ABSTRACT
Objective: This study investigated the impact of war exposure on post-traumatic stress symptoms (PTSS) and sleep disturbance across Ukraine. Subjective and objective indicators of war exposure were modelled as predictors of these symptoms.
Methods: We created two predictors: first, we used governmental and crowd-sourced data to create an objective war exposure index for each of the 21 non-occupied regions of Ukraine, based on the number of air raid alarms, explosions, and proximity to frontline; and second, we obtained self-report cross-sectional data, using convenience sampling, from a nation-wide survey (N = 991) on subjective experience of threat triggered by the war. The survey also measured the outcome variables of PTSS and sleep disturbance. Hierarchical multilevel regressions modelled the relationship of this objective war exposure index with the two outcome variables, after accounting for demographics. A final regression step modelled subjective threat as predictor of these symptoms.
Results: We observed strongly elevated levels of PTSS and sleep disturbance and strong regional differences in objective and subjective war indicators. Objective war exposure predicted PTSS but not sleep disturbance, whereas subjective threat predicted both symptom domains.
Conclusion: The study demonstrates the utility of objective war exposure data for predicting the prevalence of PTSS in the different regions. The results further underscore the prominent role of subjective appraisal processes in the symptomatology of PTSS and sleep disturbance, thus informing theories on trauma-related disorders. Our results can guide the allocation of mental health services by identifying highly affected regions.
KEYWORDS: War, Ukraine, mental health, objective war exposure, threat perception, PTSD, sleep quality
HIGHLIGHTS
Objective data on air raid alarms and explosions have been prospectively collected in Ukraine.
We related those objective data to symptom reports of 991 responders in most Ukraine regions.
Objective data explained symptoms of post-traumatic stress but not sleep disturbance.
Abstract
Objetivo: Este estudio investigó el impacto de la exposición a la guerra en los síntomas de estrés postraumático (SEPT) y los trastornos del sueño en Ucrania. Se modelaron indicadores subjetivos y objetivos de exposición a la guerra como predictores de estos síntomas.
Métodos: Creamos dos predictores: primero, utilizamos datos gubernamentales y de datos de colaboración colectiva para crear un índice objetivo de la exposición a la guerra para cada una de las 21 regiones no ocupadas de Ucrania, en función del número de alarmas de ataques aéreos, explosiones, y proximidad a la primera línea; y segundo, obtuvimos datos transversales de autoinforme, utilizando un muestreo de conveniencia, de una encuesta nacional (N = 991) sobre la experiencia subjetiva de la amenaza desencadenada por la guerra. La encuesta también midió las variables de resultado de los SEPT y los trastornos del sueño. Las regresiones jerárquicas multinivel modelaron la relación de este índice objetivo de exposición a la guerra con las dos variables de resultado, después de tener en cuenta la demografía. El paso final de regresión modeló la amenaza subjetiva como predictor de estos síntomas.
Resultados: Observamos niveles fuertemente elevados de los SEPT y los trastornos del sueño y fuertes diferencias regionales en los indicadores objetivos y subjetivos de la guerra. La exposición objetiva a la guerra predijo los SEPT, pero no los trastornos del sueño, mientras que la amenaza subjetiva predijo ambos dominios de síntomas.
Conclusión: El estudio demuestra la utilidad de los datos objetivos de exposición a la guerra para predecir la prevalencia de los SEPT en las diferentes regiones. Los resultados subrayan aún más el papel destacado de los procesos de evaluación subjetiva en la sintomatología de los SEPT y los trastornos del sueño, informando así las teorías sobre los trastornos relacionados con el trauma. Nuestros resultados pueden orientar la asignación de servicios de salud mental mediante la identificación de regiones altamente afectadas.
PALABRAS CLAVE: Guerra, Ucrania, salud mental, percepción de amenazas, TEPT, calidad del sueño, exposición objetiva a la guerra
1. Introduction
The 2022 war in Ukraine stands as the largest conflict in Europe since the Second World War right now (Jain et al., 2022). Besides intense fighting on the ground at a lately more static frontline, it is characterized by continuous, wide ranging, and mostly unpredictable airstrikes on Ukrainian territory that terrorize civilians throughout the country. Governmental and non-governmental organizations have been documenting these attacks meticulously. Thus, the war in Ukraine provides an unprecedented opportunity to study objective indices of war exposure and its impact on stress and trauma in Ukrainian civilians. In the present study, we connected this novel objective airstrike data with an online survey on perceived military threat and mental health, including post-traumatic stress symptoms (PTSS) and sleep disturbance. We examined the intensity and geographic spread of objective war exposure, and we estimated the prevalence of symptoms of post-traumatic stress (PTS) and sleep disturbance across Ukraine. Further, we tested whether objective war exposure data and subjective threat ratings can predict symptoms of PTS and sleep disturbance. In the following, we review the effects of war exposure on post-traumatic stress disorder (PTSD) and sleep quality in Ukraine, after which we discuss current conceptual debates around subjective and objective antecedents of traumatization, and we introduce the current study.
