Abstract
Background
Gluteoplasty or gluteal augmentation is a popular cosmetic procedure that is used to improve the volume, shape, and contour of the buttocks.
Objectives
This bibliometric analysis aims to characterize emerging research trends and to assess the methodological quality of the highest impact gluteoplasty research.
Methods
The 100 most-cited publications in gluteoplasty were identified on Web of Science, across all available journal years (from Inception to August 2023). Study details, including the citation count, main content focus, and outcome measures, were extracted and tabulated from each publication. Oxford Centre for Evidence Based Medicine level of evidence (LOE) of each study was assessed.
Results
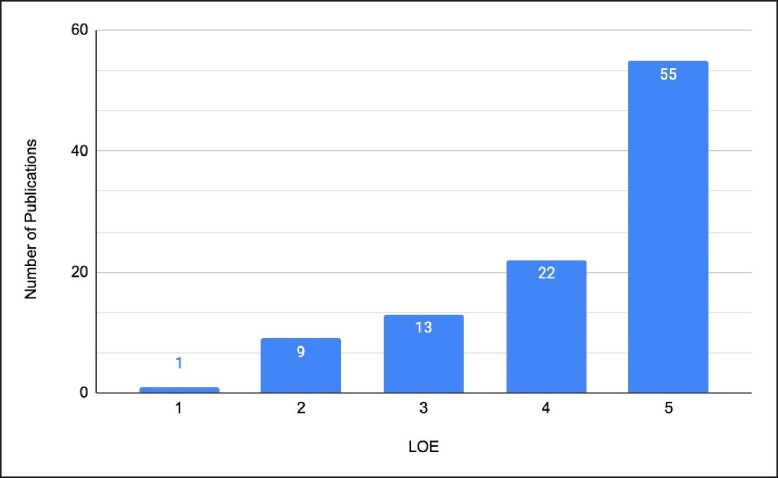
The 100 most-cited publications regarding gluteoplasty were cited by a total of 2375 publications. Citations per publication ranged from 5 to 176 (mean 23.75 ± 25.86), with the highest-cited study being authored by Simonacci, discussing autologous fat grafting (n = 176). Most publications were LOE 5 (n = 55), representative of the large number of case series and reports. The number of publications for LOE 1, 2, 3, and 4 was 1, 9, 13, and 22, respectively. The main content focus was “surgical technique” in 38 publications, followed by “outcomes” (n = 34) and “risk factors/prognosis” (n = 10). Patient-reported outcome measures (PROMs) were used in 20 publications, and 33 publications reported aesthetic outcome measures.
Conclusions
This analysis demonstrates a need for improvement in research methodologies regarding gluteoplasty research. This advancement would be facilitated by robust, high-quality research through randomized control trials and multicenter studies, as well as the further development of validated PROMs for gluteoplasty.
Level of Evidence: 2

The popularity of gluteal augmentation has increased significantly in recent years especially in south and central America.1 The first description of this procedure was documented by Bartels et al in 1969 to correct buttock asymmetry by implanting breast silicone but it has now been used increasingly for aesthetic correction.2,3 The American Society for Aesthetic Plastic Surgery reported a 280% increase in the annual number of gluteal augmentations performed in the United States of America in 2015 compared with 2011.4 Within 2022 alone, >37,000 patients underwent buttock enhancement.5 This is partly due to the increased recognition of a “beautiful buttock” which contributes to beauty and attraction in most cultures as well as increasing awareness of social media beauty.6,7
Despite cultural and geographical differences in the understanding of ideal buttocks, Mendieta argued that buttock can be classified into 4 different shapes including A shape, V shape, round shape, and square shape. The author suggested that the A shape represents the most ideal shape with equal volume on all 4 sides of the buttock providing a more youthful look.7 Other assessment methods have been utilized to aid in surgical planning and define the ideal buttock shape, including the golden waist-to-hip ratio.8,9 Despite so, beauty remained subjective to the standards of the patient, and no standardized system has yet been implemented.
Surgeons have utilized different techniques to achieve gluteal augmentation. These include autologous fat transfer/grafting (gluteal lipoinjection), prosthesis implantation, autologous tissue flaps, hyaluronic acid gel injection, and combined surgical techniques.10 Nonetheless, autologous fat transfer and prosthesis implantation have remained as the commoner techniques preferred by surgeons, due to the low complication rate associated with autologous fat grafting and high satisfaction rate of prosthesis implants. Despite their advantages, both techniques have faced scrutiny due to their limitations, which include fatal complications such as fat embolism associated with autologous fat grafting, and high complication rates associated with implants.6,10-12 Autologous fat transfer has come under increased scrutiny due to its complication profile, which includes fat embolism and associated mortality; there have been 25 confirmed pulmonary fat embolism–related deaths in the United States over a 5.75-year time frame.11,13-15 The British Association of Aesthetic Plastic Surgeons recommended to ban the procedure in 2021. This has been lifted following safety regulations being brought in with the use of ultrasound-guided fat grafting.16
There has been a growing number of publications about gluteal augmentation from 1999 to 2021 as shown by a bibliometric analysis by Dai et al.17 Bibliometrics, the quantitative analysis of publications, especially scholarly literature, produces gainful insight into research trends and impact. Our study aims to provide a qualitative and quantitative examination of the existing articles on gluteal augmentation, including autologous fat transfer, to evaluate the current research trends and past research topics and to provide a prediction of future research objectives.
METHODS
A literature review was performed to identify the 100 most highly cited publications on gluteoplasty. All journal publications available on the online database, Web of Science (Clarivate Analytics, Philadelphia, PA), were searched using the search terms: “gluteal fat grafting” OR “gluteal augmentation” OR “brazilian butt lift” OR “gluteal lipoinjection” OR “augmentation gluteoplasty” OR “buttock augmentation” as a “topic” on August 29, 2023. The timespan covered all available years (1973-2023). The inclusion criteria were journal publications from this search strategy. The exclusion criteria were publications not in English, papers not focused on gluteoplasty, animal studies, other surgical procedure, and duplicate publications. The level of evidence (LOE) was assessed as per the Oxford Centre for Evidence Based Medicine (OCEBM) system (2011).18
The search yielded a total of 285 journal publications, which were subsequently ranked based on the number of times cited. Publications with an equal number of citations were separated using the mean number of citations per year. To ensure that the publications were directly relevant to gluteoplasty, 2 reviewers (N.P.-B. and A.A.) independently screened titles and abstracts until 100 journal publications were included. Discrepancies were resolved by consensus discussion with the senior author (A.K.), with any remaining inconsistencies were ratified by review of the publication's full text. A total of 182 journal publications were screened to provide the most frequent 100 publications for inclusion. Reasons for exclusion of the other publications are specified in Figure 1.
Figure 1.
Summary flow chart of methodology. Screening and eligibility allowed the extraction of the 100 most-cited papers.
Data were extracted from full-text publications in a standardized online computer spreadsheet (Google Sheets: Google LLC, Mountain View, CA). Data extraction included publication title, author list, corresponding author list, publication year, source journal, total citations, mean number of citations per year, geographical study setting, funding source, study design, LOE, main subject/content focus, declaration of conflict of interest (CoI), and the use of validated clinical, cosmetic, and patient-reported outcome measures (PROMs).
RESULTS
Citation Analysis
The 100 most-cited publications regarding gluteoplasty were cited by 2375 publications. The number of citations accumulated per paper ranged from 5 to 176. Publications were cited with a mean of 23.75 times ± 25.86. The mean number of citations per publication per year ranged from 0.44 to 25.14 (mean 2.96; Table 1). The top 100 studies from Table 1 have been referenced.3,11,13,14,19-112
Table 1.
