Abstract
Objective:
To describe telemedicine use patterns and understand clinic’s approaches to shifting care delivery during the COVID-19 pandemic.
Methods:
We used electronic health record data from 203 community health centers across 13 states between 01/01/2019 and 6/31/2021 to describe trends in telemedicine visit rates over time. Qualitative data were collected from 13 of those community health centers to understand factors influencing adoption and implementation of telemedicine.
Results:
Most clinics in our sample were in urban areas (n = 176) and served a majority of uninsured and publicly insured patients (12.8% and 44.4%, respectively) across racial and ethnic minority groups (16.6% Black and 29.3% Hispanic). During our analysis period there was a 791% increase in telemedicine visits from before the pandemic (.06% pre- vs 47.5% during). A latent class growth analysis was used to examine differences in patterns of adoption of telemedicine across the 203 CHCs. The model resulted in 6 clusters representing various levels of telemedicine adoption. A mixed methods approach streamlined these clusters into 4 final groups. Clinics that reported rapid adoption of telemedicine attributed this change to leadership prioritization of telemedicine, robust quality improvement processes (eg, using PDSA processes), and emphasis on training and technology support.
Conclusions:
In response to the COVID-19 pandemic, telemedicine adoption rates varied across clinics. Our study highlight that organizational factors contributed to the clinic’s ability to rapidly uptake and use telemedicine services throughout the pandemic. These approaches could inform future non-pandemic practice change and care delivery.
Keywords: COVID-19, Community Health Center, telemedicine, mixed methods
Introduction
The COVID-19 pandemic had a significant impact on the delivery of primary care practically overnight. By April 6, 2020, 42 States from the United States (US) had declared stay at home orders, 1 and clinics 2 that once delivered the majority of their care via in-person visits had to pivot to telemedicine-based visits, with varying degrees of success. Community Health Centers (CHCs) are of particular interest as they provide high quality health care to more than 30 million people, despite having limited resources and underfunding compared to larger health systems. 3
Prior to the COVID-19 pandemic, telemedicine use across the US remained low for both privately- and publicly-insured patients. 4 Poor reimbursement rates, lack of uniformity of policies, and lack of appropriate resources had stunted the growth of telemedicine across the US healthcare system at-large, especially in CHC settings.5 -7 However, in response to COVID-19 and the urgency to implement telemedicine services, federal and state agencies rapidly deployed policies to expand access to telemedicine services, waived cost-sharing for telemedicine visits paid by federal healthcare programs8,9 and extended coverage to CHCs and Rural Health Centers (RHCs), 4 as well as dedicated $29 million per year over 4 years to invest in telemedicine infrastructure. 10 The results was a significant upward trend in telemedicine visit rates throughout the pandemic. 11
Uptake of telemedicine was not uniform, it varied by clinic-level factors (eg, trainings, clinic staff and patient technological literacy, and provide perceptions) and community characteristics (eg, internet availability, median income, and race/ethnicity).2,12 -15 These studies4,12,13,16 -20 focus on describing overall adoption and barriers and facilitators of telemedicine. There is a paucity of research describing longitudinal patterns of telemedicine uptake and experiences associated with these patterns, particularly within a diverse group of primary care clinics serving socioeconomically disadvantaged and racially and ethnically diverse patients. Therefore, using mixed methods, this study examines patterns of telemedicine use over a 15-month period during the pandemic across a nationally representative sample of CHCs. Using latent class modeling and semi-structured interviews, we describe and explain the different approaches clinics took to shift care delivery to and sustain use of telemedicine. This approach can help provide an understanding of the unique strengths and challenges of CHCs to rapidly adopt to a new care delivery system, and the opportunities for learning on how to best support CHCs in rapidly adopting or adapting care delivery.
Methods
Study Setting and Sample
This study uses data collected for a larger project to evaluate the impact of the COVID-19 pandemic on the delivery of cancer screenings. 21 The larger project used a parallel mixed methods design and included CHC systems within the OCHIN practice-based research network. 22 OCHIN (not an acronym) is a nonprofit health information technology organization which provides a single, patient-linked instance of the Epic® EHR. 22
Given the parallel mixed-methods design of the larger project, 21 our study refers to 2 sample populations: (1) study sites of 203 CHCs (quantitative) and (2) qualitative sample sites of 13 CHCs (qualitative).
Quantitative study sites included in this study were CHCs listed as primary care and/or had records of preventive care visits, were live on the OCHIN EHR as of 1/1/2018, and had >10 telemedicine visits for each month of the post-study period. The sample included monthly clinic level data from 203 CHCs in 13 states (AK, CA, GA, IN, MA, MN, MT, NC, OH, OR, TX, WA, and WI).
Qualitative sample sites were purposively selected for the larger project to evaluate the impact of the COVID-19 pandemic on the delivery of cancer screenings. 21 As part of the larger project, CHCs health systems eligible for participation in the study had to vary by size (number of clinical sites in their health system), patient racial and ethnic diversity (ie, Black, Hispanic, and Asian), payer mix, including proportion of uninsured patients, and geographic location (eg, urban, suburban, and rural). These CHCs remained open during the pandemic and received information technology (IT) support from OCHIN.
Data Collection
Clinical level quantitative data were collected from January 2019 through March 2020 (pre-COVID) to assess pre-COVID, baseline data. These data continued to be collected for the study period, April 2020 through June 2021, a period of more than a year after the start of the pandemic. EHR data for study sites (n = 203) were extracted from the Accelerating Data Value Across a National Community Health Center Network (ADVANCE) Clinical Research Network (CRN) housed at OCHIN.
For qualitative sample sites, OCHIN recruited the health systems and worked with system leadership to identify1 to 2 clinics per health system to participate in semi-structured interviews. Recruited health systems ranged in size from 1 to 27 clinics. At the conclusion of recruitment, of the 203 CHCs in the sample, 13 agreed to participate. Because the recruitment of these clinics stemmed from a larger project 21 for which recruitment did not specifically target clinics based on the uptake of telemedicine, we did not monitor whether saturation was reached. Interviewees included clinic leaders and staff (eg, medical directors, clinicians, and quality directors) selected for their knowledge about operational changes made at the clinic during the pandemic. We conducted 1 to 4 interviews per clinic; this number varied based on clinic size and organizational structure. A total of 29 people were interviewed.
