Abstract
Aims
To examine trends and recent changes in non-fatal and fatal stimulant overdose rates with and without opioids to improve the descriptive characterization of the US overdose epidemic.
Design
Secondaryanalysis of non-fatal (2006–16) and fatal (2006–17) drug overdose trends, focusing on the most recent years of data available to examine rate changes by demographics (2015–16 for non-fatal and 2016–17 for fatal).
Setting
Non-fatal drug overdoses from the Healthcare Cost and Utilization Project’s Nationwide Emergency Department Sample; drug overdose deaths from the National Vital Statistics System.
Participants/cases
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and Tenth Revision, Clinical Modification/Procedure Coding System (ICD-10-CM/PCS) codes for cocaine, psychostimulants and opioids were used to classify non-fatal drug overdoses. Drug overdose deaths were identified using ICD-10 multiple cause-of-death codes for cocaine, psychostimulants, all opioids, heroin and synthetic opioids.
Measurements
Percentage of changes in age-adjusted non-fatal and fatal rates of cocaine and psychostimulant-involved drug overdose with and without opioids.
Findings
Overall, cocaine-involved non-fatal overdose rates with an opioid increased from 2006 to 2016 [annual percentage change (APC) = 14.7], while rates without an opioid increased from 2006 to 2012 (APC = 11.3) and then remained stable (APC = −7.5). Psychostimulant-involved non-fatal rates with and without an opioid increased from 2006 to 2016 (APC = 49.9 with opioids; 13.9 without opioids). Cocaine-involved death rates with and without opioids increased from 2014 to 2017 (APC = 46.0 with opioids, 23.6 without opioids). Psychostimulant-involved death rates with opioids increased from 2010 to 2015 (APC = 28.6), with a dramatic increase from 2015 to 2017 (APC = 50.5), while rates without opioids increased from 2008 to 2017 (APC = 22.6). In 2016, 27% of non-fatal cocaine- and 14% of psychostimulant-involved overdoses included a reported opioid; 72.7% of cocaine- and 50.3% of psychostimulant-involved deaths involved an opioid in 2017. From 2015 to 2016, cocaine-involved and psychostimulant-involved non-fatal overdose rates with an opioid increased 17.0 and 5.9%, respectively; cocaine-involved and psychostimulant-involved non-fatal overdoses without opioids decreased 13.6 and increased 18.9%, respectively. Death rates involving stimulants increased with and without opioids from 2016 to 2017 (cocaine with and without opioids = 37.7 and 23.3%; psychostimulants with and without opioids = 52.2 and 23.0%). Death rates involving stimulants with synthetic opioids increased dramatically from 2016 to 2017 (1.3–2.3 per 100000 for cocaine and 0.3–0.8 for psychostimulants).
Conclusions
While increases in cocaine-involved deaths in the United States from 2006 seem to be driven by opioids, particularly synthetic opioids, increases in non-fatal and fatal overdoses involving psychostimulants are occurring with and without opioids.
Keywords: Cocaine, emergency department, Opioids, overdose, stimulants, United States
INTRODUCTION
The drug overdose epidemic in the United States continues to worsen. In 2017, there were 70237 drug overdose deaths and more than two-thirds involved an opioid [1]. Fatal overdoses involving stimulants (cocaine and other psychostimulants, primarily methamphetamine) have been increasing during the past few years. From 2016 to 2017, deaths involving cocaine and psychostimulants increased 34.4 and 33.3%, respectively [1].
Studies have documented that rising cocaine- and psychostimulant-involved overdose deaths increasingly involve opioids, particularly synthetic opioids [2–4]. Among cocaine-involved deaths in the United States, synthetic opioid involvement increased from 4% in 2010 to 40% in 2016 [5]. Death rates involving psychostimulants and synthetic opioids increased 142.8% annually from 2015 to 2017 [2]. While some people using drugs intentionally mix cocaine and heroin (i.e. ‘speedball’) or methamphetamine and heroin (i.e. ‘goofball’) for a stronger high or to balance the effects of either drug, studies have suggested that illicitly manufactured fentanyl (IMF) has potentially been contaminating the illicit stimulant supply [4–7]. Compared to 2015, 2016 data from the National Forensic Laboratory Information System (NFLIS) indicated a 297% increase in drug submissions (i.e. drug products obtained by law enforcement) containing mixtures of cocaine and IMF and a 134% increase in submissions containing cocaine, fentanyl and heroin [8]. Similarly, NFLIS has documented increases in methamphetamine mixed with IMF, heroin and other fentanyl-like substances [8]. From 2015 to 2016, significant increases in overdose death rates involving cocaine, heroin and synthetic opioids other than methadone (referred to as synthetic opioids) occurred primarily in the eastern part of the country, while the highest rates of and greatest increases in psychostimulant-involved death rates occurred in midwestern and western states [9].
While it is clear that fatal stimulant-involved overdoses are increasing and that synthetic opioids are driving some of theseincreases, it is less clear whether opioids are having the same impact on non-fatal stimulant-involved drug overdoses. Gaps also remain in quantifying recent increases in fatal cocaine and psychostimulant drug overdoses with and without opioids by decedent demographics and geography. To address these gaps, and to inform overdose prevention and response efforts, we described rate changes and trends of non-fatal and fatal overdoses involving stimulants with and without opioids.
METHODS
Data sources and study population
Data on non-fatal drug overdoses for 2006–16 were obtained from the Healthcare Cost and Utilization Project’s Nationwide Emergency Department Sample (NEDS) [10]. NEDS is an annual stratified sample of billing records that is weighted to produce nationally representative estimates of non-federal, hospital-based emergency department (ED) visits in the United States. Discharge data from ED visits in NEDS are collected annually from over 950 hospitals in 24–36 states and Washington, DC.
Data on drug overdose deaths for 2006–17 were obtained from National Vital Statistics System mortality files (https://www.cdc.gov/nchs/nvss/deaths.htm), with counts and rates tabulated using the CDC WONDER multiple cause-of-death query system (https://wonder.cdc.gov/mcd.html ). Data are based on death certificates for all US residents.
Identifying emergency department visits and overdose deaths with and without opioids
NEDS transitioned from using International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) diagnosis codes to International Classification of Diseases, 10th revision, Clinical Modification/Procedure Coding System (ICD-10-CM/PCS) on 1 October 2015. For non-fatal drug overdoses, ICD-9-CM codes were used to classify drug overdoses for 2006–14 and the first three quarters of 2015. These included codes for cocaine, amphetamine, other psychostimulants and opioids (Supporting information, Table S1). ICD-10-CM/PCS codes were used for the fourth quarters of 2015 and 2016. All intents (unintentional, suicide, assault and undetermined), diagnoses (not just principal) and encounters (initial, subsequent and sequelae) were included. Codes for adverse effects and underdosing were excluded. Amphetamine and other psychostimulant codes were combined to create one variable for psychostimulants to ensure consistency with fatal overdose codes that only designate psychostimulant and donot differentiate amphetamines. Visits where the patient died were excluded.
Drug overdose deaths were identified based on ICD-10 underlying cause-of-death codes X40–X44 (unintentional), X60–X64 (suicide), X85 (homicide) or Y10–Y14 (undetermined intent). Among deaths with drug overdose as the underlying cause, the type of drug is indicated by ICD-10 multiple cause-of-death codes for cocaine, psychostimulants with abuse potential and opioids (Supporting information, Table S1). To obtain counts involving cocaine and psychostimulants with opioids, we calculated deaths with the respective stimulant ICD-10 code with any opioid code. To obtain counts involving cocaine without opioids, we first calculated deaths with a cocaine ICD-10 code. We then subtracted deaths with cocaine and opioid involvement from all deaths involving cocaine. This process was repeated for psychostimulants without opioids. We also recorded deaths with a cocaine ICD-10 code and a code for synthetic opioids other than methadone (synthetic opioids [11]) and deaths with a cocaine ICD-10 code and a code for heroin. This process was repeated for psychostimulants.
Statistical analysis
Results were reported as ED visit and death counts, age-adjusted rates and standard errors. All age-adjusted ED rates from 2006 to 2016 and death rates from 2006 to 2017 per 100000 population were examined for cocaine with opioids, cocaine without opioids, psychostimulants with opioids and psychostimulants without opioids. Age-adjusted ED visit and death rates were calculated by applying age-specific rates to the 2000 US Census standard population. Age-adjusted overdose rates from 2015 to 2016 (ED) and 2016 to 2017 (death) were stratified by sex, age group (crude rates presented), US census region and urbanization level. Urbanization level was based on the 2013 National Center for Health Statistics Urban–Rural Classification Scheme for Counties (https://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf). Age-adjusted overdose death rates from 2016 to 2017 were also calculated for cocaine with synthetic opioids, cocaine with heroin, psychostimulants with synthetic opioids and psychostimulants with heroin, and stratified by the above variables. ED rates for these categories were not calculated, as ICD-9-CM/ICD-10-CM do not clearly code for synthetic opioids.
