Abstract
Background:
The United States continues to experience unprecedented rates of overdose mortality and need to identify effective policies or practices that can be implemented. This study aims to measure the prevalence, frequency, timing, and rate of touchpoints that occurred prior to a fatal overdose where communities might intervene.
Methods:
In collaboration with Indiana state government, we conducted record-linkage of statewide administrative datasets to vital records (January 1, 2015, through August 26, 2022) to identify touchpoints (jail booking, prison release, prescription medication dispensation, emergency department visits, and emergency medical services). We examined touchpoints within 12-months prior to a fatal overdose among an adult cohort and explored variation over time and by demographic characteristics.
Results:
Over the 92-month study period there were 13,882 overdose deaths (89.3% accidental poisonings, X40-X44) in our adult cohort that were record-linked to multiple administrative datasets and revealed nearly two-thirds (64.7%; n=8,980) experienced an emergency department visit, the most prevalent touchpoint followed by prescription medication dispensation, emergency medical services responses, jail booking, and prison release. However, with approximately 1 out of every 100 returning citizens dying from drug overdose within 12-months of release, prison release had the highest touchpoint rate followed by emergency medical services responses, jail booking, emergency department visits, and prescription medication dispensation.
Conclusion:
Record-linking administrative data from routine practice to vital records from overdose mortality is a viable means of identifying where resources should be situated to reduce fatal overdose, with potential to evaluate the effectiveness of overdose prevention efforts.
Keywords: nonfatal overdose, incarceration, emergency medical services, emergency department, prescription opioid dispensation
1. Introduction
Overdose deaths continue to increase across the United States, rising 15% from 2020 to 2021 (Spencer et al., 2022; Palamar et al., 2022). In the last decade, underlying substances in drug overdose deaths have shifted from prescription analgesic medications to illicit fentanyl, a synthetic opioid 50 to 100 times more potent than morphine (Ciccarone, 2021; Volkow & Blanco, 2020). Illicit fentanyl is now implicated in upwards of 66 percent of fatal overdose deaths (Centers for Disease Control and Prevention, 2022), driven by the presence of fentanyl in the illicit drug supply (Kilmer et al., 2022; Ray et al., 2017; Zibbell et al., 2022). Criminalization of opioids and persons with opioid use disorder (OUD) has contributed to rising overdose deaths (Davis et al., 2019). Further, the introduction of fentanyl into the illicit drug market has produced dramatic demographic shifts in overdose deaths, with rising fatal overdose rates among Black, Indigenous, and People of Color (Furr-Holden et al., 2021). While historical trends show opioids and stimulants alternating in periods of use, current patterns suggest co-use among these substances along with the presence of fentanyl into other substances (Hoots et al., 2020; Hughto et al., 2022; Strickland et al., 2019) in turn, marking the fourth wave of the drug epidemic.
There has been widespread analysis of the administrative records that are collected as part of routine practice to better understand and respond to the overdose crisis. These administrative data have included opioid prescribing or dispensing (Guy et al., 2017; Lowder et al., 2020; Volkow et al., 2011), calls for emergency services (McLeod et al., 2021; Ray et al., 2018; Stoové et al., 2009), patient medical records (Di Rico et al., 2018; Nechuta et al., 2018; Olfson et al., 2018; Stoové et al., 2009), and encounters with criminal-legal systems (Keen et al., 2020; O’Connor et al., 2022; Ranapurwala et al., 2018; Ray, Hedden, et al., 2022; Shefner et al., 2020; Victor et al., 2021). For example, many jurisdictions now use online dashboards on the time and location of overdose and poisoning calls for emergency medical services (EMS) to surveil trends and target outreach and overdose response activities (Anderson et al., 2019; Dasgupta & Kapadia, 2022; Marshall et al., 2017; Wu et al., 2020). Researchers have also geographically aggregated these administrative data sources to develop predictive models of overdose mortality with several studies integrating multiple jurisdictional data sources to forecast overdose trends (Marks et al., 2021; Peters et al., 2020) and utilized individual-level record linkage to understand the trajectory of system involvement leading to an overdose death (Lowder et al., 2020; Victor et al., 2021). Larochelle and colleagues worked with the Massachusetts Department of Public Health to record-link multiple administrative datasets to identify “touchpoints” or “opportunities for individuals at high-risk of opioid overdose death in order to deliver harm-reduction services to them and engage them in evidence-based treatment” (Larochelle et al., 2019).
The current study uses a similar framework with researchers partnered with Indiana state government to examine a cohort of adult overdose decedents from January 1, 2015, through August 26, 2022, providing a more recent analysis, in a post-fentanyl era, that builds on Larochelle and colleague’s prior work. We record-link five statewide administrative datasets to overdose deaths to identify touchpoints that occurred 12-months prior to fatal overdose. Touchpoints include jail booking, prison release, prescription medication dispensation, emergency department (ED) events, and EMS responses. Following a description of the overdose decedent’s demographic characteristics we (1) detail the prevalence, frequency, timing, and rate of observed touchpoints among all events, (2) explore trends in touchpoints over the seven-year period, and (3) examine variation by decedent demographic characteristics.
2. Methods
2.1. Data Sources
We conducted a retrospective cohort study of drug overdose deaths in Indiana that occurred from January 1, 2015, through August 26, 2022 (date of data acquisition), using mortality data collected via death certificates submitted by county coroners to the Indiana Department of Health Division of Vital Records that include ICD (International Classification of Diseases) codes for underlying cause of death (Indiana Department of Health, 2023). Research suggests that overdose deaths in Indiana are predominately opioid-related, specifically illicitly manufactured fentanyl (del Pozo et al., 2023; Phalen et al., 2018; Ray et al., 2017, 2020); however, current record-linkage efforts aimed at doing so in near real-time and one of the items sacrificed was the ability to look at specific substances contributing to the overdose death. Therefore, we examine cause of death codes for all accidental poisoning (X40-X44), intentional poisoning (X60-X64), undetermined intent (Y10-Y14), and assault by drugs (X85), and only include events where the decedent was a resident of Indiana. There were 13,968 events during the 92-month period (January 1, 2015, through August 26, 2022) with one case missing demographic data and 85 cases persons under 18 years of age and not able to be detected within linked administrative data resulting in a final analytic sample of 13,882 overdose deaths.
