Abstract
Objective
The study aims to examine maternal care among Hispanic birthing people by primary language and state policy environment.
Data Sources and Study Setting
Pooled data from 2016 to 2020 Pregnancy Risk Assessment Monitoring System surveys from 44 states and two jurisdictions.
Study Design
Using multivariable logistic regression, we calculated adjusted predicted probabilities of maternal care utilization (visit attendance, timeliness, adequacy) and quality (receipt of guideline‐recommended care components). We examined outcomes by primary language (Spanish, English) and two binary measures of state policy environment: (1) expanded Medicaid eligibility to those <133% Federal Poverty Level, (2) waived five‐year waiting period for pregnant immigrants to access Medicaid.
Data Collection/Extraction Methods
Survey responses from 35,779 postpartum individuals with self‐reported Hispanic ethnicity who gave birth during 2016–2020.
Principal Findings
Compared to English‐speaking Hispanic people, Spanish‐speaking individuals reported lower preconception care attendance and worse timeliness and adequacy of prenatal care.
In states without Medicaid expansion and immigrant Medicaid coverage, Hispanic birthing people had, respectively, 2.3 (95% CI:0.6, 3.9) and 3.1 (95% CI:1.6, 4.6) percentage‐point lower postpartum care attendance and 4.2 (95% CI:2.1, 6.3) and 9.2 (95% CI:7.2, 11.2) percentage‐point lower prenatal care quality than people in states with these policies.
In states with these policies, Spanish‐speaking Hispanic people had 3.3 (95% CI:1.3, 5.4) and 3.0 (95% CI:0.9, 5.1) percentage‐point lower prenatal care adequacy, but 1.3 (95% CI:−1.1, 3.6) and 2.7 (95% CI:0.2, 5.1) percentage‐point higher postpartum care quality than English‐speaking Hispanic people. In states without these policies, those same comparisons were 7.3 (95% CI:3.8, 10.8) and 7.9 (95% CI:4.6, 11.1) percentage‐points lower and 9.6 (95% CI:5.5, 13.7) and 5.3 (95% CI:1.8, 8.9) percentage‐points higher.
Conclusions
Perinatal care utilization and quality vary among Hispanic birthing people by primary language and state policy environment. States with Medicaid expansion and immigrant Medicaid coverage had greater equity between Spanish‐speaking and English‐speaking Hispanic people in adequate prenatal care and postpartum care quality among those who gave birth.
Keywords: Hispanic, Latinx, maternal health care, perinatal, postpartum, PRAMS, primary language
What is known on this topic
Hispanic birthing people face elevated risks of poor maternal outcomes compared to non‐Hispanic White people, including preeclampsia, hypertension, and gestational diabetes.
Hispanic adults in the United States access prenatal care at lower rates than non‐Hispanic White people.
Patients with limited English proficiency experience barriers to accessing high quality healthcare services, and frequently report healthcare discrimination.
What this study adds
Spanish‐speaking Hispanic individuals reported significantly lower preconception care utilization, and worse timeliness and adequacy of prenatal care, compared to English‐speaking Hispanic individuals.
States with Medicaid expansion and immigrant Medicaid coverage policies had smaller disparities in perinatal care between Spanish‐ and English‐speaking Hispanic people.
Policy efforts to increase access to and equity in perinatal care among Hispanic people could include changes in Medicaid eligibility based on income and immigration status.
1. INTRODUCTION
There are long‐standing maternal health disparities by race and ethnicity, language, immigration status, and country of origin among people who give birth in the United States. A growing body of research reports important subgroup variations in birth outcomes among Hispanic people, 1 , 2 highlighting the need for increased data disaggregation, especially considering how policies affect Hispanic subgroups differently. The ethnicity “Hispanic” is used throughout this paper to describe a diverse group of people who have Latin American or Spanish roots (e.g., people who identify as Latino/a, Latinx, or Latine).
Overall, Hispanic birthing people face elevated risks of poor maternal outcomes (e.g., preeclampsia, hypertension, gestational diabetes) than non‐Hispanic White people. 3 Hispanic people who give birth also report higher rates of discrimination in healthcare interactions, including childbirth hospitalization. 4 , 5
Hispanic adults in the United States access prenatal care at lower rates than non‐Hispanic White people 6 ; qualitative research describes lack of health insurance, language and cultural barriers, and racism and discrimination within healthcare settings as contributing factors. 6 , 7 While some studies have delineated Hispanic subgroup differences in prenatal care use by country of origin, 8 less is known about differences in utilization and quality of care across the perinatal period based on primary language spoken (English vs. Spanish). Notably, 94% of foreign‐born Hispanic people speak Spanish at home 9 and two‐thirds have limited English proficiency. 10 More than one in three Hispanic immigrants with limited English proficiency report that their ability to access health care has been impeded by language barriers, 10 indicating a need to investigate health disparities based on primary language.
Nearly one‐third of Hispanic people below age 65 are enrolled in Medicaid, an important source of health insurance during the perinatal period. 11 Over four in 10 births in the United States are financed by Medicaid, 12 and 35% of Medicaid‐insured pregnant people identify as Hispanic. 13 Medicaid eligibility varies by state and states' decisions to expand Medicaid under the Affordable Care Act to those <133% of the Federal Poverty Level. Additionally, immigration‐based eligibility rules for Medicaid either require that immigrants undergo a waiting period before they are eligible for Medicaid coverage, or fully exclude them based on their immigration status, including many Hispanic pregnant people who are immigrants. 14 Approximately 50% of births by US immigrants are by Hispanic people. 15 The Personal Responsibility and Work Opportunity Reconciliation Act of 1996 dictates that lawfully residing immigrants are only eligible for Medicaid after a five‐year waiting period. States are permitted to waive this waiting period for pregnant individuals, with 34 states and the District of Columbia having implemented this waiver by 2023. 16 Pregnant immigrants living in states that have not waived this waiting period are left without health insurance coverage during their pregnancy, childbirth, and postpartum period unless they are able to access and afford private coverage.
This study aimed to examine differences in perinatal care utilization and receipt of recommended care components for English‐speaking and Spanish‐speaking Hispanic individuals who gave birth between 2016 and 2020. Further, we examined associations between perinatal care and the state policy environment (Medicaid expansion and immigrant Medicaid coverage policies) to assess whether the policy environment was associated with differences in outcomes based on primary language.
2. METHODS
2.1. Data and study population
This study used pooled data from the Pregnancy Risk Assessment Monitoring System (PRAMS), a cross‐sectional survey of postpartum people from 44 states, the District of Columbia, and New York City. PRAMS surveys are conducted by state and local health departments in collaboration with the Centers for Disease Control and Prevention (CDC), and participants are sampled from birth certificate records and surveyed between 2 and 6 months after childbirth. This study used phase 8 PRAMS data, which surveys individuals with live births from 2016 to 2020 and are linked with birth certificate data. The CDC releases annual PRAMS data from sites that meet a minimum response rate threshold. 17 Data from phase 8 include the year 2020, during which time the COVID‐19 public health emergency affected healthcare utilization and insurance coverage through the Families First Coronavirus Response Act. We analyzed these data to include the experiences of birthing people in 2020, and we conducted sensitivity analyses excluding this year of data.