1.1. PTSD and sleep disturbance in Ukrainians exposed to war
Criterion A of the post-traumatic stress disorder (PTSD) diagnosis in the DSM-5 requires that objective traumatic events were experienced or witnessed, and subjective symptoms were developed in response (American Psychiatric Association, 2022). Given the widespread war exposure in Ukraine, almost all Ukrainians inside and outside the country would fulfil this inclusive criterion; but does this translate to high rates of actual PTSD? While not every potentially traumatic event culminates in PTSD (Lukaschek et al., 2013), the trauma endured by civilians in war zones often does (Farhood et al., 2006). This observation might hold for Ukraine as well: it has been estimated that 20% of the general population scored above the clinical cutoff in 2022 (Eshel et al., 2023; Kurapov, Danyliuk, et al., 2023; Kurapov, Kalaitzaki, et al., 2023). However, no longitudinal data is available as of yet, thus making it unclear whether the symptoms were transient.
Besides PTSD, war exposure can also lead to sleep disturbances, which include chronic insomnia (Askenasy & Lewin, 1996) and increased pre-sleep arousal (Werner et al., 2020). In the war in Ukraine, rocket and drone attacks frequently occur at night to circumvent effective defense, often forcing civilians to interrupt their sleep to seek safety by hiding in a bomb shelter or in a room without windows at home. High physiological arousal and frequent nighttime awakenings, which these attacks cause, are known to contribute to the development of sleep disturbances such as prolonged sleep onset latency and fragmented sleep (Richards et al., 2020), but there has been no research to date on the impact of the war in Ukraine on the sleep of civilians exposed to it. Critically, PTSD and sleep disturbance reinforce each other, with PTSD-related hyperarousal and nightmares impeding sleep, and non-restful sleep affecting mood and impairing trauma recovery on the next day (Richards et al., 2020), which may also be the case in Ukraine.
1.2. PTS symptoms as a function of objective stressor intensity and of the resulting stress experience
How strong is the link between objective traumatic events and the development of subsequent PTSD? Studies from Israel suggest that the intensity and proximity of a bombardment predict the likelihood of developing PTSD in those who witness it (Besser et al., 2015; Cohen et al., 1995; Somer et al., 2009). Studies from civil war zones in Africa similarly document that the severity and number of such traumatic incidents predict PTSD likelihood (Neuner et al., 2004). Given the intensity and widespread exposure to airstrikes in Ukraine, does this mean that all exposed residents bound to develop PTSD (or sleep disturbance)? Luckily not: besides the objective life-threatening nature of traumatic events that is required by the PTSD diagnosis, subjective factors also play an important role in the development of PTSD. In fact, objective characteristics of stressors, such as life events and threats, correlate rather weakly with an individual’s subjective experience of stress and related long-term mental health outcomes (Schnyder et al., 2001; Shields et al., 2023). To illustrate, a prospective study on accident survivors showed that objective injury severity did not predict PTSD likelihood 12 months later (Schnyder et al., 2001). Drawing on the research on life events and resulting mental and physical health, Lazarus and Folkman (1984) developed the now leading stress model that characterizes stress as an interaction between stressor and individual coping capabilities. According to this model, confronted events will only trigger a stress response if they overwhelm an individual’s coping resources. Likewise, leading emotion regulation models emphasize the pivotal role of (re)appraisal in emotional experience (Gross & John, 2003).
Based on this empirical and theoretical background, the current study introduced a set of novel objective war exposure data and modelled them as potential predictors of symptoms of PTS and sleep disturbance. Our central research question was whether these objective data contribute to the prediction of symptoms of PTS and sleep disturbance. If so, this would have practical relevance in helping allocate mental health resources to regions most affected by PTSS. From a theoretical perspective, we further asked whether subjective appraisals of war-related threat also predict these symptoms, in line with the described appraisal models of stress and emotions. We expected that participants with more objective war exposure (i.e. closer to the frontline, more alarms, more explosions) would show more symptoms of PTS and sleep disturbance (Besser et al., 2015; Somer et al., 2009; Somer & Ataria, 2015). Importantly, we expected that subjective threat ratings would provide additional power to predict symptoms in accordance with appraisal-based stress models.