2.2. Variables
Administrative data sources were record-linked to overdose deaths using probabilistic matching to generate five touchpoints: (1) jail booking, (2) prison release, (3) prescription medication dispensation, (4) ED events, and (5) EMS responses. Indiana Management Performance Hub is a state agency tasked with integrating administrative data sources to inform state policy and record-links persons with a probabilistic matching algorithm that utilizes string similarity to make use of probabilities for deciding when a given pair of personally identifiable information (first name, last name, date of birth, social security number, gender, race, and zip code) matches with social security number assigned the largest weight and race and gender the smallest. Information on incarceration touchpoints came from the Indiana State Police Criminal History Repository Information System, which has information on the date of jail booking events, and the Indiana Department of Corrections providing information on prison release. The Indiana Scheduled Prescription Electronic Collection and Tracking Program provided prescription medication dispensation information and includes the date for each time a controlled substance (U.S. Department of Justice, Drug Enforcement Administration, 2023) was dispensed to a patient except for those with less than a 72-hour supply and in-patient pharmacies (Indiana State Government, 2023a). For emergency medical events, information on EMS responses came from pre-hospital emergency ambulatory services that were reported to the Indiana Department of Homeland Security as part of the National EMS Information System (836 IAC 1-1-5) (Indiana Department of Homeland Security, 2023). Finally, information on ED visits came from the Electronic Surveillance System for the Early Notification of Community-Based Epidemics, a syndromic surveillance system managed by the Indiana State Department of Health that requires all non-federal acute care facilities in the state to report information on the patient’s chief complaint or symptoms, age, sex, zip code, date and time of visit, and the hospital visited (410 IAC 1-2.4) (Indiana State Government, 2023b).
Each of these administrative data sources provided information dating back to January 1, 2014, providing at least 12-months prior to death, with touchpoints representing any event identified in these data and not specific to substance use or overdose related events. We looked at the prevalence, frequency, timing, and rate the touchpoint variables. Prevalence is the percentage of total overdose deaths (N=13,882) that were identified as having an event in the linked administrative data in the 12-months prior to death. Frequency is an average of the number of events those with a touchpoint had during those 12-months and timing is the number of days between the most recent event and death. Importantly, not all events are similarly experienced (e.g., residents are more likely to have a medication dispensed than be incarcerated in prison) so to calculate the rate researchers were provided with yearly counts of all events (January 1, 2015 through December 31, 2021 but excluding January 1, 2022 through August 26, 2022) in the administrative data sources from which touchpoints are determined from. Rate is then calculated as the total number of touchpoints divided in the full year time range (2015–2021) divided by the total number of events during that period then multiplied by 100,000 to standardize allowing for cross-population comparison.
2.3. Analytic Plan
Our analysis began with demographic characteristics and overdose death classifications for decedents during the study period, and then the prevalence, frequency, timing, and rate for the five touchpoints. Following this we look at trends in the prevalence and rate of touchpoints over the study period and then examine variation by demographic characteristics. We used bivariate statistics (t-test and chi-square) to explore variation in prevalence by decedent demographic characteristics. All analyses were conducted inside the MPH Enhanced Research Environment (Indiana Management Performance Hub, 2023), a hardened environment in which no data or results can be accessed without approval following staff review export to ensure laws and security protocols are met, with IRB determining the study not human research (#00021890).
3. Results
3.1. Adult Cohort of Overdose Decedents
The sample of 13,882 overdose deaths contained 89.3% coded as accidental poisonings, followed by 6.3% as poisoning by exposure, 4.4% intentional poisoning, and 0.1% as assault by drugs (Table 1). The average age at death was 41.4 years (standard deviation [SD]=13.0, median=40.0, range 18–94). Nearly two-thirds of overdose decedents were male (65.2%), and the majority were coded as White/Caucasian (84.1%), followed by Black/African American (12.2%) and Hispanic/Latino (2.2%). It is also worth noting that while there were slight reductions in overdose deaths in 2018 and 2019, trends were consistent with national findings of increased overdose during the study period (Figure 1).
Table 1:
Overdose decedent characteristics, Indiana, January 1, 2015 – August 26, 2022
| Mean | SD | |
|---|---|---|
| Age in years | 41.43 | 13.03 |
| Race-Ethnicity Categories | N | Percent |
| American Indian/Alaska Native/Pacific Islander | 20 | 0.1% |
| Asian | 34 | 0.2% |
| Black/African American | 1,700 | 12.2% |
| Hispanic/Latino | 312 | 2.2% |
| White/Caucasian | 11,676 | 84.1% |
| Multiple racial categories | 52 | 0.4% |
| Other/Unknown racial category | 88 | 0.6% |
| Gender | ||
| Female | 4,831 | 34.8% |
| Male | 9,051 | 65.2% |
| Overdose ICD Categorization | ||
| X40-X44 (accidental poisoning) | 12,391 | 89.3% |
| X60-X64 (intentional poisoning) | 610 | 4.4% |
| Y10-Y14 (undetermined intent) | 871 | 6.3% |
| X85 (assault by drugs) | 10 | 0.1% |
Note: N=13,882.