Respondents who self‐reported their ethnicity as Hispanic on either the birth certificate record or the PRAMS survey and who completed the survey in either English or Spanish were included in this study. Other PRAMS respondents and those who completed the survey in Spanish but did not self‐report as Hispanic were examined separately in Supplemental Tables 1 and 2. Vermont does not release information about respondents' race or ethnicity and were thus excluded.
2.2. Outcome measures
Study outcomes, measured separately during the preconception, prenatal, and postpartum periods, included (1) poor perinatal care utilization and (2) poor perinatal care quality, defined as receiving less than 75% of care components recommended by the American College of Obstetricians and Gynecologists (ACOG). 18
2.2.1. Preconception
The preconception period comprised visits in the 12 months before pregnancy. Poor preconception care utilization was defined as self‐reported “no healthcare visits” during the preconception period. Among those who reported a visit, poor preconception care quality was calculated, as described above, using 12 binary (yes/no), self‐reported preconception care components that were discussed with the individual by a clinician during a visit: folic acid consumption; maintaining a healthy weight; controlling preexisting medical conditions; desire to have children; contraception and pregnancy prevention; health improvement strategies; sexually transmitted infections; smoking; physical and emotional abuse; depression; work environment; and HIV testing (Supplemental Table 3). 19
2.2.2. Prenatal
The prenatal period comprised visits during pregnancy but before childbirth. Poor prenatal care utilization was defined separately as: (1) self‐report of “no prenatal visits” on the PRAMS survey; (2) less than adequate prenatal care as per the Adequacy of Prenatal Care Utilization (APNCU) Index as indicated on the birth certificate record; and (3) self‐reported prenatal care that began after the first trimester on the PRAMS survey. The APNCU combines the timing of prenatal care initiation with the proportion of prenatal care visits received of those expected based on initiation timing and gestational age at birth. 20 We defined less than adequate prenatal care as care that began after the fourth month of pregnancy or receiving under 80% of expected visits based on the APNCU measure. Among those who had prenatal visits, poor prenatal care quality was calculated using 11 binary (yes/no), self‐reported prenatal care components discussed with the individual by a clinician during a visit: counseling on healthy weight gain; medication use; smoking; alcohol consumption; physical and emotional abuse; depression; drug use; HIV testing; breastfeeding; contraception; and vaccinations. 18
2.2.3. Postpartum
In the PRAMS questionnaire, postpartum visits were described as “the regular checkup a woman has about 4‐6 weeks after she gives birth.” However, respondents could have interpreted postpartum visits to include those that occurred up to the time of the PRAMS survey (average 4 months after childbirth). Poor postpartum care utilization was defined as self‐reported “no postpartum visits.” Among those who reported a visit, poor postpartum care quality was calculated using seven binary (yes/no), self‐reported postpartum care components discussed with the individual by a clinician during a visit: folic acid consumption; depression; contraception; smoking; physical and emotional abuse; birth spacing; and healthy eating and exercise. 21
2.3. Covariate measures
We examined sociodemographic characteristics by primary language (survey completion in English or Spanish), including insurance at childbirth (private, Medicaid, uninsured) as reported on the birth certificate, and self‐reported race (Asian, Black, Indigenous, White, other non‐White, multiple, or unknown), rural residence (micropolitan or noncore counties based on the National Center for Health Statistics urban‐rural classification scheme, as provided in PRAMS), 22 Census region (Northeast, Midwest, South, West), age (<20, 20–24, 25–34, 35+), education (<high school, high school graduate, >high school), marital status (married or not), parity (one or more previous childbirths or not), and pregnancy intention (unintended or not). Clinical characteristics included self‐reported pre‐pregnancy physical abuse, depression, diabetes, high blood pressure, obesity, and smoking.
2.4. Policy environment measures
In addition to examination by language, study outcomes were examined by two separate binary measures of state policy environment (for both Spanish‐ and English‐speaking Hispanic individuals): (1) Medicaid expansion status and (2) immigrant Medicaid coverage policies by state and year. Medicaid expansion status (yes/no) and timing were assessed using data from the Kaiser Family Foundation. 23 States with Medicaid coverage for lawfully residing pregnant immigrants that had waived the five‐year waiting period were classified as having immigrant Medicaid coverage. States without waivers (e.g., Medicaid coverage only for lawfully residing noncitizens after the five‐year waiting period and no coverage for undocumented and Deferred Action for Childhood Arrivals [DACA]‐eligible immigrants) were classified as having no immigrant Medicaid coverage. 24 , 25 States that had policy changes during the study period were coded as “no” in the years without the policy and “yes” in the years with the policy.
Citizenship, immigration documentation status, and country of origin are not available in PRAMS. Understanding the association between immigrant Medicaid coverage policies and poor perinatal care among Hispanic individuals, including both US citizens with noncitizens, is important, so we conducted a secondary analysis, estimating “likely” citizenship status using available data in PRAMS. A growing body of literature reports spillover effects for US citizens, which refers to how policies targeted at noncitizens can impact US citizens and their health. 26 , 27 Thus, we conducted stratified analysis using an estimated proxy measure of likely US citizenship status using previously published methods. 28 , 29 , 30 Those reporting Hispanic ethnicity, Spanish language, and less than a high school degree were considered likely noncitizens, while other Hispanic‐identifying respondents were considered likely US citizens. This is not a direct measure of citizenship, and has important limitations, but provides some evidence of potential differential effects among Hispanic birthing people, as a secondary analysis.
2.5. Statistical analysis
We estimated survey‐weighted proportions to describe distributional differences in sociodemographic and clinical characteristics between English‐speaking and Spanish‐speaking Hispanic postpartum individuals, testing differences with Rao–Scott chi‐square tests. Using multivariable logistic regression, we calculated adjusted predicted probabilities and percentage‐point differences with 95% confidence intervals (CIs) for study outcomes, controlling for sociodemographic and clinical factors described above. Health insurance type was not included as a covariate in adjusted analyses as insurance is likely on the causal pathway between identity categories (ethnicity, language) and perinatal care utilization.
We examined differences in outcomes for English‐speaking and Spanish‐speaking Hispanic individuals overall, by Medicaid expansion status, and by immigrant Medicaid coverage status. As a secondary analysis, differences in outcomes by immigrant Medicaid coverage status were additionally assessed by a proxy estimating likely citizen and noncitizen status. Assessment of differences by state policy environment involved models with interaction terms.
All sample sizes presented are unweighted, while percentages and analyses used PRAMS survey weights, which account for variation in sampling rates, stratification schemes, and nonresponse across study sites. Significance was assessed by 95% CIs excluding the null and defined as p < 0.05 using two‐sided hypothesis tests. All analyses were conducted using Stata, version 18 (StataCorp LLC).
This study was not determined as human subjects research by the Institutional Review Board of the University of Minnesota.
