Abstract
Epiploic appendagitis is a benign and self-limiting condition that has garnered more recognition, particularly in preoperative settings, thanks to advancements in imaging techniques, notably computed tomography (CT). Its distinct radiologic features facilitate accurate diagnosis prior to surgery. Despite its unique characteristics, the clinical presentation of epiploic appendagitis often resembles that of various other intra-abdominal medical and surgical conditions, leading to potential confusion. Here, we present the case of a 37-year-old otherwise healthy woman who was diagnosed with primary epiploic appendagitis based on CT scan findings conducted initially for suspected appendicitis. The patient received successful conservative treatment. This paper seeks to highlight the importance of recognizing this clinical condition and its characteristic imaging features, aiming to prevent unnecessary hospitalizations, antibiotic treatments, and the associated morbidity and mortality linked with surgical interventions.
Keywords: Abdominal computed tomography scan, Abdominal pain, Epiploic appendagitis, Appendicitis
Introduction
Epiploic appendagitis, a rare clinical condition resulting from torsion and inflammation of an epiploic appendix, manifests as localized abdominal pain. Typically, it follows a smooth clinical course post-diagnosis. However, the vague presentation often poses challenges in identification. Primary epiploic appendagitis is frequently mistaken for appendicitis, especially in patients with localized right lower abdominal pain. Radiological studies, particularly enhanced abdominal computed tomography (CT) scans, play a crucial role in accurate diagnosis, preventing unnecessary hospitalization or surgery in uncomplicated cases [1]. Despite this, primary epiploic appendagitis remains infrequent and can be overlooked even after imaging studies [2]. We present the case of a 37-year-old healthy woman diagnosed with primary epiploic appendagitis based on CT findings initially performed for suspected appendicitis. Successful management with conservative treatment was achieved. This paper underscores the importance of recognizing this condition and its distinct imaging features to avoid costly hospital stays, unnecessary antibiotic usage, and the associated risks of surgical interventions.
Case report
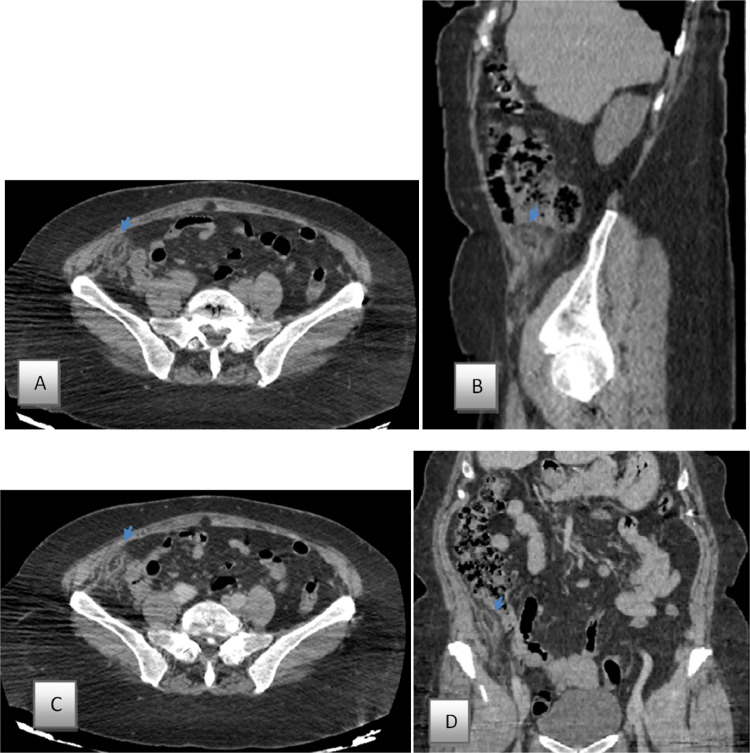
A 37-year-old woman arrived at the emergency department with complaints of sharp pain in the lower right abdomen that had been ongoing for a day. The pain started suddenly, remained constant, and intensified over time. She also experienced loss of appetite and nausea. There were no signs of fever, vomiting, diarrhea, constipation, or urinary issues. The patient had no previous medical or surgical conditions and had never experienced appendicitis or diverticulitis. Upon examination, she appeared generally healthy, with normal vital signs and a body mass index (BMI) of 34 kg/m2. An abdominal examination disclosed a soft, nondistended abdomen, with normal bowel sounds and deep tenderness at the Mc Burney point. Rebound tenderness in the right iliac fossa, Rovsing's sign, psoas sign, and obturator sign were all negative. The blood counts were unremarkable except for leukocytosis at 12,300 cells/µL (Normal value: 6000- 10,000cells/ µL) with predominance of neutrophils (82%). The patient was referred to the radiology department under suspicion of appendicitis. Contrast-enhanced computed tomography (CT) imaging of the abdomen and pelvis delineated a fat-density ovoid structure adjacent to the caecum, measuring 2.6 × 1.3 cm in diameter, exhibiting a thin high-density rim (1–3 mm thick). This was concomitant with perilesional inflammatory fat stranding and thickening of the adjacent peritoneum. Notably, a central hyperdense dot, suggestive of a thrombosed vascular pedicle, was discerned (refer to Fig. 1). Importantly, the appendix displayed normal morphology, while the remainder of the examination yielded unremarkable findings.
