Abstract
Introduction
Dispatcher-assisted cardiopulmonary resuscitation (DA-CPR) improves bystander CPR rates and survival outcomes. This study aimed to identify barriers to successful DA-CPR in patients with out-of-hospital cardiac arrest (OHCA).
Methods
This retrospective observational study used data from a nationwide OHCA database from 2017 to 2021. Adult emergency medical services (EMS)-treated patients with OHCA with a presumed cardiac etiology were enrolled. The main exposure variable was compliance with DA-CPR. The primary outcome was good neurological recovery at hospital discharge. Multivariable logistic regression analysis was conducted to identify the major factors associated with unsuccessful DA-CPR with and without multiple imputations. Causal mediation analysis was conducted using witnessed status as a mediator.
Results
In the final analysis, 49,165 patients with OHCA were included. A total of 36,865 (75.0%) patients successfully underwent DA-CPR. A higher proportion of good neurological recovery was observed in the successful DA-CPR group than in the non-successful DA-CPR group (P < 0.001). The following factors were identified as risk factors for unsuccessful DA-CPR: age > 65 years, male sex, OHCA occurring in a non-metropolitan area or private place, unwitnessed status, whether the bystander was a non-family member or non-cohabitant, female sex or had not received CPR training, and primary call dispatchers not receiving any first-aid training. Additional analyses after multiple imputations showed similar results. Mediation effect was significant for most risk factors for unsuccessful DA-CPR.
Conclusions
Bystander characteristics (non-family member or non-cohabitant, female, and uneducated status for CPR) and primary call dispatchers not receiving first-aid training were identified as risk factors for unsuccessful DA-CPR.
Keywords: Out-of-hospital cardiac arrest, Cardiopulmonary resuscitation, Emergency medical dispatcher, Compliance
Introduction
Out-of-hospital cardiac arrest (OHCA) is a significant public health issue with a high incidence rate but low survival outcomes.1, 2 Immediate bystander cardiopulmonary resuscitation (CPR) provision improves survival rates and neurological recovery of patients with OHCA.3, 4, 5 However, survival rates after bystander CPR vary across different regions and are low in some communities; this may be because of inadequate bystander CPR at the scene.2, 6, 7
Dispatcher-assisted CPR (DA-CPR) is regarded as an effective community-based intervention that reduces no-flow time before the arrival of emergency medical services (EMS) and increases bystander CPR rate.8, 9 Dispatchers in dispatch centers serve as the first link in the cardiac arrest chain of survival by recognizing cardiac arrest early and providing instant instruction with DA-CPR.10, 11
Although instructions are provided by well-trained dispatchers who follow predefined EMS protocols, DA-CPR is hindered for various reasons. Because DA-CPR is mainly provided through audio calls, communication errors between the caller and dispatcher are unavoidable.12, 13 Characteristics of the bystanders providing CPR, such as age, sex, and relationship with the patient, may influence DA-CPR compliance. Callers may refuse to provide CPR, hang up the phone, or suffer physical limitations or emotional anxiety.9, 14, 15 DA-CPR compliance can also be influenced by EMS-related factors, including local dispatch system type and experience level of each dispatcher.16, 17, 18 Additionally, several characteristics of the local community where patients with OHCA occur, including urbanization degree, socioeconomic status, and location of arrest (public or private), are associated with DA-bystander CPR.19, 20, 21
Although several communities have reported various barriers to DA-CPR, those in South Korea are yet to be fully investigated. In this study, we aimed to compare the characteristics and outcomes of patients with OHCA according to DA-CPR compliance and identify barriers to DA-CPR based on the abovementioned factors.
Methods
Study design and setting
This was an observational, cross-sectional study using data from the Korean Out-of-Hospital Cardiac Arrest Registry (KOHCAR).
The public EMS system in Korea is based on the fire department and consists of 18 provincial fire departments and dispatch centers. EMS dispatch and onsite first aid are provided in accordance with the national EMS protocol. The DA-CPR program was started as a pilot project in 2010 and implemented in all dispatch centers nationwide in 2012.22 There are two dispatcher types in each dispatch center. Primary call dispatchers are responsible for recognizing OHCAs and transferring calls to secondary call dispatchers. Most primary call dispatchers are firefighters, whereas most secondary call dispatchers are emergency medical technicians (EMT) or nurses. When primary call dispatchers recognize cardiac arrests using two key questions (abnormal mental status and breathing), they transfer the call to secondary call dispatchers, who help bystanders perform compression-only CPR until the ambulance arrives. Secondary call dispatchers record OHCA cases with dispatcher instructions in the electronic medical dispatch registry. Medical directors in the dispatch center, certified by the Ministry of Health and Welfare, are required to review randomly assigned DA-CPR audio recordings and provide feedback to primary and secondary call dispatchers for quality control.
