ABSTRACT
Problem
Our nation faces an urgent need for more primary care (PC) physicians, yet interest in PC careers is dwindling. Students from underrepresented in medicine (UIM) backgrounds are more likely to choose PC and practice in underserved areas yet their representation has declined. Accelerated PC programs have the potential to address workforce needs, lower educational debt, and diversify the physician workforce to advance health equity.
Approach
With support from Kaiser Permanente Northern California (KPNC) and the American Medical Association’s Accelerating Change in Medical Education initiative, University of California School of Medicine (UC Davis) implemented the Accelerated Competency-based Education in Primary Care (ACE-PC) program – a six-year pathway from medical school to residency for students committed to health equity and careers in family medicine or PC-internal medicine. ACE-PC accepts 6–10 students per year using the same holistic admissions process as the 4-year MD program with an additional panel interview that includes affiliated residency program faculty from UC Davis and KPNC. The undergraduate curriculum features: PC continuity clinic with a single preceptor throughout medical school; a 9-month longitudinal integrated clerkship; supportive PC faculty and culture; markedly reduced student debt with full-tuition scholarships; weekly PC didactics; and clinical rotations in affiliated residency programs with the opportunity to match into specific ACE-PC residency tracks.
Outcomes
Since 2014, 70 students have matriculated to ACE-PC, 71% from UIM groups, 64% are first-generation college students. Of the graduates, 48% have entered residency in family medicine and 52% in PC-internal medicine. In 2020, the first graduates entered the PC workforce; all are practicing in California, including 66% at federally qualified health centers, key providers of underserved care.
KEYWORDS: Primary care, competency-based education, workforce diversity, health equity, accelerated program
Problem
Despite an urgent need for more primary care (PC) physicians [1], student interest in PC continues to decline [2–4], medical education debt grows [5,6], and the culture of academic medicine discourages students from choosing PC [7]. The presence of PC physicians in a community is associated with an improved life expectancy [8–10]. Physicians from underrepresented in medicine (UIM) backgrounds (defined as American Indian or Alaska Natives, blacks, and Hispanics or Latinos) provide a disproportionate share of care to medically underserved populations helping to advance health equity [11,12]. Patient-physician racial concordance is associated with better health outcomes including lower costs [13] and improved communication [14]. However, UIM student representation in medical schools is declining [15] due to financial and educational barriers and longstanding structural inequities [16,17]. Accelerated training allows graduates to enter the workforce sooner, increasing their years in PC practice and addressing the shortage of UIM physicians [18].
In 2014, University of California Davis School of Medicine (UC Davis) implemented the Accelerated Competency-based Education in Primary Care (ACE-PC) program with Kaiser Permanente Northern California (KPNC) and the American Medical Association’s Accelerating Change in Medical Education initiative [19]. We describe this six-year undergraduate medical education (UME) to graduate medical education (GME) pathway for students committed to careers in Family Medicine (FM) or PC-Internal Medicine (PC-IM).
Approach to innovation
ACE-PC was designed with broad stakeholder input to address workforce needs, reduce medical school debt, and embed a competency-based pathway within the traditional medical school curriculum.
ACE-PC accepts 6–10 students per year using the same holistic admissions process [20] as the 4-year MD (4YMD) program with an additional panel interview prior to matriculation that includes an affiliated GME program faculty. Additional selection criteria include a demonstrated commitment to PC and underserved care. Factors that have attracted UIM students include the school’s commitment to diversity, program mission, and local media coverage. Students receive full tuition scholarships (from KPNC and UC Davis), graduating with less than one-third the debt of 4YMD students [21]. Students receive extensive longitudinal program faculty support, early clinical exposure, and GME mentoring. The small cohort and high faculty to student ratio contributes to student success and is difficult to replicate within a traditional curriculum.
ACE-PC core curriculum (Figure 1)
Figure 1.
