ABSTRACT
Background Residents and fellows as educators (RFAE) programs typically focus on clinical teaching skills in single departments, which may not be sustainable for those with limited trainees or faculty.
Objective To determine the feasibility and value of a 2-week interdepartmental RFAE elective for advanced teaching skill development and transition to practice as clinician educators.
Methods Facilitated discussion, simulation, and critiqued peer presentations developed participants’ skills in teaching, curriculum design, professional development, and scholarship. Assessments in this prospective intervention included 2 self-reported surveys addressing: (1) teaching process and motivation (Conceptions of Learning and Teaching [COLT]), and (2) skills and attitudes. We administered both surveys at baseline, immediate-post, and 3-month-post elective with data compared across time points using Kruskal-Wallis tests. Program evaluation comprised daily open-ended surveys on engagement and an end-of-course feedback survey.
Results There were 79 participants from 2019 to 2023. Survey response rates were 84.8% (67 of 79) at baseline, 58.2% (46 of 79) immediate-post, and 51.9% (41 of 79) 3-month-post. Most participants were residents (89.9%, 71 of 79), female (60.8%, 48 of 79), from pediatrics and/or medicine departments (77.2%, 61 of 79), and in their final year of training (77.2%, 61 of 79). COLT factor orientation to professional practice scores increased in the immediate-post (3.3) compared to baseline (2.5) surveys (P=.008). Teaching skills attitudes scores increased for all questions in 3-month-post compared to baseline surveys. In open-ended questions, participants emphasized the importance of professional development sessions in guiding their careers toward medical education.
Conclusions This interdepartmental elective was feasible, favorably received, and sustained over time, with observed changes in participants’ teaching skills attitudes.
Introduction
The Liaison Committee on Graduate Medical Education and the Accreditation Council for Graduate Medical Education (ACGME) identify teaching skill development as an important component of graduate medical education (GME).1,2 Consequently, residents and fellows as educators (RFAE) programs have been widely implemented, but remain heterogeneous in their goals, reproducibility, content, and assessments.3-5 Future clinician educators (faculty who are teachers, scholars, and/or leaders) require experience beyond clinical teaching to meet the ACGME Clinician Educator Milestones.6,7
The optimal content and structure of RFAE programs remain unclear. Most published RFAE interventions are short, clinically focused didactics in single departments.4,5,8 In contrast, RFAE workshops, tracks, and electives have focused on developing advanced skills in scholarship and professional identity formation.9-15 Meeting the ACGME Clinician Educator Milestones requires interventions that promote reflection and application, which can be time- and resource-intensive.6 Interdepartmental RFAE programs can leverage institutional resources and cultivate diverse perspectives, but may pose logistical challenges.9,10,16,17 Electives can consolidate time and resources, but most reported RFAE electives offer limited professional development, and we are unaware of reports of interdepartmental RFAE electives.11,12,18,19
The lack of effective early curricular interventions for transitioning educators may disadvantage residents and fellows seeking education careers. To address this need, we created and evaluated an interdepartmental GME elective to enhance existing teaching and curriculum design skills and prepare participants to embark on careers as clinician educators.
KEY POINTS
What Is Known
Small residency and fellowship programs have difficulty supporting educator training programs, which could benefit trainees entering professional educator roles after graduation.
What Is New
This 2-week interdepartmental elective model with multiple teaching modalities was highly acceptable, sustained over time, and successful in improving teaching skills attitudes.
Bottom Line
An interdepartmental elective approach is feasible and acceptable, and appears to facilitate medical education careers.
Methods
Setting and Participants
All Penn State College of Medicine residents and fellows in at least postgraduate year 2 were eligible to participate. The course was advertised to all GME trainees and program directors. We capped enrollment at 20 learners based on our experience with effective classroom size and limitations in simulation resources and facilitator recruitment. Residents and fellows in the existing interdepartmental Clinician Educator Track and those who could complete the entire elective received priority enrollment. The course directors (R.S.C., A.B.C., A.L.D.) taught most sessions and also recruited facilitators from diverse backgrounds and departments. One faculty had protected time (0.2 full-time equivalent [FTE]) and administrative support (0.05 FTE) for the RFAE program through an endowment from the Penn State Woodward Center for Excellence in Health Sciences Education. The course directors met with all facilitators and provided course syllabi. Materials included a simulation center and teaching platforms (eg, white boards, computer projection, online learning platform).
