Abstract
Background
High rates of labour augmentation with oxytocin have been found in some low- and lower-middle-income countries, causing potential perinatal harm. It is critical to understand the reasons for this overuse. Aim was to explore factors that shape practices around using oxytocin for labour augmentation in a high-volume labour ward in Dar es Salaam, Tanzania.
Methods
Mixed-methods data collection was conducted from March 2021 to February 2022, including structured observations of 234 births, 220 h of unstructured labour ward observations and 13 individual in-depth interviews with birth attendants. Thematic network analysis and descriptive statistics were used to analyse data. We used a time-lens to understand practices of oxytocin for labour augmentation in time-pressured labour wards.
Results
Birth attendants constantly had to prioritise certain care practices over others in response to time pressure. This led to overuse of oxytocin for augmentation to ensure faster labour progression and decongestion of the, often overburdened, ward. Simultaneously, birth attendants had little time to monitor foetal and maternal condition. Surprisingly, while oxytocin was used in 146 out of 234 (62.4%) structured labour observations, only 9/234 (4.2%) women had active labour lasting more than 12 h. Correspondingly, 21/48 (43.8%) women who were augmented with oxytocin in the first stage of labour had uncomplicated labour progression at the start of augmentation. While the partograph was often not used for decision-making, timing of starting oxytocin often correlated with natural cycles of ward-rounds and shift-turnovers instead of individual women’s labour progression. This resulted in co-existence of ‘too early’ and ‘too late’ use of oxytocin. Liberal use of oxytocin for labour augmentation was facilitated by an underlying fear of prolonged labour and low alertness of oxytocin-related risks.
Conclusions
Time scarcity in the labour ward often made birth attendants deviate from clinical guidelines for labour augmentation with oxytocin. Efforts to navigate time pressure resulted in too many women with uncomplicated labour progression receiving oxytocin with little monitoring of labour. Fear of prolonged labour and low alertness to oxytocin-mediated risks were crucial drivers. These findings call for research into safety and benefits of oxytocin in low-resource settings and interventions to address congestion in labour wards to prevent using oxytocin as a time-management tool.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-024-06717-3.
Keywords: Oxytocin, Prolonged labour, Partograph, Low-resource, Augmentation, Intrapartum, Guidelines, PartoMa, Time-pressure, Urbanisation
Background
Oxytocin has been used since the 1950s to augment labour by stimulating contractions. Evidence, however, remains missing that oxytocin reduces caesarean section rates, although it has shown to reduce labour duration by 2 h [1, 2]. In too high doses, oxytocin may cause harm to women and their foetuses [3, 4]. Potential complications of its use include uterine rupture and stillbirth [5]. The required dose of oxytocin differs per individual and correct dosing requires titrating oxytocin against the woman’s contractions, whilst monitoring the foetal heart rate (FHR). Risks of oxytocin-related harm appear higher in low-resource settings with substandard monitoring [3]. Dosing in such settings often happens by visual drop count rather than electronic infusion, which is time-demanding and increases the risk of under- or overdosing. Availability of cardiotocography is rare in low-resource settings and replaced by intermittent auscultation of FHR.
It is troubling that the few studies conducted in low- and lower-middle-income countries (LLMIC) find that 89.5% of women receiving oxytocin for labour augmentation had uncomplicated labour progress, with some facilities using the drug in 80%-90% of women during birth [3]. This is much higher than the suggested 9–12% [6, 7]. Despite dangerously high rates of oxytocin for labour augmentation in some LLMICs, few studies have explored the underlying reasons.
Qualitative studies of labour augmentation with oxytocin have identified local demands among labouring women in Nepal, India and Uganda [8–11]. Studies from India, Nepal, Uganda and Sierra Leone suggest that birth attendants often underestimate the risks associated with oxytocin for labour augmentation and lack of skills in diagnosing prolonged labour and timing of oxytocin for labour augmentation [8–10, 12]. Finally, Khalil et al. explain how, in an Egyptian hospital, shortages of beds and hands were the main reasons for nearly universal oxytocin used for labour augmentation [13] while Van Hollen describes how oxytocin was used as “crowd control” [11]. These studies stop short of exploring such notions any further.
In alignment with previous studies suggesting that untimely and too frequent use of oxytocin to augment labour could be related to congestion, this mixed-methods study was conducted in an urban high-volume maternity unit, which historically has been among the most congested labour wards in Dar es Salaam, the largest urban centre of Tanzania and one of the fastest growing cities on the continent. The objective of this study was to investigate factors affecting practices around labour augmentation with oxytocin in a high-volume maternity unit through the lens of time. Here, time refers to the duration of labour, birth attendant-to-women ratio, and frequency, duration and timing of care practices.
Methods
This mixed-methods study forms part of the PartoMa research project, aiming at co-creating contextualised intrapartum clinical guidelines and training [14, 15]. The study took place in a public urban maternity unit in a regional referral hospital in Dar es Salaam, Tanzania. Annual number of births was around 7,000, in 2021, much lower than the number of 16,000 in 2016 [16]. This reduction likely resulted from a policy promoting decongestion of the busiest referral facilities by re-distributing women more evenly among the facilities [16]. The Covid-19 pandemic may also have influenced the facility birth rate [17].
In the latent phase (until cervical dilatation of 4 cm), women are monitored in the antenatal ward where they often share beds with other women. In active phase (cervical dilatation 4 cm or above), they enter the labour ward. The labour ward with 16 beds is managed by two to three nurse-midwives and a varying number of nurse-midwifery students, interns, registrar doctors and obstetric specialists. Nurse-midwives mostly practice on their own. They triage women on admission, monitor and manage labour, resuscitate neonates, prepare and escort women for caesarean section, provide immediate postnatal care and escort severely ill women to the national hospital. In addition, they are responsible for cleaning up beds after birth, keeping the ward clean, filling up equipment and medication storages and documenting information in multiple registers. All these extra tasks imply that generally, 1–2 nurse-midwives provide care to the women in the 16 beds with varying occupancy. Oxytocin is administered with manual infusion lines with 5 International Units in 500 ml saline. Contractions are measured manually over ten minutes and FHR assessed using intermitted auscultation with fetoscope or doppler. The context of high-volume Tanzanian maternity wards has also been described by others [16, 18–20].
