Abstract
Introduction
The 2021 European Society of Cardiology (ESC) Guidelines recommend the use of four different classes of drugs for heart failure with reduced ejection fraction (HFrEF): beta blockers (BB), sodium-glucose cotransporter-2 inhibitors (SGLT2i), angiotensin receptor/neprilysin inhibitor (ARNI), and mineralocorticoid receptor antagonists (MRAs). Moreover, the 2023 ESC updated Guidelines suggest an intensive strategy of initiation and rapid up-titration of evidence-based treatment before discharge, based on trials not using the four-pillars. We hypothesized that an early concomitantly administration and up-titration of four-pillars, compared with a conventional stepwise approach, may impact the vulnerable phase after hospitalization owing to HF.
Methods
This prospective, single center, observational study included consecutive in-hospital patients with HFrEF. After performing propensity score matching, they were divided according to treatment strategy into group 1 (G1), with predischarge start of all four-pillars, with their up-titration within 1 month, and group 2 (G2) with the pre Guidelines update stepwise four-pillars introduction. HF hospitalization, cardiovascular (CV) death, and the composite of both were evaluated between the two groups at 6-month follow-up.
Results
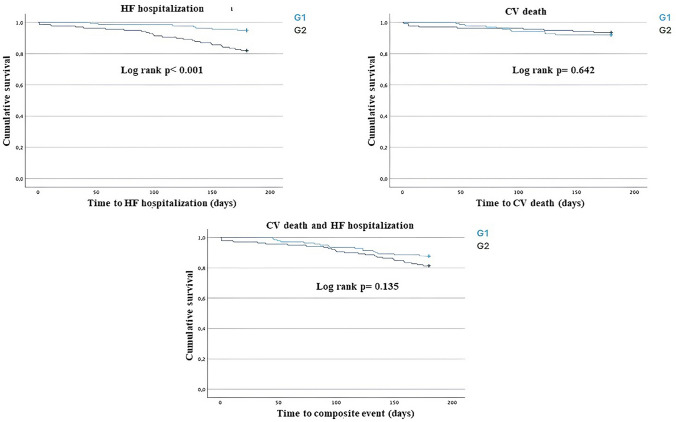
The study included a total of 278 patients who completed 6-month follow-up (139 for both groups). There were no differences in terms of baseline features between the two groups. At survival analysis, HF hospitalization risk was significantly lower in G1 compared with G2 (p < 0.001), while no significant differences were observed regarding CV death (p = 0.642) or the composite of CV death and HF hospitalization (p = 0.135).
Conclusions
In our real-world population, patients with HF treated with a predischarge and simultaneous use of four-pillars showed a reduced risk of HF hospitalization during the vulnerable phase after discharge, compared with a conventional stepwise approach.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40256-024-00660-6.
Key points
| Heart failure is a progressive disease and the period after an index hospitalization is particularly critical owing to the risk of adverse events. | |
| An early and comprehensive therapy approach is associated with reduced hospitalization in vulnerable phase after an index hospitalization. |
Introduction
Heart failure (HF) is a complex clinical syndrome, characterized by a high mortality rate, and is the second most common cause of death [1]. Hospitalization is a major issue within the HF patient population. HF is known to be the most frequent cause of hospitalization in patients over 65 years of age [1]. Hospitalization is highest within the first month post discharge, the so called “vulnerable period,” but remains high until 6 months after an index hospitalization for HF [2]. The vulnerable phase is characterized by a death and readmission risk above 25%, making HF prognosis comparable to aggressive cancers [2, 3]. HF is a multisystemic syndrome and each hospitalization is associated with further disease progression, compromising the patient’s conditions and quality of life, and burdening healthcare systems [4].
From a pathophysiological point of view, several pathways are involved in HF progression. Neurohormonal activation, renin-angiotensin-aldosterone system (RAAS), and sympathetic nervous system hyperactivation, as well as cardiac remodeling and inflammation are initially compensatory mechanisms that lead to HF and eventually result in multisystemic organ dysfunction at a more advanced stage of the disease [5]. The involvement of other organs, such as the kidneys, additionally reduces the patient’s life quality and expectancy, partially owing to impaired adequate drug up-titration [6, 7]. A prompt introduction of all four pillars of HF treatment might prevent the development of multiorgan dysfunction observed in the more advanced stages of the disease.
According to the 2021 Guidelines [1], HF management relies on a therapy based on four pharmacological pillars including RAAS inhibitors (RAASi), especially angiotensin converting enzyme inhibitors (ACEi) or aldosterone receptor/neprilysin inhibitors (ARNI), beta blockers (BB), mineralocorticoid receptor antagonists (MRAs), and sodium glucose cotransporter-2 inhibitors (SGLT2i), as they have been shown to reduce mortality and hospitalization risk [1, 8].
The recent 2023 update of European Society of Cardiology (ESC) Guidelines [8] stresses the importance of a complete therapy, with an intensive initiation strategy followed by a rapid up-titration to minimize the risk of hospitalization and death, based on the STRONG HF trial results [9]. However, the STRONG HF trial has several limits [9]. In particular, data on SGLT2i are missing, the patient population was accurately selected on the basis of NT-pro BNP values and its reduction during hospitalization, and therapy was not fully up-titrated in the control group [8, 9].