Interviews were conducted by 2 experienced qualitative researcher by phone between August 2020 and September 2021. Interviews followed a semi-structured guide developed inductively based on the original research question. The guide focused on operational and care delivery changes during the pandemic, including a question about telemedicine uptake and use. Interviews were approximately 60 min in length, were audio-recorded, professionally transcribed, and entered into Atlas.ti (Version 8.0, Atlas.ti Scientific Software Development GmbH, Berlin, Germany) for data management and analysis.
Measures
The primary quantitative outcome was telemedicine uptake and was defined as the percent of monthly telemedicine visits at the clinic level. Uptake was calculated by dividing the monthly number of telemedicine visits by the monthly number of total visits (in person or telemedicine) and multiplied by 100 to yield a rate of telemedicine visits per 100 total visits.
Other clinic-level covariates included patient panel characteristics (sex, age, race, ethnicity, Charlson Comorbidity Score Index, 23 insurance status, and billable visits), number of medical doctors (MDs) and doctors of osteopathics (DOs) at the clinic and clinic geographic location (urban/rural).
Analysis
Quantitative Analysis
First, clinic level characteristics for the entire clinic sample were described. Then, to evaluate different trajectories in telemedicine uptake over the study period, a latent class growth analysis (LCGA) was performed to classify the clinics into the optimal number of clusters based on their distinct longitudinal trends of monthly telemedicine visits between April 2020 (start of pandemic restrictions) through June 2021. In brief, LCGA models have been increasingly utilized for their ability to identify homogeneous subpopulations within the larger heterogeneous population which can yield meaningful groups of clinics. 24 The total number of unique mutually-exclusive clusters was selected by calculating the model fit indices, Bayesian Information Criterion (BIC) and the Integrated Completed Likelihood Criterion (ICL) for different number of clusters and selecting the groupings with the smallest values. 25 For ease of interpretation and to further evaluate differences in telemedicine uptake trends, the clinic characteristics for each cluster were described. The quantitative team met to classify each of the clusters based on the distinct patterns of telemedicine uptake and trajectory of use based on the LCGA analysis. Analyses were conducted in RStudio 2023.06.0.
Qualitative Data Management and Analysis
The qualitative team followed the analytic process for health services research developed by Crabtree and Miller. 26 As a team, qualitative analysts listened to and discussed interviews as a team. Interviews from the same clinic were reviewed as a set 27 to understand each site’s setting, organizational structure, and process of telemedicine implementation. Through this process, the qualitative researchers developed a list of codes. All data related to telemedicine were tagged with a broad code, and additional codes were identified to capture emerging patterns. The qualitative team met weekly to analyze data, create, and refine codes based on team discussion and emergent findings, developed case summaries for each clinic, and identified factors at each site that appeared to influence the process of telemedicine uptake and use. Following within-case analysis we used the summaries to create a cross-case matrix display, 28 allowing us to examine factors of interest across clinics (see Appendix Table A1 for the format, descriptive data have been removed). This cyclical and iterative immersion-crystallization 29 process refined our understanding of how telemedicine uptake varied by site and over time, and helped to identify the leadership and organizational characteristics that influenced telemedicine uptake and use. To ensure analytic rigor, the qualitative team used a group analytic process to minimize researcher bias and debriefed the quantitative team about findings at least once to see if they had face validity. 30 The qualitative team then systematically classified each clinic’s use of telemedicine based on these identified factors, independent of quantitative data (see Appendix Table A2).
Mixed Method Approach
To understand the factors that influenced the trajectories of telemedicine use, the quantitative and qualitative teams reviewed their independent classification together to identify overlap. Two of the clinics from the qualitative sample were excluded because they lacked the required threshold of 10 visits per month, which left 11 qualitative sites in the mixed methods analysis. Appendix Table A3 describes the distribution of study sample and qualitative sample sites before and after the mixed methods analysis (Appendix Table A3). It should be noted that the groups were quantitively determined and qualitatively harmonized, as such clinics within each group were quantitively aligned but could be qualitatively different.
Results
As seen in Table 1, most clinics in our sample were located in urban areas (n = 176) and served a majority of uninsured and publicly insured patients (12.8% and 44.4%, respectively) across racial and ethnic minority groups (16.6% Black, 29.3% Hispanic).
Table 1.
Characteristics of the 203 Study Clinics Over the Study Period (January 2019-June 2021).
| Characteristics | Mean (IQR) |
|---|---|
| % Female patient | 56.9 (53.5, 59.6) |
| % Age 30-49 years | 31.0 (27.0, 36.6) |
| % Age 50-64 years | 20.3 (15.7, 24.9) |
| % Age 65+ years | 9.5 (4.5, 12.1) |
| % Black race | 16.6 (1.1, 20.3) |
| % White race | 64.5 (46.3, 85.7) |
| % Other race | 3.0 (1.0, 4.4) |
| % Hispanic ethnicity (any race) | 29.3 (7.2, 47.0) |
| % Patients with 5-6 Charlson Score | 8.2 (5.0, 11.0) |
| % Patients with 7+ Charlson Score | 10.0 (4.0, 14) |
| % Patient Uninsured | 12.8 (4.0, 14.0) |
| % Patient with Medicaid | 44.4 (34.3, 57.0) |
| % Patient mixed insurance | 16.9 (11.9, 18.7) |
| Avg. # of MD/DO | 13.4 (4.0, 14) |
| Avg. # of patients with billable visits | 7669 (2918, 10 445) |
| # Rural clinics | 27 |
| # Urban clinics | 176 |
The 203 clinics are located in AK, CA, GA, IN, MA, MN, MT, NC, OH, OR, TX, WA, and WI. The 13 recruited clinics were located in WI, MA, IN, CA, OH, OR, TX, and WA.