3. RESULTS
Table 1 provides weighted descriptive statistics of the analytic sample by primary language. The sample contained 35,779 Hispanic postpartum respondents; 57.7% were English‐speaking and 42.3% were Spanish‐speaking. Compared to Spanish‐speaking Hispanic individuals, English‐speaking Hispanic individuals were more likely to have private health insurance (41.2% vs. 14.3%), live in rural areas (9.7% vs. 7.3%), the Midwest (19.1% vs. 12.2%) or the West (22.3% vs. 10.6%), and have more than a high school education (52.3% vs. 19.9%). Spanish‐speaking individuals were more likely to have Medicaid (69.0% vs. 55.7%) or be uninsured (16.8% vs. 3.1%) at childbirth, live in the South (46.0% vs. 31.8%) or the Northeast (31.2% vs. 26.9%), and have more than one previous live birth (72.7% vs. 60.7%). English‐speaking Hispanic individuals reported significantly higher rates of unintended pregnancy (50.5% vs. 41.2%) and pre‐pregnancy obesity (35.3% vs. 28.0%), depression (12.9% vs. 4.7%), and smoking (12.0% vs. 3.3%) than their Spanish‐speaking Hispanic counterparts.
TABLE 1.
Characteristics of postpartum Hispanic individuals by language (n = 35,779).
| Characteristics | English speaking (n = 21,742) 57.7% | Spanish speaking (n = 14,037) 42.3% | p‐value |
|---|---|---|---|
| Insurance at childbirth | <0.001 | ||
| Private | 41.2 | 14.3 | |
| Medicaid | 55.7 | 69.0 | |
| Uninsured | 3.1 | 16.8 | |
| Racial identification | <0.001 | ||
| Asian | 0.7 | 0.3 | |
| Black | 5.6 | 1.9 | |
| Indigenous | 0.9 | 0.3 | |
| White | 63.2 | 54.9 | |
| Other—non‐White | 21.6 | 37.4 | |
| Multiple | 4.4 | 1.5 | |
| Unknown | 3.7 | 3.7 | |
| Rural residence | 9.7 | 7.3 | <0.001 |
| Region | <0.001 | ||
| Northeast | 26.9 | 31.2 | |
| Midwest | 19.1 | 12.2 | |
| South | 31.8 | 46.0 | |
| West | 22.3 | 10.6 | |
| Age | <0.001 | ||
| <20 | 8.3 | 5.1 | |
| 20–24 | 26.7 | 19.1 | |
| 25–34 | 50.7 | 53.5 | |
| 35+ | 14.3 | 22.3 | |
| Education | <0.001 | ||
| Less than high school graduate | 15.5 | 47.9 | |
| High school graduate | 31.7 | 30.4 | |
| More than high school | 52.3 | 19.9 | |
| Unknown | 0.6 | 1.8 | |
| Married | 48.7 | 46.8 | 0.034 |
| Multiparous | 60.7 | 72.7 | <0.001 |
| Unintended pregnancy | 50.5 | 41.2 | <0.001 |
| Pre‐pregnancy conditions | |||
| Abuse | 4.0 | 3.0 | 0.003 |
| Depression | 12.9 | 4.7 | <0.001 |
| Diabetes | 3.6 | 3.3 | 0.504 |
| High blood pressure | 4.6 | 3.9 | 0.047 |
| Obesity | 35.3 | 28.0 | <0.001 |
| Smoking | 12.0 | 3.3 | <0.001 |
Note: Bolded values indicate statistical significance at p < 0.05.
Source: Authors' analysis of data from the Pregnancy Risk Assessment Monitoring System (PRAMS), 2016–20. N are unweighted, percentages use PRAMS survey weights, which account for variation in sampling rates, stratification schemes, and nonresponse across sites. p‐values are Rao–Scott chi‐square.
Table 2 shows adjusted predicted probabilities of poor perinatal care utilization and receipt of recommended care components, comparing English‐speaking to Spanish‐speaking Hispanic individuals. Preconception care utilization was low for both groups, with 40.5% of English‐speaking Hispanic and 52.7% of Spanish‐speaking Hispanic individuals reporting no healthcare visits preconception (difference: p < 0.001). Spanish‐speaking Hispanic individuals reported significantly worse prenatal care measures than their English‐speaking Hispanic counterparts, with 14.1% and 10.1% reporting prenatal care that began after the first trimester, and 35.0% and 30.1% reporting receiving less than adequate prenatal care, respectively (p < 0.001 for both). English‐speaking Hispanic individuals were significantly more likely to lack recommended components of preconception (78.4% vs. 73.1%) and postpartum care (58.3% vs. 53.9%) than their Spanish‐speaking Hispanic counterparts.
TABLE 2.
Perinatal care among postpartum Hispanic individuals by language (n = 35,779).
| Perinatal care utilization and quality | English speaking (n = 21,742) | Spanish speaking (n = 14,037) | p‐value (language difference) | ||
|---|---|---|---|---|---|
| Weighted % | Adjusted predicted probability (95% CI) a | Weighted % | Adjusted predicted probability (95% CI) a | ||
| Poor care utilization | |||||
| No preconception visits (12 mo. before pregnancy) | 38.3 | 40.5 (39.2,41.7) | 55.9 | 52.7 (51.3,54.2) | <0.001 |
| No prenatal care visits | 0.5 | 0.5 (0.4,0.7) | 0.7 | 0.6 (0.4,0.8) | 0.738 |
| Prenatal care began after the first trimester | 9.3 | 10.1 (9.3,11.0) | 15.8 | 14.1 (13.1,15.1) | <0.001 |
| Received less than adequate prenatal care (APNCU) | 29.4 | 30.1 (28.9,31.3) | 36.1 | 35.0 (33.6,36.4) | <0.001 |
| No postpartum care visits | 13.0 | 14.0 (13.0,14.9) | 16.7 | 15.2 (14.2,16.2) | 0.115 |
| Poor care quality (received <75% of recommended care components during visit(s)) during: | |||||
| Preconception visits b | 79.7 | 78.4 (77.1,79.8) | 70.4 | 73.1 (71.1,75.0) | <0.001 |
| Prenatal visits c | 29.7 | 30.5 (29.2,31.7) | 30.7 | 29.7 (28.4,31.0) | 0.454 |
| Postpartum visits d | 58.8 | 58.3 (56.9,59.6) | 53.2 | 53.9 (52.3,55.5) | <0.001 |
Note: Bolded values indicate statistical significance at p < 0.05.
Source: Authors' analysis of data from the Pregnancy Risk Assessment Monitoring System (PRAMS), 2016–20. NOTES: APNCU: Adequacy of Prenatal Care Utilization (Kotelchuck Index), CI: confidence interval. N are unweighted, percentages use PRAMS survey weights, which account for variation in sampling rates, stratification schemes, and nonresponse across sites. p‐values are from multivariable logistic regression models comparing adjusted predicted probabilities of each outcome between English‐speaking and Spanish‐speaking Hispanic reporting individuals.
Adjusted for rurality, region, race, age, education, marital status, parity, pregnancy intention, and pre‐pregnancy abuse, depression, diabetes, high blood pressure, obesity, and smoking.
Recommended preconception care components (n = 12) include counseling on folic acid consumption, maintaining a healthy weight, controlling preexisting medical conditions, desire to have children, pregnancy prevention, health improvement strategies, sexually transmitted infections, smoking, physical and emotional abuse screening, depression screening, work environment, and HIV testing.
