3390/ijms22126355. 10.3390/ijms22126355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tolar M, Hey JA, Power A, Abushakra S. The single toxin origin of Alzheimer’s disease and other neurodegenerative disorders enables targeted approach to treatment and prevention. Int J Mol Sci. 2024;25(5):2727. 10.3390/ijms25052727. 10.3390/ijms25052727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kocis P, Tolar M, Yu J, Sinko W, Ray S, Blennow K, et al. Elucidating the abeta42 anti-aggregation mechanism of action of tramiprosate in Alzheimer’s disease: integrating molecular analytical Methods, pharmacokinetic and clinical data. CNS Drugs. 2017;31(6):495–509. 10.1007/s40263-017-0434-z. 10.1007/s40263-017-0434-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hey JA, Kocis P, Hort J, Abushakra S, Power A, Vyhnalek M, et al. Discovery and identification of an endogenous metabolite of tramiprosate and its prodrug ALZ-801 that inhibits beta amyloid oligomer formation in the human brain. CNS Drugs. 2018;32(9):849–61. 10.1007/s40263-018-0554-0. 10.1007/s40263-018-0554-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang C, Savinov SN, Fejzo J, Eyles SJ, Chen J. Modulation of amyloid-beta42 conformation by small molecules through nonspecific binding. J Chem Theory Comput. 2019;15(10):5169–74. 10.1021/acs.jctc.9b00599. 10.1021/acs.jctc.9b00599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hey JA, Yu JY, Versavel M, Abushakra S, Kocis P, Power A, et al. Clinical pharmacokinetics and safety of ALZ-801, a novel prodrug of tramiprosate in development for the treatment of Alzheimer’s disease. Clin Pharmacokinet. 2018;57(3):315–33. 10.1007/s40262-017-0608-3. 10.1007/s40262-017-0608-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abushakra S, Porsteinsson A, Vellas B, Cummings J, Gauthier S, Hey JA, et al. Clinical benefits of tramiprosate in Alzheimer’s disease are associated with higher number of APOE4 alleles: the “APOE4 gene-dose effect.” J Prev Alz Dis. 2016;3(4):219–28. 10.14283/jpad.2016.115. 10.14283/jpad.2016.115 [DOI] [PubMed] [Google Scholar]
- 22.Abushakra S, Porsteinsson A, Scheltens P, Sadowsky C, Vellas B, Cummings J, et al. Clinical effects of tramiprosate in APOE4/4 homozygous patients with mild Alzheimer’s disease suggest disease modification potential. J Prev Alzeimers Dis. 2017;4(3):149–56. 10.14283/jpad.2017.26. 10.14283/jpad.2017.26 [DOI] [PubMed] [Google Scholar]
- 23.Hashimoto T, Serrano-Pozo A, Hori Y, Adams KW, Takeda S, Banerji AO, et al. Apolipoprotein E, especially apolipoprotein E4, increases the oligomerization of amyloid peptide. J Neurosci. 2012;32:15181–92. 10.1523/JNEUROSCI.1542-12.2012. 10.1523/JNEUROSCI.1542-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fleisher AS, Chen K, Liu X, Ayutyanont N, Roontiva A, Thiyyagura P, et al. Apolipoprotein E ε4 and age effects on florbetapir positron emission tomography in healthy aging and Alzheimer disease. Neurobiol Aging. 2013;34:1–12. 10.1016/j.neurobiolaging.2012.04.017. 10.1016/j.neurobiolaging.2012.04.017 [DOI] [PubMed] [Google Scholar]
- 25.Jansen WJ, Ossenkoppele R, Knol DL, Tijms BM, Scheltens P, Verhey FRJ, et al. Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA. 2015;313:1939–49. 10.1001/jama.2015.4669. 10.1001/jama.2015.4669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fortea J, Pegueroles J, Alcolea D, Belbin O, Dols-Icardo O, Vaque-Alcazar L, et al. APOE4 homozygozity represents a distinct genetic form of Alzheimer’s disease. Nat Med. 2024;30(5):1284–91. 10.1038/s41591-024-02931-w. 10.1038/s41591-024-02931-w [DOI] [PubMed] [Google Scholar]
- 27.Jack CR, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimer’s Dement. 2018;14:535–62. 10.1016/j.jalz.2018.02.018. 10.1016/j.jalz.2018.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hansson O, Seibyl J, Stomrud E, Zetterberg H, Trojanowski JQ, Bittner T, et al. CSF biomarkers of Alzheimer’s disease concord with amyloid-β PET and predict clinical progression: a study of fully automated immunoassays in BioFINDER and ADNI cohorts. Alzheimers Dement. 2018;14:1470–81. 10.1016/j.jalz.2018.01.010. 10.1016/j.jalz.2018.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hansson O. Biomarkers for neurodegenerative diseases. Nat Med. 2021;27:954–63. 10.1038/s41591-021-01382-x. 10.1038/s41591-021-01382-x [DOI] [PubMed] [Google Scholar]
