Abstract
Objective:
Caregiving demands may influence caregivers’ sleep duration and quality, which are essential for optimal health. We aimed to examine the association between caregiving status and sleep deficiency (i.e., short sleep duration and/or poor quality) and identify factors associated with sleep deficiency among caregivers.
Methods:
This secondary analysis used data from 3870 adults living in the United States, obtained from the 2019 Health Information National Trends Survey. Multinomial logistic regressions were performed to examine the association between caregiving status (i.e., caregivers vs. non-caregivers) and sleep status (i.e., normal duration-good quality [optimal sleep, reference], short duration-good quality, normal duration-poor quality, and short duration-poor quality), and to identify caregiving-related factors associated with sleep deficiency in the caregiver group.
Results:
Compared to non-caregivers, caregivers were more likely to report short sleep duration (<7 hours) with good quality sleep (relative risk ratio [RRR] = 1.566, 95% CI [1.238, 1.980]) or poor quality sleep (RRR = 1.376, 95% CI [1.034, 1.832]) than the optimal sleep status. Caregivers providing care for ≥20 hours per week (vs. <20 hours) and providing care to individuals with dementia (vs. no dementia caregiving) were 2.8 times more likely to report normal sleep duration with poor sleep quality than optimal sleep (RRR = 2.796, 95% CI [1.125, 6.950]; RRR = 2.776, 95% CI [1.154, 6.675], respectively).
Conclusion:
The findings of a higher risk of sleep deficiency among caregivers suggest that health care providers need to assess both caregivers’ sleep duration and quality status. Interventions tailored to the caregiving context are also warranted.
Keywords: caregivers, health surveys, self-report, sleep deprivation
Introduction
Sleep plays an essential role in restoring body systems and regulating energy balance. Problems with sleep can impact physical and psychological health, as well as quality of life. 1 Sleep deficiency, characterized by insufficient quantity and/or inadequate quality of sleep, 2 is linked to various long-term health conditions, including an increased risk for obesity, diabetes, hypertension, and cardiovascular disease.3-6 For instance, in a prospective study of adults aged 40 years or older, self-reported short sleep duration (defined as <6 hours/day) and poor sleep quality (characterized by restless sleep and difficulty falling asleep) were associated with a 13% and 40% increased risk of coronary heart disease, respectively. 7 In addition, individuals in the lowest quartile of a composite score constructed by both sleep duration and quality had a 31% increased risk of coronary heart disease compared to those in the highest quartile. 7 The mechanism by which prolonged inadequate sleep affects the cardiovascular system remains unclear; however, studies have shown that sleep deficiency alters the sympathetic nervous system and hormonal, inflammatory, and coagulation profiles. 8 These changes can lead to hypertension, type 2 diabetes, atherosclerosis, and cardiovascular diseases.9,10
Sleep Deficiency in Caregivers
Estimates suggest that 53 million adults in the United States (U.S.) have provided care to their family members with special needs. 11 Among caregivers, some type of sleep deficiency is commonly reported, and it is often presumed to be linked to overnight care, care-recipient’s sleep disturbances, and caregivers’ psychological and physical health status.12,13 Studies have shown that 60% to 80% of caregivers of people with long-term illnesses have trouble sleeping.14-16 This rate is higher than that in the general population, in which only 20% to 40% reported poor sleep quality.5,17 Caregivers are more prone to report short sleep duration (<7 hours/day) than non-caregivers. 18 In addition, caregivers who have taken on responsibilities for 5 years or longer and those who provide higher-intensity caregiving (20-39 hours per week) are more likely to experience short sleep than their counterparts. 18
Evaluating sleep status should consider both quantitative and qualitative aspects of sleep, as one aspect alone cannot fully reflect an individual’s sleep. 19 Moreover, when both dimensions are assessed, individuals can be better stratified for their risks of health problems related to sleep deficiency. Indeed, research shows that poor sleep quality combined with short sleep duration predicts greater cardiovascular morbidity risks than a single component of sleep in the general population.20-22 Despite the importance of considering both aspects concurrently, most prior studies on caregivers’ sleep examined either sleep duration or quality.15,23,24 In addition, there have been few attempts to classify sleep deficiency by considering both sleep duration and quality using nationally representative data.
Given the significant role of sleep in maintaining optimal health, it is critical to examine whether caregiving responsibilities contribute to caregivers’ sleep deficiency and to identify characteristics of caregivers at higher risk of sleep deficiency. Therefore, the aims of this secondary data analysis study were, using data from a nationally representative sample of U.S. adults, (1) to determine whether caregiving status (i.e., caregivers vs. non-caregivers) was associated with sleep deficiency and (2) to identify caregiving-related factors associated with sleep deficiency while controlling for various confounders. We hypothesized that (1) caregivers would be more likely to report sleep deficiency than non-caregivers and (2) caregivers who spend more time providing care and take care of their spouses and individuals with dementia would be more likely to report sleep deficiency than their counterparts, given the higher risk of caregiving burden related to those conditions. 25 In this study, sleep status is categorized using both quantity (i.e., sleep duration) and quality of sleep, and sleep deficiency is defined as either short sleep duration, poor sleep quality, or both.
Methods
Design and Data
This secondary data analysis used data from the Health Information National Trends Survey (HINTS) ( www.hints.cancer.gov ) administered by the National Cancer Institute. HINTS is a nationally representative survey that collects data on the public’s use of cancer-related information among non-institutionalized civilian adults in the U.S. 26 For this study, we selected samples from HINTS 5 Cycle 3, which was conducted from January 22 to May 7, 2019. 27 Data for the survey were collected through mailed paper surveys or web-based surveys, with the web-based survey following a protocol identical to the physical distribution. We used combined data from the paper and web surveys.