Intervention
This elective was implemented annually from 2019 to 2023 as a part of the Penn State RFAE program. Our design approach aligned with Kern’s framework and previously published RFAE curricula recommendations.20,21 We reviewed the literature to identify characteristics of successful RFAE programs, finding that reproducible materials focused on teaching skills and curriculum design.22-29 The course directors held iterative discussions regarding the core skills needed by transitioning clinician educators and expanded the curriculum to include career development, based on their experience in faculty development. We designed a 2-week RFAE interdepartmental elective with learning objectives, content, and assessments aligned into themes of teaching skills (eg, feedback, didactic innovations), curriculum design, professional development (eg, mentorship, job negotiation), and education scholarship (Table 1).
Table 1.
Graduate Medical Education Elective Curriculum Map
| Learning Objectives | Content | Methods | Assessment/Evaluation |
| Goal: To enhance the teaching knowledge and skills of residents and fellows and to promote their understanding of introductory concepts in medical education | |||
| Theme: teaching skills | |||
| Describe introductory concepts in adult learning theory and apply those concepts to their teaching Describe medical education clinical and didactic teaching tools and discuss the evidence for their use as best practice |
|
|
|
| Theme: curriculum design | |||
| Outline approaches to curriculum design in medical education Develop learning objectives and an assessment plan for an observed teaching session |
|
|
|
| Theme: professional development | |||
| Discuss potential careers in medical education and reflect upon this field as a career option |
|
|
|
| Theme: education scholarship | |||
| Appraise the value of medical education scholarship |
|
|
|
Abbreviations: GME, graduate medical education; OSTE, objective structured teaching examination; OSFE, objective structured feedback examination; COLT, Conceptions of Learning and Teaching.
Educational strategies promoted application and reflection through observed teaching, debriefs, journal clubs, simulation, and microteaching (Table 1). Participants presented 10-minute teaching sessions at the start and end of the elective with peer and faculty feedback. Informal lunches introduced participants to educators with different career paths.
Outcomes
The primary outcome of this prospective intervention study was teaching attitudes of participants. Participants were invited to complete anonymous electronic surveys of teaching attitudes at baseline, immediate-post, and 3-month-post elective. We sent 2 reminder emails at each time point to nonresponders. We adapted the Conceptions of Learning and Teaching (COLT) tool to assess participants’ teaching process and motivation, which aligned with our goal of promoting learner-centered education (online supplementary data Appendix A). The COLT includes factors of teacher-centeredness, appreciation of active learning, and orientation to professional practice.30,31 We changed “students” to “learners” and “tutor” to “facilitator/teacher” and omitted the item “being introduced to the day-to-day practice of their future profession motivates students to learn” to better reflect our participants. Responses were on a 5-point Likert scale (1=strongly disagree, 5=strongly agree). An additional self-reported survey from the Woodward Center for Excellence in Health Sciences Education assessed teaching skills and attitudes over the past 3 months on a scale of 0 (low) to 100 (high) and with open-ended questions (online supplementary data Appendix B). Additional validity evidence for this survey was not obtained.
The program was evaluated with daily open-ended questions about engagement and unanswered questions (online supplementary data Appendix C) to provide information to trainees in real time, and a final course evaluation on suggestions for improvement (online supplementary data Appendix D) to revise content for the subsequent year.
Analysis
We used descriptive statistics to summarize learner demographics. We compared COLT factors and the teaching skills responses at baseline, immediate-post, and 3-month-post using Kruskal-Wallis tests. Given the nonstandard score distributions, we used medians and interquartile ranges.
Open-ended responses were described using number of responses and word count averages. We analyzed the daily feedback and final evaluation open-ended responses for content related to the course themes (teaching skills, curriculum design, professional development, scholarship). Daily feedback surveys were electronically captured from 2021 to 2023 and the final evaluation from all years except 2020 (due to a distribution error). The teaching skills responses were analyzed in categories of learner- or teacher-centered approach based on the Teaching Perspectives Inventory, which aligned with the course goal to cultivate learner-centered approaches.32 For example, “they should implement my lesson into practice” is a teacher-centered response and “tailor goals to what they find relevant” is a learner-centered response about setting learning goals.
This study was determined exempt by the Penn State College of Medicine Institutional Review Board.
Results
The number of participants ranged from 10 to 20 each year (79 total). Most participants were residents (89.9%, 71 of 79), female (60.8%, 48 of 79), from pediatrics, internal medicine, or combined medicine/pediatrics programs (77.2%, 61 of 79), and in their final year of training (77.2%, 61 of 79; Table 2).
