Abstract
Purpose of the Review
In the last decade, an increasing trend towards a supposedly healthier vegan diet could be observed. However, recently, more cases of allergic reactions to plants and plant-based products such as meat-substitution products, which are often prepared with legumes, were reported. Here, we provide the current knowledge on legume allergen sources and the respective single allergens. We answer the question of which legumes beside the well-known food allergen sources peanut and soybean should be considered for diagnostic and therapeutic measures.
Recent Findings
These “non-priority” legumes, including beans, pea, lentils, chickpea, lupine, cowpea, pigeon pea, and fenugreek, are potentially new important allergen sources, causing mild-to-severe allergic reactions. Severe reactions have been described particularly for peas and lupine. An interesting aspect is the connection between anaphylactic reactions and exercise (food-dependent exercise-induced anaphylaxis), which has only recently been highlighted for legumes such as soybean, lentils and chickpea. Most allergic reactions derive from IgE cross-reactions to homologous proteins, for example between peanut and lupine, which is of particular importance for peanut-allergic individuals ignorant to these cross-reactions.
Summary
From our findings we conclude that there is a need for large-scale studies that are geographically distinctive because most studies are case reports, and geographic differences of allergic diseases towards these legumes have already been discovered for well-known “Big 9” allergen sources such as peanut and soybean. Furthermore, the review illustrates the need for a better molecular diagnostic for these emerging non-priority allergen sources to evaluate IgE cross-reactivities to known allergens and identify true allergic reactions.
Keywords: Allergen characterization, Anaphylaxis, BAT, FDEIA, Peanut, Soy
Introduction
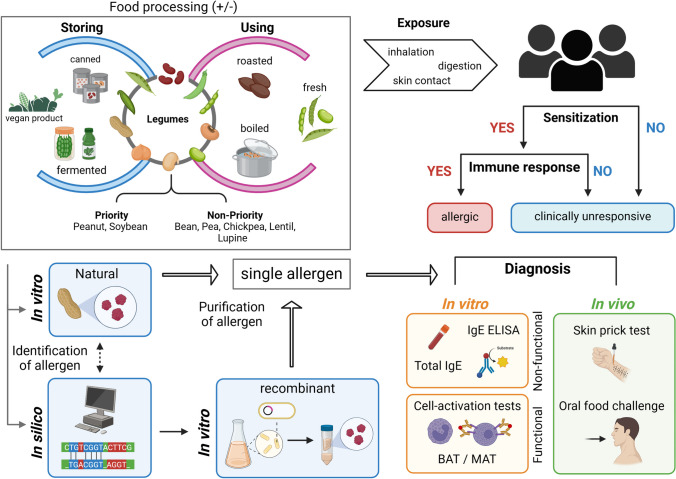
Within the last decade, the demand for plant-based dietary products including legumes has increased drastically, fueled by the rising trend of the vegan diet which is perceived as healthier and more environmentally-friendly [1]. This prompts a crucial question: Is this diet sufficient and devoid of any adverse effects on human health? The family of Leguminosae (legumes) is abundant in proteins, essential nutritional compounds and minerals [2]. In addition, their fiber components were classified as resistant starch that can be broken down by gut bacteria into short-chain fatty acids (SCFAs) which play a crucial role in energy production [3] and also seem to be involved in the maintenance of the skin barrier, reducing susceptibility to allergens [4]. In the last decades, a worldwide rise in cases of allergy was recorded. Reasons for this are complex and maybe related to epigenetic factors influenced by lifestyle, pollution, climate change and other environmental factors. EU regulation 1169/2011 (document 02011R1169-20,180,101) mandates labelling known allergen sources such as soybeans, peanuts and lupines. However, some products may contain unlisted allergens from other sources due to low case numbers of reported allergic reactions. In this review, we focus on the emerging allergens from legumes. But why legumes? Legumes carry allergens of high potency that can trigger intense anaphylactic reactions. These allergens include lipid transfer proteins (LTPs), storage proteins, pathogenesis-related (PR) proteins and structural proteins, which can be resistant to heat and digestive proteases [5, 6]. The change into a more plant-based diet leads to an increased consumption of highly processed plant-based protein products (tofu, soy milk, meat substitute products, etc.) containing concentrated plant proteins, which could trigger allergic symptoms ranging from mild oral allergy syndrome (OAS) to life-threatening anaphylactic reactions [7, 8]. It is crucial to acknowledge that individuals can react differently to allergens depending on the source, consumed status (fresh, boiled/cooked, fried, dried, roasted or fermented) and dietary practices in diverse geographical areas [9, 10]. Different assays and tests are used for allergy diagnostics. The techniques behind them differ depending on the assay (in vivo, in vitro, in silico) (Fig. 1).
Fig. 1.
Legume allergy investigation. Identification of single allergens mainly occurs via protein extraction from whole extracts using sera from well-characterized allergic patients in order to show their IgE-binding capacity in vitro. In addition, the in silico approach can be used. After identification of allergens in a whole extract they are purified from the natural source or produced recombinantly. The purified or recombinant allergen can subsequently be applied in diagnostic tests such as the basophil activation test (BAT) and mast cell activation test (MAT).
Allergen sources from legumes are categorized into two groups: priority and non-priority legumes. The priority group includes the legumes peanuts and soybeans listed within the "Big 9" major food allergens described by the Food and Drug Administration's (FDA). Legumes excluded from the “Big 9” due to low incidence of allergy – the non-priority legume allergen sources – include beans, peas, lentils, chickpeas, lupines, fenugreek, and others. Except for lupine, allergic reactions to these legumes have mostly been described in case reports. As these case reports, however, have accumulated over the past decade or so, this review will put a special emphasis on the non-priority legumes. Details on the legume allergens including tests, molecular weight, allergen source and protein function are presented in Table 1 combining the information from the World Health Organization/International Union of Immunological Societies (WHO/IUIS) Allergen Nomenclature Sub-Committee and the Allergome database. Single legume allergen classifications are listed in Table 2.
Table 1.
Single allergens or allergen homologs identified from legumes
| Species | Known Name | Database | Allergen or allergen homolog |
MW (kDa) |
In vivo |
In vitro (functional) |
In vitro (non-functional) |
Source form | Biological function | Ref |
|---|---|---|---|---|---|---|---|---|---|---|
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 1 | 64 | PST |
MAT BHRA |
IgE & IgE-Immunoblotting & Cross-reactive Carbohydrate Determinant |
Natural & Recombinant |
7S Vicilin-like Globulin | [11–14] |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 1.0101 | 60 | IgE-Immunoblotting | Recombinant | 7S Vicilin-like Globulin | [11, 15–17] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 2 | 17 | PST |
BAT MAT BHRA |
IgE & IgE-Immunoblotting |
Natural & Recombinant |
2S Albumin | [13, 14, 18–22] |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 2.0101 | 16.57 | IgE |
Natural & Recombinant |
2S Albumin | [18, 19, 23, 24] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 2.0201 | 18 | IgE | Recombinant | 2S Albumin | [18, 19] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 3 | 60 | PST |
MAT BHRA |
IgE & IgE-Immunoblotting & Cross-reactive Carbohydrate Determinant |
Natural & Recombinant |
Legumin-like Protein | [12, 13, 18, 25–28] |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 3.0101 | IgE-Immunoblotting | Recombinant | Legumin-like Protein | [25] | |||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 3.0201 | 58.84 | IgE-Immunoblotting | Recombinant | Legumin-like Protein | [18] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 5 | 15 | IgE & IgE-Immunoblotting |
Natural & Recombinant |
Profilin | [18, 29–31] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 5.0101 | 14 | IgE-Immunoblotting | Recombinant | Profilin | [18] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 6 | 15 | PST |
BAT BHRA |
IgE & IgE-Immunoblotting |
Natural & Recombinant |
2S Albumin | [18, 22] |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 6.0101 | 14.5 | BAT | IgE & IgE-Immunoblotting | Recombinant | 2S Albumin | [18] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 7 | 15 | BAT | IgE & IgE-Immunoblotting |
Natural & Recombinant |
2S Albumin | [18, 32, 33] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 7.0101 | < 20 | IgE-Immunoblotting |
Natural & Recombinant |
2S Albumin | [32] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 7.0201 | 17.34 | BAT | IgE-Immunoblotting |
Natural & Recombinant |
2S Albumin | [32, 33] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 7.0301 | 15.7 | IgE-Immunoblotting | Natural | 2S Albumin | [32] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 8 | 17 | BHRA | IgE & IgE-Immunoblotting | Recombinant | PR-Protein | [34–36] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 8.0101 | 17 | IgE-Immunoblotting | Recombinant | PR-Protein | [34] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 8.0201 | 16.28 | IgE-Immunoblotting | Recombinant | PR-Protein | [36] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 9 | 9.8 |
BAT BHRA |
IgE & IgE-Immunoblotting |
Natural & Recombinant |
nsLTP | [37–39] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 9.0101 | 9.13 | BAT | IgE & IgE-Immunoblotting |
Natural & Recombinant |
nsLTP | [37, 38] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 9.0201 | 9.04 | BAT | IgE & IgE-Immunoblotting |
Natural & Recombinant |
nsLTP | [37, 38] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 10 | 16 | BAT/MAT | IgE & IgE-Immunoblotting |
Natural & Recombinant |
Oleosin | [40–42] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 10.0101 | 16 | IgE & IgE-Immunoblotting | Natural | Oleosin | [40, 41] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 10.0102 | 16 | IgE & IgE-Immunoblotting |
Natural & Recombinant |
Oleosin | [40–42] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 11 | 14 | BAT | IgE & IgE-Immunoblotting |
Natural & Recombinant |
Oleosin | [40, 41] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 11.0101 | 14 | IgE & IgE-Immunoblotting |
Natural & Recombinant |
Oleosin | [40, 42] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 11.0102 | 14.35 | IgE & IgE-Immunoblotting | Natural | Oleosin | [40] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 12 | < 12 | BAT | IgE-Immunoblotting | Natural | Defensin | [43] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 12.0101 | 5.19 | BAT | IgE-Immunoblotting | Natural | Defensin | [43] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 13 | < 11 | BAT | IgE-Immunoblotting | Natural | Defensin | [43] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 13.0101 | 5.48 | BAT | IgE-Immunoblotting | Natural | Defensin | [43] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 13.0102 | < 8 | BAT | IgE-Immunoblotting | Natural | Defensin | [43] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 14 | 17.5 | BAT | IgE | Natural | Oleosin | [40, 41] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 14.0101 | 18.435 | BAT | IgE | Natural | Oleosin | [40, 44] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 14.0102 | 18.457 | BAT | IgE | Natural | Oleosin | [40, 44] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 14.0103 | 18.448 | BAT | IgE | Natural | Oleosin | [40] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 15 | 17 | BAT | IgE & IgE-Immunoblotting |
Natural & Recombinant |
Oleosin | [40–42, 45] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 15.0101 | 16.87 | BAT | IgE | Natural | Oleosin | [40] | |
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 16 | 8.5 | IgE-Immunoblotting | Natural | nsLTP | [46] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 16.0101 | 7.01 | IgE-Immunoblotting | Natural | nsLTP | [46] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 17 | 11 | IgE-Immunoblotting | Natural | nsLTP | [46] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 17.0101 | 9.3 | IgE-Immunoblotting | Natural | nsLTP | [46] | ||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 18 | 21 | Natural | Cyclophilin—peptidyl-prolyl cis–trans isomerase | [47] | |||
| Arachis hypogaea | Peanut | WHO/IUIS | Ara h 18.0101 | 18.2 | Natural | Cyclophilin—peptidyl-prolyl cis–trans isomerase | [47] | |||
| Arachis hypogaea | Peanut | Allergome | Ara h Agglutinin | 29 | IgE & IgE-Immunoblotting | Natural | Agglutinin | [48–51] | ||
| Cajanus cajan | Red gram (Pigeon peas) | Allergome | Caj ca 1 | 45 | IgE-Immunoblotting | Natural | Vicilin-like Protein | [52] | ||
| Cicer arietinum | Chickpea | WHO/IUIS | Cic a 1 | 42 | IgE-Immunoblotting | Natural | Late embryogenesis protein 4 | [53, 54] | ||
| Cicer arietinum | Chickpea | WHO/IUIS | Cic a 1.0101 | 34.6 | IgE-Immunoblotting | Recombinant | Late embryogenesis protein 4 | [53, 54] | ||
| Cicer arietinum | Chickpea | Allergome | Cic a 2S Albumin | 20 | IgE & IgE-Immunoblotting | Natural | 2S Albumin | [55] | ||
| Cicer arietinum | Chickpea | Allergome | Cic a 3 | In silico | nsLTP | [56] | ||||
| Cicer arietinum | Chickpea | Allergome | Cic a 4 | In silico | PR-Protein | [56] | ||||
| Cicer arietinum | Chickpea | Allergome | Cic a 6 | 56 | IgE-Immunoblotting | Natural | Legumin-like Protein | [53] | ||
| Cicer arietinum | Chickpea | Allergome | Cic a 10 | 70 | IgE-Immunoblotting | Natural | Luminal-binding Protein | [53] | ||
| Cicer arietinum | Chickpea | Allergome | Cic a Albumin | 26 | IgE | Natural | Albumin | [57, 58] | ||
| Cyamopsis tetragonoloba | Guar bean (cluster bean) | Allergome | no allergen has been identified yet | [59–61] | ||||||