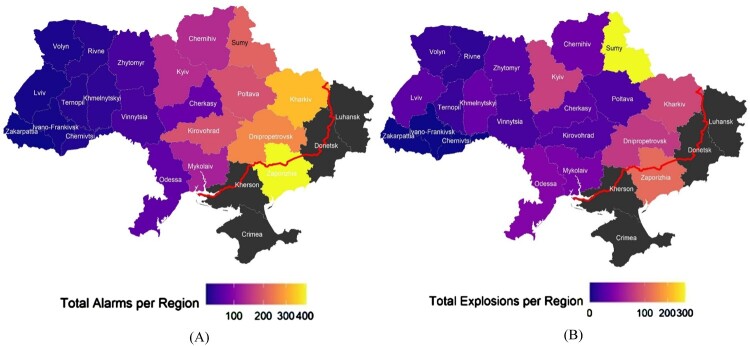
Since this, to our knowledge, is the first study that used fine-grained objective war exposure data, we complemented our predictive analyses with descriptive data: we mapped the number of explosions and air raid alarms by region to see whether war exposure corresponds closely with proximity to the frontline, or whether it has a more diffuse geographical signature. The latter would be illustrated by significant war exposure in the western regions of Ukraine. We also reported on the overall symptom load in the sample using established clinical cutoffs. We expected a relatively high symptom load given the literature on other war-struck countries (Lim et al., 2022; Somer et al., 2009). We present these data first in the results section before proceeding to the predictive modelling.
2. Methods
2.1. Design and participants
We used a snowball sampling methodology by recruiting students of the Faculty of Psychology at the Taras Shevchenko National University of Kyiv, who were asked to share the questionnaire with friends and relatives; in parallel, we utilized a convenience sampling methodology by recruiting participants from different social media channels (Telegram FZ-LLC.) and through the official Facebook page of the Faculty of Psychology, to target a wide range of demographic backgrounds and regions in Ukraine. Informed consent was obtained from all participants. The data were collected from 15 June until 28 June 2023, using an online questionnaire survey. Inclusion criteria were an age between 18 and 70 years and the ability to provide informed consent, yielding N = 991 valid responses.
2.2. Measures
2.2.1. Questionnaires
Participants were required to respond to all questions, thus yielding no missing values.
Sociodemographic information. Information on gender, age, residence, size of the settlement (e.g. town or village), and employment status were gathered.
PTSS. PTSS were measured with The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) (α = .67) (Williamson et al., 2022). The PC-PTSD-5 consists of 5 items asking about individual PTSS and it requires a ‘Yes’ or ‘No’ response to each. The number of ‘Yes’ answers is summed, resulting in a score from 0 to 5, with higher scores indicating greater symptom severity. Questions refer to a traumatic experience that happened within the last month. The questionnaire was translated by the manuscript authors: we used forward and backward translation where the original English version of the survey was first translated into Ukrainian, and the translated version was then back-translated into English by two independent Ukrainian researchers. The original and back-translated English versions were compared and any discrepancies were resolved by consensus.
Sleep disturbance. Sleep disturbance in the past month was measured with the Ukrainian version (α = .61) of the Pittsburgh Sleep Quality Index (PSQI; Mazur et al., 2021). The questionnaire includes 19 individual items grouped into 7 components. Each of the 7 components is scored on a scale from 0 to 3, leading to a global sum of 0 (no difficulty) to 21 (severe difficulty). The individual items within components vary in their response options, contributing to the component score. The questionnaire asks about sleep problems within the last month.
Subjective threat. Personal feelings of threat were measured with our self-formulated items on a horizontal visual analogue scale (left anchor ‘0’, right anchor ‘100'). Questions inquired whether participants felt physically threatened by (i) ‘the military situation inside the country and at the frontline’, (ii) ‘rocket and drone attacks in their region’, and (iii) ‘the political situation of the country’. The three items were averaged to form a ‘subjective threat index’ (α = .64) which was used in the remainder of this study.
2.2.2. Objective war exposure data
Objective war exposure data. Objective war exposure in Ukraine comes from many sources, including country-wide rocket and drone attacks, and from active combat near the frontline in the south and east. We computed three measures as proxies for objective war exposure. First, we computed proximity to the frontline as the (negative) distance to the nearest point on the frontline from the geographical centres of each region of Ukraine (for details, see Supplements A and B). Second, we computed an objective air raid alarm indicator. To alert the public of potential airstrikes, a comprehensive national alarm system is in place that includes street loudspeakers, SMS notifications, and a mobile app named ‘Повітряна Тривога’ (‘Povitriana Trivoha’, Engl.: ‘Air Alert’). These systems inform residents about the launch of rockets or drones and the potential direction of their launch trajectory, making the air raid alarms region-specific. Third, we utilized the ‘Air-alarms.in.ua’ statistical service, which logs reported explosions from both landed and intercepted rockets/drones for all 24 Ukrainian regions using media reports and individual reports from citizens (crowdsourcing). All three indicators were referenced to the 10 weeks (21 April to 30 June 2023) preceding and coinciding with the online survey data collection period (15 June to 28 June 2023): we estimated that 10 weeks would be long enough to capture war exposure that can cause symptoms of PTS and sleep disturbance, while short enough to make geographical relocation of participants unlikely.
To account for all objective war exposure indices together, we computed an aggregated objective war exposure index. First, we log-transformed total number of alarms, reported explosions, and proximity to the frontline to account for non-normal distribution. The log of frontline proximity was coded negatively, such that more negative values represent less proximity to the frontline. Lastly, the three transformed indices were z-transformed and summed.