One Hundred Most-Cited Publications Regarding Gluteal Augmentation
| Rank | Authors | Corresponding author | Total citations | Mean citations per year |
|---|---|---|---|---|
| 1 | Simonacci, F et al | Simonacci, F | 176 | 25.14 |
| 2 | Mofid, MM et al | Mofid, MM | 134 | 19.14 |
| 3 | Cárdenas-Camarena, L et al | Cárdenas-Camarena, L | 105 | 11.67 |
| 4 | Sinno, S et al | Wall, S | 81 | 10.13 |
| 5 | Gonzalez, R | Gonzalez, R | 66 | 3.3 |
| 6 | Murillo, W | Murillo, W | 66 | 3.3 |
| 7 | Oranges, CM et al | Oranges, CM | 58 | 8.29 |
| 8 | Conde-Green, A et al | Conde-Green, A | 52 | 6.5 |
| 9 | Mofid, MM et al | Mofid, MM | 52 | 4.73 |
| 10 | Villanueva, NL et al | Rohrich, RJ | 51 | 8.5 |
| 11 | Wolf, GA et al | Gallego, G | 46 | 2.56 |
| 12 | Del Vecchio, DA et al | Rohrich, RJ | 42 | 7 |
| 13 | de Pedroza, LV | de Pedroza, LV | 42 | 1.75 |
| 14 | Colwell, AS and Borud, LJ | Borud, LJ | 40 | 2.35 |
| 15 | Toledo, L | Toledo, L | 38 | 4.22 |
| 16 | Guisantes, E et al | Guisantes, E | 34 | 2.83 |
| 17 | Senderoff, D | Senderoff, D | 34 | 2.62 |
| 18 | Harrison, D and Selvaggi, G | Harrison, D | 34 | 2 |
| 19 | Nicareta, B et al | Pereira, LH | 33 | 2.54 |
| 20 | Astarita, DC et al | Astarita, DC | 32 | 3.56 |
| 21 | Serra, F et al | Serra, F | 31 | 2.21 |
| 22 | Cocke, WM and Ricketson, G | Cocke, WM | 31 | 0.61 |
| 23 | Centeno, RF and Young, VL | Centeno, RF | 30 | 1.67 |
| 24 | Mendieta, C | Mendieta, C | 30 | 1.67 |
| 25 | Vartanian, E et al | Macias, LH | 29 | 4.83 |
| 26 | Rosique, RG et al | Rosique, RG | 28 | 2.8 |
| 27 | Chopan, M et al | Katz, AJ | 27 | 5.4 |
| 28 | Abboud, MH et al | Dibo, SA | 26 | 2.89 |
| 29 | Serra, F et al | Serra, F | 26 | 2.17 |
| 30 | Wall, S et al | Wall, S | 25 | 5 |
| 31 | Centeno, RF | Centeno, RF | 25 | 1.39 |
| 32 | Cansancao, AL et al | Cansancao, AL | 24 | 4 |
| 33 | Sozer, SO et al | Sozer, SO | 24 | 1.5 |
| 34 | Hidalgo, J | Hidalgo, J | 24 | 1.33 |
| 35 | Rios, L and Gupta, V | Rios, L | 23 | 5.75 |
| 36 | Mendieta, CG and Sood, A | Sood, A | 23 | 3.83 |
| 37 | Kalaaji, A et al | Kalaaji, A | 22 | 4.4 |
| 38 | Ghavami, A and Villanueva, NL | Ghavami, A | 22 | 3.67 |
| 39 | Cardenas-Camarena, L et al | Cardenas-Camarena, L | 22 | 2.75 |
| 40 | Serra, F et al | Serra, F | 22 | 2 |
| 41 | Aboudib, JH et al | de Castro, CC | 22 | 1.83 |
| 42 | de la Pena, JA et al | de la Pena, JA | 22 | 1.22 |
| 43 | Willemsen, JCN et al | Lindenblatt, N | 20 | 1.82 |
| 44 | Flores-Lima, G et al | Flores-Lima, G | 20 | 1.82 |
| 45 | Rosique, RG and Rosique, MJF | Rosique, RG | 19 | 3.17 |
| 46 | Ramos-Gallardo, G et al | Ramos-Gallardo, G | 19 | 3.17 |
| 47 | Raposo-Amaral, CE et al | Raposo-Amaral, CE | 19 | 01.06 |
| 48 | Senderoff, D | Senderoff, D | 18 | 2.25 |
| 49 | de-Runz, A et al | de-Runz, A | 18 | 2 |
| 50 | Bayter-Marin, JE et al | Cardenas-Camarena, L | 17 | 2.83 |
| 51 | Singh, M et al | Talbot, SG | 17 | 2.13 |
| 52 | Del Vecchio, DA and Rohrich, RJ | Del Vecchio, DA | 14 | 3.5 |
| 53 | Pena, W et al | Cardenas-Camarena, L | 14 | 2.8 |
| 54 | Frank, K et al | Cotofana, S | 14 | 2.8 |
| 55 | Alvarez-Alvarez, FA et al | Alvarez-Alvarez, FA | 14 | 2.8 |
| 56 | Wang, G et al | Cao, WG | 14 | 1.27 |
| 57 | Asserson, DB et al | Asserson, DB | 13 | 2.6 |
| 58 | Mendieta, C and Stuzin, JM | Stuzin, JM | 13 | 2.17 |
| 59 | Salcedo, JAD et al | Salcedo, JAD | 13 | 0.72 |
| 60 | Serra, F et al | Serra, F | 12 | 1.33 |
| 61 | Cansancao, AL et al | Cansancao, AL | 11 | 2.2 |
| 62 | Menardias, B et al | Bertheuil, N | 11 | 1.83 |
| 63 | Andrade, GA et al | Coltro, PS | 11 | 1.57 |
| 64 | Hunstad, JP and Repta, R | Hunstad, JP | 11 | 0.73 |
| 65 | Del Vecchio, DA and Kenkel, JM | Del Vecchio, DA | 10 | 5 |
| 66 | Ordenana, C et al | Zins, JE | 10 | 2.5 |
| 67 | O'Neill, RC et al | Winocour, SJ | 10 | 2.5 |
| 68 | Shah, B | Shah, B | 10 | 1.67 |
| 69 | Levan, P and Habre, SB | Levan, P | 10 | 1.43 |
| 70 | Moscatiello, F et al | Moscatiello, F | 10 | 0.71 |
| 71 | Le Louarn, C and Pascal, JF | Le Louarn, C | 10 | 0.63 |
| 72 | Durairaj, KK et al | Durairaj, KK | 9 | 2.25 |
| 73 | Cardenas-Camarena, L and Duran, H | Cardenas-Camarena, L | 9 | 1.5 |
| 74 | Godoy, PM and Munhoz, AM | Godoy, PM | 9 | 1.5 |
| 75 | Swanson, E | Swanson, E | 9 | 1.13 |
| 76 | Paul, S et al | Paul, S | 9 | 1 |
| 77 | O'Neill, RC et al | Winocour, SJ | 8 | 2.67 |
| 78 | Che, DH and Xiao, ZB | Xiao, ZB | 8 | 2 |
| 79 | Everett, M et al | Everett, M | 8 | 1.33 |
| 80 | Nasseri, E | Nasseri, E | 8 | 1 |
| 81 | Jaimovich, CA et al | Almeida, AWR | 8 | 0.57 |
| 82 | Pazmino, P and Garcia, O | Pazmino, P | 7 | 3.5 |
| 83 | Cardenas-Camarena, L et al | Cardenas-Camarena, L | 7 | 1.75 |
| 84 | Pane, TA | Pane, TA | 7 | 1.4 |
| 85 | Chia, CT et al | Chia, CT | 7 | 1.17 |
| 86 | Wall, S and Del Vecchio, DA | Wall, S | 7 | 1 |
| 87 | Chang, H et al | Heo, C | 7 | 0.44 |
| 88 | Raposo-Amaral, CE et al | Raposo-Amaral, CE | 7 | 0.44 |
| 89 | Leyva, A et al | Leyva, A | 6 | 1 |
| 90 | Gonzalez, R and Gonzalez, R | Gonzalez, R | 6 | 1 |
| 91 | Vasilakis, V et al | Vasilakis, V | 6 | 1 |
| 92 | Whitfield, RM et al | Whitfield, RM | 6 | 0.86 |
| 93 | Muresan, C et al | Shureih, SF | 6 | 0.6 |
| 94 | Lourenço, LM et al | Lourenço, LM | 5 | 2.5 |
| 95 | Del Vecchio, DA et al | Del Vecchio, DA | 5 | 1.67 |
| 96 | Abboud, M et al | Abboud, M | 5 | 1.67 |
| 97 | Uz, I et al | Uz, I | 5 | 1.25 |
| 98 | Fadavi, D et al | Fadavi, D | 5 | 1.25 |
| 99 | Safran, T et al | Davison, PG | 5 | 1.25 |
| 100 | Singer, R | Singer, R | 5 | 1 |
The most frequently cited publication (n = 176) was authored by Simonacci et al, and was published in 2017. The authors undertook a literature review and discussed the procedure, applications, and outcomes of autologous fat grafting (lipofilling).19 It was concluded that lipofilling can be applied to various plastic surgery procedures, namely gluteoplasty; however, its effectiveness could be limited by the amount of fatty tissue a patient possesses. Publication numbers for corresponding authors were recorded and the outcomes compared first. Cárdenas-Camarena had the largest number of authorships as corresponding author, at 5 each. This was followed by Serra (n = 4), with Wall and Del Vecchio both tied at 3 each (Table 1). Following corresponding authorships being calculated, active publications were counted next, with values for authors being calculated by the frequency of first authorships. Del Vecchio, Serra, and Cárdenas-Camarena were the authors with the most number of publications, with each having 4; however, Del Vecchio also had a publication as second author. This was followed by Mendieta at 3 and 6 authors all tied at 2 publications (Cansancao, Centeno, Gonzalez, Mofid, Wall, and Senderoff; Table 1).