Non-fatal drug overdoses were analyzed in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) using SAS survey procedures (PROC SURVEYFREQ) to account for the NEDS sampling design. WONDER provides age-adjusted rates and standard errors for specific drug overdose deaths (e.g. any cocaine) and combinations of drugs (e.g. cocaine with any opioids), but does not provide age-adjusted rates and standard errors for queries assessing one drug without another (e.g. cocaine without any opioids); these were calculated outside WONDER.
Regression models were run using JoinPoint (https://surveillance.cancer.gov/joinpoint/) default criteria to examine trends from 2006 to 2016 for non-fatal overdoses and from 2006 to 2017 for fatal overdoses by calculating annual percentage change (APC) and 95% confidence intervals (CIs). Absolute rate change and percentage change were calculated for the two most recent years of data (i.e. 2015–16for non-fatal and 2016–17forfatal). Z-tests were used to determine statistical significance (P < 0.05). Statistically significant results are presented. These findings did not derive from pre-registered analyses and the analyses should be considered exploratory.
RESULTS
ED visits involving cocaine with and without opioids, 2015–16
In 2016, 26.7% of ED visits involving cocaine also involved a reported opioid. From 2015 to 2016, the rate of cocaine overdose ED visits with an opioid increased 17.0%, from 2.1 to 2.4 per 100000 (Table 1). Rates also increased among both sexes, many age groups, in all regions except the Midwest, and in large fringe (30.2%) and small metro counties (44.7%). The highest absolute rate change was in the Northeast and among those aged 35–44 years (0.8 in both).
Table 1.
Number and age-adjusted ratesa of cocaine and psychostimulant overdose emergency department visits with and without opioids, by sex, age, Census region and level of urbanization—United States, 2015 and 2016.
| Cocaine and any opioidb | Cocaine without any opioidsc | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| 2015 | 2016 | 2015 | 2016 | |||||||||
|
|
|
|
|
|||||||||
| ED visit characteristic | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate |
|
| ||||||||||||
| All | 6548 | 2.1 (0.03) | 7571 | 2.4(0.03) | 0.3 | 17.0 | 22 165 | 6.9 (0.05) | 19 131 | 5.9 (0.04) | −1.0 | −13.6 |
| Sex | ||||||||||||
| Male | 3960 | 2.6 (0.04) | 4824 | 3.1 (0.05) | 0.5 | 21.3 | 14 767 | 9.3 (0.08) | 13 306 | 8.3 (0.07) | −1.0 | −10.3 |
| Female | 2589 | 1.6 (0.03) | 2746 | 1.7(0.03) | 0.1 | 6.5 | 7399 | 4.6 (0.05) | 5820 | 3.6 (0.05) | −1.0 | −21.4 |
| Age group (years) | ||||||||||||
| 0–14 | 12 | f | f | f | - | - | 627 | 1.0 (0.04) | 125 | 0.2 (0.02) | −0.8 | −80.0 |
| 15–19 | 135 | 0.6 (0.06) | 144 | 0.7(0.06) | 0.1 | 6.8 | 564 | 2.6 (0.11) | 528 | 2.5 (0.11) | −0.1 | −5.2 |
| 19–24 | 829 | 3.6 (0.13) | 961 | 4.3 (0.14) | 0.7 | 17.8 | 1554 | 6.9 (0.17) | 1542 | 7.0 (0.18) | 0.1 | −0.1 |
| 25–34 | 2298 | 5.2 (0.11) | 2554 | 5.8(0.11) | 0.6 | 9.8 | 4032 | 9.2 (0.14) | 3988 | 9.0 (0.14) | −0.2 | −2.8 |
| 35–44 | 1355 | 3.3 (0.09) | 1652 | 4.1 (0.10) | 0.8 | 22.3 | 4334 | 10.6 (0.16) | 3612 | 9.0(0.15) | −1.6 | −16.0 |
| 45–54 | 1170 | 2.7 (0.08) | 1370 | 3.2 (0.09) | 0.5 | 18.2 | 6171 | 14.3 (0.18) | 5345 | 12.5 (0.18) | −1.8 | −12.7 |
| 55–64 | 665 | 1.6 (0.06) | 775 | 1.9 (0.07) | 0.3 | 15.0 | 3867 | 9.5 (0.15) | 3302 | 8.0 (0.14) | −1.5 | −15.8 |
| ≥65 | 84 | 0.2 (0.02) | 110 | 0.2 (0.02) | 0.0 | 27.3 | 1014 | 2.1 (0.07) | 689 | 1.4(0.05) | −0.7 | −34.1 |
| Census region | ||||||||||||
| Northeast | 192 5 | 3.5 (0.08) | 2321 | 4.3 (0.09) | 0.8 | 20.3 | 6037 | 10.6 (0.14) | 4401 | 7.9 (0.12) | −2.7 | −25.8 |
| Midwest | 1750 | 2.6 (0.06) | 1625 | 2.5 (0.06) | −0.1 | −6.0 | 4325 | 6.4 (0.10) | 3402 | 5.0(0.09) | −1.4 | −22.1 |
| South | 2478 | 2.2 (0.04) | 3132 | 2.7(0.05) | 0.5 | 23.4 | 9827 | 8.3 (0.09) | 9132 | 7.5 (0.08) | −0.8 | −8.9 |
| West | 395 | 0.5 (0.03) | 492 | 0.6 (0.03) | 0.1 | 23.6 | 1976 | 2.6 (0.06) | 2196 | 2.8 (0.06) | 0.2 | 9.3 |
| Comity urbanization level | ||||||||||||
| Large central metro | 2125 | 2.1 (0.05) | 2242 | 2.2 (0.05) | 0.1 | 3.5 | 10 593 | 10.2 (0.10) | 7487 | 7.2 (0.08) | −3.0 | −30.0 |
| Large fringe metro | 1628 | 2.2 (0.05) | 2120 | 2.8 (0.06) | 0.6 | 30.2 | 3570 | 4.7 (0.08) | 3853 | 4.9 (0.08) | 0.2 | 4.8 |
| Medium metro | 1706 | 2.7 (0.07) | 1946 | 3.0(0.07) | 0.3 | 14.0 | 4213 | 6.4 (0.10) | 4361 | 6.5 (0.10) | 0.1 | 14.0 |
| Small metro | 346 | 1.2 (0.07) | 494 | 1.8 (0.08) | 0.6 | 44.7 | 1294 | 4.6 (0.13) | 1357 | 4.8 (0.13) | 0.2 | 4.8 |
| Micropolitan (non-metro) | 422 | 1.6 (0.08) | 392 | 1.5 (0.08) | −0.1 | −6.9 | 1321 | 5.0 (0.14) | 1006 | 3.9 (0.12) | −1.1 | −23.4 |
| Non-core (non-metro) | 210 | 1.1 (0.08) | 172 | 0.9 (0.08) | −0.2 | −17.2 | 800 | 4.3 (0.16) | 489 | 2.7 (0.13) | −1.6 | −36.6 |
| Psychostimulant and any opioiifd | Psychostimulant without any opioiife | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| 2015 | 2016 | 2015 | 2016 | |||||||||
|
|
|
|
|
|||||||||
| ED visit characteristic | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate |
|
| ||||||||||||
| All | 5719 | 1.8 (0.03) | 6019 | 1.9 (0.03) | 0.1 | 5.9 | 30 218 | 9.9 (0.06) | 36 048 | 11.8 (0.06) | 1.9 | 18.9 |
| Sex | ||||||||||||
| Male | 3268 | 2.1 (0.04) | 3613 | 2.4 (0.04) | 0.3 | 12.2 | 18 064 | 12.1 (0.09) | 22 180 | 14.8 (0.10) | 2.7 | 22.5 |
| Female | 2450 | 1.6 (0.03) | 2406 | 1.5 (0.03) | −0.1 | −0.6 | 12 155 | 7.9 (0.07) | 13 868 | 9.0 (0.08) | 1.1 | 13.7 |
| Age group (years) | ||||||||||||
| 0–14 | 35 | 0.1 (0.01) | 30 | 0.1 (0.01) | 0.0 | −13.1 | 3810 | 6.2 (0.10) | 4193 | 6.9 (0.11) | 0.7 | 10.1 |
