LEARNING OBJECTIVES
Highlight the importance of Deming’s system of profound knowledge as a framework for quality improvement (QI) projects.
Provide a case study using the four pillars of Deming’s system of profound knowledge.
Shed some light on difficult IV access as a patient concern that impacts satisfaction and share practical nurse-led solutions.
INTRODUCTION
We were intrigued by a recent publication in the Global Journal on Quality and Safety in Healthcare (JQSH) called “Lens of Profound Knowledge,” by Dr. Kazzaz.[1] He thoroughly and neatly discussed the four well-known pillars of Deming’s profound knowledge: (1) appreciation of the system, (2) knowledge about variation, (3) theory of knowledge, and (4) psychology. He illustrates their importance as integrated, dynamic systems for successful QI projects.[2]
CASE STUDY
At our institution, we have an ongoing QI project that aims to solve a hospital-wide problem related to difficult intravenous (IV) access. By applying the four pillars of Deming’s profound knowledge, as mentioned above, we will use our project as a case study for this profound insight to illustrate the application to real-life scenarios.
King Faisal Specialist Hospital and Research Centre – Madinah (KFSHRC-M), is a recently established third branch of a well-known referral tertiary hospital in Saudi Arabia. Following the successful commissioning and planned operational phases, we expanded our bed capacity and the population we served. During the initial project period, our bed capacity increased from 71 beds in 2022 to 146 beds in 2023 (current phase projection is 300 beds).
As the number of inpatients increased and the services were ramped up, we observed a recurring theme of concerns regarding frequently failed peripheral intravenous access (PIV). This resulted in poor patient satisfaction as well as overuse of other specialty and critical care services such as anesthesiology staff, intensive care unit (ICU) staff, and the interventional radiology (IR) department for central venous catheters (CVCs) or peripherally inserted central catheters (PICCs) as rescue access.
Our leaders identified this issue as an area for improvement and established a QI project to assess and solve this issue with a focus on patient satisfaction concerns around many failed IV attempts. The difficult IV access (DIVA) task force was formulated, including nursing, medical supply, quality, patient safety, and physician staff.
Appreciation of the System
Peripheral intravenous (PIV) catheters remain the standard venous access for all inpatients in all hospitals worldwide; however, they have many inherent problems that include but are not limited to high failure rates on the first attempt (26% in adults, 54% in pediatric patients), very short indwelling time (average of 44 hours), and the need for repeated venipuncture either for the new cannula or for blood extraction, which leads to both decreased satisfaction and increased length of stay in patients with DIVA.[3,4]
In this vein, the DIVA task force, with its diverse members from nursing, quality, patient safety, medical engineering, medical supply, patient relations, and expert physicians in IV access, conducted several meetings, brainstormed, and conducted a limited literature review to define the problem; established the Specific, Measurable, Achievable, Relevant, and Time-bound (SMART) aim; and reviewed the current system via process mapping.
The problem was defined as frequently failed attempts to secure PIV from the first attempt for inpatients, resulting in poor patient satisfaction as well as overuse of other subspecialties like IR or critical care resources for rescue lines, with the SMART goal of successfully establishing PIV insertion in the maximum first two attempts or less within 6 to 12 months and sustaining this success for at least 6 months.
Through process mapping of the PIV flow, we identified gaps and possible contributing factors. The current flow for DIVA was vaguely defined, with no upper limit on the number of vein access attempts by bedside nurses. Furthermore, after the failure to secure the PIV, the usual process is to escalate to the on-call anesthesia team. If the anesthesia-led bedside attempts at PIV fail, the next step is usually an attempt at the central venous line by the ICU team or IR team, depending on the logistics. We also identified some unintended consequences of the current flow, including (1) suboptimal patient satisfaction, (2) overuse of anesthesia services outside the OR, and (3) overuse of ICU staff and critical care resources for DIVA patients outside critical care areas.
We identified the system processes and areas of improvement to be targeted in our project, which included (1) a lack of a clear definition of DIVA patients, (2) the presence of many brands of PIV cannulas, (3) a lack of utilization of PIV-related equipment such as vein viewers and ultrasound-guided PIV (USGPIV), and (4) a lack of clear DIVA flow and resources (ownership).
We created an initiative with a workflow that identifies potential DIVA cases based on prespecified criteria, limits the number of attempts for beside nurses, and introduces a nurse-led USGPIV and Midline line insertion program as a mitigation strategy to improve patient satisfaction and avoid overuse of anesthesia services, critical care staff, and IR services.