Different approaches for drug initiation and up-titration have been hypothesized, which were mainly based on clinical phenotype and patient tolerance [10]. However, a detailed sequential introduction schematic is mainly based on the results of recent clinical trials in which the newer drug is added on top of the older drug [6, 7]. Moreover, these approaches are often hypotheses as real-world data are scarce. At the moment, there are no evidence about the simultaneous use of the four pillars for HF therapy in real clinical practice. Before the recent update [8], the most used approach was based on the sequential addition and up-titration of each drug class. However, considering HF complexity and its pathophysiological features, some hypothesis may be made: (i) the contemporary targeting of many pathophysiological pathways may produce a more relevant effect than a sequential approach; (ii) HF disease modifying drugs begin to work early on from treatment initiation, in a time frame going from 2 to 8 weeks, depending on the specific molecule. For this reason, timing is crucial, particularly in the in-hospital and early postdischarge periods; (iii) sequential, stepwise drug initiation and up-titration require longer time to reach the optimized medical therapy (OMT), compared with a more intensive and comprehensive approach.
All these details taken together point to the need for a better definition of treatment strategies, considering that all the four classes of drugs are recommended and hence should all be used without delay [1, 8].
The aim of the following real-world monocentric study is to compare a comprehensive early introduction schematic, in predischarge phase, including all four pillars of HF therapy (BB, ARNI, SGLT2i, and MRAs) started simultaneously, even at low doses, with a classical sequential introduction approach, in terms of HF hospitalization, cardiovascular (CV) death and a composite of HF hospitalization and CV death at 6-months’ follow-up after an index hospitalization for HF.
Methods
This study is an observational, prospective, single center study, which enrolled, patients with a diagnosis of HF who have been consecutively admitted to the Department of Clinical, Internal, Anesthesiology and Cardiovascular Sciences at Policlinico Umberto I, Sapienza University of Rome between November 2022 and May 2023. Inclusion criteria were as follows: (i) written, signed, and dated informed consent; (ii) age above 18 years; and (iii) diagnosis of HF according to the Guidelines [1]. Exclusion criteria were as follows: (i) planned or history of heart transplantation or ventricular assist device (VAD); (ii) end-stage kidney failure/dialysis; (iii) any condition limiting life expectancy less than 1 year; (iv) pregnancy or nursing; and (v) noncompliance with study protocol.
We propose a strategy characterized by the early predischarge initiation of four pillars of HF disease-modifying drugs, including BB, SGLT2i, MRAs, and ARNI (the latter preferred to ACEi/ARB as first-line), to reach a complete, OMT within the first month from hospital discharge. We adopted a strategy on the basis of a prompt, in-hospital start of BB and SGLT2i, with the subsequent addition of ARNI and MRAs as soon as the renal and hemodynamic parameters were stable. Our strategy provided simultaneous initiation for all patients of each class of drug, even using low doses. Our therapeutic introduction regimen has been compared with a standard, conventional regimen, based on the sequential addition of HF disease-modifying drugs up to their maximum tolerated dose. Differently from the conventional approach we proposed a strategy using ARNI, and not ACEi/ARBs, as first line, and starting early with SGLT2i.
According to the adopted therapeutic strategy and after propensity score matching (PSM) analysis, patients were divided into two groups: group 1 (G1), patients treated with the early and comprehensive approach; and group 2 (G2), patients treated with the classical (pre-update of ESC guidelines) stepwise approach who cannot start all the drugs simultaneously for several reasons, such as transient contraindication (i.e., urinary tract infection for SGLT2i), electrolytes imbalance (i.e., hyperkalemia for RAASi), or an ongoing therapy with either ACEi or angiotensin receptor blockers (ARBs) at maximal tolerated dose.
Follow-up visits to assess adverse events was performed at 6-months from enrollment, at the end of the “vulnerable phase.” Therapy up-titration was performed during hospitalization and within the next months at HF outpatient service, according to patient tolerance.
The following parameters have been collected: (i) clinical parameters [past medical history, physical examination, electrocardiogram, arterial blood pressure, New York Heart Association (NYHA) class, pharmacological therapy], echocardiographic parameters (ventricular chambers size and function, systolic and diastolic function, valve disease and severity), and laboratory parameters (blood cell count, creatinine, electrolytes, alanine aminotransferase, aspartate aminotransferase, gamma glutamyl transferase, alkaline phosphatase, ferritin, transferrin, circulating iron, total, and direct and indirect bilirubin).
HF hospitalization, CV death, and the composite of HF hospitalization and CV death have been investigated at the 6-month follow-up after the index hospitalization.
Propensity score matching (PSM) analysis was used to homogenize the numerical differences between the two populations. Data were collected in a dedicated Excel database. The study was conducted according to the Helsinki Declaration. The study protocol was approved by the ethical committee of Policlinico Umberto I in Rome (rif.7068).