| 15–19 | 219 | 1.0(0.07) | 211 | 1.0 (0.7) | 0.0 | −3.6 | 3712 | 17.3 (0.28) | 4072 | 18.9 (0.30) | 1.6 | 9.4 |
| 19–24 | 855 | 3.8 (0.13) | 757 | 3.4 (0.12) | −0.4 | −10.1 | 4184 | 18.6 (0.29) | 4523 | 20.4 (0.30) | 1.8 | 9.9 |
| 25–34 | 2106 | 4.8(0.11) | 2210 | 4.9 (0.11) | 0.1 | 3.7 | 8050 | 18.3 (0.20) | 9812 | 22.1 (0.22) | 3.8 | 20.5 |
| 35–44 | 1150 | 2.8 (0.08) | 1339 | 3.3 (0.09) | 0.5 | 16.8 | 5284 | 12.9 (0.18) | 6428 | 15.8 (0.20) | 2.9 | 22.1 |
| 45–54 | 740 | 1.7(0.06) | 862 | 2.0 (0.07) | 0.3 | 17.6 | 3184 | 7.4 (0.13) | 4308 | 10.1 (0.15) | 2.7 | 36.5 |
| 55–64 | 477 | 1.2 (0.05) | 458 | 1.1 (0.05) | −0.1 | −5.4 | 1562 | 3.8 (0.10) | 2095 | 5.1 (0.11) | 1.3 | 32.2 |
| ≥65 | 136 | 0.3 (0.02) | 151 | 1.3 (0.02) | 1.0 | 7.7 | 432 | 0.9 (0.04) | 617 | 1.3 (0.05) | 0.4 | 38.5 |
| Census region | ||||||||||||
| Northeast | 382 | 0.7 (0.04) | 338 | 0.7 (0.04) | 0.0 | −9.7 | 2801 | 5.2 (0.10) | 3092 | 5.9 (0.11) | 0.7 | 11.8 |
| Midwest | 1288 | 2.0 (0.06) | 1321 | 2.1 (0.06) | 0.1 | 3.2 | 7285 | 11.5 (0.14) | 8216 | 13.0(0.15) | 1.5 | 12.6 |
| South | 2159 | 1.9 (0.04) | 2277 | 2.0 (0.04) | 0.1 | 4.0 | 10 766 | 9.6 (0.09) | 12 406 | 10.7 (0.10) | 1.1 | 11.6 |
| West | 1890 | 2.6 (0.06) | 2084 | 2.8 (0.06) | 0.2 | 8.3 | 9366 | 12.9 (0.14) | 12 334 | 16.6 (0.15) | 3.7 | 28.9 |
| Comity urbanization level | ||||||||||||
| Large central metro | 1432 | 1.5 (0.04) | 1535 | 1.5 (0.04) | 0.0 | 4.0 | 8571 | 9.1 (0.10) | 10430 | 10.7(0.11) | 1.6 | 17.2 |
| Large fringe metro | 960 | 1.3 (0.04) | 914 | 1.2 (0.04) | −0.1 | −5.5 | 5201 | 7.0(0.10) | 5633 | 7.5 (0.10) | 0.5 | 7.9 |
| Medium metro | 1472 | 2.3 (0.06) | 1467 | 2.3 (0.06) | 0.0 | −0.4 | 7218 | 12.1 (0.15) | 7531 | 11.8 (0.14) | −0.3 | −2.5 |
| Small metro | 692 | 2.4 (0.09) | 704 | 2.5 (0.09) | 0.1 | 1.4 | 3253 | 11.7(0.21) | 4393 | 15.9 (0.24) | 4.2 | 35.4 |
| Micropolitan (non-metro) | 629 | 2.5 (0.10) | 670 | 2.6 (0.10) | 0.1 | 6.7 | 3113 | 12.3 (0.22) | 4091 | 16.4 (0.26) | 4.1 | 33.0 |
| Non-core (non-metro) | 874 | 5.0(0.17) | 561 | 3.2 (0.14) | −1.8 | −35.7 | 2203 | 12.7(0.27) | 2985 | 17.4 (0.32) | 4.7 | 37.4 |
Source: Nationwide Emergency Department Sample. Bold type indicates statistical significance (P ≤ 0.05) determined by Z-test.
Age-adjusted emergency department visit rates were calculated by applying age-specific emergency department visit rates to the 2000 US standard population age distribution. All rates are per 100 000 population. People who died were excluded, as were visits with missing age and gender.
For the first three-quarters of 2015, includes ICD-9-CMprincipal diagnosis code 970.81 or external cause of injury codes E854.3 or E855.2 and principal diagnosis codes 965.00, 965.01 or 965.02 or external cause of injury codes E850.0, E850.1 or E850.2; for the fourth quarter of 2015 and 2016, includes ICD-10-CM/PCS contributing causes T40.5 and T40.0, T40.1, T40.2, T40.3, T40.6 or T40.69.
For the first three-quarters of 2015, includes ICD-9-CM principal diagnosis code 970.81 or external cause of injury codes E854.3 or E855.2 and not principal diagnosis codes 965.00, 965.01 or 965.02 or external cause of injury codes E850.0, E850.1 or E850.2; for the fourth quarter of 2015 and 2016, includes ICD-10-CM/PCS contributing cause T40.5 and not T40.0, T40.1, T40.2, T40.3, T40.6 or T40.69.
For the first three-quarters of 2015, includes ICD-9-CM principal diagnosis codes 969.70, 969.71, 969.72, 969.73 or 969.79 or external cause of injury code E854.2 and principal diagnosis codes 965.00, 965.01 or 965.02 or external cause of injury codes E850.0, E850.1 or E850.2; for the fourth quarter of 2015 and 2016, includes ICD-10-CM/PCS contributing causes T43.60, T43.61, T43.62, T43.63 and T43.69 and T40.0, T40.1, T40.2, T40.3, T40.6 or T40.69.
For the first three-quarters of 2015, includes ICD-9-CM principal diagnosis codes 969.70, 969.71, 969.72, 969.73 or 969.79 or external cause of injury code E854.2 and not principal diagnosis codes 965.00, 965.01 or 965.02 or external cause of injury codes E850.0, E850.1 or E850.2; for the fourth quarter of 2015 and 2016, includes ICD-10-CM/PCS contributing causes T43.60, T43.61, T43.62, T43.63 and T43.69 and NOT T40.0, T40.1, T40.2, T40.3, T40.6 or T40.69.
Emergency department visits ≤ 10 are not reported. Rates based on < 20 emergency department visits are not considered reliable and not reported. ED = emergency department; SE = standard error.
The rate of cocaine overdose ED visits without opioids decreased 13.6% from 2015 to 2016, from 6.9 to 5.9. Rates also decreased among both sexes, most age groups, all regions except the West and in large central metro (−30.0%) and non-metro counties [micropolitan (−23.4%) and non-core (−36.6%)]. Rates increased in large fringe metro (4.8%) and medium metro counties (14.0%). The West wasthe only region to experience an increase, although the absolute increase was small (0.2).
ED visits involving psychostimulants with and without opioids, 2015–16
In 2016, 14.3% of ED visits involving psychostimulants involved a reported opioid. From 2015 to 2016, the rate of psychostimulant overdose ED visits with an opioid increased 5.9%, from 1.8 to 1.9 per 100000 (Table 1). Rates increased among males (12.2%), people aged 35–44 (16.8%) and 45–54 years (17.6%) and in the West (8.3%), although absolute increases were small (0.2–0.5). Decreases were observed among those aged 19–24 years (−10.1%) and in non-core counties (−35.7%).
The rate of psychostimulant overdose ED visits without opioids increased 18.9% from 2015 to 2016, from 9.9 to 11.8. Rates increased among both sexes and all age groups, regions and urbanization levels except medium metro. The West experienced the largest absolute (3.7) and relative (28.9%) regional increases.