Recommended prenatal care components (n = 11) include counseling on healthy weight gain, medication, smoking, alcohol consumption, physical and emotional abuse screening, depression screening, drug use, HIV testing, breastfeeding counseling, postpartum contraceptive counseling, and vaccinations.
Recommended postpartum care components (n = 7) include counseling on folic acid consumption, depression screening, contraceptive counseling, smoking, physical and emotional abuse screening, birth spacing counseling, and discussions about healthy eating and exercise.
Associations between the state policy environment (Medicaid expansion status and immigrant Medicaid coverage policies) and perinatal care outcomes for Hispanic individuals are presented in Figure 1 and Supplemental Tables 4 and 5. When comparing Hispanic individuals overall (ignoring language) by state Medicaid expansion status, Hispanic individuals in non‐Medicaid expansion states were significantly more likely to have no postpartum care visits and lack recommended perinatal care components than Hispanic individuals in expansion states (all p < 0.05). When comparing Spanish‐ and English‐speaking Hispanic people within states with and without Medicaid expansion, differences in perinatal measures for English‐speaking versus Spanish‐speaking Hispanic individuals were statistically significant and similar in size in both expansion and non‐expansion states for poor preconception and prenatal care utilization measures. Rates of no preconception visits were 12.9 (95% CI: 10.8, 15.0) and 11.4‐percentage points (95% CI: 7.7, 15.1) higher, late prenatal care initiation 3.6 (95% CI: 2.1, 5.0) and 4.6‐percentage points (95% CI: 2.3, 7.0) higher, and poor preconception care quality 5.3 (95% CI: −8.0, −2.7) and 5.3‐percentage points (95% CI: −9.8, −0.8) lower for Spanish‐speaking Hispanic compared to English‐speaking Hispanic individuals in expansion and non‐expansion states, respectively.
FIGURE 1.
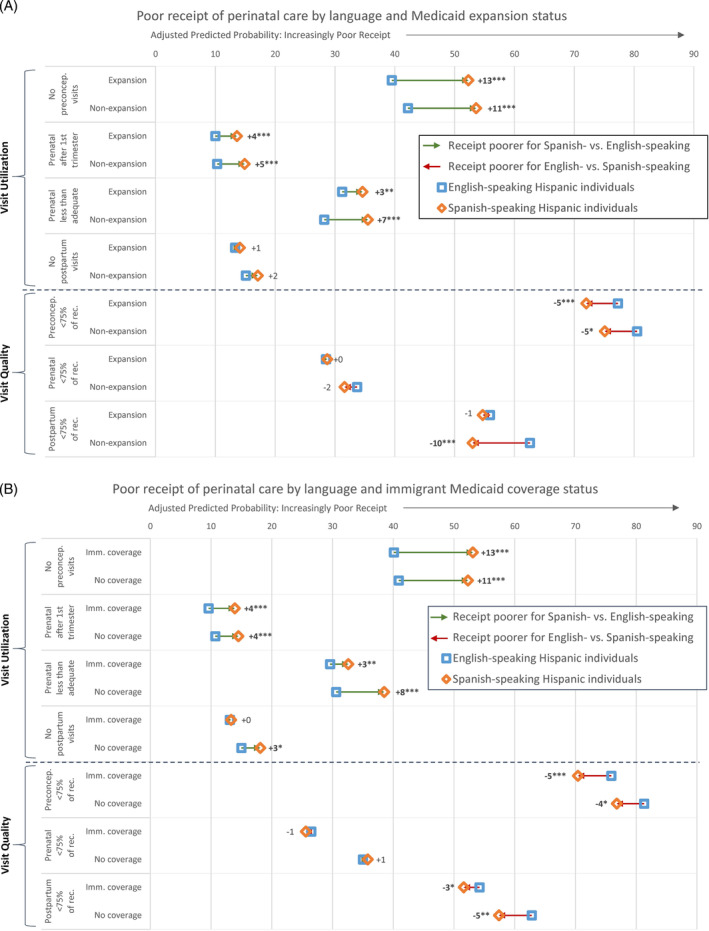
Probability of poor perinatal care utilization and quality among postpartum Hispanic individuals by primary language and by (A) Medicaid expansion status and (B) immigrant Medicaid coverage status. Source: Authors' analysis of data from the Pregnancy Risk Assessment Monitoring System (PRAMS), 2016–20. N are unweighted, percentages use PRAMS survey weights, which account for variation in sampling rates, stratification schemes, and nonresponse across sites. Data are adjusted for rurality, region, race, age, education, marital status, parity, pregnancy intention, and pre‐pregnancy abuse, depression, diabetes, high blood pressure, obesity, and smoking. Medicaid expansion states with PRAMS data available include Alaska, Arkansas, Arizona, Colorado, Connecticut, District of Columbia, Delaware, Hawaii, Iowa, Illinois, Indiana, Kentucky, Louisiana (2017–20), Massachusetts, Maryland, Maine (2019–20), Michigan, Minnesota, Montana, North Dakota, New Hampshire, New Jersey, New Mexico, New York, Oregon, Pennsylvania, Rhode Island, Utah (2020). States with PRAMS data available that did not expand Medicaid include Alabama, Florida, Georgia, Kansas, Louisiana (2016), Maine (2016–18), Missouri, Mississippi, North Carolina, Nebraska, Oklahoma, South Dakota, Tennessee, Texas, Utah (2016–19). States with immigrant Medicaid coverage (coverage for lawfully residing immigrants without the 5‐year waiting period) with PRAMS data available include Arkansas (2018–20), Colorado, Connecticut, District of Columbia, Delaware, Hawaii, Maine, Maryland, Massachusetts, Minnesota, North Carolina, Nebraska, New Jersey, New Mexico, New York, Oregon (2018–20), Pennsylvania, Virginia, Washington, Wisconsin, West Virginia, Wyoming. States with no immigrant Medicaid coverage with PRAMS data available include Alaska, Alabama, Arkansas (2016), Arizona, Florida, Georgia, Iowa, Illinois, Indiana, Kansas, Kentucky, Louisiana, Michigan, Missouri, Mississippi, Montana, North Dakota, New Hampshire, Oklahoma, Rhode Island, South Dakota, Tennessee, Texas, Utah. p‐values: *p < 0.05, **p < 0.01, ***p < 0.001.
Medicaid expansion was not associated with reduced inequities between Spanish‐ and English‐speaking Hispanic individuals across all measures of poor perinatal care utilization and receipt of recommended care components. However, there was a reduction in the differences between Spanish‐ and English‐speaking Hispanic people in receiving less than adequate prenatal care and receipt of recommended postpartum care components in expansion states. In non‐expansion states, English‐speaking Hispanic individuals had a 7.3‐percentage point (95% CI: 3.8, 10.8) lower prevalence of less than adequate prenatal care than their Spanish‐speaking Hispanic counterparts, while this difference was 3.3‐percentage points (95% CI: 1.3, 5.4) lower in expansion states. In non‐expansion states, Spanish‐speaking Hispanic individuals had a 9.6‐percentage point (95% CI: −13.7, −5.5) lower prevalence of poor postpartum care quality than their English‐speaking Hispanic counterparts, while this language difference was not significant in expansion states.