Statistical analysis
Patients were divided into two cohorts: patients treated with the comprehensive, rapid guideline directed medical therapy (GDMT) introduction (G1) and patients treated with the conventional GDMT schematic (G2). Owing to differences in baseline characteristics, we used PSM for the two cohorts and assembled a cohort for each comparison; all the measured covariates were well-balanced across the groups. A logistic regression model was used to obtain propensity scores, with the GDMT introduction protocol defined as the dependent variable, and age, sex, clinical characteristics (arterial hypertension, type II diabetes mellitus, dyslipidemia, familial history of CV disease, smoking habit, and glomerular filtration rate), and echocardiographic parameters (left ventricular ejection fraction, left ventricle end diastolic diameter, and interventricular and posterior wall thickness) assessed by estimating the standardized differences between groups. Operationally, a standardized difference > 10% represents a meaningful imbalance in a given variable between groups. The normal distribution of variables was assessed with the Kolmogorov–Smirnov test. For continuous variables, descriptive statistics were provided (number of available observations, mean, standard deviation), while the median (interquartile range) was used for non-normal data. Categorical data were described as the number (percentage). Student’s t test, the χ2 test, and the Fisher exact test were used for comparisons. For all tests, a p value < 0.05 was considered statistically significant. The Kaplan–Meier method was used to estimate cumulative event rates in the two groups. Differences in each group were compared using log-rank tests. The Cox regression hazard model was performed to obtain hazard ratio (HR) for the endpoints.
All statistical analyses were performed using SPSS version 27.0 statistical analysis software.
Results
A total of 320 patients have been enrolled in the study. After PMS analysis, 278 patients that were analyzed and followed-up within a period of 6 months were included in the study. In total, 139 patients treated with the comprehensive, rapid GDMT represented group 1 (G1) and 139 patients treated with the conventional GDMT represented the group 2 (G2).
Baseline features of the patient population before and after PMS are listed in Table 1 and Table S1 (Supplementary Information), respectively. The two groups were homogeneous in terms of past medical history, risk factors, clinical presentation, and laboratory profile. Among G1, 29 (20.9%) patients were male compared with 37 (26.6%) patients in G2. The mean age in G1 was 69.7 ± 13.2 years versus 69.7 ± 13.6 years in G2. Overall, 43 (31%) patients were previously hospitalized owing to HF in G1 compared with 45 (32%) in G2. In total, 106 (76.2%) patients in G1 had ischemic HF compared with 110 (79.1%) in G2. The mean estimated glomerular filtration rate (eGFR) was equal to 62.2 ± 24 ml/min/1.73 m2 in G1 and 64.9 ± 27.3 ml/min/1.73 m2 in G2. The average left ventricular ejection fraction (LVEF) was equal to 31.1 ± 9.9 % in G1 and 31.7 ± 9.1 % in G2 (Table S1).
Table 1.
Baseline characteristics of patients included in the study at hospital admission.
| Variable | Group 1 (n = 139) |
Group 2 (n = 139) |
p value | |
|---|---|---|---|---|
| Male gender, n (%) | 29 (20.9) | 37 (26.6) | 0.412 | |
| Arterial Hypertension, n (%) | 111 (79.9) | 104 (74.8) | 0.316 | |
| Type II Diabetes Mellitus, n (%) | 22 (15.9) | 36 (25.9) | 0.677 | |
| Dyslipidemia, n (%) | 58 (41.7) | 73 (52.5) | 0.107 | |
| CVD family history, n (%) | 34 (24.5) | 34 (24.5) | 1 | |
| Smoking habit, n (%) | 47 (33.8) | 55 (39.6) | 0.352 | |
| Age, years (SD) | 69.7 (±13.2) | 69.7 (±13.6) | 0.989 | |
| Ischemic etiology, n (%) | 106 (76.2) | 110 (79.1) | 0.66 | |
| Previous HF hospitalization, n (%) | 43 (31) | 45 (32) | 0.89 | |
| eGFR, ml/min/1.73 m2 (SD) | 62.2 (±24) | 64.9 (±27.3) | 0.384 | |
| K+, mmol/L (SD) | 4.3 (±0.8) | 4.1 (±0.9) | 0.06 | |
| Na+, mmol/L (SD) | 140.5 (±3.5) | 141(±3.5) | 0.23 | |
| LVEDD, mm (SD) | 58 (±4.2) | 57 (±4.8) | 0.07 | |
| IVS, mm (SD) | 11 (±1.1) | 11 (±0.8) | 1 | |
| PW, mm (SD) | 10 (±1.3) | 10 (±1.1) | 1 | |
| TAPSE, mm (SD) | 18.5 (±3) | 17 (±3) | 0.16 | |
| LVEF, (SD) | 31.1 (± 9.9) | 31.7 (± 9.1) | 0.624 | |
| ICD, n (%) | 75 (54) | 68 (49) | 0.47 | |
| CRT-D, n (%) | 15 (11) | 13 (9) | 0.84 | |
| CCM, n (%) | 4 (3) | 3 (2) | 1 | |
| NYHA class | I (%) | 8 (6) | 6 (4.3) | 0.8 |
| II (%) | 66 (48) | 64 (46) | 0.9 | |
| III (%) | 53 (38) | 55 (39) | 0.9 | |
| IV (%) | 12 (8.6) | 14 (10) | 0.8 | |
ACEi angiotensin-converting enzyme inhibitor, ARNI angiotensin receptor/neprilysin inhibitor, ARBs Angiotensin receptor blockers, CCM cardiac contractility modulation, CRT-D cardiac resynchronization therapy with defibrillator, CVD cardiovascular disease, eGFR glomerular filtration rate, HF heart failure, ICD implantable cardioverter defibrillator, IVS interventricular septum, LVEDD left ventricular end-diastolic diameter, LVEF left ventricular ejection fraction, MRAs mineralocorticoid receptor antagonists, NYHA new York heart association, PW posterior wall, SD standard deviation, SGLT2i sodium glucose cotransporter-2 inhibitors, TAPSE tricuspid annular plane systolic excursion
Therapy for HF at 6 months follow up has been presented in Table 2.