The HINTS survey utilized a 2-stage sampling: (1) random sampling of households using residential addresses stratified by concentrations of minority populations with oversampling from the high-minority stratum; (2) selection of one adult within each sampled household. 28 The response rates for the paper-only and web pilot groups did not significantly differ, and the overall weighted response rate for the survey was 30.3%. The detailed study design and sampling strategies are described in the HINTS 5 Cycle 3 methodology report. 28 As this study involved the analysis of publicly available de-identified data, it was exempt from review by the institutional review board.
Sample
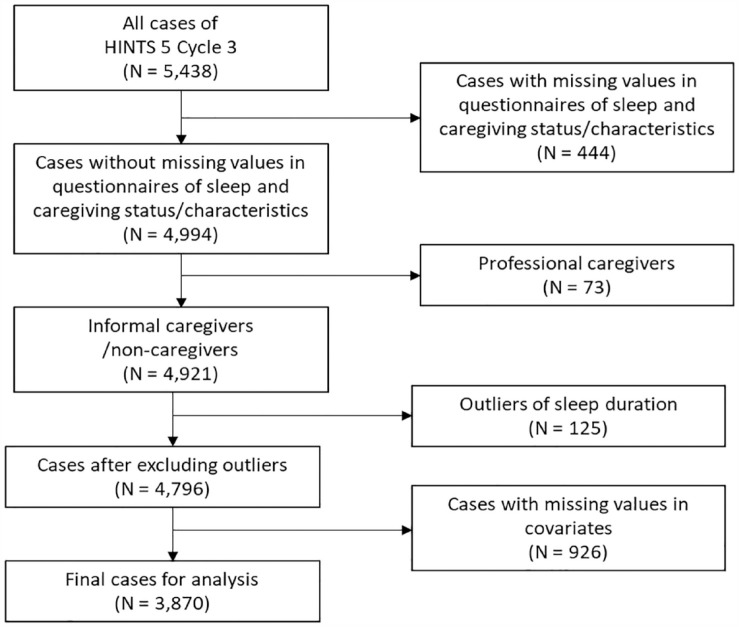
Among a total sample of 5438 adults from HINTS 5 Cycle 3, there were 4994 respondents who completed the questionnaires on sleep duration, sleep quality, caregiving status, and caregiving characteristics. We excluded respondents who provided care as part of a job (n = 73) to include only unpaid/informal caregivers. In addition, outliers of sleep duration (cases of ≤3 hours or ≥11 hours; n = 125) were excluded based on the sample’s mean sleep duration (7 hours) and interquartile range (6-8) to ensure valid data quality. Missing values in covariates ranged from 0.5% to 8.7%, and listwise deletion was conducted for complete case analysis. In summary, data from 3870 respondents were included in the analyses for this study (Figure 1).
Figure 1.
Sample selection flow diagram.
Measures
Sleep status
Sleep status was assessed using 2 questions about respondents’ sleep quantity (duration) and quality: “During the past 7 days, how many hours of sleep did you get on average per night?” and “In the past 7 days, how would you rate your sleep quality overall?” For sleep duration, respondents provided a numerical value in hours, while for sleep quality, they selected from response choices: “very bad, fairly bad, fairly good, or very good.” In this study, sleep duration responses were categorized into 2 groups using a cut-off point of 7 hours, following the American Academy of Sleep Medicine’s recommended sleep hours for adults. 29 Those reporting fewer than 7 hours were considered short sleepers. Sleep quality was dichotomized into poor (for the choices of very bad and fairly bad) and good (for choices of fairly good and very good) sleep quality. Further, accounting for the potential presence of concurrent sleep problems in terms of quantity and quality, sleep status was categorized into 4 groups using sleep duration and quality: normal sleep duration-good sleep quality (optimal sleep status, reference group), short duration-good quality, normal duration-poor quality, and short duration-poor quality (groups of sleep deficiency). Sleep deficiency was defined as short duration and/or poor sleep quality.
Caregiving status
Respondents indicated their caregiving status by answering the question, “Are you currently caring for or making healthcare decisions for someone with a medical, behavioral, disability, or other condition?” They identified their relationship with the care-recipient among the choices of “child, spouse/partner, parent(s), another family member, or friend/non-relative” or selected “No” if they were not caregivers. Caregiving status was categorized into 2 groups: caregivers who indicated the care-recipient and non-caregivers who answered “No.”
Caregiving characteristics
Caregiving characteristics included relationships with the care-recipient as described above, the care-recipient’s health conditions, and caregiving hours. Respondents who reported being a caregiver were subsequently asked to indicate “all conditions for which [they] have provided care.” Response options included cancer; Alzheimer’s, confusion, or dementia; orthopedic/musculoskeletal issues; mental health/behavioral/substance abuse issues; long-term conditions; neurological/developmental issues; acute conditions; aging/aging-related health issues; other; and not sure/don’t know. Respondents were allowed to indicate multiple caregiving conditions as applicable. In this study, care-recipients’ conditions and relationships with the care-recipient were dichotomized into either providing care for Alzheimer’s/confusion/dementia or not and either being spousal caregivers or not, as these characteristics are known to impose more caregiving burden. 25 Respondents were also asked to fill in “how many hours per week [they] spent in an average week providing care.” Caregiving hours were dichotomized into <20 hours and ≥20 hours per week, as reported previously. 18
Sociodemographic and health-related characteristics
Sociodemographic characteristics included age (<65, 65-74, ≥75 years), gender (male, female), race and ethnicity (Hispanic, non-Hispanic Asian, non-Hispanic Black or African American, non-Hispanic other [American Indian or Alaska native, Native Hawaiian or other Pacific Islander, multiple races mentioned], non-Hispanic White as prespecified in the survey data), marital status (married, not married), and household income (<$50 000, $50 000-$99 999, ≥$100 000). The variables of health behavior were smoking status (never smoker, former smoker, current smoker) and the frequency of moderate exercise (none, ≥1 time per week). In addition, the following were included as health indicators: body mass index (under/normal weight, overweight, and obesity), medical conditions (a composite number of diabetes, hypertension, heart condition, long-term lung disease, and depression or anxiety disorder; 0-1 condition, 2-5 conditions), self-rated general health (excellent/very good, good, fair/poor), and psychological distress (Patient Health Questionnaire-4; no/mild symptoms, moderate/severe symptoms). 30
Data Analyses
Due to the complex sampling procedure and different survey methods used for data collection, the final sample weights and Taylor Series variance estimation methods were used for the analyses to compute the correct variance estimates per the HINTS data analysis recommendations. 27 We conducted a chi-square independence test to describe differences in sociodemographic and health-related characteristics and sleep status between caregivers and non-caregivers.