Data source
The KOHCAR is a nationwide registry constructed by the National Fire Agency (NFA) and the Korea Disease Control and Prevention Agency (KDCA) in 2006. All EMS-assessed OHCA cases are collected using an EMS run sheet, EMS OHCA registry, emergency medical dispatch registry, and hospital medical record review. The collected information includes Utstein variables and is reported annually by the NFA and KDCA.23, 24
Study population
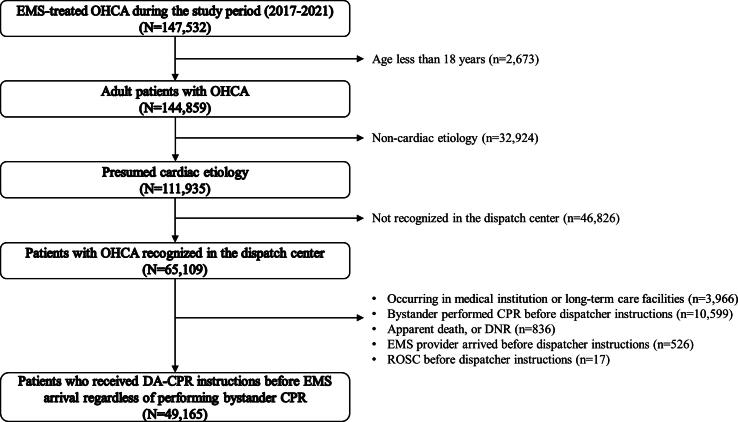
Adults with OHCA of presumed cardiac etiology treated by EMS providers between January 2017 and December 2021 were included. Cases due to hanging, asphyxiation, drowning, poisoning, and traumatic cardiac arrest were excluded. Bystanders were instructed to provide first aid such as rescue, urgent trauma care, and rescue breathing to prevent continued asphyxiation. Therefore, quickly performing compression-only CPR, provided in usual cardiac arrest, might be difficult. We enrolled only patients diagnosed with cardiac arrest at the dispatch center. Among patients where bystanders received dispatcher instructions, those who did not require DA-bystander CPR (there was apparent death or a DNR (do-not-resuscitate) order, EMS providers arrived before dispatcher instructions were issued, or spontaneous circulation was restored prior to dispatcher instruction) or where bystanders had already performed bystander CPR before DA-CPR instructions were issued, were excluded. Cases occurring in medical institutions or long-term care facilities were also excluded (Fig. 1).
Fig. 1.
Study population.
Outcome variables
The primary outcome was good neurological recovery at the time of hospital discharge, defined as a cerebral performance category (CPC) score of 1 or 2. The secondary and tertiary outcomes were survival to hospital discharge and prehospital return of spontaneous circulation (ROSC). These outcomes were identified by reviewing the medical records extracted by medical record reviewers from the KDCA.
Variables and measurements
The main exposure variable was compliance with DA-CPR: successful DA-CPR until EMS arrival versus unsuccessful DA-CPR. Successful DA-CPR was defined as bystanders continuing to perform CPR without interruption until EMS arrived. Unsuccessful DA-CPR was categorized into four groups: Interruption of DA-CPR before EMS arrival, bystanders could not perform CPR despite dispatcher instruction, no confirmation of successful DA-CPR until EMS arrival, and dispatcher instructions not performed despite suspicion of cardiac arrest. All variables were identified from dispatcher records.
We collected data on i) age, sex, day of event (weekend or weekday), and time of event (day (09:00–18:00)); ii) community variables (urbanization level (metropolitan area or non-metropolitan area), and location of arrest (public (road, commercial and industrial facilities, leisure spaces, public buildings, airports, and train stations), private (homes and mass residential facilities such as dormitories), and other)); iii) bystander characteristics, including relationship with the patient ((family member or cohabitant, facility staff, colleague or friend, passerby, medical personnel (regardless of duty status), and other), age, sex, and educational status for CPR). In general, a bystander is defined as a person who takes the lead in performing chest compressions under the dispatcher’s direction. This information is recorded at the discretion of the secondary dispatcher; iv) EMS variables (initial electrocardiogram rhythm at the scene (shockable or not), arrest to EMS CPR time interval, detection time interval (from call to detection of OHCA by the dispatcher), response time interval (from call to EMS arrival), scene time interval (from arrival at the scene to EMS departure from the scene), transport time interval (from EMS departure from the scene to arrival at the ED), qualification of primary dispatcher (EMT, nurse, first aid trainee, and others without first aid training), and secondary call dispatcher (EMT, nurse, doctor, first aid trainee, and other)); and v) hospital variables (ED level).
Statistical analysis
Continuous variables were expressed as medians and interquartile ranges, and categorical variables were expressed as counts and proportions. We used the Wilcoxon rank-sum test for continuous variables and the Pearson’s χ2 test for categorical variables. We calculated adjusted odds ratios with 95% confidence intervals using forward stepwise logistic regression analysis at a significance level of < 0.05 to evaluate risk factors related to unsuccessful DA-CPR.
We used multiple imputations to address missing data assumed to be missing at random and handled using the fully conditional specification method in SAS PROC MI, with variables related to bystander characteristics, including sex and educational status for CPR.25 Ten imputed datasets were generated and risk factors for unsuccessful DA-CPR were reassessed (Supplementary Appendix). In addition, mediation analysis was performed using the PROC CAUSALMED procedure in SAS. We evaluated whether the relevant variables affected the unsuccessful DA-CPR, mediated by witnessed status. Mediation analysis divided the total effect into direct and indirect effect, where direct effect represented the association between relevant variables and unsuccessful DA-CPR and indirect effect represented the causal mechanism through witnessed status. Percentage mediated represented the mediating effect percentage (Supplementary Appendix).26 A two-sided P < 0.05 was defined as significant. All statistical analyses were performed using SAS software (version 9.4; SAS Institute Inc., Cary, NC, USA).
