Abstract
Arterial hypertension is the most important modifiable risk factor for cardiovascular morbidity and mortality. In some countries, pharmacists’ patient-centered approach has become a common practice, and their role in supporting the management of cardiovascular disease has been successfully developed for years. In particular, recent findings have confirmed benefits of pharmacist-provided hypertension care. Current guidelines emphasize the need for regular BP measurements in subjects age 40 years and older, who are at increased risk of hypertension. A panel of experts in cardiology, hypertensiology, family medicine, and pharmacy presented a narrative review of implementing community pharmacy blood pressure (CPBP) measurements into Polish pharmacy practice to assist pharmacists in CPBP readings. The paper focuses on basic aspects of management of untreated patients with elevated blood pressure levels, as well as management of individuals diagnosed with hypertension, who should follow their primary care physicians’ recommendations for anti-hypertensive therapy. The article also includes a few important aspects related to CPBP measurement, such as equipment and techniques. Development of ready-made schemes of procedures for patients with different results of blood pressure measurement could ensure a uniform standard of services provided by pharmacists. This gives an opportunity to provide such patients with medical care and initiate treatment, and facilitates effective maintenance of BP in hypertensive subjects. This article reviews the role of pharmacists in Poland in screening for hypertension by taking blood pressure measurements.
Keywords: Blood Pressure Determination, Community Pharmacy Services, Hypertension, Education, Public Health
Introduction
In Europe, arterial hypertension (HTN) is the most common cause of morbidity and death. Elevated, poorly controlled blood pressure (BP) has been associated with a higher risk of a wide range of cardiac abnormalities, including myocardial infarction (MI), stroke, ischemic and hemorrhagic cerebral infarction, and peripheral arterial disease (PAD) [1,2]. This phenomenon is more common in eastern European countries such as Poland where the prevalence of HTN has been estimated to be as high as 49% in individuals aged 30–79 years. It is estimated that of 10.8 million Polish patients with HTN, only 2.6 million are successfully treated [3,4]. Undoubtedly, HTN is the most important modifiable risk factor for cardiovascular morbidity and mortality [5]. Measurements of BP made in a physician’s office are a basis for diagnosing HTN and initiating anti-hypertensive therapy, whereas ambulatory measurements, including those performed by pharmacists in community settings, could be a useful tool for screening untreated individuals as well as monitoring treated hypertensive patients [6].
In the United States and in some European countries, pharmacists’ patient-centered approach has become a common practice, and their role in supporting the management of cardiovascular disease (CVD) has been successfully developed for years [7]. In these countries, pharmacists have been widely employed in team-based care for HTN. A recent meta-analysis (N=2573 participants) has confirmed benefits of pharmacist-provided HTN care, which might include home-based BP telemonitoring [8]. Other findings support the idea that the healthcare professional-led interventions (physician, nurse, pharmacist) on lifestyle modifications are important for lowering blood pressure and managing cardiovascular risk, and should be widely implemented into daily practice [9].
In Poland, the concept of pharmaceutical care, defined as responsible provision of pharmacotherapy to improve patient adherence and quality of life, was incorporated into Polish legislation in 2008. This may involve pharmacist-led education of hypertensive patients on drug therapies and counseling on secondary lifestyle changes, as well as monitoring and risk screening [10]. Such activities are consistent with the need for greater interprofessional collaboration in health care, especially considering the high rates of cardiovascular morbidity and mortality in patients [11].
The recent guidelines have defined multicomponent strategies, including team-based care, as the most effective methods of BP control in hypertensive patients [12]. In line with these findings, the engagement of community pharmacists in out-of-office BP readings might facilitate recognition of untreated BP patients and provide more effective maintenance of BP goals.
