Technology means applied science. Health technology is defined as the drugs, devices, and medical and surgical procedures used in the prevention, diagnosis, treatment, and rehabilitation of disease.1
Many countries regulate pharmaceuticals and medical devices and equipment by law. This legislation concerns safety and efficacy—that is, that the risk of a technology is acceptable and that it actually does what it is supposed to do. For all other technologies, such as medical and surgical procedures, there are generally no regulations.
Summary points
Health technology includes not only equipment, pharmaceuticals, and medical devices but also surgical and medical procedures
Most countries regulate drugs and devices by law, by payment, or by placement of services—a new, multidisciplinary research called health technology assessment assists policy makers on matters of the medical, economic, social, and ethical implications of the disseminationand use of health technology
Health technology assessment synthesises the findings from clinical research and includes analysis of costs, cost effectiveness, and broader social aspects of health technology
Most countries in the European Union have established agencies for health technology assessment to provide evidence based information to health policymakers
The development of a variety of health technologies, including effective diagnostic devices (for example, radiography, computed tomography), effective pharmaceuticals (for example, antibiotics), and other interventions, represents major improvements in the history of medicine—not long ago there was little to offer patients in the way of effective health care. Until recently almost any health technology was welcome both for scientific achievements and as potential solutions to diseases.2 Many technologies, however, have not turned out to be important advances. On the contrary, some have the potential for doing more harm than good—for example, mass screening for prostate cancer and all the treatments used to immobilise patients with back pain.3
The rapid development of new and costly, although often effective, health technology such as coronary artery bypass grafting raises many concerns. For example, new technology is often viewed as the culprit behind rising healthcare costs.4
New technology may expand the temporary limits of medicine and eventually the indications for how the technology is used, for which treatment of mild hypertension or the use of genetics in diagnosis may be good examples.5 This increases the expectations and demands of the general public, patients, and providers of care. What technology promises must, however, be balanced against the limited resources for health care, and it should include assessments of the comparative value of new versus established technology.
There is a need, and indeed a movement, for evidence based and unbiased information about the consequences of the introduction of new health technologies. This seems to be a rather strong and persistent concern shared by all interested parties including manufacturers, researchers, clinicians, health policy makers, patients, and the general public.6 The challenges are by no means restricted to issues of the technical capability of health technology. Rather they are about value for money, equity, access, and quality of care including questions of financing and payment for effective health services.
Development and dissemination
Demand and supply of technology largely determine both the development and dissemination of new health technology. The forces behind technological change are many including wishes to provide health benefits to the patients, to explore, and to do research. Research in general is international, and innovations from the biomedical research community recognise no borders between countries. The biomedical industry is also increasingly multinational, operating and competing in global markets. It may take many years to develop a new medical technology, but once it is done the technology is made immediately commercially available essentially anywhere in the world.7
To a certain extent governments may control the development of health technology by funding and coordinating medical research and by their mandate to license physicians and thereby determine the number of health professionals. Yet their ability to influence through market forces seems more feasible through exercising some control over the dissemination of technology.
Regulation by payment
An array of measures explicitly launched to control rising expenditures for health care, but also implicitly to control the dissemination of technology, have been developed in different countries. Examples include the many mechanisms of paying for health care, for allocating a given budget, and of paying for the utilisation of specialised services. Health planning sometimes includes the control of technology by such programmes as certificate of need, accreditation procedures of hospitals and laboratories, quality assurance, and the development of guidelines.
The most powerful means of mastering the dissemination of technology seems to be through fiscal restriction; by global budgeting and particularly by limiting hospital budgets.8,9 The way providers of health care are paid is also a potent instrument for managing healthcare technology.10
Capitation payment schemes are used to varying extents in nearly all countries. Prospective payment systems on the basis of a fixed price per diagnosis which, in principle, does not change when additional services are provided might help rationalise the use of technology.8
In theory several policies will create incentives to make use of more cost effective technology. In reality some of these work to a certain extent, but most systems easily become either too complicated or too simple to deal with the complex ethical and economic implications of rapid technological advances in medicine.