Ethics statement
This study was approved by the Institutional Review Board of Chungbuk National University Hospital (IRB No. 2024-02-002). The requirement for informed consent was waived, and patient information was anonymized prior to analysis.
Results
Among the 147,532 OHCA cases identified during the study period, 111,935 adult patients had OHCA of presumed cardiac etiology. Of these, 65,109 patients with OHCA identified by the dispatch center were eligible for the study. We included 49,165 patients in the final analysis after excluding cases occurring in medical institution or long-term care facilities (n = 3,966), where the bystander performed CPR before dispatcher instructions were issued (n = 10,599), there was apparent death or a DNR order (n = 836), the EMS provider arrived before dispatcher instructions were issued (n = 526), and where spontaneous circulation was restored before dispatcher instructions were given (n = 17) (Fig. 1).
Table 1 shows the baseline characteristics of the enrolled patients with OHCA with regard to DA-CPR compliance. The unsuccessful DA-CPR group was more likely to be male, > 65 years old, have medical aid, and reside in a non-metropolitan area (all P < 0.001). Regarding the characteristics of bystanders, family members or cohabitants were more common in the successful DA-CPR group (79.5% and 60.7%, respectively), whereas males (56.3% and 38.8%) and bystanders educated in CPR (29.3% and 12.6%, respectively) were less common in the unsuccessful DA-CPR group. The proportion of primary call dispatchers who did not receive first-aid training was higher in the unsuccessful DA-CPR group than in the successful DA-CPR group (25.4% and 28.8%, respectively). The call to EMS dispatch, call to first compression, and response time intervals were shorter in the successful DA-CPR group than in the unsuccessful group (all P < 0.001). The unsuccessful DA-CPR group had worse clinical outcomes, including good neurological recovery, survival to hospital discharge, and prehospital ROSC than the successful group (all P < 0.001).
Table 1.
Baseline characteristics of enrolled OHCAs according to DA-CPR compliance.
| Total |
Successful DA-CPR |
Unsuccessful DA-CPR |
|||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | P-value | |
| Total | 49,165 | 36,865 | 75.0 | 12,300 | 25.0 | ||
| Sex, male | 31,086 | 63.2 | 22,910 | 62.1 | 8176 | 66.5 | <0.001 |
| Age, ≥65 | 33,497 | 68.1 | 24,522 | 66.5 | 8975 | 73.0 | <0.001 |
| Median (IQR) | 74 (61–82) | 74 (60–82) | 76 (64–82) | <0.001 | |||
| Urbanization level, metropolitan area | 20,331 | 41.4 | 15,673 | 42.5 | 4658 | 37.9 | <0.001 |
| Location of arrest | <0.001 | ||||||
| Public place | 6092 | 12.4 | 4490 | 12.2 | 1602 | 13.0 | |
| Private place | 42,456 | 86.4 | 31,976 | 86.7 | 10,480 | 85.2 | |
| Others | 617 | 1.3 | 399 | 1.1 | 218 | 1.8 | |
| Week of day, weekday | 34,747 | 70.7 | 25,901 | 70.3 | 8846 | 71.9 | <0.001 |
| Time of day, night (18:00–09:00) | 25,165 | 51.2 | 19,058 | 51.7 | 6107 | 49.7 | <0.001 |
| Witnessed arrest | 20,494 | 41.7 | 15,996 | 43.4 | 4498 | 36.6 | <0.001 |
| Bystanders, relationship | <0.001 | ||||||
| Family member or cohabitant | 36,777 | 74.8 | 29,307 | 79.5 | 7470 | 60.7 | |
| Facility staff | 1231 | 2.5 | 968 | 2.6 | 263 | 2.1 | |
| Colleague or Friend | 3835 | 7.8 | 2985 | 8.1 | 850 | 6.9 | |
| Passerby | 2431 | 4.9 | 1831 | 5.0 | 600 | 4.9 | |
| Medical personnel | 105 | 0.2 | 81 | 0.2 | 24 | 0.2 | |
| Others | 4786 | 9.7 | 1693 | 4.6 | 3093 | 25.1 | |
| Bystanders, sex | <0.001 | ||||||
| Male | 25,541 | 51.9 | 20,769 | 56.3 | 4772 | 38.8 | |
| Female | 20,422 | 41.5 | 15,557 | 42.2 | 4865 | 39.6 | |
| Unknown | 3202 | 6.5 | 539 | 1.5 | 2663 | 21.7 | |
