Abstract
This case report details the rehabilitation procedure for a 35-year-old man involved in a vehicle accident that resulted in multiple joint fractures. The patient had fractures to the proximal tibia, left bimalleolar, posterior malleolus, fourth and fifth metacarpal heads, and second and third proximal phalanges. After open reduction and internal fixation surgery, an 8-12 week physical treatment regimen was put into place. Exercises for both passive and active range of motion, isometric and progressive resistance training, and gait training were provided. The rehabilitation goals were pain relief, increased range of motion, muscle strength, flexibility, endurance, and functional independence. Pain levels, range of motion, muscle strength, and general function all significantly improved between pre- and post-rehabilitation evaluations. Early mobilization and structured physical therapy were crucial in achieving these outcomes, highlighting the importance of tailored rehabilitation protocols for post-operative recovery.
Keywords: physiotherapy, range of motion, muscle strength, multiple joint fractures, rehabilitation
Introduction
Multiple joint fractures involve two or more bone fractures on the different joints of the human body. The ankle is one of the most commonly fractured lower limbs, accounting for approximately 9% of all cases, with an annual incidence of 107-187 per thousand people [1]. The most common fractures in these age groups occur in men under 50 years of age and in women over 50 years of age. Among the most common causes of ankle fractures are motor vehicle accidents, twisting injuries, and falls [2]. The tibia is the most commonly broken of all the long bones in the human body, and it is generally broken as a result of high-energy trauma, such as being involved in a car accident or falling from a great height [3]. In approximately 88% of all metacarpal fractures, the fifth finger is the most commonly fractured. Eightteen to 44% of all hand fractures are metacarpal fractures [4]. The type and severity of the trauma, the integrity of the fracture fixation, and biological processes, particularly immunological and developmental processes related to skeletal ontology, all affect how quickly a fracture heals [5]. As the incidence of fractures among the senior population rises, so does the illness load. The senior population finds it challenging to follow restrictions on weight bearing, and being immobile comes with serious hazards and increased morbidity [6]. In proximal tibia fracture tibia, a more complicated and multi-fragmented fracture pattern may be the result of high-energy trauma, which mainly affects young people. However, in elderly individuals with lower bone density, a low-energy mechanism may result in a pure depression fracture. Preoperative classification of these fractures with the Muller AO Classification, Schatzker classification, or cutting-edge computed tomography (CT) based techniques aids in understanding the fracture pattern and aids in selecting the surgical approach and treatment plan based on estimated bone mineral density and the unique medical histories of each patient [7].
Thirty to 50% of all hand fractures are metacarpal fractures. The variety and complexity of human hand movements are made possible by the biomechanical interactions between the soft tissues of the hand. Only a sturdy skeleton structure can support the combined action of these mutually beneficial forces. The typical activities of the soft tissue result in deforming postures when the structure is violated by a fracture, which is detrimental to effective fracture therapy [8]. Orthopedic physicians treat bimalleolar ankle fractures more frequently than any other type of injury. Ankle fractures with bimalleolar bones are typically brought on by twisting injuries with numerous force mechanisms. The ligaments surrounding the medial and lateral malleoli give the ankle joint support. An intra-articular injury is a bimalleolar fracture. Normalizing anatomy is the major objective of treating these fractures. The surgical technique restores the joint's anatomy and contact-loading properties [9].
In this case, a 35-year-old male had a history of road traffic accidents (RTA). The patient came with a complaint of wrist pain and leg pain on the left side for six days and inability to walk properly for six days. Pain and swelling were progressively in nature. On radiological investigation, the patient was diagnosed with multiple joint fractures. Pain and swelling were progressively in nature after the patient was managed operatively with open reduction and internal fixation. After that, postoperative physiotherapy treatment was started on day one, and the physiotherapy protocol was 8-12 weeks. According to the level of stability attained by internal fixation, bone mineral density, and other patient-specific characteristics, rehabilitation procedures should be carefully established (age, compliance, mobility). Early functional mobilization is crucial in rehabilitation to prevent stiffness [7]. The aim of physiotherapy is to reduce pain, increase and maintain a range of motion, improve and maintain strength in the muscle of the metacarpophalangeal (MCP) joint, knee, and ankle joints, and improve flexibility and endurance as well as improve and maintain functional independence.