Table 2.
Medical therapy regarding the four pillars for heart failure at 6 months follow up according to each group
| Therapy | Group 1 (N= 139) |
Group 2 (N=139) |
p value |
|---|---|---|---|
| BB, n (%) | 136 (98) | 135 (97.6) | 1 |
| ARNI, n (%) | 126 (91) | 51 (36.5) | < 0.001 |
| ACEi/ARBs, n (%) | 0 (0) | 66 (47.2) | < 0.001 |
| SGLT2i, n (%) | 124 (89) | 126 (91) | 0.84 |
| MRAs, n (%) | 115 (83) | 114 (82) | 1 |
For patients who experienced cardiovascular death within the study period, the medical therapy at the moment of the adverse event has been recorded
ACEi angiotensin-converting enzyme inhibitors, ARBs angiotensin receptor blockers, ARNI angiontensin receptor neprilysin inhibitors, BB beta blockers, MRAs mineralcorticoid receptor antagonists, SGLT2i sodium-glucose co-transporter-2 inhibitors.
In the total population, at the end of the study period, 32 patients (18%) reached the highest dose of 97/103 mg b.i.d. for sacubitril/valsartan, 13 patients (19%) reached the highest dose of ACEi/ARBs (10 mg/die for ramipril and 300 mg/die for irbesartan), 41 patients (15%) reached the highest dose of BB (10 mg/die for bisoprolol and 25 mg b.i.d. for carvedilol), and 44 patients (19%) reached the highest dose for MRAs (100 mg/die for potassium canrenoate and 50 mg/die for spironolactone). Regarding patients on SGLT2i, 190 patients (76%) were on treatment with dapagliflozin 10 mg/die, while 60 patients (24%) were treated with empagliflozin 10 mg/die.
Regarding the safety endpoints at the end of study period, symptomatic hypotension occurred in 8 patients (3%), 3 patients (1.15%) experienced clinically significant hyperkalemia, which caused RAASi suspension and potassium binder initiation, 5 patients (1.72%) experienced clinically relevant urinary tract infection, and 9 patients (3.4%) experienced clinically significant acute kidney injury.
At the 6-month follow-up, the risk of HF hospitalization was significantly lower for G1 compared with G2 [hazard ratio (HR): 0.26; 95% confidence interval (CI) 0.112–0.601; p = 0.002], while no significant differences between the groups were reported in terms of CV death (HR 1.22; 95% CI 0.506–2.948; p = 0.65) and in terms of the composite of CV death and HF hospitalization (HR 0.63; 95% CI 0.345–1.170; p = 0.14; Table 3). The survival analyses performed with the Kaplan–Meier method demonstrated that G1 patients had a significantly lower rate of hospitalization for HF compared with those in G2 at the 6-month follow-up (log-rank p < 0.001; Fig. 1). No differences have been demonstrated regarding CV death (log-rank p = 0.642) and the composite of HF hospitalization and CV death (log-rank p = 0.135) between the two groups (Fig. 1).
Table 3.
Differences in term of event rates regarding the study outcomes between the two study groups.
| Variable | Group 1 (N= 139) |
Group 2 (N=139) |
HR (95% CI) | p value |
|---|---|---|---|---|
| CV death, n (%) | 11 (7.9) | 9 (6.5) | 1.22 (0.506–2.948) | 0.65 |
| HF hospitalization, n (%) | 7 (5) | 25 (18) | 0.26 (0.112–0.601) | 0.002 |
| Composite of HF hospitalization and CV death, n (%) | 17 (12.2) | 26 (18.7) | 0.63 (0.345–1.170) | 0.14 |
CI confidence interval, CV cardiovascular, HF heart failure, HR hazard ratio.
Fig. 1.
Survival analysis for the two groups performed using the Kaplan–Meier method regarding the occurrence of HF hospitalization, CV death, and the composite of the two above mentioned events. The comprehensive and innovative GDMT approach is represented by the blue line (G1), while the conventional GDMT approach is represented with green line (G2). Patients treated with the novel GDMT strategy (G1) had a lower rate of hospitalization compared with the patients treated with the conventional GDMT (G2) (log-rank p value < 0.001). No differences in terms of CV death (log-rank p value = 0.642) and the composite of HF hospitalization and CV death (log-rank p value = 0.135) have been demonstrated between the two groups. CV cardiovascular, HF heart failure
Discussion
HF may be compared to cancer, not only in terms of prognosis but also from a pathophysiological point of view. Indeed, as with cancer, HF is to be regarded as a multisystemic disease, which starts from the heart and spreads to all the major organs and systems [6, 7, 11–13].