This paper presents common opinions of medical practitioners on community pharmacy blood pressure (CPBP) measurements performed by pharmacists, based on the current clinical guidelines. This narrative review was performed during meetings of a panel of 16 Polish experts, including cardiologists, hypertensiologists, internists, and community and clinical pharmacists, who participated in a virtual advisory board from January to May in 2023. In particular, we discuss basic aspects of management of untreated patients with elevated BP levels, as well as of individuals diagnosed with HTN, who should follow their primary care physicians’ recommendations for anti-hypertensive therapy. The main focus was placed on the role of teaching patients how to properly perform blood pressure measurements as well as making them aware of the necessity of medication adherence. Other interventions could involve identification and management of drug-related problems (eg, dealing with adverse effects or interactions, education about proper storage and dosing schedules, patient motivation to take anti-hypertensive medication correctly and to understand the benefits of their medication), and management of cardiovascular risk factors (eg, smoking and alcohol cessation, weight reduction, restriction of sodium intake, and recommendations for daily physical activity or dietary modifications). The experts focused on using a multidisciplinary approach in evaluation and management of these patients [7]. It is expected that the proposed activities in everyday practice will improve health promotion, prevent cardiovascular diseases, facilitate BP management, reduce the proportion of undiagnosed/untreated individuals, and help to save time and costs for primary care physicians. This article reviewed the role of pharmacists in Poland in screening for HTN by taking blood pressure measurements.
BP Measurements Outside the Doctor’s Office
Scientific guidelines emphasize the importance of out-of-office BP measurements, including home BP readings [12]. Patients diagnosed with HTN should measure their BP levels regularly, as recommended by physicians, using appropriate technology. Inaccurate equipment, inappropriate cuff sizes that are commonly used, and lack of knowledge and skills can limit the usefulness of such measurements. Lack of knowledge and skills can manifest as failing to keep intervals between BP measurements; drinking coffee, eating a heavy meal, or physical exercise before measurement; fitting the cuff improperly; or taking a reading while in an incorrect posture [5]. According to previous observations in the Polish population, about 60% of patients were able to measure their BP correctly [13]. These factors may limit the usefulness of home BP monitoring and confirm the need for assistance from healthcare professionals, including pharmacists, who can educate patients by providing verbal counseling, supported by hands-on guidance and educational materials, and review the skills patients have acquired [13,14]. Automatic upper-arm cuff devices are recommended for self-measurements of BP at home [2]. In this case, the pharmacist could help the patient select the most appropriate BP monitor and cuff, considering the cost, ease of use, or existing comorbidities, such as Parkinson disease, cardiac arrhythmias, or visual disturbances, which can affect the BP measurement procedure. At-home BP measurements, if properly performed, are relatively cheap, useful for long-term self-monitoring, improve patient adherence to HTN treatment, and reduce costs to the health care system [5].
Pharmacists have already been actively involved in many for regarding health promotion and BP measurement. For example, “May Measurement Month (MMM)” is an annual global BP measurement charity campaign. Physicians and other health professionals, including pharmacists, participate in this campaign to raise awareness of BP and HTN at the individual and population levels [15]. The benefits of BP checks performed by pharmacists include accessibility and convenience for patients, reduction of health care costs, and the ability to screen untreated individuals and track diagnosed and hypertensive patients [16,17].
A pharmacist can estimate an individual’s 10-year risk for fatal and nonfatal cardiovascular events (eg, myocardial infarction and stroke risk can be estimated using the updated SCORE algorithms – SCORE2 and SCORE2-OP). Both algorithms were introduced in the 2021 Guidelines for the Prevention of Cardiovascular Disease in Clinical Practice [1] and were proposed for individuals aged 40–69 years and above 70 years of age. Estimation of an individual’s 10-year risk of CVD events requires selection of the right sex, smoking status, nearest age, non-HDL-C, and systolic blood pressure (SBP) values from the risk table. Algorithms were calibrated to 4 groups of countries (low, moderate, high, and very high CVD risk). Poland and some Eastern European countries (Albania, Bosnia and Herzegovina, Croatia, the Czech Republic, Estonia, Hungary, Kazakhstan, and Slovakia), which were classified as high-risk countries [1]. Identification of the correct country cluster should entail a further selection of variables contributing to an individual patient’s overall CVD risk [18].