Case presentation
Patient information
A 35-year-old man was apparently alright before 23/10/22. He lives in Dhapki village, and he is an astrologist. Hand dominance is right. He was in a road traffic accident, a head-on collision on 17/10/22 at Bilaspur. The patient was unable to walk immediately after the incident. Then, the patient's relative brought the patient to a nearby hospital in Bilaspur, where medication was given, and the dressing was done and managed conservatively. Pain was relieved by medication. Then, the patient came to a super-specialty hospital on 23/10/22 with complaints of wrist pain and leg pain on the left side for six days and inability to walk properly for six days. Pain and swelling were progressive in nature. Then, an orthopedic doctor prescribed medication and further investigation was done. Radiological investigation diagnosed a left-side bimalleolar fracture, posterior malleolus fracture, proximal tibia fracture, fourth and fifth metacarpal head fracture, and second and third proximal phalanx fracture. After that, the patient was referred to a musculoskeletal physiotherapy unit for further physiotherapy management.
Clinical findings
The patient was cooperative, conscious, and well-oriented to time, place, and person. In a supine position with the shoulder and the anterior superior iliac spine (ASIS), both at the same level, and the left leg was elevated. Upon physical examination, pulse rate was 77 beats/min, respiratory rate was 19 breaths/min, and blood pressure was 120/80 mmHg. On observation, the general condition of the patient is fairly built. A plaster cast is present over the left knee joint to the ankle joint and the fourth and fifth fingers to the elbow joint. On palpation, swelling and redness over the left ankle joint, lateral condyle, and metacarpal joint. Grade 2 tenderness was present over the anterolateral aspect of the lateral condyle, ankle joint, and fourth and fifth metacarpal joint. Hamstring tightness was present on the right lower limb.
Pre-rehab Visual Analogue Scale (VAS) was 4.5/10 at rest and 7.5/10 on slight movement, and post-rehab VAS was 2.5/10 at rest and 2.5/10 on slight movement. For motor examination, the goniometer was used to assess the range of motion (ROM), and the results are shown in Table 1 as being within normal limits. Table 2 shows the results of the Manual Muscle Testing (MMT) evaluation.
Table 1. Range of motion assessment.
MCP - metacarpophalangeal joint; PIP - proximal interphalangeal joint
| Joint (Left side) | Pre-rehabilitation | Post-rehabilitation |
| MCP fourth and fifth flexion | 0°-20° | 0°-75° |
| MCP fourth and fifthextension | 0°-8° | 0°-15° |
| MCP fourth and fifth abduction | 0°-8° | 0°-18° |
| PIP flexion | 0°-75° | 0°-95° |
| Wrist flexion | 0°-78° | 0°-78° |
| Wrist extension | 0°-70° | 0°-70° |
| Ulnar deviation | 0°-30° | 0°-30° |
| Radial deviation | 0°-20° | 0°-20° |
| Knee flexion | 0° | 0°-135° |
| Ankle dorsiflexion | 0° | 0°-48° |
| Ankle plantarflexion | 0° | 0°-17° |
| Ankle inversion | 0° | 0°-13° |
| Ankle eversion | 0° | 0°-28° |
Table 2. Muscle Manual Testing.