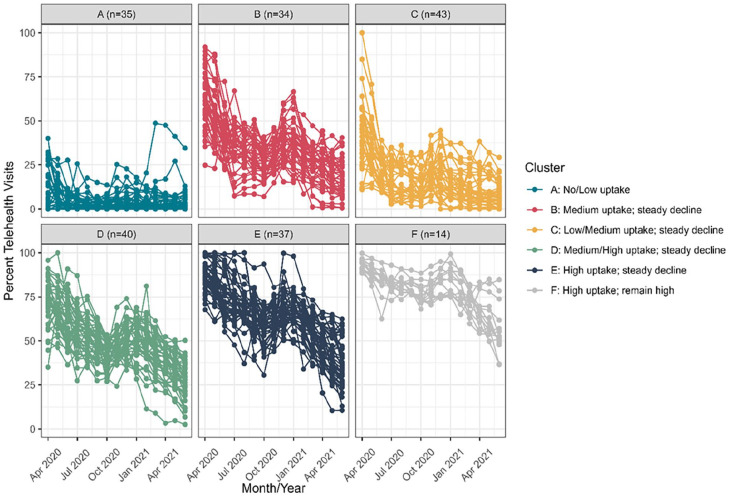
Prior to the COVID-19 pandemic, March 2019 to February 2020, 77 clinics out of the 203 clinics had a small number of telemedicine visits, which accounted for <1.0% of total visits in that timeframe. From April 2020 to June 2021, 200 out of the 203 clinics had any telemedicine visits, which accounted for 47.5% of all visits in that time period as illustrated in Figure 1.
Figure 1.
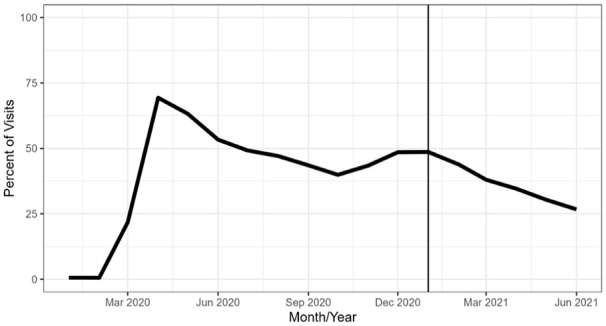
Percent of telemedicine visits by year (2019, 2020, and 2021).
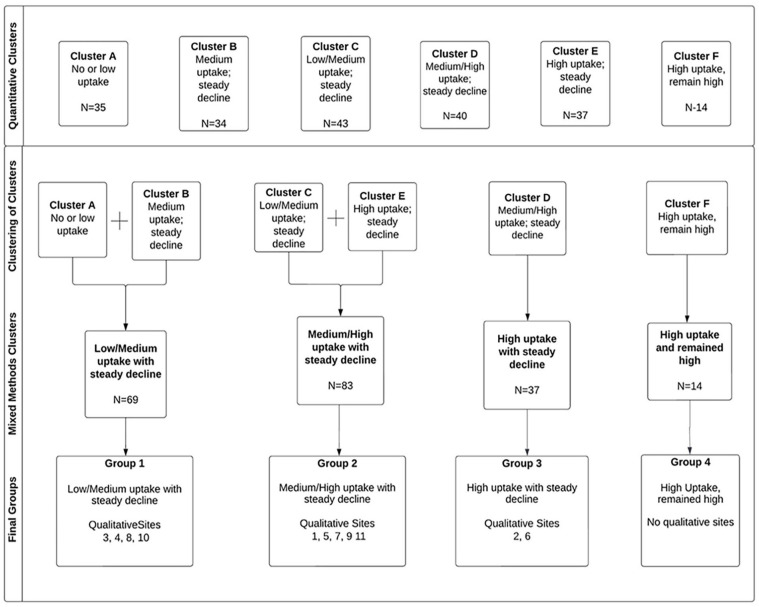
The LCG clustering procedure resulted in 6 clusters represented in Figure 2. Cluster A clinics (n = 35) had no to low uptake in telemedicine. Cluster B (n = 34) had medium uptake and had a steady decline over the rest of the study period. Cluster C (n = 43) had low/medium uptake with steady decline over time, while Cluster D (n = 37) had medium/high uptake but with steady decline. Cluster E (n = 40) had high uptake of telemedicine with a steady decline. Cluster F (n = 14) had high initial and sustained uptake of telemedicine.
Figure 2.
Distribution of telemedicine adoption at the onset of the COVID-19 pandemic across study clinics by cluster (April 2020-June 2021).
The qualitative team identified 3 categories of initial telemedicine uptake: low, medium, and high (Appendix Table A2) based on variations of the leadership and organizational characteristics that influenced telemedicine uptake. This included the ways in which health system and clinic leadership were involved in telemedicine rollout, and details about telemedicine training. Three qualitative sites were identified as having low initial uptake; 6 qualitative sites were identified as having high uptake, and 4 were identified as having medium uptake.
The mixed methods analysis reviewed alignment between quantitative clusters and qualitative categories and identified 4 final Groups as seen in Figure 3. Group 1: Clusters A and B, including 4 qualitative sites; Group 2: Clusters C and E, including 5 qualitative sites; Group 3: cluster D including 2 qualitative sites; and Group 4: cluster F, which had no qualitative sites. [Figure 3]
Figure 3.
Final groups derived from the mixed methods “clustering of clusters” analysis.
Group 1: Low/Medium Uptake of Telemedicine With Steady Decline (A and B)
Overall, this group includes 69 clinics, 4 of them recruited for semi-structured interviews. Cluster A and B clinics are mostly urban, serve a similar proportion of Hispanic patients (~20%), and over 50% of patients were uninsured or had Medicaid coverage. These clusters differed in the proportion of Black patients served (23.6% vs 10.1%) and total number of visits (n = 228 456 vs 697 315; Table 2).
Table 2.
Characteristics of Study Clinics by Telemedicine Cluster Over the Study Period (April 2020-June 2021).