Despite great advances in terms of HF management through the current GDMT suggested by the most recent Guidelines [1, 8], some major gaps remain to be filled to date regarding the most appropriate therapeutical strategy to follow to better treat and manage patients with HF. One limitation remains the difficulty to achieve proper GDMT optimization in real-life clinical settings. Partially this can be related to the fact that the conventional GDMT strategy requires several months of up-titration to obtain/achieve OMT. However, patients with HF are particularly at risk of hospitalization and death during the vulnerable phase up to 6 months after an index hospitalization. Avoiding adverse events during this critical period counteracts HF progression and increases prognosis and quality of life [2–4]. To pursue this goal, the minutiae management of HF disease modifying drugs is crucial, particularly considering two aspects: timing of initiation and sequential introduction.
Regarding these aspects, several hypotheses have been reported. McMurray and Packer [14, 15] suggest initiating BB and SGLT2i upfront, followed by ACEi/ARNI within 2 weeks, and MRAs an additional 2 weeks later. This approach was thought to be beneficial as each medication unfolds its effects individually. Therefore, an early introduction of all four pillars is of essence, regardless of their optimal up-titration. As such, a schematic implicates that most of the beneficial effects are achieved within the first 30 days from the initiation of treatment, and GDMT should be achieved within 4 weeks. Another treatment strategy was proposed by Miller et al. [16], suggesting a phenotype-based approach based on clinical clusters. Their hypothesis was to start treatment according to the clinical parameters (i.e., arterial blood pressure, heart rate) and the goal was to achieve GDMT within 6 weeks, regardless of optimal titration. Greene et al. [17] hypothesized a nearly simultaneous initiation of low doses of each of the four classes of molecules, within the first week from hospital discharge, and subsequent rapid up-titration in the following month. A similar approach has been suggested by Tomasoni et al. [18], with a specific reference to the early upfront administration of SGLT2i. The authors point out the fact that, major clinical trials have focused on testing these drugs in patients already undergoing treatment with background HF therapy, nevertheless secondary analyses have proven that the efficacy of SGLT2i is independent of the latter. Moreover, SGLT2i are usually safe and well tolerated, with minimal side effects in terms of blood pressure, hypoglycemia, and kidney injury [19, 20].
Recent updates of the HF Guidelines [8] stress the importance of a complete therapy with an intensive initiation strategy, followed by a rapid up-titration period. A relevant issue remains that the role of SGLT2i has not been investigated in the main trials on which these Guidelines are based, such as the STRONG HF trial [9]. The STRONG HF trial [9] was designed to investigate the safety and efficacy of rapid up-titration of guideline-recommended HF treatment before discharge from an acute HF admission and during the vulnerable period, compared with usual care. Of note, when speaking of guideline-recommended HF treatment, the study refers to BB, RAASi, and MRAs. The STRONG-HF study demonstrated that most patients admitted for acute HF and not treated with optimal doses of oral HF therapies can undergo rapid and safe up-titration within a few weeks postdischarge. Safety was assessed by means of frequent visits, including clinical and laboratory check-ups [9]. Nevertheless, one of the major limitations of the STRONG-HF trial is the fact that SGLT2i were only included in the last period of the study. Hence, this study is missing details about one of the current major protagonists in the field of HF management, and the possible effects of the upfront use of SGLT2i in such a clinical setting are yet to be fully elucidated [9]. In addition to the well-known cardioprotective role, SGLT2i are known to also have nephroprotective effects in the long term, further underlining the pivotal role they play in HF multisystemic management [19, 20].
A strong predictor of mortality in HF is the number of previous HF hospitalizations. This observation highlights the importance of lowering the hospitalization risk, by targeting the “vulnerable phase” [2, 21]. The EVOLUTION HF study [22] demonstrated that in clinical practice the initiation of GDMT on the basis of SGLT2i and ARNI after a hospitalization is delayed, mainly in high-risk patients with comorbidities, such as diabetes mellitus and chronic kidney disease. Those patients showed an increased rate of drug discontinuation and therapy was often downtitrated. These observations stress the importance of an upfront introduction strategy, avoiding physician inertia [22, 23].
Our study tried to meet the above-mentioned limitations regarding HF therapeutic management. We demonstrated that an upfront and prompt introduction approach within the first month from hospital discharge may reduce the hospitalization risk at 6 months from discharge after an index hospitalization.
In particular, we proposed the in-hospital initiation of BB and SGLT2i, followed by RAASi introduction (ARNI rather than ACEi/ARB) once kidney and hemodynamic parameters have been stabilized, ideally before hospital discharge, even at very-low dosage. This has been compared with the conventional GDMT strategy based on the sequential, preESC Guidelines update, stepwise introduction of ACEi/ARNI/ARBs, BB, MRAs, and SGLT2i.