For the first specific aim to determine the association between caregiving status and sleep deficiency, we conducted a multinomial logistic regression analysis while controlling for sociodemographic and health-related characteristics (age, gender, race and ethnicity, marital status, household income, smoking status, exercise, body mass index, medical conditions, general health status, and psychological distress) in the entire sample. Due to the unbalanced size of the subgroups, the sample was dichotomized into non-Hispanic White versus Hispanic, non-Hispanic Asian, non-Hispanic Black or African American, and non-Hispanic other for the inference data analysis. For the second specific aim to identify caregiving-related factors associated with sleep deficiency, we conducted a multinominal logistic regression exclusively within the caregiver group, considering caregiving factors (i.e., caregiving hours, dementia caregiving, and spousal caregiving) and controlling for sociodemographic and health-related characteristics. The type 1 error rate was set to .05, and all data analyses were performed using IBM SPSS Statistics (Version 28).
Results
Sample Characteristics
Table 1 displays the descriptive statistics for sociodemographic and health-related characteristics, as well as sleep status, of the analytic sample by caregiving status. Out of the total sample of respondents (N = 3870), 12.6% identified themselves as caregivers (n = 487). Most of the respondents (82.1%) were under 65 years of age (mean = 55, SD = 17.2), and 49.7% were female. In terms of race and ethnicity, 65.5% identified as non-Hispanic White, followed by Hispanic (14.3%), non-Hispanic Black or African American (12.2%), non-Hispanic Asian (4.9%), and non-Hispanic other (3.0%). Approximately 57.3% of respondents were married, and 38.8% lived in low-income households. The majority of respondents were never-smokers (64.8%) and reported engaging in moderate exercise at least once a week (75.3%). Regarding medical conditions, 76.3% reported having fewer than 2 conditions. Furthermore, 51.7% rated their health status as very good or good, and 86.5% had no or mild symptoms of psychological distress. More than half (56.2%) fell into the category of normal duration-good quality, followed by short duration-good quality (22.8%), short duration-poor quality (14.6%), and normal duration-poor quality (6.3%). Caregivers were more likely to be female, married, and have higher household incomes compared to non-caregivers. Other characteristics and sleep status did not differ significantly by caregiving status.
Table 1.
Study Sample Characteristics.
| Total | Caregivers | Non-caregivers | |||
|---|---|---|---|---|---|
| N = 3870 | n = 487 | n = 3383 | |||
| n (weighted %) | n (weighted %) | χ2 (df) | p | ||
| Age, years | 3.94 (2) | .327 | |||
| <65 | 2551 (82.1) | 366 (85.2) | 2185 (81.6) | ||
| 65-74 | 843 (10.8) | 80 (8.9) | 763 (11.1) | ||
| ≥75 | 476 (7.1) | 41 (5.9) | 435 (7.2) | ||
| Gender | 21.62 (1) | .004 | |||
| Male | 1708 (50.3) | 180 (40.5) | 1528 (51.7) | ||
| Female | 2162 (49.7) | 307 (59.5) | 1855 (48.3) | ||
| Race and ethnicity | 24.73 (1) | .111 | |||
| Hispanic | 555 (14.3) | 73 (15.9) | 482 (15.9) | ||
| Non-Hispanic Asian | 191 (4.9) | 29 (9.6) | 162 (5.3) | ||
| Non-Hispanic Black or African American | 473 (12.2) | 58 (7.6) | 415 (10.6) | ||
| Non-Hispanic Other a | 117 (3.0) | 20 (4.8) | 97 (2.7) | ||
| Non-Hispanic White | 2534 (65.5) | 307 (62.1) | 2227 (65.4) | ||
| Marital status | 65.43 (1) | <.001 | |||
| Married | 2217 (57.3) | 338 (73.8) | 1879 (54.9) | ||
| Not married | 1629 (42.7) | 145 (26.2) | 1484 (45.1) | ||
| Household income | 30.84 (2) | .002 | |||
| <$50 000 | 1515 (38.8) | 149 (28.0) | 1366 (40.4) | ||
| $50 000-$99 999 | 1236 (31.8) | 163 (35.1) | 1073 (31.3) | ||
| ≥$100 000 | 1113 (29.4) | 174 (36.9) | 939 (28.3) | ||
| Smoking status | 1.366 (2) | .740 | |||