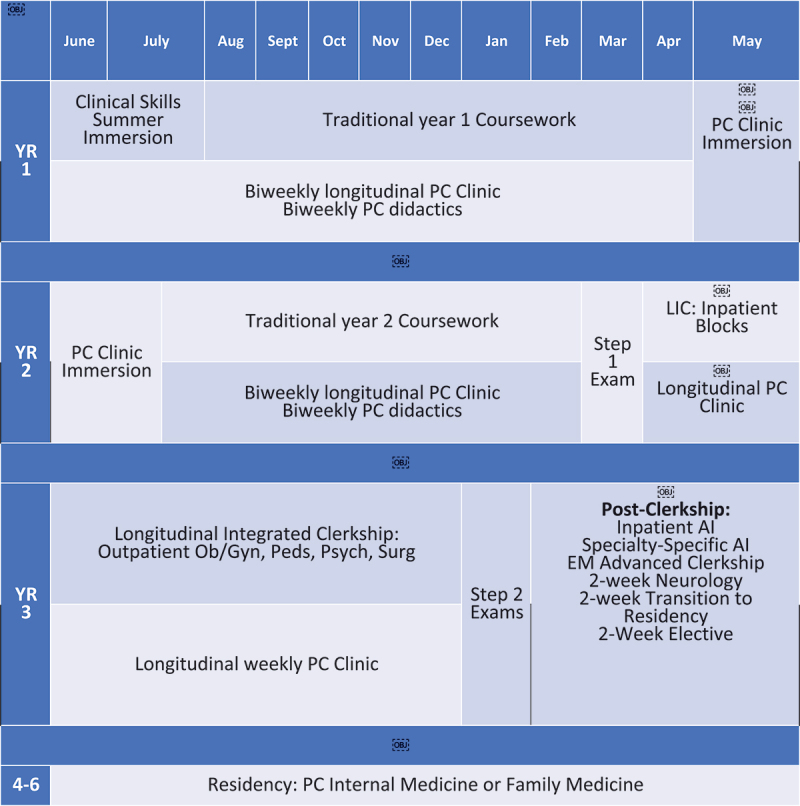
Structure of the 3-year MD curriculum.
The program emphasizes authentic PC experiences, mentoring relationships with PC physicians role models, and intentional professional identity development. Students complete the same educational objectives and assessments as 4YMD students on a modified timeline. Affiliated GME programs provide clinical training sites, exposing students to their faculty and institutional culture. Students participate in biweekly primary care didacts (Table 1) led by master clinician educators.
Table 1.
Example didactic topics with learning objectives. And change ‘The learning objectives for each session, if anchored to a UCD43 concern, are as follows’ to ‘The learning objectives for each session are as follows: The UCD43 is very specific to UCD and might not make much sense to a larger audience.