We demonstrated that our GDMT rapid strategy significantly reduced the risk of HF hospitalization (HR 0.26; 95% CI 0.112–0.601; p = 0.002) compared with the conventional stepwise GDMT approach at 6 months after an index hospitalization, thus impacting the critical vulnerable phase. Our results did not show significant differences between the two approaches in terms of CV death (p = 0.65). This could be owing to the fact that all patients were on GDMT during the study period.
Our study represents a real-life experience of Guidelines [1, 8] indications regarding patients with HF management in the post discharge phase. To our knowledge, this is the first real world study evaluating the strategy of an early simultaneous use of the four pillars for HF therapy. We highlighted the potential usefulness to early start SGLT2i administration, before the other drugs. We observed that ARNI use, compared with ACEi/ARBs, is advisable, as also recently suggested [24–26], and early in-hospital initiation of the four pillars is feasible even using very low doses of each drug.
Our study has several limitations. This was a single-center study including a non-randomized population. Data regarding natriuretic peptides at hospital admission are lacking. Data regarding safety of the two approaches have not been investigated extensively, patients were not stratified according to LVEF, and a longer follow-up and a bigger population may be useful to strengthen our results.
Conclusions
During the vulnerable period, hospitalization and therefore disease progression drastically affect patient’s prognosis. The proper optimization of GDMT remains a difficult goal to be achieved for a large number of patients in real practice [22, 23, 27–29]. Many pharmacological treatment strategies have been hypothesized regarding the management of HF [14–18]. Before the ESC Guidelines update [8], the most conventional approach was based on the sequential, stepwise introduction, until maximal up-titration of the four drugs, resulting in a delay of full treatment optimization. We suggested a comprehensive, rapid GDMT initiation strategy based on the prompt, nearly simultaneous introduction of BB, SGLT2i, ARNI, and MRAs for all patients, even using low doses of each drug. Our study demonstrates that the rapid GDMT initiation strategy significantly reduces HF hospitalization at 6 months after an index hospitalization. However, no differences in terms of CV death between the two approaches have been identified. This aspect may be explained by the assumption that both groups are on OMT and its effect on CV mortality is widely known [1, 8].
Supplementary Information
Below is the link to the electronic supplementary material.
Author Contributions
P.S., A.D., M.M., and F.F. conceptualized the study; P.S., A.D., S.P., M.V.M., V.M., A.L.F., and C.C. performed data curation; P.S., A.D., S.P., and M.V.M. conducted the formal analysis and performed the methodology; V.M., R.B., M.M., F.F., and C.D.V. supervised the study and performed validation and visualization; P.S., A.D., S.P., M.V.M., V.M., A.L.F., C.C., E.T., G.M., L.I.B., and S.M.I. performed writing—original draft and writing–review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. This work did not receive external funding.
Availability of Data and Material
Not applicable.
Code availability
Not applicable.
Declarations
Conflict of Interest
Paolo Severino, Andrea D’Amato, Silvia Prosperi, Marco Valerio Mariani, Vincenzo Myftari, Aurora Labbro Francia, Claudia Cestiè, Elisa Tomarelli, Giovanna Manzi, Lucia Ilaria Birtolo, Stefanie Marek-Iannucci, Viviana Maestrini, Massimo Mancone, Roberto Badagliacca, Francesco Fedele, and Carmine Dario Vizza declare no conflicts of interest or competing interests.
Ethics Approval
Not applicable.
Consent to Participate
All the authors participated in the study and made significant intellectual contributions to the manuscript.
Consent for Publication
The manuscript is not currently under consideration elsewhere, and the work reported will not be submitted for publication elsewhere until a final decision has been made as to its acceptability by the Journal.
Footnotes
Paolo Severino and Andrea D’Amato have contributed equally to this work.
References
- 1.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–3726. 10.1093/eurheartj/ehab368.
- 2.Cotter G, Davison B, Cohen-Solal A, Freund Y, Mebazaa A. Targeting the ‘vulnerable’ period—first 3–6 months after an acute heart failure admission - the light gets brighter. Eur J Heart Fail. 2023;25(1):30–4. 10.1002/ejhf.2754. 10.1002/ejhf.2754 [DOI] [PubMed] [Google Scholar]
- 3.Mamas MA, Sperrin M, Watson MC, Coutts A, Wilde K, Burton C, et al. Do patients have worse outcomes in heart failure than in cancer? A primary care-based cohort study with 10-year follow-up in Scotland. Eur J Heart Fail. 2017;19:1095–104. 10.1002/ejhf.822 [DOI] [PubMed] [Google Scholar]
- 4.Gheorghiade M, Vaduganathan M, Fonarow GC, Bonow RO. Rehospitalization for heart failure: problems and perspectives. J Am Coll Cardiol. 2013;61(4):391–403. 10.1016/j.jacc.2012.09.038. 10.1016/j.jacc.2012.09.038 [DOI] [PubMed] [Google Scholar]
- 5.Schwinger RHG. Pathophysiology of heart failure. Cardiovasc Diagn Ther. 2021;11(1):263–76. 10.21037/cdt-20-302. 10.21037/cdt-20-302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Severino P, D'Amato A, Prosperi S, Dei Cas A, Mattioli AV, Cevese A, Novo G, Prat M, Pedrinelli R, Raddino R, Gallina S, Schena F, Poggesi C, Pagliaro P, Mancone M, Fedele F, on Behalf of the Italian National Institute for Cardiovascular Research Inrc. Do the current guidelines for heart failure diagnosis and treatment fit with clinical complexity? J Clin Med. 2022;11(3):857. 10.3390/jcm11030857. [DOI] [PMC free article] [PubMed]
- 7.Severino P, D’Amato A, Prosperi S, Myftari V, Canuti ES, Labbro Francia A, Cestiè C, Maestrini V, Lavalle C, Badagliacca R, Mancone M, Vizza CD, Fedele F. Heart failure pharmacological management: gaps and current perspectives. J Clin Med. 2023;12(3):1020. 10.3390/jcm12031020. 10.3390/jcm12031020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Skibelund AK; ESC Scientific Document Group. 2023 Focused update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023:ehad195. 10.1093/eurheartj/ehad195.