Conceptual framework
To investigate the role of time, we draw on the concept of “Timescapes”. This concept was developed by sociologist Barbara Adam to highlight the interdependency between space and time [21]. The ‘Timescapes-concept’ allows us to examine how the spatial context of a busy labour ward (the ‘scapes’ part) combined with the duration of labour and timing of labour interventions (the ‘times’ part) will affect the use of oxytocin for labour augmentation. Table 1 details the clinical guidance around frequency and timing of oxytocin administration, indicating the time spent on key practices. Aiming to provide the best possible care, birth attendants tinker with care practices to make them work in their time pressured and overstretched realities. By exploring how time manifests in such a congested environment we examined the relationship between time scarcity, efforts to manage time and the influence on oxytocin for labour augmentation. Exploration of these efforts included obtaining an in-depth understanding of how tasks are prioritised and planned in a busy and under-resourced labour ward.
Table 1.
Routine monitoring and timing related to oxytocin use for labour augmentation
| Action | Guideline | Minimum time spent per woman |
|---|---|---|
| Measuring contractions over 10 min | At initiation of oxytocin and every 30 minutesa,b,c,d | 20 min/hour |
| Foetal Heart Rate (FHR) assessments | At initiation of oxytocin and every 30 minutesa,c,d | 4 min/hour |
| Continuous cardiotocography (CTG)b | ||
| Titration of oxytocin | Every 30 minutesa,b,c,d | 6 min/hour |
| Timing of oxytocin according to dilatation | 4 h of cervical arrestc | |
| After crossing the Partograph action linee | ||
| Cervical dilatation < 0.2—0.5 cm/hourd | ||
| Cervical dilatation < 0.5 cm/hourb |
Labour progression is determined in relation to a scientifically derived “normal” length of labour, which is still widely debated. Cervical dilatation of 0.2 to 0.5 cm per hour is the slowest yet normal progression of active labourb,d. Depending on the guidelines, oxytocin for labour augmentation should be administered if labour progresses slower than this and contractions are inadequateb,d, if there is complete arrest of labour for 4 hoursc or if the partograph’s action line is crossede. To evaluate whether contractions are adequate, these must be counted over a ten-minute time frame. To avoid hyperstimulation and related risks oxytocin must be titrated by increasing the drop rate every 30 min until contractions are strong enough. FHR must be monitored to evaluate whether the foetus tolerates increased contractions. While electronic infusion, FHR and contractions monitoring are present in high-income settings, these are often not available in labour wards in LLMICs. As seen, routine monitoring of one woman on oxytocin (FHR, contractions, titration) will take at least 30 min per hour for one birth attendant when done manually
aTanzanian National guideline and Managing complications of pregnancy and labour, WHO, 2017 [22, 23]
bNICE guideline: Intrapartum care for healthy women and babies clinical guideline, 2022 [2]
cMédecins Sans Frontiers (MSF): intrapartum guideline [24]
dWHO: Labour care guide, 2019. Normal labour progression is said to be hyperbolic therefore included as 0.2–0.5 cm/hours [25]
eWHO: Recommendations for augmentation of labour, 2014 [5]
Data collection
Data were collected between March 15th 2021 and February 15th 2022 (Table 2). We combined three methods: (i) 220 h of unstructured observations and informal conversations with staff to explore labour ward practices; (ii) 13 in-depth individual semi-structured interviews (Additional file 1) to explore birth attendants’ perceptions and (iii) 234 structured observations of labours by two research assistants to quantify oxytocin practices (timing, titration etc.).
Table 2.
Data collection methods
| Data collection methods | Period |
|---|---|
| 220 h unstructured observations by MLK | 15.03.2021 – 11.06.2021 |
| 234 Structured observations by two research assistants | 01.04.2021 – 31.06.2021 |
| 11 Individual in-depth interviews by MLK and a research assistant | 01.04.2021 – 11.06.2021 |
| Two individual in-depth reinterviews by MLK | 05.01.2022 – 15.02.2022 |
Observations were conducted equally during days, evenings and nights over three months. Extensive field notes were written during and after observations. Although being a medical doctor, MLK had no license to practice clinically within this setting and did not make clinical decisions during observations. Structured observations were carried out by two Swahili-speaking research assistants with no obstetric experience. Observed care practices were noted in pre-piloted sheets (Additional file 2). Women were included in active labour and followed till birth. Inclusion happened consecutively during each observation period and was limited to singleton cephalic pregnancies at term with positive foetal heart rate on admission. Women who were referred and women with hypertensive disorders or previous caesarean section were excluded. We aimed to study oxytocin use among a low-risk population to avoid competing factors influencing the administration of oxytocin. MLK and a Swahili-speaking research assistant conducted interviews through purposive sampling until no new topics appeared. The interview guide was adjusted after the first two interviews. Respondents included nurse-midwives (n = 3), intern doctors (n = 2), registrars (n = 3) and obstetric specialists (n = 3), all working in the labour ward at the time. Re-interviews with two respondents were conducted one year later to explore preliminary analytical findings. All interviews were conducted outside working hours and were audio-recorded, transcribed and translated ad verbatim to English by a trained translator. Translations were checked by two research assistants. To protect anonymity, staff members are referred to as respondents (R) or birth attendants throughout the text. In this manuscript, oxytocin refers to oxytocin for labour augmentation during active labour unless stated otherwise.
Analysis
A thematic network analysis was carried out using a combined deductive and inductive approach where time emerged as a central theme [26]. Text was coded using NVivo (release 1.6.2) and included predefined and emerging themes. Data from observations and interviews were triangulated and basic, organising and global themes were created within the frame of temporality (Table 3). Descriptive statistics using IBM SPSS (version 28.0.0.0) were used to analyse data from structured observations. Rate of oxytocin for labour augmentation was based on all observed women, while a subgroup of women who received oxytocin during the first stage of labour were assessed for timing of oxytocin and monitoring of labour.
Table 3.