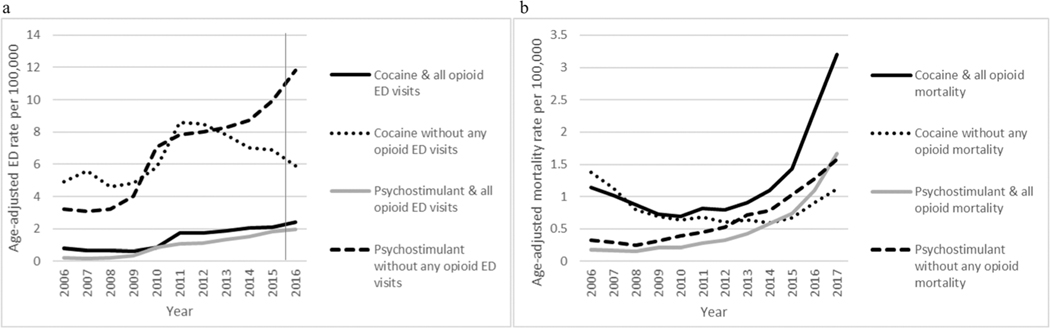
Trends in ED visits involving cocaine and psychostimulants with and without opioids, 2006–16
ED visit rates involving cocaine with an opioid increased from 2006 to 2016 (APC = 14.7, CI = 9.3, 20.4) (Fig. 1a), while rates involving cocaine without opioids increased from 2006 to 2012 (APC = 11.3, CI = 2.0, 21.5) and then remained stable from 2012 to 2016 (APC = −7.5, CI = −20.8, 7.9). ED visit rates involving psychostimulants with an opioid increased dramatically from 2006 to 2011 (APC = 49.9, CI = 21.6, 84.6), followed by a slower increase from 2011 to 2016 (14.0, CI = 3.0, 26.2). ED visit ratesinvolving psychostimulants without opioids increased from 2006 to 2016 (APC = 13.9, CI = 9.8, 18.1).
Figure 1.
Age-adjusted rate of cocaine and psychostimulant overdose emergency department visits and deaths with and without opioids, United States, 2006–17. Age-adjusted death and emergency department visit rates were calculated by applying age-specific death and emergency department visit rates to the 2000 US standard population age distribution. All rates are per 100 000 population. Cells with ≤ 9 deaths/emergency department visits are not reported. Rates based on < 20 deaths/emergency department visits were not considered reliable and are not reported. The vertical line between 2015 and 2016 on the graph of emergency department visit rates denotes the transition in the Nationwide Emergency Department Sample from using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes to International Classification of Diseases, 10th Revision, Clinical Modification/Procedure Coding System (ICD-10-CM/PCS) on 1 October 2015. Source: Nationwide Emergency Department Sample; National Vital Statistics System, Mortality file.
Deaths involving cocaine with and without opioids, 2016–17
In 2017, 72.7% of deaths involving cocaine involved at least one opioid. Death rates involving cocaine with an opioid increased 37.7% from 2016 to 2017, from 2.3 to 3.2 per 100000 (Table 2). Rates also increased among both sexes, all age groups except those aged 15–19 years (rates for 0–14 years were unstable due to small numbers and were not calculated), allregionsand all urbanization levels. Micropolitan areas experienced the largest relative increase (65.5%), while large fringe and medium metro areas experienced the largest absolute increases (1.0).
Table 2.
Number and age-adjusted rates of cocaine and psychostimulant overdose deathsa with and without opioids, by sex, age, Census region and level of urbanization—United States, 2016 and 2017.
| Cocaine and any opioidb | Cocaine without any opioidsc | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| 2016 | 2017 | 2016 | 2017 | |||||||||
|
|
|
|
|
|||||||||
| Decedent characteristic | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate |
|
| ||||||||||||
| All | 7263 | 2.3 (0.03) | 10 131 | 3.2 (0.03) | 0.9 | 37.7 | 3112 | 0.9 (0.02) | 3811 | 1.1 (0.02) | 0.2 | 23.3 |
| Sex | ||||||||||||
| Male | 5215 | 3.3 (0.05) | 7233 | 4.6 (0.05) | 1.3 | 37.9 | 2278 | 1.3 (0.03) | 2788 | 1.6 (0.03) | 0.3 | 21.4 |
| Female | 2048 | 1.3 (0.03) | 2898 | 1.8 (0.04) | 0.5 | 39.4 | 834 | 0.5 (0.02) | 1023 | 0.6 (0.02) | 0.1 | 27.9 |
| Age group (years) | ||||||||||||
| 0–14 | f | f | f | f | - | - | f | f | f | f | - | - |
| 15–19 | 73 | 0.3 (0.04) | 85 | 0.4 (0.04) | 0.1 | 16.4 | 14 | f | 26 | 0.1 (0.02) | - | - |
| 20–24 | 568 | 2.5 (0.11) | 707 | 3.2 (0.12) | 0.7 | 25.9 | 102 | 0.5 (0.05) | 106 | 0.5 (0.05) | 0 | 5.2 |
| 25–34 | 2121 | 4.7(0.10) | 2917 | 6.4(0.12) | 1.7 | 35.5 | 404 | 0.9 (0.04) | 546 | 1.2 (0.05) | 0.3 | 33.2 |
| 35–44 | 1890 | 4.7(0.10) | 2595 | 6.3 (0.12) | 1.6 | 35.9 | 541 | 1.3 (0.06) | 687 | 1.7(0.06) | 0.4 | 25.7 |
| 45–54 | 1642 | 3.8 (0.09) | 2360 | 5.6(0.11) | 1.8 | 45.1 | 987 | 2.3 (0.07) | 1137 | 2.7(0.08) | 0.4 | 16.3 |
| 55–64 | 865 | 2.1 (0.07) | 1291 | 3.1 (0.09) | 1.0 | 47.4 | 856 | 2.1 (0.07) | 1044 | 2.5 (0.08) | 0.4 | 20.4 |
| ≥65 | 103 | 0.2 (0.02) | 168 | 0.3 (0.3) | 0.1 | 61.1 | 202 | 0.4 (0.03) | 264 | 0.5 (0.03) | 0.1 | 26.5 |
| Census region | ||||||||||||
| Northeast | 2366 | 4.4 (0.09) | 3175 | 5.8 (0.11) | 1.4 | 33.9 | 591 | 1.0 (0.04) | 685 | 1.2 (0.05) | 0.2 | 14.7 |
| Midwest | 1971 | 3.1 (0.07) | 2847 | 4.4 (0.08) | 1.3 | 43.4 | 604 | 0.8 (0.04) | 864 | 1.2 (0.04) | 0.4 | 43.7 |
| South | 2468 | 2.1 (0.04) | 3539 | 3.0(0.05) | 0.9 | 40.7 | 1537 | 1.2 (0.03) | 1826 | 1.4(0.03) | 0.2 | 15.0 |
| West | 458 | 0.6 (0.03) | 570 | 0.7(0.03) | 0.1 | 24.5 | 380 | 0.4 (0.02) | 436 | 0.5 (0.03) | 0.1 | 17.0 |
| County urbanization level | ||||||||||||
| Large central metro | 2855 | 2.8 (0.05) | 3835 | 3.7(0.06) | 0.9 | 32.3 | 1446 | 1.3 (0.04) | 1678 | 1.5 (0.04) | 0.2 | 15.8 |
| Large fringe metro | 2131 | 2.8 (0.06) | 2933 | 3.8 (0.07) | 1.0 | 36.6 | 603 | 0.7 (0.03) | 768 | 0.9 (0.03) | 0.2 | 26.2 |
| Medium metro | 1414 | 2.3 (0.06) | 2064 | 3.3 (0.07) | 1.0 | 44.5 | 668 | 1.0 (0.04) | 881 | 1.2 (0.04) | 0.2 | 29.3 |
| Small metro | 396 | 1.5 (0.08) | 570 | 2.1 (0.09) | 0.6 | 44.2 | 173 | 0.6 (0.05) | 207 | 0.7(0.05) | 0.1 | 19.0 |
| Micropolitan (non-metro) | 328 | 1.3 (0.08) | 532 | 2.1 (0.10) | 0.8 | 65.5 | 146 | 0.6 (0.05) | 208 | 0.8 (0.06) | 0.2 | 37.2 |
| Non-core (non-metro) | 139 | 0.9 (0.08) | 197 | 1.3 (0.09) | 0.4 | 44.0 | 76 | 0.5 (0.05) | 69 | 0.4(0.05) | 0.1 | −18.8 |
| Psychostimulant and any opioidd | Psychostimulant without any opioide | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| 2016 | 2017 | 2016 | 2017 | |||||||||
|
|
|
|
|
|||||||||
| Decedent characteristic | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate |
|
| ||||||||||||
| All | 3416 | 1.1 (0.02) | 5203 | 1.7(0.02) | 0.6 | 52.2 | 4126 | 1.3 (0.02) | 5130 | 1.6 (0.02) | 0.3 | 23.0 |
| Sex | ||||||||||||
| Male | 2344 | 1.5 (0.03) | 3520 | 2.2 (0.04) | 0.7 | 46.7 | 3004 | 1.8 (0.04) | 3720 | 2.3 (0.04) | 0.5 | 21.7 |
| Female | 1072 | 0.7 (0.02) | 1683 | 1.1 (0.03) | 0.4 | 58.5 | 1122 | 0.7 (0.02) | 1410 | 0.9 (0.02) | 0.2 | 24.6 |
| Age group (years) | ||||||||||||
| 0–14 | f | f | f | f | - | - | f | f | f | f | - | - |
| 15–19 | 39 | 0.2 (0.03) | 61 | 0.3 (0.04) | 0.1 | 56.4 | 46 | 0.2 (0.03) | 47 | 0.2 (0.03) | 0 | 2.2 |
| 20–24 | 295 | 1.3 (0.08) | 455 | 2.1 (0.10) | 0.8 | 56.1 | 191 | 0.9 (0.06) | 217 | 1.0 (0.07) | 0.1 | 15.0 |