| Mixed methods groups | Total | Group 1 low/medium uptake with steady decline | Group 2 medium/high uptake with steady decline | Group 3 high uptake with steady decline | Group 4 high uptake, remained high | ||
|---|---|---|---|---|---|---|---|
| Quantitative analysis clusters | (A) | (B) | (C) | (E) | (D) | (F) | |
| N, Clinics | 203 | 35 | 34 | 43 | 40 | 37 | 14 |
| Rurality | |||||||
| Urban | 176 | 26 | 27 | 43 | 35 | 31 | 14 |
| Rural | 27 | 9 | 7 | 0 | 5 | 6 | 0 |
| % Female | 56.9 | 55.1 | 61.7 | 55.8 | 57.1 | 55.9 | 55.2 |
| % Hispanic | 26.7 | 20.6 | 22.4 | 33.4 | 29.2 | 35.7 | 44.4 |
| % ≥65 years | 9.5 | 10.1 | 7.8 | 9.84 | 10.5 | 9.2 | 8.5 |
| % Black | 16.6 | 23.6 | 10.1 | 33.4 | 8.7 | 13.2 | 8.6 |
| Charlson Score Index | |||||||
| 5-6 | 8.1 | 8.4 | 7.8 | 7.3 | 8.9 | 8.2 | 8.1 |
| 7+ | 10.0 | 11.1 | 8.6 | 8.6 | 11.5 | 9.8 | 10.4 |
| Insurance (04/20-06/21) | |||||||
| % Medicaid | 44.5 | 34.4 | 45.9 | 43.7 | 49.2 | 44.8 | 52.1 |
| % Uninsured | 12.8 | 22.0 | 11 | 14.9 | 8.9 | 10.5 | 8.5 |
| Number of health systems | 22 | 21 | 19 | 24 | 27 | 9 | |
| Total # of visits 4/20-6/21 | 3 533 460 | 228 456 | 697 315 | 437 008 | 1 046 280 | 907 785 | 216 616 |
| Avg % of telemedicine visits 3/19-3/20 | 0.6 | 0.2 | 1.5 | 1.0 | 0.5 | 0.3 | 0.0 |
| Total # of telemedicine visits 3/19-3/20 | 15 351 | 837 | 2465 | 7706 | 2352 | 1987 | 2 |
| Total # of patients with a visit in study period 4/20-6/21 (median (IQR)) | 5841 (2919, 10 437) | 2697 (1157, 5688) | 5846 (3547, 10 586) | 5584 (2909, 8465) | 7403 (5124, 11 538) | 8665 (4065, 11 874) | 5474 (3599 9873) |
Prior to the pandemic lockdown, in February 2020, on average <1% of visits in this group were completed via telemedicine (Table 3). At the onset of the pandemic, this group averaged 37.7% of visits completed via telemedicine in April 2020 which declined to 10.9% by the end of our study period (June 2021).
Table 3.
Average Percent of Telemedicine Visits by Mixed Methods Grouping of Clusters.
| Distinct time periods during the COVID-19 pandemic a | Group 1 (A and B) | Group 2 (C and E) | Group 3 (D) | Group 4 (F) |
|---|---|---|---|---|
| Average % telemedicine visits Feb 2020, mean (SD) | 0.28 (1.3) | 0.79 (1.8) | 0.20 (0.7) | 1.3 (2.3) |
| Average % telemedicine visits April 2020, mean (SD) | 37.7 (29.9) | 67.3 (26.7) | 71.8 (13.4) | 92.9 (3.4) |
| Average % telemedicine visits Nov 2020, mean (SD) | 17.0 (14.5) | 43.0 (22.4) | 46.1 (8.1) | 79.0 (6.3) |
| Average % telemedicine visits June 2021, mean (SD) | 10.9 (11.0) | 24.8 (17.9) | 27.5 (10.8) | 56.2 (14.2) |
| Average % telemedicine visits April 2020-June 2021, mean (SD) | 19.0 (19.0) | 43.2 (27.5) | 48.9 (15.7) | 78.0 (12.0) |
Time periods were chosen based on last full month pre-COVID-19 restrictions (February 2020) and first full month under COVID-19 restrictions (April 2020). Intermedidate time periods were chosen based on equalivalent periods of months.
Semi-structured interviews with clinical staff highlighted that these sites had a more hands-off approach from clinic and health system leadership. This led to fragmented workflow and little to no telemedicine training or dedicated time for troubleshooting telemedicine-related challenges.
At this moment, we don’t have a telemed protocol for the organization. That’s one thing that we definitely need. . .Telemedicine protocol’s probably one area that is technically still deficient in terms of our team knowing what to do. They’ve been given the framework of it, so our team knows the different platforms that we use for audio and video. . . but we don’t have in the weeds [protocols]. – Chief Medical Officer, Site 4
I mean, in terms of any real formalized training, I would say no. I think that on most provider calls, definitely, challenges came up, and some protocols, potentially, on how to handle certain illnesses for example were discussed, but I don’t think that there was a real training on how to conduct telemedicine. –NP, Site 10
Further, clinicians in this group expressed resistance to telemedicine itself due to preferences or because they did not perceive that clinical visits via telemedicine offer sufficient patient information.
We also have some telemedicine yeah advice, but myself because I’m an old guy, I’d rather see people in-person than on video. – Medical Director, Site 8
It’s hard to do some of the OB visits, or even the GYN visits, online just because the exam is so important. It’s a very personal exam, too, so it’s not anything like people feel comfortable with over the telephone. – OBGYN, Site 3
There were some providers that were, especially for new patients, wanted to use non-telehealth, because it required an examination. – Medical Director, Site 3
Group 2: Medium/High Uptake of Telemedicine With Steady Decline (C and E)
Overall, this group included the largest number of study sites with 83 clinics, 5 of them represented in our qualitative sample. Both of these clusters are mostly urban, serve a similar proportion of Hispanic patients, patients ≥65 years, and most of their patients had Medicaid coverage or were uninsured. As seen in Table 2, Cluster C clinics served a larger proportion of Black patients (33.4%) than cluster E (8.7%), and had nearly 42% fewer visits during the study period than Cluster E.
In February 2020, prior to the pandemic, on average <1% of visits in this group were completed using telemedicine. At the onset of the pandemic, this rose to 67.3% (April 2020) and steadily declined to 43.0% in November of 2020 and to 24.8% at the end of the study (June 2021).
Qualitative data from semi-structured interviews with clinical staff highlight a strong prioritization from leadership on telemedicine-specific goals, such as the ratio of telemedicine versus in-person visits, and the ratio of telemedicine visits by phone versus video. Additionally, strong leadership drove much of the telemedicine implementation process, and influenced other key factors including formal training for all staff members, guided rollout of new workflows, convening a multidisciplinary team to discuss implementation and support from information technology (IT).
The executive team for [Site 1] starting in May made an organizational goal that 50 percent of our virtual care would be over video by October. We brought together an interdisciplinary group of folks across the organization. . .that full group met monthly and we developed several subcommittees that came out of that group of key priority areas around facilities and IT around workflow development. . . . We had a group focused on training. Staff training, from providers to front office, to medical assistants to make sure that everyone understood their part of the project or they’re part of onboarding a patient. . . so by October, we actually did meet our goal. – Chief Quality Officer, Site 1
Further, clinics that quickly adopted telemedicine in their practices exhibited processes found in Quality Improvement (QI) models for implementing a change in healthcare using rapid cycle improvement, similar to the Plan-Do-Study-Act (PDSA) cycle. These sites reported previous experience in implementing and applying QI tools and processes and directly applied this experience to their implementation of telemedicine services.