| Bystander age, median (IQR) | 50 (40–60) | 50 (40–60) | 50 (40–60) | <0.001 | |||
| Bystanders, educational status for CPR | <0.001 | ||||||
| Yes | 12,364 | 25.1 | 10,813 | 29.3 | 1551 | 12.6 | |
| No | 22,301 | 45.4 | 18,067 | 49.0 | 4234 | 34.4 | |
| Unknown | 14,500 | 29.5 | 7985 | 21.7 | 6515 | 53.0 | |
| Qualification of primary call dispatcher | <0.001 | ||||||
| Emergency medical technician | 23,499 | 47.8 | 17,858 | 48.4 | 5641 | 45.9 | |
| Nurse | 3094 | 6.3 | 2283 | 6.2 | 811 | 6.6 | |
| First aid trainee | 9676 | 19.7 | 7368 | 20.0 | 2308 | 18.8 | |
| Others without first aid training | 12,896 | 26.2 | 9356 | 25.4 | 3540 | 28.8 | |
| Qualification of secondary call dispatcher | <0.001 | ||||||
| Emergency medical technician | 20,603 | 41.9 | 15,689 | 42.6 | 4914 | 40.0 | |
| Nurse | 7719 | 15.7 | 5743 | 15.6 | 1976 | 16.1 | |
| Doctor | 20 | 0.0 | 13 | 0.0 | 7 | 0.1 | |
| First aid trainee | 218 | 0.4 | 161 | 0.4 | 57 | 0.5 | |
| Others | 20,605 | 41.9 | 15,259 | 41.4 | 5346 | 43.5 | |
| Initial ECG rhythm, shockable | 6802 | 13.8 | 5461 | 14.8 | 1341 | 10.9 | <0.001 |
| EMS time interval, Median (IQR) | |||||||
| Call to EMS dispatch time interval, second | 50 (39–65) | 49 (39–63) | 53 (40–71) | <0.001 | |||
| Call to first compression time interval, second | 129 (98–189) | 127 (9–186) | 139 (101–204) | <0.001 | |||
| Response time interval, minute | 7 (6–10) | 7 (6–10) | 8 (6–11) | <0.001 | |||
| Scene time interval, minute | 14 (11–18) | 14 (11–18) | 14 (11–18) | <0.001 | |||
| Transport time interval, minute | 7 (4–11) | 7 (4–10) | 7 (4–12) | <0.001 | |||
| Level of ED | <0.001 | ||||||
| Level 1 | 10,919 | 22.2 | 8473 | 23.0 | 2446 | 19.9 | |
| Level 2 | 23,130 | 47.0 | 17,757 | 48.2 | 5373 | 43.7 | |
| Level 3 | 15,116 | 30.7 | 10,635 | 28.8 | 4481 | 36.4 | |
| Clinical outcomes | |||||||
| Good neurological recovery | 2267 | 4.6 | 1952 | 5.3 | 315 | 2.6 | <0.001 |
| Survival to hospital discharge | 3413 | 6.9 | 2849 | 7.7 | 564 | 4.6 | <0.001 |
| Prehospital ROSC | 4921 | 10.0 | 4021 | 10.9 | 900 | 7.3 | <0.001 |
OHCA, out-of-hospital cardiac arrest; DA-CPR, dispatcher-assisted cardiopulmonary resuscitation; IQR, interquartile range; ECG, electrocardiogram; EMS, emergency medical services; ED, emergency department; ROSC, return of spontaneous circulation.
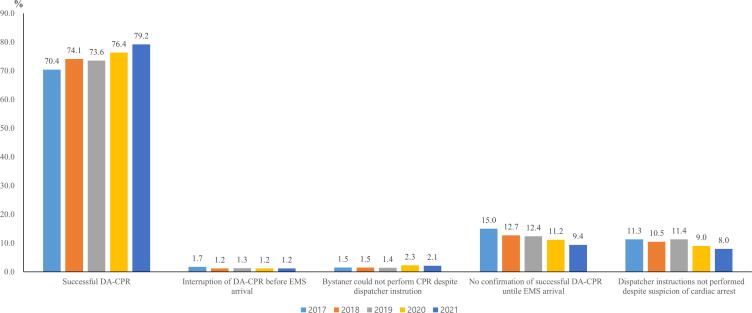
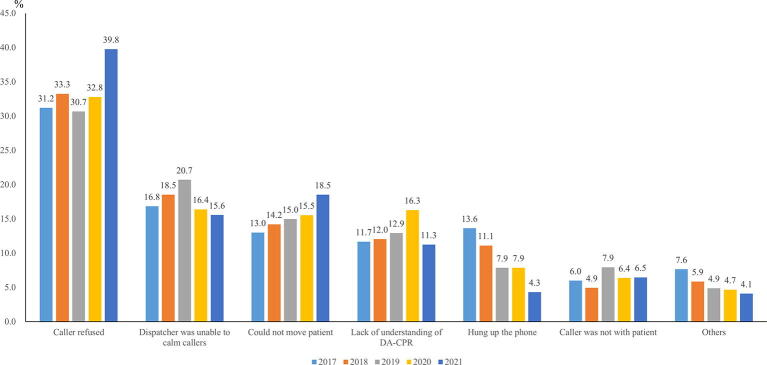
The DA-CPR success rate increased from 70.4% in 2017 to 79.2% in 2021. The proportion of dispatcher instructions not performed despite the suspicion of cardiac arrest was 8.0% in 2021 (Fig. 2). The most identified barrier was “caller refused” (39.8% in 2021), which tended to increase during the study period. This was followed by “could not move patient” (18.5%), “dispatcher was unable to calm the caller” (15.6%), “lack of understanding of DA-CPR” (11.3%), “caller was not with the patient” (6.5%), “hung up the phone” (4.3%), and “others” (4.1%) (Fig. 3). Factors identified as independent risk factors for unsuccessful DA-CPR were age > 65 years, male sex, non-metropolitan area, private place, unwitnessed status, bystander characteristics (non-family member or non-cohabitant, female sex, and uneducated status for CPR), and primary call dispatchers not receiving first-aid training (Table 2). Risk factors for unsuccessful DA-CPR showed similar results after multiple imputation (Table A.1). Table A.2 showed the estimated causal mediational effects of independent variables on unsuccessful DA-CPR via witnessed status. The effect of witnessed status as a mediator was significant for most risk factors for unsuccessful DA-CPR except age, more than 65 years old (0.9998 (0.999–1.001), P = 0.593) and male (1.000 (0.999–1.001), P = 0.989).