Figure 1:

Overdose deaths by year in Indiana, January 1, 2015—December 31, 2021
Notes: N=12,858 and includes January 1, 2015, through December 31, 2022. Includes all overdose ICD codes in Table 1. Data were not available to do monthly year-to-date analysis; however, between January 1, 2022, and August 26, 2022, there were an additional 1,024 overdose events.
3.1. Describing Observed Touchpoints
In Table 2 we provide the prevalence, frequency, timing, and rate for each of the available touchpoints. Nearly two-thirds (64.7%; n=8,980) of overdose decedents had an ED event in the 12-months prior to death, the most prevalent touchpoint, with prescription medication dispensation most frequent (12.6 dispensations in the year prior) and recent (93.8 days on average prior to death). With an average of 11,658 prison releases per year (2015–2021) the rate of this touchpoint at 560.0 per 100,000 prison releases was by far the highest, approximately 7 times higher than EMS response rate (78.4/560.0) and 8 times higher than jail booking (69.8/560.0), while the prescription medication touchpoint had the lowest rate at 8.1 per 100,000 dispensations followed by ED events at 26.8 per 100,000 events.
Table 2:
Touchpoints in the 12-months prior to fatal overdose in Indiana
| Prevalence | Frequency | Days to last event | Prevalence 2015–2021 | Total events 2015–2021 | Average events per year 2015–2021 | Rate per 100,000 events | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Percent | Mean | S.D. | Mean | S.D. | |||||
| Jail booking | 3,628 | 26.1% | 1.7 | 1.09 | 151.1 | ## ## # |
3,374 | 48,33,697 | 6,90,528 | 69.8 |
| Prison release | 477 | 3.4% | 1.1 | 0.28 | 156.4 | ## ## # |
457 | 81,606 | 11,658 | 560.0 |
| Prescription medication dispensation | 8,167 | 58.8% | 12.8 | 12.56 | 71.3 | 93.81 | 7,610 | 9,35,61,676 | 1,33,65,954 | 8.1 |
| Emergency department event | 8,980 | 64.7% | 3.5 | 4.35 | 96.3 | 99.46 | 8,348 | 3,12,00,056 | 44,57,151 | 26.8 |
| Emergency medical services response | 5,148 | 37.1% | 2.6 | 3.37 | 96.4 | ## ## # |
4,642 | 59,18,958 | 8,45,565 | 78.4 |
Notes: N=13,882. Jail is based on the date from booking into the facility while prison is time from release; dispensations refer to each unique patient interaction where medications were obtained; emergency medical events are based on the date of that encounter; DOC categorizes a release to parole as a release, so our data likely includes individuals under supervision though not specifically identified as such. Prevalence is calculated as the touchpoint N divided by the total number of overdose deaths (13,882). Rate is the touchpoint N for January 1, 2015, through December 31, 2021, divided by the total number of events from the respective administrative data set for that time frame and multiplied by 100,000.
3.2. Trends in Touchpoints
We looked at trends in the prevalence and touchpoint rates over the seven-year study period. Incarceration touchpoints (jail booking and prison release) remained relatively consistent with prescription medication dispensation decreasing from 71.5% in 2015 to 55.1% in 2021 (Figure 2a). Also notable is the increase in the EMS response touchpoint, from 19.9% in 2015 to 50.8% in 2021. Figure 2b shows trends in touchpoint rates, with prison release increasing from 270.6 per 100,000 in 2015 to 958.0 per 100,000 in 2021, while touchpoints rates for jail booking and ED events increased from 43.7 to 95.0 and 45.7 to 62.8 per 100,000 respectively.
Figure 2:
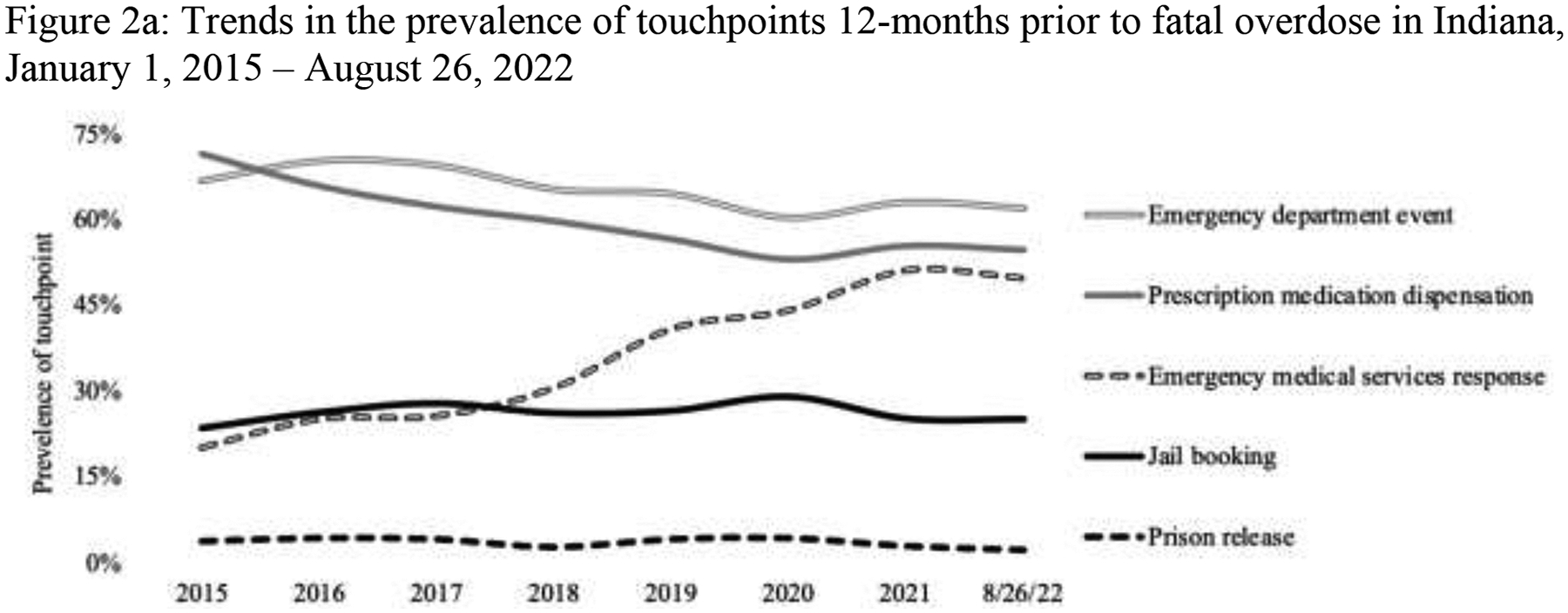

Trends in touchpoints over time
Notes: N=13,882. January 1, 2015, through August 26, 2022. Touchpoints are listed in the order of prevalence among the 1,024 overdose events between January 1, 2022, and August 26, 2022.