Pre-defined and emerging themes based on NVivo coding
| Global and organising themes | Basic themes |
|---|---|
| Time-pressure: realities of an urban congested labour ward | |
| Too many tasks and too little time | Disconnect between time availability and time demands |
| Unrealistic guidelines for labour augmentation with oxytocin | |
| Time-scarcity leading to congestion and prolonged labour | Clash between speed of labour and time-pressure in the busy labour ward |
| Negative experiences and perceptions related to prolonged labour | |
| Impractical partograph in the time-constraint labour ward | Difficult to adhere to requirements, e.g. four-hourly assessment |
| Partograph used to protect against liability/accountability | |
| Partograph often completed after birth | |
| Re-negotiating time: how birth attendants navigate in a busy urban labour ward | |
| Reducing frequencies of care practices | Prioritisation of care practices |
| Substandard care | |
| Speeding up labour leads to better outcomes | Oxytocin used as “crowd control” when labour ward fills up |
| Positive experiences and perceptions related to faster labour | |
| Hospital policy on labour duration | |
| Oxytocin is given in cycles of ward rounds and shifts | Women are mainly assessed during morning ward rounds by doctors and around change of shifts (morning and afternoon) |
| Expectations to handover a decongested labour ward | |
| Less monitoring during the night | |
| An “up-tempo” labour ward | |
| Oxytocin practices | Timing of oxytocin |
| Low alertness towards risks of oxytocin | |
| Fear of prolonged labour | |
Findings
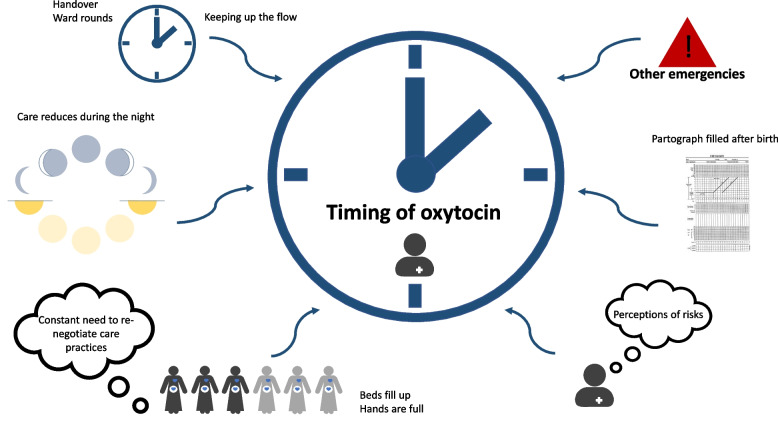
Three global, seven organising and 17 basic themes emerged from the analysis and all related to temporality (Table 3). Our findings are structured around the three global themes. Figure 1 shows the conceptual framework, which was developed from the results of our analysis.
Fig. 1.
Conceptual framework on how time factors shape practices around oxytocin for labour augmentation
Use of oxytocin was often not based on labour progression or partograph. Number of women and staff, time of the day, ward-rounds and shifts turn-over created cycles with moments where oxytocin use accelerated, sometimes leaving all women on a drip, while at other times, when the ward was too busy or during nighttime, oxytocin was given too late. Perceptions related to risks of prolonged labour and oxytocin further facilitated its use
Time-pressure: the reality of an urban congested labour ward
“It was busy, everyone was running around. Nobody kept an overview, it was impossible because the women were everywhere, constantly crying for help: “Nurse, nurse, nurse, come”. It was stressful and overwhelming. Everyone did their best and all hands were in use. Two women were pushing with assistance from students, a woman had just given birth but there was no time to clean up and help her get settled with her newborn. A foetal head was crowning in bed three, but there was no birth attendant to assist. In another bed the drip with oxytocin was running, the woman unattended. An assistant was running with birth trays and medication for prevention of haemorrhage. There were not enough suturing sets, so the intern doctor struggled to repair a bleeding tear. All hands were in use, care was limited to what was most necessary. After a few hours the labour ward became less chaotic. Exhaustion filled the room. Now the paperwork had to be filled, stocks recharged and curtains and floors cleaned for blood. Until the next wave of women filled the beds.” (Observation notes 01.04.21).
This extract describes the extreme time scarcity in the labour ward, weighing heavily on the birth attendants, who often referred to the inability to do what was required. Time scarcity in the congested labour ward was a dominating theme throughout the study and explained to cause neglect and harm: “It often happened that women were here for days because there was no overview of the too many women. Then we had bad outcomes, it was always like that” (Respondent (R) 2). Neglected prolonged labour appeared to have become a symbol of the dangerously congested and time-pressured labour ward. Thus, tackling prolonged labour had become a key strategy both at management levels and in day-to-day clinical work.
Time scarcity also influenced the ability to use the partograph. Although the partograph was viewed as a useful tool by birth attendants, it was rarely used for decision-making to time labour augmentation. For example, during observations, not all vaginal examinations were plotted on the partograph: “The nurse did not record the vaginal examination. She explained that she was not supposed to do an examination before four hours, so therefore it would be wrong to write it on the partograph (since only two hours had passed)” (observation notes 27.03.21). Correct filling of the partograph required four-hourly examinations and half-hourly monitoring, which was often impossible. Rather than using it for decision-making, staff filled the partograph so they could not be accused of mismanagement. It was, therefore, not unusual to see nurses meticulously filling it after the woman had given birth, with FHR and contractions that they never assessed.
As Table 1 illustrates, safe and timely administration of oxytocin for labour augmentation would require one-to-one care. In this congested labour ward, one to three birth attendants had to look after up to 16 women simultaneously while also having many other tasks. Consequently, guidelines were largely unattainable and therefore constantly, either deliberately or subconsciously, negotiated and prioritised to manage in time.
Re-negotiating time: how birth attendants navigate in a busy urban labour ward
Birth attendants had found their own ways to deal with the time-pressured labour ward. This section details their time management strategies.
It was generally understood that oxytocin reduces labour duration and therefore resulted in a faster flow of labouring women through the ward. Use of oxytocin for labour augmentation was, therefore, a way to manage time by decongesting the labour ward. The necessity of applying oxytocin when the labour ward got busy and beds started to fill up, was the most frequently mentioned reason for applying oxytocin. As one birth attendant explained “Oxytocin can be dangerous, but I believe that it is more dangerous if we have a congested labour ward where staff cannot monitor the women. We used to see much neglect at these times” (R4). In this way, applying oxytocin was perceived as a tool to negotiate time to provide better care by shortening the duration of labour. As a response to the harmful congestion, the hospital had made an internal standard operating guideline by which nulliparous women in active labour should give birth within eight hours and multiparous women within six hours. This guideline was unanimously viewed as helpful by birth attendants. Even though limits were flexible, this practice shows that negotiation of time had become interwoven into hospital procedures, ensuring that birth attendants would keep a steady flow of birthing women.
