Abstract
Oral squamous cell carcinoma (OSCC) is the most common of all head and neck cancers accounting for 90% of all oral malignancies. It is commonly associated with the use of tobacco smoking or quid form. The incidence of oral carcinoma is higher in males than females with a ratio of 1.4:1, though females commonly adopt tobacco quid chewing habit. OSCC metastasis to cervical lymph node at the rate of 20-42.6% according to studies reported so far. Papillary thyroid carcinoma (PTC) occurs with a higher incidence in females than males with metastasis into cervical lymph nodes though the primary lesion frequently goes undetected. Concurrent metastasis of OSCC and PTC to the cervical lymph node during neck dissection has been reported rarely in the literature. This case report presents a 48-year-old female with lymph node metastasis of carcinoma of the right mandibular posterior alveolar region concurrently with metastasis of PTC (with primary lesion clinically undetected) encountered during cervical lymph node examination.
Keywords: lymph node metastasis, metastatic thyroid carcinoma, head and neck squamous cell carcinoma, papillary thyroid carcinoma, follicular type papillary thyroid carcinoma (ptc), poorly differentiated squamous cell carcinoma
Introduction
In the adult population, at least 1% of individuals carry metastatic malignant neoplasms within their cervical lymph nodes. Notably, among patients with head and neck neoplasms, approximately 0.7% exhibit lymph nodes that house clinically occult but histologically malignant metastatic thyroid carcinomas [1]. The literature has documented approximately 49 cases of coexisting head and neck squamous cell carcinoma (HNSCC) and papillary thyroid carcinoma (PTC) [1]. PTC nodal metastasis is relatively common, with an occurrence rate of 1-10% in the population, as indicated by autopsy studies showing an incidence ranging from 6% to 35% [2]. Oral squamous cell carcinoma (OSCC) accounts for nearly 90% of malignant carcinomas arising from the oral mucosa region with a tendency to metastasize to cervical lymph nodes [3]. In patients with HNSCC, the co-incidental detection of secondary tumors like differentiated thyroid carcinoma within the cervical lymph nodes is rare [4]. This case report highlights a case of a female patient who presented with carcinoma of the right vestibular region with co-incidental nodal metastasis during lymph node examination following neck dissection.
Case presentation
A 48-year-old female patient presented with pain and swelling in the right lower back tooth region for the past 10 days. One month back, the patient felt pain in the right lower back tooth region for which she underwent 45 extractions, after which she developed a painful growth in that region. She had no relevant medical or previous surgical history.
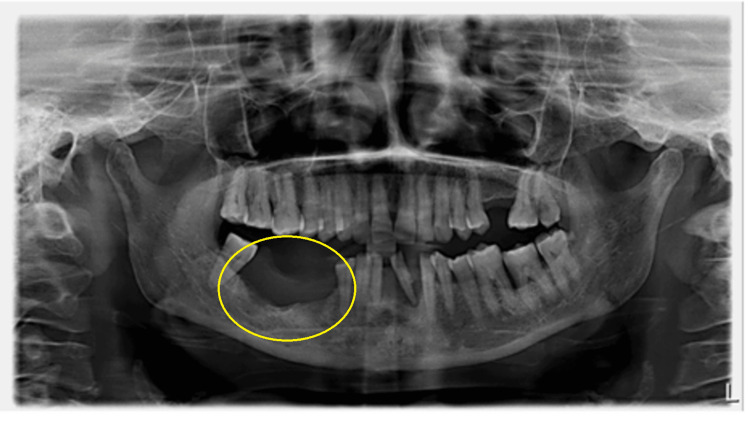
On extraoral examination, gross facial asymmetry was seen due to diffuse swelling in relation to the body of the mandible; on palpation, the swelling was hard in consistency and non-tender. A proliferative growth of size 3x2 cm was noticed in the alveolus of teeth 45, 46, and 47 with irregular surface, ulceration, and induration (Figure 1). An orthopantomogram (OPG) radiographic image showed radiolucency with a sclerotic border in the right lower mandible (Figure 2).
Figure 1. Proliferative growth in the right lower posterior alveolar mucosa of the 45, 46, and 47 regions.
Figure 2. Orthopantomogram (OPG) showing radiolucency involving the right mandible edentulous area of 45, 46, and 47.
A CT examination revealed a heterogeneous lesion involving the vestibular mucosa near the right lower third molar region, extending and infiltrating the body of the right hemimandible and adjacent soft tissue. A provisional diagnosis of carcinoma of the posterior alveolar mandible was made. An incisional biopsy was performed and histopathologically was diagnosed as poorly differentiated OSCC (PDSCC).