| Glycine max | Soybean | WHO/IUIS | Gly m 1 | 7 | IgE & IgE-Immunoblotting | Natural | Hydrophobic Seed Protein | [62] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 1.0101 | 8 | IgE-Immunoblotting | Natural | Hydrophobic Seed Protein | [63] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 1.0102 | 8 | IgE-Immunoblotting | Natural | Hydrophobic Seed Protein | [63] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 2 | 8 | IgE & IgE-Immunoblotting | Natural | Defensin | [64–66] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 2.0101 | 8 | IgE | Natural | Defensin | [64] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 3 | 14 | IgE & IgE-Immunoblotting | Natural | Profilin | [67, 68] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 3.0101 | 14.1 | IgE & IgE-Immunoblotting | Recombinant | Profilin | [67] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 3.0102 | 14.1 | IgE & IgE-Immunoblotting | Recombinant | Profilin | [67] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 4 | 17 |
BAT HR |
IgE & IgE-Immunoblotting | Natural | PR-Protein | [69–73] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 4.0101 | 17 |
BAT HR |
IgE & IgE-Immunoblotting | Recombinant | PR-Protein | [69, 73, 74] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 5 | 48 | BAT | IgE & IgE-Immunoblotting | Natural | Vicilin-like Globulin | [73, 75, 76] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 5.0101 | 63.16 | BAT | IgE & IgE-Immunoblotting | Natural | Vicilin-like Globulin | [73, 77–81] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 5.0201 | 65.14 | BAT | IgE & IgE-Immunoblotting | Natural | Vicilin-like Globulin | [73, 77–79] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 5.0301 | 47.9 | BAT | IgE & IgE-Immunoblotting | Natural | Vicilin-like Globulin | [73, 77–79] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 5.0302 | 47.97 | BAT | IgE & IgE-Immunoblotting | Natural | Vicilin-like Globulin | [73, 77–79] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 6 | 55 | BAT | IgE | Natural | Legumin-like Protein | [73, 77, 82] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 6.0101 | 53.62 | IgE & IgE-Immunoblotting | Recombinant | Legumin-like Protein | [83–85] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 6.0201 | 52.44 | IgE & IgE-Immunoblotting | Recombinant | Legumin-like Protein | [86, 87] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 6.0301 | 52.19 | IgE & IgE-Immunoblotting | Recombinant | Legumin-like Protein | [77] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 6.0401 | 61.41 | IgE & IgE-Immunoblotting | Recombinant | Legumin-like Protein | [88] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 6.0501 | 55.65 | IgE & IgE-Immunoblotting | Recombinant | Legumin-like Protein | [77] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 7 | 76.2 | BAT | IgE & IgE-Immunoblotting | Natural | Seed Biotinylated Protein | [89] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 7.0101 | 67.95 | BAT | IgE & IgE-Immunoblotting | Recombinant | Seed Biotinylated Protein | [89] | |
| Glycine max | Soybean | WHO/IUIS | Gly m 8 | 28 | IgE | Natural | 2S Albumin | [90–93] | ||
| Glycine max | Soybean | WHO/IUIS | Gly m 8.0101 | 28 | IgE & IgE-Immunoblotting | Recombinant | 2S Albumin | [90–93] | ||
| Glycine max | Soybean | Allergome | Gly m Agglutinin | 30.9 | IgE & IgE-Immunoblotting | Natural | Agglutinin | [50] | ||
| Glycine max | Soybean | Allergome | Gly m Bd28K | 28 | IgE & IgE-Immunoblotting & Cross-reactive Carbohydrate Determinant |
Natural & Recombinant |
7S Vicilin-like Globulin | [94] | ||
| Glycine max | Soybean | Allergome | Gly m Bd30K | 32–34 | IgE & IgE-Immunoblotting |
Natural & Recombinant |
Protease | [95, 96] | ||
| Glycine max | Soybean | Allergome | Gly m 39kD | 39 | IgE & IgE-Immunoblotting |
Natural & Recombinant |
Unknown | [92, 97] | ||
| Glycine max | Soybean | Allergome | Gly m 50kD | 50 | IgE-Immunoblotting | Natural | Unknown | [98] | ||
| Glycine max | Soybean | Allergome | Gly m CPI | 25 | IgE-Immunoblotting | Natural | Cysteine Protease Inhibitor | [99] | ||
| Glycine max | Soybean | Allergome | Gly m EAP | 60 | IgE-Immunoblotting | Natural | Embryonic Abundant Protein | [99] | ||
| Glycine max | Soybean | Allergome | Gly m TI | 21.5 | PST | IgE & IgE-Immunoblotting | Natural | Trypsin Inhibitor | [48] | |
| Lablab purpureus | Hyacinth bean (Lablab) | Allergome | no allergen has been identified yet | [100] | ||||||
| Lathyrus sativus | grass pea (white pea) | Allergome | no allergen has been identified yet | [101–105] | ||||||
| Lens culinaris | Lentil | WHO/IUIS | Len c 1 | 44–47 |
Natural & Recombinant |
7S Vicilin-like Globulin | [106–108] | |||
| Lens culinaris | Lentil | WHO/IUIS | Len c 1.0101 | 44–47 | Recombinant | 7S Vicilin-like Globulin | [107] | |||
| Lens culinaris | Lentil | WHO/IUIS | Len c 1.0102 | 44–47 | Recombinant | 7S Vicilin-like Globulin | [107, 109] | |||
| Lens culinaris | Lentil | WHO/IUIS | Len c 1.0103 | 7S Vicilin-like Globulin | [107] | |||||
| Lens culinaris | Lentil | WHO/IUIS | Len c 2 | 66 | IgE & IgE-Immunoblotting | Natural | Seed Biotinylated Protein | [106] | ||
| Lens culinaris | Lentil | WHO/IUIS | Len c 2.0101 | Seed Biotinylated Protein | [106] | |||||
| Lens culinaris | Lentil | WHO/IUIS | Len c 3 | 9 | IgE | Natural | nsLTP | [110, 111] | ||
| Lens culinaris | Lentil | WHO/IUIS | Len c 3.0101 | 9,283 | IgE | Recombinant | nsLTP | [111] | ||
| Lens culinaris | Lentil | Allergome | Len c Agglutinin | 30.35 | IgE | Natural | Agglutinin | [50] | ||
| Lupinus albus | White Lupine | Allergome | Lup a 1 | 62 | PST | IgE-Immunoblotting | Natural | 7S Vicilin-like Globulin | [112–114] | |
| Lupinus albus | White Lupine | Allergome | Lup a 4 | In silico | PR-Protein | [115, 116] | ||||
| Lupinus albus | White Lupine | WHO/IUIS | Lup a 5 | 15 | IgE-Immunoblotting | Recombinant | Profilin | [117] | ||
| Lupinus albus | White Lupine | WHO/IUIS | Lup a 5.0101 | 13.9 | IgE-Immunoblotting | Recombinant | Profilin | [117] | ||
| Lupinus albus | White Lupine | Allergome | Lup a alpha_Conglutin | 20 | PST | IgE-Immunoblotting | Natural | Legumin-like Protein | [112, 113, 118] | |
| Lupinus albus | White Lupine | Allergome | Lup a delta_Conglutin | 17 | PST | Natural | 2S Albumin | [112, 119] | ||
| Lupinus albus | White Lupine | Allergome | Lup a gamma_Conglutin | 62.1 | PST | IgE-Immunoblotting | Natural | Aspartic Protease | [112, 113, 120, 121] | |
| Lupinus angustifolius | Blue Lupine | WHO/IUIS | Lup an 1 | 55–61 | IgE & IgE-Immunoblotting | Natural | 7S Vicilin-like Globulin | [122–124] | ||
| Lupinus angustifolius | Blue Lupine | WHO/IUIS | Lup an 1.0101 | 55–61 | IgE | Natural | 7S Vicilin-like Globulin | [125] | ||
| Lupinus angustifolius | Blue Lupine | WHO/IUIS | Lup an 3 | 11 | IgE & IgE-Immunoblotting | Natural | nsLTP | [117] | ||
| Lupinus angustifolius | Blue Lupine | WHO/IUIS | Lup an 3.0101 | 9.23 | IgE & IgE-Immunoblotting | Natural | nsLTP | [117, 126] | ||
| Lupinus angustifolius | Blue Lupine | Allergome | Lup an alpha_Conglutin | 15.53 | IgE & IgE-Immunoblotting | Natural | Legumin-like Protein | [113, 124] | ||
| Lupinus angustifolius | Blue Lupine | Allergome | Lup an delta_Conglutin | 17.78 | IgE & IgE-Immunoblotting | Natural | 2S Albumin | [124, 127] | ||
| Lupinus angustifolius | Blue Lupine | Allergome | Lup an gamma_Conglutin | 48.91 | IgE & IgE-Immunoblotting | Natural | Aspartic Protease | [113, 124, 127, 128] | ||
| Lupinus luteus | Yellow Lupine (European Lupine) | Allergome | Lup l 4 | 16.859 | IgE | Recombinant | PR-Protein | [129, 130] | ||
| Macrotyloma uniflorum | Horse gram (kulthi bean) | Allergome | Dol b Agglutinin | 26 | PST | HR | IgE & IgE-Immunoblotting | Natural | Agglutinin | [131] |
| Pachyrhizus erosus | Yam-bean | Allergome | no allergen has been identified yet | [132, 133] | ||||||
| Phaseolus coccineus | Runner Bean | Allergome | no allergen has been identified yet | [134] | ||||||
| Phaseolus lunatus | Lima bean | Allergome | no allergen has been identified yet | [135, 136] | ||||||
| Phaseolus vulgaris | Kidney Bean (String Bean) | WHO/IUIS | Pha v 3 | 9 | HR | IgE & IgE-Immunoblotting |
Natural & Recombinant |
nsLTP | [137–139] | |
| Phaseolus vulgaris | Kidney Bean (String Bean) | WHO/IUIS | Pha v 3.0101 | 9.375 | HR | IgE-Immunoblotting | Recombinant | nsLTP | [137–139] | |
| Phaseolus vulgaris | Kidney Bean (String Bean) | WHO/IUIS | Pha v 3.0201 | 9.221 | HR | IgE-Immunoblotting | Recombinant | nsLTP | [137–139] | |
| Phaseolus vulgaris | Kidney Bean (String Bean) | Allergome | Pha v 5 | In silico | Profilin | [140] | ||||
| Phaseolus vulgaris | Kidney Bean (String Bean) | Allergome | Pha v 6 | In silico | PR-Protein | |||||
| Phaseolus vulgaris | Kidney Bean (String Bean) | Allergome | Pha v aAI | Recombinant | alpha-Amylase Inhibitor | [141] | ||||
| Phaseolus vulgaris | Kidney Bean (String Bean) | Allergome | Pha v aAI.0101 | 27.2 | Recombinant | alpha-Amylase Inhibitor | [141] | |||
| Phaseolus vulgaris | Kidney Bean (String Bean) | Allergome | Pha v Chitinase | 32 | IgE-Immunoblotting | Natural | Chitinase | [142] | ||
| Phaseolus vulgaris | Kidney Bean (String Bean) | Allergome | Pha v PHA | 29.55 | PST | BHRA | IgE & IgE-Immunoblotting | Natural | Agglutinin | [143, 144] |
| Phaseolus vulgaris | Kidney Bean (String Bean) | Allergome | Pha v Phaseolin | 47.5 | PST | IgE-Immunoblotting | Natural | Vicilin-like Protein | [145, 146] | |
| Pisum sativum | Pea | WHO/IUIS | Pis s 1 | 44–47 | IgE & IgE-Immunoblotting |
Natural & Recombinant |
Vicilin-like Protein | [108, 147] | ||
| Pisum sativum | Pea | WHO/IUIS | Pis s 1.0101 | 44 | IgE & IgE-Immunoblotting | Recombinant | Vicilin-like Protein | [108] | ||
| Pisum sativum | Pea | WHO/IUIS | Pis s 1.0102 | 44 | IgE & IgE-Immunoblotting | Recombinant | Vicilin-like Protein | [108] | ||
| Pisum sativum | Pea | WHO/IUIS | Pis s 2 | 63 | IgE-Immunoblotting | Natural | 7S Vicilin-like Globulin | [108, 148] | ||
| Pisum sativum | Pea | WHO/IUIS | Pis s 2.0101 | 67 | IgE | Recombinant | 7S Vicilin-like Globulin | [108] | ||
| Pisum sativum | Pea | WHO/IUIS | Pis s 3 | 9.5 | IgE | Natural | nsLTP | [149] | ||
| Pisum sativum | Pea | WHO/IUIS | Pis s 3.0101 | 9.5 | IgE | Recombinant | nsLTP | [149] | ||
| Pisum sativum | Pea | Allergome | Pis s 5 | Natural | Profilin | [29, 150] | ||||
| Pisum sativum | Pea | Allergome | Pis s 6 | In silico | PR-Protein | [151] | ||||
| Pisum sativum | Pea | Allergome | Pis s Agglutinin | 30.27 | IgE | Natural | Agglutinin | [50] | ||
| Pisum sativum | Pea | Allergome | Pis s Albumin | 26.23 | IgE | Natural | Albumin | [57, 148] | ||
| Trigonella foenum-graecum | Fenugreek | Allergome | Tri fg 1 | 50 | IgE-Immunoblotting | Natural | 7S Vicilin-like Globulin | [152] | ||
| Trigonella foenum-graecum | Fenugreek | Allergome | Tri fg 2 | 98 | IgE-Immunoblotting | Natural | 2S Albumin | [152] | ||
| Trigonella foenum-graecum | Fenugreek | Allergome | Tri fg 3 | 98 | IgE-Immunoblotting | Natural | Legumin-like Protein | [152] | ||
| Trigonella foenum-graecum | Fenugreek | Allergome | Tri fg 4 | 21 | IgE-Immunoblotting | Natural | PR-Protein | [152] | ||
| Vicia faba | Broad Bean | Allergome | Vic f 6 | In silico | PR-Protein | |||||
| Vigna angularis | Red Mung bean (Azuki Bean) | Allergome | Vig an 6 | In silico | PR-Protein | |||||
| Vigna mungo | Black gram | Allergome | Vig mu 28kD | 28 | PST | LPA & BHRA | IgE & IgE-Immunoblotting | Natural | Unknown | [153] |
| Vigna radiata |
Green gram (Mung bean) |
WHO/IUIS | Vig r 1 | 16 | BAT | IgE-Immunoblotting |
Natural & Recombinant |
PR-Protein | [74, 154, 155] | |
| Vigna radiata |
Green gram (Mung bean) |
WHO/IUIS | Vig r 1.0101 | 16.2 | BAT | IgE |
Natural & Recombinant |
PR-Protein | [74, 154, 155] | |
| Vigna radiata |
Green gram (Mung bean) |
WHO/IUIS | Vig r 2 | 52 | IgE-Immunoblotting | Natural | 8S Globulin | [156] | ||
| Vigna radiata | Green gram (Mung bean) | WHO/IUIS | Vig r 2.0101 | 49.3 | IgE-Immunoblotting | Recombinant | 8S Globulin | [156, 157] | ||
| Vigna radiata | Green gram (Mung bean) | WHO/IUIS | Vig r 2.0201 | 49.4 | IgE-Immunoblotting | Natural | 8S Globulin | [156, 158] | ||
| Vigna radiata | Green gram (Mung bean) | WHO/IUIS | Vig r 4 | 30 | IgE-Immunoblotting | Natural | Seed albumin | [74, 156] | ||
| Vigna radiata | Green gram (Mung bean) | WHO/IUIS | Vig r 4.0101 | 30.2 | IgE-Immunoblotting | Natural | Seed albumin | [74, 156] | ||
| Vigna radiata | Green gram (Mung bean) | Allergome | Vig r 5 | 15 | IgE-Immunoblotting | Natural | profilin-homolog | |||
| Vigna radiata | Green gram (Mung bean) | WHO/IUIS | Vig r 6 | 18 | BAT | IgE | Recombinant | PR-Protein | [74, 129] | |
| Vigna radiata | Green gram (Mung bean) | WHO/IUIS | Vig r 6.0101 | 17.49 | BAT | IgE | Recombinant | PR-Protein | [74, 129, 159] | |
| Vigna radiata | Green gram (Mung bean) | Allergome | Vig r beta-Conglycinin | 18 | IgE-Immunoblotting | Natural | Vicilin-like Protein | [156] | ||
| Vigna unguiculata | Cowpea | Allergome | Vig u 6 | In silico | PR-Protein | [160] |
The table is arranged in alphabetical order of the Latin names of the allergen source species. Basophil activation test (BAT); mast cell activation test (MAT); stripped basophil histamine release assay (BHRA); histamine release assay (HR); lymphoproliferation assay (LPA); non-specific lipid transfer proteins (nsLTP). Allergens sourced from Allergome are not recognized as official. Only those listed in the WHO/IUIS Allergen Nomenclature Sub-Committee database hold official status.
