ABSTRACT
Introduction:
Postpartum depression (PPD) is a form of depression that affects new mothers within the first year after childbirth. PPD can negatively impact both the mother’s quality of life and the child’s development. Untreated PPD can lead to adverse outcomes, such as infant growth retardation, poor child survival, impaired development, and undernutrition. The burden of PPD is a significant public health concern, with a global prevalence increase of 18.4% from 2005 to 2015. Early detection and intervention of PPD can mitigate the severity and chronicity of symptoms.
Aims:
This study aimed to determine the prevalence of PPD among mothers in an urban area of Kolkata and identify any influencing factors.
Materials and Methods:
The study utilized a cross-sectional design, surveying 189 mothers within the postpartum period of 6 weeks to 1 year. Edinburg Postnatal Depression Scale was used to identify possible PPD.
Results:
About 29% of the women had probable PPD, 19% had possible depression, and 15% had no depression. Factors associated with depression included low birth weight and primiparity, while financial independence served as a protective factor. Multinomial regression analysis revealed that low-birth-weight babies, marital conflict, lack of support at home, and primiparity had higher odds of depression, whereas financial independence was a protective factor. Age was not statistically significant.
Conclusion:
A high prevalence of PPD and significant associations with factors emphasized the importance of screening all mothers for PPD, providing medical care and counselling, and ensuring acceptance and support from partners, family, and society.
Keywords: Depression, Edinburgh Postnatal Depression Scale, marital conflict, newborn, primipara
Background
Postpartum depression (PPD) is a ‘thief that steals motherhood.’ It is defined as nonpsychotic depressive episode of mild to moderate severity beginning in or extending into the first postnatal year.[1] It usually begins within 1–12 months after delivery. Symptoms of PPD are similar to those in women with depression unrelated to childbirth.[2] Usually it appears from 3 months to up to 12 months after delivery.[3] When mothers experience severe or chronic symptoms of PPD, their infants are at a higher risk of negative developmental outcomes.[4,5] Postnatal depression increases maternal morbidity, social problems, and physical damage and may lead to suicide.[6] Similarly, there is a strong relationship between maternal well-being and child development.[7] If left untreated, PPD can result in negative outcomes such as infant growth retardation, impaired child development, poor child survival, behavioural changes, repeated diarrheal disease, and undernutrition. Additionally, PPD can also impact the quality of life of postnatal mothers.[8] The burden of PPD is a significant public health concern in low- and middle-income countries.[9] According to the World Health Organization (WHO) 2017 report, more than 322 million people had depression and of this about 29.9 million (9%) were in Africa.[10] Globally, the prevalence of PPD increased by 18.4% in the year from 2005 to 2015.[11] A prevalence of 19.8% was reported in a systematic review conducted in 17 low- and middle-income countries.[12] The well-being of a mother’s mental health is crucial for the proper growth and well-being of her child. Mental health issues like depression are prevalent during the antenatal and postnatal periods, with approximately one in three to one in five women in developing countries, and one in ten women in developed countries experiencing significant mental health problems during pregnancy and after giving birth.[13] The effects of postnatal depression on the mother, her married life, and her children make it an important condition to diagnose, treat, and prevent.[14] The WHO has launched the Mental Health Gap Action Program aimed at integrating mental health interventions with the existing maternal health services.[15] Early intervention for PPD and anxiety can help decrease the severity and duration of symptoms, and prevent negative effects on the health and development of the child. Understanding the factors that increase the risk of developing PPD and anxiety can aid in early detection. These risk factors may be present prior to pregnancy, during pregnancy, or after childbirth, providing healthcare professionals with opportunities to mitigate them at different stages and prevent the onset of depression and/or anxiety in mothers.
Against this backdrop this study was aimed to find out the prevalence of PPD among mothers and the factors influencing it if any in an urban area of Kolkata, West Bengal.
Materials and Methods
A community-based cross-sectional descriptive study was conducted in seven wards (56–59 and 63–67) of Borough VII under Kolkata Municipal Corporation from December 2022 to February 2023. Borough VII is the urban field practice area of Community Medicine Department, Calcutta National Medical College, Kolkata. Before starting data collection ethical approval was taken from the institutional ethics committee.