2.3. Statistical analysis and prediction model
All scripts and data are available on our OSF repository (https://osf.io/vukej/). Regions with fewer than 10 respondents were excluded from all analyses, allowing us to analyse data from 21 out of 24 regions. For descriptive analysis, we plot regional differences in objective war exposure using heat maps of Ukrainian regions. In all graphs, the number of explosions per region was depicted on a square root scale due to the high disparity between regions.
Our main research question was analysed with hierarchical multilevel regression analyses predicting symptoms of PTS and sleep disturbance. We predicted each of these two dependent variables by adding sets of predictors in a series of three steps. In step 1, we added the demographic variables gender, age, and employment; in step 2, we added an index of objective war exposure; and in step 3, we added subjective threat. Note that from a practical stance, demographics and objective data are easier to collect than subjective threat ratings across the country.
To account for the unequal distribution of participants across regions, we weighted our analyses on the participant level. We used the population per region in 2021 from the Ukrainian statistics service (Governmental Statistics Service of Ukraine, 2022) to down-weight participants from regions that were overrepresented in the sample, while upweighting participants from regions that were underrepresented. The weight for each participant per region was determined by dividing the proportion of the population in each region by the proportion of the sample in each region. Participants from Kyiv were thus down-weighted the most (given a weight of .38) while participants from e.g. Kharkiv were upweighted significantly (given a weight of 2.96; for details see Supplement C, Table C.1). In conjunction with multilevel regression with random intercepts per region, this allowed us to analyse the effect of region-level objective war exposure indices on individuals living in those different regions in a manner that is less biased by the degree of over- or undersampling in each region due to snowball sampling. We also repeated these analyses without any weighting (see Supplement D, Table D.1).
3. Results
The total number of participants was 991. The mean age of the sample was 28.9 (SD = 11.2). Detailed socio-demographic data are presented in Table 1. For detailed information regarding the number of participants per region see Supplement C, Table C.1.
Table 1.
Sociodemographic characteristics of the sample.
| Counts | % of Total | ||
|---|---|---|---|
| Gender | Male | 182 | 17.95 |
| Female | 796 | 80.75 | |
| No answer | 8 | .8 | |
| Other | 5 | .5 | |
| Settlement Type | Big city (>200,000) | 575 | 58.8 |
| City | 127 | 13.0 | |
| Small town (<50,000) | 104 | 10.6 | |
| Big village | 65 | 6.65 | |
| Village | 97 | 9.92 | |
| Other | 10 | 1.02 | |
| Employment | Employed | 593 | 60.6 |
| Unemployed | 384 | 39.3 |
Note: Total number of participants – 991.
3.1. Prevalence of symptoms of PTS and sleep disturbance
On the PC-PTSD-5, participants had an average score of 2.67 (SD = 1.45) and 16.57% (N = 164) were above the clinical cutoff of 4 (although validation in women is still debated, Prins et al., 2016). Likewise, on the PSQI, participants had an average score of 8.25 (SD = 3.53) with only 11.72% (N = 117) indicating no sleep issues, and 58.08% (N = 575) reporting bad sleep quality (score 5–10), or even chronic sleep problems (30.20%; N = 299) (Ong et al., 2017).
3.2. Objective war exposure by region
Regional objective war exposure in Ukraine was significant: on average per region, there were 122.81 air raid alarms (SD = 105.31) and 34.95 explosions (SD = 69.07) over the 10 weeks preceding the questionnaire. The average subjective threat rating across regions was 48.74 (SD = 4.91) on a 0–100 scale.
To visualize regional war exposure, we displayed the region-specific numbers of alarms (total of 2578) and reported explosions (734) on the map of Ukraine in Figure 1. For details on the regional distribution of the aggregated war exposure index and subjective threat, see Supplement C, Figure C.1, A, B.1 We further report correlations of individual and aggregated objective war exposure indices, subjective threat indices, and average symptom levels per region in Supplement C, Table C.3.
Figure 1.
Regional frequency of alarms (A) and explosions (B) across the 10 weeks prior to the survey.
Notes: Figure 1A depicts the number of alarms whereas Figure 1B represents the number of reported explosions (both square root transformed). The red line is the frontline as per 1 July 2023. Regions were marked in grey if they were excluded from analyses due to insufficient sample size in the survey portion of the study.
3.3. Objective war exposure vs. subjective threat as predictors of PTS and sleep disturbance symptoms
To determine whether objective war exposure indices and/or subjective threat explain variance in symptoms of PTS and sleep disturbance, we ran two separate weighted hierarchical multilevel regression analyses, as specified in the statistical analysis section (see Table 2).
Table 2.