| Didactic | Discipline/Topic specific Learning Objective(s) |
|---|---|
|
Format: – Case discussion focused on the symptom/scenario with emphasis on clinical reasoning – Presentation by faculty or by students on an approach to the symptom/concern – Discussion of specific high-yield diseases related to the symptom or concern |
The learning objectives for each session, if anchored to a UCD43 concern, are as follows: For each topic – Using a case, practice a diagnostic framework that addresses the common and life-threatening causes of the chief concern – Discuss the key elements of the history, physical exam, and diagnostic testing that are likely to lead to a diagnosis For specific disease states – Define the disease and pertinent terminology – Construct and illness script for the disease state, including prevalence, risk factors, symptoms, sings, test data, and complications if relevant – Discuss criteria for diagnosis, including the value of specific symptoms, signs, or diagnostic data in terms of likelihood ratios, if relevant – Discuss basic management |
| Chest pain | 1. Using a case, practice a diagnostic framework that addresses the common and life-threatening causes of CHEST PAIN 2. Discuss the key elements of the history, physical exam, and diagnostic testing most likely to exclude life threatening disease 3. List the common causes of CHEST PAIN |
| Edema | 1. Using a case, practice a diagnostic framework that addresses the common and life-threatening causes of EDEMA 2. Discuss the key elements of the history, physical exam, and diagnostic testing most likely to exclude life threatening disease 3. List the common causes of EDEMA |
| Dyspnea | 1. Using a case, practice a diagnostic framework that addresses the common and life-threatening causes of DYSPNEA 2. Discuss the key elements of the history, physical exam, and diagnostic testing most likely to exclude life threatening disease 3. List the common causes of DYSPNEA |
| Sleep disturbance | 1. Using a case, practice a diagnostic framework that addresses the common causes of SLEEP DISTURBANCE 2. Discuss the key elements of the history, physical exam, and diagnostic testing most likely to identify the underlying cause 3. List the common causes of SLEEP DISTURBANCE |
| Substance Use | 1. Define Substance Use Disorder 2. List DSM-V diagnostic criteria for SUD, in the context of the ‘4C’ framework 3. Review evidence-based treatment of Alcohol use disorder 4. Review evidence-based treatment of OUD |
Pre-clerkship
Students arrive 6 weeks before 4YMD students to complete an intensive summer clinical immersion that replaces the traditional Year 1 longitudinal clinical skills curriculum, including the same final Objective Structured Clinical Examination. Students attend PC continuity clinic (PCCC) three half days a week during summer immersion and every other week during Years 1 and 2 with the same preceptor that supervises them for 3 years. Between Years 1 and 2, each student completes a four-week PC clinical at an affiliated FM or PC-IM GME program.
Clerkship
After an abbreviated study period, students take USMLE Step 1 and begin a longitudinal integrated clerkship (LIC) with 4 weeks of inpatient IM and two-week inpatient rotations in Obstetrics and Gynecology, Pediatrics, Psychiatry, and Surgery; followed by six ambulatory months with weekly PCCC and clinics in each core discipline.
Post-clerkship
In January of Year 3, after an abbreviated USMLE Step 2 study period, students complete the required advanced clinical rotations for 4YMD students (IM, Emergency Medicine, and ICU); and either a pediatrics sub-internship (for FM applicants) or second IM sub-internship (for PC-IM applicants).
Residency match
During the LIC, students apply through the Electronic Residency Application Service and National Resident Matching Program (NRMP). Two FM programs and one PC-IM program have unique NRMP tracks for ACE-PC students only (unfilled spots revert to the parent categorical program). GME program directors meet with ACE-PC leadership twice yearly to discuss each student’s progress, facilitating a warm handoff from UME to GME.
Outcomes
Since 2014, 70 students have matriculated into ACE-PC, 71% from UIM backgrounds and 84% self-identifying as disadvantaged. MCAT scores, undergraduate GPA, and USMLE Step 1 and Step 2 scores are comparable between ACE-PC and 4YMD students. Only 10% have transitioned to the 4YMD program, compared to approximately 16% nationally for accelerated programs [22]. Of the first 40 graduates, 48% matched in FM and 52% matched in PC-IM: 42% at UC Davis, 18% at KP, and 40% at non-affiliated GME programs. All graduates progressed normally through GME; one resident in each of the first four graduating cohorts was selected to be chief resident. The first GME graduates entered the workforce in 2020; of the first 12 in PC practice, 8 work at a Federally Qualified Health Center, 2 at an academic medical center, and 2 at KP. Two PC-IM graduates completed geriatrics fellowship and one FM graduate is completing an addiction medicine fellowship.
Limitations
Accelerated programs are not advisable for all students, particularly those who need time to explore other specialties or who struggle to reach out for help. Disadvantaged students may experience personal hardships that affect performance [23–25], underscoring the need for flexibility and options for transitioning to the 4YMD curriculum. The program requires significant investment in scholarships, academic support, mentoring [26], consistent faculty development [27,28], and protected faculty time, which some institutions may be unwilling or unable to provide.