| Joint (left side) | Pre-rehabilitation | Post-rehabilitation |
| Wrist flexors | 4/5 | 5/5 |
| Wrist extensors | 4/5 | 5/5 |
| Knee flexors | 3/5 | 4/5 |
| Ankle plantar-flexors | 2/5 | 4/5 |
| Ankle dorsiflexors | 2/5 | 4/5 |
| Ankle invertors | 2/5 | 4/5 |
| Ankle evertors | 2/5 | 4/5 |
Investigations
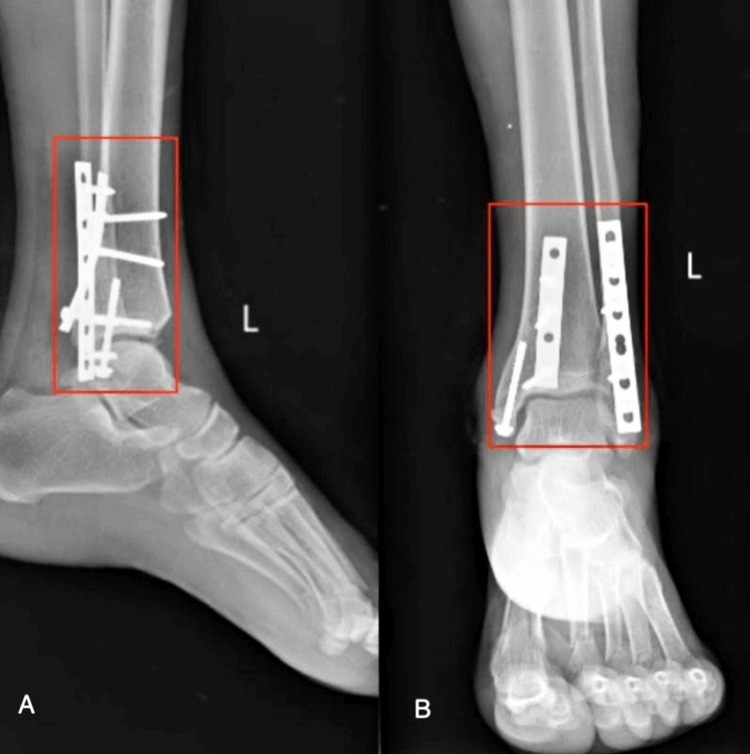
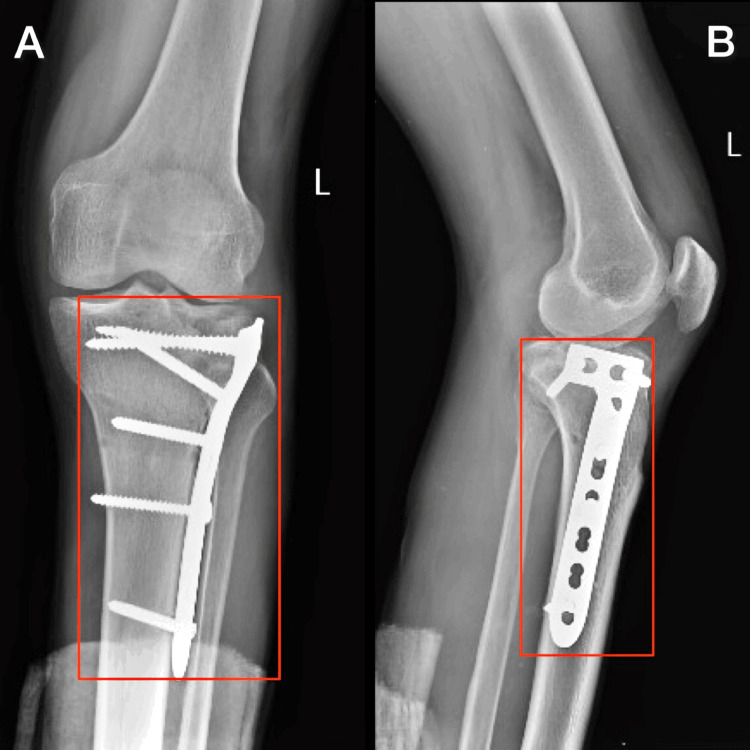
X-ray was done post-operatively. The patient has undergone an operation that is open reduction and internal fixation with plate osteosynthesis for bimalleolus fracture, posterior malleolus fracture, and proximal tibia is shown in Figure 1 and Figure 2, as well as open reduction and internal fixation for fourth and fifth metacarpal head fracture and second and third proximal phalanx fracture shown Figure 3.
Figure 1. Postoperative X-ray of the left ankle joint AP view.
AP - antero-posterior
A) Semi-tubular plate 6 hole, cortical screw; B) Semi-tubular plate 8 hole, cortical screw
Figure 2. Postoperative X-ray of the left knee joint.
AP - antero-posterior
A: AP view of knee joint showing cancellous screw and locking screw; B) Lateral view of ankle joint showing L-butress plate
Figure 3. Post-operative X-ray of the left hand.