Fig. 2.
DA-CPR compliance rate across the study period.
Fig. 3.
Reasons for dispatcher instructions not being performed despite suspicion of cardiac arrest.
Table 2.
Risk factors for unsuccessful DA-CPR.
| Independent variables | Adjusted OR (95% CI)* |
|---|---|
| Age, more than 65 years old | 1.474 (1.401–1.552) |
| Male | 1.167 (1.112–1.225) |
| Non-Metropolitan area | 1.326 (1.264–1.390) |
| Location of arrest | |
| Private place | 1.204 (1.111–1.306) |
| Others | 1.790 (1.472–2.176) |
| Public place | Ref |
| Unwitnessed | 1.324 (1.264–1.387) |
| Bystanders, family member or cohabitant | 0.591 (0.555–0.629) |
| Bystanders, sex | |
| Female | 1.363 (1.299–1.429) |
| Unknown | 9.239 (8.290–10.297) |
| Male | Ref |
| Bystanders, educational status for CPR | |
| No education | 1.699 (1.593–1.812) |
| Unknown | 3.787 (3.544–4.046) |
| Education | Ref |
| Qualification of primary call dispatcher | |
| Nurse | 1.049 (0.954–1.154) |
| First aid trainee | 1.001 (0.942–1.065) |
| Others without first aid training | 1.129 (1.070–1.190) |
| Emergency medical technician | Ref |
Hosmer-Lemeshow Goodness-of-fit: χ2 28.9952 (P = 0.0003).
DA-CPR, dispatcher-assisted cardiopulmonary resuscitation; OR, odds ratio; CI, confidence interval.
aAdjusted for age, sex, urbanization, location of arrest, day of week, time of day, witnessed status, bystander characteristics (relationship with patient, age, sex, educational status for CPR), and qualifications of primary and secondary call dispatchers.
Discussion
In this retrospective observational study, the successful DA-CPR group had a shorter call to EMS dispatch time interval, shorter call to first compression time interval, and better clinical outcomes. We also identified major risk factors for unsuccessful DA-CPR, which were particularly modifiable, including bystander characteristics and the qualification of primary call dispatcher.
The successful DA-CPR rate until EMS arrival has gradually increased, reaching nearly 80% by 2021; however, there are still various barriers to DA-CPR. Among these barriers, “caller refused” was consistently identified as the most common reason, and other reasons such as “dispatcher was unable to calm caller” and “lack of understanding of DA-CPR” also showed no clear improvement trend during the study period. These results were consistent with previous studies, and what is notable is that the above reasons are considered modifiable.15, 21 Therefore, we should consider whether the current DA-CPR protocol is appropriate and what additional strategies may be required to improve adherence. According to the latest CPR guidelines, moving a patient from the bed to the floor can cause a significant delay in providing CPR, so the reason “could not move the patient” is expected to improve in the future.27
Patients > 65 years and those with OHCA occurring in non-metropolitan areas and private places were found to be risk factors for unsuccessful DA-CPR, which is in agreement with the results of previous studies.14, 19, 21 Conversely, our results showed that male patients did not successfully receive DA-CPR until EMS arrival. This differs from previous findings that male patients are more likely to receive bystander CPR and DA-CPR.28, 29 However, this may result from differences in the study population. This study compared the characteristics of patients with OHCA according to DA-CPR compliance; cases already providing bystander CPR before dispatcher instructions were issued were excluded. In addition, previous studies have been limited to OHCAs that occurred only in public places.