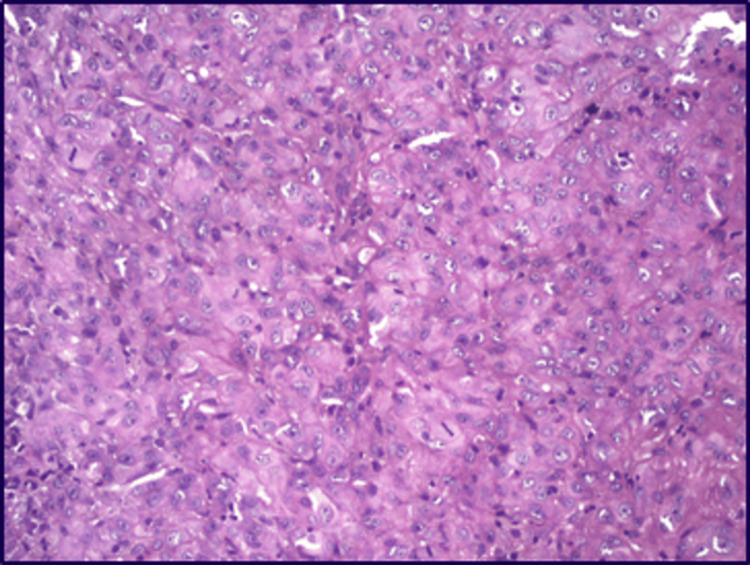
The patient underwent a wide local excision with segmental mandibulectomy along with right radical neck dissection suspecting nodal metastasis. On histopathologic analysis, the sections of the soft tissue specimen revealed dysplastic surface stratified squamous epithelium with groups and loosely dispersed tumour cells invading most of the underlying fibro-cellular connective tissue with dispersed blood vessels and inflammatory cells (Figure 3). Sheets of tumour cells are seen invading the deeper areas involving muscles and around the nerves (perineural invasion). Focal areas of necrosis/myxoid degeneration were also seen.
Figure 3. Histopathological image showing poorly differentiated oral squamous cell carcinoma.
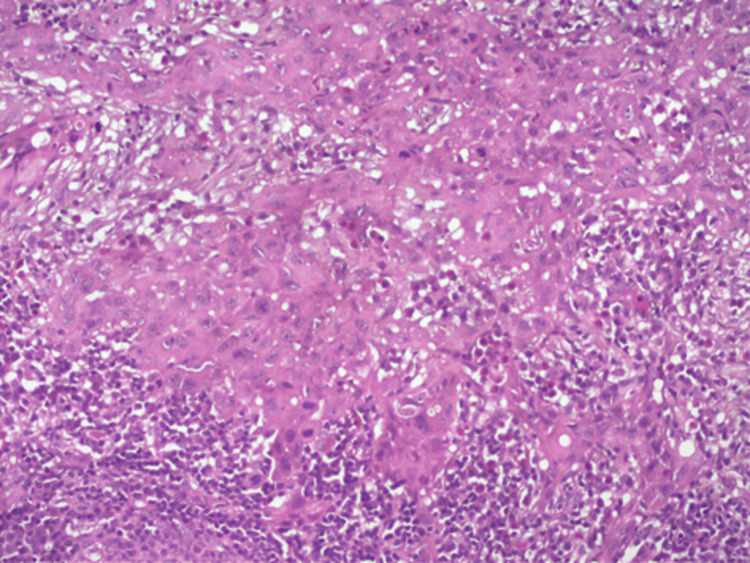
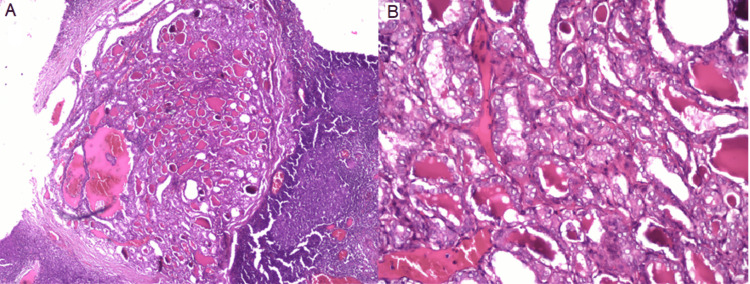
Histopathological examination revealed four metastatic positive nodes out of 21 harvested ipsilateral lymph nodes (Figure 4). One node in levels III, IV, and V showed loss of the capsule with proliferating cells in a papillary fashion, displaying a nucleus with marginal chromatin and a bland centre, resembling Orphan Annie-eye clear nuclei. In some regions, cells were seen lining the central area showing an eosinophilic colloidal substance overall resembling thyroid tissue (Figure 5).