| Never | 2415 (64.8) | 305 (63.8) | 2110 (64.9) | ||
| Former | 1033 (23.6) | 136 (25.5) | 897 (23.3) | ||
| Current | 422 (11.6) | 46 (10.7) | 376 (11.7) | ||
| Moderate exercise | 6.42 (1) | .084 | |||
| None | 957 (24.7) | 111 (20.2) | 846 (25.3) | ||
| ≥1 time per week | 2913 (75.3) | 376 (79.8) | 2537 (74.7) | ||
| Body mass index | 4.01 (2) | .464 | |||
| Under/normal weight | 1228 (31.8) | 140 (31.5) | 1088 (31.8) | ||
| Overweight | 1349 (34.8) | 156 (31.5) | 1193 (35.3) | ||
| Obesity | 1293 (33.4) | 191 (37.0) | 1102 (32.9) | ||
| Medical conditions b | 1.225 (1) | .463 | |||
| 0-1 condition | 2777 (76.3) | 352 (74.3) | 2425 (76.6) | ||
| 2-5 conditions | 1093 (23.7) | 135 (25.7) | 958 (23.4) | ||
| General health | 0.480 (2) | .914 | |||
| Very good/excellent | 1958 (51.7) | 249 (52.9) | 1709 (51.6) | ||
| Good | 1381 (34.5) | 178 (34.1) | 1203 (34.5) | ||
| Fair/poor | 531 (13.8) | 60 (12.9) | 471 (13.9) | ||
| Psychological distress | 0.008 (1) | .956 | |||
| No/mild symptoms | 3474 (86.5) | 432 (86.3) | 3042 (86.5) | ||
| Moderate/severe symptoms | 396 (13.5) | 55 (13.7) | 341 (13.5) | ||
| Sleep status | 4.377 (3) | .599 | |||
| Normal duration & good quality | 2192 (56.2) | 235 (52.9) | 1957 (56.7) | ||
| Short duration & good quality | 879 (22.8) | 137 (26.5) | 742 (22.3) | ||
| Normal duration & poor quality | 223 (6.3) | 28 (6.2) | 195 (6.4) | ||
| Short duration & poor quality | 576 (14.6) | 87 (14.4) | 489 (14.6) |
Non-Hispanic Other category includes American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and multiple races mentioned.
Medical conditions include diabetes, hypertension, heart condition (heart attack, angina, or congestive heart failure), long-term lung disease (asthma, emphysema, or long-term bronchitis), depression, and anxiety disorder.
Among the caregivers (n = 487), 31.0% provided care for a child or children, and 28.1% cared for parent(s), followed by 17.5% who were spousal caregivers and 11.3% who cared for multiple care-recipients (data not shown). Thirty-seven percent of the caregivers reported caring for long-term conditions, followed by orthopedic/musculoskeletal (27.3%), Alzheimer’s disease or dementia (25.7%), and mental or behavioral issues (25.7%). Most caregivers provided care for more than one condition (50.1%). The median caregiving hours were 10 hours per week (interquartile range = 3-30), and 37.4% of the caregivers reported spending 20 hours or more per week providing care.
Caregiving Status as an Associated Factor of Self-Reported Sleep Deficiency
As Table 2 presents, compared to non-caregivers, caregivers were 1.4 times more likely to fall into the group of short sleep duration-poor sleep quality (relative risk ratio [RRR] = 1.376, 95% confidence interval [CI] = 1.034, 1.832) rather than normal duration-good quality (i.e., optimal sleep status), controlling for the potential confounding factors. Also, caregivers were 1.6 times more likely to be in the group of short sleep duration-good sleep quality (RRR = 1.566, 95% CI = 1.238, 1.980) rather than the optimal sleep status, relative to non-caregivers. In addition to being a caregiver, race and ethnicity of Hispanic, non-Hispanic Asian, non-Hispanic Black or African American, or non-Hispanic other (vs. non-Hispanic White), current smoker (vs. never smoker), good and fair/poor self-rated general health (vs. very good/excellent), and moderate to severe psychological distress (vs. no/mild symptoms) were associated with higher odds of reporting both short sleep duration and poor sleep quality than the optimal sleep status. Conversely, older age (vs. <65 years), higher household income ≥$100 000 (vs. <$50 000), and engaging in at least 1 time of moderate exercise per week were associated with lower odds of reporting both short sleep duration and poor sleep quality than the optimal sleep status.
Table 2.
Multinominal Logistic Regression of Sleep Deficiency a (N = 3870).