A) Antero-posterior view; B) Lateral view
Physiotherapy management
Physiotherapy rehabilitation protocol for this multiple joint fractures is 8 to 12 weeks and divided into four phases. The fracture of the fourth and fifth metacarpal head and second and third proximal phalanx fracture rehabilitation protocol was four to eight weeks (Tables 3, 4), as well as left-side bimalleolar fracture, posterior malleolus fracture, proximal tibia fracture rehabilitation protocol, which was 8 to 12 weeks (Table 3, 5). Precautions taken in phase 1 were no strengthening exercise and no active range of motion (ROM) for the affected side extremity. Figure 4 and Figure 5 show the patient receiving physiotherapy treatment.
Table 3. Physiotherapy management phase-wise for the upper and lower limbs.
ROM - range of motion
| Goal | Treatment | Phase 1 | Rationale |
| Patient education | Patient education | Educating the patient and family about their condition and how physiotherapy helps to regain their normal ROM and strengthen | Patient and their family were educated about the importance of physiotherapy |
| Reducing pain and tenderness | Cryotherapy | 10 minute | Vasoconstriction to reduce inflammation and swelling |
Table 4. Upper limb physiotherapy management phase-wise.
MCP - metacarpophalangeal joint; ROM - range of motion; MET - muscle energy technique; PIR - post-isometric relaxation
| Goals | Treatment | Phase 1 (day 1-1 week) | Phase 2 (2-3 weeks) | Phase 3 (4-8 weeks) | Rationale |
| For upper limb and MCP joints. To increase and maintain ROM MCP joints. | Active range of motion exercise for elbow and shoulder | 10 repetitions 1 set | - | - | Enhancing the motion of a particular joint. The arrangement of the bone surfaces within the joint, the joint capsule, as well as the muscles, tendons, and ligaments that act on the joint all influence this motion |
| Active range of motion exercise for metacarpal joint (MCP) | - | 10 repetitions 1 set | 10 repetitions 2 set | Restore normal and increase as well as maintain joint motion | |
| To improve and maintain muscle strength. | Isokinetic exercise for deltoid, biceps, triceps and quadriceps | 10 repetitions 1 set | - | - | To maintain strength for upper limb muscle |
| Isometric exercise for wrist flexors, extensors | - | 10 repetitions 1 set | 10 repetitions 2set | To increase strength and maintain strength of wrist muscles | |
| MET and PIR for wrist extensors | - | - | 10 repetitions 1 set | Lengthen shortened muscles, increase joint range of motion | |
| Resistance exercise squeezing ball | - | 10 repetitions 1 set | 10 repetition 2 set | To increase and maintaining muscle strength MCP and PIP joint | |
| Progressive resistance exercise for hand muscle using weight cuff | - | 10 repetitions 1 set | 10 repetitions 1 set | To maintain muscle strength |
Table 5. Lower limb physiotherapy management phase-wise.
MCP - metacarpophalangeal joint; SLR - straight leg raise; ROM - range of motion, MET - muscle energy technique; PIR - post-isometric relaxation
| Goals | Treatment | Phase 1 (day1-1 week) | Phase 2 (2-3 weeks) | Phase 3 (4-8 weeks) | Phase 4 (4-8 weeks) | Rationale |
| To increase and maintain ROM | Active range of motion exercise for metatarsophalangeal joint | 10 repetitions 1 set | 10 repetitions 2 set | 10 repetitions 2 set | - | Enhancing the motion of a particular joint. The arrangement of the bone surfaces within the joint, the joint capsule, as well as the muscles, tendons, and ligaments that act on the joint all influence this motion. |
| Assisted straight leg raise | 10 repetitions 1 set | - | - | To increase the range of motion | ||
| Straight leg raise | - | 10 repetitions 1 set | - | To maintain normal ROM | ||
| Active range of motion exercise for knee joint | 10 repetitions 1 set | - | - | To increase the range of motion of the knee joint | ||
| Active range of motion exercise for ankle joint | - | - | 10 repetitions 1 set | 10 repetitions 2 set | To increase the range of motion of the ankle joint | |
| To increase and maintain muscle strength | Isometric exercise for dorsiflexors and plantar flexors | - | 10 repetitions 1 set | 10 repetitions 2 set | 10 repetitions 2 set | To increase and maintain muscle strength of dorsiflexors |
| Isometric exercise for invertors and evertors | - | - | 10 repetitions 1set | 10 repetitions 2 set | To increase and maintain muscle strength of invertors and evertors | |
| MET and PIR for dorsiflexors | - | 10 repetitions 1 set | 10 repetitions 2 set | Lengthen shortened muscles, increase joint range of motion and increase fluid | ||
| Progressive resistance exercise for lower limb using weight cuff | - | - | - | 10 repetitions 1 set | To improve muscle strength and power | |
| Dynamic quads using weight cuff | - | - | - | 10 repetitions 1 set | ||
| To improve and maintain gait pattern and balance | Gait training | Non-weight bearing stand pivot transfer | Toe touch to partial weight-bearing | Ambulation with assistive device Partial weight bearing to a 3-point stance. | Ambulation with assistive device 3-point stance to full weight bear. | Strengthen muscles and joints, improve balance and posture, build endurance |
Figure 4. Patient performing assisted SLR.