Efforts to manage time also resulted in the dropping of several time-consuming clinical practices. For instance, structured observations showed that only 3/42 women (7.1%) had contractions and 5/42 (11.9%) had FHR measured when receiving oxytocin for augmentation (Table 4). One birth attendant explained: “How is it possible to monitor contractions for ten minutes when we have so many women in labour” (R1). Also, titration of oxytocin was often neglected. Most birth attendants knew that oxytocin had to be titrated and detailed titration plans were commonly observed in case-notes. Birth attendants had no explanation as to why it did not happen. As one doctor said “I have never seen anyone titrating. You know it from school, but in hospitals, no, it doesn’t happen…” (R12). Noteworthy, some birth attendants claimed to titrate oxytocin, but were rarely observed to do so. Instead, unstructured observations showed that oxytocin drips were often almost blindly (without counting drops) increased or decreased without reference to contractions and FHR. Limited titration could reflect how cumbersome this practice was without electronic infusion pumps in a busy labour ward. These deviations from clinical guidelines illustrate how birth attendants tinkered with practices around oxytocin administration to navigate time-pressure.
Table 4.
Structured observations of 234 consecutive women in active labour
| All women | 234 |
| Characteristics | |
| Age, mean, SD | 25.5 (± 5.1) |
| n (%) | |
| Parity | |
| Nulliparous | 98 (41.9) |
| Multiparous | 136 (58.1) |
| Mode of birth | |
| Spontaneous vaginal birth | 224 (95.7) |
| Vacuum-assisted birth | 8 (3.4) |
| Caesarean section | 2 (0.9) |
| Oxytocin for labour augmentation | |
| No | 88 (37.6) |
| Yes | 146 (62.4) |
| Initiated during 1st stage | 100 (68.5) |
| Initiated during 2nd stage | 46 (31.5) |
| Duration of active laboura | |
| < 6 h | 166 (77.6) |
| 6 – 12 h | 39 (18.2) |
| > 12 h | 9 (4.2) |
| Missing | 20 |
| Birth outcome | |
| Discharged home | 214 (92.3) |
| Admitted into neonatal intensive care unit | 13 (5.6) |
| Stillbirth | 4 (1.7) |
| Neonatal death < 24 h | 1 (0.4) |
| Missing | 2 |
| Birth outcome in cases with oxytocin augmentation | 146 |
| Discharged home | 132 (90.4) |
| Admitted into neonatal intensive care unit | 8 (5.4) |
| Stillbirth | 3 (2.1) |
| Neonatal death < 24 h | 1 (0.7) |
| Missing | 2 (1.4) |
| Subgroup of women who received oxytocin during 1st stage of active labour | 58b |
| n (%) | |
| Contractions measured | |
| Yes | 3 (7.1) |
| No | 39 (92.9) |
| Missing | 16 |
| Fetal heart rate (FHR) measured | |
| Yes | 5 (11.9) |
| No | 37 (88.1) |
| Missing | 16 |
| Oxytocin rate adjusted | |
| None | 28 (48.3) |
| Once | 24 (41.4) |
| ≥ 2 times | 6 (10.3) |
| Time between active labourc and initiation of oxytocin | |
| < 2 h | 15 (28.3) |
| 2 – 4 h | 19 (35.8) |
| > 4 h | 19 (35.8) |
| Missing | 5 |
| Labour progression on initiation of oxytocind | |
| ≤ 0.5 cm/hour | 27 (56.2) |
| > 0.5 cm/hour | 21 (43.8) |
| Missing | 10 |
Legend: Data include consecutive structured observations of birthing women with low risk pregnancies
aDefined as first cervical dilatation of 4 cm and above until birth of the child
bOnly includes labours where time of oxytocin initiation was observed
cDefined as cervical dilatation of 4 cm and above
dMeasured as dilatation/hour from first cervical dilatation of 4 cm and above to time of administration of oxytocin
Birth attendants also navigated the, at times, overwhelmingly busy and unpredictable environment by adhering to the ‘natural labour ward cycles’ instead of using time-demanding surveillance cycles of individual women with reference to their partograph. Hence, labour progression was assessed mainly during ward rounds (10–12 am) and around handovers between shifts (7–8 am and 2–3 pm) or on demand (e.g., a birthing woman starting to push or a filled labour ward). It was observed on several occasions that particularly doctors were action-oriented in their management during ward rounds. They often ordered obstetric interventions (e.g., oxytocin) to enhance labour despite uncomplicated progression. When asked, one doctor explained: “Because it can become very busy as the day progresses, we never know when we are able to come back. So many hours can pass before someone is checking the woman. If I come in the morning and again in the afternoon, I know that the women who are still here have been there too long” (R7). This illustrates how birth attendants had found a system to navigate time and avoid delaying care.
Too early interventions also happened, because birth attendants were encouraged to hand over a “clean” labour ward (referring to a less crowded ward) for the next shift: “We always tell them to make sure the women in their shift give birth. That is their responsibility, these women. This is how we avoid women are there during one, two or three shifts” (R12). According to the staff, this was a helpful division because it ensured that women would not stay during several shifts. These are examples of how attempts to manage time pressure were built into existing systems. On other occasions, these natural cycles were broken because it was too busy and women were at risk of delayed care. In the morning, it sometimes happened that women had been in labour overnight without receiving appropriate interventions. For example, one woman progressed 2 cm over 17 h, without the membranes being ruptured or oxytocin given. The following day she gave birth two hours after augmentation with oxytocin was started. Surprisingly, delayed care also happened during calm moments, where care tended to be more passive and less action-oriented: “There was only one woman in labour. The birth attendant was on his/her phone while another was sleeping. I knew that time for vaginal examination was overdue, but nobody seemed to notice” (field notes, 28.3.21). This illustrates how the natural labour ward cycles had replaced structured timekeeping even when there was time.
An up-tempo labour ward
Table 4 presents data from 234 structured labour observations and includes background characteristics and birth outcomes. Data will be presented in this section to triangulate the qualitative findings on how oxytocin was used for labour augmentation.
The urge to speed up labour resulted in 146/234 (62.4%) women in active labour receiving oxytocin for labour augmentation (Table 4). Of a subgroup of women augmented in the first stage of labour, 21/48 (43.8%) had labour progressing faster than 0.5 cm per hour at the time oxytocin was applied and 5/48 (10.4%) faster than 1 cm per hour. International clinical guidelines recommend that vaginal examination should take place no more than four-hourly in uncomplicated labour. We observed, however, that 34/53 (64.1%) women received oxytocin within four hours of active labour and 15/53 (28.3%) even within two hours (Table 4).