- 9.Mebazaa A, Davison B, Chioncel O, Cohen-Solal A, Diaz R, Filippatos G, Metra M, Ponikowski P, Sliwa K, Voors AA, Edwards C, Novosadova M, Takagi K, Damasceno A, Saidu H, Gayat E, Pang PS, Celutkiene J, Cotter G. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial. Lancet. 2022;400(10367):1938–52. 10.1016/S0140-6736(22)02076-1. 10.1016/S0140-6736(22)02076-1 [DOI] [PubMed] [Google Scholar]
- 10.Rosano GMC, Moura B, Metra M, Böhm M, Bauersachs J, Ben Gal T, Adamopoulos S, Abdelhamid M, Bistola V, Čelutkienė J, Chioncel O, Farmakis D, Ferrari R, Filippatos G, Hill L, Jankowska EA, Jaarsma T, Jhund P, Lainscak M, Lopatin Y, Lund LH, Milicic D, Mullens W, Pinto F, Ponikowski P, Savarese G, Thum T, Volterrani M, Anker SD, Seferovic PM, Coats AJS. Patient profiling in heart failure for tailoring medical therapy. A consensus document of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2021;23(6):872-881. 10.1002/ejhf.2206. [DOI] [PubMed]
- 11.Fedele F, Severino P, Calcagno S, Mancone M. Heart failure: TNM-like classification. J Am Coll Cardiol. 2014;63(19):1959–60. 10.1016/j.jacc.2014.02.552. 10.1016/j.jacc.2014.02.552 [DOI] [PubMed] [Google Scholar]
- 12.Severino P, Mancone M, D’Amato A, Mariani MV, Prosperi S, Alunni Fegatelli D, Birtolo LI, Angotti D, Milanese A, Cerrato E, Maestrini V, Pizzi C, Foà A, Vestri A, Palazzuoli A, Vizza CD, Casale PN, Mather PJ, Fedele F. Heart failure ‘the cancer of the heart’: the prognostic role of the HLM score. ESC Heart Fail. 2024;11(1):390–9. 10.1002/ehf2.14594. 10.1002/ehf2.14594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Severino P, Maestrini V, Mariani MV, Birtolo LI, Scarpati R, Mancone M, Fedele F. Structural and myocardial dysfunction in heart failure beyond ejection fraction. Heart Fail Rev. 2020;25(1):9–17. 10.1007/s10741-019-09828-8. 10.1007/s10741-019-09828-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Packer M, McMurray JJV. Rapid evidence-based sequencing of foundational drugs for heart failure and a reduced ejection fraction. Eur J Heart Fail. 2021;23(6):882–94. 10.1002/ejhf.2149. 10.1002/ejhf.2149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McMurray JJV, Packer M. How should we sequence the treatments for heart failure and a reduced ejection fraction?: a redefinition of evidence-based medicine. Circulation. 2021;143(9):875–7. 10.1161/CIRCULATIONAHA.120.052926. 10.1161/CIRCULATIONAHA.120.052926 [DOI] [PubMed] [Google Scholar]
- 16.Miller RJH, Howlett JG, Fine NM. A novel approach to medical management of heart failure with reduced ejection fraction. Can J Cardiol. 2021;37(4):632–43. 10.1016/j.cjca.2020.12.028. 10.1016/j.cjca.2020.12.028 [DOI] [PubMed] [Google Scholar]
- 17.Greene SJ, Butler J, Fonarow GC. Simultaneous or rapid sequence initiation of quadruple medical therapy for heart failure-optimizing therapy with the need for speed. JAMA Cardiol. 2021;6(7):743–4. 10.1001/jamacardio.2021.0496. 10.1001/jamacardio.2021.0496 [DOI] [PubMed] [Google Scholar]
- 18.Tomasoni D, Fonarow GC, Adamo M, Anker SD, Butler J, Coats AJS, Filippatos G, Greene SJ, McDonagh TA, Ponikowski P, Rosano G, Seferovic P, Vaduganathan M, Voors AA, Metra M. Sodium-glucose co-transporter 2 inhibitors as an early, first-line therapy in patients with heart failure and reduced ejection fraction. Eur J Heart Fail. 2022;24(3):431–441. 10.1002/ejhf.2397. (Epub 2022 Jan 17. Erratum in: Eur J Heart Fail. 2023 Mar;25(3):443). [DOI] [PMC free article] [PubMed]