| 25–34 | 1052 | 2.4 (0.07) | 1694 | 3.7(0.09) | 1.3 | 58.7 | 710 | 1.6 (0.06) | 899 | 2.0 (0.07) | 0.4 | 24.8 |
| 35–44 | 865 | 2.1 (0.07) | 1343 | 3.3 (0.09) | 1.2 | 53.7 | 966 | 2.4 (0.08) | 1205 | 2.9 (0.08) | 0.5 | 23.5 |
| 45–54 | 690 | 1.6 (0.06) | 1001 | 2.4(0.07) | 0.8 | 46.5 | 1224 | 2.9 (0.08) | 476 | 3.5 (0.09) | 0.6 | 21.8 |
| 55–64 | 413 | 1.0 (0.04) | 571 | 1.4(0.06) | 0.4 | 36.5 | 831 | 2.0 (0.07) | 1077 | 2.6 (0.08) | 0.6 | 28.0 |
| ≥65 | 61 | 0.2 (0.02) | 74 | 0.3 (0.03) | 0.1 | 17.5 | 148 | 0.3 (0.02) | 204 | 0.4 (0.03) | 0.1 | 33.5 |
| Census region | ||||||||||||
| Northeast | 307 | 0.6 (0.03) | 508 | 1.0(0.04) | 0.4 | 67.8 | 124 | 0.2 (0.02) | 140 | 0.3 (0.02) | 0.1 | 13.4 |
| Midwest | 652 | 1.0 (0.04) | 1213 | 1.9 (0.06) | 0.9 | 87.4 | 524 | 0.8 (0.04) | 746 | 1.1 (0.04) | 0.3 | 39.2 |
| South | 1128 | 1.0 (0.03) | 1853 | 1.6 (0.04) | 0.6 | 63.3 | 1310 | 1.1 (0.03) | 3506 | 1.4 (0.03) | 0.3 | 21.5 |
| West | 1329 | 1.7 (0.05) | 1629 | 2.1 (0.05) | 0.4 | 21.4 | 2123 | 2.6 (0.06) | 2589 | 3.2 (0.06) | 0.6 | 21.1 |
| County urbanization level | ||||||||||||
| Large central metro | 1128 | 1.1 (0.03) | 1521 | 1.5 (0.04) | 0.4 | 32.7 | 1433 | 1.4 (0.04) | 1657 | 1.5 (0.04) | 0.1 | 13.3 |
| Large fringe metro | 653 | 0.9 (0.03) | 1076 | 1.4(0.04) | 0.5 | 60.1 | 582 | 0.8 (0.03) | 767 | 1.0 (0.04) | 0.2 | 27.6 |
| Medium metro | 818 | 1.3 (0.05) | 1345 | 2.1 (0.06) | 0.8 | 65.6 | 1003 | 1.5 (0.05) | 1327 | 2.0 (0.06) | 0.5 | 31.9 |
| Small metro | 307 | 1.1 (0.07) | 476 | 1.8 (0.08) | 0.7 | 58.7 | 391 | 1.3 (0.08) | 496 | 2.2 (0.10) | 0.9 | 65.5 |
| Micropolitan (non-metro) | 323 | 1.3 (0.08) | 510 | 2.1 (0.10) | 0.8 | 56.0 | 422 | 1.6 (0.08) | 484 | 1.9 (0.09) | 0.3 | 16.4 |
| Non-core (non-metro) | 187 | 1.1 (0.09) | 275 | 1.7(0.10) | 0.6 | 47.4 | 295 | 1.7 (0.10) | 399 | 2.2 (0.11) | 0.5 | 32.9 |
Source: National Vital Statistics System, Mortality file.
Deaths are classified using the International Classification of Diseases, 10th Revision (ICD–10). Drug overdose deaths are identified using underlying cause-of-death codes X40–X44, X60-X64, X85 and Y10–Y14. Age-adjusted death rates were calculated by applying age-specific death rates to the 2000 US standard population age distribution. All rates are per 100 000 population.
Drug overdose deaths, as defined, that have cocaine (T40.5) and any opioid (T40.0, T40.1, T40.2, T40.3, T40.4 or T40.6) as a contributing cause.
Drug overdose deaths, as defined, that have cocaine (T40.5) and do not have an opioid (T40.0, T40.1, T40.2, T40.3, T40.4 or T40.6) as a contributing cause.
Drug overdose deaths, as defined, that have psychostimulants with abuse potential (T43.6) and any opioid (T40.0, T40.1, T40.2, T40.3, T40.4 or T40.6) as a contributing cause.
Drug overdose deaths, as defined, that have psychostimulantswith abuse potential (T43.6) and do not have an opioid (T40.0, T40.1, T40.2, T40.3, T40.4 or T40.6) as a contributing cause.
Cells with ≤ 9 deaths are not reported. Rates based on < 20 deaths are not considered reliable and not reported. Bold type indicates statistical significance (P ≤ 0.05) determined by Z-test. SE = standard error.
From 2016 to 2017, the death rate involving cocaine without opioids increased 23.3%, from 0.9 to 1.1. Rates also increased among both sexes, most age groups, all regions and all urbanization levels except for non-core counties. The Midwest witnessed the largest absolute (0.4) and relative (43.7%) regional increases.
Deaths involving psychostimulants with and without opioids, 2016–17
In 2017, 50.3% of psychostimulant-involved overdose deaths involved at least one opioid. The death rate involving psychostimulants with an opioid increased 52.2% from 2016 to 2017, from 1.1 to 1.7 per 100000 (Table 2). Rates also increased among both sexes and all age groups, except those ≥ 65 years (rates not calculated for 0–14 years), all regions and all urbanization levels. Medium metro areas had the largest relative increase (65.6%), while medium metro and micropolitan areas had the largest absolute increases (0.8). The Mid-west had the largest absolute (0.9) and relative (87.4%) regional increases.
The death rate involving psychostimulants without opioids also increased from 2016 to 2017 (23.0%), from 1.3 to1.6.Rates increased among both sexes,most age groups, all regions except the Northeast and all urbanization levels. The largest absolute (0.9) and relative (65.5%) increases in rates by urbanization level were in small metro areas. While the largest relative increase by region was in the Midwest (39.2%), the largest absolute increase was in the West (0.6).
Trends in deaths involving cocaine and psychostimulants with and without opioids, 2006–17
From 2006 to 2017, death rates involving cocaine with an opioid decreased from 2006 to 2010 (APC = −12.0, CI = −18.6, −4.8), experienced a non-statistically significant increase from 2010 to 2014 (APC = 11.2, CI = −1.9, 26.0) and sharply increased from 2014 to 2017 (APC= 46.0, CI = 34.9, 58.1) (Fig. 1b). Death rates involving cocaine without opioids decreased from 2006 to 2009 (APC = −21.2, CI = −28.4, −13.2), remained stable from 2009 to 2014 (APC = −2.8, CI = −9.9, 4.9) and increased from 2014 to 2017 (APC = 23.6, CI = 11.8, 36.7). Rates involving psychostimulants with an opioid remained stable from 2006 to 2010 (APC = 5.9, CI = −9.8, 24.3) and increased from 2010 to 2015 (APC = 28.6, CI = 15.6, 43.1) and 2015 to 2017 (APC = 50.5, CI = 25.0, 81.1). Finally, death rates involving psychostimulants without opioids remained stable from 2006 to 2008 (APC = −13.6, CI = −31.3, 8.6) and increased from 2008 to 2017 (APC = 22.6, CI = 20.9, 24.3).
Deaths involving cocaine and psychostimulants and specific opioid categories, 2016–17
Death rates involving cocaine and synthetic opioids and cocaine and heroin increased from 2016 to 2017 (76.9 and 9.1%, respectively) (Table 3). While death rates involving cocaine and synthetic opioids increased for all demographics, regions (except the South, with a 16.7% decrease) and urbanization levels, death rates involving cocaine and heroin by demographic group were mostly stable. Smaller increases in death rates involving cocaine and heroin were seen among both sexes, people aged 45–54 years (22.2%), all regions except the West and large central (14.3%) and large fringe metro (15.4%) counties.