Inclusion criteria
Mothers in the postpartum period of 6 weeks to 1 year and who gave consent for data collection were included in the study.
Exclusion criteria
Mothers who had a pre-existing psychiatric disorder and were seriously ill at the time of the interview were excluded from the study.
Data were collected from the study subjects using a predesigned, pretested, and semistructured schedule. Assuming prevalence[16] of PPD in urban areas of 31.3%, design effect 2, 10% absolute error, and 10% nonresponse rate, the sample size was 189. Postnatal register of each ward of Borough VII belonging to Urban Health Centre was reviewed and mothers in between 6 weeks to 1 year of postpartum age were narrowed down. Using a simple random sampling technique 21 mothers from each ward were interviewed. Edinburg Postnatal Depression Scale (EPDS)[17] was used to determine possible PPD among mothers. Modified B. G. Prasad Socioeconomic Scale, 2022[18] was used to determine the socioeconomic status of the students.
Edinburg postnatal depression scale
EPDS is a valuable and efficient way of identifying mothers at risk for “perinatal” depression. It is easy to administer and has proven to be an effective screening tool. It consists of 10 questions about how the mother had felt during the previous week. The maximum possible score is 30. A score of 10 or more suggests the presence of possible depression and scores above 13 are likely to be suffering from a depressive illness of varying severity.
Statistical analysis
Data entry and analysis were done in Statistical Package for Social Sciences version 16.0. Frequency distribution tables were used for descriptive statistics. Multinominal logistic regression was used to assess factors influencing PPD considering significance level at 5%.
Results
Among the 189 postnatal women, most of the women were below 26 years of age (55%). The majority of the women followed Islam (60.4%) and came from nuclear families (59.3%). Though we observed that 87% of women belonged to the upper socioeconomic class (Classes I and II) according to Modified B.G. Prasad Scale, we also found that 87% of women were homemakers. A substantial portion (48.1%) of women had education above the higher secondary level [Table 1].
Table 1.
Distribution of study population according to sociodemographic variables (n=189)
| Variable | Frequency | Percentage |
|---|---|---|
| Age (years) | ||
| ≤26 | 104 | 55 |
| >26 | 85 | 45 |
| Religion | ||
| Hindu | 75 | 39.6 |
| Muslim | 114 | 60.4 |
| Type of family | ||
| Joint | 77 | 40.7 |
| Nuclear | 112 | 59.3 |
| Socioeconomic status | ||
| Upper (Classes I, II) | 78 | 87 |
| Lower (Classes III, IV, V) | 111 | 12 |
| Education | ||
| Illiterate | 03 | 1.6 |
| Upper primary | 33 | 17.5 |
| Higher secondary | 62 | 32.8 |
| Above higher secondary | 91 | 48.1 |
| Occupation | ||
| Homemaker | 165 | 87 |
| Employed | 24 | 12 |
We employed the EPDS to find the probable PPD amongst the women studied and 29% had scores above 13 which indicated probable PPD. There were 15% of women who had no PPD and 19% had possible PPD [Diagram 1].
Diagram 1.
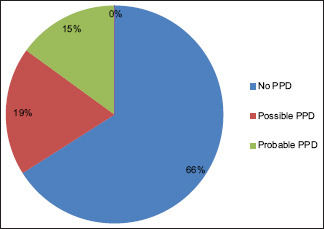
Pie diagram showing the distribution of postpartum depression as per EPDS score (n = 189)
When we tried to explore the relationship of women having possible or probable PPD, we found no significant association with age, family type, and education or addiction pattern of mothers. However, significant association of EPDS scores above 9 was found with financial independence (χ2 = 5.60, P = 0.01), marital conflict (χ2 = 12.03, P < 0.001) and supportive environment at home in the PPD (χ2 = 7.61, P = 0.005) [Table 2].
Table 2.