General Principles and Techniques of BP Measurements
Detailed equipment requirements and procedures of BP measurements have been discussed extensively [2,5]. For the purposes of this narrative review, only a few important aspects related to at-home BP or CPBP measurements are discussed.
BP measurements should be performed in an examination room, pharmaceutical care room, or other quiet place that ensures comfortable (room) temperature and makes the patient feel safe. It should be equipped with a comfortable chair with a backrest (made of hygienic and disinfectable material), which allows a comfortable posture [5]. There should also be a table at which patients can sit and rest their arms without any muscle tension. The table height should allow positioning the mid-arm at heart level (a height-adjustable table is preferred).
The equipment could also include a tape measure for measuring the circumference of the arm and a set of cuffs of different sizes from which patients can choose a cuff that correctly fits their arm circumference according to the instructions for that device [5]. Electronic (oscillometric) semi-automatic or automatic, upper-arm cuff devices with automated storage, or with mobile phone, personal computer, or internet link connection, enabling data transfer, are preferred. These devices should be certificated by the European Society of Hypertension (EAS). A list of validated blood pressure monitors is available at https://www.stridebp.org/ or https://dobrzemierze.pl. The latest models have been equipped with an additional option to screen patients for atrial fibrillation. The BP monitors should be calibrated according to the manufacturer’s recommendations at least once every 2 years [5,19].
The correct cuff size (from S to XL) is required to determine accurate BP readings. Therefore, it should be selected appropriately according to the device instructions. A cuff that is too small can overestimate readings of BP and a cuff that is too large can underestimate readings. When fitted correctly, with room for 1–2 fingers under the cuff, it should exert the same tightness at the top and bottom edges. They should be kept clean, as recommended by the manufacturer [5,19].
Community Pharmacy BP Measurement
In the current literature, CPBP readings are considered useful for screening untreated individuals and supporting patients treated with HTN in their self-monitoring. Use of non-validated devices, inappropriate cuff size, and improper conditions can limit the accuracy of measurements. Pharmacists need to consider several factors when measuring BP [5]. Patients should be seated comfortably, with the back supported by a chair, with legs uncrossed and feet flat on the floor, in a quiet environment. The patient should refrain from smoking, exercise, and consuming caffeine, alcohol, or food for 30 minutes before measurement. They should also refrain from activities such as taking a shower (bath) and house cleaning. Before a measurement, the patient should avoid taking any medication that lowers/increases BP. Conditions such as pain, fever, nervousness, and malaise might also affect measurements and these should be mentioned in the patient diary. The patient should remain seated and relaxed for 5 minutes before measurement, and should not talk during and between BP measurements [2,5,18].
The patient’s bare arm is recommended to rest on a table with the mid-arm at the heart level, preferably about 2 cm above elbow flexion so that the cable runs along the inside of the elbow. For some devices, the manufacturer recommends the measuring sensor be specifically placed (eg, on the forearm) [2,5,18–20].
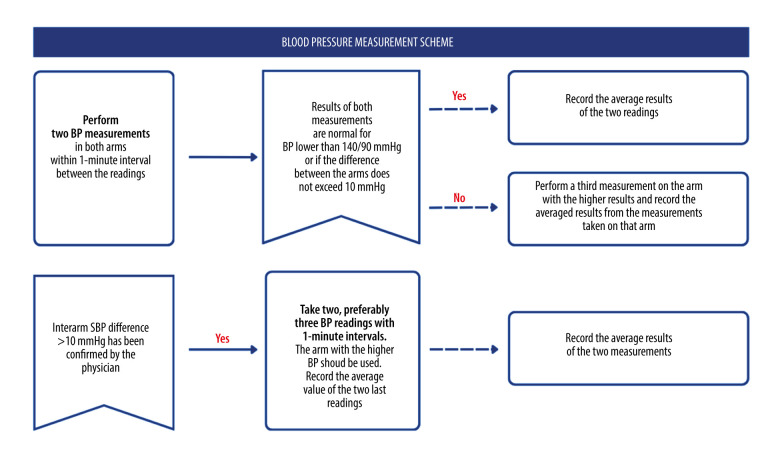
According to the current international guidelines, 2 measurements should be taken within a 1-minute interval in both arms [2]. If BP is below 140 mmHg SBP and 90 mmHg DBP, the average of these 2 readings should be recorded. If one of the results is at least 140 mmHg (SBP) or 90 mmHg (diastolic blood pressure, DBP), the third measurement should be taken in the arm with a higher BP reading, with the average of the last 2 readings. The same procedure concerns inter-arm SBP difference exceeding 10 mmHg [5]. If the inter-arm SBP difference (>10 mmHg) has been already confirmed with repeated measurements by the physician, the arm with the higher BP should be used. The result should be recorded in the patient’s diary. An inter-arm blood pressure difference may indicate hypertensive patients at increased risk of cardiovascular events, and is associated with a shorter survival time or a new cardiovascular event [21]. Thereby, detection of such difference would allow more effective targeting of resources in preventive strategies. Unless otherwise recommended by the physician, 2 BP measurements made with a 1-minute interval should be taken for 7 days before each office visit (morning and evening, before drug intake and before meals) [18–20] (Figure 1).