| Short duration & good quality | Normal duration & poor quality | Short duration & poor quality | ||||
|---|---|---|---|---|---|---|
| RRR (95% CI) | p | RRR (95% CI) | p | RRR (95% CI) | p | |
| Caregiving status | ||||||
| Non-caregivers | Ref. | Ref. | Ref. | |||
| Caregivers | 1.566 (1.238, 1.980) | <.001 | 1.297 (0.841, 1.999) | .240 | 1.376 (1.034, 1.832) | .029 |
| Age, years | ||||||
| <65 | Ref. | Ref. | Ref. | |||
| 65-74 | 0.810 (0.659, 0.996) | .046 | 0.528 (0.356, 0.783) | .001 | 0.520 (0.396, 0.682) | <.001 |
| ≥75 | 0.716 (0.546-0.941) | .016 | 0.477 (0.297, 0.773) | .003 | 0.455 (0.318, 0.650) | <.001 |
| Gender | ||||||
| Male | Ref. | Ref. | Ref. | |||
| Female | 0.886 (0.749, 1.047) | .155 | 0.867 (0.647, 1.161) | .338 | 1.011 (0.825, 1.240) | .915 |
| Race and ethnicity | ||||||
| Non-Hispanic White | Ref. | Ref. | Ref. | |||
| Hispanic, non-Hispanic Black, non-Hispanic Asian, non-Hispanic Other | 1.624 (1.369, 1.927) | <.001 | 0.630 (0.450, 0.881) | .007 | 1.289 (1.046, 1.589) | .017 |
| Marital status | ||||||
| Not married | Ref. | Ref | Ref. | |||
| Married | 0.820 (0.685, 0.981) | .030 | 0.667 (0.486, 0.915) | .012 | 0.907 (0.729, 1.129) | .383 |
| Household income | ||||||
| <$50 000 | Ref. | Ref. | Ref. | |||
| $50 000-$99 999 | 0.960 (0.776, 1.188) | .707 | 0.739 (0.502, 1.087) | .124 | 0.845 (0.655, 1.091) | .197 |
| ≥$100 000 | 0.990 (0.788, 1.243) | .929 | 0.825 (0.551, 1.235) | .350 | 0.687 (0.519, 0.908) | .008 |
| Smoking status | ||||||
| Never | Ref. | Ref. | Ref. | |||
| Former | 1.122 (0.924, 1.362) | .244 | 1.191 (0.853, 1.663) | .306 | 1.223 (0.967, 1.545) | .093 |
| Current | 1.418 (1.085, 1.853) | .010 | 0.988 (0.620, 1.574) | .959 | 1.476 (1.084, 2.011) | .014 |
| Moderate exercise | ||||||
| None | Ref. | Ref. | Ref. | |||
| ≥1 time per week | 0.883 (0.725, 1.076) | .218 | 0.800 (0.569, 1.125) | .199 | 0.701 (0.559, 0.880) | .002 |
| Body mass index | ||||||
| Under/normal weight | Ref. | Ref. | Ref. | |||
| Overweight | 1.020 (0.832, 1.251) | .848 | 0.659 (0.471, 0.920) | .014 | 1.002 (0.778, 1.291) | .988 |
| Obesity | 1.321 (1.070, 1.631) | .009 | 0.444 (0.302, 0.652) | <.001 | 1.139 (0.879, 1.475) | .325 |
| Medical conditions | ||||||
| 0-1 condition | Ref. | Ref. | Ref. | |||
| 2-5 conditions | 1.106 (0.909, 1.346) | .313 | 1.066 (0.753, 1.509) | .717 | 1.114 (0.883, 1.406) | .362 |
| General health | ||||||
| Very good/excellent | Ref. | Ref. | Ref. | |||
| Good | 1.312 (1.090, 1.579) | .004 | 1.666 (1.175, 2.363) | .004 | 2.398 (1.899, 3.027) | <.001 |
| Fair/poor | 1.707 (1.288, 2.264) | <.001 | 4.174 (2.669, 6.529) | <.001 | 3.463 (2.500, 4.797) | <.001 |
| Psychological distress | ||||||
| No/mild symptoms | Ref. | Ref. | Ref. | |||
| Moderate/severe symptoms | 0.970 (0.699, 1.345) | .853 | 3.281 (2.218, 4.853) | <.001 | 3.534 (2.659, 4.696) | <.001 |
Abbreviations: CI: confidence interval; RRR: relative risk ratio.
Reference group: normal sleep duration & good sleep quality.
Factors Associated With Self-Reported Sleep Deficiency Among Caregivers
As Table 3 presents, caregivers who spent 20 hours or longer per week providing care were 2.8 times more likely to report normal sleep duration and poor sleep quality than normal duration-good quality sleep (i.e., optimal sleep status), relative to those who spent less than 20 hours (RRR = 2.796, 95% CI = 1.125, 6.950). Caregivers who provided care for individuals with dementia were also 2.8 times more likely to report normal sleep duration and poor sleep quality (RRR = 2.776, 95% CI = 1.154, 6.675) than the optimal sleep status, relative to those caring for individuals with other health conditions. Spousal caregiving was not associated with sleep deficiency.
Table 3.
Multinomial Logistic Regression of Sleep Deficiency Among Caregivers a (n = 487).
| Short duration & good quality | Normal duration & poor quality | Short duration & poor quality | ||||
|---|---|---|---|---|---|---|
| RRR (95% CI) | p | RRR (95% CI) | p | RRR (95% CI) | p | |
| Caregiving hours b | ||||||
| <20 hours/week | Ref. | Ref. | Ref. | |||
| ≥20 hours/week | 1.618 (0.991, 2.640) | .054 | 2.796 (1.125, 6.950) | .027 | 1.357 (0.733, 2.512) | .332 |
| Dementia care b | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 1.063 (0.629, 1.795) | .821 | 2.776 (1.154, 6.675) | .023 | 1.412 (0.756, 2.637) | .279 |
| Spousal caregiver b | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 1.076 (0.592, 1.953) | .811 | 0.626 (0.168, 2.332) | .485 | 1.362 (0.652, 2.846) | .411 |
Abbreviations: CI: confidence interval; RRR: relative risk ratio.
Reference group: normal sleep duration & good sleep quality.
Age, gender, race and ethnicity, marital status, household income, smoking status, moderate exercise, body mass index, medical conditions, general health, and psychological distress controlled for.
Discussion
We examined whether caregiving status was independently associated with sleep deficiency, defined as short sleep duration and/or poor sleep quality, using the U.S. nationally representative survey data. Our findings indicate that caregivers are at a higher risk of experiencing sleep deficiency, including both short sleep duration with poor sleep quality and short sleep duration with good sleep quality, rather than the optimal sleep status (i.e., ≥7 hours of good quality sleep), compared to non-caregivers. Among caregivers, those who provide care for extended hours (≥20 hours/week) and those taking care of individuals with dementia are more likely to report normal sleep duration with poor sleep quality than normal duration-good quality sleep. This study is among a few attempts to assess the sleep status of caregivers and its associated factors using both sleep duration and quality concurrently in a nationally representative sample.