Ninety-nine percent of the most frequently cited publications were published in the 2000s and 2010–, with there being 21 publications in the 2000s and 78 publications from 2010 to present day. The most frequently cited publication was published throughout this post-2010 time period (Figure 2). The United States of America was the country with the highest number of publications (n = 50), followed by Brazil (n = 16) then Mexico (n = 9; Table 2).
Figure 2.
Decade analysis of the 100 most-cited publications in gluteal augmentation. These publications increase exponentially as decades progress.
Table 2.
Country Frequency in the 100 Most-Cited Gluteal Augmentation Publications
| Rank | Country | No. of publications |
|---|---|---|
| 1 | USA | 50 |
| 2 | Brazil | 16 |
| 3 | Mexico | 9 |
| 4 | France | 4 |
| 5 | Colombia | 3 |
| 6 | Belgium | 2 |
| 7 | China | 2 |
| 8 | Spain | 2 |
| 9 | Canada | 1 |
| 10 | Dominican Republic | 1 |
| 11 | El Salvador | 1 |
| 12 | Italy | 1 |
| 13 | Netherland | 1 |
| 14 | Norway | 1 |
| 15 | Peru | 1 |
| 16 | South Korea | 1 |
| 17 | Switzerland | 1 |
| 18 | Turkey | 1 |
| 19 | UAE | 1 |
| 20 | UK | 1 |
Six studies formally acknowledged the receipt of funding, a smaller proportion of funding (n = 2) was provided by various private entities such as Allergan (Dublin, Ireland) and Suneva Medical (San Diego, CA). Two publications stated the receival of a grant from a university- or academic-based research organizations, such as The Aesthetic Foundation (Garden Grove, CA). The remaining 2 funding sources included various charitable and private research corporations. Sixty-nine publications explicitly stated receipt of no funding, and the remaining 25 studies did not specify whether they received funding or not from external (governmental, industry, institutional, etc.) or internal (departmental, divisional levels of organizations) sources. Furthermore, 12 publications disclosed potential CoI with most authors stating that they were paid consultants, or the products being studied were provided for by a private corporation. A further 67 publications explicitly stated that there were no CoI to declare and the remaining 21 did not specify, if there were any CoIs or not.
Prevalent Research Themes
The most-cited 100 publications regarding gluteoplasty derived from 18 journals. Plastic and Reconstructive Surgery (PRS) contributed the most publications (n = 31), followed by Aesthetic Surgery Journal (n = 26), with Clinics in Plastic Surgery next (n = 13), then Aesthetic Plastic Surgery (n = 10). The remaining journals contributed 20 publications between them (Table 3). Most of the publications selected for this analysis were from dedicated plastic surgery journals such as Plastic and Reconstructive Surgery and Aesthetic Surgery Journal.
Table 3.
Journal Frequency in the 100 Most-Cited Publications
| Rank | Source journal | No. of publications | Impact factor |
|---|---|---|---|
| 1 | Plastic and Reconstructive Surgery | 31 | 3.6 |
| 2 | Aesthetic Surgery Journal | 26 | 2.9 |
| 3 | Clinics in Plastic Surgery | 13 | 2.3 |
| 4 | Aesthetic Plastic Surgery | 10 | 2.4 |
| 5 | Plastic and Reconstructive Surgery Global Open | 3 | 1.5 |
| 6 | Journal of Plastic Reconstructive and Aesthetic Surgery | 3 | 2.7 |
| 7 | Annals of Plastic Surgery | 2 | 1.5 |
| 8 | Dermatologic Surgery | 2 | 2.4 |
| 9 | Annals of Medicine and Surgery | 1 | 1.7 |
| 10 | Cureus: Journal of Medical Science | 1 | 1.2 |
| 11 | Dermatologic Therapy | 1 | 3.6 |
| 12 | European Journal of Plastic Surgery | 1 | 0.5 |
| 13 | Journal of Cosmetic Dermatology | 1 | 2.3 |
| 14 | Journal of Cutaneous Medicine and Surgery | 1 | 2.3 |
| 15 | Journal of Forensic Sciences | 1 | 1.6 |
| 16 | Journal of Investigative Surgery | 1 | 1.9 |
| 17 | Seminars in Plastic Surgery | 1 | 2.0 |
| 18 | Turkish Journal of Trauma and Emergency Surgery | 1 | 1.1 |
Ten publications on the list were published in journals not specifically related to plastic surgery which includes Dermatologic Surgery, Annals of Medicine and Surgery, Cureus: Journal of Medical Science, Dermatologic Therapy, Journal of Cosmetic Dermatology, Journal of Cutaneous Medicine and Surgery, Journal of Forensic Sciences, Journal of Investigative Surgery, and Turkish Journal of Trauma and Emergency Surgery. Among all the journals included, PRS and Dermatologic Therapy have the highest impact factor (n = 3.6).
Methodological Quality
Almost a quarter of the studies are cohort studies, with 9 having a retrospective model while 11 being prospective in nature. The most frequent study design utilized in this analysis was narrative reviews (n = 32), followed by case series and case reports tied (n = 12). Six systematic reviews were included; however, no randomized controlled trials (RCTs) are included in this study (Figure 3).
Figure 3.
Study designs of the 100 most-cited publications on gluteal augmenation. Narrative reviews were the most popular study design.
Over half of the publications on the list were assessed to be OCEBM LOE 5 (n = 55), this was represented mostly by case series and case reports. Twenty-two publications achieved LOE 4, while 13 publications achieved LOE 3. An additional 9 publications achieved LOE 2 and lastly 1 publication achieved LOE 1 (Figure 4). Upon observation of decade analysis, research output, in terms of the number of publications, greatly increased with each decade passing (1970s; n = 1, 1980s; n = 0, 1990s; n = 0, 2000s; n = 21 2010 to present; n = 78). Study designs of the 100 most-cited research studies on gluteal augmentation are presented in Figure 3.
Figure 4.
The LOE for the 100 most-cited gluteal augmentation publications. Most papers were LOE 5, with more of the remaining papers being a lower LOE than higher. LOE, level of evidence.