Figure 1.
The blood pressure measurement in community pharmacy. SBP – systolic blood pressure (Canva Pro).
Screening for Patients with Undiagnosed HTN
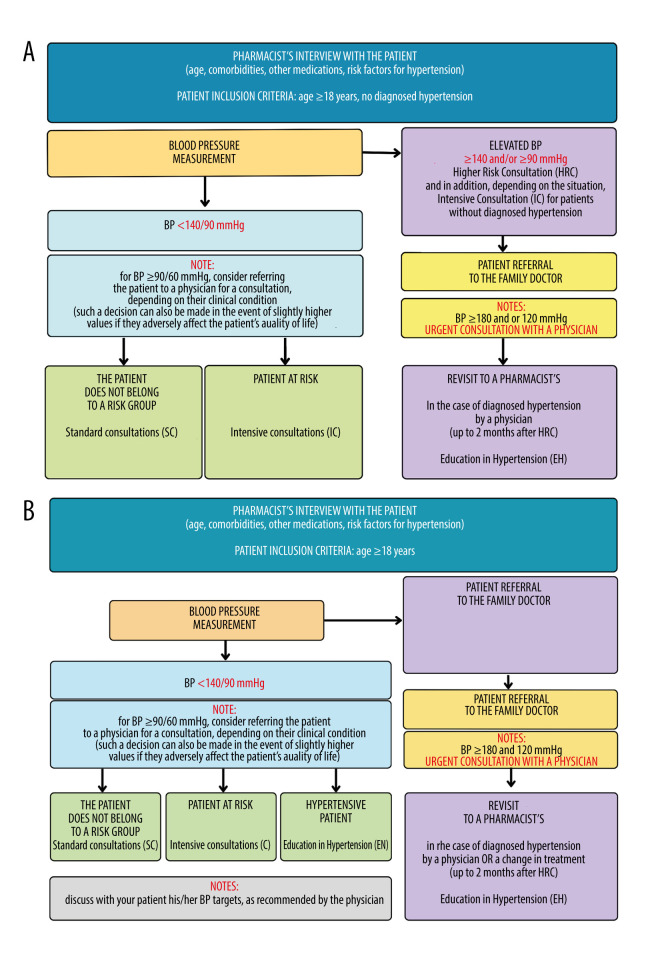
According to the current worldwide guidelines, in individuals without HTN, intervals for repeated BP measurement should be scheduled depending on the BP level and cardiovascular risk; annual follow-up is recommended, especially in adult patients at increased risk of HTN (eg, subjects with high-normal BP, overweight, or obesity) [2]. Professional advice about this regular control provided by a pharmacist is an important component of patient care. To determine risk factors for HTN, the pharmacist could interview patients to determine age, list of medications previously and currently taken, and comorbidities [17]. Figure 2A proposes a procedural scheme for screening for HTN in community pharmacy, according to previous evaluations of undiagnosed subjects [14,22]. For each of the scenarios described below, education should be tailored to the individual patient. During such screening, if the measured BP value is within the normal range (<140/90 mmHg) and the patient has no risk factors, it is useful to educate the patient about proper lifestyle and prevention of HTN (eg, diet, physical activity). If the determined BP value is normal but the patient has certain risk factors (eg, obesity, family history, or dyslipidemia), education could be expanded to include more detailed information and recommendations considering the identified risk factors. For example, if patients smoke cigarettes, the pharmacist could inform them that smoking increases the risk of chronic coronary syndromes and strokes, and contributes to development of peripheral artery disease. Then, an additional consultation with a pharmacist or physician about the tailored method of addiction treatment would support patients in quitting smoking. It would be advisable to inform patients and provide intensive counseling about benefits of smoking cessation for both smokers and those around them who are exposed to secondhand smoke [2,23].