Results of multilevel modelling of PTSS and sleep disturbance for weighted sample.
| Dependent variables | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PTSS | Sleep disturbance | ||||||||||||
| Step | Fixed effects | ΔR2m | b | SE | t | df | p | ΔR2m | b | SE | t | df | p |
| 1 | Sex: male | 2.2% | –.99 | .24 | 4.22 | 945.42 | <.001* | 4.3% | –.98 | .28 | 3.57 | 947.98 | <.001* |
| Age | –.01 | .01 | .86 | 845.53 | .392 | .05 | .01 | 5.29 | 857.89 | <.001* | |||
| Employment status: unemployed | .23 | .19 | 1.2 | 918.72 | .229 | –.3 | .22 | 1.34 | 923.17 | .181 | |||
| 2 | Aggregated objective war exposure index | .6% | .09 | .03 | 2.73 | 22.57 | .012* | 0% | –.01 | .04 | .16 | 26.02 | .874 |
| 3 | Subjective threat | 4.9% | .03 | 0 | 6.94 | 960 | <.001* | .4% | .01 | 0 | 2.34 | 959.63 | .021* |
Notes: As reference levels, we used ‘female’ for sex, and ‘employed’ for employment status. Results are presented for the weighted sample. R2m = marginal R-squared. This value represents the percentage of variance in the dependent variable explained by the fixed predictors in the model.
PTS symptoms were higher in female participants but did not differ along age or employment. In step 2, we found that higher objective war exposure predicted higher PTS symptoms, even after accounting for demographic characteristics. In step 3, we found that subjective threat also predicted higher PTS symptoms, on top of all other variables. Regarding the analyses in the unweighted sample (see Supplement D, table D.1), results were largely similar, with the exception that the aggregated objective war exposure index (step 2) did not significantly predict PTS symptoms. This can be explained by the fact that, without weighting, regions with large subsamples (e.g. Kyiv with 358 participants) all share the same objective war exposure data and thus do not carry any between participant variance.
Sleep disturbance was worse in female and older participants, whereas employment again played no role. In step 2, we found that objective war exposure did not play a role in sleep disturbance. In step 3, we found that higher subjective threat predicted higher sleep disturbance, just like it predicted PTS symptoms. Results were similar in the unweighted sample (Supplement D).
4. Discussion
To our knowledge, this is the first study on the 2022 Ukraine war that includes indices on objective war exposure and their geographical spread. We also investigated the prevalence of symptoms of PTS and sleep disturbance. Lastly, we related indices of objective war exposure to PTSS and sleep disturbance, and tested whether this prediction would improve by adding subjective threat appraisal data.
While airstrikes and explosions were high in frontline-adjacent regions, we found that several more western regions were also disproportionally struck, such as Kyiv and Lviv. Regarding the prevalence of psychiatric symptoms, about one out of six civilians in our study reported clinical levels of PTSS, which is only slightly lower than the numbers reported on veterans in other wars (Prins et al., 2016; Shahmiri Barzoki et al., 2023). Furthermore, a striking 88% of civilians in our study reported bad or very bad sleep quality.
Objective war exposure indices did not predict sleep disturbance, suggesting that other processes mediate between the presence of war and these symptoms: probably, the general feeling of uncertainty and threat in society due to the war and, given the individual’s degree of resilience, people tend to develop sleepdisturbance. In addition, people with less objective war exposure nevertheless experience significant threat and uncertainty for other reasons, perhaps due to media exposure and occasional air strikes in their regions. This pattern may be similar to the one observed during the COVID-19 pandemic, during which overall sleep quality was reduced and sleep was more restless (Bothe et al., 2022; Florea et al., 2021).
Our main research question was whether objective war exposure could predict symptoms of PTS and sleep disturbance beyond demographics. When it comes to demographics, we found that female gender is positively related to the PTSS and sleep disturbance, which is consistent with a large body of literature (Brewin et al., 2000; Lukaschek et al., 2013; Santiago et al., 2013). Current employment did not predict symptoms of PTS or sleep disturbance, and older age predicted only sleep disturbance. Critically, beyond demographics, objective war exposure was an independent (and similarly strong) predictor, explaining an additional 2.6% of variance in observed PTSS. Objective war exposure did not similarly predict sleep disturbance. These results add to the evidence that objective stress exposure is of relevance for the development of PTSS/PTSD (Besser et al., 2015; Somer et al., 2009). The observed predictive power of objective stress indicators is in line with the current DSM-5 criterion A, which requires experiencing or witnessing a potentially life-threatening traumatic event. The result also has practical implications for mental health provision regarding prevention and treatment of PTSS: it is not only regions close to the frontline that will need more mental health resources, but also the regions in the west that are disproportionally affected by airstrikes. On a finer scale, besides gender, screening for individuals who feel particularly threatened by the political/military/physical situation might help in allocating mental health support in a targeted way.