When comparing Hispanic individuals overall (ignoring language) by state immigrant Medicaid coverage policies, Hispanic individuals living in states without immigrant Medicaid coverage were significantly more likely to have less than adequate prenatal care, no postpartum care visits, and lack recommended perinatal care components than their Hispanic counterparts in states with immigrant Medicaid coverage (all p < 0.05). When adding the additional language comparison within states with and without immigrant Medicaid coverage policies, differences in perinatal measures for English‐speaking versus Spanish‐speaking Hispanic individuals were significant and similar in both immigrant Medicaid coverage and noncoverage states, with some exceptions. Differences in less than adequate prenatal care between English‐ and Spanish‐speaking Hispanic individuals were less pronounced in states with immigrant Medicaid coverage, with Spanish‐speaking Hispanic individuals 3.0‐percentage points (95% CI: 0.9, 5.1) higher than their English‐speaking Hispanic counterparts. In comparison, for those in states with no immigrant Medicaid coverage, Spanish‐speaking Hispanic individuals were 7.9‐percentage points (95% CI: 4.6, 11.1) more likely than English‐speaking Hispanic individuals to receive less than adequate prenatal care. Differences in outcomes by primary language were only significantly different for no postpartum care visits in states with no immigrant Medicaid coverage; Spanish‐speaking Hispanic individuals were 3.1‐percentage points (95% CI: 0.6, 5.6) more likely than English‐speaking Hispanic individuals to report no visit.
Table 3 and Supplemental Table 6 show results from a secondary analysis, using an estimated proxy for likely citizenship status. Results indicate adjusted predicted probabilities of poor perinatal care utilization and receipt of recommended care components among Hispanic birthing people by likely citizenship status between states with and without immigrant Medicaid coverage. Likely noncitizen Hispanic individuals had higher prevalence of no preconception visits regardless of state immigrant Medicaid coverage (12.4‐percentage points higher, 95% CI: 8.8, 15.9) than likely citizen Hispanic individuals, as well as poorer prenatal care measures (late prenatal care initiation: 5.8‐percentage points higher, 95% CI: 3.3, 8.3; less than adequate prenatal care: 4.9‐percentage points higher, 95% CI: 1.5, 8.3). Among likely noncitizen Hispanic individuals, those in states without immigrant Medicaid coverage were more likely to have late prenatal care initiation (3.3‐percentage points higher, 95% CI: 0.2, 6.3) and less than adequate prenatal care (9.0‐percentage points higher, 95% CI: 4.8, 13.1) than those with immigrant Medicaid coverage, while immigrant Medicaid coverage was not associated with significant differences for these measures among likely citizen Hispanic individuals. However, Hispanic respondents in states without immigrant Medicaid coverage had significantly higher prevalence of no postpartum care visits than those with immigrant Medicaid coverage for both likely noncitizens (5.4‐percentage points higher, 95% CI: 2.6, 8.3) and citizens (2.1‐percentage points higher, 95% CI: 0.4, 3.8). Among those who attended visits, Hispanic individuals in states without immigrant Medicaid coverage, regardless of likely citizenship status, were 5.9 to 9.4‐percentage points more likely to lack recommended perinatal care components than Hispanic individuals living in states with immigrant Medicaid coverage.
TABLE 3.
Probability of perinatal care among postpartum Hispanic individuals by an estimated proxy of likely citizenship and immigrant Medicaid coverage status.
| Perinatal care utilization and quality | Adjusted predicted probabilities (95% CI) a | |||||
|---|---|---|---|---|---|---|
| Likely noncitizen b (n = 7003) | Likely citizen b (n = 28,776) | |||||
| No immigrant Medicaid coverage c (n = 2405) | Immigrant Medicaid coverage d (n = 4598) | Adjusted difference (95% CI) a | No immigrant Medicaid coverage c (n = 10,155) | Immigrant Medicaid coverage d (n = 18,621) | Adjusted difference (95% CI) a | |
| Poor care utilization | ||||||
| No preconception visits | 55.8 (51.6,60.0) | 55.4 (52.2,58.5) | 0.5 (−3.8, 4.7) | 42.8 (41.0,44.6) | 43.6 (42.1,44.6) | ‐0.8 (−3.0,1.5) |
| No prenatal care visits | 0.7 (0.3,1.1) | 0.4 (0.1,0.7) | 0.3 (−0.3,0.8) | 0.8 (0.4,1.2) | 0.5 (0.3,0.6) | 0.3 (−0.1,0.8) |
| Prenatal care began after first trimester* | 18.2 (15.1,21.4) | 15.0 (12.9,17.1) | 3.3 (0.2,6.3) * | 10.5 (9.3,11.6) | 10.6 (9.7,11.6) | −0.2 (−1.6,1.3) |
| Received less than adequate prenatal care (APNCU)** | 41.5 (37.3,45.7) | 32.5 (29.6,35.4) | 9.0 (4.8,13.1) *** | 31.7 (30.0,33.5) | 30.7 (29.3,32.0) | 1.1 (−1.1,3.2) |
| No postpartum care visits* | 17.6 (14.7,20.5) | 12.2 (10.5,13.8) | 5.4 (2.6,8.3) *** | 15.8 (14.4,17.3) | 13.7 (12.6,14.7) | 2.1 (0.4,3.8) * |
| Poor care quality (received <75% of recommended care components during visit(s)) | ||||||
| Preconception visits | 76.6 (71.4,81.9) | 70.1 (65.5,74.8) | 6.5 (1.0,11.9) * | 80.4 (78.5,82.3) | 74.4 (72.7,76.1) | 5.9 (3.4,8.5) *** |
| Prenatal visits | 34.3 (30.1,38.5) | 25.8 (23.0,28.6) | 8.5 (4.5,12.6) *** | 35.6 (33.7,37.4) | 26.2 (24.9,27.5) | 9.4 (7.2,11.6) *** |
| Postpartum visit | 60.1 (55.5,64.7) | 53.6 (50.0,57.1) | 6.6 (1.9,11.2) ** | 60.9 (59.0,62.9) | 52.9 (51.4,54.4) | 8.0 (5.6,10.5) *** |
Note: Bolded values indicate statistical significance at p < 0.05.
Source: Authors' analysis of data from the Pregnancy Risk Assessment Monitoring System (PRAMS), 2016–20. APNCU: Adequacy of Prenatal Care Utilization (Kotelchuck Index), CI: confidence interval. N are unweighted, percentages use PRAMS survey weights, which account for variation in sampling rates, stratification schemes, and nonresponse across sites. Asterisks next to perinatal care utilization and quality labels indicate significant multiplicative interaction between immigrant Medicaid coverage status and likely citizenship status.
Adjusted for rurality, region, race, age, education, marital status, parity, pregnancy intention, and pre‐pregnancy abuse, depression, diabetes, high blood pressure, obesity, and smoking.
Likely citizenship was created by examining reported Hispanic ethnicity, language, and education. Those reporting Hispanic ethnicity, Spanish language, and less than a high school degree were considered likely noncitizens.