Association of severity of postpartum depression with sociodemographic variables (n=189)
| Variable | EPDS ≤9 | EPDS >9 | Total | Significance |
|---|---|---|---|---|
| Age (years) | ||||
| ≤26 | 69 (66.3) | 35 (33.7) | 104 (100) | χ2=0.04, P=0.94 |
| >26 | 56 (65.9) | 29 (34.1) | 85 (100) | |
| Type of family | ||||
| Joint | 49 (63.6) | 28 (36.4) | 77 (100) | χ2=3.04, P=0.08 |
| Nuclear | 76 (67.9) | 36 (32.1) | 112 (100) | |
| Socioeconomic status | ||||
| Upper (Classes I, II) | 46 (59.0) | 32 (41.0) | 78 (100) | χ2=0.96, P=0.32 |
| Lower (Classes III, IV, V) | 79 (71.2) | 32 (28.8) | 112 (100) | |
| Education | ||||
| Below higher secondary | 68 (69.4) | 30 (30.6) | 98 (100) | χ2=0.27, P=0.60 |
| Higher secondary and above | 57 (62.7) | 34 (37.3) | 91 (100) | |
| Addiction | ||||
| Present | 12 (54.5) | 10 (45.5) | 22 (100) | χ2=1.21, P=0.22 |
| Absent | 113 (67.6) | 54 (32.3) | 167 (100) | |
| Financial independence | ||||
| Present | 21 (87.5) | 3 (12.5) | 24 (100) | χ2=5.60, P=0.01 |
| Absent | 104 (63.1) | 61 (36.9) | 165 (100) | |
| Marital conflict | ||||
| Present | 45 (52.9) | 40 (47.1) | 85 (100) | χ2=12.03, P<0.001 |
| Absent | 80 (76.9) | 24 (23.1) | 104 (100) | |
| Supportive environment during the postpartum period | ||||
| Present | 70 (83.3) | 14 (16.6) | 84 (100) | χ2=7.61, P=0.005 |
| Absent | 55 (64.7) | 30 (35.3) | 85 (100) |
The various maternal and newborn factors which could be possibly related to PPD were also studied. We found that low birth weight (<2.5 kg) was significantly associated with possible and probable PPD (χ2 = 10.8, P = 0.001). Similarly, being primipara was also significantly associated with possible and probable PPD (χ2 = 18.18, P < 0.001) [Table 3].
Table 3.
Association of severity of postpartum depression with maternal and newborn factors (n=189)
| Variable | EPDS ≤9 | EPDS >9 | Total | Significance |
|---|---|---|---|---|
| Birth weight | ||||
| Low birth weight | 27 (39.8) | 41 (60.2) | 68 (100) | χ2=10.8, P=0.001 |
| Normal birth weight | 78 (64.5) | 43 (35.5) | 121 (100) | |
| Newborn complication | ||||
| Present | 45 (59.2) | 31 (40.8) | 76 (100) | χ2=2.72, P=0.09 |
| Absent | 80 (70.8) | 33 (29.2) | 113 (100) | |
| Antenatal complication | ||||
| Present | 47 (70.1) | 20 (29.8) | 67 (100) | χ2=0.16, P=0.68 |
| Absent | 89 (72.9) | 33 (27.1) | 122 (100) | |
| Postpartum complication | ||||
| Present | 25 (78.1) | 7 (21.9) | 32 (100) | χ2=0.39, P=0.53 |
| Absent | 130 (82.8) | 27 (17.2) | 157 (100) | |
| Parity | ||||
| Primipara | 22 (42.3) | 30 (57.7) | 52 (100) | χ2=18.18, P<0.001 |
| Multipara | 103 (75.1) | 34 (24.9) | 137 (100) |
For the multinomial regression model, we classified mothers into two groups that have EPDS score ≤9 (no depression) and EPDS score >9 (possible and probable depression). The goodness of fit for the model was R2 = 0.64.