SLR - straight leg raise
Figure 5. Patient performing active knee flexion exercise.
Outcome measures
Also, we used clinical outcome measures for improvement that is pre-rehabilitation and post-rehabilitation which is mentation in Table 6.
Table 6. Outcome measure using scales.
| Scales | Pre-rehabilitation | Post-rehabilitation |
| Lower extremity function scale | 55/80 | 75/80 |
| Upper extremity function scale | 40/80 | 75/80 |
| Quality of life | 50 | 70 |
| Visual Analogue Scale (VAS) | 7.5 | 2.5 |
Discussion
Multiple fractures are typically the outcome of high-energy incidents, which frequently happen to younger patients, according to the majority of surgeons. The highest prevalence of multiple fractures in the elderly was shown to be related to high-energy modes of injury, such as falls from heights or downstairs and RTAs (27.3%, 12.5%, and 36%, respectively). The majority of multiple fractures, however, actually happen after low-energy trauma (88.1%), as these kinds of injuries are rare in senior people [10]. It is asserted that the Muscular Energy Technique (MET) can stretch short muscles, expand the joint range of motion, and promote fluid drainage from peripheral locations [11]. Although there are various ways to use the MET to make muscles more extensible [12], in this case, pursuing the rehabilitation regimen helped the patient achieve functional independence and significantly reduced pain and tenderness, improving range of motion, muscle strength, and activities of daily living (ADL).
Pereira et al., in 2020, conducted a systemic review that mentioned advanced technology for hand rehabilitation that is augmented reality (AR) and virtual reality (VR) has been used to improve the rehabilitation process. Haptic gloves with a leap motion controller can be used in a home environment. Technologies like AR and VR can be utilized in conjunction with traditional treatments. The utilization of AR or VR therapies for hand rehabilitation can be advantageous to patients. AR and VR have been used to improve the rehabilitation process [13].
The study conducted by Donohoe et al. in 2020 found that early mobilization and weight bearing after a fracture are major goals of treatment in order to avoid deconditioning and the negative effects of prolonged immobility [6]. Arslan et al. conducted a study in 2015 that concluded the initiation of early ROM soft tissue lesions altered the onset of early knee joint mobility, which enhanced the clinical outcomes. Therefore, in cases like these, meniscus and ligament injuries should be taken into account as prognostic variables, as well as early passive mobilization, have been proven to reduce the incidence of deep vein thrombosis (DVT) and increase knee flexion range of motion during rehabilitation [14]. In the early stages of maintaining and improving knee mobility, electrotherapy modalities, including continuous passive motion, were used to initiate and enhance the knee range of motion [15].