Figure 2.
Detection of increased blood pressure in patients without diagnosed hypertension (A); in all patients (B) during community pharmacy blood pressure (CPBP) measurement – based on Waszyk-Nowaczyk et al (2020) [14]. SC – standard counseling session*; IC – intensive counseling session**; HRC – high-risk consultation***; HE – education in hypertension****. * It involves patient education about proper lifestyle and HTN prevention (eg, diet, physical activity). ** It might be expanded to include more detailed information considering the identified risk factors and lifestyle modification. Such advice should be tailored to the individual patient. For example, smokers should be informed that tobacco smoking is the single largest preventable cause of death, and is a significant risk factor of cardiovascular disease; they should also be encouraged and counseled regarding smoking cessation. *** If the average reading obtained from the measurements is at least 140 mmHg (systolic blood pressure, SBP) and/or 90 mmHg (diastolic blood pressure, DBP), the pharmacist can qualify the patient for a HRC with IC, bearing in mind possible development of HTN, as well as discussing risk factors for the disease. **** It would be valuable to tailor the pharmacist-led education to an individual patient with diagnosed hypertension and include information on whether the therapeutic targets set by the attending physician have been met. Education about healthy lifestyle, adherence to the doctor’s recommendations, or proper techniques of taking BP measurement could be also provided if needed.
While screening for HTN in a community pharmacy, a patient with BP 90/60 mmHg or lower should be advised to consult a physician. This is especially important if the patient demonstrates symptoms such as weakness, dizziness, or nausea. If needed, first aid should be given [18].
Average readings such as at least 140 mmHg SBP and/or 90 mmHg DBP can suggest a need to seek high-risk consultation (HRC) accompanied by a discussion of risk factors for the disease due to possible development of HTN [14,22]. During the consultation, it would be advisable to recommend patients to make an appointment with their family doctor or a specialist within the next 3 weeks [14,22]. In some situations, a BP reading of 135/85 mmHg indicates masked HTN [2], which may warrant referral to a physician. Finally, the pharmacist could play a useful role in patient education about potential effects of certain medications and dietary supplements, which can lead to increased BP [23].
If, during the screening procedure, the patient demonstrates SBP ≥180 mmHg and DBP ≥120 mmHg, the pharmacist should promptly contact the patient’s family physician or specialist to arrange an urgent medical consultation due to elevated BP. This also concerns pregnant women, if BP values reach or exceed 160 mmHg for SBP and/or 110 mmHg for DBP. Such results or symptoms indicate potential development of preeclampsia. In such situations, according to the clinical recommendations, the patient should be referred to the hospital [18].
In accordance with the Polish Society of Hypertension guidelines, patients aged 80 and above can be referred to a doctor if their BP values reach or exceed 160/90 mmHg [18].