Table 3.
Number and age-adjusted ratesa of cocaine and psychostimulant overdose deaths with synthetic opioids other than methadone and heroin, by sex, age, Census region and level of urbanization—United States, 2016 and 2017.
| Cocaine and synthetics other than methadoneb | Cocaine and heroinc | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2016 | 2017 | 2016 | 2017 | |||||||||
|
|
|
|
|
|||||||||
| Decedent characteristic | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate |
|
| ||||||||||||
| All | 4184 | 1.3 (0.02) | 7241 | 2.3 (0.03) | 1.0 | 76.9 | 3395 | 1.1 (0.02) | 3974 | 1.2 (0.02) | 0.1 | 9.1 |
| Sex | ||||||||||||
| Male | 3013 | 2.0(0.04) | 5218 | 3.3 (0.05) | 1.3 | 65.0 | 2482 | 1.6 (0.03) | 2875 | 1.8 (0.04) | 0.2 | 12.5 |
| Female | 1171 | 0.8 (0.02) | 2023 | 1.3 (0.03) | 0.5 | 62.5 | 913 | 0.6 (0.02) | 1099 | 0.7 (0.02) | 0.1 | 16.7 |
| Age group (years) | ||||||||||||
| 0–14 | f | f | f | f | - | - | f | f | f | f | - | - |
| 15–19 | 36 | 0.2 (0.03) | 64 | 0.3 (0.04) | 0.1 | 50.0 | 30 | 0.1 (0.03) | 23 | 0.1 (0.02) | 0.0 | 0.0 |
| 20–24 | 318 | 1.4(0.08) | 500 | 2.3 (0.10) | 0.9 | 64.3 | 280 | 1.3 (0.08) | 281 | 1.3 (0.08) | 0.0 | 0.0 |
| 25–34 | 1293 | 2.9 (0.08) | 2139 | 4.7 (0.10) | 1.8 | 62.1 | 1027 | 2.3 (0.08) | 1151 | 2.5 (0.08) | 0.2 | 8.7 |
| 35–44 | 1140 | 2.8 (0.08) | 1918 | 4.7 (0.11) | 1.9 | 67.9 | 883 | 2.2 (0.08) | 992 | 2.4(0.08) | 0.2 | 9.1 |
| 45–54 | 916 | 2.1 (0.07) | 1648 | 3.9 (0.10) | 1.8 | 85.7 | 754 | 1.8 (0.07) | 943 | 2.2 (0.07) | 0.4 | 22.2 |
| 55–64 | 429 | 1.0(0.05) | 867 | 2.1 (0.07) | 1.1 | 110.0 | 421 | 0.6 (0.05) | 582 | 0.7(0.05) | 0.1 | 16.7 |
| ≥65 | 51 | f | 100 | f | - | - | 49 | f | 67 | f | - | - |
| Census region | ||||||||||||
| Northeast | 1571 | 2.9 (0.08) | 2547 | 4.7 (0.10) | 1.8 | 62.1 | 1088 | 2.0 (0.06) | 1288 | 2.4 (0.07) | 0.4 | 20.0 |
| Midwest | 1151 | 1.8 (0.05) | 2085 | 3.3 (0.07) | 1.5 | 83.3 | 1050 | 1.6 (0.05) | 1152 | 1.8 (0.05) | 0.2 | 12.5 |
| South | 1360 | 1.2 (0.03) | 2410 | 1.0 (0.04) | −0.2 | −16.7 | 1027 | 0.9 (0.03) | 1307 | 1.1 (0.03) | 0.2 | 22.2 |
| West | 102 | 0.2 (0.02) | 199 | 0.3 (0.02) | 0.1 | 50.0 | 230 | 0.3 (0.02) | 227 | 0.3 (0.02) | 0.0 | 0.0 |
| County urbanization level | ||||||||||||
| Large central metro | 1608 | 1.6 (0.04) | 2675 | 2.6 (0.05) | 1.0 | 62.5 | 1437 | 1.4 (0.04) | 1699 | 1.6 (0.04) | 0.2 | 14.3 |
| Large fringe metro | 1338 | 1.8 (0.05) | 2201 | 2.8 (0.06) | 1.0 | 55.6 | 957 | 1.3 (0.04) | 1131 | 1.5 (0.04) | 0.2 | 15.4 |
| Medium metro | 778 | 1.3 (0.04) | 1482 | 2.4 (0.06) | 1.1 | 84.6 | 636 | 1.0 (0.04) | 718 | 1.1 (0.04) | 0.1 | 10.0 |
| Small metro | 214 | 0.8 (0.05) | 384 | 1.5 (0.08) | 0.7 | 87.5 | 158 | 0.6 (0.05) | 185 | 0.7(0.05) | 0.1 | 16.7 |
| Micropolitan (non-metro) | 172 | 0.7(0.05) | 356 | 1.5 (0.08) | 0.8 | 114.3 | 154 | 0.6 (0.05) | 173 | 0.7(0.06) | 0.1 | 16.7 |
| Non-core (non-metro) | 74 | 0.5 (0.05) | 143 | 0.9 (0.08) | 0.4 | 80.0 | 53 | 0.3 (0.05) | 68 | 0.4(0.05) | 0.1 | 33.3 |
| Psychostimulant and synthetics other than metliadoned | Psychostimulant and heroine | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| 2016 | 2017 | 2016 | 2017 | |||||||||
|
|
|
|
|
|||||||||
| Decedent characteristic | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate | No. | Rate (SE) | No. | Rate (SE) | Absolute change in rate | % change in rate |
|
| ||||||||||||
| All | 1042 | 0.3 (0.01) | 2 546 | 0.8 (0.02) | 0.5 | 166.7 | 1546 | 0.5 (0.01) | 2094 | 0.7(0.02) | 0.2 | 40.0 |
| Sex | ||||||||||||
| Male | 720 | 0.5 (0.02) | 1780 | 1.2 (0.03) | 0.7 | 140.0 | 1134 | 0.7(0.02) | 1472 | 0.9 (0.03) | 0.2 | 28.6 |
| Female | 322 | 0.2 (0.01) | 766 | 0.5 (0.02) | 0.3 | 150.0 | 412 | 0.3 (0.01) | 622 | 0.4 (0.02) | 0.1 | 33.3 |
| Age group (years) | ||||||||||||
| 0–14 | f | f | f | f | - | - | f | f | f | f | - | - |
| 15–19 | 14 | f | 38 | 0.2 (0.03) | - | NA | 19 | f | 20 | f | - | - |
| 20–24 | 83 | 0.4 (0.04) | 228 | 1.0(0.07) | 0.6 | 150.0 | 165 | 0.7(0.06) | 198 | 0.9 (0.06) | 0.2 | 28.6 |
| 25–34 | 365 | 0.8 (0.04) | 904 | 2.0 (0.07) | 1.2 | 150.0 | 528 | 1.2 (0.05) | 750 | 1.7(0.06) | 0.5 | 41.7 |
| 35–44 | 297 | 0.7 (0.04) | 738 | 1.8 (0.07) | 1.1 | 157.1 | 390 | 1.0(0.05) | 527 | 1.3 (0.06) | 0.3 | 30.0 |
| 45–54 | 187 | 0.4 (0.03) | 439 | 1.0 (0.05) | 0.6 | 150.0 | 275 | 0.6 (0.04) | 364 | 0.9 (0.05) | 0.3 | 50.0 |
| 55–64 | 85 | 0.2 (0.02) | 179 | 0.4 (0.03) | 0.2 | 100.0 | 151 | 0.4 (0.03) | 208 | 0.5 (0.03) | 0.1 | 25.0 |
| ≥65 | 10 | f | 19 | f | - | - | 18 | f | 26 | f | - | - |
| Census region | ||||||||||||
| Northeast | 171 | 0.3 (0.02) | 386 | 0.7 (0.04) | 0.4 | 133.3 | 117 | 0.2 (0.02) | 180 | 0.4 (0.03) | 0.2 | 100.0 |
| Midwest | 302 | 0.5 (0.03) | 829 | 1.3 (0.05) | 0.8 | 160.0 | 2 54 | 0.4 (0.03) | 388 | 0.6 (0.03) | 0.2 | 50.0 |
| South | 433 | 0.4 (0.02) | 1040 | 0.9 (0.03) | 0.5 | 125.0 | 415 | 0.4 (0.02) | 608 | 0.5 (0.02) | 0.1 | 25.0 |
| West | 136 | 0.2 (0.02) | 291 | 0.4 (0.02) | 0.2 | 100.0 | 760 | 1.0(0.04) | 918 | 1.2 (0.04) | 0.2 | 20.0 |
| County urbanization level | ||||||||||||
| Large central metro | 275 | 0.3 (0.02) | 566 | 0.6 (0.02) | 0.3 | 100.0 | 608 | 0.6 (0.02) | 781 | 0.7(0.03) | 0.1 | 16.7 |
| Large fringe metro | 257 | 0.4 (0.02) | 620 | 0.8 (0.03) | 0.4 | 100.0 | 306 | 0.4 (0.02) | 426 | 0.5 (0.03) | 0.1 | 25.0 |
| Medium metro | 234 | 0.4 (0.03) | 682 | 1.1 (0.04) | 0.7 | 175.0 | 339 | 0.5 (0.03) | 492 | 0.8 (0.04) | 0.3 | 60.0 |
| Small metro | 103 | 0.4 (0.04) | 232 | 0.9 (0.06) | 0.5 | 125.0 | 115 | 0.4 (0.04) | 169 | 0.6 (0.05) | 0.2 | 50.0 |
| Micropolitan (non-metro) | 109 | 0.4 (0.04) | 284 | 1.2 (0.07) | 0.8 | 200.0 | 123 | 0.5 (0.05) | 159 | 0.7(0.05) | 0.2 | 40.0 |
| Non-core (non-metro) | 64 | 0.4 (0.05) | 162 | 1.0 (0.08) | 0.6 | 150.0 | 55 | 0.3 (0.05) | 67 | 0.4(0.05) | 0.1 | 33.3 |
Source: National Vital Statistics System, Mortality file.