Knowledge About Variation
Through process mapping, literature review, and brainstorming, we identified the variables that could contribute to DIVA cases and determined which were modifiable, low-cost, and high-impact variables.
We created a database across hospitals to trace the percentage of PIV failures at the first attempt (Figs. 1 and 2). The samples were randomly and intermittently collected from different units because capturing all PIV attempts in real time in a large hospital is nearly impossible, given the sheer number of inpatients and PIV attempts. Initially, on average, less than 10% of patients had successful first attempts, and less than 15% had successful second attempts. In other words, the failure rate (defined as two or more failed attempts) of PIV was approximately 85%, which is above the international benchmark.[5]
Figure 1.
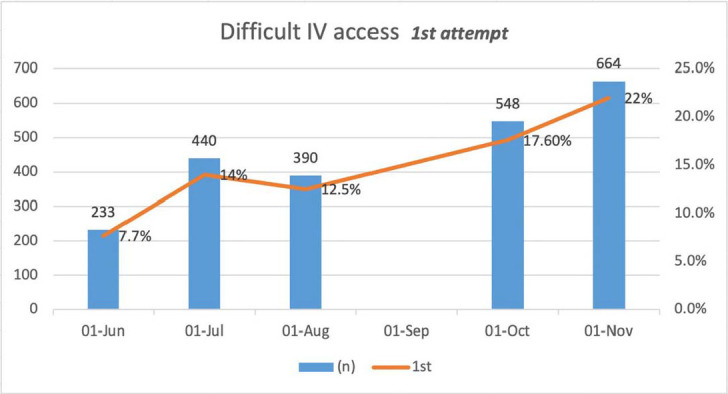
Percentage of successful first PIV attempts over time with number (n) of patients (randomly collected data from different units; only nurses attempts collected). PIV: peripheral intravenous access.
Figure 2.
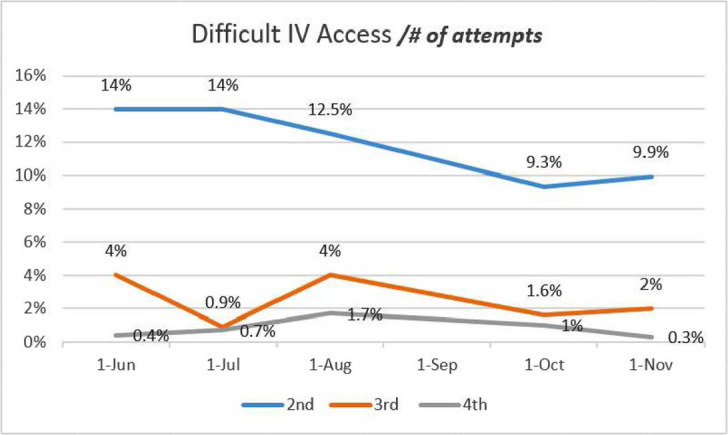
Percentage of second, third, and fourth PIV attempts (randomly collected data from different units, only nurses attempt collected). Total number of patients is the same as in Figure 1. PIV: peripheral intravenous access.
The main variations that could contribute to DIVA cases included the following: (1) new staff from different backgrounds in a new environment; (2) different brands of PIV cannulas; (3) a special population (our center’s core service is oncology, and most of these patients pose DIVA by virtue of their primary disease); (4) a lack of equipment and IV access-enhancing machines (i.e., vein viewers, USGPIV); and (5) a lack of clear flow and ownership of DIVA patients. We believe that new staff constituted a special cause of variation. The common cause variations could be (1) many brands of PIV cannulas with different techniques, (2) a clear definition of DIVA cases, and (3) the process of escalation in the case of a DIVA event and the level of competency in PIV using a vein viewer and/or USGPIV.
Theory of Knowledge
After reviewing the literature on DIVA and similar published projects, we established modified criteria by using the validated DIVA criteria and pathways.[6–8] The criteria were set to be broad in nature to capture most of the risk factors and variables that could lead to DIVA situations (Box 1). We also introduced a relatively novel approach, nurse-led USGPIV, for which many similar, successful, and cost-effective projects have been reported.[9–11]
Box 1 Difficult IV access (DIVA) case selection criteria
The presence of one or more factors qualifies the patient as a DIVA case:
No visible vein after the tourniquet
No palpable vein after the tourniquet
At least two previous attempts
Severe dehydration
Severe edema
Dark skin
An expert bedside nurse feels it is a DIVA case even with the absence of the above criteria
Family/parents are concerned about the IV access
Need for frequent blood extraction
Need IVF/antibiotics for 6 days or more and not be a candidate for PICC or CVC
IVF: intravenous fluid; PICC: peripherally inserted central venous catheter; CVC: central venous catheter.