Conclusions
According to the above case report, it is associated with a surgical approach, and early, structured physical therapy rehabilitation improved the functional goals over time, which is a crucial factor in helping postoperative patients recover successfully. The patient, in this instance, was greatly helped in achieving functional independence by adhering to the organized rehabilitation program. Reduction of discomfort and tenderness, improvement of range of motion, strengthening of muscles, and improvement of activities of daily living (ADLs) were all made possible by the combination of early, comprehensive physiotherapy rehabilitation and surgical intervention. A thorough, progressive physiotherapy approach is essential for managing difficult multiple-joint fractures, as demonstrated by the patient's notable improvement in strength and mobility. The rehabilitation procedure enhanced the patient's general health and quality of life in addition to benefiting in their recovery from injury. The successful recovery of postoperative patients with multiple joint fractures is largely dependent on early mobilization and physiotherapy rehabilitation, as this case study demonstrates.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
- 1.A prospective study on radiological and functional outcome of bimalleolar fractures: a study on 50 cases. Ejazul M, Deepthi KN, Manjunath M, Dhanda A, Supreeth ER. Natl J Clin Orthop. 2019;3:13–17. [Google Scholar]
- 2.Epidemiology of ankle fractures. A prospective population-based study of 212 cases in Aalborg, Denmark. Jensen SL, Andresen BK, Mencke S, Nielsen PT. Acta Orthop Scand. 1998;69:48–50. doi: 10.3109/17453679809002356. [DOI] [PubMed] [Google Scholar]
- 3.Evaluation of management of proximal tibia shaft fracture with interlocking tibia nail through suprapatellar approach. Sarkar UK. Int J Orthop Sci. 2022;8:375–391. [Google Scholar]
- 4.Metacarpal fractures: treatment and complications. Kollitz KM, Hammert WC, Vedder NB, Huang JI. Hand (NY) 2014;9:16–23. doi: 10.1007/s11552-013-9562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fracture healing: mechanisms and interventions. Einhorn TA, Gerstenfeld LC. Nat Rev Rheumatol. 2015;11:45–54. doi: 10.1038/nrrheum.2014.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Management of lower extremity fractures in the elderly: a focus on post-operative rehabilitation. Donohoe E, Roberts HJ, Miclau T, Kreder H. Injury. 2020;51:0–22. doi: 10.1016/j.injury.2020.04.050. [DOI] [PubMed] [Google Scholar]
- 7.Partial proximal tibia fractures. Raschke MJ, Kittl C, Domnick C. EFORT Open Rev. 2017;2:241–249. doi: 10.1302/2058-5241.2.160067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Management of metacarpal fractures. McNemar TB, Howell JW, Chang E. J Hand Ther. 2003;16:143–151. doi: 10.1016/s0894-1130(03)80009-1. [DOI] [PubMed] [Google Scholar]
- 9.Surgical management of bimalleolar ankle fractures: a narrative review. Sakthivel R, Sundararajan T, Sathyanarayana LY. Int J Orthop Sci. 2021;7:236–238. [Google Scholar]
- 10.Multiple fractures in the elderly. Clement ND, Aitken S, Duckworth AD, McQueen MM, Court-Brown CM. J Bone Joint Surg Br. 2012;94:231–236. doi: 10.1302/0301-620X.94B2.27381. [DOI] [PubMed] [Google Scholar]
- 11.The effect of muscle energy technique on hamstring extensibility: the mechanism of altered flexibility. Ballantyne F, Fryer G, McLaughlin P. J Osteopath Med. 2003;6:59–63. [Google Scholar]
- 12.A comparison of two muscle energy techniques for increasing flexibility of the hamstring muscle group. Smith M, Fryer G. J Bodyw Mov Ther. 2008;12:312–317. doi: 10.1016/j.jbmt.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Application of AR and VR in hand rehabilitation: a systematic review. Pereira MF, Prahm C, Kolbenschlag J, Oliveira E, Rodrigues NF. J Biomed Inform. 2020;111:103584. doi: 10.1016/j.jbi.2020.103584. [DOI] [PubMed] [Google Scholar]
- 14.Immediate knee joint range of motion after stable fixation of tibial plateau fractures. Arslan A, Polat M, Ciliz A, Utkan A. Open J Orthop. 2015;5:198–207. [Google Scholar]
- 15.Bawiskar D, Dhote S, Phansopkar P. Med Science. Vol. 24. Discovery: 2020. Early physical rehabilitation post-surgery in a complex type 5 schatzker tibial plateau fracture improves functional outcomes: a case report; pp. 2675–2682. [Google Scholar]