Fig. 1.
Computer tomography scan without (A: Axial section, B: sagital section), and with IV-contrast image (A: Axial section, B: coronal section), of the abdomen showing fat-density ovoid structure adjacent to the caecum (Bleu arrow), measuring 2.6 × 1.3 cm in diameter with thin high-density rim (1–3 mm thick) associated with surrounding inflammatory fat stranding, and thickening of the adjacent peritoneum. Presence of central hyperdense dot representing the thrombosed vascular pedicle.
Subsequent to admission to the surgical ward, the patient was initiated on a liquid dietary regimen, along with administration of a nonsteroidal anti-inflammatory agent and an antibiotic. Observation ensued over a brief duration, culminating in the patient's discharge in a favorable clinical state. Follow-up in the outpatient setting revealed an uneventful recovery trajectory.
Discussion
Originally documented by Vesalius in 1543, Epiploic appendages represent small, fat-filled pouches covered with serosa, typically measuring 1-2 cm in thickness and 0.5-5.0 cm in length, located on the external surface of the colon. While their precise physiological function remains elusive, it is postulated that they serve as protective cushions during peristalsis or act as a defensive mechanism against local inflammation, akin to the role played by the greater omentum [2]. This phenomenon can manifest at any age but predominantly manifests during the fourth to fifth decades of life, exhibiting a marginal male predominance [1,3]. Notably, its incidence is elevated in obese individuals, those with hernias, and individuals engaged in strenuous physical activity [4].
Appendicitis stands as the predominant cause of acute right lower quadrant pain. Clinically, epiploic appendagitis often mirrors appendicitis and can manifest as either primary or secondary in nature. Initially documented by Dockerty et al. in 1956 [5], primary epiploic appendagitis is distinguished by inflammation of the epiploic appendage triggered by torsion, potentially leading to vascular ischemia or thrombosis of the draining vein [1,6]. Conversely, secondary epiploic appendagitis tends to be more prevalent among individuals with concomitant conditions such as diverticulitis, appendicitis, cholecystitis, pancreatitis, or other inflammatory disorders affecting the abdomen or pelvis [7,8].
Primary epiploic appendagitis, often resembling acute appendicitis, may present with a diverse array of initial clinical manifestations. Predominantly, patients report acute pain localized to the right iliac fossa, characterized as dull, persistent, and unresponsive to physical maneuvers. Additional symptoms encompass postprandial fullness and premature satiety, while constitutional symptoms such as fever, nausea, vomiting, diarrhea, and constipation are infrequently encountered. Upon clinical examination, localized tenderness is commonly elicited, occasionally accompanied by rebound tenderness. Routine laboratory investigations, inclusive of lipase, pancreatic amylase, liver transaminases, inflammatory markers, and urinalysis, typically yield results within normal limits. Nonetheless, subtle elevations in C-reactive protein (CRP) and moderate leukocytosis may sporadically manifest [8].
Given the nonspecific presentation and the lack of distinctive clinical features, the diagnosis primary epiploic appendagitis without imaging is challenging. In the past, epiploic appendagitis was mainly diagnosed surgically, but developments in radiological techniques allowed Danielson et al. to describe the condition on a CT scan for the first time in 1986 [9].