Most risk factors for unsuccessful DA-CPR were largely mediated by witnessed status, indicating that witnessed bystanders play an essential role in successful DA-CPR. Therefore, successful DA-CPR requires sufficient consideration of modifiable factors related to bystander characteristics. Considering that > 80% of the OHCAs included in this study occurred in private places, most cardiac arrest patients were male, and most bystanders were family members and cohabitants, it would be appropriate to deduce most bystanders were female. In the logistic regression analysis with and without multiple imputation, female bystanders were identified as an independent risk factor for unsuccessful DA-CPR, consistent with previous studies.30, 31
Bystanders not educated in CPR were also found to be a risk factor for unsuccessful DA-CPR. Failure to recognize cardiac arrest is the most common reason for unsuccessful DA-CPR. Bystanders might have difficulty providing DA-CPR appropriately, reporting agonal breathing as a sign of life, or mistaking seizure-like movements for a seizure rather than a cardiac arrest.9, 15 Therefore, when providing CPR training to the general public, focusing on proper recognition of cardiac arrest is necessary, and dispatchers can be trained to overcome these barriers and identify cardiac arrest from a caller’s description. When bystanders were family members or cohabitants, patients with OHCA were more likely to receive DA-CPR until EMS arrival successfully. This result is different from those of previous studies where bystanders in a private place seemed to be panicked, making it difficult to provide prompt bystander CPR.32, 33 However, because most OHCAs in this study occurred in private places, most bystanders were likely family members or cohabitants. In addition, in the unsuccessful DA-CPR group, the proportion of ‘others’ in the relationship with the patients was high (24.7%), limiting the interpretation of the results.
Primary call dispatchers who did not receive first-aid training were identified as risk factors for unsuccessful DA-CPR. Because bystanders frequently panic, dispatchers should provide assertive instructions to focus their attention.8 Therefore, dispatcher competency is critical in providing high-quality DA-CPR, and as shown in this study, DA-CPR success can vary depending on the qualification level of the primary call dispatcher.18 For high-quality dispatcher instructions, it is important to pair primary call dispatchers with people who have completed a minimum level of first aid training and who maintain competency through a continuing education program. As most secondary call dispatchers are assigned as EMTs or nurses, the qualification level of secondary call dispatchers does not appear to be a risk factor for unsuccessful DA-CPR.
The high quality of the DA-CPR protocol may be attributed to the rigorous quality improvement (QI) process. It includes direct observation and real-time feedback to dispatchers, review of calls for each identified and unidentified cardiac arrest, and measurement and auditing of their performance.9, 34 However, in Korea, written-based assessment and feedback are being conducted on partially sampled DA-CPR audio recordings; therefore, systematic strategies should be considered for better quality control. Furthermore, most dispatch centers in Korea have limited staff dedicated to QI, and most emergency medical directors (EMD) in each dispatch center oversee ancillary work in addition to their jobs in the ED. Thus, there are few opportunities for EMDs and dispatchers to meet, and there is a need to create an active atmosphere that allows free communication between the EMDs and dispatchers for more effective QI activities.9
These barriers mainly emerge through audio calls and video-instructed DA-CPR has been proposed as an alternative. Video-instructed DA-CPR has advantages in that it allows dispatchers to provide bystanders with high-quality CPR with visual support and real-time feedback. It can improve the quality of bystander CPR and increase survival outcomes.13, 35 Its effectiveness has been demonstrated in Seoul and should be implemented nationwide.36 Well-constructed DA-CPR protocols allow dispatchers to quickly recognize OHCA and reinforce positive instructions until the EMS arrives. Successful DA-CPR implementation represents an essential link in the chain of survival and could save more lives in patients with OHCA.
This study had several limitations. First, this retrospective observational study may have had potential confounders that influenced exposure and outcomes. Second, our results were derived using standardized data forms, and owing to the complex nature of OHCA calls, the data might not have been uploaded properly for variables that did not fit into predefined categories. Third, the data entered by the dispatchers were ascertained through audio calls, making it challenging to eliminate inter-dispatcher variability. Fourth, there were many missing values regarding the characteristics of bystanders, especially sex and educational status for CPR. Current dispatcher protocols require dispatchers to ask questions; however, it is not mandatory for all emergency calls. Particularly in the unsuccessful DA-CPR group, DA-CPR compliance was low, making it difficult to collect such information. We attempted to reevaluate this issue using multiple imputation methods; however, there might be limitations to interpretation. Finally, data on socioeconomic status and individual dispatcher capabilities, known to affect DA-CPR compliance, were unavailable, which could have resulted in bias.
Conclusions
Successful DA-CPR until EMS arrival can shorten the chest compression time and improve survival outcomes. Bystanders who were not family members, not cohabitants, female, or not educated in CPR, and primary call dispatchers not receiving first-aid training were found to be risk factors for unsuccessful DA-CPR. Understanding the barriers to DA-CPR can help establish multidisciplinary strategies to overcome them and improve survival outcomes in patients with OHCA.
Funding acknowledgement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Dong Hyun Park: Writing – original draft, Visualization, Formal analysis. Gwan Jin Park: Writing – original draft, Methodology, Data curation, Conceptualization. Young Min Kim: Validation, Resources, Data curation. Hyun Seok Chai: Validation, Resources, Data curation. Sang Chul Kim: Writing – review & editing, Supervision, Conceptualization. Hoon Kim: Writing – review & editing, Supervision. Suk Woo Lee: Writing – review & editing, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100725.
Contributor Information
Dong Hyun Park, Email: pdh0576@naver.com.
Gwan Jin Park, Email: pkj83531@naver.com.
Young Min Kim, Email: zeliard1@empas.com.