States with no immigrant Medicaid coverage with PRAMS data available include Alaska, Alabama, Arkansas (2016), Arizona, Florida, Georgia, Iowa, Illinois, Indiana, Kansas, Kentucky, Louisiana, Michigan, Missouri, Mississippi, Montana, North Dakota, New Hampshire, Oklahoma, Rhode Island, South Dakota, Tennessee, Texas, Utah.
States with immigrant Medicaid coverage (coverage for lawfully residing immigrants without the 5‐year waiting period) with PRAMS data available include Arkansas (2018–20), Colorado, Connecticut, District of Columbia, Delaware, Hawaii, Maine, Maryland, Massachusetts, Minnesota, North Carolina, Nebraska, New Jersey, New Mexico, New York, Oregon (2018–20), Pennsylvania, Virginia, Washington, Wisconsin, West Virginia, Wyoming.
p < 0.05;
p < 0.01;
p < 0.001.
4. DISCUSSION
This study investigated perinatal care utilization and quality among Hispanic‐identifying postpartum individuals with childbirths between 2016 and 2020. Our findings revealed significant disparities in utilization and quality of care by primary language (English vs. Spanish) and state policy environment in the periods before, during, and after pregnancy. Spanish‐speaking Hispanic individuals reported significantly lower care utilization in the preconception period, and worse timeliness and adequacy of prenatal care, compared to their English‐speaking Hispanic counterparts. Conversely, English‐speaking Hispanic individuals were more likely to receive lower quality preconception and postpartum care, as defined by receiving less than 75% of guideline‐recommended care components.
Lack of Medicaid expansion and immigrant Medicaid coverage policies were associated with lower healthcare utilization and poorer quality across several measures. Hispanic people living in states without Medicaid expansion and immigrant Medicaid coverage reported lower postpartum care utilization and poorer quality of care across the perinatal period than Hispanic people living in states with these policies, regardless of primary language spoken. Associations were also identified between primary language and state policy environment; Medicaid expansion and immigrant Medicaid coverage policies were associated with greater equity between Spanish‐ and English‐speaking Hispanic people across some, but not all, measures. Specifically, differences in prenatal care adequacy and postpartum care quality between Spanish‐ and English‐speaking Hispanic individuals were attenuated in states with Medicaid expansion or immigrant Medicaid coverage. Further, in states with immigrant Medicaid coverage, differences in postpartum care utilization between Spanish‐ and English‐speaking Hispanic people were narrowed.
Finally, our secondary analysis found that the most pronounced associations between a lack of immigrant Medicaid coverage and lower prenatal and postpartum care utilization were experienced by those estimated to be likely noncitizens. However, poorer perinatal care quality was detected for Hispanic people birthing in states without immigrant Medicaid coverage regardless of likely citizenship status.
These findings of differences in perinatal care utilization among Hispanic individuals by primary language may signal a broader lack of inclusivity for non‐English speakers within healthcare systems. Patients with limited English proficiency face barriers to accessing high quality healthcare services, including difficulty scheduling appointments, challenges understanding clinicians and medical conditions, leaving visits with unaddressed concerns, and experiencing discrimination. 31 , 32 Prior policy efforts to address language inclusion have fallen short, 33 and the current findings highlight the ongoing structural healthcare system barriers that affect care before, during, and after childbirth for Hispanic patients. Language justice is an emerging framework that builds upon language inclusion concepts and language access by challenging the assumption that languages other than English are inherent barriers in the healthcare system. 34 Language justice, which is defined as acceptance and respect of a person's right to communicate and be understood in their desired language, 35 argues that language differences should be considered a strength as it can be a key resource in diminishing health inequities. Additionally, this framework urges providers to advocate for best practices that allow patients to communicate and be understood in their preferred language. 34
This study found that Spanish‐speaking Hispanic individuals had poorer perinatal care utilization outcomes than their English‐speaking Hispanic counterparts but, when they attended visits, received more recommended components care. This contrary finding is consistent with previous studies showing that persons with multiple intersecting disadvantaged identities (e.g., racially and ethnically minoritized persons, Medicaid insured, rural residents) were more likely to receive postpartum screenings for smoking, abuse, birth spacing counseling, and nutrition education than those with more advantaged identities. 36 This insight may indicate clinician and practice biases of who is considered “at risk.” Universal screening protocols could potentially address these differences in care quality by primary language.
There is substantial overlap between primary language and immigration for Hispanic individuals, 15 suggesting that some of the challenges Spanish‐speaking Hispanic people face are related to their immigration status. Restrictions to public benefits, including health insurance, based on immigration status can affect access to healthcare services and health outcomes for immigrants. 37 And, conversely, policies that drop immigration‐based restrictions may improve equity, as indicated by this study's findings of smaller disparities in perinatal care by language in states where Medicaid coverage policy is more inclusive of immigrants.
The finding that Spanish‐speaking Hispanic individuals reported worse perinatal care utilization than their English‐speaking Hispanic counterparts may reflect a lack of access to health insurance coverage. Spanish‐speaking Hispanic individuals have the highest uninsurance rates and face barriers to continuous insurance access before, during, and after childbirth. 38 , 39 Medicaid expansion is one policy lever that may mitigate some of these disparities. 40 We found that Hispanic individuals in Medicaid expansion states had better postpartum visit attendance and quality of perinatal care, as well as reduced differences in prenatal care adequacy by primary language. However, our findings also indicated that Medicaid expansion alone is not sufficient, as there was no difference between expansion and non‐expansion states in preconception care utilization and prenatal care adequacy.
Another potential policy lever is changing Medicaid eligibility policies for immigrant populations. In this study, more inclusive immigrant Medicaid coverage policies were associated with more adequate prenatal care, better postpartum visit attendance, improved perinatal care quality, and reductions in disparities by language for care access during the prenatal and postpartum periods. The lack of association in the preconception period is intuitive as most pregnancy‐related Medicaid eligibility excludes the time before pregnancy, regardless of a state's policies on immigrant eligibility.
In our secondary analysis using the estimated likely citizenship measure, we found that Hispanic people who are likely noncitizens and living in states without immigrant Medicaid coverage had worse prenatal care initiation, adequacy, and worse postpartum visit attendance compared with those living in states that had immigrant‐inclusive Medicaid eligibility policies. This suggests the potential equity‐promoting effects of Medicaid policies that are inclusive of immigrants. Yet, perinatal care quality was worse for Hispanic individuals in states without immigrant Medicaid coverage regardless of their likely citizenship status. The persistent disparities between Spanish‐ and English‐speaking Hispanic individuals in receipt of recommended perinatal care components may be explained by spillover effects from immigration policies, which can be felt by Hispanic individuals facing discrimination despite English language proficiency or citizenship. 27 , 41
Evidence from this analysis indicates that policies designed to improve access to and quality of perinatal care for Hispanic individuals who give birth must attend to potential consequences of policy features related to language, immigration or citizenship status, and to structures within healthcare systems that may reinforce these policy fissures. Medicaid policy may hold particular promise for narrowing disparities in access by language through broader inclusion of noncitizens, and universal screenings that may improve equity in the quality of perinatal care Hispanic individuals receive.