Last, and of high theoretical and practical importance, our results show that individuals who report elevated subjective threat by the military situation also report more symptoms of PTS and sleep disturbance, even after accounting for demographics and objective war exposure. Beyond demographics and objective war exposure, subjective threat was an independent and similarly strong predictor, explaining an additional 4.9% of variance in PTSS and 4.0% of variance in sleep disturbance. This aligns with previous studies where subjective stress severity was more important in comparison to objective stressors (Harel-Fisch et al., 2010; Heir et al., 2016; Shields et al., 2023). The most plausible explanation is that individual residents of a region experience the same regional situation quite differently and these appraisals mediate how they respond in terms of mental health, in line with the transactional stress model (Lazarus & Folkman, 1984) and appraisal theories of emotion (Gross & John, 2003), previously discussed in the introduction. Of course, the cross-sectional nature of the study cannot exclude an inverse relationship; PTSS and sleep disturbance may also increase perceived threat.
We see three groups of limitations. A first major limitation concerns the representativeness of the current sample. Since we focused on civilians, we oversampled groups less affected by army drafting: we strongly oversampled women, young adults, and urban residents. We did not emphasize representativity within each region. This, however, would have been difficult given the high prevalence of internal displacement: we cannot exclude that some of our participants moved across regions during our assessment period of objective data, which would lead to a mismatch of objective war exposure and subjective threat.
A second limitation concerns the survey. For practical reasons, our survey was short and thus lacked many established variables of interest, such as peritraumatic dissociation and trauma history. The sleep disturbance measurement did not distinguish between external causes for sleep disturbance, such as airstrikes during the night, and internal causes, such as high physiological arousal, worry, or anxiety. As such, we cannot tell whether sleep would return to normal once the alarms would stop or whether sleep is disturbed on in a more long-term manner, e.g., due to learning processes or hyperarousal.
A third major limitation of the current study pertains to the measurement of the objective war exposure variables. Some objective data were partially subjective, being crowdsourced from residents that report sounds and sights of explosions, rockets, or drones.
Given the ubiquity of smartphones in Ukraine, future studies could use ecological momentary assessment to record day-level explosion exposure and symptoms prospectively (Stieger et al., 2023), together with objective physiological parameters of daily stress and sleep quality (e.g., using ambulatory heart rate and motility recordings) to gain more precision. Our methodology for gauging the distance to the frontline was also inherently imprecise (for more details, see Supplement A). However, even if the objective war exposure variables were accurately measured, there is still a risk that some individuals’ personal exposure could have strongly deviated from the regional average, given the large expanse of the Ukrainian regions. If we could get more precision on individual exposure to alarms and actual explosions, we could resort to Pavlovian conditioning models of PTSS as data suggest slightly stronger associations with alarms (conditioned stimuli) than with explosions (unconditioned stimuli) (Blechert et al., 2007).
Supplementary Material
Acknowledgements
AK – data collection, data analysis, manuscript writing; MS – manuscript review and editing; SK – data analysis, manuscript review and editing; FW – study design, manuscript review and editing; JB – study design and methodology, manuscript review and editing.
Funding Statement
This research was funded by the MSCA4Ukraine a funding scheme that is implemented by a consortium comprised of Scholars at Risk Europe (SAR Europe) hosted at Maynooth University, Ireland (project coordinator), the German Alexander von Humboldt Foundation (AvH) and the European University Association (EUA) [grant number 1233157].
Note
Details on values for specific regions in the ten weeks preceding data collection (21 April 2023 to 30 June 2023) can be found online (https://ankurapovshine.shinyapps.io/alarms/).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committees of Paris Lodron University of Salzburg (EK-GZ 26/2023) and Taras Shevchenko National University of Kyiv (11-22/7). The participants provided their written informed consent to participate in this study.
Data availability statement
The data and R scripts for analysis of this study are provided on OSF repository (https://osf.io/vukej/).