Clinical outcomes were reported in 54 of the top 100 most highly cited publications. Outcome measures were categorized in studies. Twenty publications incorporated PROMs, namely patient satisfaction questionnaires, although a majority of these were unvalidated, generic scales. Thirty-three publications incorporated cosmetic outcome measures, including preoperative and postoperative photography, including the Global Aesthetic Improvement Scale and the Mendieta and Sood buttock ptosis classification.51,113
DISCUSSION
This bibliometric analysis, conducted with careful adherence to the predefined methodology, reveals a surge in scholarly engagement and research output on gluteal grafting over the past 2 decades. This escalation reflects the evolution of aesthetic gluteal surgery, driven by innovations in surgical techniques and heightened prioritization of patient safety measures. The 2000s marked a significant turning point, highlighted by an exponential increase in scholarly publications—from none in the preceding decade to 2021. Moreover, an overwhelming 99% of the most-cited articles in gluteal grafting literature originate from this decade, underlining the period's critical role in this field's development. This finding coincides with the introduction of innovative fat grafting techniques and efforts to address safety concerns, particularly fat embolism syndrome—a significant risk associated with gluteal augmentation.114
The top 5 most-cited studies are a modest reflection of current research themes and present as a guide toward potential future literature trends and points toward the themes of our study. The main takeaways from Simonacci et al included that autologous fat grafting is safe for general applications; however, an inherent risk of complications exists when improper technique is applied in the buttocks.19 Both Mofid et al and Cardenas-Camarena et al highlighted the associated increased mortality rate in gluteal fat grafting, most likely due to gluteal blood vessel damage, causing microscopic and macroscopic fat embolism to occur.20,21 From Sinno's study, we can conclude that autologous fat grafting, when compared with silicone buttock implants, has lower complication rates overall.11 Lastly, in 2004 study, Gonzalez outlined the “XYZ method” of inserting implants, which was shown to be a safe method that produces very natural and long-lasting results, with very low rates of complication.22
Our study brings forth several important themes, namely the lack of validated PROMs applicable to gluteal augmentation and the optimization of safety—and by extension, the associated complications. Over a third of the studies’ main subject was “outcomes” (n = 34); a majority of these discussed the safety and efficacy of gluteal augmentation, where there were pitfalls and potential avenues of improvement. Nine studies explored complications as their main subject, where they mentioned all the various complications that can occur with gluteal augmentation and how their risk can be minimized. Our study demonstrates that there is a shortfall of objective evaluations in combination with patient satisfaction questionnaires, with the Mendieta and Sood buttock ptosis classification being the sole validated PROM utilized.51 This bibliometric analysis shows that although there are numerous studies exploring safety, more needs to be done to mitigate the risks associated with this only-increasingly popular procedure.
The pronounced contribution of research from the United States, Brazil, and Mexico (n = 50, 16, and 9 publications, respectively) reflects the greater demand for aesthetic gluteal procedures within these nations.1 It also reflects their pivotal role in pioneering the development of safer, more productive gluteal augmentation techniques. Such contributions have been instrumental in shaping international standards and practices in aesthetic surgery.115 Nonetheless, reliance on studies characterized by lower-level evidence (n = 55), such as case reports and expert opinions (LOE 5), reveals a void in the existing literature—the scarcity of rigorous, evidence-based research to inform and refine clinical practice and policy.116
A particularly optimistic discovery of this analysis is the growing focus on patient-reported outcomes (PROs) as a metric for assessing the success of gluteal augmentation surgeries. Within the realm of cosmetic plastic surgery, experienced surgeons acknowledge that many patients exist who have stellar results but are not satisfied with their results and the converse can also hold true—less than ideal results but the patient is extremely satisfied with their results; in some cases, this can be considered body dysmorphia, although it is context dependent.117 Consequently, it should be acknowledged that to move the field forward, quantitative evaluations must be combined with satisfaction-related outcome instruments.118 Ultimately providing plastic surgeons a means to determine whether the procedure was a success, failure, or somewhere in between. This paradigm shift toward patient-centric measures marks a stride toward acknowledging the centrality of patient satisfaction and overall quality of life as the most important benchmarks of aesthetic surgery's success. Integrating PROs into research has significantly enriched global comprehension of patient experiences, offering a well-rounded perspective on the efficacy of procedures beyond conventional clinical or cosmetic measures.119
The strength of this study lies in its exhaustive analysis of the worldwide research landscape on gluteal grafting, shedding light on prevailing trends, geographical variances, and thematic concentrations within the domain. This exploration aids in identifying specific areas for further inquiry, notably the need for high-caliber comparative studies to determine the safest and most effective gluteal augmentation techniques.
Nevertheless, this bibliometric analysis has inherent limitations. The primary concern among these is the potential inadequacy of citation counts as a measure of research impact, which might not fully represent the significance of more recent studies or those published in niche journals. Additionally, the focus on English literature may overlook relevant studies published in other languages, such as Portuguese or Spanish, possibly skewing the comprehension of global research trends.
Addressing these gaps necessitates future research efforts to prioritize the execution of RCTs and prospective cohort studies, which yield superior evidence on the safety, efficacy, and patient satisfaction rates associated with various gluteal augmentation techniques.120 Equally important is developing and validating standardized, PROMs tailored explicitly for gluteal augmentation patients. Such tools are already present and enable outcome comparisons across studies in facial and breast cosmetic surgery, enriching the evidence base that informs clinical practice and optimizes patient care in aesthetic surgery.121,122
CONCLUSIONS
This extensive bibliometric analysis comprehensively examines the top 100 most highly cited publications regarding the gluteoplasty procedure and shows the evolution and trends in the field over the past 10 decades. Emerging research areas within this field include a multitude of refinements in safety and surgical technique to optimize for aesthetic outcomes and to mitigate complications. Improvements in the quality of gluteoplasty literature must be sought by active prioritization of the publication of methodologically robust studies with higher OCEBM LOE, such as well-designed RCTs or multicenter studies. Furthermore, the adoption of validated PROMs designed for gluteoplasty is centrally important for aligning patient satisfaction with clinical outcomes and providing high-quality evidence-based patient care.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article, including payment of the article processing charge.
REFERENCES
- 1. Rueda JDA, Miranda-Diaz AJ, Cely AG, Leon DCN. A rare case of implant displacement to the contralateral side after gluteal augmentation. Archiv Plast Surg. 2020;47(4):360–364. doi: 10.5999/aps.2019.00325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bartels RJ, O'Malley JE, Douglas WM, Wilson RG. An unusual use of the Cronin breast prosthesis. Case report. Plast Reconstr Surg. 1969;44(5):500. doi: 10.1097/00006534-196944050-00023 [DOI] [PubMed] [Google Scholar]
- 3. Cocke WM, Ricketson G. Gluteal augmentation. Plast Reconstr Surg. 1973;52(1):93. doi: 10.1097/00006534-197307000-00026 [DOI] [PubMed] [Google Scholar]
- 4.The American Society for Aesthetic Plastic Surgery 2015 Procedural Statistics. Accessed October 24, 2023. http://www.surgery.org/sites/default/files/ASAPS-Stats2015.pdf.
- 5.The American Society for Aesthetic Plastic Surgery 2022 Procedural Statistics. Accessed May 12, 2024. https://cdn.theaestheticsociety.org/media/statistics/2022-TheAestheticSocietyStatistics.pdf.
- 6. Park TH, Whang KW. Buttock reshaping with intramuscular gluteal augmentation in an Asian ethnic group: a six-year experience with 130 patients. Ann Plast Surg. 2016;77(3):272–279. doi: 10.1097/SAP.0000000000000399 [DOI] [PubMed] [Google Scholar]
- 7. Ortiz-Ospina E. Our World in Data. The rise in plastic surgery. Accessed October 24, 2023. https://ourworldindata.org/rise-of-social-media.