Sleep is increasingly recognized as a critical lifestyle factor that affects health. A growing body of evidence demonstrates that suboptimal sleep is closely linked to adverse psychological and physical health outcomes, including mood disorders, obesity, type 2 diabetes, cancer, hypertension, cardiovascular disease, and mortality.31-36 Despite the importance of sleep for health and the vulnerability of caregivers to sleep deficiency, research investigating how sleep problems can lead to long-term health conditions and manifest diseases in the caregiver population remains scarce. Further investigation into these relationships would provide valuable insight into the mechanism underlying the health impacts of caregiving.
Research suggests that individuals with both short sleep duration and poor sleep quality, often characterized by insomnia symptoms, have a greater risk of hypertension, cardiovascular diseases,20-22 and mortality 37 compared to those with either condition alone. In our study, the subgroup experiencing short sleep duration and poor sleep quality, which represents the most severe phenotype in terms of health consequences, 38 accounted for approximately 15% of both the total sample and the caregiver sub-sample. Each phenotype of sleep deficiency, such as short sleep duration only, poor sleep quality only, or short sleep duration with poor sleep quality, is known to potentially have different causes, pathophysiologies, and subsequent treatment options. 38 For instance, the phenotype of poor sleep quality with short sleep duration appears to be related to physiological hyperarousal and may respond better to biological treatments (e.g., medication) aimed at reducing the hyperarousal and increasing sleep duration. 38 On the other hand, the phenotype of poor sleep quality with normal sleep duration is associated with cognitive-emotional hyperarousal, which may benefit more from cognitive and behavioral therapy targeting the reduction of hyperarousal and restructuring of sleep-related perceptions. 38 Therefore, further exploration of different phenotypes of sleep deficiency, their associated factors, and their impacts on health outcomes in caregivers is warranted to develop targeted approaches for improving their sleep health.
Among caregivers in the current study, those who spent 20 hours or longer per week providing care appeared to be more likely to experience the sleep deficiency type of normal duration-poor quality of sleep rather than normal duration-good quality sleep, compared to those with fewer hours of caregiving. Caregivers providing care for longer hours also tended to experience short sleep duration-good quality, but the association did not reach statistical significance. Longer caregiving hours, one of the indicators of objective caregiving burden, have been associated with suboptimal sleep status among caregivers. For example, longer hours dedicated to caregiving predicted poorer self-reported sleep quality, 39 and short sleep duration was more prevalent in caregivers who provided 20 to 39 hours of caregiving per week, compared to those with fewer than 20 hours of caregiving. 18 Our findings build upon the existing evidence that extended hours of caregiving may affect caregivers’ sleep quality as well as may curtail the absolute bedtime of caregivers. Given that caregivers experiencing sleep deficiency are more susceptible to physical strain and psychological symptoms compared to those who do not, 40 these findings underscore the importance of implementing sleep interventions and establishing support systems that facilitate uninterrupted sleep or allow for catch-up sleep for highly committed caregivers.
Caregivers who cared for individuals with dementia were also nearly 3 times more likely to experience the sleep deficiency type of normal sleep duration with poor sleep quality, compared to other types of caregivers. This result contradicts a recent population-based study that reported no difference in self-reported sleep quality between dementia and non-dementia caregivers. 41 Most studies on sleep in caregivers have predominantly focused on those providing care for individuals with dementia, and there is limited data comparing sleep between dementia caregivers and caregivers for other conditions. However, behavioral, psychiatric, and psychological symptoms, especially nocturnal disturbances of people with dementia, are known to contribute to the onset and progression of caregivers’ sleep problems.13,42 The responsibilities of nighttime caregiving disrupt caregivers’ sleep, and they may be less satisfied with their sleep quality compared to caregivers of individuals with other health conditions, regardless of their actual sleep duration. Considering the potential reciprocal relationship between the sleep of the caregiver and care-recipient, 43 further studies are needed to identify care-recipient factors, such as diagnoses, levels of dependence, sleep quality of the care-recipient, and the dyadic association of sleep deficiency. Such studies will help in identifying caregivers at a high risk of sleep deficiency and inform dyadic approaches to interventions.
Limitations
A few points should be considered when interpreting the findings. First, due to the nature of cross-sectional data, the study design precludes causal inferences. A longitudinal assessment is suggested to determine whether caregiving causes sleep deficiency. Second, additional confounders related to caregiving, which would have been accounted for in the analysis among caregivers, were not collected in HINTS 5, Cycle 3. Further research is warranted to determine whether the sleep status of caregivers varies by diverse caregiving characteristics, such as duration and intensity of caregiving, the care-recipient’s age and functional status, and caregivers’ psychological, behavioral, and environmental factors. Third, because HINTS is based on self-reporting, the data are susceptible to recall bias. In addition, a single question about sleep quality may not have fully captured respondents’ quality of habitual sleep. Studies indicate that self-reported sleep tends to either under- or overestimate the actual sleep duration when compared to objective sleep measures. 44 Also, self-reported sleep quality is subject to perceptions that vary by individual and contextual characteristics (e.g., age, caregiving context). Objective measures can provide more detailed information on sleep quality, such as sleep latency, fragmentation, and sleep-wake cycles. Thus, as the National Sleep Foundation recommends, it is imperative to use objective measures concurrently with self-reporting to obtain more reliable and comprehensive evidence of the association between caregiving status and sleep. 45 Lastly, selection bias related to the low response rate in the survey might have influenced our study findings.