- 19.Severino P, D’Amato A, Prosperi S, Costi B, Angotti D, Birtolo LI, Chimenti C, Lavalle C, Maestrini V, Mancone M, Fedele F. Sodium-glucose cotransporter 2 inhibitors and heart failure: the best timing for the right patient. Heart Fail Rev. 2023;28(3):709–21. 10.1007/s10741-021-10170-1. 10.1007/s10741-021-10170-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zelniker TA, Braunwald E. Mechanisms of cardiorenal effects of sodium-glucose cotransporter 2 inhibitors: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(4):422–34. 10.1016/j.jacc.2019.11.031.Erratum.In:JAmCollCardiol.2020Sep22;76(12):1505. 10.1016/j.jacc.2019.11.031.Erratum.In:JAmCollCardiol.2020Sep22;76(12):1505 [DOI] [PubMed] [Google Scholar]
- 21.Abdin A, Anker SD, Butler J, Coats AJS, Kindermann I, Lainscak M, Lund LH, Metra M, Mullens W, Rosano G, Slawik J, Wintrich J, Böhm M. ‘Time is prognosis’ in heart failure: time-to-treatment initiation as a modifiable risk factor. ESC Heart Fail. 2021;8(6):4444–53. 10.1002/ehf2.13646. 10.1002/ehf2.13646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Savarese G, Kishi T, Vardeny O, Adamsson Eryd S, Bodegård J, Lund LH, Thuresson M, Bozkurt B. Heart failure drug treatment-inertia, titration, and discontinuation: a multinational observational study (EVOLUTION HF). JACC Heart Fail. 2023;11(1):1–14. 10.1016/j.jchf.2022.08.009. 10.1016/j.jchf.2022.08.009 [DOI] [PubMed] [Google Scholar]
- 23.Severino P, D’Amato A, Prosperi S, Magnocavallo M, Maraone A, Notari C, Papisca I, Mancone M, Fedele F. Clinical support through telemedicine in heart failure outpatients during the COVID-19 pandemic period: results of a 12-months follow up. J Clin Med. 2022;11(10):2790. 10.3390/jcm11102790. 10.3390/jcm11102790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tan NY, Sangaralingham LR, Sangaralingham SJ, Yao X, Shah ND, Dunlay SM. Comparative effectiveness of sacubitril-valsartan versus ACE/ARB therapy in heart failure with reduced ejection fraction. JACC Heart Fail. 2020;8(1):43–54. 10.1016/j.jchf.2019.08.003. 10.1016/j.jchf.2019.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gao J, Zhang X, Xu M, Deng S, Chen X. The efficacy and safety of sacubitril/valsartan compared with ACEI/ARB in the treatment of heart failure following acute myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Front Pharmacol. 2023;4(14):1237210. 10.3389/fphar.2023.1237210. 10.3389/fphar.2023.1237210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang HR, Xu XD, Shaikh AS, Zhou BT. Efficacy and safety of sacubitril/valsartan compared with ACEI/ARB on health-related quality of life in heart failure patients: a meta-analysis. Ann Pharmacother. 2023;57(8):907–17. 10.1177/10600280221140575. 10.1177/10600280221140575 [DOI] [PubMed] [Google Scholar]
- 27.Severino P, Prosperi S, D’Amato A, Cestiè C, Myftari V, Maestrini V, Birtolo LI, Filomena D, Mariani MV, Lavalle C, Badagliacca R, Mancone M, Fedele F, Vizza CD. Telemedicine: an effective and low-cost lesson from the COVID-19 pandemic for the management of heart failure patients. Curr Heart Fail Rep. 2023. 10.1007/s11897-023-00624-y. 10.1007/s11897-023-00624-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.D’Amato A, Prosperi S, Severino P, Myftari V, Labbro Francia A, Cestiè C, Pierucci N, Marek-Iannucci S, Mariani MV, Germanò R, Fanisio F, Lavalle C, Maestrini V, Badagliacca R, Mancone M, Fedele F, Vizza CD. Current approaches to worsening heart failure: pathophysiological and molecular insights. Int J Mol Sci. 2024;25(3):1574. 10.3390/ijms25031574. 10.3390/ijms25031574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Girerd N, Von Hunolstein JJ, Pellicori P, Bayés-Genís A, Jaarsma T, Lund LH, Bilbault P, Boivin JM, Chouihed T, Costa J, Eicher JC, Fall E, Kenizou D, Maillier B, Nazeyrollas P, Roul G, Zannad N, Rossignol P, Seronde MF; EF-HF Group. Therapeutic inertia in the pharmacological management of heart failure with reduced ejection fraction. ESC Heart Fail. 2022;9(4):2063-2069. 10.1002/ehf2.13929. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.
Not applicable.