Table 2.
Learner Demographics (N=79)
| Demographic | n (%) |
| Sex | |
| Male | 31 (39.2) |
| Female | 48 (60.8) |
| Resident/fellow | |
| Fellow | 8 (10.1) |
| Resident | 71 (89.9) |
| Year training | |
| 2 | 18 (22.8) |
| 3 | 50 (63.3) |
| 4+ | 11 (13.9) |
| Department | |
| Anesthesia | 2 (2.5) |
| Cardiology | 1 (1.3) |
| Dermatology | 1 (1.3) |
| Family and community medicine | 3 (3.8) |
| Internal medicine | 22 (27.8) |
| Combined medicine/pediatrics | 3 (3.8) |
| Neonatal-perinatal medicine | 2 (2.5) |
| Neurology | 2 (2.5) |
| Physical medicine and rehabilitation | 1 (1.3) |
| Pediatrics | 36 (45.6) |
| Pediatric cardiology | 3 (3.8) |
| Pulmonary critical care | 2 (2.5) |
| Surgery | 1 (1.3) |
Feasibility and Acceptability
Dedicated administrative support was crucial for coordinating course facilitators, rooms, and equipment. All facilitators needed initial training to align session and course objectives, which was time intensive in the first year. We fortunately had accessible facilities, equipment, and a learning management system at no additional cost. The elective was viewed favorably by participants, and the number of interested participants eventually exceeded the available slots. Invited facilitators consistently agreed to teach in the course over multiple years.
Assessment
In total, 67 of 79 participants (84.8%) completed the baseline, 46 (58.2%) the immediate-post, and 41 (51.9%) the 3-month-post surveys.
Orientation to professional practice increased between the baseline and immediate-post surveys and decreased in the 3-month-post survey (Figure). There was no change in teacher-centeredness or appreciation of active learning (Figure) or in comparisons of COLT factors when analyzed by year (data not shown).
Figure.
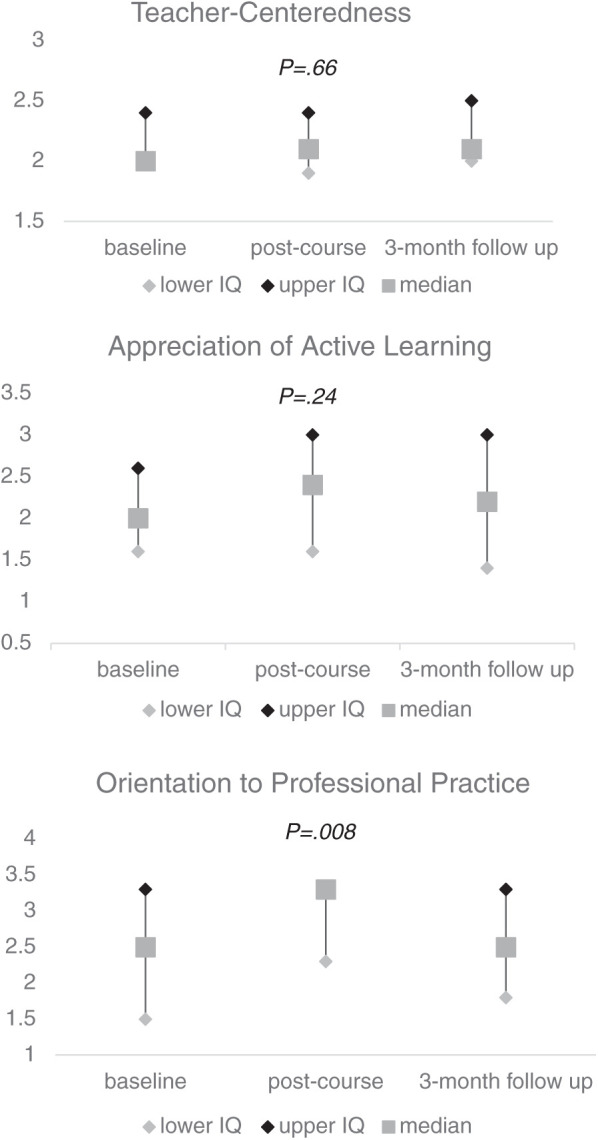
Conceptions of Learning and Teaching (COLT) Survey Responses
Note: The COLT survey is analyzed in factors of teacher-centeredness, appreciation of active learning, and orientation to professional practice. This figure shows the median and IQRs of survey responses for each subscore compared at baseline, immediate-post course, and 3-months post course. Scores for orientation to professional practice increased between the immediate-post compared to baseline surveys, but this change was not sustained at 3-months post course. Survey responses did not significantly differ for the teacher centeredness or appreciation of active learning subscores.