- 30.Jack CR, et al. Revised criteria for diagnosis and staging of Alzheimer's disease: Alzheimer’s Association Workgroup. 2023. [DOI] [PMC free article] [PubMed]
- 31.Mattsson-Carlgren N, Andersson E, Janelidze S, Ossenkoppele R, Insel P, Strandberg O, et al. Aβ deposition is associated with increases in soluble and phosphorylated tau that precede a positive Tau PET in Alzheimer’s disease. Sci Adv. 2020;6(16):eaaz2387. 10.1126/sciadv.aaz2387. 10.1126/sciadv.aaz2387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moscoso A, Grothe MJ, Ashton NJ, Karikari TK, Lantero Rodríguez J, Snellman A, et al. Longitudinal associations of blood phosphorylated tau181 and neurofilament light chain with neurodegeneration in Alzheimer’s disease. JAMA Neurol. 2021;78(4):396–406. 10.1001/jamaneurol.2020.4986. 10.1001/jamaneurol.2020.4986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karikari TK, Pascoal TA, Ashton NJ, Janelidze S, Benedet AL, Rodriguez JL, et al. Blood phosphorylated tau 181 as a biomarker for Alzheimer’s disease: a diagnostic performance and prediction modelling study using data from four prospective cohorts. Lancet Neurol. 2020;19:422–33. 10.1016/s1474-4422(20)30071-5. 10.1016/s1474-4422(20)30071-5 [DOI] [PubMed] [Google Scholar]
- 34.Therriault J, Vermeiren M, Servaes S, Tissot C, Zimmer ER, Benedet AL, et al. Association of phosphorylated tau biomarkers with amyloid-PET vs with tau-PET. JAMA Neurol. 2022;80(2):188–99. 10.1001/jamaneurol.2022.4485. 10.1001/jamaneurol.2022.4485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Budd Haeberlein S, Aisen PS, Barkhof F, Chalkias S, Chen T, Cohen S, et al. Two randomized phase 3 studies of aducanumab in early Alzheimer’s disease. J Prev Alzheimers Dis. 2022;9(2):197–210. 10.14283/jpad.2022.30. 10.14283/jpad.2022.30 [DOI] [PubMed] [Google Scholar]
- 36.McKhann G, Knopman DS, Chertkow H, Hymann B, Jack CR, Kawas C, et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9. 10.1016/j.jalz.2011.03.005. 10.1016/j.jalz.2011.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement. 2011;7:270–9. 10.1016/j.jalz.2011.03.008. 10.1016/j.jalz.2011.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blennow K, Galasko D, Perneczky R, Quevenco FC, van der Flier WM, Akinwonmi A, et al. The potential clinical value of plasma biomarkers in Alzheimer’s disease. Alzheimers Dement. 2023;19:5805–16. 10.1002/alz.13455. 10.1002/alz.13455 [DOI] [PubMed] [Google Scholar]
- 39.Abushakra S, Porsteinsson AP, Sabbagh M, Bracoud L, Schaerer J, Power A, et al. APOE ε4/ε4 homozygotes with early Alzheimer’s disease show accelerated hippocampal atrophy and cortical thinning that correlates with cognitive decline. Alzheimers Dement (N Y). 2020;6(1): e12117. 10.1002/trc2.12117. 10.1002/trc2.12117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abushakra S, Mandelbaum R, Barakos J, Scheltens P, Porsteinsson AP, Watson D, et al. Prevalence of amyloid-related imaging abnormalities in APOE4/4 homozygotes with early Alzheimer’s disease (AD): baseline findings from ongoing clinical trials of the oral anti-amyloid agent ALZ-801 (valiltramiprosate) (P5–6.003). Neurology. 2023. 10.1212/WNL.000000000020355. 10.1212/WNL.000000000020355 [DOI] [Google Scholar]
- 41.Wechsler D. Wechsler adult intelligence scale-revised manual. New York: The Psychological Corporation; 1981. [Google Scholar]
- 42.Lezak MD, Howieson DB, Loring DW. Neuropsychological assessment. 4th ed. New York: Oxford University Press; 2004. [Google Scholar]
- 43.Salthouse TA. The role of memory in the age decline in digit-symbol substitution performance. J Gerontol. 1978;33:232–8. 10.1093/geronj/33.2.232. 10.1093/geronj/33.2.232 [DOI] [PubMed] [Google Scholar]