In the multinomial regression we found that women of age above 26 years had greater chances of having PPD; however, this was not statistically significant. The regression analysis showed that mothers with low-birth-weight babies had 4.22 times more chances of having PPD and this was statistically significant. Mothers with marital conflict had an adjusted odds ratio of 3.54 which was found to be statistically significant. Women who had no support at home during the postpartum period were 3.64 times more likely to have PPD than those who had a supportive environment at home. Primiparas were 3.10 times more likely to have PPD than multipara as per the multinomial regression model. Being financially independent was found to be a statistically significant protective factor with 0.41 odds of having PPD than their dependent counterparts [Table 4].
Table 4.
Logistic regression for association of postpartum depression with different factors (n=189)
| Variable | Constant | Wald | df | P | AOR | 95% CI for Exp(B) |
|---|---|---|---|---|---|---|
| Age (>26) | 0.252 | 0.352 | 1 | 0.55 | 1.2 | 0.98–2.81 |
| Addiction | −0.652 | 0.108 | 1 | 0.74 | 0.74 | 0.42–3.75 |
| Financial independence | −0.982 | 0.213 | 1 | 0.04 | 0.41* | 0.32–0.82 |
| Marital conflict | 0.841 | 9.71 | 1 | <0.001 | 3.54* | 1.69–5.78 |
| Absence of a supportive environment | 0.913 | 9.82 | 1 | <0.001 | 3.61* | 1.81–6.84 |
| Low birth weight | 1.447 | 12.33 | 1 | <0.001 | 4.22* | 1.91–9.47 |
| Newborn complication | 0.476 | 0.513 | 1 | 0.47 | 1.7 | 0.61–6.42 |
| Antenatal complication | 0.721 | 5.93 | 1 | 0.14 | 1.10 | 0.37–4.92 |
| Postnatal complication | 0.827 | 8.22 | 1 | 0.41 | 1.13 | 0.84–3.79 |
| Primipara | 0.95 | 10.11 | 1 | <0.001 | 3.10* | 1.52–6.32 |
*Statistically significant (p<0.05). AOR= Adjusted Odds Ratio
Discussion
PPD is a pressing problem in the public health context. Most studies that have been done in this regard were hospital or clinic based.[19] Our study was a community-based study in Kolkata, West Bengal.
In our study, we found that 29% of women had probable PPD (EPDS >13). This is similar to the study done by Neelakanthi et al.[16] which showed that 31.3% of women had PPD. The study conducted by Patel et al.[20] found the prevalence of PPD to be 48.5%. This high prevalence was probably due to the fact that they took the cut off to be 10.5 in the EPDS, which is lower than our cut off.
In our study, we conducted a multinomial regression with important factors related to PPD. We categorized women with a score <9 (no depression) and score ≥9 (possible and probable PPD) as two groups for this regression analysis. Our analysis showed that maternal age above 26 years had 1.2 times greater odds of having PPD though it was not statistically significant. In a meta-analysis by Upadhyay et al.,[21] four studies have reported high maternal age as a risk factor, though the final pooled analysis did not show any significant difference between high or low maternal age. When we look into global data we find that the risk of PPD shows a U-shaped curve where the risk appears to be high for women below 24 years, then again decreases between 24 and 35 years and shows an increasing trend above 35 years.[22]
In our study, the presence of postnatal complications had 1.13 times higher odds of having PPD. However, this was not found to be statistically significant. Similarly, the presence of complications during the antenatal period showed the odds of developing PPD to be 1.10, which was again not statistically significant. In the study conducted by Neelakanthi et al.,[16] pregnancy complications showed an odd of 1.60 which, however, was not statistically significant. Obstetric complications and comorbidities during pregnancy were also found to be important risk factors for PPD by Upadhyay et al.[21]
The multinomial regression model showed that mothers with low-birth-weight babies had 4.22 times more chances of developing PPD and this was also statistically significant. Similar results were seen in a study done by Helle et al.[23] where low birth weight was a significant risk factor for PPD.
Our study also showed that mothers with financial independence were an important determinant and mothers who were financially independent had 0.41 times less odds of developing PPD. A similar finding is seen in a study by Modi et al.[24] where financial dependence was a significant factor in mothers suffering from PPD. Financially independent women experience more freedom to make choices both for themselves and their babies; this might be the reason that they suffer less from PPD.