Table 2.
Classification of single legume allergen and allergen homologs by protein families
| Source/Function |
7S globulins (vicilins) |
11S globulins (legumins) | 2S albumins | Profilins | PR proteins | Biotinylated Proteins | nsLTP | Agglutinins | Defensins | Oleosins | Diverse |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Peanut | Ara h 1 | Ara h 3 |
Ara h 2 Ara h 6 Ara h 7 |
Ara h 5 | Ara h 8 |
Ara h 9 Ara h 16 Ara h 17 |
Ara h Agglutinin |
Ara h 12 Ara h 13 |
Ara h 10 Ara h 11 Ara h 14 Ara h 15 |
Ara h 18 | |
| Soybean |
Gly m 5 Gly m Bd28K |
Gly m 6 | Gly m 8 | Gly m 3 | Gly m 4 | Gly m 7 | Gly m Agglutinin | Gly m 2 |
Gly m 1 Gly m TI Gly m Bd30K Gly m 39kD Gly m 50kD Gly m CPI Gly m EAP |
||
| White Lupine | Lup a 1 | Lup a alpha-Conglutin | Lup a delta-Conglutin | Lup a 5 | Lup a 4 | ||||||
| Blue Lupine | Lup an 1 | Lup an alpha-Conglutin | Lup an delta-Conglutin | Lup an 3 | |||||||
| Yellow Lupine | Lup l 4 | ||||||||||
| Pea |
Pis s 1 Pis s 2 |
Pis s 5 | Pis s 6 | Pis s 3 | Pis s Agglutinin | Pis s Albumin | |||||
| Lentil | Len c 1 | Len c 2 | Len c 3 | Len c Agglutinin | |||||||
| Chickpea | Cic a 6 | Cic a 2S Albumin | Cic a 4 | Cic a 3 |
Cic a 1 Cic a 10 |
||||||
| Fenugreek | Tri fg 1 | Tri fg 3 | Tri fg 2 | Tri fg 4 | |||||||
| Kidney Bean | Pha v 5 | Pha v 6 | Pha v 3 | Pha v PHA |
Pha v aAI Pha v chitinase |
||||||
| Mung Bean | Vig r beta-Conglycinin | Vig r 5 |
Vig r 1 Vig r 6 |
||||||||
| Broad Bean | Vic f 6 | ||||||||||
| Azuki Bean | Vig an 6 | ||||||||||
| Cowpea | Vig u 6 | ||||||||||
| Pigeon Pea | Caj ca 1 | ||||||||||
| Horse Gram | Dol b Agglutinin |
Non-specific lipid transfer proteins (nsLTP). Allergens sourced from Allergome are not recognized as official. Only those listed in the WHO/IUIS Allergen Nomenclature Sub-Committee database hold official status.
Priority Legumes
Among the priority legumes, peanuts and soybeans are the most common triggers of anaphylaxis in countries such as Germany, Austria, and Switzerland [161]. Interestingly, these oilseeds [162] can provoke intense allergic reactions, while non-oilseed legumes may cause less obvious responses (hidden allergic reactions). Oil bodies (oleosomes) as part of the lipid content of the seed are stabilized by different proteins (oleosins, steroleosins, caleosins) [40, 163, 164]. Moreover, Schwager et al. showed by basophil activation test (BAT) measurements that oleosins can be used as marker allergens to reliably distinguish peanut allergic patients with severe allergic reactions from simply sensitized individuals [41]. Extracts for diagnostic and therapeutic purposes are aqueous extracts and therefore lack lipophilic compounds such as oleosins. Hidden allergic reactions highlight the importance of identifying allergens in each type of legume to avoid risks when using these plants in the manufactured products consumed worldwide [7, 165] and to improve the quality of diagnostic and therapeutic applications. Peanut (Arachis hypogaea) seeds are the most prevalent among all legumes [166].
Peanut allergy symptoms can vary from mild to severe to even life-threatening anaphylactic reactions [167, 168]. Identifying peanut allergens was done extensively in the last decade [40, 41, 43, 47]. Many isoforms from peanuts were characterized over the years (Table 1). People with peanut allergy might also have allergic reactions to other legumes (cross-reactivity): A cohort study with 195 peanut-allergic children showed positive IgE reactivities towards lupine, fenugreek, soy and lentils [169]. However, the clinical relevance of cross-reactivities to soy are questionable [170, 171]. Soybean (Glycine max) is also listed in the “Big 9”, however, the recent ad hoc Joint FAO/WHO expert consultation on risk assessment of food allergens [172] recommended to remove soybean from this list as the overall prevalence is rather low and soybean allergy is only predominant in certain geographic areas (2% in Japan [173], 0.6% in the US [174, 175] and 0.5% in Europe [176]) according to self-reported surveys. Eight official soybean allergens are listed in the WHO/IUIS Allergen Nomenclature Sub-Committee database. Eight additional IgE-binding proteins from soybean are also listed in the Allergome database (Table 1). Anaphylactic reactions towards soy are severe for around one third of the cases and are more frequent in adults when compared to children [161]. They are mostly associated with Gly m 3 to 6 [77, 177, 178], and some case studies even suggest exercise as a co-factor of anaphylaxis to soybean allergens (food-dependent exercise-induced anaphylaxis (FDEIA)) [179, 180]. Although sensitization towards profilin (Gly m 3) and PR10 protein (Gly m 4) was the most frequent cause for systemic reactions in a large retrospective study [178], Gly m 4 seems to be the predominating trigger [70, 181]. While it is well-known that the storage proteins Gly m 5 to 8 are resistant to heat and/or digestion [89, 93, 182–184], Gly m 4 was only recently shown to refold after heating and trigger an IgE response, with or without homologous Bet v 1-related epitopes [185]. Furthermore, this allergen can cross the intestinal barrier, especially if the gastric pH is too high for proper digestion [185]. This might explain why soybean-based drinks can be dangerous for people with birch or alder pollen allergy [73].
Non-Priority Legumes
Beans
Allergy towards beans is rare and is frequently accompanied by IgE cross-reactivity to other legumes, though exceptions occur as described below. Although beans have fewer known allergens, cross-reactivities with soybeans and peanuts have been reported [165]. The route of sensitization includes the oral mucosa and the respiratory tract as well as the skin (contact urticaria), although only one case has been reported for the latter: An 84-year-old man experienced skin swelling after skin contact with runner bean plants (Phaseolus coccineus) in his garden [160]. Bean allergy highly depends on the genus and species of the bean. For instance, allergic reactions to the white bean (Phaseolus vulgaris) were highlighted by recent case reports. Matsui et al. reported an allergic reaction to white beans in a child [186]. IgE-reactivity determined by ImmunoCAP occurred to bean allergens such as phytohemagglutinin, Group 3 LEA, lipoxygenase, and legumin. Another report published in 2023 described two children exhibiting allergic reactions to both white and red beans, yet showed no reactions to other legumes. Western blot analysis using sera of two patients that reacted to extracts from white and red beans identified two IgE-binding proteins in the extracts with molecular weights in the ranges of 47–50 kDa and 28–31 kDa [187]. The mung bean (Vigna radiata) is used in meat-substitution products, which are consumed worldwide. Two cases of OAS have been described, one in a teenage Japanese girl, and another involving a male in his twenties [188]. Both cases tested positive for IgE specific to soybean Gly m 4 and birch Bet v 1 [154] (Table 1). Lima beans (Phaseolus lunatus) induce positive skin test reactions in patients with other legume allergies but with a low percentage (3.4%) as shown by a survey for asthma and rhinitis patients in Delhi [135], which mostly correlates to cross-reactivity with other legumes [189, 190]. No allergen has been identified from broad bean (Vicia faba), despite an instance where a 5-year-old boy (no allergy history) experienced an anaphylaxis after eating a legume-based snack containing fried broad beans. The immunoblotting results with 3 different extracts of broad bean (raw, cooked, and fried) were IgE-positive for the fried bean only, detecting allergens at 37, 21, 17, and 15 kDa [191]. Although considered as a food allergen, a rare case related to occupational asthma from inhaling lima bean vapors was reported in 2012, whereby a new worker in a food factory (a 41-year-old male) developed asthma-like symptoms after 4 months of working on boiling, mincing, and drying large amounts of lima beans [192]. A study conducted in India, which included 815 patients suffering from asthma and allergic rhinitis, revealed that 4% of them were hypersensitive to black gram (Vigna mungo) [193]. Subsequently, the single IgE-binding protein Vig mu 28 kD from black gram was characterized [153].
Peas
The high protein content in peas (Pisum sativum) makes them an important nutritional source. Their ability to absorb water has led to their widespread use in the production of meat-substitution products. Case reports for pea allergy have been more frequent as of late including descriptions of severe reactions, which indicate that a switch to a plant-based diet can harbor risks for certain individuals. For example, Abi-Melhem et al. [194] described six cases of pea allergy, five of which were children less than 10 years old and a 15-year-old boy with a history of cashew allergy but tolerance to peanut. The latter immediately developed hives on his face and neck in three incidences after consumption of processed food that contained green peas, such as substitute milk, substitute chicken nuggets and pea-based protein powder. The severe response was accompanied by an elevated IgE level to pea extract. Another report described a 28-year-old woman with asthma who had a severe reaction to falafel containing peas [195]. She had a similar reaction to peas when she was 10 years old and has since been cautiously avoiding peas and peanuts. Her skin prick test (SPT) was positive, and specific IgE to pea was slightly increased. However, other legumes, nuts and sesame showed negative in the SPT. These cases raised a question whether peas are safe for people with sensitization to homologous allergens. Cohort data from Italy demonstrated that pea LTP (Pis s 3) is safe to consume for LTP-allergic patients [196], whilst a German cohort study discovered the seed storage protein Pis s 1 as major immunodominant allergen [197].
Lentils
Lentils (Lens culinaris) are a rich source of protein with antioxidant and anti-inflammatory benefits [198, 199]. The lentils’ unique flavor has led to their widespread use in vegan products [8, 200]. Routes of entry include digesting, inhaling and skin contact. Several unique case studies highlighted the potential allergenic risk of lentils. For example, a 9-year-old boy developed anaphylaxis after consuming lentil soup. Following this incident, the boy removed lentils from his diet. However, during a separate incident involving direct skin contact with lentil soup, he experienced itching, redness, and swelling of the skin [201]. Another example involves a 22-months-old girl who developed an allergic reaction shortly after inhaling the vapors from cooking lentils. A positive specific IgE signal for lentils confirmed the lentil sensitization [202]. Further cases include an 8½-year-old boy who experienced swelling of his eyelids, cough and wheezing after exposure to steam from boiling lentils. Similar reactions were reported after eating lentil soup, chickpeas and peas. His blood tests showed eosinophilia and high total IgE levels, and his diagnosis was confirmed via SPT [203]. A 12-year-old girl without any pollen allergy observed an OAS after lentil and cashew consumption. She developed a reaction after having consumed lentil soup in the Kindergarden. A subsequent investigation revealed that the lentil soup contained peanuts (50 g/L) (Jappe, personal communication). Suspecting an underlying reaction to peanuts as the causative agent, the patient underwent diagnostics confirming an IgE reaction to both, peanut (87.10 kU/L) and lentil (6.08 kU/L) extracts. Specific IgE was positive to Ara h 1 (77.6 kU/L), Ara h 2 (14.8 kU/L), and Ara h 3 (1.7 kU/L), but not towards Ara h 8 and Ara h 9. Oral provocation with 4 spoons of lentil soup without peanuts induced OAS, whereas oral provocation with peanuts led to bronchoconstriction, flush and laryngeal edema at a cumulative dose of ca. 14 mg of peanuts (Jappe, personal communication). More recently, a rare case of FDEIA after eating lentils was published by Alnabulsi et al., where a 16-year-old girl experienced respiratory distress with urticaria-like symptoms upon exercising within an hour after eating lentils. These symptoms recurred again under similar circumstances. Interestingly, her IgE levels for lentils were low [204]. A similar reaction was observed for a 17-year-old boy with four different encounters after eating lentils and exercising [205]. These cases highlight the need for more specific tests and a detailed clinical history regarding activities after consumption (e.g. exercising) when investigating lentil allergy due to the observed cross-reactivities with peanuts, peas, and chickpeas [169, 206, 207].