Teaching skills scores increased across all questions in both the immediate-post and 3-month-post surveys compared to baseline. Comparisons reached statistical significance for most questions in the baseline compared to immediate-post surveys and for all questions in the baseline compared to 3-month-post surveys (Table 3). Responses did not significantly differ in the immediate-post compared to 3-month-post surveys or in comparisons at all time points by year (data not shown). Most open-ended responses were learner-centered at baseline (387 of 638, 60.7%), immediate-post (288 of 451, 63.9%), and 3-month-post (193 of 319, 60.5%; online supplementary data Appendix E).
Table 3.
Teaching Skills Survey Responses
| Survey Itema | Baseline vs Immediate Post,a Median (IQR) | P value | Baseline vs 3 Month Post,a Median (IQR) | P value |
| Maintaining a positive learning environment | 75.0 (68.5, 80.0) vs 80.0 (70.0, 90.0) | .07 | 75.0 (68.5, 80.0) vs 80.0 (77.5, 87.5) | .0001 |
| Introducing session and expectations | 62.0 (55.0, 74.0) vs 72.5 (60.0, 84.0) | .02 | 62.0 (55.0, 74.0) vs 75.0 (65.0, 81.0) | .0018 |
| Establishing goals with learner | 60.0 (50.0, 75.0) vs 70.0 (60.0, 82.0) | .03 | 60.0 (50.0, 75.0) vs 75.0 (67.0, 85.0) | .0021 |
| Incorporating appropriate questioning (knowledge/skills) | 63.5 (50.0, 74.5) vs 70.0 (60.0, 80.0) | .05 | 63.5 (50.0, 74.5) vs 71.0 (59.5, 80.5) | .0440 |
| Incorporating appropriate questioning (clinical reasoning) | 60.0 (50.0, 75.0) vs 70.5 (60.0, 80.0) | .003 | 60.0 (50.0, 75.0) vs 75.0 (66.5, 85.0) | .0006 |
| Actively engaging learner during patient care activities | 60.0 (50.0, 76.0) vs 70.0 (60.0, 80.0) | .09 | 60.0 (50.0, 76.0) vs 74.5 (68.5, 82.5) | .0010 |
| Assessing learner’s clinical skills through direct observation | 55.0 (50.0, 68.0) vs 70.0 (55.0, 80.0) | .005 | 55.0 (50.0, 68.0 vs 74.5 (64.0, 82.5) | <.001 |
| Assessing learner’s oral presentation(s) | 56.0 (47.5, 70.0) vs 70.0 (52.0, 80.0) | .004 | 56.0 (47.5, 70.0) vs 72.5 (60.5, 80.0) | .0016 |
| Providing verbal feedback | 60.0 (50.0, 71.5) vs 73.5 (60.0, 88.0) | .004 | 60.0 (50.0, 71.5) vs 75.0 (60.0, 85.0) | .0050 |
| Providing written feedback | 50.0 (30.0, 60.0) vs 63.5 (50.0, 80.0) | <.001 | 50.0 30.0, 60.0) vs 67.5 (59.0, 79.0) | <.001 |
| Helping learner develop a (specific) plan to improve knowledge or skills | 50.0 (40.0, 60.5) vs 63.5 (50.0, 77.0) | .001 | 50.0 (40.0, 60.5) vs 65.0 (55.0, 77.0) | <.001 |
Survey items are abbreviated in this table with full survey questions available in online supplementary data Appendix 2. Responses were on a scale of 0 (low) to 100 (high).
Program Evaluation
Daily Feedback Survey:
Participants completed 356 daily feedback surveys, which averaged 16.2 words per response (2021-2023). The most engaging sessions were about teaching skills (59.3%, 211 of 356) and professional development (30.6%, 109 of 356; online supplementary data Appendix F). Perceived engagement with professional development was disproportionate to the relative content hours (3 hours compared to 21 hours for teaching skills).