Using plan-do-study-act cycles of improvement, we implemented different interventions. First, we created a DIVA team—a group of PIV experts available during working hours—as a clinical resource; this team is planned to be available after work hours and on weekends until we reach the advanced stage of the project. Second, we clearly defined the criteria used for screening DIVA cases and triggering DIVA requests (Box 1). Third, we created a DIVA pathway suited to our resources (Supplement 2: DIVA pathway). Fourth, we standardized the brands of PIV cannula used. We also used a vein viewer and USGPIV, including use of Midlines, as a long peripheral line with Midline guidelines (Box 2).
DIVA general guidelines for Midlines and rescue central lines
The decision to try another attempt at PIV versus Midline versus PICC shall be made as a joint decision between the DIVA team and the primary team based on the expected LOS and the need for frequent blood work.
The Midline line is not a central line and shall be used as a peripheral line with precaution, with maximum indwelling duration of 28 days.
PICC lines shall be inserted in radiology, whereas central lines shall be inserted in OR/ICU when indicated.
For adult patients, the central line shall be inserted by a consultant anesthetist (adult ICU), whereas for pediatric patients, the central line shall be inserted by a pediatric ICU consultant.
The primary physician of the patient is responsible for liaising with other departments to arrange for CVC and PICC.
PIV: peripheral intravenous; PICC: peripherally inserted central catheter; LOS: length of stay; OR: operating room; ICU: intensive care unit; CVC: central venous catheter.
Assessment, monitoring, and auditing live PIV insertions in different units was conducted by the DIVA team following efforts to increase awareness of DIVA cases via grand round lectures and physical rounds to different units by the DIVA team, over time, the number of failed PIV attempts declined, and use of Midline increasing over time (Figs. 1 and 2).
The Midline training program (called the DIVA program) started with carefully selected nursing staff (DIVA champions), who first had to master standard PIV lines under supervision (a minimum of 25 successful PIV insertions), master basic US skills via blue phantom simulations, assess Midline insertion on real patients (5 to 10 Midlines), and finally, complete a check-off list with at least 25 successful supervised Midline insertions on actual patients. After completing this training, the individual was acknowledged as a DIVA champion, with privileges to do USGPIV, including Midlines. Over time, we found the Midline to be a powerful, cost-effective PIV that improved patient satisfaction and prevented escalation to the insertion of central venous catheter (CVC) or peripherally inserted central catheter (PICC) lines, where the CVC or PICC was the ultimate intervention after many failed attempts at PIV.
Psychology
For the DIVA core team, we created incentivized measures for those who took the training and successfully passed the DIVA program, where they were recognized as DIVA champions with a certificate from our academic training affairs as well as an upgraded privilege in their credential file (we have three DIVA champions so far). This step creates a competitive spirit among staff to excel in their skills and credit those who accomplish the task.
For the general staff, the DIVA Taskforce held both group and individual meetings with frontline healthcare providers, mainly nursing staff. Discussions with frontline staff focused on DIVA cases, barriers, challenges, and potential solutions. Most of the implemented intervention ideas were developed during meetings, interviews, and discussions with the frontline staff, keeping them engaged and actively involved in the process. We also surveyed all our staff during the project’s initial phase to elicit their feedback regarding their impression of DIVA services, to keep them engaged and informed in this endeavor, and to advance the change in culture, where the DIVA case is everyone’s business and on everyone’s mind. Patient and staff survey results are presented in Figures 3 and 4 and supplemental material.
Figure 3.
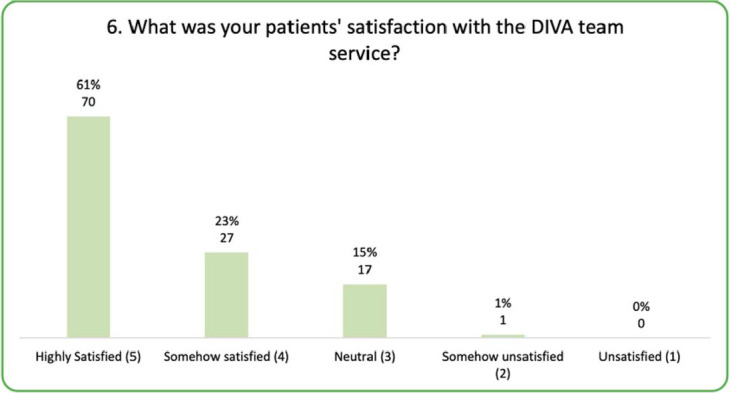
Perceived patient satisfaction with DIVA services. DIVA: difficult IV access.