- 8. Mendieta CG. Classification system for gluteal evaluation. Clin Plast Surg. 2006;33(3):333–346. 10.1016/j.cps.2006.04.006 [DOI] [PubMed] [Google Scholar]
- 9. Dorfman RG, Gupta N, Saadat S, Delong M, Roostaeian J. Gluteal shape framework for augmentation surgery: a systematic review of the literature and proposed classification system. Plast Reconstr Surg. 2023;151(5):748e–757e. doi: 10.1097/PRS.0000000000010078 [DOI] [PubMed] [Google Scholar]
- 10. Oranges CM, Haug M, Schaefer DJ. Body contouring. Plast Reconstr Surg. 2016;138(5):944e–945e. doi: 10.1097/PRS.0000000000002724 [DOI] [PubMed] [Google Scholar]
- 11. Sinno S, Chang JB, Brownstone ND, Saadeh PB, WallS, Jr. Determining the safety and efficacy of gluteal augmentation: a systematic review of outcomes and complications. Plast Reconstr Surg. 2016;137(4):1151–1156. doi: 10.1097/PRS.0000000000002005 [DOI] [PubMed] [Google Scholar]
- 12. Cárdenas-Camarena L, Lacouture AM, Tobar-Losada A. Combined gluteoplasty: liposuction and lipoinjection. Plast Reconstr Surg. 1999;104(5):1524–1531. doi: 10.1097/00006534-199910000-00045 [DOI] [PubMed] [Google Scholar]
- 13. Asserson DB, Kulinich AG, Orbay H, Sahar DE. Differences in complication rates of gluteoplasty procedures that utilize autologous fat grafting, implants, or local flaps. Ann Plast Surg. 2019;82(5S):S342–S344. doi: 10.1097/SAP.0000000000001765 [DOI] [PubMed] [Google Scholar]
- 14. Rosique RG, Rosique MJF, De Moraes CG. Gluteoplasty with autologous fat tissue: experience with 106 consecutive cases. Plast Reconstr Surg. 2015;135(5):1381–1389. doi: 10.1097/PRS.0000000000001167 [DOI] [PubMed] [Google Scholar]
- 15. Wall S, Jr., Del Vecchio D. Commentary on: report on mortality from gluteal fat grafting: recommendations from the ASERF Task Force. Aesthet Surg J. 2017;37(7):807–810. doi: 10.1093/asj/sjx080 [DOI] [PubMed] [Google Scholar]
- 16. Pazmiño P, Del Vecchio D. Static Injection, Migration, and Equalization (SIME): a new paradigm for safe ultrasound-guided Brazilian Butt Lift: safer, faster, better. Aesthet Surg J. 2023;43(11):1295–1306. doi: 10.1093/asj/sjad142 [DOI] [PubMed] [Google Scholar]
- 17. Dai Y, Chen Y, Hu Y, Zhang L. Current knowledge and future perspectives of buttock augmentation: a bibliometric analysis from 1999 to 2021. Aesthet Plast Surg. 2023;47(3):1091–1103. doi: 10.1007/s00266-022-03140-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. OCEBM Levels of Evidence Working Group* . The Oxford Levels of Evidence 2. Oxford Centre for Evidence-Based Medicine; 2011. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. [Google Scholar]
- 19. Simonacci F, Bertozzi N, Grieco MP, Grignaffini E, Raposio E. Procedure, applications, and outcomes of autologous fat grafting. Ann Med Surg (Lond). 2017;20:49–60. doi: 10.1016/j.amsu.2017.06.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mofid MM, Teitelbaum S, Suissa D, Ramirez-Montanana A, Astarita DC, Mendieta C, Singer R. Report on mortality from gluteal fat grafting: recommendations from the ASERF Task Force. Aesthet Surg J. 2017;37(7):796–806. doi: 10.1093/asj/sjx004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cardenas-Camarena L, Bayter JE, Aguirre-Serrano H, Cuenca-Pardo J. Deaths caused by gluteal lipoinjection: what are we doing wrong? Plast Reconstr Surg. 2015;136(1):58–66. doi: 10.1097/PRS.0000000000001364 [DOI] [PubMed] [Google Scholar]
- 22. Gonzalez R. Augmentation gluteoplasty: the XYZ method. Aesthet Plast Surg. 2004;28(6):417–425. doi: 10.1007/s00266-004-3130-6 [DOI] [PubMed] [Google Scholar]
- 23. Murillo WL. Buttock augmentation: case studies of fat injection monitored by magnetic resonance imaging. Plast Reconstr Surg. 2004;114(6):1606–1614. discussion 15-6. doi: 10.1097/01.PRS.0000138760.29273.5D [DOI] [PubMed] [Google Scholar]
- 24. Oranges CM, Tremp M, di Summa PG, Haug M, Kalbermatten DF, Harder Y, Schaefer DJ. Gluteal augmentation techniques: a comprehensive literature review. Aesthet Surg J. 2017;37(5):560–569. doi: 10.1093/asj/sjw240 [DOI] [PubMed] [Google Scholar]
- 25. Condé-Green A, Kotamarti V, Nini KT, Wey PD, Ahuja NK, Granick MS, Lee ES. Fat grafting for gluteal augmentation: a systematic review of the literature and meta-analysis. Plast Reconstr Surg. 2016;138(3):437e–446e. doi: 10.1097/PRS.0000000000002435 [DOI] [PubMed] [Google Scholar]
- 26. Mofid MM, Gonzalez R, de la Peña JA, Mendieta CG, Senderoff DM, Jorjani S. Buttock augmentation with silicone implants: a multicenter survey review of 2226 patients. Plast Reconstr Surg. 2013;131(4):897–901. doi: 10.1097/PRS.0b013e3182818ec0 [DOI] [PubMed] [Google Scholar]
- 27. Villanueva NL, Del Vecchio DA, Afrooz PN, Carboy JA, Rohrich RJ. Staying safe during gluteal fat transplantation. Plast Reconstr Surg. 2018;141(1):79–86. doi: 10.1097/PRS.0000000000003934 [DOI] [PubMed] [Google Scholar]
- 28. Wolf GA, Gallego S, Patron AS, Ramirez F, de Delgado JA, Echeverri A, García GMM. Magnetic resonance imaging assessment of gluteal fat grafts. Aesthet Plast Surg. 2006;30(4):460–468. doi: 10.1007/s00266-005-0202-1 [DOI] [PubMed] [Google Scholar]
- 29. Del Vecchio DA, Villanueva NL, Mohan R, Johnson B, Wan D, Venkataram A, Rohrich RJ. Clinical implications of gluteal fat graft migration: a dynamic anatomical study. Plast Reconstr Surg. 2018;142(5):1180–1192. doi: 10.1097/PRS.0000000000005020 [DOI] [PubMed] [Google Scholar]
- 30. de Pedroza LV. Fat transplantation to the buttocks and legs for aesthetic enhancement or correction of deformities: long-term results of large volumes of fat transplant. Dermatol Surg. 2000;26(12):1145–1149. doi: 10.1046/j.1524-4725.2000.00276.x [DOI] [PubMed] [Google Scholar]
- 31. Colwell AS, Borud LJ. Autologous gluteal augmentation after massive weight loss: aesthetic analysis and role of the superior gluteal artery perforator flap. Plast Reconstr Surg. 2007;119(1):345–356. doi: 10.1097/01.prs.0000244906.48448.5d [DOI] [PubMed] [Google Scholar]
- 32. Toledo LS. Gluteal augmentation with fat grafting: the Brazilian buttock technique: 30 years’ experience. Clin Plast Surg. 2015;42(2):253–261. doi: 10.1016/j.cps.2014.12.004 [DOI] [PubMed] [Google Scholar]
- 33. Guisantes E, Fontdevila J, Rodriguez G. Autologous fat grafting for correction of unaesthetic scars. Ann Plast Surg. 2012;69(5):550–554. doi: 10.1097/SAP.0b013e31821ee386 [DOI] [PubMed] [Google Scholar]
- 34. Senderoff DM. Buttock augmentation with solid silicone implants. Aesthet Surg J. 2011;31(3):320–327. doi: 10.1177/1090820X10396701 [DOI] [PubMed] [Google Scholar]
- 35. Harrison D, Selvaggi G. Gluteal augmentation surgery: indications and surgical management. J Plast Reconstr Aesthet Surg. 2007;60(8):922–928. doi: 10.1016/j.bjps.2006.01.057 [DOI] [PubMed] [Google Scholar]
- 36. Nicareta B, Pereira LH, Sterodimas A, Illouz YG. Autologous gluteal lipograft. Aesthet Plast Surg. 2011;35(2):216–224. doi: 10.1007/s00266-010-9590-y [DOI] [PubMed] [Google Scholar]