Management of Treated Hypertensive Patients in Community Pharmacy
CPBP readings can be also useful for treated hypertensive patients. Figure 2B shows a proposal for the procedural scheme for conducting a control measurement of BP, which could be addressed to patients without a diagnosed HTN (section above) and those already receiving anti-hypertensive treatment. In the latter case, the pharmacist can conduct a basic interview and perform a control measurement of arterial BP following the current guidelines of the Polish Society of Hypertension, along with providing education, if needed [4,18,22]. When the values are below the normal range (<140/90 mmHg), pharmacists could provide hypertension education (HE). Educational material tailored to the individual patient would support such consultation, and it may concern healthy lifestyle, adherence to the doctor’s recommendations, or proper performance of BP measurement. The pharmacist can also verify whether the therapeutic targets set by the attending physician have been met, including achieving the target BP values established in a consultation meeting with the doctor. This is especially important for patients with additional chronic conditions like diabetes or kidney disease [2,18].
For BP 90/60 mmHg or lower, patients can be referred for a medical consultation, depending on their clinical condition (eg weakness, dizziness, nausea). Asymptomatic patients with confirmed HTN could receive education on a healthy lifestyle and proper BP management. Particular attention could be given to the medications the patient is taking, especially anti-hypertensive drugs, to ensure they do not excessively lower BP [18]. When the values are above the normal range (≥140/90 mmHg) for patients already diagnosed with HTN, it would be valuable to raise patient awareness about the risks associated with not initiating treatment or poorly controlled BP (eg, general health, quality of life). When the patient’s BP reaches at least the level of 180 mmHg (SBP) and/or 120 mmHg (DBP), the pharmacist can contact the patient’s family doctor or a specialist to arrange an urgent medical consultation, or, depending on the patient’s condition, call the Emergency Medical Team [2]. In the event of elevated blood pressure, the pharmacist may also check if the patient has been correctly taking the appropriate medication if it has been prescribed previously by a physician [2].
In each of the described situations (high or low BP readings in the patient), the pharmacist could complete and submit a report to the doctor. Pharmacist could also schedule the next appointment within 2 months of the previous visit to the pharmacy if the doctor has introduced some treatment modifications [14,22]. During this meeting pharmacist might provide instructions how to use newly prescribed medications and offer BP self-monitoring training with the use of educational materials, like self-monitoring diary to record BP measurement results if needed (hypertension education, HE). Additionally, the patient may be enrolled in pharmaceutical care services such as “New Medicine Service” or “Medication Use Review” [24–26] (Table 1).
Table 1.
Take-home messages.
| Elevated BP is the biggest single contributing risk factor for global mortality |
| Regular BP monitoring is crucial for everyone, including individuals without diagnosed HTN and those already undergoing anti-hypertensive treatment |
| Screening for patients with undiagnosed HTN in community pharmacy would increase the number of adult participants who are regularly getting their BP monitored |
| CPBP readings can be also useful for treated hypertensive patients; it is crucial to use a validated device and appropriate cuff size and to provide appropriate conditions |
| Management of hypertensive patient could include pharmacist-led education about healthy lifestyle habits, analysis of medications for potential impacts on BP, and ensuring adherence to therapeutic targets set by physicians |
| When the values are above the normal range (≥140/90 mmHg), the patient should be made aware of risks associated with not initiating treatment or poorly controlled BP |
| If the patient’s BP reaches at least the level of 180 mmHg (SBP) and/or 120 mmHg (DBP), the pharmacist can contact the patient’s family doctor or a specialist to arrange an urgent medical consultation, or, depending on the patient’s condition, call the Emergency Medical Team |
| BP readings below 90/60 mmHg require immediate attention, especially if accompanied by symptoms like weakness or dizziness |
| After the physician diagnoses the HTN and initiates tailored intervention, follow-up appointment with pharmacists could ensure continued education on medication usage and proper BP self-monitoring |
BP – blood pressure; CPBP – community pharmacy blood pressure; DBP – diastolic blood pressure; HTN – hypertension; SBP – systolic blood pressure.
Future Directions
Community pharmacists taking an active role in managing blood pressure hold significant potential to enhance HTN outcomes across entire populations. This potential is particularly amplified when pharmacists engage in collaborative efforts with other members of the healthcare community through interdisciplinary activities. This holistic approach to patient health can coordinate interventions that address pharmacological and non-pharmacological aspects of HTN management. Personalized care approaches to blood pressure management and utilizing patient-specific factors such as demographics, comorbidities, and lifestyle habits can make interventions and treatment plans effectively tailored. Such interventions should be widely implemented, being supported by further guidelines for collaborative practice between physicians and pharmacists.