Regulation of pharmaceuticals
Public discussion about drug safety has a surprisingly short history. It began in the 1960s, spurred by disasters like the thalidomide affair. Today many countries have well developed systems for premarket approval. Postmarket surveillance of drugs—a system for reporting unexpected side effects—is also developing in several countries.
Essentially all countries regulate pharmaceuticals by law, which means that drugs must be tested in controlled trials for safety and efficacy before they are allowed to be licensed and marketed. This requirement means that pharmaceuticals are more controlled than any other health technology. It does not necessarily mean, however, that a new drug is superior to an older one. In most cases it means that the foreseeable risk of the drug is known from trials and that it does what it is supposed to do. For example, a drug for hypertension needs to show that it is safe and that it lowers the blood pressure—not necessarily to what extent it affects mortality, morbidity, or quality of life compared with an already approved drug.
The pricing of drugs in many European countries is determined by voluntary agreements or by negotiations between the governments and the manufacturers. Licensing of a drug has almost automatically meant that it would be reimbursed by governments or by private health insurance. This is no longer as automatic as it used to be. To limit governments' increasing costs for pharmaceuticals there is an emerging trend in many countries to explicitly vary reimbursement rates among drugs or to review the effectiveness of the drug and base reimbursement on comparisons of prices of drugs for similar indications.8,11
Regulation of medical devices
Medical devices are not as strictly regulated as pharmaceuticals, although many countries have regulations about safety and efficacy even in this discipline. In general, regulatory matters are restricted to the purely technical aspects of devices, such as reliability, performance, and electrical and radiation safety. The requirements for evidence of efficacy are much lower than for drugs.
Except for reviewing safety and efficacy, and enforcing the European Union directives which require that manufacturers report malfunctioning equipment to each country's agency for medical devices, the European countries, Canada, and Australia exercise little central control over devices.12–14
It has been observed—even among the general public—that regulation in this field is comparatively weak when serious problems arise with medical devices.10 This was the case in several countries in the mid-1970s with, for example, intraocular lenses, pacemakers, and intrauterine devices, and more recently for breast implants and heart valves. Insurance coverage is not as automatic for approved devices as for drugs, sometimes with reference to the lower standard of evidence required for approval.10
Regulating placement of expensive capital equipment
The United States, Canada, and Australia have developed regulatory certificate of need programmes to control technology.15 In principle these programmes require some mechanism for review including government approval of expensive medical equipment which is capital intensive.
In the Netherlands a small but important fraction of expensive technologies are regulated under the so called article 18 of a law from 1970. By this law, hospitals need permission from the ministry of health to invest in new, specialised, and expensive equipment. The ministry determines which technologies fall under article 18 and defines the criteria for their implementation and use. The law was originally intended only for new and expensive technology like scanners for computed tomography and magnetic resonance imaging, linear accelerators, and dialysis services. Article 18 has, however, become a planning tool for specialised services generally.16
A similar system is used in parts of Canada and Spain. In Quebec and Catalonia, for example, authorisation is required from a regional authority to acquire certain technologies, such as imaging, radiation therapy, and pacemaker implantation. For establishing so called superspecialised services, for example, organ transplantation, written authorisation must be given by the minister of health.17,18
France has developed a system of regulating technology by defining the need of technology and hospital beds in different regions of the country, so called health mapping.19 The ministry of health defines the need, and hospitals, by law, must receive approval from the ministry to establish specialised services, including “major” medical equipment such as hyperbaric chambers, cyclotrons, and scanners for computed tomography and magnetic resonance imaging.
Other countries, for example, Sweden and the United Kingdom, take the approach of regionalising specialised services that require expensive capital investments either on the basis of negotiations, voluntary agreements, or bids for technology.
Health technology assessment
In the absence of powerful measures to limit overall spending on health care and to balance technological advances with available resources, a new specialty of assistance to health policy making has emerged under the concept of health technology assessment.