Notes: Notes: N=12,858 and includes January 1, 2015, through December 31, 2022. Touchpoints are listed in the order of highest rates for 2021. Rates are calculated by dividing the total number of touchpoint events in that year by the total number of those events in that year.
3.2. Variation in Touchpoints
We also examined variation in touchpoints across demographic measures. Decedents booked in jail and released from prison were younger than those who did not experience these touchpoints (36.2 vs. 43.3 [p<.000] and 37.6 vs. 41.6 [p<.000], respectively), and those dispensed medications older (43.1 vs. 39.0, p<.000). Differences in the EMS response touchpoint were negligible though trending toward younger decedents (41.2 vs. 41.8, p=.008). In looking at a dichotomous measure of gender (female, male) and race-ethnicity (nonwhite, white) we found that men were more likely to have the jail booking (28.4% vs. 21.8%, p<.000) and prison release (4.3% vs. 1.8%, p<.000) touchpoint than females, and nonwhites more likely to have the jail touchpoint than whites (26.5% and 24.1%, p=.018) with no differences in the prison touchpoint. Females were more likely to have the prescription medication touchpoint (70.4% vs. 52.7%, p< .000) than males, along with white decedents more likely (62.3% vs. 40.4%, p<.000) that nonwhite decedents. Females were also more likely to have the ED event touchpoint (71.8% vs. 60.9%, p< .000) and EMS response touchpoint (40.4% vs. 35.3%, p<.000) than males, and whites more likely to have the ED event touchpoint (65.8% and 58.7% respectively, p<.000), than nonwhites with no differences in the EMS response touchpoint.
4. Discussion
An analysis of touchpoints from more than seven years of individual-level record-linked data from multiple statewide administrative datasets identified five touchpoints: jail booking, prison release, prescription medication dispensation, ED events, and EMS responses. Analysis of these touchpoints revealed that ED events as the most prevalent touchpoint, with prescription medication dispensations as the most frequent and recent, and release from prison with the highest touchpoint rate. Over the study period the prevalence of prescription medication dispensations as a touchpoint decreased, with the EMS response touchpoint increasing in both prevalence and rate. There were similar increases in the jail booking touchpoint and extreme increases in the prison release touchpoint; for example, in 2020 approximately 1 out of every 100 returning citizens died from an accidental drug overdose within 12-months of release. Rates of EMS and jail booking were the next highest (about 1 out of a 1,000 and 1 out of 6,000 respectively that same year) and might reflect incarceration following overdose calls for services (Ray, Hedden, et al., 2022). Our analysis also revealed demographic trends in touchpoints with females more likely to experience medical events (prescription medication dispensation, ED events, and EMS responses) and males more likely experience incarceration touchpoints (jail booking and prison release).
Findings reveal opportunities for the implementation of evidence-based interventions to mitigate rising overdose rates which remain largely opioid-related (Ciccarone, 2021; Palamar et al., 2022; Volkow & Blanco, 2020). While national experts call for easier access to methadone (Jones et al., 2022)—a touchpoint we were unable to measure in this study—it remains highly regulated making buprenorphine the front runner for evidence-based medications for OUD (Wakeman et al., 2020). It is critically important that providers create low-barrier options for these medications, particularly in non-traditional settings (Gilbert et al., 2022) and for marginalized populations (Hansen et al., 2013), and recognize that discontinuation of buprenorphine is associated with overdose risk (Glanz et al., 2022). This is especially true in a highly unregulated illicit opioid supply (Ciccarone, 2021; Phalen et al., 2018; Ray et al., 2020), with levels of fentanyl and tolerance unknown to users and suppliers (Carroll et al., 2020). Moreover, for those who are fentanyl dependent, recommended dosing guidelines may not be enough (Selitsky et al., 2022.; Socias et al., 2022) which could prompt the use of unregulated opioids, and reduced treatment retention. Prescribers should consider relaxed concerns about diversion (del Pozo et al., 2020), with research showing buprenorphine diversion at community levels associated with reduced overdose (Clemency et al., 2022; Davis et al., 2021; Hern et al., 2022). Additional consideration should be given when interpreting the prescription medication dispensation touchpoint and the potential for overdose and other drug related harms that come from long-term prescription opioid analgesic treatments being disrupted, often resulting in transitioning to illicit supplies (Gaertner et al., 2022).