Chickpea
Chickpeas (Cicer arietinum) are among the most frequently eaten legumes and are used in a variety of popular vegan recipes such as falafel and hummus. Despite the low incidence of chickpea allergy, some old reports back to 2008 have documented cases of FDEIA related to eating chickpea. For example, both, a 16-year-old boy [205] and a 17-year-old girl [208] experienced anaphylaxis after eating chickpeas and performing subsequent exercise. Both showed SPT positive results for chickpea, whilst IgE was only determined for the latter, indicating high IgE titers for chickpea and soybean [208]. These cases point out the potential allergenic risk of chickpeas and the need for further research.
Lupine
Lupinus species are comparable to soy with regard to their nutritional value, which is why they are being used not only as ingredient to foods but as food themselves [209–211]. Lupine seeds or the respective flour are used as nutritional substitute for people with allergies or intolerances to wheat, milk, eggs, and gluten [212]. Lupine allergy has first been described in the USA [212], then in Germany [213] and recently in a Canadian child with peanut allergy [214]. Despite lupine being listed on EU food ingredients since 2006 (Directive 2000/13/EC), individuals unaware of their allergy to lupine via cross-reactivity to peanuts, for example, may still be unknowingly exposed. Due to this individually unclear situation, lupine allergens are still considered as “hidden allergens” [7, 215, 216]. Mainly three lupine species are used for human nutrition: L. angustifolius, L. albus, and L. luteus. A fourth species is used in South America (L. mutabilis) [215]. Allergy to lupine occurs as mono-allergy or as a result of cross-reactivity between the allergenic proteins of different legumes, of which peanut is the most relevant culprit [215]. The most common patterns of clinical cross-reactivity among legumes are between peanut, lupine, soy, chickpea and lentil, although this is highly dependent on geography and prevalence of these foods in the diet [217]. Despite the lupine’s potential as an anaphylactic allergen source, only three allergens have been accepted by the WHO/IUIS Allergen Nomenclature Sub-Committee due to variations in protein content, allergen composition and structure across different lupine species [117]: Lup an 1 (a β-conglutin of L. angustifolius), Lup an 3, a non-specific LTP of L. angustifolius, and Lup a 5, the profilin of L. albus. Sequences of the same protein in different species and cultivars can differ, for example the β-conglutin in blue lupine is 60–70% identical to β-conglutin of white lupine [114]. Lupine sensitization rates reported in Europe range between 0.27% and 4.1%, but these may not reflect the true prevalence of lupine allergy, which remains unknown in the general population. In a study involving 14 food allergy sources, allergic reactions were observed in 5% of the population, including 25 individuals with lupine allergy. These reactions were triggered by both discrete and cumulative doses. However, it is important to note the significant variation in the doses that caused these reactions, as indicated by the wide ranges of the confidence intervals [218]. Due to the significant variability among patients, efforts to identify the threshold doses of lupine that trigger allergic reactions have been unsuccessful [215]. SPT can be performed with the flour of all three species whereas only the L. albus extract is available for in vitro testing. The value of new single lupine allergens, however, has been confirmed in an optimized BAT [219] using whole blood from a patient with LTP-syndrome [220], indicating the necessity of introducing more single allergens for reliable antibody- and cell-based allergy diagnostic tests in the future.
The “Beyond” (Cowpea, Pigeon Pea and Fenugreek)
In contrast to the legumes mentioned above, reports for cowpea, pigeon pea, and fenugreek are few, but at least some single allergens were identified in contrast to no identified allergens from Lima bean, Hyacinth bean, white pea, Guar bean, Yam-bean or Runner Bean (Table 1).
The cowpea (Vigna unguiculata) is an annual herbaceous plant known for its drought resilience. A study conducted in Luxemburg showed that a majority of legume allergy patients was sensitized to cowpea proteins [160]. It described four allergens with potential cross-reactivity to other legumes by in silico analysis. A previous study identified a potential allergen from the 2S albumin family in cowpea (25 kDa) using crystallographic characterization [221]. As the 2S albumin family is known for its resistance to digestion and its interaction with membranes—both crucial factors for food allergenicity—a further investigation into cowpea 2S albumins may be recommended.
The pigeon pea (Cajanus cajan) is a perennial legume. Despite its low intake in Europe, there has been a recent increase in its popularity due to its low cost and the growing vegan trend. The allergenicity of pigeon pea has not been extensively studied compared to peanuts and soybeans, although potential allergens from pigeon pea have already been identified by in silico analysis in 2010 without any follow-up studies [52].
Fenugreek (Trigonella foenum-graecum) is a legume commonly used in spice mixes as its flavor is similar to maple as well as in traditional medicine. While it was generally deemed safe for consumption, the probably first case of fenugreek allergy was reported in 1993 with occupational asthma due to inhalation of fenugreek seed powder [222] followed by reports on asthma and anaphylaxis after inhalation and skin contact [223]. In addition, oral provocation of these patients revealed its potency as food allergen source which was later confirmed [224, 225]. Two publications describe anaphylaxis to fenugreek in curry spice [226]. Four potential fenugreek allergens have been described since 2009 without further characterization [152, 227]. There is a potential cross-reactivity between fenugreek and other legumes. In 2009, Faeste and co-authors published a systematic study on a total of 31 patients, 29 with IgE to peanut, on allergenicity and possible cross-reactivity between fenugreek and other legumes. They documented an elicitation dose for fenugreek of 2 mg for the occurrence of objective allergic symptoms. They interpreted the sensitization to fenugreek as a result of peanut sensitization. Only one case of primary sensitization to fenugreek was found to date [227]. A recent study on the extent of cross-reactivity among legumes in 195 peanut-allergic children showed a sensitization to lupine, fenugreek, soy and lentils in descending order of frequency [169]. For routine diagnostics, only total fenugreek extract can currently be used in ImmunoCAP. There are no approved solutions for skin tests, i.e. only the prick-to-prick test with sponged fenugreek seed is available for detecting sensitization.
Legume Allergy Diagnosis
Many diagnostic methods are used when investigating legume allergies, like in vivo tests (SPT, oral food challenge), functional tests in vitro and ex vivo (BAT, mast cell activation test (MAT), stripped basophil histamine release assay (BHRA), histamine release assay (HR) and lymphoproliferation assay (LPA)), in vitro non-functional tests (specific IgE, total IgE, IgE-immunoblotting, cross-reactive carbohydrate determinant (CCD)-IgE) and in silico (BLAST). Despite the increasing accuracy of both BAT and MAT most legume allergy studies have used in vitro IgE-binding assays while investigating allergens. This is due to the low number of allergic individuals. However, the recent increase of incidences might help identifying the allergenic potency of each consumed legume. It is important to provide more studies that investigate legume allergens’ stability. It is known that the sensitizing capacity and elicitation of an allergic immune response are what distinguishes allergens from non-allergenic proteins [228, 229]. However, allergens must have unique molecular properties that allow them to pass through barriers such as mucosa and skin [6]. Naturally, food processing can change the molecular structure of proteins and influence the biological activities of the respective protein [230, 231], and sometimes modify immunogenic reactivity [232]. This might increase or decrease the allergenic potential of allergens, depending on the applied process, protein structure [233–235] and whether the patient reacts towards linear and/or conformational epitopes. Physical, chemical and enzymatic processing methods have different effects on the allergenic potency of legumes [236]. However, the route of exposure via inhalation, skin (touch) or gastrointestinal tract by consumption of food, can also influence the allergenic potency. Therefore, it is important to combine knowledge about protein stability to food processing and exposure routes to be able to provide the appropriate testing method for each legume.
Introducing new products containing legume ingredients may pose risks for sensitized individuals. Furthermore, the processing methods used to produce the final product can influence the allergenicity of foods. Identifying the possible allergens in each consumed legume, and understanding their stability and the modifications they undergo (e.g. Maillard reaction) throughout the production process until the final product is obtained, will provide us with the necessary information to adjust the processing steps to an optimal level that results in a lower allergenicity of the product. This necessitates more rigorous research as the trend of vegan food is still on the rise.
Conclusions
In addition to priority legumes (peanut, soybean), non-priority legumes (lupines, chickpea, lentils, beans) are also associated with anaphylaxis, often enough in patients allergic to priority legumes. A number of single allergens has been identified and more or less characterized from different legume families and even different legume species such as Lupinus. However, this knowledge on both extracts and single allergens has not been used to adapt commercially available diagnostic tests. This might become a problem in the near future as more and more individuals take to vegetarian and vegan dietary practices, therefore becoming more and more exposed to these potentially anaphylactic allergen sources. Not only are sensitization tests depending on more single allergens for improved accuracy in the detection of individual sensitization profiles, they are also important for elucidating potential cross-reactivities. In addition, as already shown for peanut and alpha-Gal, the application of single marker allergens in cell-based assays like BAT may even allow discrimination between sensitization and true allergy, providing allergologists with adequate information for individual doctoral advice for individual allergy prevention (precision medicine).
Author Contributions
Literature research, MAR, EMR, MP and UJ; Tables and figure, MAR; Writing – Review & Editing, MAR, EMR, MP and UJ.
Funding
Open Access funding enabled and organized by Projekt DEAL. MAR is funded by the Federal Ministry of Education and Science (BMBF), German Center for Lung Research (DZL 001C1). EMR is funded by the Federal Ministry of Education and Science (BMBF) with INDICATE-FH project. UJ has projects funded by German Research Foundation (DFG) no. JA 1007/2–1 and no. JA 1007/2–3, BMBF (DZL and INDICATE-FH (01EA2109B)).
Compliance with Ethical Standards
Conflict of Interest
The authors declare no conflict of interest. The graphical abstract in Fig. 1 was created with biorender.com.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alcorta A, et al. Foods for Plant-Based Diets: Challenges and Innovations. Foods. 2021;10(2). [DOI] [PMC free article] [PubMed]
- 2.Iqbal A, et al. Nutritional quality of important food legumes. Food Chem. 2006;97(2):331–5. 10.1016/j.foodchem.2005.05.011 [DOI] [Google Scholar]
- 3.Birt DF, et al. Resistant starch: promise for improving human health. Adv Nutr. 2013;4(6):587–601. 10.3945/an.113.004325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trompette A, et al. Gut-derived short-chain fatty acids modulate skin barrier integrity by promoting keratinocyte metabolism and differentiation. Mucosal Immunol. 2022;15(5):908–26. 10.1038/s41385-022-00524-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verma AK, et al. A comprehensive review of legume allergy. Clin Rev Allergy Immunol. 2013;45(1):30–46. 10.1007/s12016-012-8310-6 [DOI] [PubMed] [Google Scholar]
- 6.Pekar J, Ret D, Untersmayr E. Stability of allergens. Mol Immunol. 2018;100:14–20. 10.1016/j.molimm.2018.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skypala IJ. Food-Induced Anaphylaxis: Role of Hidden Allergens and Cofactors. Front Immunol. 2019;10:673. 10.3389/fimmu.2019.00673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Präger L, Simon JC, Treudler R. Food allergy - New risks through vegan diet? Overview of new allergen sources and current data on the potential risk of anaphylaxis. J Dtsch Dermatol Ges. 2023;21(11):1308–13. [DOI] [PubMed] [Google Scholar]
- 9.San Ireneo MM, et al. Clinical features of legume allergy in children from a Mediterranean area. Ann Allergy Asthma Immunol. 2008;101(2):179–84. 10.1016/S1081-1206(10)60207-4 [DOI] [PubMed] [Google Scholar]
- 10.Patil SP, Niphadkar PV, Bapat MM. Chickpea: a major food allergen in the Indian subcontinent and its clinical and immunochemical correlation. Ann Allergy Asthma Immunol. 2001;87(2):140–5. 10.1016/S1081-1206(10)62209-0 [DOI] [PubMed] [Google Scholar]
- 11.Burks AW, et al. Recombinant peanut allergen Ara h I expression and IgE binding in patients with peanut hypersensitivity. J Clin Invest. 1995;96(4):1715–21. 10.1172/JCI118216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waritani T, et al. Development and evaluation of mouse anti-Ara h 1 and Ara h 3 IgE monoclonal antibodies for advancing peanut allergy research. MethodsX. 2023;11:102470. 10.1016/j.mex.2023.102470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koppelman SJ, et al. Relevance of Ara h1, Ara h2 and Ara h3 in peanut-allergic patients, as determined by immunoglobulin E Western blotting, basophil-histamine release and intracutaneous testing: Ara h2 is the most important peanut allergen. Clin Exp Allergy. 2004;34(4):583–90. 10.1111/j.1365-2222.2004.1923.x [DOI] [PubMed] [Google Scholar]