Deaths are classified using the International Classification of Diseases, 10th Revision (ICD–10). Drug overdose deaths are identified using underlying cause-of-death codes X40–X44, X60-X64, X85 and Y10–Y14. Age-adjusted death rates were calculated by applying age-specific death rates to the 2000 US standard population age distribution. All rates are per 100 000 population.
Drug overdose deaths, as defined, that have cocaine (T40.5) and synthetic opioids other than methadone (T40.4) as a contributing cause.
Drug overdose deaths, as defined, that have cocaine (T40.5) and heroin (T40.1) as a contributing cause.
Drug overdose deaths, as defined, that have psychostimulants with abuse potential (T43.6) and synthetic opioids other than methadone (T40.4) as a contributing cause.
Drug overdose deaths, as defined, that have psychostimulants with abuse potential (T43.6) and heroin (T40.1) as a contributing cause.
Cells with ≤ 9 deaths are not reported. Rates based on < 20 deaths are not considered reliable and not reported. Bold type indicates statistical significance (P ≤ 0.05) determined by Z-test. SE= standard error.
Death rates involving psychostimulants and synthetic opioids also increased from 2016 to 2017 (166.7%), from 0.3 to 0.8 per 100000. Increases were also observed in all demographics. Increases in death rates involving psychostimulants and heroin were observed overall (40.0%) and among most demographic groups, although increases were not as large as those with psychostimulants and synthetic opioids.
DISCUSSION
In 2016, 27% of overdose ED visits involving cocaine and 14% involving psychostimulants also involved a reported opioid. In 2017, almost 75% of overdose deaths involving cocaine and half involving psychostimulants involved at least one opioid. Overall, we found that rates of overdose ED visits involving cocaine and psychostimulants with an opioid increased in recent years, as did those involving psychostimulants without opioids. Non-fatal cocaine overdoses without opioids decreased from 2015 to 2016. Overdose deaths involving cocaine and psychostimulants increased in the past several years with and without opioids. Of particular note, these increases occurred across a broad range of demographic groups and geographic areas, underscoring the dynamic and evolving overdose crisis in the United States.
Our analysis of ED visit data with mortality data provides a better understanding of the recent increases in stimulant-involved fatal overdoses. Rates of cocaine- and psychostimulant-involved overdose ED visits with any opioid were relatively low, and while increasing from 2015 to 2016, they did not increase as dramatically as death rates involving cocaine and psychostimulants with opioids. In contrast to mortality data, cocaine overdose ED visits without an opioid decreased 13.6% from 2015 to 2016. However, because poisoning codes are influenced by self-report and provider observations, overdoses seen in the ED involving stimulants with fentanyl may be coded as stimulants only due to a lack of toxicological testing [12]. Therefore, stimulants with opioid ED visit estimates may underestimate their actual values, and the without opioid categories may be overestimated.
Deaths involving cocaine and opioids increased more than cocaine deaths without an opioid from 2016 to 2017, suggesting that the opioid overdose epidemic is contributing to recent increases in cocaine-involved deaths. Data from 2016 to 2017 on psychostimulant-involved deaths with and without opioids also point to increasing opioid involvement. These findings point to the importance of ensuring that the response to the opioid overdose crisis is sufficiently nimble to incorporate evolving drug use patterns. Current efforts to expand medication-assisted treatment for opioid use disorder should consider the polysubstance nature of addiction and incorporate a continuum of treatment and recovery support services targeted to the multiple substances an individual may be using when engaging in treatment.
Analyses of stimulant overdose deaths and specific opioids support the finding that synthetic opioids (e.g. IMF) are the primary opioids found in deaths involving both stimulants and opioids. While deaths involving cocaine and heroin increased, the rate was much lower than those involving cocaine and synthetic opioids from 2016 to 2017. However, this could be attributable to changes in the drug supply rather than underlying changes in use in the population. While heroin drug submissions in NFLIS increased from 2006 to 2015, they decreased from 2015 to 2017 [13]. Conversely, fentanyl drug submissions increased dramatically from 2014 to 2017, and in some areas in the Northeast and Midwest are the predominant illicit opioid available in some illicit drug markets [13]. We also observed large relative increases in deaths involving psychostimulants and synthetic opioids from 2016 to 2017, particularly in the Midwest, although rates were relatively low. In 2017, 30% of methamphetamine-caused deaths in Florida had fentanyl as a co-occurring substance [14]. Fentanyl mixed with cocaine or methamphetamine poses a substantially heightened risk of overdose among people who only use stimulants or use opioids infrequently and thus lack opioid tolerance [15]. This also underscores the importance of naloxone access not onlyamong individuals knowingly using opioids, but also among individuals using other illicit drugs that might be contaminated with IMF [16].
ED visits for psychostimulant overdose without an opioid also increased from 2015 to 2016. The West has historically had higher methamphetamine use rates [17], and experienced particularly large increases in ED visits for psychostimulant overdose from 2015 to 2016. This is probably attributable to a shift in production of methamphetamine by Mexican cartels in recent years after a decline in US domestic production following laws limiting access to methamphetamine precursors, pseudoephedrine, phenylpropanolamine and ephedrine [18,19]. Since 2010, there has been a nearly 10-fold increase in the amount of methamphetamine seized by US Customs and Border Protection, from 8900 to more than 80000 pounds in 2018 [8]. Continued research and development of medications for treatment of methamphetamine use disorder, as well as other stimulant use disorders, are needed. Some data suggest that medications used to treat opioid use disorder, such as buprenorphine and extended-release naltrexone, may have a role in treating methamphetamine use disorder, but more research is needed [20,21].
Limitations
For overdose ED visits, comprehensive toxicological testing of biological samples from patients experiencing overdose rarely occurs [22], and may have led to misclassification of overdoses involving stimulants with and without opioids. As poisoning codes on ED medical records are influenced by patient self-report or observations by ED personnel [12], inclusion of opioid codes in combination with a stimulant code may be underestimated in ED data, especially in cases where patients use a stimulant unknowingly mixed with fentanyl [23,24]. For overdose deaths, improvements in toxicological testing over time might account for some increases. In addition, the types of drugs involved in overdose deaths were not included on 15% of death certificates in 2016 and 12% in 2017, potentially leading to an underestimate of stimulant-involved overdose deaths. The NEDS transition from ICD-9-CM to ICD-10-CM/PCS codes probably affected comparisons between overdose ED visits from 2015 to 2016 and also precluded us from performing comparisons in earlier years. To minimize the transition’s impact, we included all overdose intents since the transition modified coding guidelines, and previous analyses of overdose data have shown drastic differences across the transition by intent [25–27]. We also conducted sensitivity analyses comparing the fourth quarter of 2015 to the fourth quarter of 2016, both of which used ICD-10-CM codes, and found similar results (data not shown). Because of the time lag in NEDS data, we were unable to compare the exact most recent years in both ED and mortality data. While NEDS sample weights are used to extrapolate NEDS sample data to the universe of ED visits, the sample weights cannot control for different policy environments with respect to opioids in the sampling units, and some of the observed changes over time may be attributable to differences in policies in the states or regions sampled. Finally, there is overlap in the involvement of synthetic opioid- and heroin-involved overdose deaths presented in Table 4 (e.g. deaths involving cocaine and heroin do not exclude deaths involving cocaine, heroin and synthetic opioids). This limits our ability to discuss these as distinct categories.