- 37. Astarita DC, Scheinin LA, Sathyavagiswaran L. Fat transfer and fatal macroembolization. J Forensic Sci. 2015;60(2):509–510. doi: 10.1111/1556-4029.12549 [DOI] [PubMed] [Google Scholar]
- 38. Serra F, Aboudib JH, Cedrola JP, de Castro CC. Gluteoplasty: anatomic basis and technique. Aesthet Surg J. 2010;30(4):579–592. doi: 10.1177/1090820X10380389 [DOI] [PubMed] [Google Scholar]
- 39. Centeno RF, Young VL. Clinical anatomy in aesthetic gluteal body contouring surgery. Clin Plast Surg. 2006;33(3):347–358. doi: 10.1016/j.cps.2006.05.005 [DOI] [PubMed] [Google Scholar]
- 40. Mendieta CG. Intramuscular gluteal augmentation technique. Clin Plast Surg. 2006;33(3):423–434. doi: 10.1016/j.cps.2006.05.004 [DOI] [PubMed] [Google Scholar]
- 41. Vartanian E, Gould DJ, Hammoudeh ZS, Azadgoli B, Stevens WG, Macias LH. The ideal thigh: a crowdsourcing-based assessment of ideal thigh aesthetic and implications for gluteal fat grafting. Aesthet Surg J. 2018;38(8):861–869. doi: 10.1093/asj/sjx191 [DOI] [PubMed] [Google Scholar]
- 42. Chopan M, White JA, Sayadi LR, Buchanan PJ, Katz AJ. Autogenous fat grafting to the breast and gluteal regions: safety profile including risks and complications. Plast Reconstr Surg. 2019;143(6):1625–1632. doi: 10.1097/PRS.0000000000005617 [DOI] [PubMed] [Google Scholar]
- 43. Abboud MH, Dibo SA, Abboud NM. Power-assisted gluteal augmentation: a new technique for sculpting, harvesting, and transferring fat. Aesthet Surg J. 2015;35(8):987–994. doi: 10.1093/asj/sjv161 [DOI] [PubMed] [Google Scholar]
- 44. Serra F, Aboudib JH, Marques RG. Reducing wound complications in gluteal augmentation surgery. Plast Reconstr Surg. 2012;130(5):706e–713e. doi: 10.1097/PRS.0b013e318267d716 [DOI] [PubMed] [Google Scholar]
- 45. Wall SJ, Delvecchio D, Teitelbaum S, et al. Subcutaneous migration: a dynamic anatomical study of gluteal fat grafting. Plast Reconstr Surg. 2019;143(5):1343–1351. doi: 10.1097/PRS.0000000000005521 [DOI] [PubMed] [Google Scholar]
- 46. Centeno RF. Autologous gluteal augmentation with circumferential body lift in the massive weight loss and aesthetic patient. Clin Plast Surg. 2006;33(3):479–496. doi: 10.1016/j.cps.2006.05.006 [DOI] [PubMed] [Google Scholar]
- 47. Cansancao AL, Conde-Green A, Vidigal RA, Rodriguez RL, D'Amico RA. Real-time ultrasound-assisted gluteal fat grafting. Plast Reconstr Surg. 2018;142(2):372–376. doi: 10.1097/PRS.0000000000004602 [DOI] [PubMed] [Google Scholar]
- 48. Sozer SO, Agullo FJ, Palladino H. Spiral lift: medial and lateral thigh lift with buttock lift and augmentation. Aesthet Plast Surg. 2008;32(1):120–125. doi: 10.1007/s00266-007-9036-3 [DOI] [PubMed] [Google Scholar]
- 49. Hidalgo JE. Submuscular gluteal augmentation: 17 years of experience with gel and elastomer silicone implants. Clin Plast Surg. 2006;33(3):435–447. doi: 10.1016/j.cps.2006.04.001 [DOI] [PubMed] [Google Scholar]
- 50. Rios L, Gupta V. Improvement in Brazilian Butt Lift (BBL) safety with the current recommendations from ASERF, ASAPS, and ISAPS. Aesthet Surg J. 2020;40(8):864–870. doi: 10.1093/asj/sjaa098 [DOI] [PubMed] [Google Scholar]
- 51. Mendieta CG, Sood A. Classification system for gluteal evaluation: revisited. Clin Plast Surg. 2018;45(2):159–177. doi: 10.1016/j.cps.2017.12.013 [DOI] [PubMed] [Google Scholar]
- 52. Kalaaji A, Dreyer S, Vadseth L, Maric I, Jonsson V, Haukeboe TH. Gluteal augmentation with fat: retrospective safety study and literature review. Aesthet Surg J. 2019;39(3):292–305. doi: 10.1093/asj/sjy153 [DOI] [PubMed] [Google Scholar]
- 53. Ghavami A, Villanueva NL. Gluteal augmentation and contouring with autologous fat transfer: part I. Clin Plast Surg. 2018;45(2):249–259. doi: 10.1016/j.cps.2017.12.009 [DOI] [PubMed] [Google Scholar]
- 54. Serra F, Aboudib JH, Marques RG. Intramuscular technique for gluteal augmentation: determination and quantification of muscle atrophy and implant position by computed tomographic scan. Plast Reconstr Surg. 2013;131(2):253e–259e. doi: 10.1097/PRS.0b013e3182789d68 [DOI] [PubMed] [Google Scholar]
- 55. Aboudib JH, Serra F, de Castro CC. Gluteal augmentation: technique, indications, and implant selection. Plast Reconstr Surg. 2012;130(4):933–935. doi: 10.1097/PRS.0b013e31825dc3da [DOI] [PubMed] [Google Scholar]
- 56. de la Peña JA, Rubio OV, Cano JP, Cedillo MC, Garcés MT. History of gluteal augmentation. Clin Plast Surg. 2006;33(3):307–319. doi: 10.1016/j.cps.2006.04.003 [DOI] [PubMed] [Google Scholar]
- 57. Willemsen JC, Lindenblatt N, Stevens HP. Results and long-term patient satisfaction after gluteal augmentation with platelet-rich plasma-enriched autologous fat. Eur J Plast Surg. 2013;36(12):777–782. doi: 10.1007/s00238-013-0887-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Flores-Lima G, Eppley BL, Dimas JR, Navarro DE. Surgical pocket location for gluteal implants: a systematic review. Aesthet Plast Surg. 2013;37(2):240–245. doi: 10.1007/s00266-012-0018-8 [DOI] [PubMed] [Google Scholar]
- 59. Rosique RG, Rosique MJF. Augmentation gluteoplasty: a Brazilian perspective. Plast Reconstr Surg. 2018;142(4):910–919. doi: 10.1097/PRS.0000000000004809 [DOI] [PubMed] [Google Scholar]
- 60. Ramos-Gallardo G, Orozco-Renteria D, Medina-Zamora P, et al. Prevention of fat embolism in fat injection for gluteal augmentation, anatomic study in fresh cadavers. J Invest Surg. 2018;31(4):292–297. doi: 10.1080/08941939.2017.1321703 [DOI] [PubMed] [Google Scholar]
- 61. Raposo-Amaral CE, Cetrulo CL Jr, Guidi MdC, Ferreira DM, Raposo-Amaral CM. Bilateral lumbar hip dermal fat rotation flaps: a novel technique for autologous augmentation gluteoplasty. Plast Reconstr Surg. 2006;117(6):1781–1788. doi: 10.1097/01.prs.0000209923.91677.24 [DOI] [PubMed] [Google Scholar]
- 62. Senderoff DM. Aesthetic surgery of the buttocks using implants: practice-based recommendations. Aesthet Surg J. 2016;36(5):559–576. doi: 10.1093/asj/sjv251 [DOI] [PubMed] [Google Scholar]
- 63. de Runz A, Brix M, Gisquet H, et al. Satisfaction and complications after lower body lift with autologous gluteal augmentation by island fat flap: 55 case series over 3 years. J Plast Reconstr Aesthet Surg. 2015;68(3):410–418. doi: 10.1016/j.bjps.2014.10.043 [DOI] [PubMed] [Google Scholar]
- 64. Bayter-Marin JE, Cardenas-Camarena L, Aguirre-Serrano H, Duran H, Ramos-Gallardo G, Robles-Cervantes JA. Understanding fatal fat embolism in gluteal lipoinjection: a review of the medical records and autopsy reports of 16 patients. Plast Reconstr Surg. 2018;142(5):1198–1208. doi: 10.1097/PRS.0000000000004904 [DOI] [PubMed] [Google Scholar]
- 65. Singh M, Solomon IH, Calderwood MS, Talbot SG. Silicone-induced granuloma after buttock augmentation. Plast Reconstr Surg Glob Open. 2016;4(2):e624. doi: 10.1097/GOX.0000000000000618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Del Vecchio DA, Rohrich RJ. A changing paradigm: the Brazilian Butt Lift is neither Brazilian nor a lift-why it needs to be called safe subcutaneous buttock augmentation. Plast Reconstr Surg. 2020;145(1):281–283. doi: 10.1097/PRS.0000000000006369 [DOI] [PubMed] [Google Scholar]