Conclusions
The developed ready-made schemes of procedures for patients with different blood pressure measurement results ensure a uniform standard of services provided by pharmacists. Involvement of a pharmacist in measuring BP can help identify patients with undiagnosed HTN. This gives an opportunity to provide such patients with medical care and initiate treatment, and also facilitates effective maintenance of BP goals in hypertensive subjects. Together with patient education on associated risk factors, drug therapies, or secondary lifestyle changes, CPBP measurement is an element of health prevention. Such an approach might provide real help for patients and ease the burden on the health care system. Several reports support the clinical relevance of SBP reduction by 5 mmHg [9], and there is a great need to conduct further studies to assess monetary savings for Polish public health that might result from such a pharmacist-led consultation.
Footnotes
Conflict of interest: None declared
Declaration of Figures’ Authenticity: All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Visseren FLJ, Mach F, Smulders YM, et al. ESC National Cardiac Societies; ESC Scientific Document Group. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–37. doi: 10.1093/eurheartj/ehab484. [DOI] [PubMed] [Google Scholar]
- 2.Mancia G, Kreutz R, Brunström M, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA) J Hypertens. 2023;41(12):1874–2071. doi: 10.1097/HJH.0000000000003480. [DOI] [PubMed] [Google Scholar]
- 3.Niklas A, Flotyńska A, Puch-Walczak A, et al. Prevalence, awareness, treatment and control of hypertension in the adult Polish population – Multi-center National Population Health Examination Surveys – WOBASZ studies. Arch Med Sci. 2018;14(5):951–61. doi: 10.5114/aoms.2017.72423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Global report on hypertension: The race against a silent killer. Geneva: 2023. Available from: https://www.who.int/publications/i/item/9789240081062. [Google Scholar]
- 5.Stergiou GS, Palatini P, Parati G, et al. European Society of Hypertension Council and the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39(7):1293–302. doi: 10.1097/HJH.0000000000002843. [DOI] [PubMed] [Google Scholar]
- 6.Brouwers S, Sudano I, Kokubo Y, Sulaica EM. Arterial hypertension. Lancet. 2021;398(10296):249–61. doi: 10.1016/S0140-6736(21)00221-X. [DOI] [PubMed] [Google Scholar]
- 7.Cheema E, Sutcliffe P, Singer DR. The impact of interventions by pharmacists in community pharmacies on control of hypertension: A systematic review and meta-analysis of randomized controlled trials. Br J Clin Pharmacol. 2014;78(6):1238–47. doi: 10.1111/bcp.12452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakanishi M, Mizuno T, Mizokami F, et al. Impact of pharmacist intervention for blood pressure control in patients with chronic kidney disease: A meta-analysis of randomized clinical trials. J Clin Pharm Ther. 2021;46(1):114–20. doi: 10.1111/jcpt.13262. [DOI] [PubMed] [Google Scholar]
- 9.Treciokiene I, Postma M, Nguyen T, et al. Healthcare professional-led interventions on lifestyle modifications for hypertensive patients – a systematic review and meta-analysis. BMC Fam Pract. 2021;22(1):63. doi: 10.1186/s12875-021-01421-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Milosavljevic A, Aspden T, Harrison J. Community pharmacist-led interventions and their impact on patients’ medication adherence and other health outcomes: A systematic review. Int J Pharm Pract. 2018;26(5):387–97. doi: 10.1111/ijpp.12462. [DOI] [PubMed] [Google Scholar]