Exploring substandard monitoring of women on oxytocin revealed that birth attendants had little awareness of the risks associated with oxytocin. Birth attendants used expressions like “Why not speed up labour, if you can” (R4) and referred to oxytocin as a way of helping women give birth faster. One birth attendant described the events of a woman with a stillborn baby: “He [the doctor] even added an extra bottle of oxytocin [to help the baby]” (R5). This showed the perceived harmlessness of oxytocin, which is crucial in understanding why injudicious use had developed. In contrast, experiences related to delay in care seemed to have a strong impact on birth attendants. They had daunting memories from the past when the labour ward had been busier, with women presenting from home whilst having been in labour for several days and with a dead foetus in utero. When adverse outcomes happened, prolonged labour was seen as a determinant while oxytocin was considered helpful. These perceptions persisted even though experiences of such horrifying delays mostly belonged to the past. In fact, during the structured labour observations, prolonged labour was a rare event: only 9/214 (4.2%) women were in active labour for more than 12 h, while 166/214 (77.6%) were in active labour for less than 6 h (Table 4). These findings crucially show how efforts to bring flow to the labour ward and avoid prolonged labour had been successful, but to an extent where oxytocin was given even in the absence of prolonged labour largely detached from individual women’s needs. What remains to be explored is what the consequences of such “up-tempo” labour ward management are in terms of caesarean sections and foetal outcomes. Four of five perinatal deaths happened in the oxytocin group (Table 4). It is, however, beyond the scope of this study to assess causal associations.
Discussion
In the study’s high-volume, urban maternity ward with severe time scarcity and shortage of staff, birth attendants were forced to renegotiate care practices. Of the 234 women in active labour, 146 (62.4%) received oxytocin for labour augmentation, most often despite uncomplicated labour progress. Several time factors influenced oxytocin use (Fig. 1). The strongest driver was to fasten labour when the ward became too busy or to prevent overcrowding. In the absence of electronic monitoring devices, many women received oxytocin at unregulated doses with little monitoring. In many ways, birth attendants found augmentation of labour with oxytocin a preferred choice: it was perceived to prevent congestion and responded to the fear of prolonged labour, while there appeared to be little focus on potential oxytocin-mediated risks. Importantly, among the 234 observed women, only nine were in active labour for > 12 h (4.2%) and prolonged labour was a rare complication. This illustrates how efforts to avoid dangerous congestion and delayed care had been successful, but consequently resulted in overuse of oxytocin with little reference to individual women’s needs.
Navigating time-pressure in maternity care globally
Time pressure is not unique to this labour ward. Hospital environments globally face increasing demands for providing constantly better care without a simultaneous increase in resources [27]. High-volume understaffed hospitals are increasingly common in cities of LLMIC as urbanisation continues, and communities increasingly respond to the push for facility births [16, 28]. As reported from Egypt and India, we argue that overburdened time-pressured mega maternity units are a crucial driver of the overuse of oxytocin and likely a driver of urban disadvantages in maternal health [28]. Reporting a 50% deficiency in health workforce, literature increasingly reports poor health outcomes in Dar es Salaam, one of the fastest-growing cities of the world [29]. This emphasises, that simply training birth attendants better will not solve overmedicalisation caused by underfunded health care systems. Referring to “tricks of the trade”, Celine et al. emphasised how medical doctors in Switzerland avoided time-consuming practices, just as birth attendants did in our study [30]. They explain how everything that takes time was seen as ‘bumps on the road’. Although effective, if time management becomes the end goal, unintended, less obvious consequences may occur. Oxytocin overuse is an example of an unintended side effect of navigating time pressure. Oxytocin has been shown to reduce labour by two hours. While such a reduction in labour duration may not seem crucial for the individual, administering oxytocin to many women could save time for care and bed space (if not considering the increased need for monitoring). This explains why excess oxytocin can be used as a time management strategy [11, 13, 31]. Birth attendants in our study had been successful in managing congestion and avoiding delayed care, but at a price of overmedicalisation. Recognising that increasing staff-patient ratios must be seen as a central part of the solution in a human resource crisis is therefore important.
With increasing urbanisation and the formation of mega-cities, such as Dar es Salaam, the time lens could become a crucial tool to understand care provision in these settings more broadly. This requires investigating time scarcity including health provider-to-patient ratio and the gap between guidelines and reality, as well as strategies that health providers use to navigate time pressure.
Normalisation of deviance
While time pressure appeared to be a key driver of overusing oxytocin for labour augmentation, practices remained, even when the labour ward was calm. This emphasises the complexity of deviations from the clinical guidelines [32]. Drawing on previous literature which describes the process of normalisation of deviance, three factors appear central: 1) unrealistic clinical guidelines and structures requiring deviation, 2) low alertness to harmful effects and 3) limited accountability measures [33]. These factors are elaborated in the context of labour augmentation with oxytocin [34].
First, the current guidelines for oxytocin use are cumbersome and not made for settings with a shortage of staff and no electronic devices to dose or monitor oxytocin. Therefore, birth attendants have to find alternative ways that work for them. Adaptations happen all the time in complex, imperfect hospital settings, but as Freedman emphasises, more commonly in low-resource settings [35, 36]. The further away from reality clinical guidelines are, the harder they are to adapt, and adaptations may become unintentionally harmful [37]. When adapted, evidence from which the guidelines were originally based, may no longer be applicable. Deviant practices often start with small changes that move further away from the intended use [33]. It is likely that the current deviations in this labour ward are a result of many years of adjustment to meet continuous congestion with constantly fewer resources [16].
Second, the scarcity of evidence of adverse effects results in low alertness toward oxytocin [3]. Collectively, because of the bad experiences with prolonged labour, clinicians blamed labour duration rather than oxytocin when adverse events occurred. Behavioural scientist Soyer and psychologist Hogart unfold this well-known phenomenon in their article “Fooled by experience” [38]. Additionally, RCTs including oxytocin were small and not powered to investigate rare events which further downplays the risk of oxytocin [1, 39–44].