Lessons learned
ACE-PC is a successful 3-year MD pathway for diverse students committed to PC and health equity. The program leverages holistic admissions, robust scholarships, authentic PC experiences, and direct linkages to GME programs. Early PCCC cultivates professional identity development and mentoring relationships with supportive PC role models. Frequent faculty development helps develop preceptor assessment and feedback skills. The LIC cultivates long-term preceptor-student relationships while meeting the requirements of multiple core clerkships. Student success is enhanced by weekly didactics with master educators, coaching from diverse faculty mentors, and a supportive environment in which students can learn and grow with like-minded peers.
Funding Statement
Drs. Fancher, Henderson and Gonzalez-Flores effort on this project was supported by a grant from the American Medical Associations ChangeMedEd grant.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].AAMC Association of American Medical Colleges . 2019 state of the physician workforce. Washington (DC): Association of American Medical Colleges; 2019. [cited 2024 Mar 20]. Available from: https://www.aamc.org/services/member-capacity-building/holistic-review [Google Scholar]
- [2].Connelly MT, Sullivan AM, Peters AS, et al. Variation in predictors of primary care career choice by year and stage of training. J Gen Intern Med. 2003;18(3):159–5. doi: 10.1046/j.1525-1497.2003.01208.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300(10):1154–1164. doi: 10.1001/jama.300.10.1154 [DOI] [PubMed] [Google Scholar]
- [4].Kost A, Bentley A, Phillips J, et al. Graduating medical student perspectives on factors influencing specialty choice: an AAFP national survey. Fam Med. 2019;51(2):129–136. doi: 10.22454/FamMed.2019.136973 [DOI] [PubMed] [Google Scholar]
- [5].Rogalsky DK. Medical students with median debt: an endangered species? [comment letter]. Academ Med. 2013;88(5):555. doi: 10.1097/ACM.0b013e31828a0cf9 [DOI] [PubMed] [Google Scholar]
- [6].Rosenblatt RA, Andrilla CHA. The impact of US medical students? Debt on their choice of primary care careers: an analysis of data from the 2002 medical school graduation questionnaire. Academic Med. 2005;80(9):815–819. doi: 10.1097/00001888-200509000-00006 [DOI] [PubMed] [Google Scholar]
- [7].Warm EJ, Goetz C. Too smart for primary care? Ann Intern Med. 2013;159(10):709–710. doi: 10.7326/0003-4819-159-10-201311190-00009 [DOI] [PubMed] [Google Scholar]
- [8].Basu S, Berkowitz SA, Phillips RL, et al. Association of primary care physician supply with population mortality in the United States, 2005-2015. JAMA Intern Med. 2019;179(4):506–514. doi: 10.1001/jamainternmed.2018.7624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Snyder JE, Upton RD, Hassett TC, et al. Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the US. JAMA Netw Open. 2023;6(4):e236687. doi: 10.1001/jamanetworkopen.2023.6687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Washko MM, Syder JE, Zangaro G. Where do physicians train? Investigating public and private institutional pipelines. Health Aff. 2015;34(5):852–856. doi: 10.1377/hlthaff.2014.1356 [DOI] [PubMed] [Google Scholar]
- [11].Marrast LM, Zallman L, Woodhandler S, et al. Minority physicians’ role in the care of underserved patients: diverisfying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174(2):289–291. doi: 10.1001/jamainternmed.2013.12756 [DOI] [PubMed] [Google Scholar]