Despite these limitations, this study presents evidence that caregiving status is an independent risk factor for sleep deficiency. By using nationally representative survey data, the results are rather generalizable. Furthermore, a set of potential confounders regarding health conditions and health behaviors, in addition to sociodemographic factors, were controlled for in the analyses. This inclusion helped examine the sole impact of caregiving status on sleep deficiency. This study is also distinctive from most previous studies of caregivers’ sleep in that it included caregivers who provided care for various conditions, allowing the examination of sleep status across different disease conditions of care-recipients.
As the aging population grows and the demand for family/informal caregivers steadily rises, sleep deficiency among caregivers emerges as a substantial health concern impacting a considerable segment of the population. Consequently, there is a pressing need to prioritize caregivers’ sleep as an integral aspect of their overall health needs. Health care providers are recommended to pay more attention to caregivers’ quantity and quality of sleep status, which is a modifiable behavioral factor. It is also important to educate caregivers to report their sleep problems to primary health care providers so that they can receive timely and appropriate help. The development of interventions tailored to types of sleep deficiency, caregiving context, and underlying needs of caregivers is needed in an effort to mitigate the risk of subsequent health outcomes. These efforts will create more supportive and empowering environments in which caregivers can maintain their optimal health status.
Conclusions
The results of this study provide evidence that caregivers are more likely to be at risk for sleep deficiency and that the risk may be even higher when caregivers provide care for longer hours and to loved ones with dementia. Given that sleep deficiency and accumulating sleep debt may affect one’s ability to care for their loved ones and increase the risk of developing diseases in the future, it is critical to take caregivers’ sleep status into account in an effort to improve the health of caregivers.
Footnotes
All author(s) declare that they have no conflicts of interest.
Funding: The author(s) received no financial support for the research, authorship, or publication of this article.
ORCID iDs: Soojung Ahn  https://orcid.org/0000-0002-4234-3576
https://orcid.org/0000-0002-4234-3576
Jeongok G. Logan  https://orcid.org/0000-0002-6599-6975
https://orcid.org/0000-0002-6599-6975
References
- 1. Lo CMH, Lee PH. Prevalence and impacts of poor sleep on quality of life and associated factors of good sleepers in a sample of older Chinese adults. Health Qual Life Outcomes. 2012;10:72. doi: 10.1186/1477-7525-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jackson CL, Redline S, Emmons KM. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health. 2015;36(1):417-440. doi: 10.1146/annurev-publhealth-031914-122838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Buxton OM, Cain SW, O’Connor SP, et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med. 2012;4(129):129ra43. doi: 10.1126/scitranslmed.3003200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Knutson KL, Van Cauter E, Rathouz PJ, et al. Association between sleep and blood pressure in midlife: the CARDIA sleep study. Arch Intern Med. 2009;169(11):1055-1061. doi: 10.1001/archinternmed.2009.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Krittanawong C, Kumar A, Wang Z, et al. Sleep duration and [cardiovascular health in a representative community population (from NHANES, 2005 to 2016). Am J Cardiol. 2020;127:149-155. doi: 10.1016/j.amjcard.2020.04.012. [DOI] [PubMed] [Google Scholar]
- 6. Kwok CS, Kontopantelis E, Kuligowski G, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: a dose-response meta-analysis. J Am Heart Assoc. 2018;7(15):e008522. doi: 10.1161/JAHA.118.008552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lao XQ, Liu X, Deng HB, et al. Sleep quality, sleep duration, and the risk of coronary heart disease: a prospective cohort study with 60, 586 adults. J Clin Sleep Med. 2018;14(1):109-117. doi: 10.5664/jcsm.6894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tobaldini E, Costantino G, Solbiati M, et al. Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases. Neurosci Biobehav Rev. 2017;74(PtB):321-329. doi: 10.1016/j.neubiorev.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 9. Mullington JM, Haack M, Toth M, Serrador JM, Meier-Ewert HK. Cardiovascular, inflammatory, and metabolic consequences of sleep deprivation. Prog Cardiovasc Dis. 2009;51(4):294-302. doi: 10.1016/j.pcad.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zheng B, Yu C, Lv J, et al. Insomnia symptoms and risk of cardiovascular diseases among 0.5 million adults: a 10-year cohort. Neurology. 2019;93(23):e2110-e2120. doi: 10.1212/WNL.0000000000008581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. National Alliance for Caregiving and AARP. Caregiving in the U.S. 2020: AARP research report. 2020. Accessed June 9, 2020. https://www.caregiving.org/caregiving-in-the-us-2020/
- 12. McCurry SM, Song Y, Martin JL. Sleep in caregivers. Curr Opin Psychiatry. 2015;28(6):497-503. doi: 10.1097/YCO.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 13. McCurry SM, Logsdon RG, Teri L, Vitiello MV. Sleep disturbances in caregivers of persons with dementia: contributing factors and treatment implications. Sleep Med Rev. 2007;11(2):143-153. doi: 10.1016/j.smrv.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chiu Y-C, Lee Y-N, Wang P-C, et al. Family caregivers’ sleep disturbance and its associations with multilevel stressors when caring for patients with dementia. Aging Ment Health. 2014;18(1):92-101. doi: 10.1080/13607863.2013.837141. [DOI] [PubMed] [Google Scholar]
- 15. Cupidi C, Realmuto S, Lo Coco G, et al. Sleep quality in caregivers of patients with Alzheimer’s disease and Parkinson’s disease and its relationship to quality of life. Int Psychogeriatr. 2012;24(11):1827-1835. doi: 10.1017/S1041610212001032. [DOI] [PubMed] [Google Scholar]