These are things that have just been tested out of the little PDSA cycles that had worked. We’ve also, for staffing issues with our medical assistants, if they’re able to help remotely, so right now while we’re having our meeting, my medical assistant is able to help other sites remotely. She doesn’t need to go in person, but she can call and help triage it and room the patient, patients at other sites. –Medical Director, Site 11
Another characteristic of clinics in this group was training clinic staff beyond clinicians, such as Medical Assistants (MA) and front desk staff, to provide technical support to patients, either during the virtual rooming or scheduling processes. Some clinics with large Hispanic populations were provided education about telemedicine in Spanish, and brought in Spanish-speaking interpreters to provide support during telemedicine visits.
Then one of the MAs, or sometimes we have a front desk dedicated to that when they were going through the schedule, to try to help all the patients have MyChart activation ready before the appointment. Then the providers don’t have to deal with that during that time. –Operations & Revenue Director, Site 5
Lastly, clinics in this cluster expressed a preference for keeping telemedicine in some capacity due to its accessibility for people with physical and mental health conditions or transportation barriers.
Again, telemedicine has been really important with my patient population and a lot of elderly folks, people dealing with dementia, people dealing with not being able to care for themselves as well at home. Telemedicine’s actually been wonderful. Twice now, at least, that out-of-town family member has been able to be part of the appointment on video. . .That’s really enhanced that patient’s care enormously. – Medical Director, Site 1
Group 3: High Uptake of Telemedicine With a Steady Decline (Cluster D)
This group included 37 study sites with 2 sites recruited for semi-structured interviews. Clinics in this group are mostly urban however, 20% of the clinics in this group were rural, the second most in our sample. One third of the patients identify as Hispanic (35.7%), nearly half of the patients have Medicaid insurance (44.8%), and saw an average of 8665 patients during the study period which accounted for 907 785 visits (Table 2).
February 2020, prior to the pandemic, on average <1% of visits were completed via telemedicine. At the onset of the pandemic, average telemedicine visits spiked to 71.8% of all visits (April 2020), slightly higher than the medium uptake seen in Group2. This steadily decreased to average 46.1% (November 2020) and 27.5% (June 2021) of all visits, respectively.
Qualitative data are limited in providing further insight into this group’s trajectory because of misalignment between the qualitative and quantitative data. The 2 qualitative sites included in this group were categorized as having either Low or Medium telemedicine adoption. These sites did not report on leadership prioritization or specific training for telemedicine, and instead preferred to remain open to in-person visits.
The low uptake qualitative sites is an employer-sponsored health system for agricultural workers. They already had telemedicine fully implemented prior to the start of the pandemic, but their priority was keeping the clinics open for the workers on-site.
We were never exclusively phone or virtual because people were always on site, and so my thought was if they’re on-site doing food stuff and they’re sick, I’d rather see ‘em in person, and pull them off the lines, and get them home than being like, “Oh, talk to us on the phone, even though you’re at work processing food.” We did have a in-person clinic throughout the entire pandemic. –Executive Medical Officer, Site 2
The medium uptake qualitative site reported a patient death from COVID-19 at the onset of the pandemic, which prompted them to quickly switch to telemedicine, despite limited guidance from leadership and no telemedicine training—although they did have access to IT support.
We weren’t really hit until end of March when my patient got sick and she died, and then another patient, also mine, came in coughing. We didn’t know what to do. Like, “Get her in a room. Isolate her. Do something.”. . .All of a sudden, it just arrived at [Clinic 6]. Also, at that same time, we started telemedicine, so—and honestly, once we started telemedicine, maybe the first week was a little slow, but once the patients got the hang of telemedicine, we were busy. – MD, Site 6
Group 4: High Uptake of Telemedicine and Remained High (F)
Group 4 included 14 clinics from the study sample, and none of our qualitative sites. All 14 sites were located in urban areas, served a large proportion of Hispanic patients (44.4%), and patients with Medicaid coverage (52.1%).
Prior to the pandemic, February 2020, clinics in this group averaged 1.3% of visits via telemedicine. These clinics switched almost entirely to telemedicine at the onset of the pandemic, with an average of 92.9% of all visits completed via telemedicine, which declined to 56.2% by the end of the study period (June 2021). We are unable to characterize the factors leading to this high uptake and sustained use of telemedicine, a limitation of our qualitative sampling design which was not based on initial quantitative groupings.
Discussion
This mixed methods study of primary care CHCs identified 4 distinct trajectories of telemedicine during the pandemic. To date, many previous studies have shown the uptake of telemedicine at the onset of the pandemic and the factors associated with use of telemedicine, but only use quantitative or qualitative work, or only focus on certain states or geographic regions.4,12,13,16 -20 This study adds to this body of evidence by examining sustained use, using qualitative semi-structured interviews to characterize the clinic experience associated with the patterns of adopting telemedicine, and using a national sample of clinics. The results show the critical importance of leadership support and experience with quality improvement to facilitate rapid uptake and support sustained use, and dedicated time for formal and informal trainings across all clinic staff members, rather than a specific subgroup (eg, clinician).
Experience with quality improvement was particularly indicative of a clinic’s familiarity with practice change management in our study. This primed clinics with the skills and potentially the resources to adapt their healthcare delivery rapidly (Group 2). These findings suggest the need for supporting increased capacity for QI in CHCs, provide trainings and internal or external support31 -34 to increase preparedness for rapid uptake of a new care delivery system, like telemedicine.