The multinomial regression revealed two important parameters that are marital conflict and the absence of a supportive environment at home both of which had significant associations with PPD. Mothers with marital conflict had 3.54 times odds of being depressed in the postpartum period. This resonates with the findings from a study by Faisal-Cury et al.[25] where partner relationship quality was significantly associated with PPD. A woman who has no marital conflict and is in sync with her partner feels more secure and is well equipped to handle the challenges of motherhood, probably that is the reason that marital conflict is such an important determinant of PPD.
In our study, mothers who had no supportive environment at home had an adjusted odds ratio of 3.64; i.e. they were 3.64 times more likely to develop PPD. Robertson and Beck also concluded from their study that inadequate social support is linked to depression in mothers during pregnancy and the postpartum period.[26] A good emotionally supportive environment is paramount for a postpartum woman to overcome her physical and mental exhaustion and not let her slip into depression.
In our study, we also found primipara women with odds of 3.10 times of having PPD than multipara women. A study conducted by Martínez-Galiano et al.[27] also showed primiparous women had more mental health-related problems like anxiety and depression in the postpartum period. A plausible reason for such an occurrence could be that multiparous women can handle their emotions better since they have been through the experience once. Hence, they can understand their problems and address those issues with previous experience.
The prevalence of PPD was quite substantial in the population studied. From our study, we can conclude that PPD is a relevant public health problem and is significantly associated with factors like low-birth-weight baby, parity, marital conflict, financial dependence, and a supportive environment at home. It is important that all mothers are screened for signs of PPD and are provided with prompt medical care and counselling. Mothers need to be accepted and loved by their partners, family members, and society at large.
Limitations
The study was constrained by its focus on a single community, limiting its ability to generalize findings to the wider population. Conducting larger studies that encompass both urban and rural areas would be necessary to address this limitation. Additionally, the study was constrained by a limited time frame and the women could not be tracked to see whether they developed any severe symptoms or postpartum psychosis in future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors sincerely thank all the participants and authorities for conducting the study.
References
- 1.Beck CT. Postpartum depression: It isn't just the blues. Am J Nurs. 2006;106:40–50. doi: 10.1097/00000446-200605000-00020. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Report of the WHO Meeting. Geneva: World Health Organization; 2008. Maternal Mental Health and Child Health and Development in Low and Middle Income Countries. [Google Scholar]
- 3.Abdollahi F, Rezai Abhari F, Zarghami M. Post-partum depression effect on child health and development. Acta Med Iran. 2017;55:109–14. [PubMed] [Google Scholar]
- 4.Netsi E, Pearson RM, Murray L, Cooper P, Craske MG, Stein A. Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry. 2018;75:247–53. doi: 10.1001/jamapsychiatry.2017.4363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Waerden J, Galera C, Larroque B, Saurel-Cubizolles MJ, Sutter-Dallay AL, Melchior M EDEN Mother–Child Cohort Study Group. Maternal depression trajectories and children's behavior at age 5 years. J Pediatr. 2015;166:1440–8.e1. doi: 10.1016/j.jpeds.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Antelman G, Kaaya S, Wei R, Mbwambo J, Msamanga GI, Fawzi WW, et al. Depressive symptoms increase risk of HIV disease progression and mortality among women in Tanzania. JAIDS J Acquir Immune Defic Syndr. 2007;44:470–7. doi: 10.1097/QAI.0b013e31802f1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Black MM, Surkan PJ. Child development and maternal wellbeing: Family perspectives for low-income and middle-income countries. Lancet Glob Health. 2015;3:e426–7. doi: 10.1016/S2214-109X(15)00084-4. [DOI] [PubMed] [Google Scholar]