- 14.van der Veen MJ, et al. Poor biologic activity of cross-reactive IgE directed to carbohydrate determinants of glycoproteins. J Allergy Clin Immunol. 1997;100(3):327–34. 10.1016/S0091-6749(97)70245-8 [DOI] [PubMed] [Google Scholar]
- 15.Knoll JE, et al. TILLING for allergen reduction and improvement of quality traits in peanut (Arachis hypogaea L.). BMC Plant Biol. 2011;11:81. [DOI] [PMC free article] [PubMed]
- 16.Wichers HJ, et al. The major peanut allergen Ara h 1 and its cleaved-off N-terminal peptide; possible implications for peanut allergen detection. J Agric Food Chem. 2004;52(15):4903–7. 10.1021/jf049697o [DOI] [PubMed] [Google Scholar]
- 17.Burks AW, et al. Isolation, identification, and characterization of clones encoding antigens responsible for peanut hypersensitivity. Int Arch Allergy Immunol. 1995;107(1–3):248–50. 10.1159/000236993 [DOI] [PubMed] [Google Scholar]
- 18.Kleber-Janke T, et al. Selective cloning of peanut allergens, including profilin and 2S albumins, by phage display technology. Int Arch Allergy Immunol. 1999;119(4):265–74. 10.1159/000024203 [DOI] [PubMed] [Google Scholar]
- 19.Chatel JM, Bernard H, Orson FM. Isolation and characterization of two complete Ara h 2 isoforms cDNA. Int Arch Allergy Immunol. 2003;131(1):14–8. 10.1159/000070429 [DOI] [PubMed] [Google Scholar]
- 20.Conway AE, et al. Serologic measurements for peanut allergy: Predicting clinical severity is complex. Ann Allergy Asthma Immunol. 2024. [DOI] [PubMed]
- 21.Ji C, et al. Ara h 2-Specific IgE Presence Rather Than Its Function Is the Best Predictor of Mast Cell Activation in Children. J Allergy Clin Immunol Pract. 2023;11(4):1154-1161.e3. 10.1016/j.jaip.2022.12.026 [DOI] [PubMed] [Google Scholar]
- 22.Vissers YM, et al. Effect of heating and glycation on the allergenicity of 2S albumins (Ara h 2/6) from peanut. PLoS ONE. 2011;6(8):e23998. 10.1371/journal.pone.0023998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hales BJ, et al. Isoforms of the major peanut allergen Ara h 2: IgE binding in children with peanut allergy. Int Arch Allergy Immunol. 2004;135(2):101–7. 10.1159/000080652 [DOI] [PubMed] [Google Scholar]
- 24.Stanley JS, et al. Identification and mutational analysis of the immunodominant IgE binding epitopes of the major peanut allergen Ara h 2. Arch Biochem Biophys. 1997;342(2):244–53. 10.1006/abbi.1997.9998 [DOI] [PubMed] [Google Scholar]
- 25.Rabjohn P, et al. Molecular cloning and epitope analysis of the peanut allergen Ara h 3. J Clin Invest. 1999;103(4):535–42. 10.1172/JCI5349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Szabó I, Eigenmann PA. Allergenicity of major cow’s milk and peanut proteins determined by IgE and IgG immunoblotting. Allergy. 2000;55(1):42–9. 10.1034/j.1398-9995.2000.00256.x [DOI] [PubMed] [Google Scholar]
- 27.Mayorga C, et al. Basophil response to peanut allergens in Mediterranean peanut-allergic patients. Allergy. 2014;69(7):964–8. 10.1111/all.12421 [DOI] [PubMed] [Google Scholar]
- 28.Amoah AS, et al. Peanut-specific IgE antibodies in asymptomatic Ghanaian children possibly caused by carbohydrate determinant cross-reactivity. J Allergy Clin Immunol. 2013;132(3):639–47. 10.1016/j.jaci.2013.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Ree R, et al. Profilin is a cross-reactive allergen in pollen and vegetable foods. Int Arch Allergy Immunol. 1992;98(2):97–104. 10.1159/000236171 [DOI] [PubMed] [Google Scholar]
- 30.Kleber-Janke T, et al. Patient-tailored cloning of allergens by phage display: peanut (Arachis hypogaea) profilin, a food allergen derived from a rare mRNA. J Chromatogr B Biomed Sci Appl. 2001;756(1–2):295–305. 10.1016/S0378-4347(01)00088-3 [DOI] [PubMed] [Google Scholar]
- 31.Cabanos C, et al. Expression, purification, cross-reactivity and homology modeling of peanut profilin. Protein Expr Purif. 2010;73(1):36–45. 10.1016/j.pep.2010.03.005 [DOI] [PubMed] [Google Scholar]
- 32.Schmidt H, et al. Detection and structural characterization of natural Ara h 7, the third peanut allergen of the 2S albumin family. J Proteome Res. 2010;9(7):3701–9. 10.1021/pr1002406 [DOI] [PubMed] [Google Scholar]
- 33.Hayen SM, et al. 2S protein Ara h 7.0201 has unique epitopes compared to other Ara h 7 isoforms and is comparable to 2S proteins Ara h 2 and 6 in basophil degranulation capacity. Clin Exp Allergy. 2018;48(7):890–7. 10.1111/cea.13134 [DOI] [PubMed] [Google Scholar]
- 34.Mittag D, et al. Ara h 8, a Bet v 1-homologous allergen from peanut, is a major allergen in patients with combined birch pollen and peanut allergy. J Allergy Clin Immunol. 2004;114(6):1410–7. 10.1016/j.jaci.2004.09.014 [DOI] [PubMed] [Google Scholar]
- 35.Mittag D, et al. A novel approach for investigation of specific and cross-reactive IgE epitopes on Bet v 1 and homologous food allergens in individual patients. Mol Immunol. 2006;43(3):268–78. 10.1016/j.molimm.2005.02.008 [DOI] [PubMed] [Google Scholar]
- 36.Riecken S, et al. Purification and characterization of natural Ara h 8, the Bet v 1 homologous allergen from peanut, provides a novel isoform. Biol Chem. 2008;389(4):415–23. 10.1515/BC.2008.038 [DOI] [PubMed] [Google Scholar]
- 37.Krause S, et al. Lipid transfer protein (Ara h 9) as a new peanut allergen relevant for a Mediterranean allergic population. J Allergy Clin Immunol. 2009;124(4):771-8.e5. 10.1016/j.jaci.2009.06.008 [DOI] [PubMed] [Google Scholar]
- 38.Cañas JA, et al. Basophil Activation Test Utility as a Diagnostic Tool in LTP Allergy. Int J Mol Sci. 2022;23(9). [DOI] [PMC free article] [PubMed]
- 39.Lauer I, et al. The non-specific lipid transfer protein, Ara h 9, is an important allergen in peanut. Clin Exp Allergy. 2009;39(9):1427–37. 10.1111/j.1365-2222.2009.03312.x [DOI] [PubMed] [Google Scholar]
- 40.Schwager C, et al. Development of a novel strategy to isolate lipophilic allergens (oleosins) from peanuts. PLoS ONE. 2015;10(4):e0123419. 10.1371/journal.pone.0123419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schwager C, et al. Peanut oleosins associated with severe peanut allergy-importance of lipophilic allergens for comprehensive allergy diagnostics. J Allergy Clin Immunol. 2017;140(5):1331-1338.e8. 10.1016/j.jaci.2017.02.020 [DOI] [PubMed] [Google Scholar]
- 42.Cabanos C, et al. Expression and purification of peanut oleosins in insect cells. Protein J. 2011;30(7):457–63. 10.1007/s10930-011-9351-z [DOI] [PubMed] [Google Scholar]
- 43.Petersen A, et al. Peanut defensins: Novel allergens isolated from lipophilic peanut extract. J Allergy Clin Immunol. 2015;136(5):1295–301.e1–5. [DOI] [PubMed]
- 44.Pons L, et al. Purification and cloning of two high molecular mass isoforms of peanut seed oleosin encoded by cDNAs of equal sizes. Plant Physiol Biochem. 2005;43(7):659–68. 10.1016/j.plaphy.2005.06.002 [DOI] [PubMed] [Google Scholar]
- 45.Pons L, et al. The 18 kDa peanut oleosin is a candidate allergen for IgE-mediated reactions to peanuts. Allergy. 2002;57(Suppl 72):88–93. 10.1034/j.1398-9995.57.s72.16.x [DOI] [PubMed] [Google Scholar]
- 46.Aalberse RC, et al. Identification of the amino-terminal fragment of Ara h 1 as a major target of the IgE-binding activity in the basic peanut protein fraction. Clin Exp Allergy. 2020;50(3):401–5. 10.1111/cea.13554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mattsson L, et al. Cyclophilin - A novel cross-reactive determinant in peanut. Clin Exp Allergy. 2021;51(4):620–2. 10.1111/cea.13833 [DOI] [PubMed] [Google Scholar]
- 48.Burks AW, et al. Identification of peanut agglutinin and soybean trypsin inhibitor as minor legume allergens. Int Arch Allergy Immunol. 1994;105(2):143–9. 10.1159/000236816 [DOI] [PubMed] [Google Scholar]
- 49.Gruber P, Becker WM, Hofmann T. Influence of the maillard reaction on the allergenicity of rAra h 2, a recombinant major allergen from peanut (Arachis hypogaea), its major epitopes, and peanut agglutinin. J Agric Food Chem. 2005;53(6):2289–96. 10.1021/jf048398w [DOI] [PubMed] [Google Scholar]
- 50.Rougé P, et al. Characterization of IgE-binding epitopes of peanut (Arachis hypogaea) PNA lectin allergen cross-reacting with other structurally related legume lectins. Mol Immunol. 2010;47(14):2359–66. 10.1016/j.molimm.2010.05.006 [DOI] [PubMed] [Google Scholar]
- 51.Rouge P, et al. Peanut lectin. Rev Fr Allergol. 2010;50(3):281–4. [Google Scholar]
- 52.Misra A, et al. Partial characterization of red gram (Cajanus cajan L. Millsp) polypeptides recognized by patients exhibiting rhinitis and bronchial asthma. Food Chem Toxicol. 2010;48(10):2725–36. 10.1016/j.fct.2010.06.047 [DOI] [PubMed] [Google Scholar]
- 53.Bar-El Dadon S, et al. Vicilin and the basic subunit of legumin are putative chickpea allergens. Food Chem. 2013;138(1):13–8. 10.1016/j.foodchem.2012.10.031 [DOI] [PubMed] [Google Scholar]
- 54.Wangorsch A, et al. Identification and Characterization of IgE-Reactive Proteins and a New Allergen (Cic a 1.01) from Chickpea (Cicer arietinum). Mol Nutr Food Res. 2020;64(19):e2000560. 10.1002/mnfr.202000560 [DOI] [PubMed] [Google Scholar]
- 55.Vioque J, et al. Purification and partial characterization of chickpea 2S albumin. J Agric Food Chem. 1999;47(4):1405–9. 10.1021/jf980819k [DOI] [PubMed] [Google Scholar]
- 56.Kulkarni A, Ananthanarayan L, Raman K. Identification of putative and potential cross-reactive chickpea (Cicer arietinum) allergens through an in silico approach. Comput Biol Chem. 2013;47:149–55. 10.1016/j.compbiolchem.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 57.Vioque J, et al. Comparative Study of Chickpea and Pea Pa2 Albumins. J Agric Food Chem. 1998;46(9):3609–13. 10.1021/jf980351l [DOI] [Google Scholar]
- 58.Verma AK, et al. Purification, characterization and allergenicity assessment of 26kDa protein, a major allergen from Cicer arietinum. Mol Immunol. 2016;74:113–24. 10.1016/j.molimm.2016.05.002 [DOI] [PubMed] [Google Scholar]
- 59.Castano R. Occupational rhinitis caused by concurrent sensitization to two different allergens. Occup Med (Lond). 2012;62(6):466–8. 10.1093/occmed/kqs063 [DOI] [PubMed] [Google Scholar]
- 60.Papanikolaou I, et al. Anaphylactic shock to guar gum (food additive E412) contained in a meal substitute. Allergy. 2007;62(7):822. 10.1111/j.1398-9995.2007.01369.x [DOI] [PubMed] [Google Scholar]
- 61.Roesch A, et al. Severe contact urticaria to guar gum included as gelling agent in a local anaesthetic. Contact Dermatitis. 2005;52(6):307–8. 10.1111/j.0105-1873.2005.00589.x [DOI] [PubMed] [Google Scholar]
- 62.González R, et al. Identification of soybean proteins responsible for respiratory allergies. Int Arch Allergy Appl Immunol. 1991;95(1):53–7. 10.1159/000235454 [DOI] [PubMed] [Google Scholar]
- 63.González R, et al. Soybean hydrophobic protein and soybean hull allergy. Lancet. 1995;346:48–9. 10.1016/S0140-6736(95)92676-3 [DOI] [PubMed] [Google Scholar]
- 64.Codina R, et al. Purification and characterization of a soybean hull allergen responsible for the Barcelona asthma outbreaks. II. Purification and sequencing of the Gly m 2 allergen. Clin Exp Allergy. 1997;27(4):424–30. 10.1111/j.1365-2222.1997.tb00728.x [DOI] [PubMed] [Google Scholar]
- 65.Codina R, et al. Identification of the soybean hull allergens responsible for the Barcelona asthma outbreaks. Int Arch Allergy Immunol. 1999;119(1):69–71. 10.1159/000024178 [DOI] [PubMed] [Google Scholar]
- 66.Codina R, Oehling AG Jr, Lockey RF. Neoallergens in heated soybean hull. Int Arch Allergy Immunol. 1998;117(2):120–5. 10.1159/000023998 [DOI] [PubMed] [Google Scholar]
- 67.Rihs HP, et al. IgE binding of the recombinant allergen soybean profilin (rGly m 3) is mediated by conformational epitopes. J Allergy Clin Immunol. 1999;104(6):1293–301. 10.1016/S0091-6749(99)70027-8 [DOI] [PubMed] [Google Scholar]
- 68.Amnuaycheewa P, de Mejia EG. Purification, characterisation, and quantification of the soy allergen profilin (Gly m 3) in soy products. Food Chem. 2010;119(4):1671–80. 10.1016/j.foodchem.2009.09.034 [DOI] [Google Scholar]
- 69.Crowell DN, et al. Characterization of a stress-induced, developmentally regulated gene family from soybean. Plant Mol Biol. 1992;18(3):459–66. 10.1007/BF00040662 [DOI] [PubMed] [Google Scholar]
- 70.Mittag D, et al. Soybean allergy in patients allergic to birch pollen: clinical investigation and molecular characterization of allergens. J Allergy Clin Immunol. 2004;113(1):148–54. 10.1016/j.jaci.2003.09.030 [DOI] [PubMed] [Google Scholar]
- 71.Berkner H, et al. Cross-reactivity of pollen and food allergens: soybean Gly m 4 is a member of the Bet v 1 superfamily and closely resembles yellow lupine proteins. Biosci Rep. 2009;29(3):183–92. 10.1042/BSR20080117 [DOI] [PubMed] [Google Scholar]
- 72.Kleine-Tebbe J, et al. Severe oral allergy syndrome and anaphylactic reactions caused by a Bet v 1- related PR-10 protein in soybean, SAM22. 2002;110(5):797–804. [DOI] [PubMed]
- 73.Evrard B, et al. Utility of the Basophil Activation Test Using Gly m 4, Gly m 5 and Gly m 6 Molecular Allergens for Characterizing Anaphylactic Reactions to Soy. Front Allergy. 2022;3:908435. 10.3389/falgy.2022.908435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Guhsl EE, et al. Vig r 6, the cytokinin-specific binding protein from mung bean (Vigna radiata) sprouts, cross-reacts with Bet v 1-related allergens and binds IgE from birch pollen allergic patients’ sera. Mol Nutr Food Res. 2014;58(3):625–34. 10.1002/mnfr.201300153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ogawa T, et al. Investigation of the IgE-binding proteins in soybeans by immunoblotting with the sera of the soybean-sensitive patients with atopic dermatitis. J Nutr Sci Vitaminol (Tokyo). 1991;37(6):555–65. 10.3177/jnsv.37.555 [DOI] [PubMed] [Google Scholar]
- 76.Petruccelli S, Chirdo FG, Anon MC. Immunochemical reactivity of soybean b -conglycinin subunits. Food Agric Immunol. 2005;16(1):17–28. 10.1080/09540100500054727 [DOI] [Google Scholar]
- 77.Holzhauser T, et al. Soybean (Glycine max) allergy in Europe: Gly m 5 (beta-conglycinin) and Gly m 6 (glycinin) are potential diagnostic markers for severe allergic reactions to soy. J Allergy Clin Immunol. 2009;123(2):452–8. 10.1016/j.jaci.2008.09.034 [DOI] [PubMed] [Google Scholar]
- 78.Krishnan HB, et al. All three subunits of soybean beta-conglycinin are potential food allergens. J Agric Food Chem. 2009;57(3):938–43. 10.1021/jf802451g [DOI] [PubMed] [Google Scholar]
- 79.Zheng S, et al. Purification and IgE-binding properties of soybean b -conglycinin subunits. Process Biochem. 2012;47(12):2531–7. 10.1016/j.procbio.2012.07.003 [DOI] [Google Scholar]
- 80.Taliercio E, Kim SW. Identification of a second major antigenic epitope in the a -subunit of soy b -conglycinin. Food Agric Immunol. 2013(0).