References
- American Psychiatric Association . (2022). Diagnostic and statistical manual of mental disorders. American Psychiatric Association Publishing. 10.1176/appi.books.9780890425787 [DOI] [Google Scholar]
- Askenasy, J. J. M., & Lewin, I. (1996). The impact of missile warfare on self-reported sleep quality. Part 1. Sleep, 19(1), 47–51. 10.1093/sleep/19.1.47 [DOI] [PubMed] [Google Scholar]
- Besser, A., Zeigler-Hill, V., Weinberg, M., Pincus, A. L., & Neria, Y. (2015). Intrapersonal resilience moderates the association between exposure-severity and PTSD symptoms among civilians exposed to the 2014 Israel–Gaza conflict. Self and Identity, 14(1), 1–15. 10.1080/15298868.2014.966143 [DOI] [Google Scholar]
- Blechert, J., Michael, T., Vriends, N., Margraf, J., & Wilhelm, F. H. (2007). Fear conditioning in posttraumatic stress disorder: Evidence for delayed extinction of autonomic, experiential, and behavioural responses. Behaviour Research and Therapy, 45(9), 2019–2033. 10.1016/j.brat.2007.02.012 [DOI] [PubMed] [Google Scholar]
- Bothe, K., Schabus, M., Eigl, E.-S., Kerbl, R., & Hoedlmoser, K. (2022). Self-reported changes in sleep patterns and behavior in children and adolescents during COVID-19. Scientific Reports, 12(1), 20412. 10.1038/s41598-022-24509-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. 10.1037/0022-006X.68.5.748 [DOI] [PubMed] [Google Scholar]
- Cohen, S., Kessler, R. C., & Gordon, L. U. (1995). Strategies for measuring stress in studies of psychiatric and physical disorders. In Cohen S., Kessler R. C., & Gordon L. U. (Eds.), Measuring stress: A guide for health and social scientists (pp. 3–26). Oxford University Press. [Google Scholar]
- Eshel, Y., Kimhi, S., Marciano, H., & Adini, B. (2023). Predictors of PTSD and psychological distress symptoms of Ukraine civilians during war. Disaster Medicine and Public Health Preparedness, 17, e429. 10.1017/dmp.2023.69 [DOI] [PubMed] [Google Scholar]
- Farhood, L., Dimassi, H., & Lehtinen, T. (2006). Exposure to war-related traumatic events, prevalence of PTSD, and general psychiatric morbidity in a civilian population from southern Lebanon. Journal of Transcultural Nursing, 17(4), 333–340. 10.1177/1043659606291549 [DOI] [PubMed] [Google Scholar]
- Florea, C., Topalidis, P., Hauser, T., Angerer, M., Kurapov, A., Beltran Leon, C. A., Soares Brandão, D., & Schabus, M. (2021). Sleep during COVID-19 lockdown: A cross-cultural study investigating job system relevance. Biochemical Pharmacology, 191, Article 114463. 10.1016/j.bcp.2021.114463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Governmental Statistics Service of Ukraine . (2022). https://ukrstat.gov.ua/operativ/operativ2022/ds/kn/kn_0122_ue.xls
- Gross, J. J., & John, O. P. (2003). Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85(2), 348–362. 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- Harel-Fisch, Y., Radwan, Q., Walsh, S. D., Laufer, A., Amitai, G., Fogel-Grinvald, H., & Abdeen, Z. (2010). Psychosocial outcomes related to subjective threat from armed conflict events (STACE): Findings from the Israeli-Palestinian cross-cultural HBSC study. Child Abuse & Neglect, 34(9), 623–638. 10.1016/j.chiabu.2009.12.007 [DOI] [PubMed] [Google Scholar]
- Heir, T., Blix, I., & Knatten, C. K. (2016). Thinking that one’s life was in danger: Perceived life threat in individuals directly or indirectly exposed to terror. British Journal of Psychiatry, 209(4), 306–310. 10.1192/bjp.bp.115.170167 [DOI] [PubMed] [Google Scholar]
- Jain, N., Prasad, S., Bordeniuc, A., Tanasov, A., Shirinskaya, A. V., Béla, B., Cheuk, C. P., Banica, D. C. N., Panag, D. S., Świątek, D., Savchenko, E., Platos, E., Lolita, J., Betka, M. M., Phiri, M., Patel, S., Czárth, Z. C., Krygowska, A. M., Jain, S., & Reinis, A. (2022). European countries step-up humanitarian and medical assistance to Ukraine as the conflict continues. Journal of Primary Care & Community Health, 13, 215013192210953. 10.1177/21501319221095358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurapov, A., Danyliuk, I., Loboda, A., Kalaitzaki, A., Kowatsch, T., Klimash, T., & Predko, V. (2023). Six months into the war: A first-wave study of stress, anxiety, and depression among in Ukraine. Frontiers in Psychiatry, 14, Article 1190465. 10.3389/fpsyt.2023.1190465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurapov, A., Kalaitzaki, A., Keller, V., Danyliuk, I., & Kowatsch, T. (2023). The mental health impact of the ongoing Russian-Ukrainian war 6 months after the Russian invasion of Ukraine. Frontiers in Psychiatry, 14, Article 1134780. 10.3389/fpsyt.2023.1134780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. Springer Publishing Company. [Google Scholar]