Figure 4. Histopathological image showing nodal invasion of tumour cells.
Figure 5. Metastatic papillary thyroid carcinoma in cervical lymph nodes (A: 10x, B: 20x).
The other cortical and paracortical regions of the lymph node show lymphoid follicles, large blood vessels, adipose tissues, areas of haemorrhage, and extensive infiltration of metastatic thyroid carcinoma cells, which display classic papillary architecture (follicular type) in lymph nodes of III, IV, and V levels. Following histopathological reporting, the patient was referred for a CT scan investigation and the primary thyroid tumour was surgically excised.
Discussion
Cervical nodal metastasis accompanies nearly 50% of patients diagnosed with squamous cell carcinoma in the head and neck region [5]. The incidental finding of metastatic thyroid carcinoma in cervical lymph nodes during neck dissection for HNSCC has a reported prevalence rate of 0.3% to 1.6% according to the literature [6]. An incidental identification of metastatic PTC, during neck dissection, is considered rare, with an estimated incidence of less than 0.5% according to studies. Distinct histological changes in cervical lymph nodes raise concern for malignant metastases from primary tumours like those of the oesophagus, breast, stomach, lung, prostate, head-neck, and thyroid [7].
Cervical metastases are reported in approximately 50% of small PTC tumours and 75% of larger ones. In the case of our patient, the incidental finding of PTC metastasis in a cervical lymph node during the evaluation of OSCC raises important considerations. The lymph nodes most frequently affected by metastatic thyroid carcinoma are those at levels II, III, and IV, similar to our case [8]. Therefore, comprehensive sampling and meticulous examination of all specimens are imperative for an accurate diagnosis. The identification of PTC in this context underscores the necessity of a multidisciplinary approach involving otolaryngologists, oncologists, pathologists and endocrinologists to guide appropriate treatment strategies and optimize prognostic outcomes [9].
To the best of our knowledge, approximately 49 cases of coexistent HNSCC and PTC have been described in the literature [7]. Butler et al. reported that up to 3% of patients with head and neck cancer may have clinically undetected thyroid cancer [10]. Périé et al. recommended computed tomography and/or ultrasound examination of the neck and thyroid to look for a primary thyroid tumour during follow-up [11]. Despite variations in histological characteristics of thyroid tissue involvement, the prognosis remains favourable, with a reported 10-year survival rate exceeding 90%, and metastasis does not significantly impact overall outcomes, although older patients may face elevated risks, as suggested by existing literature [4]. Gerard-Marchant et al. describe benign thyroid inclusions as small clusters of histologically normal thyroid follicles within lateral cervical lymph nodes. While typically benign, they have a 0.03% incidence of potentially undergoing malignant transformation [12]. Accidentally discovered metastatic thyroid lesions in lymph nodes are less significant compared to more aggressive primary squamous cell tumours. Therefore, greater focus should be directed towards managing the primary tumour [13]. In our follow-up of the case, we are encouraged to report no evidence of recurrence of both OSCC and PTC in the past six months, indicating a favourable prognosis despite the initial discovery of metastases of thyroid carcinoma during neck dissection for HNSCC. Previous reports have similarly highlighted promising outcomes in such cases. Close surveillance and long-term follow-up are imperative to monitor for disease recurrence or metastasis from the primary tumour [14].