- 81.Sun X, et al. Prediction and characterization of the linear IgE epitopes for the major soybean allergen β-conglycinin using immunoinformatics tools. Food Chem Toxicol. 2013;56:254–60. 10.1016/j.fct.2013.02.014 [DOI] [PubMed] [Google Scholar]
- 82.Pedersen MH, et al. Soybean allergen detection methods–a comparison study. Mol Nutr Food Res. 2008;52(12):1486–96. 10.1002/mnfr.200700394 [DOI] [PubMed] [Google Scholar]
- 83.Zeece MG, et al. Identification of an IgE-binding region in soybean acidic glycinin G1. Food Agric Immunol. 1999;11(1):83–90. 10.1080/09540109999942 [DOI] [Google Scholar]
- 84.Beardslee TA, et al. Soybean glycinin G1 acidic chain shares IgE epitopes with peanut allergen Ara h 3. Int Arch Allergy Immunol. 2000;123(4):299–307. 10.1159/000053642 [DOI] [PubMed] [Google Scholar]
- 85.Xiang P, et al. Identification and analysis of a conserved immunoglobulin E-binding epitope in soybean G1a and G2a and peanut Ara h 3 glycinins. Arch Biochem Biophys. 2002;408(1):51–7. 10.1016/S0003-9861(02)00534-9 [DOI] [PubMed] [Google Scholar]
- 86.Helm RM, et al. A soybean G2 glycinin allergen. 2. Epitope mapping and three-dimensional modeling. Int Arch Allergy Immunol. 2000;123(3):213–9. 10.1159/000024446 [DOI] [PubMed] [Google Scholar]
- 87.Helm RM, et al. A soybean G2 glycinin allergen. 1. Identification and characterization. Int Arch Allergy Immunol. 2000;123(3):205–12. 10.1159/000024445 [DOI] [PubMed] [Google Scholar]
- 88.Magni C, et al. Two-dimensional electrophoresis and western-blotting analyses with anti Ara h 3 basic subunit IgG evidence the cross-reacting polypeptides of Arachis hypogaea, Glycine max, and Lupinus albus seed proteomes. J Agric Food Chem. 2005;53(6):2275–81. 10.1021/jf0491512 [DOI] [PubMed] [Google Scholar]
- 89.Riascos JJ, et al. The Seed Biotinylated Protein of Soybean (Glycine max): A Boiling-Resistant New Allergen (Gly m 7) with the Capacity To Induce IgE-Mediated Allergic Responses. J Agric Food Chem. 2016;64(19):3890–900. 10.1021/acs.jafc.5b05873 [DOI] [PubMed] [Google Scholar]
- 90.Ebisawa M, et al. Gly m 2S albumin is a major allergen with a high diagnostic value in soybean-allergic children. J Allergy Clin Immunol. 2013;132(4):976–8.e1–5. [DOI] [PubMed]
- 91.Klemans RJ, et al. Components in soy allergy diagnostics: Gly m 2S albumin has the best diagnostic value in adults. Allergy. 2013;68(11):1396–402. 10.1111/all.12259 [DOI] [PubMed] [Google Scholar]
- 92.Gu X, et al. Identification of IgE-binding proteins in soy lecithin. Int Arch Allergy Immunol. 2001;126(3):218–25. 10.1159/000049517 [DOI] [PubMed] [Google Scholar]
- 93.Lin J, et al. The potential allergenicity of two 2S albumins from soybean (Glycine max): a protein microarray approach. Int Arch Allergy Immunol. 2006;141(2):91–102. 10.1159/000094535 [DOI] [PubMed] [Google Scholar]
- 94.Tsuji H, et al. Purification of characterization of soybean allergen Gly m Bd 28K. Biosci Biotechnol Biochem. 1997;61(6):942–7. 10.1271/bbb.61.942 [DOI] [PubMed] [Google Scholar]
- 95.Helm RM, et al. Mutational analysis of the IgE-binding epitopes of P34/Gly m Bd 30K. J Allergy Clin Immunol. 2000;105(2 Pt 1):378–84. 10.1016/S0091-6749(00)90091-5 [DOI] [PubMed] [Google Scholar]
- 96.Babiker EE, et al. Immunological characterization of recombinant soy protein allergen produced by Escherichia coli expression system. J Agric Food Chem. 2000;48(2):571–5. 10.1021/jf990314+ [DOI] [PubMed] [Google Scholar]
- 97.Xiang P, et al. P39, a novel soybean protein allergen, belongs to a plant-specific protein family and is present in protein storage vacuoles. J Agric Food Chem. 2008;56(6):2266–72. 10.1021/jf073292x [DOI] [PubMed] [Google Scholar]
- 98.Codina R, et al. Identification of the soybean hull allergens involved in sensitization to soybean dust in a rural population from Argentina and N-terminal sequence of a major 50 KD allergen. Clin Exp Allergy. 2002;32(7):1059–63. 10.1046/j.1365-2222.2002.01411.x [DOI] [PubMed] [Google Scholar]
- 99.Batista R, et al. A proteomic study to identify soya allergens–the human response to transgenic versus non-transgenic soya samples. Int Arch Allergy Immunol. 2007;144(1):29–38. 10.1159/000102611 [DOI] [PubMed] [Google Scholar]
- 100.Gubesch M, et al. Strategy for allergenicity assessment of “natural novel foods”: clinical and molecular investigation of exotic vegetables (water spinach, hyacinth bean and Ethiopian eggplant). Allergy. 2007;62(11):1243–50. 10.1111/j.1398-9995.2007.01474.x [DOI] [PubMed] [Google Scholar]
- 101.Valdivieso R, Quirce S, Sainz T. Bronchial asthma caused by Lathyrus sativus flour. Allergy. 1988;43(7):536–9. 10.1111/j.1398-9995.1988.tb01633.x [DOI] [PubMed] [Google Scholar]
- 102.San Ireneo MM, et al. Allergenicity of vetchling (Lathyrus sativus). Rev Esp Alergol Inmunol Clin. 1998;13(5):282–6. [Google Scholar]
- 103.Porcel S, et al. Occupational asthma caused by grass pea used in the industrial processing of parquet. Allergol Immunopathol (Madr). 2001;29(5):207–11. 10.1016/S0301-0546(01)79058-1 [DOI] [PubMed] [Google Scholar]
- 104.Porcel S, et al. Occupational rhinitis and asthma by Lathyrus sativus flour: characterization of allergens. J Allergy Clin Immunol. 2001;107(4):743–4. 10.1067/mai.2001.113567 [DOI] [PubMed] [Google Scholar]
- 105.Qureshi IA, Sethi DK, Salunke DM. Purification, identification and preliminary crystallographic studies of an allergenic protein from Lathyrus sativus. Acta Crystallogr Sect F Struct Biol Cryst Commun. 2006;62(Pt 9):869–72. 10.1107/S1744309106028077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sánchez-Monge R, et al. Isolation and characterization of relevant allergens from boiled lentils. J Allergy Clin Immunol. 2000;106(5):955–61. 10.1067/mai.2000.109912 [DOI] [PubMed] [Google Scholar]
- 107.Lopez-Torrejon G, et al. Len c 1, a major allergen and vicilin from lentil seeds: Protein isolation and cDNA cloning. J Allergy Clin Immunol. 2003;112(6):1208–15. 10.1016/j.jaci.2003.08.035 [DOI] [PubMed] [Google Scholar]
- 108.Sanchez-Monge R, et al. Vicilin and convicilin are potential major allergens from pea. Clin Exp Allergy. 2004;34(11):1747–53. 10.1111/j.1365-2222.2004.02085.x [DOI] [PubMed] [Google Scholar]
- 109.Scippa GS, et al. The proteome of lentil (Lens culinaris Medik.) seeds: Discriminating between landraces. Electrophoresis. 2010;31(3):497–506. 10.1002/elps.200900459 [DOI] [PubMed] [Google Scholar]
- 110.Akkerdaas J, et al. Lentil (Lens culinaris) lipid transfer protein Len c 3: a novel legume allergen. Int Arch Allergy Immunol. 2012;157(1):51–7. 10.1159/000324946 [DOI] [PubMed] [Google Scholar]
- 111.Finkina EI, et al. Purification and primary structure of novel lipid transfer proteins from germinated lentil (Lens culinaris) seeds. Biochemistry (Mosc). 2007;72(4):430–8. 10.1134/S0006297907040104 [DOI] [PubMed] [Google Scholar]
- 112.Ballabio C, et al. Characterization of the sensitization profile to lupin in peanut-allergic children and assessment of cross-reactivity risk. Pediatr Allergy Immunol. 2013;24(3):270–5. 10.1111/pai.12054 [DOI] [PubMed] [Google Scholar]
- 113.Sirtori E, et al. Cross-reactivity between peanut and lupin proteins. Food Chem. 2011;126(3):902–10. 10.1016/j.foodchem.2010.11.073 [DOI] [Google Scholar]
- 114.Guillamón E, et al. Characterization of lupin major allergens (Lupinus albus L.). Mol Nutr Food Res. 2010;54(11):1668–76. 10.1002/mnfr.200900452 [DOI] [PubMed] [Google Scholar]
- 115.Pinto MP, Ricardo CP. Lupinus albus L. pathogenesis-related proteins that show similarity to PR-10 proteins. Plant Physiol. 1995;109(4):1345–51. 10.1104/pp.109.4.1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tian L, et al. Transcript and proteomic analysis of developing white lupin (Lupinus albus L.) roots. BMC Plant Biol. 2009;9(0):1. 10.1186/1471-2229-9-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jappe U, et al. Identification and Purification of Novel Low-Molecular-Weight Lupine Allergens as Components for Personalized Diagnostics. Nutrients. 2021;13(2). First study that shows differences in protein/allergen content and composition of different lupine species and the identification of new lupine allergens. [DOI] [PMC free article] [PubMed]
- 118.Dooper MM, et al. Monoclonal Antibodies against the Candidate Lupin Allergens a-Conglutin and b-Conglutin. Int Arch Allergy Immunol. 2007;143(1):49–58. 10.1159/000098224 [DOI] [PubMed] [Google Scholar]
- 119.Fiocchi A, et al. Assessment of the tolerance to lupine-enriched pasta in peanut-allergic children. Clin Exp Allergy. 2009;39(7):1045–51. 10.1111/j.1365-2222.2009.03199.x [DOI] [PubMed] [Google Scholar]
- 120.Nakamura R, Teshima R. Immunoproteomics analysis of food allergens. Methods Mol Biol. 2014;1072:725–35. 10.1007/978-1-62703-631-3_50 [DOI] [PubMed] [Google Scholar]
- 121.Magni C, et al. One- and Two-Dimensional Electrophoretic Identification of IgE-Binding Polypeptides of Lupinus albus and Other Legume Seeds. J Agric Food Chem. 2005;53(11):4567–71. 10.1021/jf0500785 [DOI] [PubMed] [Google Scholar]
- 122.Goggin DE, et al. Proteomic analysis of lupin seed proteins to identify conglutin Beta as an allergen, Lup an 1. J Agric Food Chem. 2008;56(15):6370–7. 10.1021/jf800840u [DOI] [PubMed] [Google Scholar]
- 123.Mairal T, et al. FRET-based dimeric aptamer probe for selective and sensitive Lup an 1 allergen detection. Biosens Bioelectron. 2014;54C:207–10. 10.1016/j.bios.2013.10.070 [DOI] [PubMed] [Google Scholar]
- 124.Foley RC, et al. Identification and characterisation of seed storage protein transcripts from Lupinus angustifolius. BMC Plant Biol. 2011;11(1):59. 10.1186/1471-2229-11-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jimenez-Lopez JC, et al. Characterization of narrow-leaf lupin (Lupinus angustifolius L.) recombinant major allergen IgE-binding proteins and the natural β-conglutin counterparts in sweet lupin seed species. Food Chem. 2018;244:60–70. 10.1016/j.foodchem.2017.10.015 [DOI] [PubMed] [Google Scholar]
- 126.Hane JK, et al. A comprehensive draft genome sequence for lupin (Lupinus angustifolius), an emerging health food: insights into plant-microbe interactions and legume evolution. Plant Biotechnol J. 2017;15(3):318–30. 10.1111/pbi.12615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Dooper MM, et al. Immunoglobulin E Cross-Reactivity Between Lupine Conglutins and Peanut Allergens in Serum of Lupine-Allergic Individuals. J Investig Allergol Clin Immunol. 2009;19(4):283–91. [PubMed] [Google Scholar]
- 128.Klos P, et al. Identification of a specific IgE-binding protein from narrow-leafed lupin (L. Angustifolius) seeds. J Food Sci. 2010;75(1):H39–43. 10.1111/j.1750-3841.2009.01440.x [DOI] [PubMed] [Google Scholar]
- 129.Dall’Antonia F, et al. Prediction of IgE-binding epitopes by means of allergen surface comparison and correlation to cross-reactivity. J Allergy Clin Immunol. 2011;128(4):872–879.e8. 10.1016/j.jaci.2011.07.007 [DOI] [PubMed] [Google Scholar]
- 130.Fernandes H, et al. Lupinus luteus pathogenesis-related protein as a reservoir for cytokinin. J Mol Biol. 2008;378(5):1040–51. 10.1016/j.jmb.2008.03.027 [DOI] [PubMed] [Google Scholar]
- 131.Pramod SN, Krishnakantha TP, Venkatesh YP. Effect of horse gram lectin (Dolichos biflorus agglutinin) on degranulation of mast cells and basophils of atopic subjects: identification as an allergen. Int Immunopharmacol. 2006;6(11):1714–22. 10.1016/j.intimp.2006.07.006 [DOI] [PubMed] [Google Scholar]
- 132.Fine AJ. Hypersensitivity reaction to jicama (Pachyrhizus, yam bean). Ann Allergy. 1991;66(2):173–4. [PubMed] [Google Scholar]