Results from the present study highlight also harms associated with criminal-legal system involvement. Seeking opportunities to reduce the role of law of enforcement at overdose events could reduce incarceration (Ray, Hedden, et al., 2022) and remove the risk of overdose after release, where tolerance decreases during incarceration (Fox et al., 2015). Law enforcement agencies might use their discretion in encounters with persons who use drugs as an opportunity to provide referral to treatment and services aimed at overdose prevention (del Pozo et al., 2021). This study also illustrates the importance of assuring that medications for OUD are provided to persons while they are incarcerated with a plan for continued care after leaving carceral settings (Evans et al., 2022; Macmadu et al., 2020; Ray, Victor, et al., 2022). Additionally, they suggest the potential need for immediate induction of buprenorphine following emergency medical services events which could include both the ED (Stewart et al., 2021; Suffoletto & Zeigler, 2020) and following an EMS call for service (Carroll et al., 2023; Carroll et al., 2021). Finally, this analysis also presents opportunities to provide naloxone (the antidote that can reverse opioid-related overdoses) in the community through targeted approaches across the touchpoints identified in these settings. Providing barrier and stigma free naloxone following incarceration, at the scene of emergency medical events and hospital or health care settings, and as part of standard prescribing and dispensation practices, has potential to reduce overdose in the community (Clark et al., 2014).
4.1. Limitations
To conduct this study researchers collaborated with state government around efforts in Indiana aimed at rapidly identifying these touchpoints to inform local policy decisions. Though state governments are increasingly using administrative records to address the ongoing overdose crisis, record-linkage efforts can draw concerns around privacy infringements, profiling, and a lack of informed consent (Volkow et al., 2022). While innovative in its approach, this study does not speak to these concerns. Additionally, this study is limited by the available administrative records monitored by state agencies and because of data security researchers were unable to fully assess data quality or protocols of these records or record-linkage procedures which could impact findings. For example, during the study period the number of unique agencies providing data fluctuated by year which could impact the prevalence of touchpoints; however, this is also one of the reasons that we included the touchpoint rate which would account for some of these changes in the denominator. Future work should examine touchpoints by county and over time which could reveal geographic limitations in the data. This should also include a more thorough analysis on the impact of the COVID-19 pandemic, which is reflected in increased overdoses deaths but beyond the scope of this study to examine the impact on touchpoints and the underlying events (e.g, incarceration, prescription dispensation, emergency medical events). The lack of raw data also limited our ability to detect multiple touchpoints within the same individual over time; therefore, we could not determine if a person who is incarcerated for half a year may be unlikely to have emergency medical events and vice versa. Our analysis also lacks information about the characteristics underlying the touchpoint events; further exploration should focus on analyzing specific types of emergency medical events or criminal charges among these touchpoints. For example, high-risk prescribing such as high dosage, co-prescribing of benzodiazepine, and multiple prescribers may serve as more precise risk factors for overdose (Larochelle et al., 2016, 2019). In a similar way, arrest for a drug-related offenses (such as syringe possession) may indicate higher risk for non-fatal or fatal overdose (Grella et al., 2021; Victor et al., 2021). Finally, we are limited in external validity and generalizability by looking at one US state and touchpoints might be different given state policies. Ideally these touchpoints can inform the implementation of overdose prevention strategies in Indiana and be replicated through additional state efforts to look at policy differences.
5. Conclusion
This study demonstrates state government’s ability to harness multiple administrative data systems to identify overdose touchpoints in near real-time. While limited by the available data, we find that more than one in four overdose decedents were involved in criminal-legal systems in the 12 months prior to death and two-thirds an emergency medical event. The identification of these touchpoints provides an opportunity to bring data to action by providing timely surveillance that can inform the implementation of overdose prevention strategies. Moreover, information on these touchpoints can also be used to evaluate the effectiveness of these efforts. Future efforts should focus on localizing these touchpoints to smaller geographic levels and providing this information to communities assist in overdose prevention efforts.
Figure 3:



Variation in touchpoint prevalence by demographic factors
Notes: N=13,882. January 1, 2015, through August 26, 2022.
Highlights.
Record-linkage between mortality and statewide administrative data identify touchpoints
More than 1 in 4 overdose decedents has criminal justice involvement year prior
Nearly two-thirds had an emergency department visit in the year prior
More than 1 in 3 had emergency medical services engagement in the year prior
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflict declared.
References
- Anderson JA, Demeter N, & Wirtz S (2019). Using the CA Opioid Overdose Surveillance Dashboard to track opioid overdose deaths. Online Journal of Public Health Informatics, 11(1). [Google Scholar]
- Carroll GG, Wasserman DD, Shah AA, Salzman MS, Baston KE, Rohrbach RA, Jones IL, & Haroz R (2021). Buprenorphine field initiation of ReScue treatment by emergency medical services (Bupe FIRST EMS): A case series. Prehospital Emergency Care, 25(2), 289–293. [DOI] [PubMed] [Google Scholar]