Abdominal CT scanning stands as the current gold standard for diagnosing primary epiploic appendagitis. This diagnostic modality relies on 5 distinct imaging criteria, irrespective of the localization of the condition. These criteria include an oval mass, typically measuring between 1 and 3.5 cm in diameter, exhibiting fat attenuation. Additionally, the presence of a hyperdense ring sign encircling the oval mass signifies inflammation of the visceral peritoneum. Another characteristic, the central dot sign, denotes the presence of a hyperdense dot at the center of the mass, indicative of thrombosed veins. Moreover, the fat stranding sign highlights severe inflammation of the mesentery in contrast to minimal asymmetric thickening of the adjacent bowel wall. Finally, thickening of the parietal peritoneum, attributed to the attachment of the inflamed epiploic appendage, is observed. The identification of fat stranding suggests that the primary site of inflammation involves the epiploic appendage rather than the intestinal wall [8].
In pediatric and obstetric populations, ultrasound and magnetic resonance imaging (MRI) are frequently employed modalities for assessing acute abdominal pain. On MRI, discernible features encompass an ovoid mass exhibiting high signal intensity in both T1 and T2 weighted images, while rim enhancement becomes evident in gadolinium-enhanced T1 images [8]. Conversely, abdominal ultrasonography reveals a hyperechoic ovoid mass, non-compressible in nature, enveloped by a subtle hypoechoic rim. This mass is positioned adjacent to the gut wall, with the surrounding fat displaying hyperechoic characteristics due to inflammation. Notably, ultrasound can delineate the inflamed epiploic appendage extending towards the anterior abdominal wall. A distinctive feature discernible on Doppler imaging is the absence of blood flow within the mass, while augmented blood flow may be apparent in the adjacent inflamed fat. Nonetheless, it's noteworthy to acknowledge that primary epiploic appendagitis may not invariably manifest on abdominal ultrasonography, an examination heavily reliant on operator proficiency [8].
The most frequently affected locations, in descending order of prevalence, include the rectosigmoid junction (57%), ileocaecal region (26%), ascending colon (9%), transverse colon (6%), and descending colon (2%). Recent radiological literature assessing the CT presentation of epiploic appendagitis has indicated a lack of occurrence in the caecum. Furthermore, conventional anatomy and surgical pathology references suggest that either epiploic appendages are sparse and rudimentary in the caecum or are altogether absent [[10], [11], [12]]. Notably, in our patient, a CT scan revealed the presence of the mass adjacent to the caecum.
When contemplating the differential diagnosis, below are some essential aspects. 1) Acute Appendicitis: Epiploic appendagitis might be mistaken for acute appendicitis, especially if it develops on the right. The CT image of epiploic appendagitis (fat-density ovoid shape with a hyperattenuating rim) is distinguishing, as is the lack of considerable intestinal wall thickening. 2) Diverticulitis: Clinically, epiploic appendagitis might be mistaken for diverticulitis. Imaging findings contribute in differentiation: epiploic appendagitis appears as a confined, non-compressible, hyperechoic mass on ultrasound or a fat-density ovoid shape on CT, whereas diverticulitis is characterized by colonic outpouchings with surrounding inflammatory alterations. Acute omental infarction, sclerosing mesenteritis, and a tumor or metastasis to the mesocolon are potential diagnoses. For females, it is crucial to consider ovarian torsion, ovarian cyst rupture, and ectopic pregnancy.
The therapeutic approach to epiploic appendagitis remains a subject of contention; however, the prevailing consensus in the literature advocates for conservative management involving antibiotic therapy and analgesics when the condition is identified prior to surgical intervention. In cases where surgery is not pursued, symptoms typically abate completely within a week, with an average resolution time of 4.7 days. However, the radiological findings on CT imaging may take approximately six months to resolve [13]. In instances where intraoperative diagnosis is made, the optimal course of action involves excising the affected appendage and performing seromuscular inversion of the involved segment of the intestine. Laparoscopy serves as both a therapeutic and diagnostic tool in managing this condition [13]. Surgical intervention becomes necessary for patients who exhibit inadequate response to conservative treatment or develop complications such as obstruction, intussusception, or abscess formation [14].
Conclusion
Our objective was to enhance clinicians' awareness regarding the less frequent origin of localized lower abdominal pain attributable to cecal epiploic appendagitis on the right side, which can closely resemble the clinical manifestations of more prevalent causes of acute abdominal conditions, notably acute appendicitis, thereby presenting a diagnostic challenge. General surgeons should remain vigilant in considering this self-resolving condition as a potential differential diagnosis in cases of acute abdominal presentations. Furthermore, we sought to underscore the significance of employing CT scanning to discern ambiguous clinical presentations, ultimately averting unwarranted surgical interventions and hospital admissions.