- 44.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. 10.1016/0022-3956(75)90026-6. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 45.Petersen RC, Aisen PS, Beckett LA, Donohue MC, Gamst AC, Harveyet DJ, et al. Alzheimer’s disease neuroimaging initiative (ADNI): clinical characterization. Neurology. 2010;74:201–9. 10.1212/WNL.0b013e3181cb3e25. 10.1212/WNL.0b013e3181cb3e25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abushakra S. Effects of oral ALZ-801 on plasma and MRI biomarkers in APOE4 carriers with Early AD: 52-week analysis from Phase 2 biomarker study. San Francisco: Clinical Trials on Alzheimer’s Disease (CTAD); 2022. [Google Scholar]
- 47.O’Bryant SE, Waring SC, Cullum CM, Hall J, Lacritz L, Massman PJ, et al. Staging dementia using Clinical Dementia Rating Scale Sum of Boxes scores: a Texas Alzheimer’s research consortium study. Arch Neurol. 2008;65(8):1091–5. 10.1001/archneur.65.8.1091. 10.1001/archneur.65.8.1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mungas D, Harvey D, Reed BR, Jagust WJ, DeCarli C, Beckett L, et al. Longitudinal volumetric MRI change and rate of cognitive decline. Neurology. 2005;65:565–71. 10.1212/01.wnl.0000172913.88973.0d. 10.1212/01.wnl.0000172913.88973.0d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Angioni D, Hansson O, Bateman RJ, Rabe C, Toloue M, Braunstein JB, et al. Can we use blood biomarkers as entry criteria and for monitoring drug treatment effects in clinical trials? A report from the EU/US CTAD Task Force. J Prev Alzheimers Dis. 2023;10:418–25. 10.14283/jpad.2023.68. 10.14283/jpad.2023.68 [DOI] [PubMed] [Google Scholar]
- 50.Tarasoff-Conway J, Carare RO, Osorio RS, Glodzik L, Butler T, Fieremans E, et al. Clearance systems in the brain - implications for Alzheimer disease. Nat Rev Neurol. 2015;11(8):457–70. 10.1038/nrneurol.2015.119. 10.1038/nrneurol.2015.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roher AE, Esh CL, Kokjohn TA, Castaño EM, Van Vickle GD, Kalback WM, et al. Aβ peptides in human plasma and tissues and their significance for Alzheimer’s disease. Alzheimers Dement. 2009;5(1):18–29. 10.1016/j.jalz.2008.10.004. 10.1016/j.jalz.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gervais F, Paquette J, Morissette C, Krzywkowski P, Yu M, Azzi M, et al. Targeting soluble Aβ peptide with Tramiprosate for the treatment of brain amyloidosis. Neurobiol Aging. 2007;28:537–47. 10.1016/j.neurobiolaging.2023.04.003. 10.1016/j.neurobiolaging.2023.04.003 [DOI] [PubMed] [Google Scholar]
- 53.Cogswell PM, Lundt ES, Therneau TM, Wiste HJ, Graff-Radford J, Algeciras-Schimnich A, et al. Modeling the temporal evolution of plasma p-tau in relation to amyloid beta and tau PET. Alzheimers Dement. 2024;20(2):1225–38. 10.1002/alz.13539. 10.1002/alz.13539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.La Joie R, Visani AV, Lesman-Segev OH, Baker SL, Edwards L, Iaccarino L, et al. Association of APOE4 and clinical variability in Alzheimer disease with the pattern of tau- and amyloid-PET. Neurology. 2021;96(5):e650–61. 10.1212/WNL.0000000000011270. 10.1212/WNL.0000000000011270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sims JR, Zimmer JA, Evans CD, Lu M, Ardayfio P, Sparks J, et al. Donanemab in early symptomatic Alzheimer disease: the TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA. 2023;330(6):512–27. 10.1001/jama.2023.13239. 10.1001/jama.2023.13239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cummings JL, Apostolova L, Rabinovici GD, Atri A, Aisen P, Greenberg S, et al. Lecanemab: appropriate use recommendations. J Prev Alzheimers Dis. 2023;10(3):362–77. 10.14283/jpad.2023.30. 10.14283/jpad.2023.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hey JA, Yu JY, Abushakra S, Schaefer JF, Power A, Kesslak P, et al. Analysis of cerebrospinal fluid, plasma β-amyloid biomarkers and cognition from 2-year phase 2 trial evaluating oral ALZ-801/valiltramiprosate in APOE4 carriers with early Alzheimer’s disease using quantitative systems pharmacology model. Drugs 2024;84. 10.1007/s40265-024-02068-7. [DOI] [PMC free article] [PubMed]