Finally, the low focus on substandard, unrestricted and unaudited use reflects the limited accountability for oxytocin. In contrast, birth attendants were held accountable for perfectly filled partographs, where prolonged labour was not accepted. Meanwhile, oxytocin was freely available and mostly in stock in the fridge next to the labour ward. While this may increase life-saving oxytocin for third stage of labour, it may have facilitated liberal use during labour. Establishing accountability measures that hold birth attendants accountable for realistic oxytocin guidelines based on the partograph as a decision, and not a liability tool, thus, seems crucial.
Improving the use of oxytocin in this labour ward requires de-normalising its use. Consequently, we recommend addressing the congestion of urban high-volume labour wards, as this fundamentally sustains excessive oxytocin use. We further emphasise the sensitisation of oxytocin as a high-alert medication, while global evidence is crucially needed to unfold the risk profile and long-term effects of oxytocin stratified in low-, middle- and high-income countries. Meanwhile, the development of realistic oxytocin guidelines for low-resource settings is crucial for providing safer use.
A few studies from LLMIC have succeeded in reducing oxytocin use. A Tanzanian study decreased labour augmentation with oxytocin from 22 to 12% after implementing context-adjusted guidelines co-created with frontline health workers and three-monthly seminars (the PartoMa intervention) [7, 45]. The guideline restricted oxytocin to women crossing the partograph’s action line [7]. An Indian study reported a reduction in oxytocin from 78 to 32% after implementing a coaching-based intervention using the WHO childbirth checklist which prohibits routine oxytocin for labour augmentation altogether [31]. Oxytocin, however, increased to 48% six months after the intervention had ended [31]. Finally, a study from a Palestinian hospital reported a decrease in the use of oxytocin for labour augmentation from 32.1 to 10.9% after implementing a multifaceted intervention [46]. The intervention consisted of on-the-job training 2–3 days a week, audit of practices, feedback during interactive audit meetings every 2–3 months, five training workshops and informal meetings with managers and midwives to understand barriers and providers’ opinions of the intervention [46]. Two years post-implementation the oxytocin rate, however, increased to 17% [46]. None of these interventions negatively affected caesarean section rates or birth outcomes. Concludingly, it appears that reducing use of oxytocin for labour augmentation is possible through clinical guidelines and training but contextual factors that withhold its use, such as crowded labour wards, must be tackled to make changes sustainable.
Strengths and limitations
Our mixed-methods design allowed a deeper understanding of the mechanisms which shape practices around labour augmentation with oxytocin. The primary researcher’s position as an “outsider” with obstetric experience from another setting and our diverse author group appeared crucial in recognizing and reflecting on deviant normalized practices. BSD, MA and DN have in-depth clinical experience from the study hospital ensuring findings were recognizable. Translated transcripts have limitations since nuances may have been missed in the translation process. Observations may be subject to the Hawthorne effect where birth attendants performed better than they would usually. Though assistants were not trained obstetricians and had no reason to over- or underestimate oxytocin observer’s bias cannot be ruled out. We included only women with low-risk pregnancies and quantitative findings are therefore comparable to this population primarily. Underlying perceptions and culture are specific to this labour ward with limited generalizability. Our findings are of interest to other LLMICs where congestion is an issue. Rural hospitals may experience underuse of oxytocin due to absence of staff, lack of storage capacity, stock-outs of oxytocin or low quality of oxytocin. Findings, however, are of global health concern, as unindicated oxytocin use is also increasingly observed in HIC [43, 47–49].
Conclusion
In this labour ward, almost two out of three women in active labour received oxytocin for labour augmentation, most with uncomplicated labour progress and limited monitoring and titration. Overcrowding appeared to be the strongest driver, forcing birth attendants to keep up the flow in the busy labour ward by using oxytocin as a decongestion tool. Low alertness towards oxytocin-mediated risks, along with fear of prolonged labour, further facilitated liberal oxytocin use. Evidence-based, context-adjusted training and guidelines for prolonged labour management in time-pressured labour wards are required to avoid medically unindicated use of oxytocin. Further, myths and perceptions must be addressed to de-normalise its use. With increasing urbanisation, facility births and the formation of mega-cities, the time lens could become a crucial tool to understand the effect of time pressure and congestion on care practices in low-resource settings more broadly.
Supplementary Information
Acknowledgements
Dorkasi L. Mwakawanga, Assistant Lecturer, School of Nursing-Muhimbili University of Health and Allied Sciences.
Bavelyne Machumu, Kilimanjaro Clinical Research Institute.
Siah Hakim Nyange, Management and Development for Health—Temeke Regional Referral Hospital.
Abbreviations
- LLMIC
Low- and lower-middle-income countries
- LIC
Low-income countries
- HIC
High-income countries
- FHR
Fetal heart rate
- WHO
World Health Organisation
Authors’ contributions
MLK, JBS, MS, EP, NM, TvdA and FK contributed to the conception and design of the work. MLK, MS, JBS and DN contributed to the acquisition, analysis, interpretation of data. MLK drafted the manuscript. All authors substantively revised the draft. All authors have approved the submitted version (and any substantially modified version that involves the author's contribution to the study). All authors have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Funding
Funding was obtained from: Danida Research Fellowship Centre, Laerdal Foundation, Thorvald Madsens Legat, Bodil Pedersen Fonden and Reinholt W. Jorcks Fond.
The funding sources had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets are not publicly available due to privacy of respondents, but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
All respondents for interview gave their written informed consent. Informed verbal consent was obtained from women and staff during observations. The research project, including verbal consent, received ethical approval from the ethics committee of the Tanzanian National Institute for Medical Research (NIMR) through the Tanzanian National Health Research Ethics Review Sub-Committee (NatHREC) (NIMR/HQ/R.8a/Vol. IX/3324) (approval of protocol) and NIMR/HQ/P.12VOLXXXV/111 (permission to publish). Approvals were obtained from the Ministry of Health, Tanzania and facility management. Methods were performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests, apart from Jos van Roosmalen, who is a senior board member of BMC Pregnancy Childbirth.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bugg GJ, Siddiqui F, Thornton JG. Oxytocin versus no treatment or delayed treatment for slow progress in the first stage of spontaneous labour. Cochrane Database Syst Rev. 2013;6:CD007123. [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Health and Care Excellence (NICE). Intrapartum care for healthy women and babies. NICE Clinical Guidelines. 2022; No 190. [PubMed]
- 3.Kujabi ML, Mikkelsen E, Housseine N, Obel J, D’Mello BS, Meyrowitsch DW, et al. Labor augmentation with oxytocin in low- and lower-middle-income countries: a systematic review and meta-analysis. AJOG global reports. 2022;2:100123. 10.1016/j.xagr.2022.100123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burgod C, Pant S, Morales MM, Montaldo P, Ivain P, Elangovan R, et al. Effect of intra-partum oxytocin on neonatal encephalopathy: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2021;21:736. 10.1186/s12884-021-04216-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organisation. WHO recommendations for augmentation of labour. WHO library; 2014. ISBN 978 92 4 150736 3.