- Carroll G, Solomon KT, Heil J, Saloner B, Stuart EA, Patel EY, Greifer N, Salzman M, Murphy E, & Baston K (2023). Impact of Administering Buprenorphine to Overdose Survivors Using Emergency Medical Services. Annals of Emergency Medicine, 81(2), 165–175. [DOI] [PubMed] [Google Scholar]
- Carroll JJ, Rich JD, & Green TC (2020). The protective effect of trusted dealers against opioid overdose in the U.S. The International Journal on Drug Policy, 78, 102695. 10.1016/j.drugpo.2020.102695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2022, May 11). U.S. Overdose Deaths In 2021 Increased Half as Much as in 2020—But Are Still Up 15%. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm
- Ciccarone D (2021). The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Current Opinion in Psychiatry, 34(4), 344–350. 10.1097/YCO.0000000000000717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark AK, Wilder CM, & Winstanley EL (2014). A Systematic Review of Community Opioid Overdose Prevention and Naloxone Distribution Programs. Journal of Addiction Medicine, 8(3), 153–163. 10.1097/ADM.0000000000000034 [DOI] [PubMed] [Google Scholar]
- Clemency BM, Hoopsick RA, Burnett SJ, Kahn LS, & Lynch JJ (2022). Implementing a Novel Statewide Network to Support Emergency Department-initiated Buprenorphine Treatment. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta N, & Kapadia F (2022). The future of the public health data dashboard. American Journal of Public Health, 112(6), 886–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CS, Carr DH, Glenn MJ, & Samuels EA (2021). Legal authority for emergency medical services to increase access to buprenorphine treatment for opioid use disorder. Annals of Emergency Medicine, 78(1), 102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CS, Carr DH, & Samuels EA (2019). Paraphernalia Laws, Criminalizing Possession and Distribution of Items Used to Consume Illicit Drugs, and Injection-Related Harm. American Journal of Public Health, 109(11), 1564–1567. 10.2105/AJPH.2019.305268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Pozo B, Atkins D, Andraka-Christou B, Wightman R, Clark M, Huynh P, & Ray B (2023). Buprenorphine involvement in opioid overdose deaths: A retrospective analysis of postmortem toxicology in Marion County, Indiana, 2015–2021. Drug and Alcohol Dependence Reports, 100131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Pozo B, Krasner LS, & George SF (2020). Decriminalization of Diverted Buprenorphine in Burlington, Vermont and Philadelphia: An Intervention to Reduce Opioid Overdose Deaths. The Journal of Law, Medicine & Ethics: A Journal of the American Society of Law, Medicine & Ethics, 48(2), 373–375. 10.1177/1073110520935353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Pozo B, Sightes E, Goulka J, Ray B, Wood CA, Siddiqui S, & Beletsky LA (2021). Police discretion in encounters with people who use drugs: Operationalizing the theory of planned behavior. Harm Reduction Journal, 18(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Rico R, Nambiar D, Stoové M, & Dietze P (2018). Drug overdose in the ED: a record linkage study examining emergency department ICD-10 coding practices in a cohort of people who inject drugs. BMC Health Services Research, 18(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans EA, Pivovarova E, Stopka TJ, Santelices C, Ferguson WJ, & Friedmann PD (2022). Uncommon and preventable: Perceptions of diversion of medication for opioid use disorder in jail. Journal of Substance Abuse Treatment, 138, 108746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox AD, Maradiaga J, Weiss L, Sanchez J, Starrels JL, & Cunningham CO (2015). Release from incarceration, relapse to opioid use and the potential for buprenorphine maintenance treatment: A qualitative study of the perceptions of former inmates with opioid use disorder. Addiction Science & Clinical Practice, 10(1), 2. 10.1186/s13722-014-0023-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furr-Holden D, Milam AJ, Wang L, & Sadler R (2021). African Americans now outpace whites in opioid-involved overdose deaths: A comparison of temporal trends from 1999 to 2018. Addiction, 116(3), 677–683. 10.1111/add.15233 [DOI] [PubMed] [Google Scholar]
- Gaertner SJ, Krishnasamy VP, Simone PM, & Schuchat A (2022). Leveraging Rapid Response Activities to Build Public Health Capacity: Development of the Opioid Rapid Response Team Model. Health Security, 20(1), 87–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert LR, Starks S, Gray J, Reitzel LR, & Obasi EM (2022). Exploring the provider and organization level barriers to medication for opioid use disorder treatment for Black Americans: A study protocol. Public Health in Practice, 100308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Ostlie E, Scott CK, Dennis ML, Carnevale J, & Watson DP (2021). A scoping review of factors that influence opioid overdose prevention for justice-involved populations. Substance Abuse Treatment, Prevention, and Policy, 16(1), 19. 10.1186/s13011-021-00346-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy GP, Zhang K, Bohm MK, Losby J, Lewis B, Young R, Murphy LB, & Dowell D (2017). Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015. MMWR. Morbidity and Mortality Weekly Report, 66(26), 697–704. 10.15585/mmwr.mm6626a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen HB, Siegel CE, Case BG, Bertollo DN, DiRocco D, & Galanter M (2013). Variation in use of Buprenorphine and Methadone Treatment by Racial, Ethnic and Income Characteristics of Residential Social Areas in New York City. The Journal of Behavioral Health Services & Research, 40(3). 10.1007/s11414-013-9341-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hern HG, Lara V, Goldstein D, Kalmin M, Kidane S, Shoptaw S, Tzvieli O, & Herring AA (2022). Prehospital Buprenorphine Treatment for Opioid Use Disorder by Paramedics: First Year Results of the EMS Buprenorphine Use Pilot. Prehospital Emergency Care, 1–9. [DOI] [PubMed] [Google Scholar]