Hyun Seok Chai, Email: viot-33@hanmail.net.
Sang Chul Kim, Email: ooiarahan@nate.com.
Hoon Kim, Email: nichekh2000@hanmail.net.
Suk Woo Lee, Email: drrhec@chungbuk.ac.kr.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Tsao C.W., Aday A.W., Almarzooq Z.I., et al. Heart disease and stroke Statistics-2023 update: a report from the American Heart Association. Circulation. 2023;147:e93–e621. doi: 10.1161/CIR.0000000000001123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gräsner J.T., Wnent J., Herlitz J., et al. Survival after out-of-hospital cardiac arrest in Europe – Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 3.Hasselqvist-Ax I., Riva G., Herlitz J., et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 4.Bobrow B.J., Spaite D.W., Berg R.A., et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447–1454. doi: 10.1001/jama.2010.1392. [DOI] [PubMed] [Google Scholar]
- 5.Park G.J., Song K.J., Shin S.D., et al. Timely bystander CPR improves outcomes despite longer EMS times. Am J Emerg Med. 2017;35:1049–1055. doi: 10.1016/j.ajem.2017.02.033. [DOI] [PubMed] [Google Scholar]
- 6.Girotra S., van Diepen S., Nallamothu B.K., et al. Regional variation in out-of-hospital cardiac arrest survival in the United States. Circulation. 2016;133:2159–2168. doi: 10.1161/CIRCULATIONAHA.115.018175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ong M.E., Shin S.D., De Souza N.N., et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: the Pan Asian Resuscitation Outcomes Study (PAROS) Resuscitation. 2015;96:100–108. doi: 10.1016/j.resuscitation.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 8.Bobrow B.J., Panczyk M., Subido C. Dispatch-assisted cardiopulmonary resuscitation: the anchor link in the chain of survival. Curr Opin Crit Care. 2012;18:228–233. doi: 10.1097/MCC.0b013e328351736b. [DOI] [PubMed] [Google Scholar]
- 9.Kurz M.C., Bobrow B.J., Buckingham J., et al. Telecommunicator cardiopulmonary resuscitation: a policy statement from the American Heart Association. Circulation. 2020;141:e686–e700. doi: 10.1161/CIR.0000000000000744. [DOI] [PubMed] [Google Scholar]
- 10.Berg K.M., Cheng A., Panchal A.R., et al. Part 7: Systems of care: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S580–S604. doi: 10.1161/CIR.0000000000000899. [DOI] [PubMed] [Google Scholar]
- 11.Ong M.E.H., Shin S.D., Ko P.C., et al. International multi-center real world implementation trial to increase out-of-hospital cardiac arrest survival with a dispatcher-assisted cardio-pulmonary resuscitation package (Pan-Asian resuscitation outcomes study phase 2) Resuscitation. 2022;171:80–89. doi: 10.1016/j.resuscitation.2021.12.032. [DOI] [PubMed] [Google Scholar]
- 12.Kim M.W., Kim T.H., Song K.J., et al. Comparison between dispatcher-assisted bystander CPR and self-led bystander CPR in out-of-hospital cardiac arrest (OHCA) Resuscitation. 2021;158:64–70. doi: 10.1016/j.resuscitation.2020.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Bielski K., Böttiger B.W., Pruc M., et al. Outcomes of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation: a systematic review and meta-analysis. Ann Med. 2022;54:464–471. doi: 10.1080/07853890.2022.2032314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hauff S.R., Rea T.D., Culley L.L., Kerry F., Becker L., Eisenberg M.S. Factors impeding dispatcher-assisted telephone cardiopulmonary resuscitation. Ann Emerg Med. 2003;42:731–737. doi: 10.1016/s0196-0644(03)00423-2. [DOI] [PubMed] [Google Scholar]
- 15.Ho A.F., Sim Z.J., Shahidah N., et al. Barriers to dispatcher-assisted cardiopulmonary resuscitation in Singapore. Resuscitation. 2016;105:149–155. doi: 10.1016/j.resuscitation.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 16.Castrén M., Karlsten R., Lippert F., et al. Recommended guidelines for reporting on emergency medical dispatch when conducting research in emergency medicine: the Utstein style. Resuscitation. 2008;79:193–197. doi: 10.1016/j.resuscitation.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Hardeland C., Olasveengen T.M., Lawrence R., et al. Comparison of Medical Priority Dispatch (MPD) and Criteria Based Dispatch (CBD) relating to cardiac arrest calls. Resuscitation. 2014;85:612–616. doi: 10.1016/j.resuscitation.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 18.Riou M., Ball S., Whiteside A., et al. ‘We’re going to do CPR’: a linguistic study of the words used to initiate dispatcher-assisted CPR and their association with caller agreement. Resuscitation. 2018;133:95–100. doi: 10.1016/j.resuscitation.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 19.Park J.H., Ro Y.S., Shin S.D., Song K.J., Hong K.J., Kong S.Y. Dispatcher-assisted bystander cardiopulmonary resuscitation in rural and urban areas and survival outcomes after out-of-hospital cardiac arrest. Resuscitation. 2018;125:1–7. doi: 10.1016/j.resuscitation.2018.01.026. [DOI] [PubMed] [Google Scholar]