There are several limitations that should be considered in this study. First, PRAMS surveys allow respondents to identify as “Hispanic” but do not include Latina, Latinx, or Latine options or more specific subcategories of Hispanic identity (e.g. Puerto Rican, Mexican, Central American, Cuban, South American, Spanish). We conducted sensitivity analyses comparing Spanish‐speaking respondents by “Hispanic” identification, and results were generally unchanged (Supplemental Table 2), but we acknowledge the complexity of ethnic identity; these data also do not distinguish among “Hispanic” people from different countries of origin. Second, PRAMS surveys did not contain information on citizenship, immigration, year of arrival, or country of origin, which limited this study's ability to determine immigration status. Using previously published methods to estimate a proxy for likely citizenship, we conducted secondary analyses to try to understand perinatal care patterns among Hispanic birthing people along dimensions correlated with citizenship status, even though we could not measure and assess this directly. Third, there are differences across states/municipalities in how different PRAMS survey languages are offered, which has the potential to bias results that account for state policy environments. Fourth, sample sizes were limited by available PRAMS data, and response rates vary across sites, though all achieve minimum standards for inclusion. Fifth, study data includes births from the year 2020, during which time the COVID‐19 public health emergency may have affected healthcare utilization and insurance coverage. However, in sensitivity analyses excluding 2020, results were substantively unchanged. Sixth, the PRAMS questionnaire provides wording on a specific time frame for a postpartum visit (4–6 weeks), but respondents could have understood postpartum visits to include those that occurred up to the time of the PRAMS survey. This potential discrepancy could lead to inconsistent interpretation by respondents, and we were not able to account for differences in the timing of postpartum visits, visits that may have occurred after completion of the PRAMS survey, or visit during which recommended care components were received but the respondent did not deem the visit to fit within the PRAMS definition. Finally, while this study's data include 44 states, DC, and New York City, this sample does not represent all births. States like California and Nevada, with substantial Hispanic populations, are not included, thus affecting the generalizability of these results.
5. CONCLUSIONS
Spanish‐speaking Hispanic individuals reported lower rates of perinatal care utilization than did their English‐speaking Hispanic counterparts. However, for those who attended visits, Spanish‐speaking Hispanic individuals received more recommended components of perinatal care. The state policy environment may play a role in improving access to perinatal care and could help attenuate differences in care by language based on the target outcome. However, reducing disparities in care access and quality across the entire perinatal period for Hispanic individuals may require more targeted interventions beyond Medicaid expansion and immigrant Medicaid coverage, such as universal screening policies. This study can help inform the creation of more effective perinatal healthcare programs and policies to reduce disparities and improve the health of Hispanic birthing people.
Supporting information
Data S1. Supporting information.
ACKNOWLEDGMENTS
Support for this research was provided by the Robert Wood Johnson Foundation's Policies for Action (P4A) program. The information, conclusions, and opinions expressed in this paper are those of the authors and no endorsement by the funder is intended or should be inferred.
The authors would like to thank the participants of the Pregnancy Risk Assessment Monitoring System (PRAMS) study and the PRAMS working group at the US Centers for Disease Control and Prevention (CDC) for their time and for providing the data used in this analysis. The authors gratefully acknowledge Dr. Lindsay K. Admon for collaboration and Dr. Maria W. Steenland for her input on early ideas for the study question and design used in this manuscript.
Interrante JD, Pando C, Fritz AH, Kozhimannil KB. Perinatal care among Hispanic birthing people: Differences by primary language and state policy environment. Health Serv Res. 2024;59(5):e14339. doi: 10.1111/1475-6773.14339
REFERENCES
- 1. DeSisto CL, McDonald JA. Variation in birth outcomes by Mother's country of birth among Hispanic women in the United States, 2013. Public Health Rep. 2018;133(3):318‐328. doi: 10.1177/0033354918765444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Montoya‐Williams D, Williamson VG, Cardel M, Fuentes‐Afflick E, Maldonado‐Molina M, Thompson L. The Hispanic/Latinx perinatal paradox in the United States: a scoping review and recommendations to guide future research. J Immigr Minor Health. 2021;23(5):1078‐1091. doi: 10.1007/s10903-020-01117-z [DOI] [PubMed] [Google Scholar]
- 3. Richardson DM, Andrea SB, Ziring A, Robinson C, Messer LC. Pregnancy outcomes and documentation status among Latina women: a systematic review. Health Equity. 2020;4(1):158‐182. doi: 10.1089/heq.2019.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Janevic T, Piverger N, Afzal O, Howell EA. “Just because you have ears Doesn't mean you can hear”—perception of racial‐ethnic discrimination during childbirth. Ethn Dis. 2020;30(4):533‐542. doi: 10.18865/ed.30.4.533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McLemore MR, Altman MR, Cooper N, Williams S, Rand L, Franck L. Health care experiences of pregnant, birthing and postnatal women of color at risk for preterm birth. Soc Sci Med. 2018;201:127‐135. doi: 10.1016/j.socscimed.2018.02.013 [DOI] [PubMed] [Google Scholar]
- 6. Escarce JJ, Kapur K. Access to and quality of health care. In: Tienda M, Mitchell F, eds. Hispanics and the Future of America. National Academies Press (US); 2006. https://www.ncbi.nlm.nih.gov/books/NBK19910/ Accessed May 15, 2023. [PubMed] [Google Scholar]
- 7. Fryer K, Lewis G, Munoz C, Stuebe AM. Identifying barriers and facilitators to prenatal Care for Spanish‐Speaking Women. N C Med J. 2021;82(1):7‐13. doi: 10.18043/ncm.82.1.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. U.S. Department of Health and Human Services Office of Minority Health . Infant Mortality and Hispanic Americans. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=68. Published July 9, 2021. Accessed May 17, 2023
- 9. Funk C, Hugo LM. Hispanic Americans' Trust in and Engagement with Science. Pew Research Center; 2022. https://www.pewresearch.org/science/?p=3596. Accessed June 11, 2023. [Google Scholar]
- 10. Schumacher S, Hamel L, Artiga S, et al. Most Hispanic Immigrants Say Their Lives Are Better In The U.S. But Face Financial And Health Care Challenges: The 2023 KFF/LA Times Survey of Immigrants. KFF January 2024. https://www.kff.org/racial-equity-and-health-policy/poll-finding/most-hispanic-immigrants-say-lives-are-better-in-the-us/ Accessed March 5, 2024.
- 11. KFF . Medicaid Coverage Rates for the Nonelderly by Race/Ethnicity. State Health Facts. https://www.kff.org/a873cc0/. Accessed May 15, 2023.
- 12. Valenzuela C, Osterman JKM. Characteristics of Mothers by Source of Payment for the Delivery: United States, 2021. National Center for Health Statistics (U.S.); 2023. doi: 10.15620/cdc:127266 [DOI] [PubMed] [Google Scholar]
- 13. Medicaid and CHIP Payment and Access Commission (MACPAC) . Medicaid's Role in Financing Maternity Care. https://www.macpac.gov/wp‐content/uploads/2020/01/Medicaid%E2%80%99s‐Role‐in‐Financing‐Maternity‐Care.pdf. Published January 2020.