- 67. Pena W, Cárdenas-Camarena L, Bayter-Marin JE, et al. Macro fat embolism after gluteal augmentation with fat: first survival case report. Aesthet Surg J. 2019;39(9):NP380–NP383. doi: 10.1093/asj/sjz151 [DOI] [PubMed] [Google Scholar]
- 68. Frank K, Casabona G, Gotkin RH, et al. Influence of age, sex, and body mass index on the thickness of the gluteal subcutaneous fat: implications for safe buttock augmentation procedures. Plast Reconstr Surg. 2019;144(1):83–92. doi: 10.1097/PRS.0000000000005707 [DOI] [PubMed] [Google Scholar]
- 69. Alvarez-Alvarez FA, González-Gutiérrez HO, Ploneda-Valencia CF. Safe gluteal fat graft avoiding a vascular or nervous injury: an anatomical study in cadavers. Aesthet Surg J. 2019;39(2):174–184. doi: 10.1093/asj/sjy237 [DOI] [PubMed] [Google Scholar]
- 70. Wang G, Ren Y, Cao W, Yang Y, Li S. Liposculpture and fat grafting for aesthetic correction of the gluteal concave deformity associated with multiple intragluteal injection of penicillin in childhood. Aesthet Plast Surg. 2013;37(1):39–45. doi: 10.1007/s00266-012-9997-8 [DOI] [PubMed] [Google Scholar]
- 71. Mendieta C, Stuzin JM. Gluteal augmentation and enhancement of the female silhouette: analysis and technique. Plast Reconstr Surg. 2018;141(2):306–311. doi: 10.1097/PRS.0000000000004094 [DOI] [PubMed] [Google Scholar]
- 72. de la Pena Salcedo JA, Gallardo GJ, Alvarenga GE. Subfascial gluteal implant augmentation. Clin Plast Surg. 2018;45(2):225–236. doi: 10.1016/j.cps.2017.12.012 [DOI] [PubMed] [Google Scholar]
- 73. Serra F, Aboudib JH, Neto JIS, Cossich VRA, Rodrigues NCP, de Oliveira KF, Marques RG. Volumetric and functional evaluation of the gluteus maximus muscle after augmentation gluteoplasty using silicone implants. Plast Reconstr Surg. 2015;135(3):533e–541e. doi: 10.1097/PRS.0000000000000970 [DOI] [PubMed] [Google Scholar]
- 74. Cansancao AL, Conde-Green A, David JA, Vidigal RA. Subcutaneous-only gluteal fat grafting: a prospective study of the long-term results with ultrasound analysis. Plast Reconstr Surg. 2019;143(2):447–451. doi: 10.1097/PRS.0000000000005203 [DOI] [PubMed] [Google Scholar]
- 75. Menardais B, Kerfant N, Chaput B, Watier E, Pluvy I, Bertheuil N. Lower body lift in the massive weight loss patient: a new classification and algorithm for gluteal augmentation. Plast Reconstr Surg. 2018;142(4):596e–598e. doi: 10.1097/PRS.0000000000004790 [DOI] [PubMed] [Google Scholar]
- 76. Andrade GA, Coltro PS, Ando A, Lima RV, Muller Neto BF, Silva VZ, Farina Junior JA. Gluteal augmentation with silicone implants: a new proposal for intramuscular dissection. Aesthet Plast Surg. 2017;41(4):872–877. doi: 10.1007/s00266-017-0823-1 [DOI] [PubMed] [Google Scholar]
- 77. Hunstad JP, Repta R. Purse-string gluteoplasty. Plast Reconstr Surg. 2009;123(3):123e–125e. doi: 10.1097/PRS.0b013e31819c1add [DOI] [PubMed] [Google Scholar]
- 78. Del Vecchio D, Kenkel JM. Practice advisory on gluteal fat grafting. Aesthet Surg J. 2022;42(9):1019–1029. doi: 10.1093/asj/sjac082 [DOI] [PubMed] [Google Scholar]
- 79. Ordenana C, Dallapozza E, Said S, Zins JE. Objectifying the risk of vascular complications in gluteal augmentation with fat grafting: a latex casted cadaveric study. Aesthet Surg J. 2020;40(4):402–409. doi: 10.1093/asj/sjz237 [DOI] [PubMed] [Google Scholar]
- 80. O'Neill RC, Abu-Ghname A, Davis MJ, Chamata E, Rammos CK, Winocour SJ. The role of fat grafting in buttock augmentation. Semin Plast Surg. 2020;34(1):38–46. doi: 10.1055/s-0039-3401038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Shah B. Complications in gluteal augmentation. Clin Plast Surg. 2018;45(2):179–186. doi: 10.1016/j.cps.2017.12.001 [DOI] [PubMed] [Google Scholar]
- 82. Levan P, Bassilios Habre S. Gluteal implants versus autologous flaps in patients with postbariatric surgery weight loss: a prospective comparative study of 3-dimensional gluteal projection after lower body lift. Aesthet Surg J. 2017;37(9):1012–1021. doi: 10.1093/asj/sjx033 [DOI] [PubMed] [Google Scholar]
- 83. Moscatiello F, Aznar-Benitah S, Grella R, Jover JH. Gluteal augmentation with cryopreserved fat. Aesthet Surg J. 2010;30(2):211–216. doi: 10.1177/1090820X10369347 [DOI] [PubMed] [Google Scholar]
- 84. Le Louarn C, Pascal JF. Autologous gluteal augmentation after massive weight loss. Plast Reconstr Surg. 2008;121(4):1515–1516. doi: 10.1097/01.prs.0000305369.21408.92 [DOI] [PubMed] [Google Scholar]
- 85. Durairaj KK, Devgan L, Lee Bs A, Khachatourian Bs N, Nguyen Bs V, Issa Bs T, Baker O. Poly-L-lactic acid for gluteal augmentation found to be safe and effective in retrospective clinical review of 60 patients. Dermatol Surg. 2020;46(1):S46–S53. doi: 10.1097/DSS.0000000000002598 [DOI] [PubMed] [Google Scholar]
- 86. Cardenas-Camarena L, Duran H. Improvement of the gluteal contour: modern concepts with systematized lipoinjection. Clin Plast Surg. 2018;45(2):237–247. doi: 10.1016/j.cps.2017.12.005 [DOI] [PubMed] [Google Scholar]
- 87. Godoy PM, Munhoz AM. Intramuscular gluteal augmentation with implants associated with immediate fat grafting. Clin Plast Surg. 2018;45(2):203–215. doi: 10.1016/j.cps.2017.12.004 [DOI] [PubMed] [Google Scholar]
- 88. Swanson E. Prospective controlled study of buttock fat transfer using ultrasound and photographic measurements. Plast Reconstr Surg Glob Open. 2016;4(5):e697. doi: 10.1097/GOX.0000000000000700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Paul S, Goyal A, Duncan LM, Smith GP. Granulomatous reaction to liquid injectable silicone for gluteal enhancement: review of management options and success of doxycycline. Dermatol Ther. 2015;28(2):98–101. doi: 10.1111/dth.12204 [DOI] [PubMed] [Google Scholar]
- 90. O'Neill RC, Hanson SE, Reece E, Winocour S. Safety considerations of fat grafting in buttock augmentation. Aesthet Surg J. 2021;41(Supplement_1):S25–S30. doi: 10.1093/asj/sjab092 [DOI] [PubMed] [Google Scholar]
- 91. Che DH, Xiao ZB. Gluteal augmentation with fat grafting: literature review. Aesthet Plast Surg. 2021;45(4):1633–1641. doi: 10.1007/s00266-020-02038-w [DOI] [PubMed] [Google Scholar]
- 92. Everett M, MoralesR, Jr., Newall G, Fortes PF, Hustak KL, Patronella CK, Mentz HA. Safest practices for autologous buttock augmentation with fat grafting using a roller pump injection technique. Aesthet Surg J. 2018;38(7):751–762. doi: 10.1093/asj/sjx113 [DOI] [PubMed] [Google Scholar]
- 93. Nasseri E. Gluteal augmentation with liquid silicone of unknown purity causes granulomas in an adult female: case report and review of the literature. J Cutan Med Surg. 2016;20(1):72–79. doi: 10.1177/1203475415598065 [DOI] [PubMed] [Google Scholar]
- 94. Jaimovich CA, Almeida MW, Aguiar LF, da Silva ML, Pitanguy I. Internal suture technique for improving projection and stability in secondary gluteoplasty. Aesthet Surg J. 2010;30(3):411–413. doi: 10.1177/1090820X10374107 [DOI] [PubMed] [Google Scholar]