The importance of leadership support and training was evident especially among clinics who had lower uptake. Although the majority of our CHC’s rates of telemedicine increased dramatically at the onset of the pandemic, some clinics had lower rates of uptake (Group 1) and did not sustain use throughout the pandemic. Factors cited as limiting their uptake were the lack of formal training for clinical teams, clinician resistance to or preferences about adopting telemedicine, technology literacy, and a more hands-off approach from leadership which aligns with previously published literature.35 -37
The results for sustainability highlight that clinics with supportive environments to adopt telemedicine and rapidly increase its use were more likely to continue to sustain use with some variations (Groups 2 and 4). These results cannot inform the specific circumstances that explain the variation in sustained use from 70% to 50% of the visits. It is likely that the reasons are multifactorial and based on patients and clinicians needs and preferences, 35 payment reforms, and clinic resources. With the end of the Public Health Emergency (May 2023), Centers for Medicare and Medicaid and state programs are making changes to telehealth reimbursement.38,39 The provisional nature of these policies could lead to changes in coverage for services or parity in payment, impacting the sustainability of telemedicine in CHCs. 38 Specifically, for CHCs, changes to telehealth reimbursement mean fewer telehealth visits offered to their patients to ensure revenue. Many CHCs are in rural areas where lack of adequate broadband impedes the ability to conduct video visits. Reimbursement for telephone visits is more restricted in most states with some only reimbursing telephone visits occurring in underserved or rural areas and CMS not allowing reimbursement for Medicaid patients. Considering that telehealth significantly improved access to various services (eg, mental health care) to patients with access barriers, a reduction in the availability of telehealth in safety-net clinics is step backward to addressing health equity.
Strengths and Limitations
The strengths of this study include the nationally representative and highly varied sample of clinics in both the qualitative and quantitative samples. Additionally, many previously published studies about telemedicine use during the pandemic highlight only qualitative or quantitative findings,12,35,36,40 -43 while ours combines both methods.
However, this study has limitations. First, the qualitative data that we analyzed for this study was collected for a larger project about cancer prevention during the pandemic. While interviews contained useful data on telehealth implementation, the CHCs that participated in qualitative data collection were not selected specifically to inform the latent class analysis. As such, some of the clusters do not have sufficient clinics represented with interview data and we know little about the clinic’s telemedicine trajectory. Second, the qualitative data that we analyzed were collected at 1 time point, which limits our understanding of the factors that might explain the longitudinal trends we observed with regard to telehealth use in the quantitative data. Third, the interviews that we analyzed were not specifically focused on implementation and sustained use of telemedicine and the data we analyzed did not differentiate between phone and video visits, which is an important distinction with regard to reimbursement rates. Specifically, rural patients are more likely to rely on phone over video for telemedicine due to broadband issues.44,45 Additionally, reimbursement for phone visits is a barrier for these clinics, especially as healthcare payors such as Medicare are changing their pandemic-era reimbursement, which is particularly challenging to CHCs in rural areas. 46 To promote equity, policy makers need to identify reimbursement system to ensure that CHCs and their rural patients are not penalized for their geographic locations. Lastly, because the interview data were collected for another project, we could not monitor if saturation was reached, which may limit the transferability of our findings.
Conclusion
In this cohort of CHCs, experience with quality improvement, support from leadership, dedicated training, and IT assistance were found to be indicators of rapid uptake and sustained use of telemedicine during the COVID-19 pandemic. However, barriers to rapid uptake were also noted, including physician preferences and lack of support from leadership. In the event of a future need to rapidly adopt a new care delivery process, such as telemedicine, it would beseech health systems to consider these strengths and limitations to ensure the capacity of their clinics is adequate to make rapid changes to best support the communities they serve.
Acknowledgments
The authors acknowledge the participation of the health systems and interviewees. OCHIN is the implementation laboratory of the BRIDGE-C2 Center, Building Research in Implementation and Dissemination to close Gaps and achieve Equity in Cancer Control, is 1 of 7 Implementation Science Centers in Cancer Control. OCHIN EHR data are part of Accelerating Data Value Across a National Community Health Center Network (ADVANCE) Clinical Research Network (CRN). The research reported in this work was powered by PCORnet®. PCORnet has been developed with funding from the Patient-Centered Outcomes Research Institute® (PCORI®) and conducted with the Accelerating Data Value Across a National Community Health Center Network (ADVANCE) Clinical Research Network (CRN). ADVANCE is a Clinical Research Network in PCORnet® led by OCHIN in partnership with Health Choice Network, Fenway Health, University of Washington, and Oregon Health & Science University. ADVANCE’s participation in PCORnet® is funded through the PCORI Award RI-OCHIN-01-MC.
Appendix
Table A1.
Exploratory Qualitative Cross-Site Matrix.
| Site ID | Staff outbreak of COVID-19 | Leadership engagement in telemedicine uptake | Leadership support of staff | Previous QI experience | QI application during telemedicine uptake | Patient support through change | Telemedicine adoption | Care delivery adaptation |
|---|---|---|---|---|---|---|---|---|
| 1 | No | Engaged | Supportive | Experienced | Applied | Yes | High | High |
| 2 | [Unclear] | Unengaged | [Unclear] | Limited | Unapplied | No | Low | Low |
| 3 | Yes | Unengaged | Unsuportive | Limited | Unapplied | No | Medium | Low |
| 4 | Yes | Unengaged | Unsupportive | Limited | Unapplied | No | Medium | Medium |
| 5 | No | Engaged | Supportive | Experienced | Applied | Yes | High | High |
| 6 | Yes | Unengaged | Supportive | Limited | Unapplied | Yes | Medium | Low |
| 7 | [Unclear] | Engaged | Supportive | Experienced | Applied | Yes | High | Low |
| 8 | Yes | Unengaged | Unsupportive | Limited | Unapplied | No | Low | Low |
| 9 | No | Engaged | Supportive | Experienced | Applied | Yes | High | High |
| 10 | Yes | Engaged | Unsupportive | Limited | Unapplied | No | Low | Low |
| 11 | No | Engaged | Supportive | Experienced | Applied | Yes | Medium | Medium |
Table A2.
Qualitative Categorization for Telemedicine Uptake.
| Categorization | Features |
|---|---|
| High | Evidence of prioritization from leadership (eg, specific telemedicine goals) and all clinic staff trained formally |
| Medium | Limited formal training but evidence of some support (eg, regular discussion at clinician meetings, IT support available) |
| Low | Limited formal training and not all staff were trained and evidence of clinician resistance to telemedicine |
Table A3.