CONCLUSIONS
While increases in deaths involving cocaine seem to be driven primarily by the opioid overdose epidemic, increases in psychostimulant-involved ED visits and overdose deaths were occurring with and without opioids. Increases in deaths involving stimulants with opioids are driven by synthetic opioids (e.g. IMF). Increased toxicological testing of ED patient samples could be beneficial, from a surveillance standpoint, to more clearly understand drugs involved in non-fatal overdoses. Additionally, as opioids are driving increases in stimulant overdoses, opioid overdose interventions, including access to and distribution of naloxone, linkage into risk reduction services, and medicationassisted treatment would be beneficial. Health-care providers have a unique opportunity to intervene with people who are treated in the ED for an overdose. Post-overdose protocols, buprenorphine induction in the ED and linkage into services may also be beneficial at point of care. Expansion of these interventions to people using stimulants and consideration for the polysubstance nature of addiction and the provision of comprehensive, evidence-based treatment for underlying stimulant use disorders are also necessary. Increased efforts are required to identify and improve access to treatment and risk reduction services for people using multiple substances, to implement upstream prevention efforts focusing on shared risk and protective factors that address substance use/misuse and to improve risk reduction messaging to focus on polysubstance misuse. Moreover, interventions that target the illicit drug supply and continued partnerships between public safetyand public health are needed. Given observed increases in overdoses involving stimulants without opioids, particularly in psychostimulants, novel, evidence-based interventions are necessary to address the expanding drug overdose epidemic. While effective medication for stimulant use disorder does not exist [28], expansion of the public health approach to combat the opioid crisis, including access to syringe services programs [29] and a broader approach to address socio-economic factors associated with drug use, may reduce the use of stimulants as well as opioids. Continued research and development of medications to treat stimulant use disorders are also needed.
Supplementary Material
Table S1 Overdose discharge diagnosis and cause of death codes for mortality and emergency department visits.
Footnotes
Declaration of interests
None.
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC). Use of trade names is for identification onlyand does not imply endorsement by the US Department of Health and Human Services, thePublicHealth Service or theCDC.
Supporting Information
Additional supporting information may be found online in the Supporting Information section at the end of the article.
References
- 1.Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug andopioid-involved overdose deaths—United States, 2013–2017. Morb Mortal Wkly Rep 2018; 67: 1419–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kariisa M, Scholl L, Wilson N, Seth P. Drug overdose deaths involving cocaine and psychostimulants with abuse potential —United States, 2003–2017. Morb Mortal Wkly Rep 2019; 68: 388–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCall Jones C, Baldwin GT, Compton WM Recent increases in cocaine-related overdose deaths and the role of opioids. Am J Public Health 2017; 107: 430–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nolan ML, Shamasunder S, Colon-Berezin C, Kunins HV,Paone D. Increased presence of fentanyl in cocaine-involved fatal overdoses: implications for prevention. J Urban Health 2019; 96: 49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones CM, Einstein EB, Compton WM Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA 2018; 319: 1819–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park JN, Weir BW, Allen ST, Chaulk P, Sherman SG Fentanyl-contaminated drugs and non-fatal overdose among people who inject drugs in Baltimore, MD. Harm Reduct J 2018; 15: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones CM, Christensen A, Gladden RM Increases in prescription opioid injection abuse among treatment admissions in the United States, 2004–2013. Drug Alcohol Depend 2017; 176: 89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Drug Enforcement Administration (USDEA). 2018 National Drug Threat Assessment. Springfield, VA: USDEA; 2018. [Google Scholar]
- 9.Seth P., Scholl L,Rudd RA, Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015-–2016. Morb Mortal Wkly Rep 2018; 67: 349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agencyfor Healthcare Qualityand Research. NEDS Overview.Healthcare Cost and Utilization Project (HCUP). Available at: www.hcup-us.ahrq.gov/nedsoverview.jsp (accessed 15 April 2019).
- 11.Seth P, Rudd RA, Noonan RK, Haegerich TM Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health 2018; 108: 500–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shah AD, Wood DM, Dargan PI Survey of ICD-10 coding of hospital admissions in the UK due to recreational drug toxicity. QJM 2011; 104: 779–84. [DOI] [PubMed] [Google Scholar]
- 13.US Drug Enforcement Administration (USDEA). DCD National Forensic Laboratory Information System: NFLIS-drug. 2017 Annual Report. Springfield, VA: USDEA; 2018. [Google Scholar]
- 14.Wang Y,Goldberger BA,Delcher C Florida drug-Related Outcomes and Surveillance Tracking System (FROST). Gainsville, FL: University of Florida; 2019. [Google Scholar]
- 15.National Institute on Drug Abuse (NIDA) Fentanyl. NIDA; 20 February 2019. [Google Scholar]
- 16.US Department of Health and Human Services (USDHHS). Naloxone: the Opioid Reversal Drug that Saves Lives. Washington, DC: USDHHS; 2018. [Google Scholar]
- 17.Gonzales R, Mooney L, Rawson RA The methamphetamine problem in the United States. Annu Rev Public Health 2010; 31: 385–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shukla RK, Crump JL, Chrisco ES An evolving problem: methamphetamine production and trafficking in the United States. Int J Drug Policy 2012; 23: 426–35. [DOI] [PubMed] [Google Scholar]
- 19.Maxwell JC, Brecht ML Methamphetamine: here we goagain? Addict Behav 2011; 36: 1168–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salehi M, Emadossadat A, Kheirabadi GR, Maracy MR,Sharbafchi MR The effect of buprenorphine on methamphetamine cravings. J Clin Psychopharmacol 2015; 35: 724–7. [DOI] [PubMed] [Google Scholar]
- 21.Coffin PO, Santos GM, Hern J, Vittinghoff E, Santos D, Matheson T, et al. Extended-release naltrexone for methamphetamine dependence among men who have sex with men: a randomized placebo-controlled trial. Addiction 2018; 113: 268–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu AH, McKay C, Broussard LA, Hoffman RS, Kwong TC, Moyer TP et al. National academyof clinical biochemistry laboratory medicine practice guidelines: recommendations for the use of laboratory tests to support poisoned patients who present to the emergency department. Clin Chem 2003; 49: 357–79. [DOI] [PubMed] [Google Scholar]
- 23.Di Rico R, Nambiar D, Stoove M, Dietze P. Drug overdose inthe ED: a record linkage study examining emergency department ICD-10 coding practices in a cohort of people who inject drugs. BMC Health Serv Res 2018; 18: 945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rowe C, Santos GM, Behar E, Coffin PO Correlates of overdose risk perception among illicit opioid users. Drug Alcohol Depend 2016; 159: 234–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moore BJ, Barrett ML. Case study: exploring how opioid-related diagnosis codes translate from ICD-9-CM to ICD-10-CM. 24 April 2017. Available at: https://www.hcup-us.ahrq.gov/datainnovations/icd10_resources.jsp. (accessed February 28, 2019).
- 26.Slavova S, Costich JF, Luu H, Fields J, Gabella BA, Tarima S. et al. Interrupted time series design to evaluate the effect of the ICD-9-CM to ICD-10-CM coding transition on injury hospitalization trends. Inj Epidemiol 2018; 5: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stewart C, Crawford PM, Simon GE Changes in coding of suicide attempts or self-harm with transition from ICD-9 to ICD-10. Psychiatr Serv 2017; 68: 215. [DOI] [PubMed] [Google Scholar]
- 28.Hartel-Petri R, Krampe-Scheidler A, Braunwarth WD, Havemann-Reinecke U, Jeschke P, Looser W. et al. Evidencebased guidelines for the pharmacologic management of methamphetamine dependence, relapse prevention, chronic methamphetamine-related, and comorbid psychiatric disorders in post-acute settings. Pharmacopsychiatry 2017; 50: 96–104. [DOI] [PubMed] [Google Scholar]
- 29.Rich JD, Adashi EY Ideological anachronism involving needle and syringe exchange programs: lessons from the Indiana HIV outbreak. JAMA 2015; 314: 23–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Overdose discharge diagnosis and cause of death codes for mortality and emergency department visits.