- 20.Lee S.Y., Ro Y.S., Shin S.D., et al. Interaction effects between highly-educated neighborhoods and dispatcher-provided instructions on provision of bystander cardiopulmonary resuscitation. Resuscitation. 2016;99:84–91. doi: 10.1016/j.resuscitation.2015.11.027. [DOI] [PubMed] [Google Scholar]
- 21.Fukushima H., Panczyk M., Spaite D.W., et al. Barriers to telephone cardiopulmonary resuscitation in public and residential locations. Resuscitation. 2016;109:116–120. doi: 10.1016/j.resuscitation.2016.07.241. [DOI] [PubMed] [Google Scholar]
- 22.Song K.J., Shin S.D., Park C.B., et al. Dispatcher-assisted bystander cardiopulmonary resuscitation in a metropolitan city: a before-after population-based study. Resuscitation. 2014;85:34–41. doi: 10.1016/j.resuscitation.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Park J.H., Song K.J., Shin S.D. The prehospital emergency medical service system in Korea: Its current status and future direction. Clin Exp Emerg Med. 2023;10:251–254. doi: 10.15441/ceem.23.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perkins G.D., Jacobs I.G., Nadkarni V.M., et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand council on resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, resuscitation council of Southern Africa, resuscitation council of Asia); and the American Heart Association emergency cardiovascular care committee and the council on cardiopulmonary, critical care, perioperative and resuscitation. Resuscitation. 2015;96:328–340. doi: 10.1016/j.resuscitation.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Liu Y., De A. Multiple imputation by fully conditional specification for dealing with missing data in a large epidemiologic study. Int J Stat Med Res. 2015;4(3):287–295. doi: 10.6000/1929-6029.2015.04.03.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rijnhart J.J.M., Lamp S.J., Valente M.J., MacKinnon D.P., Twisk J.W.R., Heymans M.W. Mediation analysis methods used in observational research: a scoping review and recommendations. BMC Med Res Methodol. 2021;21(1):226. doi: 10.1186/s12874-021-01426-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olasveengen T.M., Mancini M.E., Perkins G.D., et al. Adult basic life support: International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A35–A79. doi: 10.1016/j.resuscitation.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blewer A.L., McGovern S.K., Schmicker R.H., et al. Gender disparities among adult recipients of bystander cardiopulmonary resuscitation in the public. Circ Cardiovasc Qual Outcomes. 2018;11 doi: 10.1161/CIRCOUTCOMES.118.004710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ko S.Y., Ahn K.O., Do Shin S., Park J.H., Lee S.Y. Effects of telephone-assisted cardiopulmonary resuscitation on the sex disparity in provision of bystander cardiopulmonary resuscitation in public locations. Resuscitation. 2021;164:101–107. doi: 10.1016/j.resuscitation.2021.03.014. [DOI] [PubMed] [Google Scholar]
- 30.Aldridge E.S., Perera N., Ball S., et al. Barriers to CPR initiation and continuation during the emergency call relating to out-of-hospital cardiac arrest: a descriptive cohort study. Resuscitation. 2024;195 doi: 10.1016/j.resuscitation.2023.110104. [DOI] [PubMed] [Google Scholar]
- 31.Case R., Cartledge S., Siedenburg J., et al. Identifying barriers to the provision of bystander cardiopulmonary resuscitation (CPR) in high-risk regions: a qualitative review of emergency calls. Resuscitation. 2018;129:43–47. doi: 10.1016/j.resuscitation.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 32.Aldridge E.S., Perera N., Ball S., Finn J., Bray J. A scoping review to determine the barriers and facilitators to initiation and performance of bystander cardiopulmonary resuscitation during emergency calls. Resusc plus. 2022;11 doi: 10.1016/j.resplu.2022.100290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martinage A., Penverne Y., Le Conte P., et al. Predictive factors of successful telephone-assisted cardiopulmonary resuscitation. J Emerg Med. 2013;44:406–412. doi: 10.1016/j.jemermed.2012.02.066. [DOI] [PubMed] [Google Scholar]
- 34.Tanaka Y., Taniguchi J., Wato Y., Yoshida Y., Inaba H. The continuous quality improvement project for telephone-assisted instruction of cardiopulmonary resuscitation increased the incidence of bystander CPR and improved the outcomes of out-of-hospital cardiac arrests. Resuscitation. 2012;83:1235–1241. doi: 10.1016/j.resuscitation.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 35.Linderoth G., Rosenkrantz O., Lippert F., et al. Live video from bystanders’ smartphones to improve cardiopulmonary resuscitation. Resuscitation. 2021;168:35–43. doi: 10.1016/j.resuscitation.2021.08.048. [DOI] [PubMed] [Google Scholar]
- 36.Lee H.S., You K., Jeon J.P., Kim C., Kim S. The effect of video-instructed versus audio-instructed dispatcher-assisted cardiopulmonary resuscitation on patient outcomes following out of hospital cardiac arrest in Seoul. Sci Rep. 2021;11:15555. doi: 10.1038/s41598-021-95077-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.