- 6.World Health Organization. World health organization partograph in management of labour. Lancet. 1994;343:1399–404. [PubMed] [Google Scholar]
- 7.Maaløe N, Housseine N, Meguid T, Nielsen BB, Jensen AKG, Khamis RS, et al. Effect of locally-tailored labour management guidelines on intrahospital stillbirths and birth asphyxia at the referral hospital of Zanzibar: a quasi-experimental pre-post-study (the PartoMa study). BJOG. 2018;125:235–45. 10.1111/1471-0528.14933 [DOI] [PubMed] [Google Scholar]
- 8.Deepak NN, Mirzabagi E, Koski A, Tripathi V. Knowledge, attitudes, and practices related to uterotonic drugs during childbirth in Karnataka, India: a qualitative research study. PLoS One. 2013;8:e62801. 10.1371/journal.pone.0062801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mirzabagi E, Deepak NN, Koski A, Tripathi V. Uterotonic use during childbirth in Uttar Pradesh: accounts from community members and health providers. Midwifery. 2013;29:902–10. 10.1016/j.midw.2012.11.004 [DOI] [PubMed] [Google Scholar]
- 10.Koski A, Mirzabagi E, Cofie P, Tripathi V. Uterotonic use at childbirth in Ghana: a qualitative study of practices, perceptions, and knowledge among facility-based health care providers and community members. Int J Childbirth. 2014;4:25–38. 10.1891/2156-5287.4.1.25 [DOI] [Google Scholar]
- 11.Van Hollen C. Invoking vali: painful technologies of modern birth in south India. Med Anthropol Q. 2003;17:49–77. 10.1525/maq.2003.17.1.49 [DOI] [PubMed] [Google Scholar]
- 12.Forna F, Titulaer P, Sesay S, Conteh S, Muoghalu S, Kanu P, et al. Prevalence of use of highly concentrated oxytocin or “pepper injection” in labor among clinicians undergoing emergency obstetric training in Sierra Leone. Int J Gynecol Obstet. 2020;151:450–5. 10.1002/ijgo.13354 [DOI] [PubMed] [Google Scholar]
- 13.Khalil K, Cherine M, Elnoury A, Sholkamy H, Breebaart M, Hassanein N. Labor augmentation in an Egyptian teaching hospital. Int J Gynaecol Obstet. 2004;85:74–80. 10.1016/S0020-7292(03)00311-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sørensen JB, Housseine N, Maaløe N, Bygbjerg IC, Pinkowski Tersbøl B, Konradsen F, et al. Scaling up locally adapted clinical practice guidelines for improving childbirth care in Tanzania: a protocol for programme theory and qualitative methods of the PartoMa scale-up study. Glob Health Action. 2022;15:2034136. 10.1080/16549716.2022.2034136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maaløe N, Housseine N, Sørensen JB, Obel J, Sequeira DMello B, Kujabi ML, et al. Scaling up context-tailored clinical guidelines and training to improve childbirth care in urban, low-resource maternity units in Tanzania: a protocol for a stepped-wedged cluster randomized trial with embedded qualitative and economic analyses (the PartoMa scale-up study). Glob Health Action. 2022;15:2034135. 10.1080/16549716.2022.2034135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sequeira Dmello B, Sellah Z, Magembe G, Housseine N, Maaløe N, Van Den Akker T, et al. Learning from changes concurrent with implementing a complex and dynamic intervention to improve urban maternal and perinatal health in Dar es Salaam, Tanzania, 2011–2019. BMJ Glob Health. 2021;6:e004022. 10.1136/bmjgh-2020-004022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dmello BS, Housseine N, van den Akker T, van Roosmalen J, Maaløe N. Impact of COVID-19 on maternal and child health. Lancet Glob Health. 2020;8:e1259. 10.1016/S2214-109X(20)30328-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miltenburg AS, Kiritta RF, Meguid T, Sundby J, et al. Quality of care during childbirth in Tanzania: identification of areas that need improvement. Reprod Health. 2018;15:14. 10.1186/s12978-018-0463-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Housseine N, Punt MC, Mohamed AG, Said SM, Maaløe N, Zuithoff NPA, et al. Quality of intrapartum care: direct observations in a low-resource tertiary hospital. Reprod Health. 2020;17:1–11. 10.1186/s12978-020-0849-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maaløe N, Housseine N, Bygbjerg IC, Meguid T, Khamis RS, Mohamed AG, et al. Stillbirths and quality of care during labour at the low resource referral hospital of Zanzibar : a case-control study. BMC Pregnancy Childbirth. 2016;16:1–12. 10.1186/s12884-016-1142-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adam B. Of timescapes, futurescapes and timeprints. Lüneburg Talk Web. 2008;070708:1–9.
- 22.World Health Organization. Managing complications in pregnancy and childbirth: a guide for midwives and doctors – 2nd ed. Geneva; 2017. ISBN 978-92-4-156549-3
- 23.The United Republic of Tanzania, ministry of health, community development, gender, elderly and children. Clinical practice guidelines on appropriate use of uterotonics: for post-abortion care, induction of labour, prevention and treatment of postpartum haemorrhage. 2019.
- 24.Médecins Sans Frontières. Essential obstetric and newborn care practical guide for midwives, doctors with obstetrics training and health care personnel who deal with obstetric emergencies. 2019. [Google Scholar]
- 25.World Health Organization. WHO labour care guide: user’s manual. Geneva; 2020.
- 26.Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual Res. 2001;1:385–405. 10.1177/146879410100100307 [DOI] [Google Scholar]
- 27.How can health services keep pace with the rapid growth of cities? | Healthcare Network | The Guardian. https://www.theguardian.com/sustainable-business/2017/feb/24/how-can-health-services-keep-pace-with-the-rapid-growth-of-cities. Accessed 12 Dec 2022.