- 133.Bedolla-Barajas M, et al. Oral Allergy Syndrome Associated with Jicama. Med J Islam Repub Iran. 2022;36:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Narayan S, Sansom JE. Contact urticaria from runner bean (Phaseolus coccineus). Contact Dermatitis. 2002;47(4):243. 10.1034/j.1600-0536.2002.4704172.x [DOI] [PubMed] [Google Scholar]
- 135.Dhyani A, et al. Immunoglobulin E (IgE)-mediated cross-reactivity between mesquite pollen proteins and lima bean, an edible legume. Clin Exp Immunol. 2007;149(3):517–24. 10.1111/j.1365-2249.2007.03446.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Sharma GM, Roux KH, Sathe SK. A sensitive and robust competitive enzyme-linked immunosorbent assay for Brazil nut ( Bertholletia excelsa L.) detection. J Agric Food Chem. 2009;57(2):769–76. 10.1021/jf803003z [DOI] [PubMed] [Google Scholar]
- 137.Palacín A, et al. Graph based study of allergen cross-reactivity of plant lipid transfer proteins (LTPs) using microarray in a multicenter study. PLoS ONE. 2012;7(12):e50799. 10.1371/journal.pone.0050799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zoccatelli G, et al. Identification and characterization of the major allergen of green bean (Phaseolus vulgaris) as a non-specific lipid transfer protein (Pha v 3). Mol Immunol. 2010;47(7–8):1561–8. 10.1016/j.molimm.2010.01.009 [DOI] [PubMed] [Google Scholar]
- 139.Pastorello EA, et al. Green bean (Phaseolus vulgaris): a new source of IgE-binding lipid transfer protein. J Agric Food Chem. 2010;58(7):4513–6. 10.1021/jf100213g [DOI] [PubMed] [Google Scholar]
- 140.Vidali L, et al. Purification, characterization, and cDNA cloning of profilin from Phaseolus vulgaris. Plant Physiol. 1995;108(1):115–23. 10.1104/pp.108.1.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Campbell PM, et al. Comparison of the α-amylase inhibitor-1 from common bean (Phaseolus vulgaris) varieties and transgenic expression in other legumes–post-translational modifications and immunogenicity. J Agric Food Chem. 2011;59(11):6047–54. 10.1021/jf200456j [DOI] [PubMed] [Google Scholar]
- 142.Sánchez-Monge R, et al. Class I chitinases, the panallergens responsible for the latex-fruit syndrome, are induced by ethylene treatment and inactivated by heating. J Allergy Clin Immunol. 2000;106(1 Pt 1):190–5. 10.1067/mai.2000.107599 [DOI] [PubMed] [Google Scholar]
- 143.Kumar S, et al. Leucoagglutinating phytohemagglutinin: purification, characterization, proteolytic digestion and assessment for allergenicity potential in BALB/c mice. Immunopharmacol Immunotoxicol. 2014;36(2):138–44. 10.3109/08923973.2014.884136 [DOI] [PubMed] [Google Scholar]
- 144.Kasera R, et al. Purification and immunobiochemical characterization of a 31 kDa cross-reactive allergen from Phaseolus vulgaris (kidney bean). PLoS ONE. 2013;8(5):e63063. 10.1371/journal.pone.0063063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kumar S, et al. Phaseolin: a 47.5kDa protein of red kidney bean (Phaseolus vulgaris L.) plays a pivotal role in hypersensitivity induction. Int Immunopharmacol. 2014;19(1):178–90. 10.1016/j.intimp.2014.01.014 [DOI] [PubMed] [Google Scholar]
- 146.Rougé P, et al. A case of severe anaphylaxis to kidney bean: phaseolin (vicilin) and PHA (lectin) identified as putative allergens. Allergy. 2011;66(2):301–2. 10.1111/j.1398-9995.2010.02466.x [DOI] [PubMed] [Google Scholar]
- 147.Wensing M, et al. Patients with anaphylaxis to pea can have peanut allergy caused by cross-reactive IgE to vicilin (Ara h 1). J Allergy Clin Immunol. 2003;111(2):420–4. 10.1067/mai.2003.61 [DOI] [PubMed] [Google Scholar]
- 148.Dziuba J, et al. Proteomic analysis of albumin and globulin fractions of pea (Pisum sativum L.) seeds. Acta Sci Pol Technol Aliment. 2014;13(2):181–90. 10.17306/J.AFS.2014.2.7 [DOI] [PubMed] [Google Scholar]
- 149.Bogdanov IV, et al. A novel lipid transfer protein from the pea Pisum sativum: isolation, recombinant expression, solution structure, antifungal activity, lipid binding, and allergenic properties. BMC Plant Biol. 2016;16:107. 10.1186/s12870-016-0792-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Barkholt V, et al. Protein modification by fermentation: effect of fermentation on the potential allergenicity of pea. Allergy. 1998;53(46 Suppl):106–8. 10.1111/j.1398-9995.1998.tb04976.x [DOI] [PubMed] [Google Scholar]
- 151.Srivastava S, et al. Pea PR 10.1 is a Ribonuclease and its Transgenic Expression Elevates Cytokinin Levels. Plant Growth Regul. 2006;49(1):17–25. 10.1007/s10725-006-0022-6 [DOI] [Google Scholar]
- 152.Faeste CK, et al. Characterization of potential allergens in fenugreek (Trigonella foenum-graecum) using patient sera and MS-based proteomic analysis. J Proteomics. 2010;73(7):1321–33. 10.1016/j.jprot.2010.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kumari D, et al. Isolation and characterization of a 28 kDa major allergen from blackgram (Phaseolus mungo). Immunobiology. 2012;217(9):895–904. 10.1016/j.imbio.2011.12.011 [DOI] [PubMed] [Google Scholar]
- 154.Mittag D, et al. Birch pollen-related food allergy to legumes: identification and characterization of the Bet v 1 homologue in mungbean (Vigna radiata), Vig r 1. Clin Exp Allergy. 2005;35(8):1049–55. 10.1111/j.1365-2222.2005.02309.x [DOI] [PubMed] [Google Scholar]
- 155.Guhsl EE, et al. IgE, IgG4 and IgA specific to Bet v 1-related food allergens do not predict oral allergy syndrome. Allergy. 2015;70(1):59–66. 10.1111/all.12534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Misra A, et al. Potential allergens of green gram (Vigna radiata L. Millsp) identified as members of cupin superfamily and seed albumin. Clin Exp Allergy. 2011;41(8):1157–68. 10.1111/j.1365-2222.2011.03780.x [DOI] [PubMed] [Google Scholar]
- 157.Bernardo AE, et al. 8S globulin of mungbean [Vigna radiata (L.) Wilczek]: cloning and characterization of its cDNA isoforms, expression in Escherichia coli, purification, and crystallization of the major recombinant 8S isoform. J Agric Food Chem. 2004;52(9):2552–60. 10.1021/jf0305938 [DOI] [PubMed] [Google Scholar]
- 158.Ding LW, et al. Using silica particles to isolate total RNA from plant tissues recalcitrant to extraction in guanidine thiocyanate. Anal Biochem. 2008;374(2):426–8. 10.1016/j.ab.2007.11.030 [DOI] [PubMed] [Google Scholar]
- 159.Fujimoto Y, et al. Purification and cDNA cloning of cytokinin-specific binding protein from mung bean (Vigna radiata). Eur J Biochem. 1998;258(2):794–802. 10.1046/j.1432-1327.1998.2580794.x [DOI] [PubMed] [Google Scholar]
- 160.Chentouh MM, et al. Allergenic risk assessment of cowpea and its cross-reactivity with pea and peanut. Pediatr Allergy Immunol. 2022;33(12):e13889. 10.1111/pai.13889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Dölle-Bierke S, et al. Food-Induced Anaphylaxis: Data From the European Anaphylaxis Registry. J Allergy Clin Immunol Pract. 2023;11(7):2069-2079.e7. 10.1016/j.jaip.2023.03.026 [DOI] [PubMed] [Google Scholar]
- 162.Didinger C, Thompson HJ. Defining Nutritional and Functional Niches of Legumes: A Call for Clarity to Distinguish a Future Role for Pulses in the Dietary Guidelines for Americans. Nutrients. 2021;13(4). [DOI] [PMC free article] [PubMed]
- 163.Shao Q, et al. New Insights Into the Role of Seed Oil Body Proteins in Metabolism and Plant Development. Front Plant Sci. 2019;10:1568. 10.3389/fpls.2019.01568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Parthibane V, et al. Oleosin is bifunctional enzyme that has both monoacylglycerol acyltransferase and phospholipase activities. J Biol Chem. 2012;287(3):1946–54. 10.1074/jbc.M111.309955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Cabanillas B, Jappe U, Novak N. Allergy to Peanut, Soybean, and Other Legumes: Recent Advances in Allergen Characterization, Stability to Processing and IgE Cross-Reactivity. Mol Nutr Food Res. 2018;62(1). [DOI] [PubMed]
- 166.Lieberman JA, et al. The global burden of illness of peanut allergy: A comprehensive literature review. Allergy. 2021;76(5):1367–84. 10.1111/all.14666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Novembre E, et al. Fatal food anaphylaxis in adults and children. Ital J Pediatr. 2024;50(1):40. 10.1186/s13052-024-01608-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Al-Muhsen S, Clarke AE, Kagan RS. Peanut allergy: an overview. CMAJ. 2003;168(10):1279–85. [PMC free article] [PubMed] [Google Scholar]
- 169.Muller T, et al. Relevance of sensitization to legumes in peanut-allergic children. Pediatr Allergy Immunol. 2022;33(9):e13846. First large-scale study that elucidated the sensitization profile towards eight different legumes such as lupine and pea in peanut-allergic children (n=195), indicating the need for more comprehensive diagnostic measures. 10.1111/pai.13846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Briceno D, et al. Soy Gly m 8 sIgE Has Limited Value in the Diagnosis of Soy Allergy in Peanut Ara h 2-Sensitized Adults. Int Arch Allergy Immunol. 2023;184(8):767–75. 10.1159/000530026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Peeters KA, et al. Clinical relevance of sensitization to lupine in peanut-sensitized adults. Allergy. 2009;64(4):549–55. 10.1111/j.1398-9995.2008.01818.x [DOI] [PubMed] [Google Scholar]
- 172.World Health Organization & Food and Agriculture Organization of the United Nations. (2022). Risk assessment of food allergens: part 1: review and validation of Codex alimentarius priority allergen list through risk assessment: meeting report. World Health Organization. 10.4060/cb9070en. License: CC BY-NC-SA 3.0 IGO
- 173.Akiyama H, Imai T, Ebisawa M. Japan food allergen labeling regulation–history and evaluation. Adv Food Nutr Res. 2011;62:139–71. 10.1016/B978-0-12-385989-1.00004-1 [DOI] [PubMed] [Google Scholar]
- 174.Gupta RS, et al. Prevalence and Severity of Food Allergies Among US Adults. JAMA Netw Open. 2019;2(1):e185630. 10.1001/jamanetworkopen.2018.5630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Hultquist H, et al. Phenotypic characterization of childhood- and adult-onset food allergy among adults in the United States. J Allergy Clin Immunol Glob. 2022;1(4):257–64. 10.1016/j.jacig.2022.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Spolidoro GCI, et al. Prevalence estimates of eight big food allergies in Europe: Updated systematic review and meta-analysis. Allergy. 2023;78(9):2361–417. An updated systematic review and meta-analysis by the European Academy of Allergy and Clinical Immunology on the frequency of food allergy and food sensitization towards the eight most common food allergen sources in Europe between 2000-2021. 10.1111/all.15801 [DOI] [PubMed] [Google Scholar]
- 177.Ito K, et al. IgE to Gly m 5 and Gly m 6 is associated with severe allergic reactions to soybean in Japanese children. J Allergy Clin Immunol. 2011;128(3):673–5. 10.1016/j.jaci.2011.04.025 [DOI] [PubMed] [Google Scholar]
- 178.Asero R, et al. Systemic allergic reactions induced by labile plant-food allergens: Seeking potential cofactors. A multicenter study Allergy. 2021;76(5):1473–9. [DOI] [PubMed] [Google Scholar]
- 179.Hayashi M, et al. Food-dependent exercise-induced anaphylaxis to soybean: Gly m 5 and Gly m 6 as causative allergen components. World Allergy Organ J. 2020;13(7):100439. 10.1016/j.waojou.2020.100439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Adachi A, et al. Soybean β‐conglycinin as the main allergen in a patient with food‐dependent exercise‐induced anaphylaxis by tofu: food processing alters pepsin resistance. 2009;39. [DOI] [PubMed]