- 8.Bener A, Burgut FT, Ghuloum S, Sheikh J. A study of postpartum depression in a fast developing country: Prevalence and related factors. Int J Psychiatry Med. 2012;43:325–37. doi: 10.2190/PM.43.4.c. [DOI] [PubMed] [Google Scholar]
- 9.Gelaye B, Rondon M, Araya R, Williams MA. Epidemiology of maternal depression, risk factors and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3:973–82. doi: 10.1016/S2215-0366(16)30284-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. World Health Organization. 2017 [Google Scholar]
- 11.Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England) 2016;388:1545–602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bull World Health Organ. 2012;90:139–49H. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agrati D, Lonsteinb J. Affective changes during the postpartum period: Influences of genetic and experiential factors. Horm Behav. 2016;77:141–52. doi: 10.1016/j.yhbeh.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 14.Robinson GE, Stewart DE. Postpartum disorders. In: Stotland NL, Stewart DE, editors. Psychological Aspects of Women's Health Care. 2nd ed. Washington, DC: American Psychiatric Press, Inc.; 2001. pp. 117–39. [Google Scholar]
- 15.WHO Guidelines Approved by the Guidelines Review Committee. mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings: Mental Health Gap Action Programme (mhGAP) Geneva: World Health Organization World Health Organization; 2010. [PubMed] [Google Scholar]
- 16.Neelakanthi A, Venkatesh S, Babu D, Nachiketha SRR, Gopalakrishnan U. Prevalence and risk factors of depressive symptoms in postpartum period: A cross-sectional study. Perinatology. 2021;21:166–73. [Google Scholar]
- 17.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 18.Majhi MM, Bhatnagar N. Updated B. G Prasad's classification for the year 2021: Consideration for new base year 2016. J Family Med Prim Care. 2021;10:4318–9. doi: 10.4103/jfmpc.jfmpc_987_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poçan AG, Aki OE, Parlakgümüs AH, Gereklioglu C, Dolgun AB. The incidence of and risk factors for postpartum depression at an urban maternity clinic in Turkey. Int J Psychiatry Med. 2013;46:179–94. doi: 10.2190/PM.46.2.e. [DOI] [PubMed] [Google Scholar]
- 20.Patel HL, Ganjiwale JD, Nimbalkar AS, Vani SN, Vasa RK, Nimbalkar SM. Characteristics of postpartum depression in Anand District, Gujarat, India. J Trop Pediatr. 2015;61:364–9. doi: 10.1093/tropej/fmv046. [DOI] [PubMed] [Google Scholar]
- 21.Upadhyay RP, Chowdhury R, Salehi A, Sarkar K, Singh SK, Sinha B, et al. Postpartum depression in India: A systematic review and meta-analysis. Bull World Health Organ. 2017;95:706–17. doi: 10.2471/BLT.17.192237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guintivano J, Manuck T, Meltzer-Brody S. Predictors of postpartum depression: A comprehensive review of the last decade of evidence. Clin Obstet Gynecol. 2018;61:591–603. doi: 10.1097/GRF.0000000000000368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Helle N, Barkmann C, Bartz-Seel J, Diehl T, Ehrhardt S, Hendel A, et al. Very low birth-weight as a risk factor for postpartum depression four to six weeks post birth in mothers and fathers: Cross-sectional results from a controlled multicentre cohort study. J Affect Disord. 2015;180:154–61. doi: 10.1016/j.jad.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 24.Modi VP, Parikh MN, Valipay SK. Prevalence of postpartum depression and correlation with risk factors. Ann Indian Psychiatry. 2018;2:27–32. [Google Scholar]
- 25.Faisal-Cury A, Tabb K, Matijasevich A. Partner relationship quality predicts later postpartum depression independently of the chronicity of depressive symptoms. Braz J Psychiatry. 2021;43:12–21. doi: 10.1590/1516-4446-2019-0764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: A synthesis of recent literature. Gen Hosp Psychiatry. 2004;26:289–95. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 27.Martínez-Galiano JM, Hernández-Martínez A, Rodríguez-Almagro J, Delgado-Rodríguez M, Gómez-Salgado J. Relationship between parity and the problems that appear in the postpartum period. Sci Rep. 2019;9:11763. doi: 10.1038/s41598-019-47881-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