Health technology assessment began when the policy implications of the computed tomography scanner were discussed in the 1970s. Since then the specialty has expanded substantially from being preoccupied with assessing medical equipment to evaluating policy concerning major public health problems—for example, treatment of back pain, misuse of alcohol and substances, and mass screening for disease.20
The main focus of health technology assessment is synthesising scientific evidence including an analysis of the social, ethical, and economic implications of the dissemination and use of health technology.
Health technology assessment is organised by country. For example, in Sweden, Spain, France, and Canada governmental agencies assess health technology. In addition, many research institutions are concerned with health technology assessment.7 In the United Kingdom a major activity of the NHS research and development programme is “assessments of the effectiveness, costs, and broader impact of all procedures used by healthcare professionals to promote health and to prevent or treat illness.”21
The main methodology in health technology assessment concerns systematic reviews of the scientific literature, largely inspired by the work of the Cochrane Collaboration. Health technology assessment is, however, more oriented toward the synthesis of clinical and other information such as cost effectiveness and evidence of cost as well as consideration of the ethical and social implications of technology. To avoid the duplication of efforts in health technology assessment a worldwide network of over 30 agencies and institutions from 18 different countries, including developing countries such as Cuba and Chile, has been formed.22 Currently this network is dealing with hundreds of comprehensive assessments, from treatment in hyperbaric chambers to optional treatments of psychosis. A European network is also under construction with support from the European Union. The base of this network is the governmental agencies in health technology assessment, now established in almost all countries of the European Union.
Governmental interest in health technology assessment has paralleled the growth in healthcare spending. It is important then to emphasise that the main purpose of health technology assessment is not to save money by denying services or to sacrifice the individual for some “public good.”10 The aim of health technology assessment is to promote a more rational use of healthcare services. With such a broad ambition it is also virtually impossible to estimate the impact that health technology assessment may have on the dissemination and use of technology. There are, however, several specific examples to show that health technology assessment has substantially impacted on both health policy making and clinical practice.10,23
Conclusions
Rising expenditures for health care are fostered not only by increased technology but by such factors as changing patterns of disease, ageing populations, and rising demands from the public. The problems and issues we have described now affect all countries, which makes the management of technology a global concern and a long term challenge.
Many organisations and individuals are involved in the efforts to promote more rational use of limited resources for health care by assessing health technology in its broad meaning. The efforts of, for example, the Cochrane Collaboration, other centres for reviews and evidence based medicine, and the people concerned with health technology assessment are interrelated. Through this collaborative effort it seems feasible that patients in the future can be assured of medical technology that is both effective and cost effective.
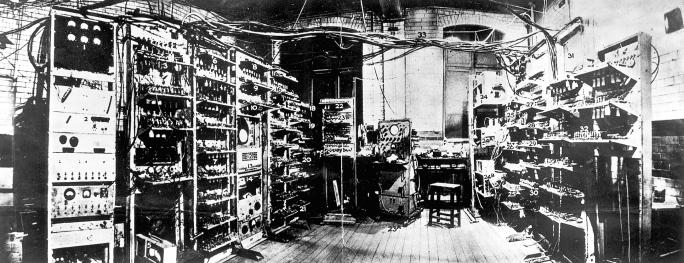
Figure.
SCIENCE & SOCIETY PICTURE LIBRARY
Technological dawn: Manchester Mark 1, the first fully electronic stored-program computer, built in June 1949
Footnotes
Competing interests: None declared.
References
- 1.Banta D, Behney C, Sisk J. Springer series on health care and society. Vol. 5. New York: Springer; 1981. Toward rational technology in medicine. [PubMed] [Google Scholar]
- 2.Drummond M. Economic appraisal of health technology in the European Community. Oxford: Oxford University Press; 1987. [Google Scholar]
- 3.Warren K, Mosteller F. Doing more good than harm: the evaluation of health care interventions. New York: New York Academy of Sciences; 1993. [PubMed] [Google Scholar]
- 4.Altman S, Blendon R. Medical technology: the culprit behind health care costs? Proceedings of the 1977 Sun Valley forum on national health. Washington, DC: United States Department of Health, Education, and Welfare, 1979.