Patient consent
Written informed consent for publication was obtained from patient.
Author's contributions
All authors contributed to this work. All authors have read and approved the final version of the manuscript.
Footnotes
Guarantor of submission: The corresponding author is the guarantor of submission.
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Almuhanna AF, Alghamdi ZM, Alshammari E. Acute epiploic appendagitis: a rare cause of acute abdomen and a diagnostic dilemma. J Family Community Med. 2016;23(1):48–50. doi: 10.4103/2230-8229.172234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hwang JA, Kim SM, Song HJ, Lee YM, Moon KM, Moon CG, et al. Differential diagnosis of left-sided abdominal pain: primary epiploic appendagitis vs colonic diverticulitis. World J Gastroenterol. 2013;19(40):6842–6848. doi: 10.3748/wjg.v19.i40.6842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chu EA, Kaminer E. Epiploic appendagitis: a rare cause of acute abdomen. Radiol Case Rep. 2018;13(3):599–601. doi: 10.1016/j.radcr.2018.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaur S, Jawahar RP, Prasad R, Prabakaran M. Epiploic appendagitis-a rare cause of acute lower abdominal pain. Radiol Case Rep. 2021;16(5):1144–1147. doi: 10.1016/j.radcr.2021.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dockerty MB, Lynn TE, Waugh JM. A clinicopathologic study of the epiploic appendages. Surg Gynecol Obstet. 1956;103(4):423–433. [PubMed] [Google Scholar]
- 6.Boardman J, Kaplan KJ, Hollcraft C, Bui-Mansfield LT. Radiologic-pathologic conference of Keller Army Community Hospital at West Point, the United States Military Academy: torsion of the epiploic appendage. AJR Am J Roentgenol. 2003;180:748. doi: 10.2214/ajr.180.3.1800748. [DOI] [PubMed] [Google Scholar]
- 7.Jalaguier A, Zins M, Rodallec M, Nakache JP, Boulay-Coletta I, Jullès MC. Accuracy of multidetector computed tomography in differentiating primary epiploic appendagitis from left acute colonic diverticulitis associated with secondary epiploic appendagitis. Emerg Radiol. 2010;17:51–56. doi: 10.1007/s10140-009-0822-x. [DOI] [PubMed] [Google Scholar]
- 8.Kefala MA, Tepelenis K, Stefanou CK, Stefanou SK, Papathanakos G, Kitsouli A, et al. Primary epiploic appendagitis mimicking acute appendicitis: a case report and narrative review of the literature. Korean J Gastroenterol. 2020;76(2):88–93. doi: 10.4166/kjg.2020.76.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Danielson K, Chernin MM, Amberg JR, Goff S, Durham JR. Epiploic appendicitis: CT characteristics. J Comput Assist Tomogr. 1986;10:142–143. doi: 10.1097/00004728-198601000-00032. [DOI] [PubMed] [Google Scholar]
- 10.Macari M, Laks S, Hajdu C, Babb J. Caecal epiploic appendagitis: an unlikely occurrence. Clin Radiol. 2008;63(8):895–900. doi: 10.1016/j.crad.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 11.Singh A.K., Gervais D.A., Hahn P.F., Rhea J., Mueller P.R. CT appearance of acute appendagitis. AJR Am J Roentgenol. 2004;183(5):1303–1307. doi: 10.2214/ajr.183.5.1831303. [DOI] [PubMed] [Google Scholar]
- 12.Ng K.S., Tan A.G.S., Chen K.K.O.W., Wong S.K., Tan H.M. CT features of primary epiploic appendagitis. Eur J Radiol. 2006;59(2):284–288. doi: 10.1016/j.ejrad.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 13.Rashid A, Nazir S, Hakim SY, Chalkoo MA. Epiploic appendagitis of caecum: a diagnostic dilemma. Ger Med Sci. 2012;10:Doc14. doi: 10.3205/000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan E, El-Banna A. A case report of epiploic appendagitis as a mimic of acute cholecystitis. Int J Surg Case Rep. 2018;53:327–329. doi: 10.1016/j.ijscr.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]