Figure 4.
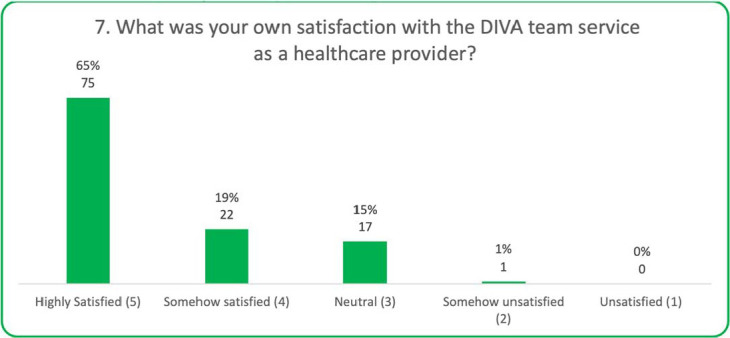
Staff satisfaction with DIVA services. DIVA: difficult IV access.
Limitations
This was a single-center project in a minimally diverse population, which might limit generalization of the findings.
SUMMARY
The lens of profound knowledge is a great conceptual framework that helps healthcare providers navigate through the process of creating and implementing a QI project. Using this tool can create a shared mental model among stakeholders and enable them to translate this shared model at the bedside.
Supplementary Material
Acknowledgment
We acknowledge Ms. Kathyrine Tayag (PICU-NICU Head Nurse, KFSHRC-M) for sorting PIV data and creating PIV attempt figures. We also acknowledge Ms. Dalal Aldhafeeri (Quality Data Management Coordinator, KFSHRC-M) for her work on the DIVA survey and for creating DIVA survey figures.
Footnotes
Source of Support: None. Conflict of Interest: Hakem Alomani is Chairperson of the Difficult IV Access (DIVA) Taskforce.
Supplemental Material
Supplemental materials are available online with the article.
References
- 1.Kazzaz Y. The lens of profound knowledge. Glob J Qual Saf Healthc. 2023;6:96–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deming WE. The New Economics for Industry, Government, Education. 2nd ed. MIT Press; 2000. [Google Scholar]
- 3.Helm RE Klausner JD Klemperer JD et al.. Accepted but unacceptable: peripheral IV catheter failure . J Infus Nurs. 2015;38:189–203. [DOI] [PubMed] [Google Scholar]
- 4.Sabri A Szalas J Holmes KS et al.. Failed attempts and improvement strategies in peripheral intravenous catheterization. Biomed Mater Eng. 2013;23:93–108. [DOI] [PubMed] [Google Scholar]
- 5.Pittiruti M Van Boxtel T Scoppettuolo G et al.. European recommendations on the proper indication and use of peripheral venous access devices (the ERPIUP consensus): a WoCoVA project. J Vasc Access. 2023;24:165–182. [DOI] [PubMed] [Google Scholar]
- 6.van Loon, FHJ van Hooff LWE de Boer HD et al.. The modified A-DIVA scale as a predictive tool for prospective identification of adult patients at risk of a difficult intravenous access: a multicenter validation study. J Clin Med. 2019;8:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Girotto C Arpone M Frigo AC et al.. External validation of the DIVA and DIVA3 clinical predictive rules to identify difficult intravenous access in paediatric patients. Emerg Med J. 2020;37:762–767. [DOI] [PubMed] [Google Scholar]
- 8.Sou V McManus C Mifflin N et al.. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore, C. An emergency department nurse-driven ultrasound-guided peripheral intravenous line program. J Assoc Vasc Acc. 2013;18:45–51. [Google Scholar]
- 10.Bahl A, Pandurangadu AV, Tucker J, Bagan M. A randomized controlled trial assessing the use of ultrasound for nurse-performed IV placement in difficult access ED patients. Am J Emerg Med. 2016;10:1950–1954. [DOI] [PubMed] [Google Scholar]
- 11.Davis EM Feinsmith S Amick AE et al.. Difficult intravenous access in the emergency department: Performance and impact of ultrasound-guided IV insertion performed by nurses. Am J Emerg Med. 2021;46:539–544. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