- Hoots B, Vivolo‐Kantor A, & Seth P (2020). The rise in non-fatal and fatal overdoses involving stimulants with and without opioids in the United States. Addiction. 10.1111/add.14878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughto JM, Gordon LK, Stopka TJ, Case P, Palacios WR, Tapper A, & Green TC (2022). Understanding opioid overdose risk and response preparedness among people who use cocaine and other drugs: Mixed-methods findings from a large, multi-city study. Substance Abuse, 43(1), 465–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [dataset] Indiana Department of Health (2023). Indiana Mortality Report, State and County Data [Data set]. Stats Explorer. https://www.in.gov/health/vital-records/vital-statistics/death-reports/
- Indiana Department of Homeland Security (2023). Emergency Medical Services. https://www.in.gov/dhs/ems/
- Indiana Management Performance Hub (2023). Enhanced Research Environment. https://www.in.gov/mph/projects/enhanced-research-environment/
- Indiana State Government (2023a). What Sort of Information is Collected by INSPECT?. Frequently Asked Questions. https://faqs.in.gov/hc/en-us/articles/115005045347-What-sort-of-information-is-collected-by-INSPECT-
- Indiana State Government (2023b). Syndromic Surveillance. NEDSS Base System (NBS) & Surveillance. https://www.in.gov/health/erc/nedss-base-system-nbs-and-surveillance/syndromic-surveillance/
- Jones CM, Compton WM, Han B, Baldwin G, & Volkow ND (2022). Methadone-involved overdose deaths in the US before and after federal policy changes expanding take-home methadone doses from opioid treatment programs. JAMA Psychiatry, 79(9), 932–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keen C, Young JT, Borschmann R, & Kinner SA (2020). Non-fatal drug overdose after release from prison: A prospective data linkage study. Drug and Alcohol Dependence, 206, 107707. 10.1016/j.drugalcdep.2019.107707 [DOI] [PubMed] [Google Scholar]
- Kilmer B, Pardo B, Pujol TA, & Caulkins JP (2022). Rapid changes in illegally manufactured fentanyl products and prices in the United States. Addiction, 117(10), 2745–2749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larochelle MR, Bernstein R, Bernson D, Land T, Stopka TJ, Rose AJ, Bharel M, Liebschutz JM, & Walley AY (2019). Touchpoints – Opportunities to predict and prevent opioid overdose: A cohort study. Drug and Alcohol Dependence, 204, 107537. 10.1016/j.drugalcdep.2019.06.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larochelle MR, Liebschutz JM, Zhang F, Ross-Degnan D, & Wharam JF (2016). Opioid prescribing after nonfatal overdose and association with repeated overdose: A cohort study. Annals of Internal Medicine, 164(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Lowder EM, Amlung J, & Ray B (2020). Individual and county-level variation in outcomes following non-fatal opioid-involved overdose. Journal of Epidemiology and Community Health, jech-2019–212915. 10.1136/jech-2019-212915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macmadu A, Goedel WC, Adams JW, Brinkley-Rubinstein L, Green TC, Clarke JG, Martin RA, Rich JD, & Marshall BDL (2020). Estimating the impact of wide scale uptake of screening and medications for opioid use disorder in US prisons and jails. Drug and Alcohol Dependence, 208, 107858. 10.1016/j.drugalcdep.2020.107858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks C, Abramovitz D, Donnelly CA, Carrasco-Escobar G, Carrasco-Hernández R, Ciccarone D, González-Izquierdo A, Martin NK, Strathdee SA, & Smith DM (2021). Identifying counties at risk of high overdose mortality burden during the emerging fentanyl epidemic in the USA: a predictive statistical modelling study. The Lancet Public Health, 6(10), e720–e728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall BDL, Yedinak JL, Goyer J, Green TC, Koziol JA, & Alexander-Scott N (2017). Development of a Statewide, Publicly Accessible Drug Overdose Surveillance and Information System. American Journal of Public Health, 107(11), 1760–1763. 10.2105/AJPH.2017.304007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod KE, Slaunwhite AK, Zhao B, Moe J, Purssell R, Gan W, Xavier C, Kuo M, Mill C, & Buxton JA (2021). Comparing mortality and healthcare utilization in the year following a paramedic-attended non-fatal overdose among people who were and were not transported to hospital: A prospective cohort study using linked administrative health data. Drug and Alcohol Dependence, 218, 108381. [DOI] [PubMed] [Google Scholar]
- Nechuta SJ, Tyndall BD, Mukhopadhyay S, & McPheeters ML (2018). Sociodemographic factors, prescription history and opioid overdose deaths: A statewide analysis using linked PDMP and mortality data. Drug and Alcohol Dependence, 190, 62–71. 10.1016/j.drugalcdep.2018.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor AW, Sears JM, & Fulton-Kehoe D (2022). Overdose and substance-related mortality after release from prison in Washington State: 2014–2019. Drug and Alcohol Dependence, 241, 109655. [DOI] [PubMed] [Google Scholar]
- Olfson M, Wall M, Wang S, Crystal S, & Blanco C (2018). Risks of fatal opioid overdose during the first year following nonfatal overdose. Drug and Alcohol Dependence, 190, 112–119. 10.1016/j.drugalcdep.2018.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Cottler LB, Goldberger BA, Severtson SG, Grundy DJ, Iwanicki JL, & Ciccarone D (2022). Trends in characteristics of fentanyl-related poisonings in the United States, 2015–2021. The American Journal of Drug and Alcohol Abuse, 48(4), 471–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters DJ, Monnat SM, Hochstetler AL, & Berg MT (2020). The Opioid Hydra: Understanding Overdose Mortality Epidemics and Syndemics Across the Rural-Urban Continuum. Rural Sociology, 85(3), 589–622. 10.1111/ruso.12307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phalen P, Ray B, Watson DP, Huynh P, & Greene MS (2018). Fentanyl related overdose in Indianapolis: Estimating trends using multilevel Bayesian models. Addictive Behaviors, 86, 4–10. 10.1016/j.addbeh.2018.03.010 [DOI] [PubMed] [Google Scholar]