The amount of planning in instructional design was eye opening to some: “Fascinating to look at a different portion of medical education we lack during our training as we never see the ins and outs of curriculum development.” The professional development sessions highlighted clinician educator careers in a way that was not otherwise available: “A lot of attending life is sort of behind a curtain…it’s hard to guess what is realistic to ask for or expect in a job. It was helpful to identify people who might be good resources.”
Final Course Evaluation:
Participants completed 67 of 79 (84.8% response rate) final course evaluations (2019, 2021-2023). Most participants agreed or strongly agreed with questions about the overall quality of the course and their understanding of topics due to course participation (online supplementary data Appendix G). Open-ended responses averaged 39 words with most responses commenting on curricular design (39 of 57, 68.4%) and professional development (14 of 57, 24.6%; online supplementary data Appendix H). The course prompted participants to consider their professional development as educators: “It helped me clarify my career goals…I think these topics are going to help me in so many arenas in my career, as a senior, as a resident, as an attending” and “It was fantastic in enhancing my internal outward philosophy on my future career.” Participants reflected positively on the course design and their engagement: “Each session had a purpose that was thoughtfully and deliberately included in the curriculum, and built on itself in a way that really strengthened my understanding of how to improve as an educator.” Suggestions for session improvement varied, with some participants desiring increased interaction (ie, “redesigning the curriculum design lecture to a brainstorm group project”) and some less (ie, “some days it became tiresome to constantly be discussing in small groups and I found myself wishing for one session that was just a PowerPoint”).
Discussion
This interdepartmental RFAE elective, developed to prepare trainees for future clinical educator careers, was highly acceptable to those selecting the experience, feasible and sustainable in terms of faculty and administrative supports, and indicative of some changes in attitudes toward teaching.
Elective participants’ orientation to professional practice, assessed via the COLT survey, increased during the elective, but was not maintained 3 months post-survey. The lack of change in other COLT factors was unexpected as the course content appeared to align well with the COLT: we spent more curricular time on classroom than clinical teaching techniques. A short elective may be insufficient to significantly affect other professional elements. We saw significant increases in all surveyed teaching skills attitudes between baseline and 3-month-post. It is likely, however, that varied skill application opportunities following the course impacted the later survey results. Published RFAE interventions also show positive changes in teaching attitudes, but direct comparisons are difficult related to different assessment tools.5,33
This elective was a resource-efficient way to implement an RFAE intervention across departments at Penn State. We found that, like existing interventions, interdepartmental representation cultivated diverse perspectives, but we did not directly measure this outcome.9,10,16 Of note, participation was not feasible for trainees from all departments (particularly surgical) due to competing priorities. Although professional development skills are similar across departments, focused interventions may be better suited for certain departments (eg, procedural teaching skills for anesthesia and surgery).34,35
This study represents the experience of a single large academic institution. Participants were self-selected and highly interested in education; results may not reflect groups with differing interest levels. Self-reported assessments and decreased response rates over time could lead to response bias. Additional longitudinal qualitative data is needed to assess the relative impact of the elective and outside experiences on teaching skills, professional identity, and interdepartmental community building.9,17,36,37 We acknowledge that the open-ended responses may not represent the views of all participants and that themes may be missing.
In the future, additional educational opportunities could be offered following the elective to facilitate skill application and observation. Future assessments could include higher-level outcomes and career trajectory after graduation.
Conclusions
This interdepartmental elective focusing on RFAE skill development and exploring educational themes not otherwise included during training was feasible, sustained, and highly acceptable to participants. Residents and fellows found the content on professional development to be particularly useful toward the end of their training.
Supplementary Material
Acknowledgments
The authors would like to thank Benjamin D. Hoover, an Access Services and Instruction Librarian at the Harrell Health Sciences Library Research and Learning Commons at Penn State Milton S. Hershey Medical Center, who assisted with the literature review for this study.
Editor’s Note
The online supplementary data contains further data from the study including the surveys used in the study.