- 16. Lee K, Yiin J, Lu S, Chao Y. The burden of caregiving and sleep disturbance among family caregivers of advanced cancer patients. Cancer Nurs. 2015;38(4):E10-E18. doi: 10.1097/NCC.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 17. Grandner MA. Sleep, health, and society. Sleep Med Clin. 2017;12(1):1-22. doi: 10.1016/j.jsmc.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Liu Y, Wheaton AG, Edwards VJ, Xu F, Greenlund KJ, Croft JB. Short self-reported sleep duration among caregivers and non-caregivers in 2016. Sleep Health. 2020;6(5):651-656. doi: 10.1016/j.sleh.2020.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Malik SW, Kaplan J. Sleep deprivation. Prim Care. 2005;32(2):475-490. doi: 10.1016/j.pop.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 20. Fernandez-Mendoza J, Vgontzas AN, Liao D, et al. Insomnia with objective short sleep duration and incident hypertension: the Penn State Cohort. Hypertension. 2012;60(4):929-935. doi: 10.1161/HYPERTENSIONAHA.112.193268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32(4):491-497. doi: 10.1093/sleep/32.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bertisch SM, Pollock BD, Mittleman MA, et al. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep. 2018;41(6):zsy047. doi: 10.1093/SLEEP/ZSY047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sakurai S, Onishi J, Hirai M. Impaired autonomic nervous system activity during sleep in family caregivers of ambulatory dementia patients in Japan. Biol Res Nurs. 2015;17(1):21-28. doi: 10.1177/1099800414524050. [DOI] [PubMed] [Google Scholar]
- 24. Willette-Murphy K, Todero C, Yeaworth R. Mental health and sleep of older wife caregivers for spouses with Alzheimer’s disease and related disorders. Issues Ment Health Nurs. 2006;27(8):837-852. doi: 10.1080/01612840600840711. [DOI] [PubMed] [Google Scholar]
- 25. Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. Am J Nurs. 2008;108(9 suppl):23-27; quiz 27. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nelson DE, Kreps GL, Hesse BW, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9(5):443-460; discussion 81. doi: 10.1080/10810730490504233. [DOI] [PubMed] [Google Scholar]
- 27. National Cancer Institute. Health Information National Trends Survey (HINTS) 5 cycle 3: survey overview and data analysis recommendations. Published 2019. Accessed May 4, 2020. https://hints.cancer.gov/data/download-data.aspx
- 28. National Cancer Institute. Health Information National Trends Survey 5 (HINTS 5). Published 2019. Accessed May 4, 2020. https://hints.cancer.gov/docs/Instruments/HINTS5_Cycle3_MethodologyReport.pdf
- 29. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843-844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kroenke K, Spitzer RL, Williams JBW, Lowe B. An Ultra-Brief Screening Scale for Anxiety and Depression: the PHQ-4. Psychosomatics. 2009;50(6):613-621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 31. Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18(2):148-158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 32. Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2016;16(1):375. doi: 10.1186/s12888-016-1075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Li Y, Cai S, Ling Y, et al. Association between total sleep time and all cancer mortality: non-linear dose-response meta-analysis of cohort studies. Sleep Med. 2019;60:211-218. doi: 10.1016/j.sleep.2019.03.026. [DOI] [PubMed] [Google Scholar]
- 34. Calhoun DA, Harding SM. Sleep and hypertension. Chest. 2010;138(2):434-443. doi: 10.1378/chest.09-2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414-420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Heal. 2017;3(5):383-388. doi: 10.1016/j.sleh.2017.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Vgontzas AN, Liao D, Pejovic S, et al. Insomnia with short sleep duration and mortality: the Penn State cohort. Sleep. 2010;33(9):1159-1164. doi: 10.1093/sleep/33.9.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17(4):241-254. doi: 10.1016/j.smrv.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Valero-Cantero I, Wärnberg J, Carrión-Velasco Y, Martínez-Valero FJ, Casals C, Vázquez-Sánchez MÁ. Predictors of sleep disturbances in caregivers of patients with advanced cancer receiving home palliative care: a descriptive cross-sectional study. Eur J Oncol Nurs. 2021;51:101907. doi: 10.1016/j.ejon.2021.101907. [DOI] [PubMed] [Google Scholar]
- 40. Kahn M, Sheppes G, Sadeh A. Sleep and emotions: bidirectional links and underlying mechanisms. Int J Psychophysiol. 2013;89(2):218-228. doi: 10.1016/j.ijpsycho.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 41. Blinka MD, Spira AP, Sheehan OC, et al. Sleep quality reports from family caregivers and matched non-caregiving controls in a population-based study. J Appl Gerontol. 2022;41(6):1568-1575. doi: 10.1177/07334648221079110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Simpson C, Carter P. Dementia behavioural and psychiatric symptoms: effect on caregiver’s sleep. J Clin Nurs. 2013;22(21-22):3042-3052. doi: 10.1111/jocn.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kotronoulas G, Wengström Y, Kearney N. Sleep and sleep-wake disturbances in care recipient-caregiver dyads in the context of a chronic illness: a critical review of the literature. J Pain Symptom Manage. 2013;45(3):579-594. doi: 10.1016/j.jpainsymman.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 44. Jackson CL, Patel SR, Jackson WB, 2nd, Lutsey PL, Redline S. Agreement between self-reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: Multi-Ethnic Study of Atherosclerosis. Sleep. 2018;41(6). doi: 10.1093/sleep/zsy057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ohayon M, Wickwire EM, Hirshkowitz M, et al. National Sleep Foundation’s sleep quality recommendations: first report. Sleep Health. 2017;3(1):6-19. doi: 10.1016/j.sleh.2016.11.006. [DOI] [PubMed] [Google Scholar]