- Ranapurwala SI, Shanahan ME, Alexandridis AA, Proescholdbell SK, Naumann RB, Edwards D, & Marshall SW (2018). Opioid Overdose Mortality Among Former North Carolina Inmates: 2000–2015. American Journal of Public Health, 108(9), 1207–1213. 10.2105/AJPH.2018.304514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray B, Hedden BJ, Carroll JJ, del Pozo B, Wagner K, Kral AH, O’Donnell D, Victor G, & Huynh P (2022). Prevalence and correlates of incarceration following emergency medical services response to overdose. Drug and Alcohol Dependence, 238, 109571. 10.1016/j.drugalcdep.2022.109571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray B, Lowder E, Bailey K, Huynh P, Benton R, & Watson D (2020). Racial differences in overdose events and polydrug detection in Indianapolis, Indiana. Drug and Alcohol Dependence, 206, 107658. 10.1016/j.drugalcdep.2019.107658 [DOI] [PubMed] [Google Scholar]
- Ray B, Lowder EM, Kivisto AJ, Phalen P, & Gil H (2018). EMS naloxone administration as non-fatal opioid overdose surveillance: 6-year outcomes in Marion County, Indiana. Addiction (Abingdon, England), 113(12), 2271–2279. 10.1111/add.14426 [DOI] [PubMed] [Google Scholar]
- Ray B, Quinet K, Dickinson T, Watson DP, & Ballew A (2017). Examining Fatal Opioid Overdoses in Marion County, Indiana. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 94(2), 301–310. 10.1007/s11524-016-0113-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray B, Victor G, Cason R, Hamameh N, Kubiak S, Zettner C, Dunnigan M, Comartin E, & Costello M (2022). Developing a cascade of care for opioid use disorder among individuals in jail. Journal of Substance Abuse Treatment, 108751. 10.1016/j.jsat.2022.108751 [DOI] [PubMed] [Google Scholar]
- Selitsky LJ, Nordeck C, Truong A, Agus D, & Buresh ME (2022). Higher Buprenorphine Dose Associated with Increased Treatment Retention at Mobile Buprenorphine Clinic: A Retrospective Cohort Study [Preprint]. 10.2139/ssrn.4188937 [DOI] [PubMed] [Google Scholar]
- Shefner RT, Sloan JS, Sandler KR, & Anderson ED (2020). Missed opportunities: Arrest and court touchpoints for individuals who fatally overdosed in Philadelphia in 2016. International Journal of Drug Policy, 78, 102724. 10.1016/j.drugpo.2020.102724 [DOI] [PubMed] [Google Scholar]
- Socias ME, Wood E, Le Foll B, Lim R, Choi JC, Mok WY, Bruneau J, Rehm J, Wild TC, & Bozinoff N (2022). Impact of fentanyl use on initiation and discontinuation of methadone and buprenorphine/naloxone among people with prescription-type opioid use disorder: Secondary analysis of a Canadian treatment trial. Addiction, 117(10), 2662–2672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer MR, Miniño AM, Warner M. Drug overdose deaths in the United States, 2001–2021. NCHS Data Brief, no 457. Hyattsville, MD: National Center for Health Statistics. 2022. DOI: 10.15620/cdc:122556. [DOI] [PubMed] [Google Scholar]
- Stewart MT, Coulibaly N, Schwartz D, Dey J, & Thomas CP (2021). Emergency department–based efforts to offer medication treatment for opioid use disorder: What can we learn from current approaches? Journal of Substance Abuse Treatment, 129, 108479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoové MA, Dietze PM, & Jolley D (2009). Overdose deaths following previous non-fatal heroin overdose: Record linkage of ambulance attendance and death registry data. Drug and Alcohol Review, 28(4), 347–352. 10.1111/j.1465-3362.2009.00057.x [DOI] [PubMed] [Google Scholar]
- Strickland JC, Havens JR, & Stoops WW (2019). A nationally representative analysis of ―twin epidemics‖: Rising rates of methamphetamine use among persons who use opioids. Drug and Alcohol Dependence, 204, 107592. 10.1016/j.drugalcdep.2019.107592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suffoletto B, & Zeigler A (2020). Risk and protective factors for repeated overdose after opioid overdose survival. Drug and Alcohol Dependence, 209, 107890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Justice, Drug Enforcement Administration. (2023). Controlled Substance Schedules. https://www.deadiversion.usdoj.gov/schedules/
- Victor GA, Bailey K, & Ray B (2021). Buprenorphine Treatment Intake and Critical Encounters following a Nonfatal Opioid Overdose. Substance Use & Misuse, 1–9. 10.1080/10826084.2021.1901933 [DOI] [PubMed] [Google Scholar]
- Victor G, Zettner C, Huynh P, Ray B, & Sightes E (2021). Jail and Overdose: Assessing the Community Impact of Incarceration on Overdose. Addiction, 117, 433–441. [DOI] [PubMed] [Google Scholar]
- Volkow ND, & Blanco C (2020). The changing opioid crisis: Development, challenges and opportunities. Molecular Psychiatry, 1–16. 10.1038/s41380-020-0661-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Chandler RK, & Villani J (2022). Need for comprehensive and timely data to address the opioid overdose epidemic without a blindfold. Addiction, 117(8), 2132. 10.1111/add.15957 [DOI] [PubMed] [Google Scholar]
- Volkow ND, McLellan TA, Cotto JH, Karithanom M, & Weiss SR (2011). Characteristics of opioid prescriptions in 2009. Jama, 305(13), 1299–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman SE, Larochelle MR, Ameli O, Chaisson CE, McPheeters JT, Crown WH, Azocar F, & Sanghavi DM (2020). Comparative Effectiveness of Different Treatment Pathways for Opioid Use Disorder. JAMA Network Open, 3(2), e1920622–e1920622. 10.1001/jamanetworkopen.2019.20622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu E, Villani J, Davis A, Fareed N, Harris DR, Huerta TR, LaRochelle MR, Miller CC, & Oga EA (2020). Community dashboards to support data-informed decision-making in the HEALing Communities Study. Drug and Alcohol Dependence, 217, 108331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell JE, Clarke SD, Kral AH, Richardson NJ, Cauchon D, & Aldridge A (2022). Association between law enforcement seizures of illicit drugs and drug overdose deaths involving cocaine and methamphetamine, Ohio, 2014–2019. Drug and Alcohol Dependence, 232, 109341. 10.1016/j.drugalcdep.2022.109341 [DOI] [PubMed] [Google Scholar]