- 5.Swedish Council on Technology Assessment in Health Care. Moderately elevated blood pressure. J Intern Med 1995;238(suppl 737). [PubMed]
- 6.Banta D. Report from the EUR-ASSESS project. EUR-ASSESS. Int J Technol Assess Health Care. 1997;13:133–333. doi: 10.1017/s0266462300009259. [DOI] [PubMed] [Google Scholar]
- 7.Banta D. Health technology assessment and the European Union. Int J Technol Assess Health Care (in press.) [DOI] [PubMed]
- 8.Abel-Smith B. Value for money in health services: a comparative study. London: Heinemann; 1976. [Google Scholar]
- 9.Mossialos E. Contract report prepared for the EUR-ASSESS project. London: London School of Economics; 1996. The regulation of the EU pharmaceutical market. [Google Scholar]
- 10.Tunis S, Gelband H. Health care technology in the United States. In: Banta D, Battista R, Gelband H, Jonsson E, editors. Health care technology and its assessment in eight countries. Washington, DC: United States Congress; 1995. pp. 275–334. [Google Scholar]
- 11.Mossialos E. Regulating expenditure on medicines in European Union countries. In: Saltman R, Figueras J, Sakellarides C, editors. Critical challenges for health care reform in Europe. Milton Keynes: Open University Press; 1998. pp. 261–286. [Google Scholar]
- 12.Banta D, Battista R, Gelband H, Jonsson E. Health care technology and its assessment in eight countries. Washington, DC: United States Congress; 1995. [Google Scholar]
- 13.Kessler D, Pape S, Sundwall D. The federal regulation of medical devices. N Engl J Med. 1987;317:357–366. doi: 10.1056/NEJM198708063170606. [DOI] [PubMed] [Google Scholar]
- 14.Brown L. Common sense meets implementation: certificate-of-need regulation in the States. J Health Polit, Policy Law. 1983;8:480–494. doi: 10.1215/03616878-8-3-480. [DOI] [PubMed] [Google Scholar]
- 15.Hillman B. Physicians' acquisition and use of new technology in an era of economic constraints. In: Gelijns A, editor. Technology and health care in an era of limits. Washington, DC: National Academy Press; 1992. [Google Scholar]
- 16.Bos M. Health care technology in the Netherlands. In: Banta D, Battista R, Gelband H, Jonsson E, editors. Health care technology and its assessment in eight countries. Washington, DC: United States Congress; 1995. pp. 171–208. [Google Scholar]
- 17.Battista R, Jacob R, Hodge M. Health care technology in Canada (with special reference to Quebec) In: Banta D, Battista R, Gelband H, Jonsson E, editors. Health care technology and its assessment in eight countries. Washington, DC: United States Congress; 1995. pp. 61–102. [Google Scholar]
- 18.Granados A, Sampriedo L, Asua J. Health technology assessment in Spain. Int J Technol Assess Health Care (in press.) [DOI] [PubMed]
- 19.Weill C. Health care technology in France. In: Banta D, Battista R, Gelband H, Jonsson E, editors. Health care technology and its assessment in eight countries. Washington, DC: United States Congress; 1995. pp. 103–135. [Google Scholar]
- 20.Swedish Council on Technology Assessment in Health Care. Publications from INAHTA agencies. Stockholm: SBU, May; 1999. [Google Scholar]
- 21.Woolf S. Health technology assessment in the United Kingdom. Int J Technol Assess Health Care (in press.) [DOI] [PubMed]
- 22.This is INAHTA. Stockholm: Swedish Council on Technology Assessment in Health Care; 1998. www.inahta.org www.inahta.org. [Google Scholar]
- 23.Brorsson B, Arvidsson S. The effect of dissemination of recommendations on use: preoperative routines in Sweden, 1989-91. Int J Technol Assess Health Care. 1997;13:547–553. doi: 10.1017/s0266462300010023. [DOI] [PubMed] [Google Scholar]