Conclusions
This unique case underscores the importance of thorough evaluation and multidisciplinary collaboration in managing patients with concurrent malignancies. Clinicians should maintain a high index of suspicion for synchronous tumours, especially when dealing with cervical lymph node metastases. The coexistence of OSCC and incidental PTC in cervical lymph nodes necessitates vigilant diagnostic approaches and tailored treatment strategies.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Adhithya Baskaran, Shamala Ravikumar, Kokila Sivakumar, Janani Ilango, Radhika Chelliah
Acquisition, analysis, or interpretation of data: Adhithya Baskaran, Shamala Ravikumar, Kokila Sivakumar, Janani Ilango, Radhika Chelliah
Drafting of the manuscript: Adhithya Baskaran, Shamala Ravikumar, Kokila Sivakumar, Janani Ilango, Radhika Chelliah
Critical review of the manuscript for important intellectual content: Adhithya Baskaran, Shamala Ravikumar, Kokila Sivakumar, Janani Ilango, Radhika Chelliah
References
- 1.Simultaneous metastases of papillary thyroid carcinoma and oral squamous cell carcinoma in the cervical lymph nodes of neck dissection specimens. Chen CY, Tseng CH, Hsu CW, Chen YK. J Dent Sci. 2024;19:717–719. doi: 10.1016/j.jds.2023.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collision metastasis of squamous carcinoma of the oral tongue and incidental thyroid papillary carcinoma to a single cervical lymph node. Lim YC, Kim WS, Choi EC. Int J Oral Maxillofac Surg. 2008;37:494–496. doi: 10.1016/j.ijom.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 3.Expression of matrix metalloproteinase-21 in oral squamous cell carcinoma. Baskaran A, Santhadevy A, Vezhavendhan N, Sivaramakrishnan M, Santhanam VL, Suganya R. Cureus. 2023;15:0. doi: 10.7759/cureus.34256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Papillary thyroid carcinoma coexistent with oral squamous cell carcinoma: a case report and review of literature. Jaafari-Ashkavandi Z, Danesteh H, Keshvari H. J Dent (Shiraz) 2019;20:215–219. doi: 10.30476/DENTJODS.2019.44901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The prevalence and significance of clinically unsuspected neoplasms in cervical lymph nodes. Ansari-Lari MA, Westra WH. Head Neck. 2003;25:841–847. doi: 10.1002/hed.10304. [DOI] [PubMed] [Google Scholar]
- 6.Incidental nodal metastasis of differentiated thyroid carcinoma in neck dissection specimens from head and neck cancer patients. Lenzi R, Marchetti M, Muscatello L. J Laryngol Otol. 2017;131:368–371. doi: 10.1017/S002221511700024X. [DOI] [PubMed] [Google Scholar]
- 7.Incidental cervical lymph node metastasis of papillary thyroid cancer in neck dissection specimens from a tongue squamous cell carcinoma patient: a case report. Ishibashi-Kanno N, Yamagata K, Fukuzawa S, Uchida F, Yanagawa T, Bukawa H. Oral Maxillofac Surg. 2021;25:127–132. doi: 10.1007/s10006-020-00894-z. [DOI] [PubMed] [Google Scholar]
- 8.Significance and management of thyroid lesions in lymph nodes as an incidental finding during neck dissection. Fliegelman LJ, Genden EM, Brandwein M, Mechanick J, Urken ML. Head Neck. 2001;23:885–891. doi: 10.1002/hed.1128. [DOI] [PubMed] [Google Scholar]
- 9.Pediatric thyroid cancer. Diercks G, Bauer AJ, Rastatter J, Kazahaya K, Parikh S. Surgery of the Thyroid and Parathyroid Gland. 2021:255–263. [Google Scholar]
- 10.Significance of thyroid tissue in lymph nodes associated with carcinoma of the head, neck or lung. Butler JJ, Tulinius H, Ibanez ML, Ballantyne AJ, Clark RL. Cancer. 1967;20:1–103. doi: 10.1002/1097-0142(1967)20:1<103::aid-cncr2820200116>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 11.Incidental cervical metastases from thyroid carcinoma during neck dissection. Périé S, Torti F, Lefevre M, Chabbert-Buffet N, Jafari A, Lacau St Guily J. Eur Ann Otorhinolaryngol Head Neck Dis. 2016;133:383–386. doi: 10.1016/j.anorl.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 12.Thyroid follicle inclusions in cervical lymph nodes. Gerard-Marchant R. https://pubmed.ncbi.nlm.nih.gov/14130049/ Arch Pathol. 1964;77:633–637. [PubMed] [Google Scholar]
- 13.Metastatic papillary carcinoma thyroid co-existing with oral cavity squamous cell carcinoma: a case report and review of literature. Verma RK, Tripathi N, Aggarwal P, Panda NK. Egypt J Ear Nose Throat Allied Sci. 2014;15:125–128. [Google Scholar]
- 14.Coexistence of gastrointestinal stromal tumours (GIST) and malignant neoplasms of different origin: prognostic implications. Vassos N, Agaimy A, Hohenberger W, Croner RS. Int J Surg. 2014;12:371–377. doi: 10.1016/j.ijsu.2014.03.004. [DOI] [PubMed] [Google Scholar]