- 181.Kleine‐Tebbe J, et al. Severe oral allergy syndrome and anaphylactic reactions caused by a Bet v 1- related PR-10 protein in soybean, SAM22. J Allergy Clin Immunol. 2002;110(5):797–804. 10.1067/mai.2002.128946 [DOI] [PubMed] [Google Scholar]
- 182.Moreno FJ, Clemente A. 2S Albumin Storage Proteins: What Makes them Food Allergens? Open Biochem J. 2008;2:16–28. 10.2174/1874091X00802010016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Zheng S, et al. Three-dimensional structure of Gly m 5 (β-conglycinin) plays an important role in its stability and overall allergenicity. Food Chem. 2017;234:381–8. 10.1016/j.foodchem.2017.05.020 [DOI] [PubMed] [Google Scholar]
- 184.Zhou F, et al. Prediction and characterization of the T cell epitopes for the major soybean protein allergens using bioinformatics approaches. Proteins. 2022;90(2):418–34. 10.1002/prot.26233 [DOI] [PubMed] [Google Scholar]
- 185.Finkina EI, et al. Structural and Immunologic Properties of the Major Soybean Allergen Gly m 4 Causing Anaphylaxis. Int J Mol Sci. 2022;23(23). [DOI] [PMC free article] [PubMed]
- 186.Matsui T, et al. A case of white bean allergy. Asia Pac Allergy. 2023;13(4):201–4. 10.5415/apallergy.0000000000000111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Laiseca García J, et al. Allergy to White Kidney Beans With Cross-reactivity to Red Kidney Beans: Report of 2 Cases in Children. J Investig Allergol Clin Immunol. 2023;33(2):141–2. 10.18176/jiaci.0818 [DOI] [PubMed] [Google Scholar]
- 188.Kobayashi T, et al. TWO CASES OF ALLERGY WITH MUNG BEAN SPROUTS. Arerugi. 2023;72(8):1046–50. [DOI] [PubMed] [Google Scholar]
- 189.Bernhisel-Broadbent J, Sampson HA. Cross-allergenicity in the legume botanical family in children with food hypersensitivity. J Allergy Clin Immunol. 1989;83(2, Part 1):435–440. [DOI] [PubMed]
- 190.Bernhisel-Broadbent J, Taylor S, Sampson HA. Cross-allergenicity in the legume botanical family in children with food hypersensitivity: II. Laboratory correlates. J Allergy Clin Immunol. 1989;84(5, Part 1):701–709. [DOI] [PubMed]
- 191.Rodríguez-Mazariego ME, et al. Broad Bean-Induced Anaphylaxis: A Case Report. J Investig Allergol Clin Immunol. 2016;26(6):374–5. 10.18176/jiaci.0096 [DOI] [PubMed] [Google Scholar]
- 192.Tonini S, et al. Occupational asthma induced by exposure to lima bean (Phaseolus lunatus). Ann Allergy Asthma Immunol. 2012;108(1):66–7. 10.1016/j.anai.2011.10.009 [DOI] [PubMed] [Google Scholar]
- 193.Kumari D, et al. Sensitization to blackgram in patients with bronchial asthma and rhinitis: clinical evaluation and characterization of allergens. Allergy. 2006;61(1):104–10. 10.1111/j.1398-9995.2006.00990.x [DOI] [PubMed] [Google Scholar]
- 194.Abi-Melhem R, Hassoun Y. Is pea our hidden allergen? An American pediatric case series. J Allergy Clin Immunol Glob. 2023;2(2):100090. 10.1016/j.jacig.2023.100090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Dölle-Bierke S, Grünhagen J, Worm M. Role of vegan diets in food allergies-risk of developing food anaphylaxis? Hautarzt. 2022;73(3):208–11. 10.1007/s00105-022-04949-y [DOI] [PubMed] [Google Scholar]
- 196.Alessandri C, et al. Are peas a safe food for lipid transfer protein allergic patients? Allergy. 2021;76(8):2587–9. 10.1111/all.14801 [DOI] [PubMed] [Google Scholar]
- 197.Popp J, et al. Pea (Pisum sativum) allergy in children: Pis s 1 is an immunodominant major pea allergen and presents IgE binding sites with potential diagnostic value. Clin Exp Allergy. 2020;50(5):625–35. 10.1111/cea.13590 [DOI] [PubMed] [Google Scholar]
- 198.Joehnke MS, et al. Nutritional and anti-nutritional properties of lentil (Lens culinaris) protein isolates prepared by pilot-scale processing. Food Chem X. 2021;9: 100112. 10.1016/j.fochx.2020.100112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Mustafa AM, et al. Polyphenols, Saponins and Phytosterols in Lentils and Their Health Benefits: An Overview. Pharmaceuticals (Basel). 2022;15(10). [DOI] [PMC free article] [PubMed]
- 200.Reese I, et al. Vegan diets from an allergy point of view - Position paper of the DGAKI working group on food allergy. Allergol Select. 2023;7:57–83. 10.5414/ALX02400E [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Akpınar O. Urticaria and Anaphylaxis in a Child after Skin Contact of Lentil Soup. Indian J Pediatr. 2018;85(7):575. 10.1007/s12098-018-2670-8 [DOI] [PubMed] [Google Scholar]
- 202.Vitaliti G, et al. Urticaria and anaphylaxis in a child after inhalation of lentil vapours: a case report and literature review. Ital J Pediatr. 2012;38:71. 10.1186/1824-7288-38-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Ayşenur K, et al. Anaphylaxis induced by lentil inhalation. Asian Pac J Allergy Immunol. 2012;30(2):167–9. [PubMed] [Google Scholar]
- 204.Alnabulsi R, Pak Y, Pasha M. LENTILS, AN UNCOMMON FOOD CAUSING FOOD DEPENDENT EXERCISE INDUCED ANAPHYLAXIS. Ann Allergy Asthma Immunol. 2023;131(5):S97. 10.1016/j.anai.2023.08.286 [DOI] [Google Scholar]
- 205.Orhan F, Karakas T. Food-dependent exercise-induced anaphylaxis to lentil and anaphylaxis to chickpea in a 17-year-old boy. J Investig Allergol Clin Immunol. 2008;18(6):465–8. [PubMed] [Google Scholar]
- 206.Hildebrand HV, et al. Adult and Pediatric Food Allergy to Chickpea, Pea, Lentil, and Lupine: A Scoping Review. J Allergy Clin Immunol Pract. 2021;9(1):290-301.e2. 10.1016/j.jaip.2020.10.046 [DOI] [PubMed] [Google Scholar]
- 207.Bar-El Dadon S, Pascual CY, Reifen R. Food allergy and cross-reactivity-chickpea as a test case. Food Chem. 2014;165:483–8. 10.1016/j.foodchem.2014.05.138 [DOI] [PubMed] [Google Scholar]
- 208.Roberts H, Ben-Shoshan M. Food-dependent exercise-induced anaphylaxis to chickpea in a 17-year-old female: a case report. J Med Case Rep. 2015;9:186. 10.1186/s13256-015-0669-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Cabello-Hurtado F, et al. Proteomics for exploiting diversity of lupin seed storage proteins and their use as nutraceuticals for health and welfare. J Proteomics. 2016;143:57–68. 10.1016/j.jprot.2016.03.026 [DOI] [PubMed] [Google Scholar]
- 210.de Jong NW, et al. Sensitization to lupine flour: is it clinically relevant? Clin Exp Allergy. 2010;40(10):1571–7. 10.1111/j.1365-2222.2010.03496.x [DOI] [PubMed] [Google Scholar]
- 211.Röder M, et al. Detectability of lupine seeds by ELISA and PCR may be strongly influenced by potential differences between cultivars. J Agric Food Chem. 2013;61(25):5936–45. 10.1021/jf400508a [DOI] [PubMed] [Google Scholar]
- 212.Hefle SL, Lemanske RF Jr, Bush RK. Adverse reaction to lupine-fortified pasta. J Allergy Clin Immunol. 1994;94(2 Pt 1):167–72. 10.1053/ai.1994.v94.a54942 [DOI] [PubMed] [Google Scholar]
- 213.Brennecke S, et al. Anaphylactic reaction to lupine flour. J Dtsch Dermatol Ges. 2007;5(9):774–6. 10.1111/j.1610-0387.2007.06457.x [DOI] [PubMed] [Google Scholar]
- 214.Soller L, La Vieille S, Chan ES. First reported case in Canada of anaphylaxis to lupine in a child with peanut allergy. Allergy Asthma Clin Immunol. 2018;14:64. 10.1186/s13223-018-0303-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Jappe U, Vieths S. Lupine, a source of new as well as hidden food allergens. Mol Nutr Food Res. 2010;54(1):113–26. 10.1002/mnfr.200900365 [DOI] [PubMed] [Google Scholar]
- 216.Jardim-Botelho A, et al. Nutritional management of immediate hypersensitivity to legumes in vegetarians. Allergol Immunopathol (Madr). 2022;50(S Pt 1):37–45. [DOI] [PubMed]
- 217.Chan ES, et al. Managing Cross-Reactivity in Those with Peanut Allergy. J Allergy Clin Immunol Pract. 2019;7(2):381–6. 10.1016/j.jaip.2018.11.012 [DOI] [PubMed] [Google Scholar]
- 218.Remington BC, et al. Updated population minimal eliciting dose distributions for use in risk assessment of 14 priority food allergens. Food Chem Toxicol. 2020;139: 111259. 10.1016/j.fct.2020.111259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Behrends J, et al. Innovative robust basophil activation test using a novel gating strategy reliably diagnosing allergy with full automation. Allergy. 2021;76(12):3776–88. 10.1111/all.14900 [DOI] [PubMed] [Google Scholar]
- 220.Albert E, et al. Lipid transfer protein syndrome in a Northern European patient: An unusual case report. Front Med (Lausanne). 2023;10:1049477. 10.3389/fmed.2023.1049477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Chanana V, Kaur KJ, Salunke DM. Purification, identification and preliminary crystallographic characterization of a novel seed protein from Vigna unguiculata. Acta Crystallogr D Biol Crystallogr. 2004;60(Pt 11):2100–3. 10.1107/S0907444904023868 [DOI] [PubMed] [Google Scholar]
- 222.Dugué P, Bel J, Figueredo M. Fenugreek causing a new type of occupational asthma. Presse Med. 1993;22(19):922. [PubMed] [Google Scholar]
- 223.Patil SP, Niphadkar PV, Bapat MM. Allergy to fenugreek (Trigonella foenum graecum). Ann Allergy Asthma Immunol. 1997;78(3):297–300. 10.1016/S1081-1206(10)63185-7 [DOI] [PubMed] [Google Scholar]
- 224.Aurich S, et al. Report of a Case of IgE-Mediated Anaphylaxis to Fenugreek. J Investig Allergol Clin Immunol. 2019;29(1):56–8. 10.18176/jiaci.0328 [DOI] [PubMed] [Google Scholar]
- 225.Joseph NI, et al. Fenugreek Anaphylaxis in a Pediatric Patient. Allergy Rhinol (Providence). 2018;9:2152656718764134. 10.1177/2152656718764134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Ohnuma N, Yamaguchi E, Kawakami Y. Anaphylaxis to curry powder. Allergy. 1998;53(4):452–4. 10.1111/j.1398-9995.1998.tb03924.x [DOI] [PubMed] [Google Scholar]
- 227.Fæste CK, Namork E, Lindvik H. Allergenicity and antigenicity of fenugreek (Trigonella foenum-graecum) proteins in foods. J Allergy Clin Immunol. 2009;123(1):187–94. 10.1016/j.jaci.2008.09.012 [DOI] [PubMed] [Google Scholar]
- 228.Aalberse RC. Structural biology of allergens. J Allergy Clin Immunol. 2000;106(2):228–38. 10.1067/mai.2000.108434 [DOI] [PubMed] [Google Scholar]
- 229.Masilamani M, Commins S, Shreffler W. Determinants of Food Allergy. Immunol Allergy Clin North Am. 2012;32(1):11–33. 10.1016/j.iac.2011.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Barroso da Silva FL, et al. Understanding and Controlling Food Protein Structure and Function in Foods: Perspectives from Experiments and Computer Simulations. Annu Rev Food Sci Technol. 2020;11:365–87. 10.1146/annurev-food-032519-051640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Wu D, et al. Biological and conventional food processing modifications on food proteins: Structure, functionality, and bioactivity. Biotechnol Adv. 2020;40:107491. 10.1016/j.biotechadv.2019.107491 [DOI] [PubMed] [Google Scholar]
- 232.Bhalla PL, Singh MB. Biotechnology-based allergy diagnosis and vaccination. Trends Biotechnol. 2008;26(3):153–61. 10.1016/j.tibtech.2007.11.010 [DOI] [PubMed] [Google Scholar]
- 233.Verhoeckx KCM, et al. Food processing and allergenicity. Food Chem Toxicol. 2015;80:223–40. 10.1016/j.fct.2015.03.005 [DOI] [PubMed] [Google Scholar]
- 234.Sathe SK, Sharma GM. Effects of food processing on food allergens. Mol Nutr Food Res. 2009;53(8):970–8. 10.1002/mnfr.200800194 [DOI] [PubMed] [Google Scholar]
- 235.Koidl L, Gentile SA, Untersmayr E. Allergen Stability in Food Allergy: A Clinician’s Perspective. Curr Allergy Asthma Rep. 2023;23(10):601–12. 10.1007/s11882-023-01107-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Lokya V, et al. Prospects for developing allergen-depleted food crops. Plant Genome. 2023;16(4):e20375. 10.1002/tpg2.20375 [DOI] [PubMed] [Google Scholar]