Author Notes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.Accreditation Council for Graduate Medical Education Program Director Guide to the Common Program Requirements, Version 3.0. Published 2023. Accessed December 5, 2023. https://www.acgme.org/meetings-and-educational-activities/program-directors-guide-to-the-common-program-requirements/
- 2.Liaison Committee on Medical Education Functions and structure of a medical school: standards for accreditation of medical education programs leading to the MD degree. Accessed December 5, 2023. https://lcme.org/publications/
- 3.Al Achkar M, Hanauer M, Morrison EH, Davies MK, Oh RC. Changing trends in residents-as-teachers across graduate medical education. Adv Med Educ Pract . 2017;8:299–306. doi: 10.2147/AMEP.S127007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bree KK, Whicker SA, Fromme HB, Paik S, Greenberg L. Residents-as-teachers publications: what can programs learn from the literature when starting a new or refining an established curriculum? J Grad Med Educ . 2014;6(2):237–248. doi: 10.4300/JGME-D-13-00308.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dannaway J, Ng H, Schoo A. Literature review of teaching skills programs for junior medical officers. Int J Med Educ . 2016;7:25–31. doi: 10.5116/ijme.5685.14da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Accreditation Council for Graduate Medical Education Clinician educator milestones. Accessed December 5, 2023. https://www.acgme.org/milestones/resources/clinician-educator-milestones/
- 7.Helflin MT, Pinheiro S, Kaminetzky CP, McNeill D. “So you want to be a clinician-educator…”: designing a clinician-educator curriculum for internal medicine residents. Med Teach . 2009;31(6):e233–e240. doi: 10.1080/01421590802516772. [DOI] [PubMed] [Google Scholar]
- 8.Wamsley MA, Julian KA, Wipf JE. A literature review of “resident-as-teacher” curricula: do teaching courses make a difference? J Gen Intern Med . 2004;19(5 Pt 2):574–581. doi: 10.1111/j.1525-1497.2004.30116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen HC, Wamsley MA, Azzam A, Julian K, Irby DM, O’Sullivan PS. The health professions education pathway: preparing students, residents, and fellows to become future educators. Teach Learn Med . 2017;29(2):216–227. doi: 10.1080/10401334.2016.1230500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahn J, Martin S, Farnan J, Fromme B. The graduate medical education scholars track: developing residents as clinician-educators during clinical training via a longitudinal, multimodal, and multidisciplinary track. Acad Med . 2018;93(2):214–219. doi: 10.1097/ACM.0000000000001815. [DOI] [PubMed] [Google Scholar]
- 11.Martins AR, Arbuckle MR, Alicia AA, Cabaniss DL. Growing teachers: using electives to teach senior residents how to teach. Acad Psychiatry . 2010;34(4):291–293. doi: 10.1176/appi.ap.34.4.291. [DOI] [PubMed] [Google Scholar]
- 12.Drum BM, Sheffield CR, Mulcaire-Jones J, Gradick C. Formation and evaluation of an academic elective for residents in a combined internal medicine-pediatrics residency program. Cureus . 2021;13(7):e16287. doi: 10.7759/cureus.16287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohlwes RJ, Cornett P, Dandu M, et al. Developing educators, investigators, and leaders during internal medicine residency: the area of distinction program. J Grad Med Educ . 2011;3(4):535–540. doi: 10.4300/JGME-D-11-00029.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rowat J, Johnson K, Antes L, White K, Rosenbaum M, Suneja M. Successful implementation of a longitudinal skill-based teaching curriculum for residents. BMC Med Educ . 2021;21(1):346. doi: 10.1186/s12909-021-02765-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedman K, Lester J, Young JQ. Clinician-educator tracks for trainees in graduate medical education: a scoping review. Acad Med . 2019;94(10):1599–1609. doi: 10.1097/ACM.0000000000002814. [DOI] [PubMed] [Google Scholar]
- 16.Nagler A, Chudgar SM, Rudd M, et al. GME concentrations: a collaborative interdisciplinary approach to learner-driven education. J Grad Med Educ . 2015;7(3):422–429. doi: 10.4300/JGME-D-14-00599.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Theophanous C, Itani R. Residents teaching residents: the case for interdepartmental resident lecture programs. Med Educ . 2020;54(11):1058–1059. doi: 10.1111/medu.14316. [DOI] [PubMed] [Google Scholar]
- 18.Ilgen JS, Takayesu JK, Bhatia K, et al. Back to the bedside: the 8-year evolution of a resident-as-teacher rotation. J Emerg Med . 2011;41(2):190–195. doi: 10.1016/j.jemermed.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 19.Weissman MA, Bensinger L, Koestler JL. Resident as teacher: educating the educators. Mt Sinai J Med . 2006;73(8):1165–1169. [PubMed] [Google Scholar]
- 20.Kern ED, Thomas P, Howard D, Bass E. Curriculum Development for Medical Education: A Six Step Approach . The Johns Hopkins University Press; 1998. [Google Scholar]
- 21.Mann KV, Sutton E, Frank B. Twelve tips for preparing residents as teachers. Med Teach . 2007;29(4):301–306. doi: 10.1080/01421590701477431. [DOI] [PubMed] [Google Scholar]
- 22.Newman L, Tibbles CD, Atkins KM, et al. Resident-as-teacher DVD series. MedEdPORTAL . 2015;11:10152. doi: 10.15766/mep_2374-8265.10152. [DOI] [Google Scholar]
- 23.Martin SK, Ahn J, Farnan JM, Fromme HB. Introduction to curriculum development and medical education scholarship for resident trainees: a webinar series. MedEdPORTAL . 2016;12:10454. doi: 10.15766/mep_2374-8265.10454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.UC Riverside School of Medicine Resident Teaching Skills BEST: bringing education & service together. Accessed May 9, 2024. https://residentteachingskills.ucr.edu/bringing-education-service-together-curriculum-best.