- 28.Save the Children. The urban disadvantage: state of the world’s mothers. 2015. [Google Scholar]
- 29.Norris M, Klabbers G, Pembe AB, Hanson C, Baker U, Aung K, et al. A growing disadvantage of being born in an urban area? Analysing urban–rural disparities in neonatal mortality in 21 African countries with a focus on Tanzania. BMJ Glob Health. 2022;7:e007544. 10.1136/bmjgh-2021-007544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Céline B, Matteo M, Michael S, Friedrich S, Vanessa K, David G, et al. Running against the clock: a qualitative study of internal medicine residents’ work experience. Swiss Med Wkly. 2022;152:w30216. 10.4414/SMW.2022.w30216 [DOI] [PubMed] [Google Scholar]
- 31.Marx Delaney M, Kalita T, Hawrusik B, Neal B, Miller K, Ketchum R, et al. Modification of oxytocin use through a coaching-based intervention based on the WHO safe childbirth checklist in Uttar Pradesh, India: a secondary analysis of a cluster randomised controlled trial. BJOG. 2021;128:2013–21. 10.1111/1471-0528.16856 [DOI] [PubMed] [Google Scholar]
- 32.Baartmans MC, Hooftman J, Zwaan L, van Schoten SM, Erwich JJHM, Wagner C. What can we learn from in-depth analysis of human errors resulting in diagnostic errors in the emergency department: an analysis of serious adverse event reports. J Patient Saf. 2022;18:e1135–41. 10.1097/PTS.0000000000001007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Price MR, Williams TC. When doing wrong feels so right: normalization of deviance. J Patient Saf. 2018;14:1–2. 10.1097/PTS.0000000000000157 [DOI] [PubMed] [Google Scholar]
- 34.Clark SL, Simpson KR, Knox GE, Garite TJ. Oxytocin: new perspectives on an old drug. Am J Obstet Gynecol. 2009;200:35.e1-35.e6. 10.1016/j.ajog.2008.06.010 [DOI] [PubMed] [Google Scholar]
- 35.The elusive quest: accountability in hospitals - Carolyn L. Wiener. https://books.google.dk/books?hl=da&lr=&id=MoeeDXObhk8C&oi=fnd&pg=PR11&ots=2Cg1RukT7F&sig=qCtxYnObmbTTmhb_8JI_hN10AMg&redir_esc=y#v=onepage&q&f=false. Accessed 28 Nov 2022.
- 36.Freedman LP. Implementation and aspiration gaps: whose view counts? Lancet. 2016;388:2068–9. 10.1016/S0140-6736(16)31530-6 [DOI] [PubMed] [Google Scholar]
- 37.Maaløe N, Ørtved A, Sørensen J, Sequeira Dmello B, van den Akker T, Kujabi M, et al. The injustice of unfit clinical practice guidelines in low-resource realities. Lancet Glob Health. 2021;9:e875–9. 10.1016/S2214-109X(21)00059-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Soyer E, Hogarth R. Fooled by experience. Harv Bus Rev. 2015;May:72–7.
- 39.Berglund S, Grunewald C, Pettersson H, Cnattingius S. Severe asphyxia due to delivery-related malpractice in Sweden 1990–2005. BJOG. 2008;115:316. 10.1111/j.1471-0528.2007.01602.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simpson K, James D. Effects of oxytocin-induced uterine hyperstimulation during labor on fetal oxygen status and fetal heart rate patterns. Am J Obstet Gynecol. 2008;199:34.e1-34.e5. 10.1016/j.ajog.2007.12.015 [DOI] [PubMed] [Google Scholar]
- 41.Jonsson M, Nordén S, Hanson U. Analysis of malpractice claims with a focus on oxytocin use in labour. Acta Obstet Gynecol Scand. 2007;86:315–9. 10.1080/00016340601181318 [DOI] [PubMed] [Google Scholar]
- 42.Milsom I, Ladfors L, Thiringer K, Niklasson A, Odeback A, Thornberg E. Influence of maternal, obstetric and fetal risk factors on the prevalence of birth asphyxia at term in a Swedish urban population. Acta Obstet Gynecol Scand. 2002;81:909–17. 10.1034/j.1600-0412.2002.811003.x [DOI] [PubMed] [Google Scholar]
- 43.Dalbye R, Bernitz S, Olsen IC, Zhang J, Eggebø TM, Rozsa D, et al. The labor progression study: the use of oxytocin augmentation during labor following Zhang’s guideline and the WHO partograph in a cluster randomized trial. Acta Obstet Gynecol Scand. 2019;98:1187–94. 10.1111/aogs.13629 [DOI] [PubMed] [Google Scholar]
- 44.Rossen J, Østborg T, Lindtjørn E, Schulz J, Eggebø T. Judicious use of oxytocin augmentation for the management of prolonged labor. Acta Obstet Gynecol Scand. 2016;95:355–61. 10.1111/aogs.12821 [DOI] [PubMed] [Google Scholar]
- 45.Maaløe N, Meguid T, Housseine N, Kragelund Nielsen K, van Roosmalen JJM, Bygbjerg IC, et al. Locally-adapted intrapartum clinical guidelines in Zanzibar’s tertiary hospital, United Republic of Tanzania. Lessons from the field. Bull World Health Organ. 2019;97:365–70. 10.2471/BLT.18.220830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hassan S, Sundby J, Husseini A. Translating evidence into practice in childbirth: a case from the occupied Palestinian territory. Women and Birth. 2013;26:e82–9. 10.1016/j.wombi.2012.12.002 [DOI] [PubMed] [Google Scholar]
- 47.Selin L, Almström E, Wallin G, Berg M. Use and abuse of oxytocin for augmentation of labor. Acta Obstet Gynecol Scand. 2009;88:1352–7. 10.3109/00016340903358812 [DOI] [PubMed] [Google Scholar]
- 48.Gaudernack LC, Frøslie KF, Michelsen TM, Voldner N, Lukasse M. De-medicalization of birth by reducing the use of oxytocin for augmentation among first-time mothers - a prospective intervention study. BMC Pregnancy Childbirth. 2018;18:1–9. 10.1186/s12884-018-1706-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Girault A, Blondel B, Goffinet F, le Ray C. Frequency and determinants of misuse of augmentation of labor in France: a population-based study. PLoS One. 2021;16:e0246729. 10.1371/journal.pone.0246729 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets are not publicly available due to privacy of respondents, but are available from the corresponding author on reasonable request.