- 14. U.S. Centers for Medicare & Medicaid Services . Health coverage for lawfully present immigrants. HealthCare.gov. https://www.healthcare.gov/immigrants/lawfully-present-immigrants/. Accessed May 17, 2023.
- 15. Livingston G. Hispanic women no longer account for the majority of immigrant births in the U.S. Pew Research Center August 2019. https://pewrsr.ch/2YzvLa8. Accessed May 17, 2023.
- 16. Brooks T, Gardner A, Osorio A, et al. Medicaid and CHIP Eligibility and Enrollment Policies as of January 2022: Findings from a 50‐State Survey. Kaiser Family Foundation; 2022. [Google Scholar]
- 17. Shulman HB, D'Angelo DV, Harrison L, Smith RA, Warner L. The pregnancy risk assessment monitoring system (PRAMS): overview of design and methodology. Am J Public Health. 2018;108(10):1305‐1313. doi: 10.2105/AJPH.2018.304563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kilpatrick SJ, Papile LA, Macones GA, Watterberg KL. Guidelines for Perinatal Care. 8th ed. American Academy of Pediatrics; 2017. [Google Scholar]
- 19. Centers for Disease Control and Prevention . Planning for Pregnancy. Centers for Disease Control and Prevention. https://www.cdc.gov/preconception/planning.html. Published February 15, 2023. Accessed May 15, 2023.
- 20. Kotelchuck M. An evaluation of the Kessner adequacy of prenatal care index and a proposed adequacy of prenatal care utilization index. Am J Public Health. 1994;84(9):1414‐1420. doi: 10.2105/ajph.84.9.1414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. ACOG Committee opinion No. 736: optimizing postpartum care. Obstet Gynecol. 2018;131(5):e140‐e150. doi: 10.1097/AOG.0000000000002633 [DOI] [PubMed] [Google Scholar]
- 22. National Center for Health Statistics . NCHS Urban Rural Classification Scheme for Counties. https://www.cdc.gov/nchs/data_access/urban_rural.htm. Published June 1, 2017. Accessed May 16, 2023.
- 23. KFF . Status of State Medicaid Expansion Decisions: Interactive Map. Medicaid. https://www.kff.org/734275c/. Published May 8, 2023. Accessed May 16, 2023.
- 24. The Commonwealth Fund . State Policies to Improve Maternal Health Outcomes. https://www.commonwealthfund.org/publications/maps‐and‐interactives/2020/nov/state‐policies‐improve‐maternal‐health‐outcomes. Published November 19, 2020. Accessed May 16, 2023.
- 25. Steenland MW, Fabi RE, Bellerose M, Desir A, White MS, Wherry LR. State public insurance coverage policies and postpartum care among immigrants. JAMA. 2023;330(3):238‐246. doi: 10.1001/jama.2023.10249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pedraza FI, Zhu L. The “chilling effect” of America's new immigration enforcement regime. Pathways. 2015; 1‐5. https://www.immigrationresearch.org/system/files/Chilling_Effects_Public_Charge_Rule.pdf [Google Scholar]
- 27. Sabo S, Lee AE. The spillover of US immigration policy on citizens and permanent residents of Mexican descent: how internalizing “illegality” impacts public health in the borderlands. Front Public Health. 2015;3:155. doi: 10.3389/fpubh.2015.00155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Amuedo‐Dorantes C, Arenas‐Arroyo E, Sevilla A. Immigration enforcement and economic resources of children with likely unauthorized parents. J Public Econ. 2018;158:63‐78. [Google Scholar]
- 29. Passel JS, Cohn D. Unauthorized Immigrant Population: National and State Trends. 2010. 2010.
- 30. Passel JS, Cohn D. A Portrait of Unauthorized Immigrants in the United States. Pew Hispanic Center; 2009. https://www.pewresearch.org/hispanic/2009/04/14/a-portrait-of-unauthorized-immigrants-in-the-united-states/. Accessed March 10, 2024. [Google Scholar]
- 31. Togioka BM, Seligman KM, Delgado CM. Limited English proficiency in the labor and delivery unit. Curr Opin Anaesthesiol. 2022;35(3):285‐291. doi: 10.1097/ACO.0000000000001131 [DOI] [PubMed] [Google Scholar]
- 32. Yeheskel A, Rawal S. Exploring the “patient experience” of individuals with limited English proficiency: a scoping review. J Immigr Minor Health. 2019;21(4):853‐878. doi: 10.1007/s10903-018-0816-4 [DOI] [PubMed] [Google Scholar]
- 33. Himmelstein J, Himmelstein DU, Woolhandler S, et al. Health care spending and use among Hispanic adults with and without limited English proficiency, 1999–2018. Health Affairs (Millwood). 2021;40(7):1126‐1134. doi: 10.1377/hlthaff.2020.02510 [DOI] [PubMed] [Google Scholar]
- 34. Quadri NS, Wilkins S, Krohn K, Mann EM, Stauffer WM, Walker PF. Language justice: addressing linguistic disparities begins with language data collection. Am J Trop Med Hyg. 2023;109(1):1‐3. doi: 10.4269/ajtmh.23-0237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Payton C, Lee J, Noguez Mercado AP, Uliasz A. Language Justice During COVID‐19. American Bar Association. https://www.americanbar.org/groups/young_lawyers/about/initiatives/disaster-legal-services/language-justice-during-covid-19/. Published May 13, 2020. Accessed March 10, 2024.
- 36. Interrante JD, Admon LK, Carroll C, Henning‐Smith C, Chastain P, Kozhimannil KB. Association of Health Insurance, geography, and race and ethnicity with disparities in receipt of recommended postpartum care in the US. JAMA Health Forum. 2022;3(10):e223292. doi: 10.1001/jamahealthforum.2022.3292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rhodes SD, Mann L, Simán FM, et al. The impact of local immigration enforcement policies on the health of immigrant Hispanics/Latinos in the United States. Am J Public Health. 2015;105(2):329‐337. doi: 10.2105/AJPH.2014.302218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Daw JR, Kolenic GE, Dalton VK, et al. Racial and ethnic disparities in perinatal insurance coverage. Obstet Gynecol. 2020;135(4):917‐924. doi: 10.1097/AOG.0000000000003728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Admon LK, Daw JR, Winkelman TNA, et al. Insurance coverage and perinatal health care use among low‐income women in the US, 2015–2017. JAMA Netw Open. 2021;4(1):e2034549. doi: 10.1001/jamanetworkopen.2020.34549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Daw JR, Winkelman TNA, Dalton VK, Kozhimannil KB, Admon LK. Medicaid expansion improved perinatal insurance continuity for low‐income women. Health Affairs (Millwood). 2020;39(9):1531‐1539. doi: 10.1377/hlthaff.2019.01835 [DOI] [PubMed] [Google Scholar]
- 41. Romero M. The inclusion of citizenship status in intersectionality: what immigration raids tells us about mixed status Famiies, the state, and assimilation. Int J Sociol Fam. 2008;34(2):131‐152. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information.