- 11.Santschi V, Wuerzner G, Pais B, et al. Team-based care for improving hypertension management: A pragmatic randomized controlled trial. Front Cardiovasc Med. 2021;8:760662. doi: 10.3389/fcvm.2021.760662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carey RM, Wright JT, Jr, Taler SJ, Whelton PK. Guideline-driven management of hypertension: An evidence-based update. Circ Res. 2021;128(7):827–46. doi: 10.1161/CIRCRESAHA.121.318083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dymek J, Gołda A, Polak W, et al. Effect of education for hypertensive patients with correctly performed Self-Blood Pressure Monitoring (SBPM) Pharmacy. 2019;7(3):75. doi: 10.3390/pharmacy7030075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waszyk-Nowaczyk M, Guzenda W, Plewka B, et al. Screening services in a community pharmacy in Poznan (Poland) to increase early detection of hypertension. J Clin Med. 2020;9(8):2572. doi: 10.3390/jcm9082572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beaney T, Wang W, Schlaich MP, et al. Global blood pressure screening during the COVID-19 pandemic: Results from the May Measurement Month 2021 campaign. J Hypertens. 2023;41(9):1446–55. doi: 10.1097/HJH.0000000000003488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barrett R, Hodgkinson J. Quality evaluation of community pharmacy blood pressure (BP) screening services: An English cross-sectional survey with geospatial analysis. BMJ Open. 2019;9(12):e032342. doi: 10.1136/bmjopen-2019-032342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tompson AC, Fleming SG, Heneghan CJ, et al. Current and potential providers of blood pressure self-screening: A mixed methods study in Oxfordshire. BMJ Open. 2017;7(3):e013938. doi: 10.1136/bmjopen-2016-013938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tykarski A, Filipiak KJ, Januszewicz A, et al. [The rule of management of hypertension – 2019]. Nadciśnienie Tętnicze w Praktyce. 2019;5(1):1–86. Available from: https://journals.viamedica.pl/nadcisnienie_tetnicze_w_praktyce/article/view/64385 [in Polish] [Google Scholar]
- 19.Vischer AS, Burkard T. Principles of blood pressure measurement – current techniques, office vs ambulatory blood pressure measurement. Adv Exp Med Biol. 2017;956:85–96. doi: 10.1007/5584_2016_49. [DOI] [PubMed] [Google Scholar]
- 20.Clark CE, Taylor RS, Shore AC, Campbell JL. Prevalence of systolic inter-arm differences in blood pressure for different primary care populations: Systematic review and meta-analysis. Br J Gen Pract. 2016;66(652):e838–e47. doi: 10.3399/bjgp16X687553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark CE, Campbell JL, Powell RJ. The interarm blood pressure difference as predictor of cardiovascular events in patients with hypertension in primary care: Cohort study. J Hum Hypertens. 2007;21(8):633–38. doi: 10.1038/sj.jhh.1002209. [DOI] [PubMed] [Google Scholar]
- 22.Pongwecharak J, Treeranurat T. Screening for pre-hypertension and elevated cardiovascular risk factors in a Thai community pharmacy. Pharm World Sci. 2010;32(3):329–33. doi: 10.1007/s11096-010-9373-1. [DOI] [PubMed] [Google Scholar]
- 23.Waszyk-Nowaczyk M, Jasińska-Stroschein M, Drozd M, et al. 2023. Available from: https://nowy-lek.pl/wytyczne/ [in Polish]
- 24.Stewart D, Whittlesea C, Dhital R, et al. Community pharmacist led medication reviews in the UK: A scoping review of the medicines use review and the new medicine service literatures. Res Social Adm Pharm. 2020;16(2):111–22. doi: 10.1016/j.sapharm.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 25.Jasińska-Stroschein M, Dymek J, Drozd M, et al. An evaluation of written materials for supporting hypertensive patient education and counselling when performing a new medicine service in Poland. BMC Med Educ. 2024;24(1):521. doi: 10.1186/s12909-024-05523-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waszyk-Nowaczyk M, Jasińska-Stroschein M, Drozd M, et al. A. Guidelines for performing New Medical Pharmaceutical Service. Position of the Team for the Standardization of Pharmaceutical Care of the Chamber of Pharmacy and the Polish Pharmaceutical Society. 2024. Available from: https://opiekafarmaceutyczna.nia.org.pl [in Polish]