- Lim, I. C. Z. Y., Tam, W. W. S., Chudzicka-Czupała, A., McIntyre, R. S., Teopiz, K. M., Ho, R. C., & Ho, C. S. H. (2022). Prevalence of depression, anxiety and post-traumatic stress in war- and conflict-afflicted areas: A meta-analysis. Frontiers in Psychiatry, 13, Article 978703. 10.3389/fpsyt.2022.978703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukaschek, K., Kruse, J., Emeny, R. T., Lacruz, M. E., von Eisenhart Rothe, A., & Ladwig, K.-H. (2013). Lifetime traumatic experiences and their impact on PTSD: A general population study. Social Psychiatry and Psychiatric Epidemiology, 48(4), 525–532. 10.1007/s00127-012-0585-7 [DOI] [PubMed] [Google Scholar]
- Mazur, L. P., Marushchak, M. I., & Batiukh, O. V. (2021). Opytuvalnyky yak osnovni instrumenty v diahnostytsi rozladiv snu. Visnyk Medychnykh i Biolohichnykh Doslidzhen, 3, 96–100. 10.11603/bmbr.2706-6290.2021.3.12575 [DOI] [Google Scholar]
- Neuner, F., Schauer, M., Karunakara, U., Klaschik, C., Robert, C., & Elbert, T. (2004). Psychological trauma and evidence for enhanced vulnerability for posttraumatic stress disorder through previous trauma among West Nile refugees. BMC Psychiatry, 4(1), 34. 10.1186/1471-244X-4-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong, J. C., Arnedt, J. T., & Gehrman, P. R. (2017). Insomnia diagnosis, assessment, and evaluation. In Kryger M. H., Roth T., & Dement W. C. (Eds.), Principles and practice of sleep medicine (6th ed., pp. 785–793). Elsevier. [Google Scholar]
- Prins, A., Bovin, M. J., Smolenski, D. J., Marx, B. P., Kimerling, R., Jenkins-Guarnieri, M. A., Kaloupek, D. G., Schnurr, P. P., Kaiser, A. P., Leyva, Y. E., & Tiet, Q. Q. (2016). The primary care PTSD screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 31(10), 1206–1211. 10.1007/s11606-016-3703-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards, A., Kanady, J. C., & Neylan, T. C. (2020). Sleep disturbance in PTSD and other anxiety-related disorders: An updated review of clinical features, physiological characteristics, and psychological and neurobiological mechanisms. Neuropsychopharmacology, 45(1), 55–73. 10.1038/s41386-019-0486-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santiago, P. N., Ursano, R. J., Gray, C. L., Pynoos, R. S., Spiegel, D., Lewis-Fernandez, R., Friedman, M. J., & Fullerton, C. S. (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLoS One, 8(4), e59236. 10.1371/journal.pone.0059236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnyder, U., Moergeli, H., Klaghofer, R., & Buddeberg, C. (2001). Incidence and prediction of posttraumatic stress disorder symptoms in severely injured accident victims. American Journal of Psychiatry, 158(4), 594–599. 10.1176/appi.ajp.158.4.594 [DOI] [PubMed] [Google Scholar]
- Shahmiri Barzoki, H., Ebrahimi, M., Khoshdel, A., Noorbala, A. A., Rahnejat, A. M., Avarzamani, L., Shahed Hagh Ghadam, H., & Avakh, F. (2023). Studying the prevalence of PTSD in veterans, combatants and freed soldiers of Iran-Iraq war: A systematic and meta-analysis review. Psychology, Health & Medicine, 28(3), 812–818. 10.1080/13548506.2021.1981408 [DOI] [PubMed] [Google Scholar]
- Shields, G. S., Fassett-Carman, A., Gray, Z. J., Gonzales, J. E., Snyder, H. R., & Slavich, G. M. (2023). Why is subjective stress severity a stronger predictor of health than stressor exposure? A preregistered two-study test of two hypotheses. Stress and Health, 39(1), 87–102. 10.1002/smi.3165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somer, E., & Ataria, Y. (2015). Adverse outcome of continuous traumatic stress: A qualitative inquiry. International Journal of Stress Management, 22(3), 287–305. 10.1037/a0038300 [DOI] [Google Scholar]
- Somer, E., Zrihan-Weitzman, A., Fusé, T., Parker, H., Dickstein, B., Maguen, S., & Litz, B. T. (2009). Israeli civilians under heavy bombardment: Prediction of the severity of post-traumatic symptoms. Prehospital and Disaster Medicine, 24(5), 389–394. 10.1017/S1049023X00007196 [DOI] [PubMed] [Google Scholar]
- Stieger, S., Lewetz, D., Paschenko, S., & Kurapov, A. (2023). Examining terror management theory in Ukraine: Impact of air-raid alarms and explosions on mental health, somatic symptoms, and well-being. Frontiers in Psychiatry, 14, Article 1244335. 10.3389/fpsyt.2023.1244335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner, G. G., Danböck, S. K., Metodiev, S., & Kunze, A. E. (2020). Pre-sleep arousal and fear of sleep in trauma-related sleep disturbances: A cluster-analytic approach. Clinical Psychology in Europe, 2(2), e2699. 10.32872/cpe.v2i2.2699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson, M. L. C., Stickley, M. M., Armstrong, T. W., Jackson, K., & Console, K. (2022). Diagnostic accuracy of the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) within a civilian primary care sample. Journal of Clinical Psychology, 78(11), 2299–2308. 10.1002/jclp.23405 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data and R scripts for analysis of this study are provided on OSF repository (https://osf.io/vukej/).