- 95. Pazmiño P, Garcia O. Brazilian Butt Lift-associated mortality: the South Florida experience. Aesthet Surg J. 2023;43(2):162–178. doi: 10.1093/asj/sjac224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Cardenas-Camarena L, Trujillo-Méndez R, Diaz-Barriga JC. Tridimensional combined gluteoplasty: liposuction, buttock implants, and fat transfer. Plast Reconstr Surg. 2020;146(1):53–63. doi: 10.1097/PRS.0000000000006918 [DOI] [PubMed] [Google Scholar]
- 97. Pane TA. Experience with high-volume buttock fat transfer: a report of 137 cases. Aesthet Surg J. 2019;39(5):526–532. doi: 10.1093/asj/sjy191 [DOI] [PubMed] [Google Scholar]
- 98. Chia CT, Theodorou SJ, Dayan E, Tabbal G, Del Vecchio D. “Brazilian Butt Lift” under local anesthesia: a novel technique addressing safety concerns. Plast Reconstr Surg. 2018;142(6):1468–1475. doi: 10.1097/PRS.0000000000005067 [DOI] [PubMed] [Google Scholar]
- 99. Chang H, Heo C, Jeong J, Baek R, Minn K, Yoon C. Unilateral buttock reconstruction using contralateral inferior gluteal artery perforator flap with the aid of multi-detector CT. J Plast Reconstr Aesthet Surg. 2008;61(12):1534–1538. doi: 10.1016/j.bjps.2006.12.013 [DOI] [PubMed] [Google Scholar]
- 100. Raposo-Amaral CE, Ferreira DM, Warren SM, Magna LA, Ferreira LM. Quantifying augmentation gluteoplasty outcomes: a comparison of three instruments used to measure gluteal projection. Aesthet Plast Surg. 2008;32(2):333–338. doi: 10.1007/s00266-007-9058-x [DOI] [PubMed] [Google Scholar]
- 101. Leyva A, Tran T, Cibulas AT, Warden D, Danger FJ, Scherer K, Wasyliw C. Filler migration and granuloma formation after gluteal augmentation with free-silicone injections. Cureus. 2018;10(9):e3294. doi: 10.7759/cureus.3294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Gonzalez R, Gonzalez R. Intramuscular gluteal augmentation: the XYZ method. Clin Plast Surg. 2018;45(2):217–223. doi: 10.1016/j.cps.2017.12.006 [DOI] [PubMed] [Google Scholar]
- 103. Vasilakis V, Hamade M, Stavrides SA, Davenport TA. Bilateral sciatic neuropathy following gluteal augmentation with autologous fat grafting. Plast Reconstr Surg Glob Open. 2018;6(3):e1696. doi: 10.1097/GOX.0000000000001696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Whitfield RM, Rios LM Jr, DiBernardo BE. Making fat transfer to buttocks safer. Aesthet Surg J. 2017;37(10):1199–1200. doi: 10.1093/asj/sjx185 [DOI] [PubMed] [Google Scholar]
- 105. Muresan C, Brownstein GM, Shureih SF. Abdominoplasty-derived dermal-fat graft augmentation gluteoplasty. Aesthet Surg J. 2014;34(8):1234–1243. doi: 10.1177/1090820X14545159 [DOI] [PubMed] [Google Scholar]
- 106. Lourenco LM, de Noronha MGO, Colla LA, Izzo TR, Sigrist R, Braz A. LL body contour technique—a new way of gluteal contouring and augmentation with hyaluronic acid filler. J Cosmet Dermatol. 2022;21(5):1967–1972. doi: 10.1111/jocd.14763 [DOI] [PubMed] [Google Scholar]
- 107. Del Vecchio DA, Wall SJ Jr, Mendieta CG, Aslani AA, Hoyos AE, Mallucci PL, Whitaker IS. Safety comparison of abdominoplasty and Brazilian Butt Lift: what the literature tells us. Plast Reconstr Surg. 2021;148(6):1270–1277. doi: 10.1097/PRS.0000000000008599 [DOI] [PubMed] [Google Scholar]
- 108. Abboud M, Geeroms M, El Hajj H, Abboud N. Improving the female silhouette and gluteal projection: an anatomy-based, safe, and harmonious approach through liposuction, suspension loops, and moderate lipofilling. Aesthet Surg J. 2021;41(4):474–489. doi: 10.1093/asj/sjaa157 [DOI] [PubMed] [Google Scholar]
- 109. Uz I, Yalcinli S, Efe M. Fat embolism syndrome after gluteal augmentation with hyaluronic acid: a case report. Ulus Travma Acil Cerrahi Derg. 2020;26(6):960–962. doi: 10.14744/tjtes.2019.08433 [DOI] [PubMed] [Google Scholar]
- 110. Fadavi D, He W, Kraenzlin F, Darrach H, Shetty P, Xun H, Sacks JM. Risk and reward: public perception of gluteal fat grafting safety. Aesthet Plast Surg. 2020;44(5):1628–1638. doi: 10.1007/s00266-020-01728-9 [DOI] [PubMed] [Google Scholar]
- 111. Safran T, Abi-Rafeh J, Alhalabi B, Davison PG. The potential role of corticosteroid prophylaxis for the prevention of microscopic fat embolism syndrome in gluteal augmentations. Aesthet Surg J. 2020;40(1):78–89. doi: 10.1093/asj/sjz166 [DOI] [PubMed] [Google Scholar]
- 112. Singer R. Commentary on: macro fat embolism after gluteal augmentation with fat: first survival case report. Aesthet Surg J. 2019;39(9):NP384–NP386. doi: 10.1093/asj/sjz171 [DOI] [PubMed] [Google Scholar]
- 113. Narins RS, Brandt F, Leyden J, Lorenc ZP, Rubin M, Smith S. A randomized, double-blind, multicenter comparison of the efficacy and tolerability of Restylane versus Zyplast for the correction of nasolabial folds. Dermatol Surg. 2003;29(6):588–595. doi: 10.1046/j.1524-4725.2003.29150.x [DOI] [PubMed] [Google Scholar]
- 114. Weidman AA, Foppiani J, Valentine L, et al. Complications from fat grafting and gluteal augmentation in outpatient plastic surgery: an Analysis of American Association for Accreditation of Ambulatory Surgical Facilities (AAAASF, Quad A) data. Aesthet Surg J. 2024;44(7):722–730. doi: 10.1093/asj/sjad345 [DOI] [PubMed] [Google Scholar]
- 115. Lee E, Roberts T, Bruner T. Ethnic considerations in buttock aesthetics. Semin Plast Surg. 2009;23(3):232–243. doi: 10.1055/s-0029-1224803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical guidelines: potential benefits, limitations, and harms of clinical guidelines. BMJ. 1999;318(7182):527–530. doi: 10.1136/bmj.318.7182.527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Castle DJ, Honigman RJ, Phillips KA. Does cosmetic surgery improve psychosocial wellbeing? Med J Aust. 2002;176(12):601–604. doi: 10.5694/j.1326-5377.2002.tb04593.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Clapham PJ, Pushman AG, Chung KC. A systematic review of applying patient satisfaction outcomes in plastic surgery. Plast Reconstr Surg. 2010;125(6):1826–1833. doi: 10.1097/PRS.0b013e3181d51276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Mercieca-Bebber R, King MT, Calvert MJ, Stockler MR, Friedlander M. The importance of patient-reported outcomes in clinical trials and strategies for future optimization. Patient Relat Outcome Meas. 2018;9:353–367. doi: 10.2147/PROM.S156279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Blumenstein BA, Crowley JJ. Randomized design and analysis of randomized clinical trials. Control Clin Trials. 1986;7(3):235. doi: 10.1016/0197-2456(86)90074-7 [DOI] [Google Scholar]
- 121. Ottenhof MJ, Veldhuizen IJ, Hensbergen LJV, et al. The use of the FACE-Q aesthetic: a narrative review. Aesthet Plast Surg. 2022;46(6):2769–2780. doi: 10.1007/s00266-022-02974-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Liu LQ, Branford OA, Mehigan S. BREAST-Q measurement of the patient perspective in oncoplastic breast surgery: a systematic review. Plast Reconstr Surg Glob Open. 2018;6(8):e1904. doi: 10.1097/GOX.0000000000001904 [DOI] [PMC free article] [PubMed] [Google Scholar]