Quantitative and Qualitative Harmonization for Mixed Method Clusters.
| Qualitative site number a | Qualitative categorization | Quantitative cluster | Quantitative cluster name | Mixed method cluster |
|---|---|---|---|---|
| 3 | Medium | A | No or low Uptake |
Group 1 Low/Medium uptake with steady decline |
| 4 | Medium | B | Medium uptake; steady decline | |
| 8 | Low | A | No or low Uptake | |
| 10 | Low | B | Medium uptake; steady decline | |
| 1 | High | C | Low/Medium uptake; steady decline |
Group 2
Medium/High uptake with steady decline |
| 5 | High | C | Low/Medium uptake; steady decline | |
| 7 | High | C | Low/Medium uptake; steady decline | |
| 9 | High | E | High uptake; steady decline | |
| 11 | Medium | E | High uptake; steady decline | |
| 2 | Low | D | Medium/High uptake; steady decline |
Group 3
High uptake with steady decline |
| 6 | Medium | D | Medium/High uptake; steady decline |
Two clinics are excluded from quantitative analysis for not meeting the minimum required number of visits per month. There were no qualitative sites in Group 4, therefore it is excluded from this table.
Footnotes
Authors Contributions: HH provided conceptualization, supervision, and writing—original draft. NH, AB, TH, MD, JO, DC, MM provided data curation, formal analysis, and writing—review and editing. NH provided funding acquisition. All authors contributed writing, review, and editing, and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Cancer Institute of the National Institutes of Health (grant numbers P50CA244289 and P50CA244289-02S1). This P50 program was launched by NCI as part of the Cancer Moonshot.SM The funding source had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Ethical Approval: This study has been reviewed and approved by the Oregon Health & Science University Institutional Review Board (eIRB # 00021553). Participating health center management provided written consent for their health center to participate in the interview. Individual staff who were interviewed provided verbal consent to participate. Verbal consent was deemed sufficient because of the neutral content being discussed and the fact that all data were deidentified.
ORCID iDs: Heather Holderness  https://orcid.org/0000-0003-3915-8510
https://orcid.org/0000-0003-3915-8510
Nathalie Huguet  https://orcid.org/0000-0002-4064-1553
https://orcid.org/0000-0002-4064-1553
Data Availability: Raw data underlying this article were generated from multiple health systems across institutions in the OCHIN Network; restrictions apply to the availability and re-release of data under organizational agreements.
References
- 1. Kates J, Michaud J, Tobert J. Stay-at-home orders to fight COVID-19 in the United States: The risks of a scattershot approach. 2020. Accessed December 2022. https://www.kff.org/policy-watch/stay-at-home-orders-to-fight-covid19/
- 2. Luo J, Tong L, Crotty BH, et al. Telemedicine adoption during the COVID-19 pandemic: gaps and inequalities. Appl Clin Inform. 2021;12(4):836-844. doi: 10.1055/s-0041-1733848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Community Health Center Chartbook . 2023. Accessed March 2023. https://www.nachc.org/wp-content/uploads/2023/07/Community-Health-Center-Chartbook-2023-2021UDS.pdf
- 4. Weigel G, Ramaswamy A, Sobel L, Salganicoff A, Cubanski J, Freed M. Opportunities and barriers for telemedicine in the U.S. during the COVID-19 emergency and beyond. 2020. Accessed March 2022. https://www.kff.org/womens-health-policy/issue-brief/opportunities-and-barriers-for-telemedicine-in-the-u-s-during-the-covid-19-emergency-and-beyond/
- 5. Kim JH, Desai E, Cole MB. How The rapid shift to telehealth leaves many community health centers behind during the COVID-19 pandemic. Health Affairs Blog blog. 2020. Accessed 2021. https://www.healthaffairs.org/do/10.1377/forefront.20200529.449762/full/
- 6. Shaver J. The state of telehealth before and after the COVID-19 pandemic. Prim Care. 2022;49(4):517-530. doi: 10.1016/j.pop.2022.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shin P, Sharac J, Jacobs F. Provision of telemedicine services by community health centers. Online J Public Health Inform. 2014;6(2):e185. doi: 10.5210/ojphi.v6i2.5421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Centers for Medicare & Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet. Centers for Medicare & Medicaid Services. 2020. Accessed 2021. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- 9. Coronavirus Aid, Relief, and Economic Security Act, CARES Act, H.R. 748, United States Congress. 2020. Accessed 2021. https://www.congress.gov/116/bills/hr748/BILLS-116hr748enr.pdf
- 10. American Society of Hospital Pharmacists. Issue Brief: COVID-19 and Telehealth Changes. American Society of Hospital Pharmacists. 2022. Accessed 2022. https://www.ashp.org/advocacy-and-issues/key-issues/other-issues/additional-advocacy-efforts/issue-brief-covid-19?loginreturnUrl=SSOCheckOnly
- 11. Karimi M, Lee EC, Couture SJ, et al. National Trends in Telehealth Use in 2021: Disparities in Utilization and Audio vs. Video Services. Office of The Assistant Secretary for Planning and Evaluation USDoHaHS; 2022. HP-2022-04. [Google Scholar]
- 12. Gomez T, Anaya YB, Shih KJ, Tarn DM. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34:S61-S70. doi: 10.3122/jabfm.2021.S1.200517 [DOI] [PubMed] [Google Scholar]
- 13. Malhotra K, Sivaraman A, Regunath H. Coronavirus disease 2019 pandemic as catalyst for telemedicine adoption: a single-center experience. Telemed Rep. 2020;1(1):16-21. doi: 10.1089/tmr.2020.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lopez AM, Lam K, Thota R. Barriers and facilitators to telemedicine: can you hear me now? Am Soc Clin Oncol Educ Book. 2021;41:25-36. doi: 10.1200/edbk_320827 [DOI] [PubMed] [Google Scholar]