- [12].Salhi RA, Dupati A, Burkhardt JC. Interest in serving the underserved: role of race, gender, and medical specialty plans. Health Equity. 2022;6(1):933–941. doi: 10.1089/heq.2022.0064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Jetty A, Jabbarpour Y, Pollack J, et al. Patient-physician racial concordance associated with improved healthcare use and lower healthcare expenditures in minority populations. J Racial Ethn Health Disparities. 2022. Feb;9(1):68–8. doi: 10.1007/s40615-020-00930-4 [DOI] [PubMed] [Google Scholar]
- [14].Shen MJ, Peterson EB, Costas-Muñiz R, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018. Feb;5(1):117–140. doi: 10.1007/s40615-017-0350-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Talamantes E, Henderson MC, Fancher TL, et al. Closing the gap — making medical school admissions more equitable. N Engl J Med. 2019;380(9):803–805. doi: 10.1056/NEJMp1808582 [DOI] [PubMed] [Google Scholar]
- [16].Faiz J, Essien UR, Washington DL, et al. Racial and ethnic differences in barriers faced by medical college admission test examinees and their association with medical school application and matriculation. JAMA Health Forum. 2023;4(4):e230498. doi: 10.1001/jamahealthforum.2023.0498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Guevara JP, Wade R, Aysola J. Racial and ethnic diversity at medical schools — why aren’t we there yet? N Engl J Med. 2021. Nov 4 [cited 2021 Oct 30];385(19):1732–1734. doi: 10.1056/NEJMp2105578 [DOI] [PubMed] [Google Scholar]
- [18].Cangiarella J, Fancher T, Jones B, et al. 2017. Available from: https://www.ncbi.nlm.nih.gov/pubmed/?term=Hunsaker%20M%5BAuthor%5D&cauthor=true&cauthor_uid=27805950
- [19].Skochelak SE, Stack SJ. Creating the medical schools of the future. Academic Med. 2017;92(1):16–19. doi: 10.1097/ACM.0000000000001160 [DOI] [PubMed] [Google Scholar]
- [20].Henderson MC, Fancher TL, Murin S. Holistic admissions at UC davis—journey toward equity. JAMA. 2023;330(11):1037–1038. doi: 10.1001/jama.2023.15872 [DOI] [PubMed] [Google Scholar]
- [21].Abramson S, Jacob D, Rosenfeld M, et al. A 3-year MD — accelerating careers, diminishing debt. N Engl J Med. 2013;369(12):1085–1087. doi: 10.1056/NEJMp1304681 [DOI] [PubMed] [Google Scholar]
- [22].Macerollo A, Brenner J, Cangiarella J, et al. When accelerated MD program is not the right path: the why and how to support our learners in the transition. Med Ed Online (Under Rev). 2023. [Google Scholar]
- [23].Henderson MC, Green C, Chen C. What does it mean for medical school admissions to be socially accountable? AMA J Ethics. 2021. Dec 1;23(12):E965–974. [DOI] [PubMed] [Google Scholar]
- [24].Nguyen M, Chaudhry SI, Desai MM, et al. Association of sociodemographic characteristics with US medical student attrition. JAMA Intern Med. 2022;182(9):917–924. doi: 10.1001/jamainternmed.2022.2194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].O’Marr JM, Chan SM, Crawford L, et al. Perceptions on burnout and the medical school learning environment of medical students who are underrepresented in medicine. JAMA Netw Open. 2022;5(2). doi: 10.1001/jamanetworkopen.2022.0115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Farkas AH, Allenbaugh J, Bonifacino E, et al. Mentorship of US medical students: a systematic review. J Gen Intern Med. 2019;34(11):2602–2609. doi: 10.1007/s11606-019-05256-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Bensimon EM. The underestimated significance of practitioner knowledge in the scholarship on student success. Rev Higher Educ: J Assoc For The Study of Higher Educ. 2007;30(4):441–469. doi: 10.1353/rhe.2007.0032 [DOI] [Google Scholar]
- [28].Schmid ME, Gillian-Daniel DL, Kraemer S, et al. Promoting student academic achievement through faculty development about inclusive teaching. Change: The Mag of Higher Learn. 2016;48(5):16–25. doi: 10.1080/00091383.2016.1227672 [DOI] [Google Scholar]