- 25.Society of Teachers of Family Medicine Residents as educators. Accessed May 9, 2024. https://www.stfm.org/teachingresources/curriculum/residentsaseducatorscurriculum/overview/
- 26.Harrell H, Wipf J, Aronowitz P, et al. Resident as teacher curriculum. MedEdPORTAL . 2015;11:10001. doi: 10.15766/mep_2374-8265.10001. [DOI] [Google Scholar]
- 27.Columbia College of Physicians and Surgeons Residents as teachers. Accessed May 9, 2024. https://resteach.ccnmtl.columbia.edu/
- 28.Sherbino J, Joshi N, Lin M. JGME-ALiEM hot topics in medical education online journal club: an analysis of a virtual discussion about resident teachers. J Grad Med Educ . 2015;7(3):437–444. doi: 10.4300/JGME-D-15-00071.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seelig S, Bright E, Bod J, et al. Educating future educators-resident distinction in education: a longitudinal curriculum for physician educators. West J Emerg Med . 2021;23(1):100–102. doi: 10.5811/westjem.2021.11.53890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jacobs JC, Van luijk SJ, Van Berkel H, Van der Vleuten CP, Croiset G, Scheele F. Development of an instrument (the COLT) to measure conceptions on learning and teaching of teachers, in student-centred medical education. Med Teach . 2012;34(7):e483-91. doi: 10.3109/0142159X.2012.668630. [DOI] [PubMed] [Google Scholar]
- 31.Pacifico JL, van Mook W, Jacobs JCG, van der Vleuten C, Heeneman S. Extending the use of the conceptions of learning and teaching (COLT) instrument to the postgraduate setting. BMC Med Educ . 2021;21(1):32. doi: 10.1186/s12909-020-02461-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Collins JB, Pratt DD. The teaching perspectives inventory at 10 years and 100,000 respondents: reliability and validity of a teacher self-report inventory. Adult Educ Quart . 2011;61(4):358–375. doi: 10.1177/0741713610392763. [DOI] [Google Scholar]
- 33.Coverdale JH, Ismail N, Mian A, Dewey C. Toolbox for evaluating residents as teachers. Acad Psychiatry . 2010;34(4):298–301. doi: 10.1176/appi.ap.34.4.298. [DOI] [PubMed] [Google Scholar]
- 34.Hoyler MM, Pryor KO, Gotian R, Brumberger ED, Chan JM. Resident physicians as clinical educators in anesthesiology: a narrative review. Anesth Analg . 2023;136(2):270–281. doi: 10.1213/ANE.0000000000006243. [DOI] [PubMed] [Google Scholar]
- 35.Geary A, Hess DT, Pernar LIM. Resident-as-teacher programs in general surgery residency—a review of published curricula. Am J Surg . 2019;217(2):209–213. doi: 10.1016/j.amjsurg.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 36.Barnhoorn PC, Nierkens V, Numans ME, Steinert Y, Kramer AWM, van Mook WNKA. General practice residents’ perspectives on their professional identity formation: a qualitative study. BMJ Open . 2022;12(7):e059691. doi: 10.1136/bmjopen-2021-059691. [DOI] [Google Scholar]
- 37.Pacifico JL, Donkers J, Jacobs J, van der Vleuten C, Heeneman S. Understanding teaching and learning conceptions among clinical faculty as a means to improve postgraduate training. Int J Med Educ . 2020;11:175–185. doi: 10.5116/ijme.5f2a.76eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