- 15. Molina F, Soulos P, Oldfield B. Clinical and sociodemographic factors associated with telemedicine engagement in an urban community health center cohort during the COVID-19 pandemic. Telemed e-Health. 2023;29(6):875-885. doi: 10.1089/tmj.2022.0389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LHI, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469-e476. doi: 10.5435/jaaos-d-20-00380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Annapragada A, Jenkins S, Chang A, Jain A, Srikumaran D, Srikuraman U. Factors driving rapid adoption of telemedicine in an academic orthopedic surgery department. Telemed e-Health. 2022;28(3):415-421. doi: 10.1089/tmj.2020.0539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chang JE, Lai AY, Gupta A, Nguyen AM, Berry CA, Shelley DR. Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post-COVID era. Milbank Q. 2021;99(2):340-368. doi: 10.1111/1468-0009.12509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Uscher-Pines L, Sousa J, Jones M, et al. Telehealth use among safety-net organizations in california during the COVID-19 pandemic. JAMA. 2021;325(11):1106-1107. doi: 10.1001/jama.2021.0282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rabinowitz G, Cho LD, Benda NC, et al. The telemedicine experience in primary care practices in the united states: insights from practice leaders. Ann Fam Med. 2023;21(3):207-212. doi: 10.1370/afm.2967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Huguet N, Danna M, Baron A, et al. Delivery of cervical and colorectal cancer screenings during the pandemic in community health centers: practice changes and recovery strategies. Med Care. 2023;61(8):554-561. doi: 10.1097/mlr.0000000000001879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. DeVoe JE, Likumahuwa-Ackman SM, Angier HE, et al. A practice-based research network (PBRN) roadmap for evaluating COVID-19 in community health centers: a report from the OCHIN PBRN. J Am Board Fam Med. 2020;33(5):774-778. doi: 10.3122/jabfm.2020.05.200053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-83. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 24. Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. 2008;2(1):302-317. doi: 10.1111/j.1751-9004.2007.00054.x [DOI] [Google Scholar]
- 25. Lezhnina O, Kismihók G. Latent class cluster analysis: selecting the number of clusters. MethodsX. 2022;9:101747. doi: 10.1016/j.mex.2022.101747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Crabtree BF, Miller WF. Doing Qualitative Research, vol. 3. Immersion/Crystallization Organizing Style of Analysis. Sage Publications Inc; 1992. [Google Scholar]
- 27. Crabtree BF, Miller WF. A template approach to text analysis: Developing and using codebooks. In: B. F. Crabtree & W. L. Miller (Eds.), Doing Qualitative Research. Research Methods for Primary Care, vol. 3. Sage Publications, Inc; 1992:93-109. [Google Scholar]
- 28. Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis: A Methods Sourcebook. 3rd edn. Sage Publications, Inc; 2014:381. [Google Scholar]
- 29. Borkan JM. Immersion-Crystallization: a valuable analytic tool for healthcare research. Fam Pract. 2022;39(4):785-789. doi: 10.1093/fampra/cmab158 [DOI] [PubMed] [Google Scholar]
- 30. Cohen DJ, Crabtree BF. Evaluative criteria for qualitative research in health care: controversies and recommendations. Ann Fam Med. 2008;6(4):331-339. doi: 10.1370/afm.818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Grumbach K, Bainbridge E, Bodenheimer T. Facilitating improvement in primary care: the promise of practice coaching. Issue Brief (Commonw Fund). 2012;15:1-14. [PubMed] [Google Scholar]
- 32. Harvey G, Loftus-Hills A, Rycroft-Malone J, et al. Getting evidence into practice: the role and function of facilitation. J Adv Nurs. 2002;37(6):577-588. doi: 10.1046/j.1365-2648.2002.02126.x [DOI] [PubMed] [Google Scholar]
- 33. Harvey G, Lynch E. Enabling continuous quality improvement in practice: the role and contribution of facilitation. Front Public Health. 2017;5:27. doi: 10.3389/fpubh.2017.00027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Webne-Behrman H. The Practice of Facilitation: Managing Group Process and Solving Problems. Greenwood Publishing Group; 1998. [Google Scholar]
- 35. SteelFisher GK, McMurtry CL, Caporello H, et al. Video telemedicine experiences in COVID-19 were positive, but physicians and patients prefer in-person care for the future. Health Aff. 2023;42(4):575-584. doi: 10.1377/hlthaff.2022.01027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Etz RS, Solid CA, Gonzalez MM, Britton E, Stange KC, Reves SR. Telemedicine in primary care: lessons learned about implementing health care innovations during the COVID-19 pandemic. Ann Fam Med. 2023;21(4):297-304. doi: 10.1370/afm.2979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Schinasi DA, Foster CC, Bohling MK, Barrera L, Macy ML. Attitudes and perceptions of telemedicine in response to the COVID-19 pandemic: a survey of naive healthcare providers. Front Pediatr. 2021;9:647937. doi: 10.3389/fped.2021.647937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Center for Connected Health Policy. State Telehealth Laws and Medicaid Program Policies. 2023. Accessed 2023. https://www.cchpca.org/2023/10/Fall2023_ExecutiveSummaryfinal.pdf
- 39. Reimbursement Tips: FQHC Requirements for Medicare Telehealth Services. Accessed 2023. https://www.nachc.org/wp-content/uploads/2023/07/Reimbursement-Tips_Telehealth.pdf
- 40. Uscher-Pines L, Raja P, Mehrotra A, Huskamp HA. Health center implementation of telemedicine for opioid use disorders: a qualitative assessment of adopters and nonadopters. J Subst Abuse Treat. 2020;115:108037. doi: 10.1016/j.jsat.2020.108037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Segal JB, Dukhanin V, Davis S. Telemedicine in primary care: qualitative work towards a framework for appropriate use. J Am Board Fam Med. 2022;35(3):507-516. doi: 10.3122/jabfm.2022.03.210229 [DOI] [PubMed] [Google Scholar]
- 42. Larson AE, Zahnd WE, Davis MM, et al. Before and during pandemic telemedicine use: an analysis of rural and urban safety-net clinics. Am J Prevent Med. 2022;63(6):1031-1036. doi: 10.1016/j.amepre.2022.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Star J, Han X, Makaroff LA, Minihan AK, Jemal A, Bandi P. The first year of the COVID-19 pandemic: changes in preventive services in community health centers. Am J Prevent Med. 2023;64(2):184-193. doi: 10.1016/j.amepre.2022.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chen J, Li KY, Andino J, et al. Predictors of audio-only versus video telehealth visits during the COVID-19 pandemic. J Gen Intern Med. 2022;37(5):1138-1144. doi: 10.1007/s11606-021-07172-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cubanski J, Neuman T. Medicare and Telehealth: Coverage and Use During the COVID-19 Pandemic and Options for the Future. 2021. Accessed 2022. https://www.kff.org/medicare/issue-brief/medicare-and-telehealth-coverage-and-use-during-the-covid-19-pandemic-and-options-for-the-future/
- 46. Goodman R, Lacktman N, Ferrante T. CMS Finalizes Changes for Telehealth Services for 2023. Health Care Law Today blog. 2022. Accessed 2023. https://www.foley.com/en/insights/publications/2022/11/cms-finalizes-changes-telehealth-services-2023